Abstract
Congenital nephrogenic diabetes insipidus (NDI; also known as arginine vasopressin resistance) is a rare inherited disorder of water homeostasis, caused by insensitivity of the distal nephron to arginine vasopressin. Consequently, the kidney loses its ability to concentrate urine, which leads to polyuria, polydipsia and the risk of hypertonic dehydration. The diagnosis and management of NDI are very challenging and require an integrated, multidisciplinary approach. Here, we present 36 recommendations for diagnosis, treatment and follow-up in both children and adults, as well as emergency management, genetic counselling and family planning, for patients with NDI. These recommendations were formulated and graded by an international group of experts in NDI from paediatric and adult nephrology, urology and clinical genetics from the European Rare Kidney Disease Reference Network and the European Society of Paediatric Nephrology, as well as patient advocates, and were validated by a voting panel in a Delphi process. The goal of these recommendations is to provide guidance to health care professionals who care for patients with NDI and to patients and their families. In addition, we emphasize the need for further research on different aspects of this potentially life-threatening disorder to support the development of evidence-based guidelines in the future.
Similar content being viewed by others
Introduction
Congenital nephrogenic diabetes insipidus (NDI) is a rare inherited disorder of water homeostasis, characterized by insensitivity of the distal nephron to antidiuretic hormone (ADH; also known as arginine vasopressin (AVP)) (Fig. 1). Consequently, the kidney loses its ability to concentrate urine, which leads to polyuria, polydipsia and the risk of hypertonic dehydration1.
Arginine vasopressin (AVP) binds to the vasopressin V2 receptor (V2R) expressed on the basolateral membrane of collecting duct cells and initiates a cascade of events that involves receptor-linked activation of G protein, activation of adenylyl cyclase, production of cyclic adenosine monophosphate (cAMP) and stimulation of protein kinase A (PKA). These processes lead to the final step of the antidiuretic action of AVP — the exocytic insertion of aquaporin water channels into the luminal membrane — thereby increasing the water permeability of that membrane and allowing water to flow from the tubule lumen to the hypertonic medullary interstitium. This water transport occurs via AQP2 in the apical membrane and via AQP3 and AQP4 (constitutive water channels) in the basolateral membrane, and enables the formation of concentrated urine.
In 2022, the Working Group for Renaming Diabetes Insipidus, representing the global endocrinology community, proposed changing NDI to arginine vasopressin resistance, which distinguishes it from arginine vasopressin deficiency for central aetiologies2. However, this new terminology has not been officially adopted and is not yet included in the International Statistical Classification of Diseases and Related Health Problems (ICD-11)3. Therefore, here we will use the term NDI to describe the disease caused by insensitivity of the kidney to AVP.
Patients with NDI are usually born at term; polyuria in utero is absent or mild and polyhydramnios is not observed1. The urinary concentration defect is present at birth but rarely causes overt symptoms in breastfed infants because human milk is relatively poor in salt and protein, thereby limiting polyuria and preventing hypernatraemia. Conversely, formulas and solid foods increase the kidney solute load and cause polyuria.
The mean age at diagnosis is ~4 months4, with polyuria, failure to thrive and signs of dehydration as typical presenting symptoms (Box 1). Serum osmolality is usually >300 mOsm/kg H2O owing to hypernatraemia4, whereas urine is inappropriately diluted, with osmolality usually <200 mOsm/kg H2O (urine osmolality < plasma osmolality). However, urine osmolality can be higher than 200 mOsm/kg H2O in milder cases5,6. Infants are particularly at risk of dehydration as they have no free access to fluid. In addition, the intake of large fluid volumes can cause gastro-oesophageal reflux and vomiting7. In older children and adults, polydipsia is the predominant symptom at diagnosis.
The exact incidence and prevalence of congenital NDI are unknown, but the disease is considered to be rare. Secondary forms of NDI are more frequent and can be caused by other (inherited) kidney diseases that affect the ability to concentrate urine or medications1,7. Owing to the rarity of the condition, many practitioners are unfamiliar with this diagnosis, let alone its pathophysiology and management. Consequently, the diagnosis of NDI is frequently delayed and no evidence-based treatment recommendations have been formulated to date. Therefore, the European Reference Network on Rare Kidney Diseases (ERKNet), the European Society for Paediatric Nephrology and patient advocates took the initiative to develop Clinical Practice Recommendations (CPR).
In this Consensus Statement, we provide CPR for clinicians who are confronted in their practice with the diagnosis, treatment and genetic counselling of NDI, which is a challenging and potentially life-threatening condition. In addition, we have aimed to set up a research agenda that can aid the development of novel therapies and evidence-based guidelines in the future. Of note, our recommendations do not address secondary genetic or acquired forms of NDI.
Methods
Expert groups
For this CPR consensus paper, we followed the Reporting Items for Practical Guidelines in Healthcare statement8. The core group of experts comprised specialists from paediatric (G.A., D.Bo., F.E., L.K.K., E.L., R.V-P.) and adult (D.Bi., E.H., T.N., F.T., S.W.) nephrology, urology (O.A.F.), a clinical geneticist (N.K.) and patient advocates. The voting panel comprised 30 members with expertise in paediatric and adult inherited kidney diseases, and included members of the supporting societies and networks (voting members are listed in the Supplementary Information). Members of the voting panel provided their expert opinion on the recommendations based on a five-point scale (strongly disagree, disagree, neither agree nor disagree, agree, or strongly agree) according to the Delphi method using an electronic questionnaire. When a 70% level of consensus was not reached among the voting panel members, recommendations were adjusted after discussion in the core group and reviewed again by the voting panel until a consensus level of at least 70% was achieved.
Development of PICO questions
To ensure that the statements derived from this work could be translated into actionable recommendations, the core group developed patient population, intervention, comparator and outcomes (PICO) questions9 (Supplementary Table 1) to be addressed in the literature searches. Each PICO question formed the basis for one recommendation and the population included children and adults with congenital NDI. Recommendations were developed based on available studies investigating the clinical phenotype, genetics and management of NDI. Regarding outcomes, we provide recommendations for diagnosis, genetic counselling, family planning, follow-up and treatment with respect to kidney and urinary tract diseases, children’s growth and emergency situations, as well as treatment-associated or disease-associated complications and comorbidities.
Literature search
A literature search was conducted for each PICO question. The PubMed database was searched for papers published between 1950 and December 2023. All papers regarding human studies in English were considered, including prospective randomized controlled trials, uncontrolled or observational studies, registries, summaries and case series. In vitro and animal studies were selected to inform the future research agenda for the development of new targeted therapies. The following key medical subject headings terms were identified: nephrogenic diabetes insipidus, NDI, arginine vasopressin type 2 receptor (AVPR2; also known as vasopressin V2 receptor (V2R)) and aquaporin 2 (AQP2). The search retrieved 231 results and 102 articles (85 in the main text and 17 additional non-overlapping articles listed in the Supplementary Information).
Grading of recommendations
We followed the grading system from the American Academy of Paediatrics to evaluate and grade the recommendations10,11. The quality of evidence is graded high (A), moderate (B), low (C), very low (D) or not applicable (X). Grade X was used for exceptional situations in which validating studies cannot be performed, and benefit or harm clearly predominate. The strength of a recommendation is graded strong, moderate, weak or discretionary (when no recommendation can be made).
