Abstract
Despite advances in HIV-1 prophylaxis, vertical transmission remains a pressing problem in developing countries1. Given the promise of broadly neutralizing antibodies (bNAbs) for HIV-1 prevention2, we hypothesized that neonatal delivery of bNAbs using adeno-associated virus (AAV) could provide durable HIV-1 immunity during infancy. Here, using infant rhesus macaques (Macaca mulatta) as a model, we show that a one-time administration of an AAV vector encoding bNAb 3BNC117 at birth led to sustained bNAb expression for more than three years without redosing. This approach significantly protected both infant and pre-adolescent rhesus macaques from infection with simian–human immunodeficiency virus in mucosal challenge models that mimic HIV-1 transmission through breastfeeding and sexual intercourse. Age at the time of AAV-3BNC117 administration was a main determinant of success and was inversely correlated with the incidence of host anti-drug antibodies that restricted bNAb expression. Consistent with principles of neonatal tolerance3,4, newborn rhesus macaques exhibited higher levels of bNAb expression than older infants and juveniles following AAV-3BNC117 dosing. Furthermore, in utero exposure to recombinant 3BNC117 suppressed anti-drug antibodies and improved AAV-vectored delivery of this bNAb in older infants. Thus, our results suggest that neonatal and fetal immunological tolerance can be leveraged to improve postnatal AAV delivery of HIV-1 bNAbs in primates. Since years-long HIV-1 immunity can be generated in rhesus macaques from a one-time AAV vector administration at birth, future studies should evaluate the ability of this strategy to prevent perinatal and adolescent HIV-1 infections in humans.
Similar content being viewed by others
Main
Every year, more than 100,000 children acquire HIV-1, with the majority of cases occurring in sub-Saharan Africa due to vertical transmission1. Complex social and economic barriers continue to hinder efforts to eliminate perinatal HIV-1 transmission in the region, with gender power imbalances having a key role5. Many women lack the ability to negotiate condom use with their male partners, leaving them vulnerable to HIV-1 and unintended pregnancies. Compounding these issues, only half of pregnant and breastfeeding women who are living with HIV-1 in western and central Africa were receiving antiretroviral (ARV) therapy in 20231. These regions now account for 41% of all paediatric HIV-1 infections worldwide1. Adherence to ARV therapy often declines postpartum, particularly among young mothers who disengage from care after delivery1. Treatment lapses increase maternal viraemia and the risk of transmission through breastfeeding. Meanwhile, paediatric formulations of ARV therapies, which are used for both prophylaxis and therapy, are limited, difficult to administer and undermined by drug toxicity and resistance6,7. Although long-acting ARV therapies may improve patient compliance, their use in infants remains unproven and constrained by access8.
One promising strategy for averting paediatric HIV-1 infections is passive immunization with recombinant bNAbs9. These antibodies are safe for use in infants and have shown efficacy in preclinical and clinical studies10,11,12. However, their protective effect depends on repeated infusions, which are costly and logistically difficult to implement in low-resource settings. AAV-mediated gene transfer offers a potential ‘one-shot’ solution by enabling sustained in vivo bNAb expression from transduced cells13. The genome of the AAV vector persists in the nucleus as episomes and encodes only the transgene product14; as long as the delivered protein is non-toxic and does not induce host immune responses, transgene expression can persist for the entire lifespan of the transduced cell14. Because myocytes are abundant, easily accessible and long-lived15, skeletal muscle is a preferred tissue for AAV-based immunotherapies aimed at achieving durable bNAb expression.
Given that childbirth represents a reliable clinical touchpoint between healthcare providers and the mother–baby pair, a single intramuscular injection of AAV-bNAb vectors at this stage could protect infants from HIV-1 throughout the breastfeeding period. This intervention may be particularly valuable where access to ARV therapy is limited, and could even benefit infants of HIV-negative mothers in high-burden settings. Since the neonatal immune system is characterized by reduced pro-inflammatory signalling16,17,18, high numbers of regulatory T cells19,20 and a predisposition to develop tolerance, rather than immunity, to alloantigens3,21, we hypothesized that infants would be less prone to produce anti-drug antibodies (ADAs) and therefore more likely to maintain persistent expression of HIV-1 bNAbs following AAV-mediated gene transfer.
