Abstract
In 2017, the Food and Drug Administration (FDA) approved valbenazine and deutetrabenazine, two vesicular monoamine transporter 2 (VMAT2) inhibitors, as treatments for tardive dyskinesia (TD). Additionally, some trials have suggested that vitamin E may benefit TD patients. However, the mechanistic basis for these treatments remains unclear. The objective of this study was to analyze and compare the mechanisms of valbenazine, deutetrabenazine, and vitamin E in TD treatment utilizing network pharmacology and molecular docking approaches. Putative target genes associated with valbenazine, deutetrabenazine, and vitamin E were retrieved from the PharmMapper, CTD, GeneCards, SwissTargetPrediction, and DrugBank databases. TD-related targets were identified using the GeneCards, DisGeNET, OMIM, and TTD databases. A protein-protein interaction (PPI) network was created to identify core targets. Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analyses were conducted via DAVID, and Cytoscape was used to build a drug-pathway-target-disease network. Molecular docking evaluated drug-target interactions. A total of 32, 36, and 62 targets relevant to the treatment of TD were identified for valbenazine, deutetrabenazine, and vitamin E, respectively. PPI and KEGG pathway analyses suggested that valbenazine and deutetrabenazine may influence TD through the dopaminergic synapse signaling pathway via common core targets (e.g., Dopamine Receptor D1 (DRD1), DRD2, Monoamine Oxidase B (MAOB), Solute Carrier Family 6 Member 3 (SLC6A3), SLC18A2) and specific targets (DRD3 for valbenazine, MAOA for deutetrabenazine). Vitamin E may affect TD by targeting the PI3K-Akt pathway through AKT Serine/Threonine Kinase 1 (AKT1), Brain-Derived Neurotrophic Factor (BDNF), Insulin (INS), Nitric Oxide Synthase 3 (NOS3), and Toll-Like Receptor 4 (TLR4). This study provides insights into the common and unique molecular mechanisms by which valbenazine, deutetrabenazine, and vitamin E may treat TD. Pharmacological experiments should be conducted to verify and further explore these results. The findings offer a theoretical basis for further pharmacological investigation and a resource for TD drug screening.
Similar content being viewed by others
Introduction
Tardive dyskinesia (TD) was first described by Faurbye et al. in 19641. TD is characterized by involuntary movements, mainly affecting the orofacial region, but can also involve the trunk and limbs. TD includes three clinical forms: classical TD (orofacial TD), peripheral TD (limb-truncal TD), and respiratory TD2. TD typically arises after exposure to dopamine receptor-blocking agents (DRBAs)3,4. In addition to antipsychotic medications, antiemetic drugs such as metoclopramide5, antidepressants6, and calcium channel blockers such as flunarizine7 are also associated with TD. TD may persist or even worsen after DRBAs are discontinued, often becoming irreversible. This condition imposes significant economic burdens8, social isolation4, work impairment9, reduced quality of life10, and higher mortality rates11. The prevalence of TD is lower with second-generation antipsychotics (21%) compared to that with first-generation antipsychotics (30%)3. The pathophysiology of TD remains unclear but may involve oxidative stress12, dopamine receptor hypersensitivity13, and damage to striatal GABAergic and cholinergic neurons13. Managing TD is challenging due to the unpredictable onset, variable presentation, and the necessity of ongoing DRBA treatment for psychiatric or gastrointestinal disorders.
In 2017, the US Food and Drug Administration (FDA) granted breakthrough therapy designations to valbenazine and deutetrabenazine for treating TD, offering new management options for affected patients. The introduction of these VMAT2 inhibitors has rekindled interest in TD treatment. VMAT2 is a protein that transports monoamine neurotransmitters, including dopamine, serotonin, and norepinephrine, into synaptic vesicles in neurons. Valbenazine, a derivative of tetrabenazine, is gradually released after administration and subsequently metabolized to its active form, (+)-α-dihydrotetrabenazine14,15,16. In contrast, deutetrabenazine is a deuterated form of racemic (+/–) tetrabenazine14,17,18. Recent guidelines and expert opinions recommend both valbenazine and deutetrabenazine as first-line therapies for TD18,19. Vitamin E, an essential lipid-soluble antioxidant, protects cell membranes from oxidative damage20. A recent review suggests vitamin E may prevent the deterioration of TD21. Of these treatments, valbenazine and deutetrabenazine are derived from tetrabenazine, which differs from vitamin E in terms of its pharmacology. The common and distinct mechanisms of action for these three agents in the context of TD treatment warrant further investigation.
Network pharmacology is an emerging field that combines systems biology, biological network analysis, and multi-target drug design to predict how drugs can treat specific diseases22. By constructing “drug-pathway-target-disease” networks, this approach uses large datasets to analyze drug interventions, enhancing the understanding of disease mechanisms and therapeutic strategies. Molecular docking, a common virtual screening method, is used to study interactions between receptors and small molecules. Many studies have employed network pharmacology and molecular docking to explore the molecular mechanisms underlying the therapeutic effects of Western medicines on various diseases23,24.
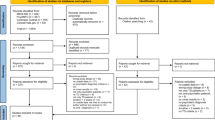
This study utilized integrated database resources to perform a multilevel analysis of valbenazine, deutetrabenazine, and vitamin E. Key methods included target identification, PPI network analysis, GO and KEGG enrichment, and drug-pathway-target-disease network construction, aiming to uncover the shared and distinct molecular mechanisms of these agents in treating TD, as depicted in Fig. 1. By deepening the understanding of TD and its treatment options, this analysis provides a theoretical foundation for developing effective therapies and offers guidance for future advancements in therapeutic strategies.