Diagnostic approach
Rationale for diagnostic approach
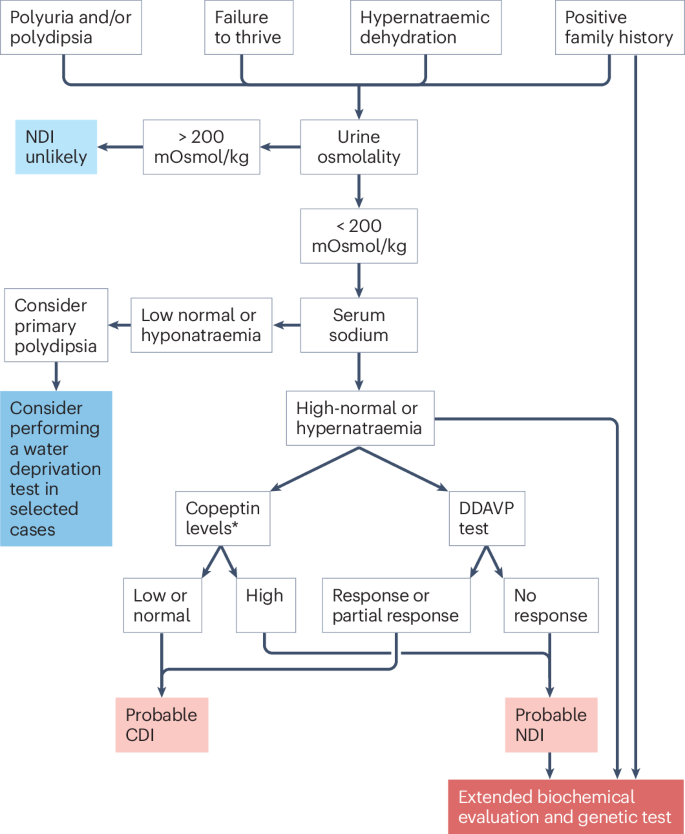
We recommend suspecting NDI in infants and children who present with polyuria, polydipsia, failure to thrive and hypernatraemic dehydration, and in adults with unexplained polyuria and polydipsia. A comprehensive family history and pedigree construction is essential to identify family cases. The initial work-up consists of measuring serum sodium, serum osmolality and urine osmolality. The detection of inappropriately diluted urine (that is, urinary osmolality <200 mOsm/kg H2O), in combination with high–normal or elevated serum sodium is pathognomonic for the diagnosis of diabetes insipidus (nephrogenic or central) and warrants early genetic testing if NDI is suspected (Fig. 2).
Nephrogenic diabetes insipidus (NDI) should be suspected in patients with unexplained polyuria, polydipsia, failure to thrive and/or hypernatraemic dehydration. The initial biochemical work-up consists of measuring urine and serum osmolality, and serum sodium. In patients with urine osmolality <200 mOsm/kg H2O and normal or high serum sodium, the diagnosis of DI is probable and early genetic testing is recommended. Early genetic testing should also be performed in patients at risk of NDI (for example, male offspring of a mother carrying an AVPR2 mutation). When early genetic testing is not available, other diagnostic tests can be recommended. Extended biochemical evaluation is performed to exclude polyuric disorders other than NDI. Plasma copeptin measurements are validated in adults, but not in children. The desmopressin (DDAVP) test can distinguish patients with central DI (CDI) (normal urine concentration capacity after the administration of DDAVP) and NDI (no response to DDAVP). Partial response to DDAVP is defined as an ability to increase urine osmolality above the baseline, but not reaching the reference values (600 mOsm/kg H2O in children <1 year; 600–800 mOsm/kg H2O in children aged 1–2 years; 800 mOsm/kg H2O in children aged >2 years). In patients with suspected primary polydipsia, a water deprivation test can be considered, although its diagnostic accuracy is limited. Of note, a water deprivation test is contraindicated in patients with a history of hypernatraemic dehydration and inappropriately diluted urine. In adults, copeptin levels after stimulation with hypertonic saline or arginine can help to distinguish primary polyuria and DI. *An assessment of copeptin levels is only useful to exclude CDI (arginine vasopressin (AVP) deficiency) if they are ≥21.4 pmol/l (indicative of NDI) and sodium levels are above 147 mmol/l because there is a large overlap between unstimulated copeptin levels in patients with AVP deficiency and primary polydipsia.
We recommend, when possible, starting the diagnostic process with genetic testing in all patients with clinical and biochemical symptoms of NDI. For practical reasons, in patients who present with polyuria and polydipsia, an extended biochemical work-up is usually performed simultaneously with the initial work-up to exclude other polyuric disorders, including diabetes mellitus, renal Fanconi syndrome or Bartter syndrome (Table 1).
Rationale for early genetic testing
Approximately 90% of all affected patients have the X-linked form of NDI (OMIM #304800) caused by pathogenic variants in AVPR2 (chromosome Xq28), and most patients are male6. A minority of patients (<10%) have autosomal forms of NDI caused by pathogenic variants in AQP2 (chromosome 12q13.12), which encodes the AQP2 water channel. These autosomal forms are inherited as autosomal-recessive (OMIM #222000) or autosomal-dominant (OMIM #125800) traits, affecting males and females equally7,12,13,14,15. Autosomal-dominant NDI caused by pathogenic AQP2 variants might be underdiagnosed, as these patients might be able to compensate for the AQP2 loss and therefore not show all symptoms.
Genetic testing can provide an early and definite diagnosis, with important implications for clinical management and outcome, and can avoid unpleasant, challenging, and potentially harmful diagnostic procedures, including the desmopressin (DDAVP) test or the water deprivation test. An early diagnosis also prevents prolonged, unrecognized periods of severe hypertonic dehydration, which can result in seizures, developmental delay and cognitive impairment16,17,18.
A minority of individuals with X-linked NDI have AVPR2 pathogenic variants associated with partial insensitivity to AVP15,19,20. A genetic diagnosis can help to identify these patients with partial NDI, in whom laboratory test results can be difficult to interpret and distinction from (partial) central diabetes insipidus (AVP deficiency) is challenging.
An early genetic diagnosis is also crucial for precise genetic counselling. It informs recurrence risks and can support patient decision-making regarding family planning, including reproductive options such as prenatal and preimplantation genetic testing. In addition, a genetic diagnosis offers presymptomatic testing opportunities for family members at risk. Especially in cases of X-linked NDI, awareness of carrier status of a familial AVPR2 pathogenic variant in female family members can support them and their partners in making an informed decision regarding their reproductive options. Finally, the identification of a genetic cause of NDI can have implications for determining the eligibility of patients for future genetically stratified clinical trials.
In families without a history of NDI, molecular genetic testing might identify de novo pathogenic variants, which is important to determine the genetic risk status of the extended family. A study of a large global cohort of patients with NDI revealed that a de novo pathogenic variant arose during oogenesis in the mother in 20% of isolated cases21.
In male offspring of heterozygote AVPR2 mutation carriers, we strongly recommend genetic testing in umbilical cord blood directly after birth (when this has not been performed at the prenatal stage), as it might prevent primary manifestations of the disorder by facilitating early treatment and monitoring18.
We strongly recommend performing genetic testing in a laboratory accredited for diagnostic genetic testing. We recommend the use of a massively parallel sequencing-based multigene panel that includes at least AQP2, AVPR2 and AVP (for differential diagnosis of central diabetes insipidus) to identify the genetic cause of NDI at the most reasonable cost while limiting incidental findings. The use of a multigene panel that additionally includes copy number variant analysis is highly recommended. Of note, genetic testing with such a multigene panel is recommended even for females with overt NDI. Overt NDI in females can be caused by biallelic pathogenic variants in AQP2, but some females with AVPR2 pathogenic variants (10%) also develop the complete NDI phenotype22,23. The latter phenomenon is most likely due to X-inactivation of the chromosome that does not carry the AVPR2 pathogenic variant24,25.
Other diagnostic tests
If genetic testing is not available or inconclusive (5–10% of cases, personal communication of Daniel G. Bichet, Rosa Vargas-Poussou), we recommend performing the following diagnostic tests (Box 2 and Fig. 2).
Plasma copeptin
Measurement of blood AVP is challenging as the hormone is unstable and the measurement is cumbersome. In adults, we recommend measuring plasma copeptin as a suitable alternative, as copeptin (CT-proAVP) is released in an equimolar 1:1 ratio with AVP26. Baseline plasma copeptin levels above 21.4 pmol/l have been reported as diagnostic for NDI in adult patients26. Because these copeptin values are significantly higher than those observed in patients with other polyuric disorders27,28,29, for most adult patients with NDI no additional testing is necessary. Adults with plasma copeptin <21.4 pmol/l should be tested for AVP deficiency (central DI) and primary polydipsia using infusion tests with hypertonic saline or arginine28,30,31. Only a few reports have evaluated the diagnostic values of plasma copeptin in paediatric polyuric disorders32,33,34,35,36.