Efficacy against oral SHIV challenge
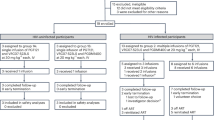
Using infant rhesus macaques as a model, we evaluated the efficacy of neonatal gene therapy with AAV-bNAb vectors against HIV-1 transmission through breastfeeding. Our first study comprised nine newborn rhesus macaques that were equally divided into three groups. Monkeys in each group were treated with an AAV serotype-1 (AAV-1) and/or AAV-8 vector encoding ‘rhesusized’ (rh) versions of the immunoadhesin eCD4-Ig22 or the bNAb 3BNC11723, both specific for the CD4 binding site of the HIV-1 envelope (Env) glyocoprotein. Monkeys in group 1 were treated by intramuscular injection at birth with an AAV-1 vector encoding a rh-IgG2 version of eCD4-Ig containing the pharmacokinetics-enhancing LS mutations (rh-eCD4-IgG2-LS) (Extended Data Fig. 1a). Monkeys in group 2 were first treated intravenously with an AAV-8-rh-eCD4-IgG2-LS vector at birth and then intramuscularly with the same AAV-1 construct used in group 1 four weeks later (Extended Data Fig. 1b). Monkeys in group 3 were treated intramuscularly at birth with an AAV-8 vector expressing a rh-IgG1-LS version of 3BNC117 (rh-3BNC117-IgG1-LS) (Extended Data Fig. 1c). All AAV vectors were delivered within 24 h of birth. No AAV-associated adverse events were recorded in any of the infants in groups 1–3, which gained weight at the expected rate during their first year of life (Extended Data Fig. 2a–c).
AAV-expressed rh-eCD4-IgG2-LS could be detected in sera from all infants in groups 1 and 2 as early as 2 weeks after the first vector administrations. (Fig. 1a–f). Although monkeys rh1-1 (group 1) and rh2-1 (group 2) developed ADAs, these responses did not abrogate rh-eCD4-IgG2-LS expression (Fig. 1a,d). In group 3, two infants developed persistent levels of rh-3BNC117-IgG1-LS (Fig. 1g,h), but the third, rh3-3, produced an ADA response that promptly shut down bNAb expression (Fig. 1i). Notably, in vivo-produced rh-eCD4-IgG2-LS and rh-3BNC117-IgG1-LS were biologically active, as serum concentrations of each molecule were directly proportional to their reciprocal neutralizing antibody (NAb) titres against the simian–human immunodeficiency virus (SHIV)-AD8EO clone (Extended Data Fig. 3). As the 9 infants in groups 1–3 approached 20 weeks of age, a per-protocol transition to paired housing necessitated the removal of a monkey from the study. As serum concentrations of rh-3BNC117-IgG1-LS had fallen below detection limits in the group 3 infant rh3-3 after week 12, this monkey was removed from the study.
a–i, Serum concentrations of rh-eCD4-IgG2-LS (a–f) or rh-3BNC117-IgG1-LS (g–i) and ADA levels (a–i) in infant rhesus macaques in group 1 (rh1-1 (a), rh1-2 (b) and rh1-3 (c)), group 2 (rh2-1 (d), rh2-2 (e) and rh2-3 (f)), and group 3 (rh3-1 (g), rh3-2 (h) and rh3-3 (i)). ADA responses for groups 1–3 are depicted as the serum immunoglobulin reactivity (absorbance values at 450 nm (A450 nm)) against plate-bound rh-eCD4-IgG2-LS or rh-3BNC117-IgG1-LS. j, Kaplan–Meier analysis of SHIV acquisition in each experimental group (groups 1–3) versus the control group (group 4) after oral challenges with increasing doses of SHIV-AD8EO expressed as Gag p27 content. P values were calculated using the Mantel–Cox test. k,l, log10-transformed plasma viral loads in the group 4 macaques (n = 6) (k) and in the only group 1 (l) monkey (rh1-1) that acquired infection. Empty red bars in l indicate the post-infection serum rh-eCD4-IgG2-LS concentrations.
To mimic HIV-1 exposures through breastfeeding, the eight remaining monkeys in groups 1–3 and six age-matched AAV vector-naive control infant monkeys (group 4) were subjected to weekly oral challenges with SHIV-AD8EO beginning at postnatal weeks 30–34 (Extended Data Fig. 1a–d). It took 12 consecutive challenges with escalating doses of SHIV-AD8EO to infect all control monkeys (Fig. 1j). By contrast, all AAV-treated infants, except for rh1-1 in group 1, remained uninfected, even after being challenged with undiluted (329,728 pg Gag p27) virus at the 12th–14th exposures. The differences in SHIV-AD8EO acquisition between group 4 and groups 1, 2 and 3 were statistically significant (P = 0.03, 0.01 and 0.04, respectively; Fig. 1j). Following SHIV-AD8EO infection, the group 1 monkey rh1-1 maintained persistent expression of rh-eCD4-IgG2-LS, which coincided with partial control of viraemia compared with the group 4 controls (Fig. 1k,l). Thus, in this proof-of-principle experiment, neonatal gene therapy with HIV-1 IgG biologics was safe and protected infant macaques against oral SHIV acquisition.