Methods
Target identification for valbenazine, deutetrabenazine, and vitamin E
The chemical structures of valbenazine, deutetrabenazine, and vitamin E were obtained from the DrugBank database (https://go.drugbank.com)25. Targets for three drugs were predicted using the PharmMapper (http://www.lilab-ecust.cn/pharmmapper/)26, Comparative Toxicogenomics Database (CTD) (https://ctdbase.org/)27, GeneCards (https://www.genecards.org/)28, SwissTargetPrediction (http://www.swisstargetprediction.ch/)29, and DrugBank databases. Drug targets were identified after removing duplicates.
Target screening for TD
TD-related targets were identified using the GeneCards, DisGeNET (https://www.disgenet.org/)30, Online Mendelian Inheritance in Man (OMIM) (https://www.omim.org/)31, and Therapeutic Target Database (TTD) (https://db.idrblab.net/ttd/)32. Using “tardive dyskinesia” as a keyword, disease targets were identified after removing duplicates.
Drug-disease target intersection
Venny 2.1.0 (https://bioinfogp.cnb.csic.es/tools/venny) was used to identify intersecting targets between drug-related and TD-related targets. The results were visualized using the bioinformatics platform (http://www.bioinformatics.com.cn/).
PPI network construction and core target screening
Intersecting targets were imported into the STRING database (https://string-db.org) to construct the PPI networks33, restricting the species to Homo sapiens, with a confidence score set to ≥0.4 and excluding disconnected nodes. Cytoscape 3.10.0 (https://www.cytoscape.org/) was used to visualize and analyze the PPI networks34. The CytoHubba plug-in identified the top 10 hub genes using the Maximal Clique Centrality (MCC) method.
GO and KEGG enrichment analyses
Intersecting targets were evaluated by GO and KEGG enrichment analyses using the Database for Annotation, Visualization, and Integrated Discovery (DAVID) (https://david.ncifcrf.gov/)35. GO analysis included biological processes (BPs), cellular components (CCs), and molecular functions (MFs). The top 10 GO terms and KEGG pathways (P < 0.05) were selected for further analysis. Results were visualized using the bioinformatics platform (http://www.bioinformatics.com.cn/).
Drug-pathway-target-disease network construction
Drug-pathway-target-disease networks were constructed and visualized using Cytoscape 3.10.0, highlighting the common and unique core targets and pathways of valbenazine, deutetrabenazine, and vitamin E in treating TD.
Molecular docking verification
Molecular docking was used to predict the binding affinities between three drugs and core target proteins. AutoDockTools 1.5.6 and AutoDock Vina were employed for this process36. Ligand preparation involved downloading structure files for valbenazine, deutetrabenazine, and vitamin E (in sdf format) from PubChem (https://pubchem.ncbi.nlm.nih.gov/) and DrugBank37, followed by conversion to 3D structures using ChemBio3D Ultra 14.0 for energy minimization. These were subsequently processed in AutoDockTools 1.5.6 and saved as pdbqt files. For protein preparation, crystal structures of target proteins were obtained from the RCSB Protein Data Bank (http://www.rcsb.org) and processed in PyMOL 2.4.1 to remove water and ligands38. Hydrogen atoms were added, and charges/atom types were assigned using AutoDockTools, with final pdbqt files saved. Grid preparation involved defining the docking box size and coordinates based on predicted binding sites from DoGSiteScorer (https://proteins.plus/). Molecular docking and binding energy calculations were performed using AutoDock Vina. Finally, Discovery Studio 2021 and PyMOL 2.4.1 were used for interaction analysis and visualization.
Table 1 offers an overview of the tools and databases employed in our research, helping readers better understand the specific methods and supporting materials used.
Results
Identification of TD-related targets of valbenazine, deutetrabenazine, and vitamin E
Targets for valbenazine, deutetrabenazine, and vitamin E were identified using PharmMapper, CTD, GeneCards, SwissTargetPrediction, and DrugBank databases, yielding 288, 10, 4, 100, and 1 targets for valbenazine; 195, 1, 7, 105, and 1 for deutetrabenazine; and 245, 1941, 917, 22, and 10 for vitamin E, respectively. After removing duplicates, 377 targets for valbenazine, 290 for deutetrabenazine, and 2689 for vitamin E were obtained.
TD-related targets were identified from GeneCards, DisGeNET, OMIM, and TTD databases, with 138, 30, 59, and 1 targets, respectively. After eliminating duplicates, 205 potential TD-related targets were identified. Venn diagrams showed 32 overlapping targets between valbenazine and TD (Fig. 2A), 36 between deutetrabenazine and TD (Fig. 2E), and 62 between vitamin E and TD (Fig. 3A).
A, E Venn diagrams indicating the common drug-disease targets. A valbenazine and TD; (E) deutetrabenazine and TD. B, F PPI network diagrams for the common targets obtained from the STRING database. B valbenazine; (F) deutetrabenazine. C, G PPI network maps generated using Cytoscape. C valbenazine; G deutetrabenazine. Redder coloration and larger size indicate a higher degree value in the PPI network. D, H Top 10 hub targets selected from the PPI network using the CytoHubba plugin, as ranked using the MCC method. D valbenazine; (H) deutetrabenazine.