DDAVP test
The urine concentration test uses DDAVP, a synthetic AVP analogue with specific affinity for AVPR2, to assess the responsiveness of the kidney to AVP1,37. The test should be performed with caution, especially in patients who cannot adapt their fluid intake according to thirst (for example, infants or patients who receive water through intravenous lines or nasogastric tubes). Patients with NDI usually show complete unresponsiveness to DDAVP. Patients need to be carefully monitored for their fluid intake, as ongoing fluid intake in patients with intact urinary concentration (for example, those with habitual polydipsia, can cause severe hyponatraemia). Protocols for intranasal and intravenous DDAVP tests are provided (Supplementary Boxes 1 and 2).
Water deprivation test
A water deprivation test (Supplementary Boxes 3 and 4) can be of value to assess a urinary concentration defect in selected patients (children and adults) with polyuria of unclear aetiology. However, in patients who present with high-normal or elevated serum sodium, and inappropriately diluted urine, the diagnosis of diabetes insipidus is already established. In such situations, performing a water deprivation test is not only unnecessary but poses a risk of severe dehydration38. Of note, the interpretation of urinary concentration ability after water deprivation can be difficult, as individuals with long-standing polydipsia do not concentrate urine up to the normal limits39, presumably owing to decreased AQP2 expression in the renal collecting duct, limiting the response to exogenous ADH40.
Treatment and follow-up in children
Rationale for treatment in children
Treating children with NDI is particularly challenging, especially in infants and toddlers who cannot clearly express their thirst. Feeding difficulties and frequent vomiting place a significant burden on families. Managing these patients requires specialized expertise, not only from the responsible physician but also from the entire paramedic team, including specialized nurses, dietitians, psychologists and social workers1.
Fluid intake
We recommend ad libitum access to fluid in all patients with NDI to prevent dehydration, hypernatraemia, growth failure and constipation (Box 3). In patients who are old enough and capable of self-regulating their fluid intake, the determination of the optimal amount of fluid is best left to their own thirst sensation; the patient’s osmosensors and the subsequent development (or suppression) of thirst1 tend to be more sensitive and accurate than any medical calculation. Consequently, most patients exhibit normal serum sodium levels at steady state and with free access to water. For patients who cannot self-regulate their fluid intake (for example, infants or individuals with a cognitive impairment), water should be offered frequently on top of their regular fluid intake. If patients need to fast for prolonged periods (>4 h), for example, prior to anaesthesia, intravenous water administration should be provided. A reasonable initial approach is 5% dextrose (glucose) in water at the usual maintenance rate41. In these patients, close monitoring of weight, fluid balance and biochemistry is crucial to inform adjustments to the rate of administration and fluid composition. Of note, given that this intravenous fluid provides no renal osmotic load, urine volume typically decreases considerably. Moreover, the infusion of glucose can lead to hyperglycaemia with subsequent osmotic diuresis42 and regular control of blood glucose is therefore recommended.
Adequate caloric intake and tube feeding
We recommend normal-for-age milk intake (instead of water) in infants with NDI to guarantee adequate caloric intake. ‘Greedy’ drinking followed by vomiting is commonly reported, especially in infants, and is thought to reflect gastro-oesophageal reflux exacerbated by the large fluid volume43. Careful spacing of oral feeds and fluid might ease this problem and reduce the vomiting.
The commencement of tube feeding (either by nasogastric tube or gastrostomy) is a case-by-case decision that should be carefully discussed and considered with the family. In NDI, as in other kidney diseases, we recommend tube feeding if patients have repeated episodes of vomiting and dehydration and/or growth failure44. This can be helpful to ensure adequate fluid, energy and nutritional intake. Especially for parents of young infants, the use of tube feeding can reduce the stress associated with trying to achieve adequate nutrition. Many infants and young children with NDI will show a preference for water over more nutritional fluids and the transition to solid foods can be delayed. However, many infants and children manage to grow well and avoid serious dehydration with oral intake alone45,46. In three retrospective studies, 20–30% of children with NDI had received tube feeding at some point, with ~25% of them having had a gastrostomy4,46,47. Tube feeding is rarely continued beyond 4 years of age.
Slow tube feeding by use of a feeding pump will allow a steady administration of the fluid or feed volume, which can reduce vomiting and improve growth. For infants and children who receive tube feeding for more than 3 months, insertion of a gastrostomy should be considered. A gastrostomy allows continuous tube feeds to be administered safely overnight without the risks associated with dislodgement of a nasogastric tube (that is, inadvertent fluid aspiration and associated respiratory infections). For many parents, provision of a continuous overnight nutritious feed (especially in infancy) relieves anxiety. This approach enables families to encourage oral intake of liquid or solid food during the day without the added pressure of nutritional concerns. The volume of administered fluid and food should be gradually tailed off once consistent growth and weight gain have been achieved. This will allow reassessment of the benefit of tube feeding and ensure the development and maintenance of oral feeding skills.
We recommend support from a dietitian who has experience with NDI to ensure nutritional adequacy and provide practical advice on energy supplementation of oral fluids, salt and protein intake, or tube feeds if required.
Dietary salt and protein intake
We recommend monitoring dietary salt and protein intake to reduce renal osmotic load and hence minimize urine volume. As maximal urine osmolality is reduced in NDI, patient urinary output is mainly dependent on their renal osmotic load, which, in turn, is mainly determined by salt and protein intake. In infancy, a feed with a low renal osmotic load (15 mOsm/kg body weight/day) is recommended to reduce polyuria and polydipsia, and to achieve feed tolerance, weight gain and growth. In clinical practice, a simplified formula is used to quantify the renal osmotic load: mOsm = total protein content (g) × 4 + 2 × (sodium mmol + potassium mmol)48 (Supplementary Box 5).
Beyond infancy, this calculation is usually not necessary, although for patients on tube feeding, it can be helpful to minimize the renal osmotic load of the feed to allow a more liberal oral diet. Salt control can be gradually eased, transitioning to a reduced-salt diet (or ‘no added salt diet’) by the age of 2 years. Strict avoidance of salt is not necessary and can contribute to growth failure49 as salt has a crucial role in growth by stimulating cell proliferation, enhancing protein synthesis and increasing cell mass50. Salt tolerance will vary between children, and this will usually be self-regulated to minimize problems related to polyuria and bedwetting. In clinical practice, the reduction in dietary salt intake advised is broadly in line with population goals for salt or sodium consumption51 (Table 2).
Protein and electrolytes other than sodium also contribute to renal solute load but restriction of these solutes is usually not necessary beyond infancy as it can compromise nutrition and contribute to poor growth1,15, unless intake is excessive (for example, protein supplements for bodybuilding). Protein intake should match the recommended dietary intake to support growth52. However, for children with problematic polyuria, adjusting protein intake closer to the theoretical minimum requirements for age (or height-age) might be helpful.
Drug treatment for reducing polyuria
In addition to dietary modifications, which decrease the renal osmotic load, medications to reduce urine output are available, most notably diuretics and prostaglandin synthesis (cyclooxygenase (COX)) inhibitors4,43,46,53,54 (Table 3 and Supplementary Box 6).
In symptomatic infants and children with NDI, we recommend starting treatment with a thiazide and prostaglandin synthesis inhibitors. Thiazide diuretics act by inducing mild volume depletion and can reduce diuresis by up to 50% in the short term, when combined with a low-salt diet. This effect is presumably mediated by hypovolaemia-induced increase in proximal sodium and water reabsorption, thereby diminishing water delivery to the anti-diuretic hormone-sensitive sites in the collecting tubules and reducing the urine output55. Of note, in the long term, a much more moderate reduction in urine volume is usually observed.