Age dictates AAV-bNAb therapy outcomes
Most juvenile and adult rhesus macaques treated with AAV-bNAb vectors mount ADAs that reduce or eliminate bNAb production in vivo24,25. This is not a macaque-specific phenomenon, as AAV-mediated delivery of human HIV-1 bNAbs can also induce anti-bNAb antibody responses in adult humans26,27. By contrast, only one out of the nine AAV-treated newborn macaques in groups 1–3 developed ADAs that inhibited transgene expression (Fig. 1a–i). To directly address the hypothesis that AAV-delivered bNAbs are less immunogenic in neonates than in older monkeys, we enroled six infants (group 5) and six juvenile (group 6) rhesus macaques in a second study. Both groups were inoculated intramuscularly with the same AAV-8-rh-3BNC117-IgG1-LS vector used in group 3, since AAV-expressed rh-3BNC117-IgG1-LS consistently elicits ADAs in most older monkeys24,25. The group 6 juveniles were approximately 2 years old at the time of the vector inoculation, whereas all but one group 5 infants were treated within 48 h of birth (Extended Data Table 1). The group 5 infant rh5-6 was born below the pre-specified weight criterion to be enroled in the study and thus did not receive the AAV-8-rh-3BNC117-IgG1-LS vector until it had met the minimum size requirement at four weeks of age. Because rh5-6 was one month older than its group 5 counterparts at the time of the AAV vector administration, this monkey was not considered a newborn for analysis purposes. Notably, all five group 5 newborns developed increased serum concentrations of rh-3BNC117-IgG1-LS that persisted for at least 20 weeks (Fig. 2a), with little or no ADAs detected (Fig. 2b). Monkey rh5-6 was unique in that it produced the highest levels of ADAs in group 5 and exhibited a biphasic pattern of transgene expression, characterized by a small wave of rh-3BNC117-IgG1-LS production ending at week 6, followed by a rebound in bNAb concentrations that continued to increase over the ensuing months (Fig. 2a,b). By contrast, two-thirds of the group 6 juveniles experienced a transient wave of bNAb expression that ended by week 10 (Fig. 2c). In those monkeys, the clearance of AAV-expressed rh-3BNC117-IgG1-LS from circulation was temporally associated with the emergence and maintenance of ADAs (Fig. 2d). Surprisingly, persistent expression of rh-3BNC117-IgG1-LS and no ADAs were observed in two juveniles, one of which (rh6-6) developed bNAb levels resembling those in the group 5 newborns (Fig. 2c,d). In spite of this outlier in group 6, the serum concentrations of rh-3BNC117-IgG1-LS at week 20 after intervention were higher in newborns than in juveniles, whereas the opposite pattern was true for the cumulative levels of ADAs measured over the 20-week follow-up period (Fig. 2k,l). Moreover, the incidence of macaques exhibiting durable bNAb expression following AAV-bNAb gene therapy was significantly higher among newborns (5 out of 5) than juveniles (2 out of 6) (P = 0.02, Fisher’s exact test). Of note, the reduced frequency of ADAs in group 5 was not due to a general deficit in humoral immune responses in early life, as all infants seroconverted to AAV-8 following the AAV-8-rh-3BNC117-IgG1-LS inoculation, albeit at a significantly delayed rate compared with the group 6 juveniles (Extended Data Fig. 4). In sum, these results suggest that developmental age can affect the outcome of AAV-bNAb therapy by increasing (in the case of juveniles) or limiting (in the case of newborns) the frequency of ADA responses.
a–j, The AAV-8-rh-3BNC117-IgG1-LS vector was administered to rhesus macaques across four age groups: group 5 (a,b; 48 h, except for rh5-6 (see below)); group 6 (c,d; approximately 2 years); group 7 (e,f; 4 weeks); group 8 (g,h; 8 weeks); and group 9 (i,j; 12 weeks). LLOQ, lower limit of quantification. a,c,e,g,i, Serum rh-3BNC117-IgG1-LS concentrations. b,d,f,h,j, Anti-rh-3BNC117-IgG1-LS responses, or ADAs, in each group. k, Serum concentrations of rh-3BNC117-IgG1-LS at week 20 in the group 5 newborns (n = 5) and group 6 juveniles (n = 6). l, Comparison of cumulative levels of ADAs produced by the group 5 newborns and group 6 juveniles during the 20 weeks of follow-up. AUC, area under the curve. In k,l, the group 5 infant rh5-6 was not included in the comparisons because it received the AAV-8-rh-3BNC117-IgG1-LS vector 4 weeks after birth. m, Monkeys in groups 3 and 5–9 were divided into three age brackets and their serum rh-3BNC117-IgG1-LS concentrations at week 20 were compared. In k–m, bars correspond to medians and P values were two-sided and calculated using the Mann–Whitney U-test. P values in brackets were calculated without the group 6 outlier rh6-6. n, Correlation between the age (in weeks) of each monkey at the time of AAV inoculation and serum rh-3BNC117-IgG1-LS concentration at week 20.