A Venn diagrams indicating the common drug-disease targets. B PPI network diagrams for the common targets obtained from the STRING database. C PPI network maps generated using Cytoscape; a redder coloration and larger size indicate a higher degree in the PPI network. D Top 10 hub targets selected from the PPI network using the CytoHubba plugin, as ranked using the MCC method.
PPI network construction and core target identification
The 32, 36, and 62 common TD-related targets of valbenazine, deutetrabenazine, and vitamin E were uploaded to the STRING database to construct PPI networks (Figs. 2B, F and 3B). The resulting PPI data were imported into Cytoscape 3.10.0 for further analysis. The PPI network for valbenazine and TD consisted of 32 nodes and 131 edges (Fig. 2C), for deutetrabenazine and TD, 36 nodes and 181 edges (Fig. 2G), and for vitamin E and TD, 54 nodes and 399 edges (Fig. 3C). The top 10 hub targets were identified using the MCC method via the CytoHubba plug-in (Figs. 2D, H and 3D).
GO enrichment analyses
To investigate the molecular mechanisms of valbenazine, deutetrabenazine, and vitamin E in TD, GO enrichment analyses were performed on the common targets. The top 10 BP, CC, and MF terms were displayed in column charts (Fig. 4A–I).
A–I Bar charts from GO enrichment analyses. J–L Bubble charts presenting the results of KEGG pathway enrichment analyses. A–C, J GO and KEGG pathway enrichment analyses of common targets shared between valbenazine and TD. D–F, K GO and KEGG pathway enrichment analyses of common targets shared between deutetrabenazine and TD. G–I, L GO and KEGG pathway enrichment analyses of common targets shared between vitamin E and TD. A–G The top 10 biological processes. B–H The top 10 cellular components. (C–I) The top 10 molecular functions. J–L The top 10 KEGG signaling pathways. The color and size of each bubble indicate the P-value and gene count, respectively.
For valbenazine, 120 BPs, 22 CCs, and 44 MFs were identified. Enriched BP terms included the adenylate cyclase-activating adrenergic receptor signaling pathway, response to xenobiotic stimulus, and xenobiotic catabolic process. Key CC terms were synapse, dopaminergic synapse, and presynaptic membrane, while notable MFs were heterotrimeric G-protein binding, dopamine binding, and monoamine transmembrane transporter activity.
For deutetrabenazine, 120 BPs, 21 CCs, and 47 MFs were identified. Significant BP terms included the G protein-coupled receptor signaling pathway, coupled to cyclic nucleotide second messenger, and response to xenobiotic stimulus. Key CC terms were dendrite, synapse, plasma membrane, and presynaptic membrane, and notable MFs included serotonin binding, G protein-coupled serotonin receptor activity, and dopamine binding.
For vitamin E, 182 BPs, 25 CCs, and 46 MFs were identified. Enriched BP terms included response to xenobiotic stimulus, response to lipopolysaccharide, and xenobiotic catabolic process. Important CC terms included intracellular membrane-bounded organelle, mitochondrion, and extracellular region, while key MFs included heme binding, oxygen binding, and oxidoreductase activity.
KEGG pathway analyses and drug-pathway-target-disease network construction
The analysis identified the top 10 enriched KEGG pathways associated with common targets of valbenazine and TD (Table 2, Fig. 4J). The dopaminergic synapse signaling pathway emerged as the most significant potential pathway, characterized by the lowest P-value and the highest number of enriched core targets. The resulting drug-pathway-target-disease network diagram illustrated the effects of valbenazine on TD, comprising 37 nodes and 77 edges (Fig. 5).
Drug-pathway-target-disease network diagrams relating to the effects of valbenazine (A), deutetrabenazine (C), and vitamin E (E) on TD. The orange inverted triangles represent the drug and disease. The green round rectangles represent the pathways affected by three agents in the treatment of TD, while the red rounded rectangles represent the critical pathways. The blue circles represent the targets of these three agents associated with the treatment of TD. The red triangles represent core targets. B The distribution of the six selected core targets (DRD1, DRD2, DRD3, MAOB, SLC6A3, and SLC18A2) in the dopaminergic synapse signaling pathway. D The distribution of the six selected core targets (DRD1, DRD2, MAOA, MAOB, SLC6A3, and SLC18A2) in the dopaminergic synapse signaling pathway. (F) The distribution of the five selected core targets (AKT1, BDNF, INS, NOS3, and TLR4) in the PI3K-Akt signaling pathway.
Similarly, the top 10 enriched KEGG pathways for deutetrabenazine and TD were analyzed (Table 3, Fig. 4K). The dopaminergic synapse signaling pathway again featured prominently and was identified as the most critical pathway with the highest number of enriched core targets. The corresponding network diagram included 44 nodes and 91 edges (Fig. 5).
Last, the top 10 enriched KEGG pathways associated with vitamin E and TD were examined (Table 4, Fig. 4L). The PI3K-Akt signaling pathway was recognized as the most significant potential pathway due to the largest number of enriched core targets. The corresponding network diagram consisted of 41 nodes and 95 edges (Fig. 5).