Drug treatment can be very effective in infancy, with reported instances of marked hyponatraemia in patients who maintained an unchanged high fluid intake after commencement of drug treatment56,57. Thus, close monitoring of fluid balance, weight and biochemistry is recommended at the start of treatment and patients should be given as much control as possible to self-determine their fluid intake. In patients with hypokalaemia induced by thiazides, we recommend the addition of amiloride58.
Drug treatment is often discontinued with increasing age — in a multi-centre study, treatment with at least one medication decreased from 85% in childhood to 56% in adulthood, likely reflecting a perceived lack of efficacy and/or concern about side effects47. Whether lack of efficacy reflects inadequate dose adjustment, non-adherence to the prescribed medications or a true change in the physiological response to the treatment is currently unclear.
Similarly, the extent to which chronic use of prostaglandin synthesis inhibitors contributes to the progression of chronic kidney disease (CKD) — ~50% of adult patients with NDI also have CKD stage ≥2 — remains unclear47. Arguably, effective reduction in urine volume not only improves quality of life but can help to preserve kidney function by ameliorating urinary tract dilatation, bladder dysfunction and/or bladder-emptying problems. Thus, we recommend regular assessment of ongoing drug treatment based on a careful balance of risks and benefits.
Rationale for follow-up in children
A key symptom of NDI, especially in infancy, is growth failure. Consequently, height and weight are key parameters at each follow-up (Table 4). Basic plasma (Na, K, Cl, HCO3, creatinine, osmolality) and urine (osmolality) biochemistry also helps to monitor treatment, including the potential side effects of diuretics (if used).
Toilet training
No studies have investigated toilet training in patients with NDI. No data suggest that control of bladder function by the nervous system is different in children with NDI from that in others. Hence, we recommend performing toilet training in children with NDI as in any other child59. However, given the large urine volumes in NDI, accidents can be more frequent and noticeable than in children with intact urinary concentrating ability, and full continence is usually reached only in the second decade of life.
Some studies report a high incidence of night incontinence (referred to as ‘bed flooding’ by some parents because of the large urine volumes) in children with NDI, with urine continence at night achieved at a median age of 8–11 years46,47. Some parents use ‘double nappies’ to contain the urine volumes at night (that is, the use of a larger (for example, adult) nappy around the child’s usual nappy, so that overflow from the inner nappy is absorbed by the outer one). As indicated by our patient representatives, some parents use one or two mattress covers and change diapers several times during the night.
Urinary tract pathology
Based on our clinical experience, we recommend kidney ultrasound at least once every 2 years to monitor for urinary tract pathology, referred by some clinicians as ‘flow uropathy’, to describe the dilatation of the upper urinary tract, and/or bladder dysfunction caused by polyuria46,47.
In a single-centre retrospective study, urological complications were noted in 46% of patients with NDI. Nocturnal enuresis and incomplete voiding were most frequently observed, but large bladder capacity and unilateral or bilateral hydronephrosis were also reported46. In a retrospective study involving 315 patients with NDI, hydronephrosis was reported in 34% of cases47. However, in some patients, this alteration can be physiological and radiologists therefore commonly advise performing an ultrasound of the urinary tract with a filled bladder, which can lead to a transient upper tract dilatation that resolves after voiding. However, repeated or ongoing dilatation can lead to permanent damage to the urinary tract and/or the kidneys.
Anecdotal reports show evidence of obstruction in patients with a thick-walled bladder and post-micturition residual volume, which can be managed by cystostomy button drainage60. In another small retrospective study of 26 patients with diabetes insipidus (CDI and NDI) and hydroureteronephrosis, diagnostic tests revealed detrusor underactivity (42.3%), a contractile detrusor (15.4%) and reduced bladder sensations (53.9%)61.
For diagnostic evaluation, uroflowmetry is advised to exclude dysfunctional voiding. In addition, (video)urodynamic studies can be performed to assess bladder dysfunction in more detail. In patients with signs of urinary tract pathology, we recommend involvement of urologists, especially when invasive diagnostic tests or treatments such as clean intermittent catheterization are considered. Obviously, the importance of regular and frequent bladder emptying should be discussed with the patient to minimize further damage from ongoing dilatation. In addition, maximizing medical treatment to reduce urine volume can be considered.
Treatment and follow-up in adults
Rationale for dietary recommendations
As NDI is characterized by water diuresis, patients should be advised to primarily drink water or other non-caloric beverages. The consumption of high-calorie drinks can contribute to the high incidence of obesity (41% versus 16% European average; P < 0.001) that is observed in adult patients with NDI47. To reduce the renal osmotic load, the recommended dietary targets are reduction of salt intake to ≤6 g/day and protein intake to ≤1 g/kg/day (Box 4). In practice, adherence to these recommendations is often challenging and malnutrition should be avoided. We recommend dietetic counselling to assess salt and protein intake, and provide individualized advice based on these recommendations.
Rationale for drug treatment in adults
Adults typically have an intact thirst drive and can maintain appropriate fluid intake to match their large urinary output. No studies have systematically investigated the impact of tapering or withdrawing COX inhibitors and/or thiazides in adult patients with NDI. Therefore, we recommend continuing or withdrawing thiazide diuretics depending on patient preference and on medical reasons (for example, development of thiazide-induced chronic hypokalaemia, gout, hypercholesterolaemia or non-melanoma skin cancer62). Owing to concerns of nephrotoxicity, we recommend discontinuing COX inhibitors once patients reach adulthood (≥18 years of age), or even earlier if full continence is achieved. Our personal observation (Stephen B. Walsh) suggests that most patients do not experience or mind a change in urine volume after discontinuing COX inhibitors or thiazide diuretics. However, our patient representatives mentioned that some patients drink more after discontinuation of these medications and feel more tired than before. In patients who prefer to continue treatment with thiazide diuretics, hydrochlorothiazide 25 mg once or twice daily is typically recommended. Moreover, we recommend reducing salt intake as salt restriction potentiates the efficacy of diuretics.
In the case of thiazide-induced hypokalaemia, thiazide diuretics can be combined with amiloride, potentially leading to a further reduction in urine output63,64. The effects of chronic thiazide use on long-term kidney outcomes are unknown.
Rationale for follow-up in adults
For adults with stable disease and stable estimated glomerular filtration rate, annual follow-up can be sufficient (Table 4). For those with unresolved bladder dysfunction, more frequent follow-up by nephrologists and urologists might be desirable (for example, every 3–4 months). A more frequent follow-up schedule is warranted when withdrawing diuretics and COX inhibitors. As mentioned earlier, NDI is associated with an increased prevalence of CKD compared with a population-based cohort47. which is probably related to voluntary retention of urine leading to ‘flow uropathy’. Patients with progressive CKD or CKD stage ≥G4 benefit from more frequent follow-up as per KDIGO65 or local guidelines. Unless an acute indication for imaging is present, we recommend conducting surveillance imaging once every 2 years (extended to 5 years, if the patient is stable). Kidney ultrasound for evaluating dilatation of ureters and the kidney pelvis should ideally be performed before and after emptying the bladder because in approximately one third of patients, dilatation will improve with double voiding rather than urological interventions (personal experience of Daniel G. Bichet).
As NDI is a rare disease and inadequate treatment, particularly of functional bladder outflow obstruction, is associated with poorer long-term outcome, we recommend that patients should have access to tertiary care centres with experience in NDI management. This approach facilitates clinical and genetic diagnosis, as well as access to specialist bladder outflow urology, if needed, and optimizes treatment and patient education. For patients who reside far from a specialist centre, follow-up can be shared with a local nephrologist and urologist.
Polyuria and polydipsia seem to ameliorate with age, independent of estimated glomerular filtration rate (personal experience of Daniel G. Bichet). Therefore, we suggest revising dietary and pharmacological prescriptions in patients from the age of 60. Finally, we emphasize that patient education and attention to psychosocial aspects of the disease are important, including sleep problems and limitations during work and daily life.