Treatment success decreases with age
The results obtained from groups 5 and 6 were consistent with our hypothesis that newborns are less prone to producing ADAs and, consequently, can develop greater and more durable levels of bNAb expression than juveniles following AAV-bNAb gene therapy. However, it remained unclear whether this pattern would also apply to older infants. The observation that the 4-week-old infant macaque rh5-6 produced higher levels of ADAs than its newborn counterparts in group 5 hinted that the immunogenicity of AAV-delivered bNAbs increases proportionately with postnatal age. To address this possibility, we enrolled 8 infant rhesus macaques born to AAV-8 seronegative dams (group A; Extended Data Tables 1 and 2) in a third study and treated them intramuscularly with the AAV-8-rh-3BNC117-IgG1-LS vector at 4 weeks (group 7; n = 3), 8 weeks (group 8; n = 3) or 12 weeks (group 9; n = 2) after birth (Extended Data Fig. 5). Of the three infants in group 7, two did not produce ADAs and developed steadily increasing concentrations of rh-3BNC117-IgG1-LS that plateaued at 61–85 µg ml–1 serum (Fig. 2e,f). By contrast, the remaining monkey in group 7 (rh7-2) produced an ADA response that curbed bNAb production after week 4 (Fig. 2e,f). In group 8, the only monkey to have detectable rh-3BNC117-IgG1-LS in serum at week 20 was rh8-2, but this monkey still made ADAs and displayed the same two-phase pattern of bNAb expression seen in rh5-6 (Fig. 2g,h). AAV-driven bNAb expression in the other two monkeys in group 8 was short-lived and quelled by ADAs within the first few study months (Fig. 2g,h). Of the two 12-week-old infants in group 9, one monkey developed sustained bNAb expression and no ADAs, and the other one displayed the opposite pattern (Fig. 2i,j).
Next, we subdivided the 20 monkeys in groups 3 and 5–9 into 3 categories based on their age range at the time of the AAV vector inoculation and compared the serum concentrations of rh-3BNC117-IgG1-LS measured at week 20 between each subgroup. This analysis revealed that neonates (aged 0–4 weeks) exhibited higher bNAb expression levels than older infants (aged 8–12 weeks; P = 0.025) and 2-year-old juveniles (P = 0.058; Fig. 2m). We also observed an inverse correlation between the age of the monkeys at the time of AAV vector administration and their serum concentrations of rh-3BNC117-IgG1-LS at week 20 (P = 0.029, r = –0.46; Fig. 2n). Collectively, these results suggest that the first four weeks after birth comprise an optimal period for achieving high and sustained levels of AAV-driven bNAb expression in rhesus macaques. Beyond this period, AAV-mediated bNAb gene transfer can still induce durable HIV-1 immunity in older infants and juveniles, but with lower success rates owing to the induction of ADAs.
Transcriptional signatures in blood
To investigate why the neonatal immune system tolerates AAV-delivered bNAbs, we performed bulk RNA sequencing (RNA-seq) on whole blood collected from the monkeys in groups 5 and 6 on day 0, day 3 and week 4 after AAV-8-rh-3BNC117-IgG1-LS administration. Owing to limited blood volumes from infants, we used bulk transcriptomics for this analysis. Reads were pseudoaligned with Kallisto, and differential gene expression was assessed using Sleuth.
Minimal transcriptomic changes were observed at day 3 (Extended Data Fig. 6a,b). By week 4, however, both infants and juveniles showed marked shifts from baseline, though the magnitude and nature of these changes differed by age. For instance, the juvenile volcano plot contained significantly more differentially expressed genes (DEGs) than the infant plot (P = 10–10; Extended Data Fig. 6c,d). In infants, pathway enrichment pointed to altered B and T cell signalling, including upregulation of immunoglobulin light chains and co-stimulatory molecules (Extended Data Fig. 6e,g). By contrast, juveniles showed broader changes involving cellular housekeeping functions such as RNA processing and protein synthesis but lacked transcriptional signatures of lymphocyte activation (Extended Data Fig. 6f,h).
We applied the same RNA-seq strategy to blood samples from groups 7–9. Groups 8 and 9 were pooled, while group 7 was analysed independently. At week 4, both datasets showed enrichment in B cell receptor signalling pathways (Extended Data Fig. 7a,c). However, the younger monkeys (group 7) displayed additional changes in platelet activation and coagulation genes, whereas the older ones (groups 8 and 9) showed enhanced expression of protein synthesis machinery (Extended Data Fig. 7c,d). Together, these data demonstrate that developmental age influences the transcriptional response to intramuscular AAV-bNAb gene therapy. However, because of limited resolution in bulk transcriptomics and small cohort sizes, we were unable to identify DEGs that consistently differentiated monkeys with or without persistent bNAb expression.