Molecular docking verification
To validate the network pharmacology findings, molecular docking was performed to assess the binding affinity of valbenazine, deutetrabenazine, and vitamin E with selected core targets. Discovery Studio 2021 and PyMOL 2.4.1 were used to visualize the drug-target interactions (Figs. 6 and 7). Based on the degree of hub targets in the PPI network and KEGG enrichment analyses, six core targets were identified for valbenazine and deutetrabenazine, and five for vitamin E. Valbenazine and deutetrabenazine shared five core targets: SLC18A2, SLC6A3, DRD1, DRD2, and MAOB, with DRD3 unique to valbenazine and MAOA unique to deutetrabenazine. The distinct core targets for vitamin E were AKT1, BDNF, INS, NOS3, and TLR4. Details of these potential core targets are listed in Table 5. Docking scores for valbenazine ranged from −7.8 to −8.8 kcal/mol, deutetrabenazine from −6.9 to −8.5 kcal/mol, and vitamin E from −7.1 to −8.7 kcal/mol, indicating stable binding (Table 6).
A Valbenazine-DRD1; (B) Valbenazine-DRD2; (C) Valbenazine-DRD3; (D) Valbenazine-MAOB; (E) Valbenazine-SLC6A3; (F) Valbenazine-SLC18A2; (G) Deutetrabenazine-DRD1; (H) Deutetrabenazine-DRD2; (I) Deutetrabenazine-MAOA; (J) Deutetrabenazine-MAOB; (K) Deutetrabenazine-SLC6A3; (L) Deutetrabenazine-SLC18A2.
Discussion
TD is a potentially irreversible and disabling adverse effect of DRBAs. Although the FDA has approved VMAT2 inhibitors valbenazine and deutetrabenazine for TD treatment, their precise mechanisms of action beyond VMAT2 interaction (encoded by SLC18A2) remain unclear39,40,41,42. A Cochrane review suggested that vitamin E may help prevent TD progression21, but its exact mechanism is not well understood. This study aimed to explore the molecular targets and pathways of these three agents in TD treatment. Bioinformatics analysis revealed both shared and distinct core targets, suggesting they act through common and unique mechanisms.
Screening for common targets revealed 32 genes shared between valbenazine and TD, 36 between deutetrabenazine and TD, and 62 between vitamin E and TD. These genes may serve as potential targets for TD treatment. From the PPI network and KEGG pathway analyses, we selected six core targets for valbenazine and deutetrabenazine, and five for vitamin E. Valbenazine and deutetrabenazine shared five core targets: DRD1, DRD2, MAOB, SLC6A3, and SLC18A2. Valbenazine uniquely targeted DRD3, while deutetrabenazine specifically targeted MAOA. The five core targets for vitamin E—AKT1, BDNF, INS, NOS3, and TLR4—were distinct from those of the other two agents. These results indicate that valbenazine and deutetrabenazine may exert overlapping pharmacological effects on TD, whereas vitamin E likely operates through different mechanisms.
Abnormalities in dopaminergic neurotransmission, involving VMAT (VMAT1 and VMAT2)40,41,42, dopaminergic receptor genes43, the dopamine transporter (DAT) encoded by SLC6A344, and monoamine oxidase (MAO) activity44,45, may contribute to the pathogenesis and treatment of TD. VMAT2 plays a crucial role in storing and releasing monoamines, such as dopamine, which are implicated in TD42. The VMAT2 inhibitors valbenazine and deutetrabenazine reduce dopamine transport into synaptic vesicles, decreasing dopamine release in the dorsal striatum, a region that regulates movement. This mechanism is thought to mitigate TD, supported by several randomized controlled trials16,17,46,47,48. A review identified associations between DRD1, DRD2, and DRD3 and antipsychotic-induced TD49. Vacuous chewing movements (VCMs), which are unconscious chewing motions without food, often signal neurological or psychological issues and are a symptom of TD. A recent animal study found a positive correlation between VCMs and DAT immunoreactivity in the substantia nigra44. MAO, involved in metabolizing monoamine neurotransmitters, also played a role; chronic VCMs were linked to reduced MAOB activity in rat striatum45. Increased MAO activity can lead to overproduction of hydrogen peroxide50, and dopamine autoxidation can generate dopamine quinones51, which are strong oxidants. These findings, alongside our network pharmacology analysis, support the hypothesis that oxidative stress and dopamine receptor hypersensitivity in nigrostriatal circuits contribute to TD’s pathophysiology and the therapeutic effects of valbenazine and deutetrabenazine.
In addition to dopaminergic dysregulation, immunological mechanisms may play a crucial role in TD development52. AKT1 is downstream of DRD2, which is partially inhibited by antipsychotics. Recently, a genetic study demonstrated the interaction between rs3730358 in AKT1 and rs6275 in DRD2 in patients with TD53. Brain-derived neurotrophic factor (BDNF) possesses neuroprotective and antioxidant properties, mitigating striatal dopamine reductions induced by neurotoxins54. Several studies have reported lower serum BDNF levels in patients with schizophrenia and TD compared to those without TD55,56, suggesting a possible link between neuroimmune dysfunction and TD pathogenesis. Additionally, a study indicated that patients with schizophrenia and TD exhibited reduced movement when treated with low-dose insulin (INS) injections over 3 months57, hinting at potential interactions among metabolic dysregulation, inflammation, and TD severity. Nitric oxide (NO), a physiological free radical, plays a dual role: under normal conditions, it provides neuroprotection, whereas excessive NO production leads to neurotoxicity. Excess NO can form toxic compounds such as reactive nitrogen species, peroxynitrite, and nitrogen dioxide radicals, which induce oxidative stress and inflammatory damage in the central nervous system58. The brain produces NO via two enzymes: neuronal nitric oxide synthase (NOS1) and endothelial NOS (NOS3). Previous research has identified an association between NOS3 gene polymorphisms and TD susceptibility59, further supporting the role of oxidative stress and immune dysfunction in TD pathogenesis. Toll-like receptor 4 (TLR4), a key regulator of innate immunity and neuroinflammatory processes, has been implicated in TD pathophysiology. Evidence suggests that dysregulation of the TLR4 signaling pathway contributes to neuroinflammation and cognitive impairment in schizophrenia patients with TD60. Growing evidence supports that TD results from a complex interplay between oxidative stress, neuroinflammation, and immune system dysregulation, with immunological mechanisms playing a critical role in its pathogenesis. These insights highlight the potential of targeting immune-inflammatory pathways for therapeutic intervention in TD. Notably, Vitamin E, with its potent antioxidant and immunomodulatory properties, may counteract oxidative stress and neuroinflammation, thereby reducing TD progression. A Cochrane review21 indicated that while Vitamin E may not significantly reverse established TD symptoms, it could prevent symptom deterioration by mitigating oxidative damage and modulating immune responses, although the evidence remains of low quality. Additionally, another review20 on Vitamin E supplementation highlighted its role in stabilizing neuronal membranes and scavenging free radicals, further supporting its therapeutic potential in TD. These findings suggest that Vitamin E may provide neuroprotection by reducing oxidative stress-induced neuronal damage and modulating immune responses, making it a promising adjunct therapy for TD.