Emergency management
When patients with NDI have incidental disease, especially when they are admitted to hospital, their specific fluid requirements are often not appreciated by medical and nursing staff. This oversight is especially problematic if patients cannot maintain adequate oral intake and/or receive parenteral fluids. Close liaison with a specialist from the tertiary specialized centre should be sought in these circumstances (Box 5); patients should have contact details of their specialist physicians and wear medic alert bracelets or cards (Supplementary Box 7).
The typical emergency in NDI is hypernatraemic dehydration because of excessive water loss (for example, due to diarrhoea) and/or the inability to maintain adequate fluid intake (for example, vomiting). Hypernatraemic dehydration indicates a deficiency in water and consequently patients should be treated with water. By the time a patient with NDI presents with hypernatraemic dehydration, oral rehydration has usually failed and consequently, there should be a low threshold for intravenous rehydration.
Salt-containing solutions, especially NaCl 0.9% solutions, should be avoided because of their large renal osmotic load. The tonicity of such fluids (~300 mOsm/kg H2O) exceeds the typical urine osmolality in NDI (~100 mOsm/kg H2O) by about 3-fold. Consequently, around 3 l of urine are needed to excrete the renal osmotic load provided by 1 l of isotonic fluid, risking serious hypernatraemia43,66. Therefore, we recommend using water with dextrose (for example, 5% dextrose) and to calculate the initial rate of fluid administration based on a physiological demand. Routine maintenance rate (in children — first 10 kg: 100 ml/kg/24 h; 10–20 kg: 50 ml/kg/24 h; remaining 50 kg: 20 ml/kg/24 h; in adults — 25–30 ml/kg/24 h) is usually a good starting volume67,68. As 5% dextrose delivers no renal osmotic load, application at this rate will result in a slow decrease in plasma osmolality, unless there are excessive ongoing fluid losses (for example, diarrhoea). A common concern associated with the use of dextrose 5% solutions is a rapid decrease in plasma sodium concentration, which poses the risk of brain oedema. This concern does not usually apply to patients with NDI, as their urine is diluted with a very low sodium concentration and consequently, the hypotonic intravenous fluid matches the urinary losses. Importantly, dextrose 5% solution should not be administered as a bolus because of the risk of a rapid decrease in serum sodium. Isotonic fluids are appropriate for acute fluid resuscitation in patients in hypovolaemic shock. However, as intravascular volume is relatively well preserved in hypernatraemic dehydration, this is an exceedingly rare scenario in patients with NDI. Following the administration of isotonic fluid, sufficient free water should be provided to allow excretion of the renal osmotic load. If possible, the patient should be allowed to drink to thirst. Oral feeding should be provided as soon as tolerated and oral fluids should be included in the fluid balance.
In hospitalized patients, we recommend a close observation of clinical status, including neurological condition, fluid balance, weight and electrolytes. Placement of a urinary catheter should be considered to ensure proper monitoring of diuresis. Fluid composition and administration rate might need to be adjusted based on the rate and composition of ongoing losses — if the losses contain substantial concentrations of sodium, replacement of those losses with a fluid that contains a similar sodium concentration is appropriate. The aim for the overall administration rate is to balance losses, plus replacement of the fluid deficit over 48 h, and to avoid a decrease in serum sodium above 8 mmol/l/day in case of hypertonic dehydration.
We recommend treatment of patients with NDI and hypernatraemic dehydration in specialized centres to avoid potential life-threatening complications of inadequate fluid administration. Expert consultations are recommended for patients undergoing anaesthesia or surgery.
Genetic counselling and family planning
The detection of pathogenic variant(s) in either AVPR2 or AQP2 is crucial for genetic counselling. We strongly recommend counselling for young adults who are affected (hemizygous for AVPR2 pathogenic variant), who are heterozygotes for an AVPR2 or AQP2 pathogenic variant, or who are at risk of being heterozygous (Box 6). They should be informed about the inheritance of NDI, the related recurrence risks, and the implications of the results of the genetic test for family planning, including reproductive options. This discussion should take place soon after the genetic diagnosis has been confirmed and certainly before pregnancy15. Prenatal testing for a pregnancy at increased risk and preimplantation genetic testing (PGT) are, however, only possible if the disease-causing pathogenic variant(s) has/have been identified. The use of these tests should be discussed by a multidisciplinary team, according to the legislation of each country.
In the case of X-linked NDI or dominant NDI, counselling should also include information about the potential implications of the pathogenic variant(s) for family members. Patients should be encouraged to share that information with their family members at risk. These family members can then be counselled and, when applicable, undergo genetic testing.
Unanswered questions and research agenda
The expert group identified several knowledge gaps and unmet needs regarding NDI that demand further research (Box 7). One important unanswered question concerns the long-term psychosocial outcomes of patients with NDI. Although a few studies have indicated that mental health conditions are more prevalent in patients with NDI than in the general population4,17,46,47, the degree of these problems remains to be determined, as well as their aetiology (for example, these conditions might reflect a primary manifestation of the disease or a secondary manifestation owing to complications such as dehydration-induced brain alterations).
Another pressing need is the development of targeted therapies for NDI based on the current knowledge of the underlying molecular defects. Here, we discuss some potential targeted therapies studied in vitro and/or in animal models in vivo. Only very few clinical trials in NDI have been performed, and these ended prematurely, owing to safety issues or lack of efficacy.
In vitro expression studies have demonstrated that most AVPR2 pathogenic variants associated with X-linked NDI, as well as all AQP2 pathogenic variants related to autosomal-recessive NDI, lead to the production of fully translated proteins. However, these proteins are misfolded and are consequently retained within the endoplasmic reticulum (ER). Agents that restore routing from the ER to the plasma membrane are under investigation as potential treatments. Promising agents for X-linked NDI include cell-permeable AVPR2 antagonists and agonists that rescue the intracellular retention of several AVPR2 mutants69,70,71,72. Remarkably, certain cell-permeable AVPR2 agonists have been shown to activate NDI-causing V2R mutant proteins at their intracellular location without changing their maturation and at a sufficient level to induce the translocation of AQP2 to the apical membrane. This finding indicates that non-peptide AVPR2 agonists constitute another promising treatment for NDI resulting from intracellularly retained AVPR2 mutants73. A clinical study in which patients with NDI and AVPR2 missense mutations were treated with a vasopressin 1a receptor (AVPR1A) antagonist had to be terminated early owing to possible interference with the cytochrome P450 metabolic pathway74, despite having beneficial effects on urine volume and osmolality.
Other therapeutic approaches relying on AVP-independent trafficking of AQP2 to the apical membrane have been proposed and tested in vitro and/or in animal models. One example of these AVP-independent approaches relies on activation of the cyclic adenosine monophosphate (cAMP) pathway by stimulating other G protein coupled receptors (GPCRs) such as the E-prostanoid receptors. Stimulation of the E-prostanoid receptor EP4 greatly reduced urine volumes in a conditional Avpr2-deletion mouse model by raising AQP2 levels75. The rise in AQP2 levels most probably resulted from enhanced cAMP production induced by EP4 stimulation. A similar effect was observed after stimulation of the EP2 receptor with the agonist butaprost76. The EP2 receptor is a more interesting candidate for treatment of NDI than the EP4 receptor because EP2 agonists have already been tested in clinical studies for other diseases with promising results and an acceptable safety profile77,78,79. Another potential AVP-independent therapeutic strategy involves the activation of the cyclic guanosine monophosphate (cGMP) signalling pathway. Several research groups have shown that nitric oxide donors and atrial natriuretic factor stimulate the insertion of AQP2 in kidney epithelial cells in vitro and in vivo via a cGMP-dependent pathway80,81. The selective cGMP phosphodiesterase inhibitor sildenafil citrate (also known as Viagra), prevents degradation of cGMP, resulting in increased membrane expression in AQP2 in vitro and in vivo82. However, in a small clinical trial in patients with NDI, treatment with sildenafil citrate or riociguat (soluble guanylate cyclase stimulator) neither decreased urine volume nor increased urine osmolality83. Given that the oral antidiabetic drug metformin increases AQP2 phosphorylation and accumulation in the apical membrane in animal models, a trial in a small number of individuals with hereditary NDI was started in 2015 but was quickly terminated because of lack of efficacy84. Interestingly, a 2021 report demonstrated that a direct activator of AMP-activated protein kinase (AMPK), which also phosphorylates AQP2, increased urine concentration in NDI rats treated with the V2R blocker tolvaptan and in V2R-deficient mice85.