BNAb tolerization in utero
The inverse relationship between age at the time of AAV-bNAb inoculation and bNAb expression levels makes a strong argument for treating infants at risk of vertically acquiring HIV-1 as close to birth as possible. However, children might miss this window of opportunity for a variety of reasons, which would reduce their odds of benefiting from AAV-vectored bNAb gene transfer. Considering that even older infants and toddlers can acquire HIV-1 through breastfeeding28, we sought ways to limit ADAs in cases where AAV-bNAb gene therapy might occur beyond the neonatal period. Seminal work by Medawar and colleagues in the mid-twentieth century showed that prenatal exposure to allogeneic cells enabled adult mice and chickens to accept skin grafts from the same strain or donor that provided the cells for the fetal injection3,4. Guided by these findings, we hypothesized that monkeys exposed to recombinant forms of the AAV-encoded bNAb in utero would acquire tolerance to the bNAb, thereby improving the success rate of AAV-bNAb therapy later in infancy through inhibition of ADA responses. To address this possibility, we designed a fourth study in which eight AAV-8-seronegative female rhesus macaques were treated with recombinant forms of rh-3BNC117-IgG1 during late pregnancy (groups B and C; Extended Data Table 2). Because the placenta actively transfers maternal IgG antibodies to the fetus in a neonatal Fc receptor-dependent way, a maternally delivered IgG bNAb would be expected to reach the fetus shortly after the infusion. The group B and group C dams were identified in the same birth season and were housed in the same facility as the group A mothers of the infants in groups 7–9 (Extended Data Fig. 5). When the selected dams approached the end of their third trimesters (approximately gestational week 22), they were treated intravenously with 30 mg kg−1 of recombinant rh-3BNC117-IgG1-LS (group B; n = 4) or the same dose of rh-3BNC117-IgG1 (group C; n = 4) lacking the pharmacokinetics-enhancing LS mutations (Extended Data Fig. 5). The bNAb infusions were well tolerated and resulted in typical pharmacokinetics profiles of systemically administered monoclonal antibodies (Extended Data Fig. 8a–h). Two weeks after each bNAb infusion, pregnancies in both groups reached term, the dams underwent caesarean section and their offspring were immediately transferred to the nursery for rearing. The eight newborns were then assigned to new groups, depending on whether they received the AAV-8-rh-3BNC117-IgG1-LS vector at postnatal week 8 (group 10; n = 4) or week 12 (group 11; n = 4) (Extended Data Fig. 5). Of note, groups 10 and 11 contained equal numbers of infants born to the group A and group B mothers (Extended Data Fig. 5 and Extended Data Tables 1 and 2). At the time of caesarian section, both rh-3BNC117-IgG1-LS and rh-3BNC117-IgG1 were detected in newborn circulation, demonstrating successful transplacental bNAb transfer (Extended Data Fig. 8i). Of note, following intramuscular administration of the same AAV-8-rh-3BNC117-IgG1-LS vector described above, all 8 monkeys in groups 10 and 11 developed persistent bNAb expression, with virtually no ADAs detected throughout the 20 weeks of follow-up (Fig. 3a–d). By comparison, sustained production of rh-3BNC117-IgG1-LS was observed in only two out of the five age-matched infants without prior fetal bNAb exposure in groups 8 and 9 (Fig. 2g,i). This difference was statistically significant (P = 0.035; Fisher’s exact test). We also compared the cumulative serum concentrations of rh-3BNC117-IgG1-LS and cumulative levels of ADAs between infants with (groups 10 and 11) and without (groups 8 and 9) prior fetal bNAb exposure. This analysis revealed significantly higher bNAb amounts and markedly lower ADA levels in sera from the prenatally bNAb-exposed monkeys in groups 10 and 11 compared with their bNAb-naive counterparts in groups 8 and 9 (Fig. 3e,f). Together, these results suggest that fetal exposure to recombinant forms of an AAV-encoded bNAb can tolerize rhesus macaques to this molecule, effectively inhibiting ADAs and improving bNAb expression following postnatal AAV-mediated delivery of the same bNAb at 8–12 weeks of age.