GO enrichment analyses revealed that, in the context of TD treatment, both valbenazine and deutetrabenazine predominantly target genes involved in dopaminergic synapses, presynaptic and postsynaptic membranes, plasma membranes, and dendrites. Their biological functions include dopamine binding, G-protein binding, and oxidoreductase activity. These GO results align with the proposed etiologies of TD, which involve dopamine receptor hypersensitivity and oxidative stress12,13. Furthermore, KEGG pathway analyses identified the dopaminergic synapse signaling pathway as the most critical common pathway, exhibiting the highest number of core genes, in the effects of valbenazine and deutetrabenazine on TD.
The precise etiology of TD remains unclear. However, one hypothesis is that chronic blockade of dopamine D2 receptors leads to compensatory hypersensitivity of postsynaptic dopamine receptors due to increased receptor density61. This hypothesis does not fully explain why TD persists after the cessation of DRBA use. An alternative hypothesis is that DRBAs block postsynaptic D2 receptors, leading to an excess of unbound synaptic dopamine, which is then reuptaken by the presynaptic neuron via the dopamine transporter. Dopamine autoxidation or enzymatic oxidation via MAO produces reactive oxygen species. Both valbenazine and deutetrabenazine are effective in treating TD by downregulating presynaptic dopamine packaging and release at neuronal synapses62,63. Consequently, the effects of these two drugs on TD may involve targets associated with postsynaptic, synaptic, and presynaptic changes, oxidative stress, and the dopaminergic synapse signaling pathway.
GO enrichment analysis revealed that gene targets of vitamin E in the treatment of TD are predominantly enriched in intracellular membrane-bounded organelles, mitochondria, extracellular regions, and the cytoplasm. Key biological functions include heme binding, aromatase activity, oxygen binding, and oxidoreductase activity. These GO results are in line with previous studies, highlighting the involvement of oxidative stress and inflammation in the effects of vitamin E on TD64,65,66. KEGG pathway analysis identified the PI3K-Akt signaling pathway as the most critical pathway for vitamin E in treating TD. Several studies have demonstrated that activation of the G-protein-coupled estrogen receptor-1 (GPER) enhances the transcription of the ERK1/2 and PI3K/Akt/GSK-3β signaling pathways. This, in turn, can halt the progression of neurodegenerative diseases such as Parkinson’s disease, Huntington’s disease, epilepsy, and TD by reducing oxidative stress, neuroinflammation, and apoptosis67,68,69. Tocotrienols (T3s), a form of vitamin E, particularly γT3/δT3, have demonstrated antioxidant effects and receptor-mediated protection through the GPERβ/PI3K/Akt pathway70.
Blocking the dopamine D2 receptor leads to excessive dopamine metabolism, generating free radicals that contribute to mitochondrial dysfunction, neuroinflammation, apoptosis, and neuronal degeneration. Thus, the effects of vitamin E on TD may be mediated through targets associated with oxidative stress, neuroinflammation, apoptosis, and the PI3K-Akt signaling pathway.
Molecular docking is a widely used tool in computer-aided drug design. We used this approach to further validate the accuracy of our network pharmacology results. The docking scores for the three agents and their corresponding core targets ranged from −6.9 to −8.8 kcal/mol (all <−5 kcal/mol), suggesting strong binding affinities between the ligands and their respective core proteins71. These findings suggest that the effectiveness of the three agents in treating TD may be attributed to their interactions with these core targets. A recent meta-analysis72 suggested that valbenazine and deutetrabenazine are first-line treatments for TD, while vitamin E potentially serves as a second-line treatment. However, given the high cost of valbenazine and deutetrabenazine, these medications remain inaccessible to many TD patients, particularly those from low-income families or developing countries. In contrast, vitamin E is a practical alternative treatment option with its safety profile and affordability. Our study provides computational insights into the molecular mechanisms of these three drugs, further supporting the clinical findings regarding their therapeutic potential. By integrating target identification, pathway enrichment, and network analyses, we demonstrate that vitamin E may exert beneficial effects through mechanisms distinct from or complementary to those of valbenazine and deutetrabenazine. These findings underscore the need to consider both clinical efficacy and accessibility when formulating treatment strategies for TD.