In knock-in-dominant NDI mice, the phosphodiesterase-4 inhibitor rolipram increased cAMP levels, leading to increased AQP2 phosphorylation and translocation to the apical membrane86. However, phosphodiesterase-4 is an abundantly expressed protein involved in immunosuppressive and anti-inflammatory pathways, and its inhibition can therefore have severe side effects. Rolipram was tested decades ago in two male patients with X-linked NDI and did not cause any relief of symptoms87, but the potential for other PDE inhibitors in the treatment of NDI should be examined further. Another drug that has recently received attention is the antifungal fluconazole, which increased plasma membrane AQP2 expression in collecting duct principal cells, independently from AVP, and reduced urinary output in mice treated with tolvaptan88. An ongoing clinical trial will test the efficacy of fluconazole in patients with NDI89. Gene therapy might represent a future treatment option for NDI but many challenges remain for gene-therapeutic approaches, especially in terms of efficiency90.
Conclusions
Despite enormous advances in the understanding of the genetic causes and pathophysiology of congenital NDI in recent decades, the clinical care for patients remains challenging. Here, we formulate clinical practice recommendations for diagnostics, treatment, follow-up, emergency management, genetic counselling and family planning in patients with NDI (Boxes 2–6). These recommendations are largely expert-based consensus opinions of the core group, validated by a voting panel in a Delphi process. For most of these recommendations, full supportive evidence is not yet available; one-third of these recommendations are graded at level X, indicating exceptional situations where validating studies cannot be performed. To generate additional evidence for the other recommendations, longitudinal studies in large patient groups (both children and adults), and clinical trials are necessary. For now, we hope that the recommendations presented here can serve as a foundational framework to guide clinicians in their care for patients with NDI.
References
Knoers, N. V. A. M., Levtchenko, E. & Bichet, D. G. In Pediatric Nephrology (eds Francesco, E. et al.) 1063–1085 (Springer International, 2022).
Arima, H. et al. Changing the name of diabetes insipidus: a position statement of the working group for renaming diabetes insipidus. J. Clin. Endocrinol. Metab. 108, 1–3 (2022).
Bockenhauer, D., Knoers, N. & Bichet, D. G. What’s in a name? That which we call diabetes does not taste sweet! Pediatr. Nephrol. 38, 937–939 (2023).
D’Alessandri-Silva, C. et al. Diagnosis, treatment, and outcomes in children with congenital nephrogenic diabetes insipidus: a pediatric nephrology research consortium study. Front. Pediatr. 7, 550 (2019).
Prosperi, F. et al. Characterization of five novel vasopressin V2 receptor mutants causing nephrogenic diabetes insipidus reveals a role of tolvaptan for M272R-V2R mutation. Sci. Rep. 10, 16383 (2020).
Bichet, D. G. & Bockenhauer, D. Genetic forms of nephrogenic diabetes insipidus (NDI): vasopressin receptor defect (X-linked) and aquaporin defect (autosomal recessive and dominant). Best. Pract. Res. Clin. Endocrinol. Metab. 30, 263–276 (2016).
Bockenhauer, D. & Bichet, D. G. Pathophysiology, diagnosis and management of nephrogenic diabetes insipidus. Nat. Rev. Nephrol. 11, 576–588 (2015).
Chen, Y. et al. A reporting tool for practice guidelines in health care: the RIGHT Statement. Ann. Intern. Med. 166, 128–132 (2017).
Guyatt, G. H. et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J. Clin. Epidemiol. 64, 395–400 (2011).
Management, A. A. O. P. S. C. O. Q. I. a. Classifying recommendations for clinical practice guidelines. Pediatrics 114, 874–877 (2004).
Flynn, J. T. et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140, e20171904 (2017).
Wesche, D., Deen, P. M. & Knoers, N. V. Congenital nephrogenic diabetes insipidus: the current state of affairs. Pediatr. Nephrol. 27, 2183–2204 (2012).
Moeller, H. B., Rittig, S. & Fenton, R. A. Nephrogenic diabetes insipidus: essential insights into the molecular background and potential therapies for treatment. Endocr. Rev. 34, 278–301 (2013).
Joshi, S. et al. Novel and recurrent variants in AVPR2 in 19 families with X-linked congenital nephrogenic diabetes insipidus. Eur. J. Pediatr. 177, 1399–1405 (2018).
Knoers, N. & Lemmink, H. Hereditary nephrogenic diabetes insipidus. in: M. P. Adam et al. (eds) GeneReviews(®) (University of Washington, Seattle Copyright © 1993–2023, University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved., 1993) (2000, updated 2020).
Forssman, H. Is hereditary diabetes insipidus of nephrogenic type associated with mental deficiency? Acta Psychiatr. Neurol. Scand. 30, 577–587 (1955).
Hoekstra, J. A., van Lieburg, A. F., Monnens, L. A., Hulstijn-Dirkmaat, G. M. & Knoers, V. V. Cognitive and psychosocial functioning of patients with congenital nephrogenic diabetes insipidus. Am. J. Med. Genet. 61, 81–88 (1996).
Bichet, D. G. Genetics in endocrinology pathophysiology, diagnosis and treatment of familial nephrogenic diabetes insipidus. Eur. J. Endocrinol. 183, R29–r40 (2020).
Hureaux, M. & Vargas-Poussou, R. Genetic basis of nephrogenic diabetes insipidus. Mol. Cell Endocrinol. 560, 111825 (2023).
Ishida, A. et al. Partial nephrogenic diabetes insipidus with a novel arginine vasopressin receptor 2 gene variant. Clin. Pediatr. Endocrinol. 31, 44–49 (2022).
Arthus, M. F. et al. Report of 33 novel AVPR2 mutations and analysis of 117 families with X-linked nephrogenic diabetes insipidus. J. Am. Soc. Nephrol. 11, 1044–1054 (2000).
Moses, A. M., Sangani, G. & Miller, J. L. Proposed cause of marked vasopressin resistance in a female with an X-linked recessive V2 receptor abnormality. J. Clin. Endocrinol. Metab. 80, 1184–1186 (1995).
van Lieburg, A. F. et al. Clinical phenotype of nephrogenic diabetes insipidus in females heterozygous for a vasopressin type 2 receptor mutation. Hum. Genet. 96, 70–78 (1995).
Migeon, B. R. X inactivation, female mosaicism, and sex differences in renal diseases. J. Am. Soc. Nephrol. 19, 2052–2059 (2008).
Satoh, M., Ogikubo, S. & Yoshizawa-Ogasawara, A. Correlation between clinical phenotypes and X-inactivation patterns in six female carriers with heterozygote vasopressin type 2 receptor gene mutations. Endocr. J. 55, 277–284 (2008).
Morgenthaler, N. G., Struck, J., Alonso, C. & Bergmann, A. Assay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressin. Clin. Chem. 52, 112–119 (2006).
Timper, K. et al. Diagnostic accuracy of copeptin in the differential diagnosis of the polyuria-polydipsia syndrome: a prospective multicenter study. J. Clin. Endocrinol. Metab. 100, 2268–2274 (2015).
Fenske, W. et al. A copeptin-based approach in the diagnosis of diabetes insipidus. N. Engl. J. Med. 379, 428–439 (2018).
Christ-Crain, M. & Gaisl, O. Diabetes insipidus. Presse Med. 50, 104093 (2021).