While the macaques in groups 10 and 11 were in their final weeks of gestation, their mothers were treated intravenously with recombinant rh-3BNC117-IgG1-LS or rh-3BNC117-IgG1, leading to transplacental transfer of these molecules. The macaques that were prenatally exposed to the bNAb were delivered two weeks later and then treated with the AAV-8-rh-3BNC117-IgG1-LS vector at 8 weeks (group 10) or 12 weeks (group 11) of age. a,c, Serum rh-3BNC117-IgG1-LS concentrations in group 10 (a) and group 11 (c). ADAs were assessed as described in Fig. 1 for group 10 (b) and group 11 (d). All samples from groups 7–11 were screened for anti-rh-3BNC117-IgG1-LS antibodies in the same 384-well enzyme-linked immunosorbent assay (ELISA) plate. e,f, Cumulative serum rh-3BNC117-IgG1-LS concentrations (e) and ADA levels (absorbance values of anti-rh-3BNC117-IgG1-LS reactivity in serum) (f) measured over the first 20 weeks post-intervention were compared between infant macaques exposed to recombinant forms of rh-3BNC117-IgG1 in utero (groups 10 and 11) and age-matched bNAb-naive infants (groups 8 and 9). Bars correspond to medians. All P values were two-sided and calculated using the Mann–Whitney U-test.
Years-long HIV immunity induced at birth
Although breast milk is a major route of HIV-1 transmission in sub-Saharan Africa28, the World Health Organization (WHO) still recommends mothers living with HIV-1 who cannot access ARV therapies to practice exclusive breastfeeding during the first six months of their child’s life29. This guidance is based on evidence that formula-fed or mixed-fed infants face higher risks of death from malnutrition, pneumonia or gastrointestinal infections compared with exclusively breastfed infants30. Since breastfeeding can last beyond two years in sub-Saharan Africa28, an important endpoint for neonatal HIV-1 immune interventions is how long they can provide protective immunity to nursing infants. With this mind, we continued to follow four of the seven monkeys in groups 1–3 that remained uninfected after the oral SHIV-AD8EO challenge phase for three to four years, during which time these monkeys were not re-dosed with AAV vectors. Both group 3 monkeys (rh3-1 and rh3-2) maintained stable expression of rh-3BNC117-IgG1-LS for at least 157 weeks, with serum concentrations in the 11–20 µg ml–1 range (Fig. 4a,b). In the case of rh1-2 (group 1) and rh2-3 (group 2), both monkeys had 12–48 µg ml–1 of rh-eCD4-IgG2-LS in serum at 4 years of age (Fig. 4c,d). All four monkeys continued to exhibit detectable anti-SHIV-AD8EO NAbs throughout the three to four years of follow-up, indicating sustained antiviral activity of the in vivo-produced IgG biologics. Thus, infant primates treated with AAV vectors at birth can continue to produce functional IgG HIV-1 biologics for at least four years, significantly longer than the duration of breastfeeding recommended by the WHO.
Four out of the seven AAV-treated macaques in groups 1–3 that resisted oral challenges with SHIV-AD8EO were kept alive for up to four years, and AAV-driven transgene expression in serum was monitored. These macaques were not re-dosed with AAV vectors after the neonatal period. a–d, Serum concentrations of rh-3BNC117-IgG1-LS (a,b) or rh-eCD4-IgG2-LS (c,d) and NAb titres against SHIV-AD8EO for rh3-1 (a), rh3-2 (b), rh1-2 (c), and rh2-3 (d). Date of birth (DOB) and date of the last rh-3BNC117-IgG1-LS or rh-eCD4-IgG2-LS measurement are shown. ID50, half-maximal infectious dose. e–i, The six macaques in group 5 were kept alive beyond the 20-week follow-up period described in Fig. 2 and their serum concentrations of rh-3BNC117-IgG1-LS (e) and NAb titres against SHIV-AD8EO (f) were monitored until the animals reached approximately 2.5 years of age. Beginning at weeks 133–140 post-intervention, the group 5 monkeys and six controls (group 12) were subjected to repeated intrarectal (IR) challenges with a fixed marginal dose of SHIV-AD8EO. g, Kaplan–Meier analysis of SHIV acquisition in groups 5 and 12. The P value was calculated using the Mantel–Cox test. h,i, Plasma viral loads in the group 12 macaques (n = 6) (h) and in the only group 5 monkey (rh5-2) (i) that acquired infection.
Given the years-long transgene expression observed in the four macaques above, we investigated whether neonatally AAV-treated monkeys would be protected against mucosal SHIV challenges later in life, as they approached sexual maturity. We investigated this possibility by reassigning the monkeys in group 5 to a fifth study nearly three years after they were dosed with the AAV-8-rh-3BNC117-IgG1-LS vector in their first month of life. In keeping with the results above, all monkeys in group 5 continued to express rh-3BNC117-IgG1-LS and display neutralizing SHIV activity in serum throughout the extended follow-up period (Fig. 4e,f). Beginning at weeks 133–140 after intervention, the six group 5 monkeys and six age- and sex-matched monkeys without prior AAV vector exposure (group 12) were subjected to weekly intrarectal challenges with a marginal dose (3.8 ng Gag p27) of SHIV-AD8EO to mimic sexual HIV-1 exposures during adolescence. After five intrarectal SHIV challenges, all six group 12 controls but only one group 5 monkey became infected (Fig. 4g). This difference in SHIV acquisition between groups 5 and 12 was statistically significant (P = 0.001). The only group 5 macaque to acquire infection was rh5-2, which became viraemic after the fifth intrarectal SHIV exposure. After infection, rh5-2 experienced lower acute phase viraemia than the control monkeys in group 12, probably owing to rh-3BNC117-IgG1-LS expression persisting after SHIV acquisition (Fig. 4h,i). In sum, our studies suggest that, at least in rhesus macaques, the persistent HIV-1 immunity afforded by neonatal AAV-bNAb gene therapy is sufficient to confer significant protection against rectal acquisition of a neutralization-sensitive SHIV for at least three years without redosing.