Limitation
This study has several limitations. First, the target data were predicted using various databases, so their reliability depends on the quality of the underlying data. Moreover, the databases used may be more focused on well-established drug targets, potentially overlooking lesser-known or emerging targets that could also play important roles in drug action. Second, network pharmacology mainly relies on qualitative assessments, lacking quantitative analysis of drug dosage effects. Third, how well or poorly vitamin E works compared to valbenazine and deutetrabenazine cannot be ascertained from this study. Our analysis is only a preliminary exploration of the potential mechanisms of these drugs in treating TD. Finally, although this study utilized a data mining approach, further in vivo and in vitro experiments, as well as clinical trials, are required to validate these findings.
Conclusion
This study employed bioinformatics techniques to investigate the pharmacological mechanisms of valbenazine, deutetrabenazine, and vitamin E in treating TD. The findings indicate valbenazine and deutetrabenazine may share common mechanisms by targeting the dopaminergic synapse signaling pathway through core proteins such as DRD1, DRD2, MAOB, SLC6A3, and SLC18A2. However, they also differ in their interactions with specific targets; valbenazine uniquely affects DRD3, while deutetrabenazine targets MAOA. In contrast, vitamin E may operate through a distinct mechanism by regulating the PI3K-Akt signaling pathway via interactions with different core targets, including AKT1, BDNF, INS, NOS3, and TLR4. Our findings provide a foundational understanding for future research and drug development efforts, offering clinicians deeper insights into the pathophysiology of TD. This work may inform targeted therapeutic strategies, ultimately advancing the clinical treatment of TD.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Faurbye, A., Rasch, P. J., Petersen, P. B., Brandborg, G. & Pakkenberg, H. Neurological symptoms in pharmacotherapy of psychoses. Acta Psychiatr. Scand. 40, 10–27 (1964).
van Harten, P. N. & Tenback, D. E. Tardive dyskinesia: clinical presentation and treatment. Int Rev Neurobiol. 98, 187–210 (2011).
Widschwendter, C. G. & Hofer, A. Antipsychotic-induced tardive dyskinesia: update on epidemiology and management. Curr. Opin. Psychiatry 32, 179–184 (2019).
Atlas, S. J., Agboola, F. & Curfman, G. Effectiveness and value of 2 novel treatments for tardive dyskinesia. JAMA Intern. Med. 178, 1110–1112 (2018).
Kenney, C., Hunter, C., Davidson, A. & Jankovic, J. Metoclopramide, an increasingly recognized cause of tardive dyskinesia. J. Clin. Pharmacol. 48, 379–384 (2008).
Vandewalle, W., Boon, E. & Sienaert, P. [Movement disorders due to modern antidepressants and mood stabilizers]. Tijdschr. Psychiatr 57, 132–137 (2015).
Chouza, C. et al. Parkinsonism, tardive dyskinesia, akathisia, and depression induced by flunarizine. Lancet 1, 1303–1304 (1986).
Barer, Y. et al. The clinical and economic burden of tardive dyskinesia in Israel: real-world data analysis. J. Clin. Psychopharmacol. 42, 454–460 (2022).
Jain, R. et al. Impact of tardive dyskinesia on physical, psychological, social, and professional domains of patient lives: a survey of patients in the United States. J. Clin. Psychiatry. 84, 22m14694 (2023).
Arya, D., Khan, T., Margolius, A. J. & Fernandez, H. H. Tardive Dyskinesia: treatment update. Curr. Neurol. Neurosci. Rep. 19, 69 (2019).
Dean, C. E. & Thuras, P. D. Mortality and tardive dyskinesia: long-term study using the US national death index. Br. J. Psychiatry 194, 360–364 (2009).
Cho, C. H. & Lee, H. J. Oxidative stress and tardive dyskinesia: pharmacogenetic evidence. Prog. Neuropsychopharmacol. Biol. Psychiatry 46, 207–213 (2013).
Margolese, H. C., Chouinard, G., Kolivakis, T. T., Beauclair, L. & Miller, R. Tardive dyskinesia in the era of typical and atypical antipsychotics. Part 1: pathophysiology and mechanisms of induction. Can. J. Psychiatry 50, 541–547 (2005).
Niemann, N. & Jankovic, J. Treatment of tardive dyskinesia: a general overview with focus on the vesicular monoamine transporter 2 inhibitors. Drugs 78, 525–541 (2018).
Freudenreich, O. & Remington, G. Valbenazine for tardive dyskinesia. Clin. Schizophr. Relat. Psychoses 11, 113–119 (2017).
Hauser, R. A. et al. KINECT 3: A phase 3 randomized, double-blind, placebo-controlled trial of valbenazine for Tardive Dyskinesia. Am. J. Psychiatry 174, 476–484 (2017).
Fernandez, H. H. et al. Randomized controlled trial of deutetrabenazine for tardive dyskinesia: the ARM-TD study. Neurology 88, 2003–2010 (2017).
Scorr, L. M. & Factor, S. A. VMAT2 inhibitors for the treatment of tardive dyskinesia. J. Neurol. Sci. 389, 43–47 (2018).
Bhidayasiri, R., Jitkritsadakul, O., Friedman, J. H. & Fahn, S. Updating the recommendations for treatment of tardive syndromes: a systematic review of new evidence and practical treatment algorithm. J. Neurol. Sci. 389, 67–75 (2018).
Okebukola, P. O., Kansra, S. & Barrett, J. Vitamin E supplementation in people with cystic fibrosis. Cochrane Database Syst. Rev. 3, Cd009422 (2017).