Winzeler, B. et al. Arginine-stimulated copeptin measurements in the differential diagnosis of diabetes insipidus: a prospective diagnostic study. Lancet 394, 587–595 (2019).
Refardt, J. et al. Arginine or hypertonic saline-stimulated copeptin to diagnose AVP deficiency. N. Engl. J. Med. 389, 1877–1887 (2023).
Vergier, J. et al. Rapid differential diagnosis of diabetes insipidus in a 7-month-old infant: the copeptin approach. Arch. Pediatr. 25, 45–47 (2018).
Tuli, G., Tessaris, D., Einaudi, S., Matarazzo, P. & De Sanctis, L. Copeptin role in polyuria-polydipsia syndrome differential diagnosis and reference range in paediatric age. Clin. Endocrinol. 88, 873–879 (2018).
Bitencourt, L. et al. The usefulness of copeptin for the diagnosis of nephrogenic diabetes insipidus in infancy: a case report. J. Pediatr. Endocrinol. Metab. 34, 1475–1479 (2021).
Bonnet, L. et al. Copeptin assays in children for the differential diagnosis of polyuria-polydipsia syndrome and reference levels in hospitalized children. Clin. Endocrinol. 96, 47–53 (2022).
Binder, G., Weber, K., Peter, A. & Schweizer, R. Arginine-stimulated copeptin in children and adolescents. Clin. Endocrinol. 98, 548–553 (2023).
Monnens, L., Smulders, Y., van Lier, H. & de Boo, T. DDAVP test for assessment of renal concentrating capacity in infants and children. Nephron 29, 151–154 (1981).
Bichet, D. G. Evaluation of Patients with Polyuria. http://www.uptodate.com (2023).
De Wardener, H. E. & Herxheimer, A. The effect of a high water intake on the kidney’s ability to concentrate the urine in man. J. Physiol. 139, 42–52 (1957).
Verbalis, J. G. Whole-body volume regulation and escape from antidiuresis. Am. J. Med. 119, S21–S29 (2006).
Moritz, M. L. & Ayus, J. C. Maintenance intravenous fluids in acutely Ill patients. N. Engl. J. Med. 373, 1350–1360 (2015).
Gennari, F. J. & Kassirer, J. P. Osmotic diuresis. N. Engl. J. Med. 291, 714–720 (1974).
Bockenhauer, D. & Bichet, D. G. Nephrogenic diabetes insipidus. Curr. Opin. Pediatr. 29, 199–205 (2017).
Rees, L. et al. Delivery of a nutritional prescription by enteral tube feeding in children with chronic kidney disease stages 2–5 and on dialysis — clinical practice recommendations from the Pediatric Renal Nutrition Taskforce. Pediatr. Nephrol. 36, 187–204 (2021).
Lejarraga, H., Caletti, M. G., Caino, S. & Jiménez, A. Long-term growth of children with nephrogenic diabetes insipidus. Pediatr. Nephrol. 23, 2007–2012 (2008).
Sharma, S. et al. Long-term outcome in inherited nephrogenic diabetes insipidus. Clin. Kidney J. 12, 180–187 (2019).
Lopez-Garcia, S. C. et al. Treatment and long-term outcome in primary nephrogenic diabetes insipidus. Nephrol. Dial. Transpl. https://doi.org/10.1093/ndt/gfaa243 (2020).
Qizalbash, L., Cleghorn, S., McAlister, L. in: V. Shaw (ed.) Clinical Paediatric Dietetics. 238 (Wiley-Blackwell 2020).
Sasaki, G. et al. Growth failure in an infant with congenital nephrogenic diabetes insipidus during sodium restriction. Clin. Pediatr. Endocrinol. 16, 95–98 (2007).
Haycock, G. B. The influence of sodium on growth in infancy. Pediatr. Nephrol. 7, 871–875 (1993).
Scientific advisory committee on nutrition. Salt and Health. (The Stationery Office, 2003).
Coleman, J. in: V. Shaw, Lawson, M. (eds) Clinical Paediatric Dietetics. 1324, (Blackwell Science Ltd, 2001).
Bockenhauer, D. & Bichet, D. G. Urinary concentration: different ways to open and close the tap. Pediatr. Nephrol. 29, 1297–1303 (2014).
Mortensen, L. A., Bistrup, C., Jensen, B. L. & Hinrichs, G. R. A mini-review of pharmacological strategies used to ameliorate polyuria associated with X-linked nephrogenic diabetes insipidus. Am. J. Physiol. Renal Physiol. 319, F746–F753 (2020).
Earley, L. E. & Orloff, J. The mechanism of antidiuresis associated with the administration of hydrochlorothiazide to patients with vasopressin-resistant diabetes insipidus. J. Clin. Invest. 41, 1988–1997 (1962).
Anton-Gamero, M., Garcia-Martinez, E., Fernandez-Ramos, J., Rodríguez-Salas, M. & Gil-Campos, M. Nephrogenic diabetes insipidus: the key element of paradoxical hyponatremia. Pediatr. Nephrol. 24, 2277–2278 (2009).
Boussemart, T., Nsota, J., Martin-Coignard, D. & Champion, G. Nephrogenic diabetes insipidus: treat with caution. Pediatr. Nephrol. 24, 1761–1763 (2009).
Kirchlechner, V., Koller, D. Y., Seidl, R. & Waldhauser, F. Treatment of nephrogenic diabetes insipidus with hydrochlorothiazide and amiloride. Arch. Dis. Child. 80, 548–552 (1999).
Wu, H. Y. Achieving urinary continence in children. Nat. Rev. Urol. 7, 371–377 (2010).
Colliver, D., Storey, R., Dickens, H. & Subramaniam, R. Nonobstructive urinary tract dilatation in children with diabetes insipidus. J. Pediatr. Surg. 47, 752–755 (2012).
Wang, X. et al. Upper urinary dilatation and treatment of 26 patients with diabetes insipidus: a single-center retrospective study. Front. Endocrinol. 13, 941453 (2022).
Pedersen, S. A. et al. Hydrochlorothiazide use and risk of nonmelanoma skin cancer: a nationwide case-control study from Denmark. J. Am. Acad. Dermatol. 78, 673–681.e679 (2018).
Alon, U. & Chan, J. C. Hydrochlorothiazide-amiloride in the treatment of congenital nephrogenic diabetes insipidus. Am. J. Nephrol. 5, 9–13 (1985).
Konoshita, T. et al. Treatment of congenital nephrogenic diabetes insipidus with hydrochlorothiazide and amiloride in an adult patient. Horm. Res. 61, 63–67 (2004).
Levin, A. et al. Kidney disease: improving global outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 3, 1–150 (2013).
Guarino, S. et al. Nephrogenic diabetes insipidus in childhood: assessment of volume status and appropriate fluid replenishment. Pediatr. Emerg. Care 36, e402–e404 (2020).
Holliday, M. A. & Segar, W. E. The maintenance need for water in parenteral fluid therapy. Pediatrics 19, 823–832 (1957).
National Institute for Health and Care Excellence. Intravenous fluid therapy in adults in hospital. Clinical guideline [CG174], http://www.nice.org.uk/Guidance/CG174 (2013, updated 2017).
Erdem Tuncdemir, B., Mergen, H. & Saglar Ozer, E. Evaluation of pharmacochaperone-mediated rescue of mutant V2 receptor proteins. Eur. J. Pharmacol. 865, 172803 (2019).
Morello, J. P. et al. Pharmacological chaperones rescue cell-surface expression and function of misfolded V2 vasopressin receptor mutants. J. Clin. Invest. 105, 887–895 (2000).
Ranadive, S. A. et al. Identification, characterization and rescue of a novel vasopressin-2 receptor mutation causing nephrogenic diabetes insipidus. Clin. Endocrinol. 71, 388–393 (2009).