Discussion
Here we show that rhesus macaques can develop durable HIV-1 bNAb immunity after receiving a single intramuscular dose of AAV-bNAb vectors at birth. Critically, as the monkeys matured from infancy into adolescence, the AAV-encoded IgG molecules continued to be produced in vivo and retained their antiviral functions, successfully blocking SHIV infection in models designed to simulate vertical and sexual transmission of HIV-1. Our data also illustrate how developmental age and prenatal exposure to the AAV-encoded bNAb can modulate postnatal immune responses to AAV-bNAb therapy and, consequently, its success rate in primates. Collectively, these findings hold promise for improving HIV-1 prophylaxis, especially in places with high HIV-1 prevalence. Because childbirth is one of the most consistent times of interaction between healthcare providers and the mother–child dyad, treating at-risk babies at this stage could offer sustained protection against perinatal HIV-1 infection even if the infant is lost to follow-up. Our data also offer the tantalizing possibility that the HIV-1 immunity afforded by neonatal gene therapy with AAV-bNAb vectors might last until adolescence or beyond, potentially safeguarding against sexually transmitted HIV-1.
The tolerance-prone immune system in early life makes a strong argument for advancing neonatal AAV-bNAb gene therapies for averting postpartum HIV-1 infections. It is well established from transplantation studies that neonates, unlike adults, are predisposed to developing tolerance, rather than immunity, to alloantigens3,4,21. Although the success of AAV-bNAb therapies in adults is often limited by the induction of host anti-bNAb antibody responses, we show here that this is not the case in newborn rhesus macaques. Indeed, following administration of an AAV-8-rh-3BNC117-IgG1-LS vector, newborns displayed lower incidence and magnitude of ADAs than older monkeys and, consequently, developed and maintained higher bNAb concentrations in serum. Notably, this ability to acquire tolerance to the AAV-delivered bNAb diminishes with age, as infant macaques aged 8–12 weeks exhibited lower serum bNAb concentrations than their neonate (aged 0–4 weeks) counterparts. Note that these timeframes may not translate directly to humans given that rhesus macaques age approximately three times faster31. Nonetheless, our findings are still relevant for designing future clinical trials of paediatric AAV-bNAb gene therapies since they suggest that the age of the participants at the time of the vector administration might affect treatment success rates.
Paediatric AAV-bNAb gene therapies would have the greatest impact in preventing vertical HIV-1 transmission if they could be administered to breastfeeding children of all ages without eliciting ADAs. In this regard, our finding that prenatal exposure to recombinant versions of rh-3BNC117-IgG1 prevented ADA responses in AAV-8-rh-3BNC117-IgG1-LS-treated older infants is encouraging, since it demonstrates that a classical tolerization strategy can suppress the immunogenicity of an AAV-encoded bNAb. This experimental paradigm was established in the 1950s by Medawar and others who showed that rodents injected in utero with allogeneic cells were later capable of accepting skin grafts from donors of the same lineage as the prenatally injected cells3,4. The theory underpinning these results is that antigens encountered under non-inflammatory conditions during intrauterine life are perceived as ‘self’ by the fetal immune system, leading to the deletion or functional inactivation of antigen-reactive lymphocytes19,32. Although leveraging prenatal tolerization as a strategy for avoiding ADAs in AAV-bNAb-treated children may seem challenging at first, it would not be impossible considering that pregnant women living in regions of high HIV-1 prevalence are among the key populations that the WHO is prioritizing for receiving passive immunizations with bNAbs for HIV-1 prevention33.