Soares-Weiser, K., Maayan, N. & Bergman, H. Vitamin E for antipsychotic-induced tardive dyskinesia. Cochrane Database Syst. Rev. 1, Cd000209 (2018).
Hopkins, A. L. Network pharmacology. Nat. Biotechnol. 25, 1110–1111 (2007).
Li, C. et al. Molecular mechanisms of quetiapine bidirectional regulation of bipolar depression and mania based on network pharmacology and molecular docking: evidence from computational biology. J. Affect. Disord. 355, 528–539 (2024).
Altê G. A. & Rodrigues A. L. S. Exploring the molecular targets for the antidepressant and antisuicidal effects of ketamine enantiomers by using network pharmacology and molecular docking. Pharmaceuticals (Basel). 16, 1013 (2023).
Wishart, D. S. et al. DrugBank 5.0: a major update to the DrugBank database for 2018. Nucleic Acids Res. 46, D1074–d1082 (2018).
Wang, X. et al. PharmMapper 2017 update: a web server for potential drug target identification with a comprehensive target pharmacophore database. Nucleic Acids Res. 45, W356–w360 (2017).
Davis, A. P. et al. Comparative toxicogenomics database (CTD): update 2023. Nucleic Acids Res. 51, D1257–d1262 (2023).
Safran, M. et al. GeneCards Version 3: the human gene integrator. Database 2010, baq020 (2010).
Daina, A., Michielin, O. & Zoete, V. SwissTargetPrediction: updated data and new features for efficient prediction of protein targets of small molecules. Nucleic Acids Res. 47(Jul), W357–w364 (2019).
Piñero, J. et al. The DisGeNET knowledge platform for disease genomics: 2019 update. Nucleic Acids Res. 48, D845–d855 (2020).
Amberger, J. S., Bocchini, C. A., Scott, A. F. & Hamosh, A. OMIM.org: leveraging knowledge across phenotype-gene relationships. Nucleic Acids Res. 47, D1038–d1043 (2019).
Zhou, Y. et al. TTD: Therapeutic target database describing target druggability information. Nucleic Acids Res. 52, D1465–d1477 (2024).
Szklarczyk, D. et al. The STRING database in 2023: protein-protein association networks and functional enrichment analyses for any sequenced genome of interest. Nucleic Acids Res. 51, D638–d646 (2023).
Shannon, P. et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 13, 2498–2504 (2003).
Dennis, G. Jr et al. DAVID: Database for annotation, visualization, and integrated discovery. Genome Biol. 4, P3 (2003).
Trott, O. & Olson, A. J. AutoDock Vina: improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 31, 455–461 (2010).
Kim, S. et al. PubChem in 2021: new data content and improved web interfaces. Nucleic Acids Res. 49, D1388–d1395 (2021).
Burley, S. K. et al. Protein data bank (PDB): the single global macromolecular structure archive. Methods Mol. Biol. 1607, 627–641 (2017).
Zai, C. C. et al. Genetics of tardive dyskinesia: promising leads and ways forward. J. Neurol. Sci. 389, 28–34 (2018).
Zai, C. C. et al. Association study of the vesicular monoamine transporter gene SLC18A2 with tardive dyskinesia. J. Psychiatr. Res. 47, 1760–1765 (2013).
Huang, M. et al. Effects of NBI-98782, a selective vesicular monoamine transporter 2 (VMAT2) inhibitor, on neurotransmitter efflux and phencyclidine-induced locomotor activity: relevance to tardive dyskinesia and antipsychotic action. Pharmacol. Biochem. Behav. 190, 172872 (2020).
Islam, F., Men, X., Yoshida, K., Zai, C. C. & Müller, D. J. Pharmacogenetics-guided advances in antipsychotic treatment. Clin. Pharmacol. Ther. 110, 582–588 (2021).
Lee, H. J. & Kang, S. G. Genetics of tardive dyskinesia. Int. Rev. Neurobiol. 98, 231–264 (2011).
de Freitas, C. M. et al. Behavioral and neurochemical effects induced by reserpine in mice. Psychopharmacology 233, 457–467 (2016).
Busanello, A. et al. Resveratrol protects against vacuous chewing movements induced by chronic treatment with fluphenazine. Neurochem Res. 42, 3033–3040 (2017).
Factor, S. A. et al. The effects of valbenazine in participants with tardive dyskinesia: results of the 1 year KINECT 3 extension study. J. Clin. Psychiatry 78, 1344–1350 (2017).
Fernandez, H. H. et al. Long-term safety and efficacy of deutetrabenazine for the treatment of tardive dyskinesia. J. Neurol. Neurosurg. Psychiatry 90, 1317–1323 (2019).
Anderson, K. E. et al. Deutetrabenazine for treatment of involuntary movements in patients with tardive dyskinesia (AIM-TD): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Psychiatry 4, 595–604 (2017).
Vaiman E. E. et al. Candidate genes encoding dopamine receptors as predictors of the risk of antipsychotic-induced parkinsonism and tardive dyskinesia in schizophrenic patients. Biomedicines. 9, 879 (2023).
Youdim, M. B. & Bakhle, Y. S. Monoamine oxidase: isoforms and inhibitors in Parkinson’s disease and depressive illness. Br. J. Pharmacol. 147, S287–S296 (2006).
Lohr, J. B., Kuczenski, R. & Niculescu, A. B. Oxidative mechanisms and tardive dyskinesia. CNS Drugs 17, 47–62 (2003).