Robben, J. H., Sze, M., Knoers, N. V. & Deen, P. M. Functional rescue of vasopressin V2 receptor mutants in MDCK cells by pharmacochaperones: relevance to therapy of nephrogenic diabetes insipidus. Am. J. Physiol. Renal Physiol. 292, F253–F260 (2007).
Robben, J. H. et al. Intracellular activation of vasopressin V2 receptor mutants in nephrogenic diabetes insipidus by nonpeptide agonists. Proc. Natl Acad. Sci. USA 106, 12195–12200 (2009).
Bernier, V. et al. Pharmacologic chaperones as a potential treatment for X-linked nephrogenic diabetes insipidus. J. Am. Soc. Nephrol. 17, 232–243 (2006).
Li, J. H. et al. A selective EP4 PGE2 receptor agonist alleviates disease in a new mouse model of X-linked nephrogenic diabetes insipidus. J. Clin. Invest. 119, 3115–3126 (2009).
Olesen, E. T., Rützler, M. R., Moeller, H. B., Praetorius, H. A. & Fenton, R. A. Vasopressin-independent targeting of aquaporin-2 by selective E-prostanoid receptor agonists alleviates nephrogenic diabetes insipidus. Proc. Natl Acad. Sci. USA 108, 12949–12954 (2011).
Aihara, M. et al. Pharmacokinetics, safety, and intraocular pressure-lowering profile of omidenepag isopropyl, a selective, nonprostaglandin, prostanoid EP2 receptor agonist, in healthy Japanese and Caucasian volunteers (phase I study). J. Ocul. Pharmacol. Ther. 35, 542–550 (2019).
Steinwall, M., Akerlund, M., Bossmar, T., Nishii, M. & Wright, M. ONO-8815Ly, an EP2 agonist that markedly inhibits uterine contractions in women. BJOG 111, 120–124 (2004).
Aihara, M. et al. Phase 2, randomized, dose-finding studies of omidenepag isopropyl, a selective EP2 agonist, in patients with primary open-angle glaucoma or ocular hypertension. J. Glaucoma 28, 375–385 (2019).
Boone, M., Kortenoeven, M., Robben, J. H. & Deen, P. M. Effect of the cGMP pathway on AQP2 expression and translocation: potential implications for nephrogenic diabetes insipidus. Nephrol. Dial. Transpl. 25, 48–54 (2010).
Bouley, R. et al. Nitric oxide and atrial natriuretic factor stimulate cGMP-dependent membrane insertion of aquaporin 2 in renal epithelial cells. J. Clin. Invest. 106, 1115–1126 (2000).
Bouley, R. et al. Stimulation of AQP2 membrane insertion in renal epithelial cells in vitro and in vivo by the cGMP phosphodiesterase inhibitor sildenafil citrate (Viagra). Am. J. Physiol. Renal Physiol. 288, F1103–F1112 (2005).
Hinrichs, G. R. et al. Treatment of nephrogenic diabetes insipidus patients with cGMP-stimulating drugs does not mitigate polyuria or increase urinary concentrating ability. Kidney Int. Rep. 5, 1319–1325 (2020).
ClinicalTrials.gov. US National Library of Medicine. https://clinicaltrials.gov/study/NCT02460354 (2018).
Klein, J. D. et al. An AMPK activator as a therapeutic option for congenital nephrogenic diabetes insipidus. JCI Insight 6, e146419 (2021).
Sohara, E. et al. Pathogenesis and treatment of autosomal-dominant nephrogenic diabetes insipidus caused by an aquaporin 2 mutation. Proc. Natl Acad. Sci. USA 103, 14217–14222 (2006).
Bichet, D. G., Ruel, N., Arthus, M. F. & Lonergan, M. Rolipram, a phosphodiesterase inhibitor, in the treatment of two male patients with congenital nephrogenic diabetes insipidus. Nephron 56, 449–450 (1990).
Vukićević, T. et al. Fluconazole increases osmotic water transport in renal collecting duct through effects on aquaporin-2 trafficking. J. Am. Soc. Nephrol. 30, 795–810 (2019).
Treatment of congenital nephrogenic diabetes insipidus with fluconazole, an antifungal medication. https://www.clinicaltrialsregister.eu/ctr-search/trial/2020-002204-38/DK.
Davis, L. & Park, F. Gene therapy research for kidney diseases. Physiol. Genomics 51, 449–461 (2019).
Bockenhauer, D. & Bichet, D. G. Inherited secondary nephrogenic diabetes insipidus: concentrating on humans. Am. J. Physiol. Renal Physiol. 304, F1037–F1042 (2013).
Hudson, J. L., Baum, J. I., Diaz, E. C. & Børsheim, E. Dietary protein requirements in children: methods for consideration. Nutrients 13, 1554 (2021).
Richter, M. et al. Revised reference values for the intake of protein. Ann. Nutr. Metab. 74, 242–250 (2019).
Crawford, J. D. & Kennedy, G. C. Chlorothiazid in diabetes insipidus. Nature 183, 891–892 (1959).
Kennedy, G. C. & Crawford, J. D. Treatment of diabetes insipidus with hydrochlorothiazide. Lancet 1, 866–867 (1959).
Knoers, N. & Monnens, L. A. Amiloride-hydrochlorothiazide versus indomethacin-hydrochlorothiazide in the treatment of nephrogenic diabetes insipidus. J. Pediatr. 117, 499–502 (1990).
Gambaro, G. & Perazella, M. A. Adverse renal effects of anti-inflammatory agents: evaluation of selective and nonselective cyclooxygenase inhibitors. J. Intern. Med. 253, 643–652 (2003).
Jakobsson, B. & Berg, U. Effect of hydrochlorothiazide and indomethacin treatment on renal function in nephrogenic diabetes insipidus. Acta Paediatr. 83, 522–525 (1994).
Monnens, L., Jonkman, A. & Thomas, C. Response to indomethacin and hydrochlorothiazide in nephrogenic diabetes insipidus. Clin. Sci. 66, 709–715 (1984).
Rascher, W., Rosendahl, W., Henrichs, I. A., Maier, R. & Seyberth, H. W. Congenital nephrogenic diabetes insipidus-vasopressin and prostaglandins in response to treatment with hydrochlorothiazide and indomethacin. Pediatr. Nephrol. 1, 485–490 (1987).
Harris, R. C. Jr Cyclooxygenase-2 inhibition and renal physiology. Am. J. Cardiol. 89, 10d–17d (2002).
Libber, S., Harrison, H. & Spector, D. Treatment of nephrogenic diabetes insipidus with prostaglandin synthesis inhibitors. J. Pediatr. 108, 305–311 (1986).
Pattaragarn, A. & Alon, U. S. Treatment of congenital nephrogenic diabetes insipidus by hydrochlorothiazide and cyclooxygenase-2 inhibitor. Pediatr. Nephrol. 18, 1073–1076 (2003).
Acknowledgements
This project was initiated by the Working Group for Tubulopathies of ERKNet. ERKNet is funded by the European Union within the framework of the EU4Health Programme (101085068). We thank patient advocates, Elodie Martin and Lucas van Baelen, for their important participation in our discussions, bringing in their personal experiences and those of other patients, Louise McAlister (Great Ormond Street Hospital for Children NHS Foundation Trust, UK) for dietary advice, Tanja Wlodkowski and Stefanie Häberle (ERKNet project managers) for project support, and members of the voting panel for their careful evaluation of the recommendations.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, made substantial contributions to discussions of the content, and wrote, reviewed or edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Nephrology thanks Gitte Hinrichs, Julie Refardt and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Levtchenko, E., Ariceta, G., Arguedas Flores, O. et al. International expert consensus statement on the diagnosis and management of congenital nephrogenic diabetes insipidus (arginine vasopressin resistance). Nat Rev Nephrol 21, 83–96 (2025). https://doi.org/10.1038/s41581-024-00897-z
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41581-024-00897-z
This article is cited by
-
Copeptin in the diagnosis and management of renal tubular disorders
Pediatric Nephrology (2025)