Loonen, A. J. M. Putative role of immune reactions in the mechanism of tardive dyskinesia. Brain Behav. Immun. Health 33, 100687 (2023).
Zai, C. C. et al. Genetic study of eight AKT1 gene polymorphisms and their interaction with DRD2 gene polymorphisms in tardive dyskinesia. Schizophr. Res. 106, 248–252 (2008).
Angelucci, F., Brenè, S. & Mathé, A. A. BDNF in schizophrenia, depression and corresponding animal models. Mol. Psychiatry 10, 345–352 (2005).
Zhang, X. Y. et al. Brain-derived neurotrophic factor levels and its Val66Met gene polymorphism predict tardive dyskinesia treatment response to Ginkgo biloba. Biol. Psychiatry 72, 700–706 (2012).
Yang, Y. Q. et al. Decreased serum brain-derived neurotrophic factor levels in schizophrenic patients with tardive dyskinesia. Neurosci. Lett. 502, 37–40 (2011).
Mouret, J., Khomais, M., Lemoine, P. & Sebert, P. Low doses of insulin as a treatment of tardive dyskinesia: conjuncture or conjecture? Eur. Neurol. 31, 199–203 (1991).
Lipton, S. A. et al. A redox-based mechanism for the neuroprotective and neurodestructive effects of nitric oxide and related nitroso-compounds. Nature 364, 626–632 (1993).
Liou, Y. J. et al. Haplotype analysis of endothelial nitric oxide synthase (NOS3) genetic variants and tardive dyskinesia in patients with schizophrenia. Pharmacogenet Genomics 16, 151–157 (2006).
Li, N. et al. Dysfunctional monocytic toll-like receptor 4 signaling pathway and cognitive deficits in chronic schizophrenia patients with tardive dyskinesia. Neurosci. Lett. 777, 136581 (2022).
Cornett, E. M., Novitch, M., Kaye, A. D., Kata, V. & Kaye, A. M. Medication-induced tardive dyskinesia: a review and update. Ochsner J. Summer 17, 162–174 (2017).
Farber, R. H. et al. Clinical development of valbenazine for tics associated with Tourette syndrome. Expert Rev. Neurother 21, 393–404 (2021).
Golsorkhi, M. et al. Comparative analysis of deutetrabenazine and valbenazine as VMAT2 inhibitors for tardive dyskinesia: a systematic review. Tremor. Other Hyperkinet Mov.14, 13 (2024).
Lewis, E. D., Meydani, S. N. & Wu, D. Regulatory role of vitamin E in the immune system and inflammation. IUBMB Life 71, 487–494 (2019).
Nguyen T. T. U., Yeom J. H., Kim W. Beneficial effects of vitamin e supplementation on endothelial dysfunction, inflammation, and oxidative stress biomarkers in patients receiving hemodialysis: a systematic review and meta-analysis of randomized controlled trials. Int. J. Mol. Sci. 22, 11923 (2021).
Singh, U., Devaraj, S. & Jialal, I. Vitamin E, oxidative stress, and inflammation. Annu. Rev. Nutr. 25, 151–174 (2005).
Upadhayay, S. et al. Involvement of the G-protein-coupled estrogen receptor-1 (GPER) signaling pathway in neurodegenerative disorders: a review. Cell Mol. Neurobiol. 43, 1833–1847 (2023).
Guan, J., Yang, B., Fan, Y. & Zhang, J. GPER agonist G1 attenuates neuroinflammation and dopaminergic neurodegeneration in Parkinson disease. Neuroimmunomodulation 24, 60–66 (2017).
Correa, J., Ronchetti, S., Labombarda, F., De Nicola, A. F. & Pietranera, L. Activation of the G protein-coupled estrogen receptor (GPER) increases neurogenesis and ameliorates neuroinflammation in the hippocampus of male spontaneously hypertensive rats. Cell Mol. Neurobiol. 40, 711–723 (2020).
Nakaso, K. et al. The estrogen receptor β-PI3K/Akt pathway mediates the cytoprotective effects of tocotrienol in a cellular Parkinson’s disease model. Biochim. Biophys. Acta 1842, 1303–1312 (2014).
Deng, H. et al. Exploring the differences of chemical components of citri reticulatae pericarpium powder decoction and pieces decoction based on UHPLC-Q-exactive orbitrap MS/MS and network pharmacology. J. Sep. Sci. 47, e70034 (2024).
Solmi, M. et al. Efficacy and acceptability of pharmacological interventions for tardive dyskinesia in people with schizophrenia or mood disorders: a systematic review and network meta-analysis. Mol. Psychiatry 30, 1207–1222 (2025).
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (Nos. 81871052 and 8187053) to Chuanjun Zhuo.
Author information
Authors and Affiliations
Contributions
C.L. wrote the original draft, contributed to methodology design, formal analysis, data curation, and reviewed and edited the manuscript. X.M., R.L., and X.C. contributed to the methodology and formal analysis and reviewed and edited the manuscript. Y.L., Q.Z., and L.Y. contributed to resources, the methodology, and the quality control of collected data. H.T. and L.W. supervised the project, amended the manuscript, and provided suggestions for data analysis. C.Z. was responsible for the conceptualization of the study, conducted the investigation, and contributed to methodology design.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, C., Zhuo, C., Ma, X. et al. Unique and overlapping mechanisms of valbenazine, deutetrabenazine, and vitamin E for tardive dyskinesia. Schizophr 11, 69 (2025). https://doi.org/10.1038/s41537-025-00618-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41537-025-00618-w