Notably, the ability to develop tolerance to foreign antigens is not an intrinsic property of the immune system in early life. In mice, the same allogeneic cells that can induce tolerance in neonates can also do so in adults when larger doses are used34. Similarly, in the context of living donor renal transplantation, perioperative infusions of donor-derived haematopoietic cells to the organ recipient can improve allograft survival through the induction of tolerance35. These observations from transplantation immunology have parallels with the long recognized but poorly understood phenomenon of high zone tolerance (HZT)—that is, the ability of systemic injections of large amounts of soluble non-aggregated and non-adjuvanted antigens to induce a state of immune unresponsiveness specific to the delivered antigen36,37. HZT has shown efficacy in the context of replacement therapy with recombinant factor XIII in patients with haemophilia A38. This clinical precedent raises the intriguing possibility that HZT could be used to tolerize older children or even adults to recombinant HIV-1 bNAbs. Given the excellent safety and efficacy records of passive immunizations with HIV-1 bNAbs in children, future studies should evaluate the extent to which prior administration of large doses of recombinant versions of the same HIV-1 bNAbs encoded by AAV vectors can prevent ADAs following AAV-bNAb gene therapy.
Because wild-type AAV is endemic in humans39, pre-existing cross-reactive NAbs against AAV vectors pose a significant obstacle to the clinical deployment of these gene therapies. Although nearly nothing is known about the seroprevalence of AAV vectors in African children, Calcedo et al. have reported that less than 20% of North American newborns display AAV-8 NAb titres greater than 1:20 and this figure eventually drops to 0% by the seventh month of life, consistent with the clearance of maternal anti-AAV IgG NAbs40. Although pre-existing serum titres of 1:20 can abrogate AAV-8-mediated liver transduction following systemic delivery41, this threshold is less severe when vectors are administered directly to skeletal muscle. Indeed, intramuscular gene therapy with AAV-8 can result in unabated transgene expression in monkeys with AAV-8 NAb titres of up to 1:160 at the time of vector inoculation42. Given the high rates of perinatal HIV-1 transmission in sub-Saharan Africa, more work is needed to characterize the seroprevalence of muscle-tropic AAV serotypes in the region so that appropriate capsids can be selected to maximize coverage of AAV-bNAb therapies among infants with greater likelihood of acquiring HIV-1.
Our investigation into infant responses to AAV-8-rh-3BNC117-IgG1-LS gene therapy suggests a diminished capacity for acquiring tolerance to AAV-encoded bNAbs with increasing age, as evidenced by a positive correlation with increasing frequency of ADA responses and a corresponding negative correlation between the age at vector administration and bNAb expression levels. This aligns with the transition of the neonatal immune system from a tolerogenic state, which is crucial for not reacting against maternal antigens in utero, to an active immunity mode for defence against postnatal infections. Elucidating the immunological mechanisms of this early-life transition may uncover new strategies for dampening unwanted immune responses, including the ADAs that undermine the efficacy AAV-bNAb therapies in adults. To explore these mechanisms, we characterized the transcriptional signatures elicited by the AAV-8-rh-3BNC117-IgG1-LS vector administration in groups 5–9. Our analysis uncovered substantial differences in how rhesus macaques respond to AAV-bNAb therapy during early infancy compared with later stages. However, we were unable to identify a specific set of DEGs associated with the development or suppression of ADA responses. This limitation may be due to the use of bulk transcriptomics, which relies on averaged transcript abundances in whole blood and lacks resolution at the cellular level. Single-cell RNA-seq could have provided higher resolution, but its application was constrained by the limited blood volume obtainable from infant macaques at each time point. Moreover, the small group sizes and high intra-group variability in DEGs further reduced the statistical power of our analysis.
In sum, here we show that newborn and prenatally bNAb-exposed older infant macaques can develop persistent bNAb expression lasting for years after a single intramuscular administration of AAV-bNAb vectors. If these results are reproduced in humans, AAV-vectored delivery of HIV-1 IgG biologics could provide a practical and scalable tool for combating paediatric HIV-1 infections in the developing world. The appeal of this approach is further bolstered by the thermostability of AAVs43 and the simplicity of intramuscular injections, which could facilitate the deployment of AAV-bNAb vectors to remote areas where cold chains may be difficult to maintain. In addition to HIV-1, insights gained from this study are also potentially applicable to other intractable infectious diseases that disproportionately affect paediatric populations. For example, malaria is a leading cause of death among children below five years of age in developing countries44. Although the WHO has recently approved two vaccines for the prevention of malaria in children, the protection that they afford is short-lived and requires multiple booster doses to sustain efficacy45. Since plasmodium-specific monoclonal antibodies capable of preventing malaria infection in adults and children have been isolated45, AAV-vectored delivery of these molecules at birth could afford potent malaria prophylaxis for years without the need for redosing. Thus, successful deployment and uptake of intramuscular gene therapies with pathogen-specific monoclonal antibodies could simplify efforts to prevent and treat communicable diseases in low-income countries.
This study has several limitations. First, we evaluated AAV-delivered HIV-1 bNAbs using a single bNAb-sensitive SHIV strain, which does not reflect the genetic diversity of circulating HIV-1 variants in humans. Second, species differences in body size and the uncertain allometric scaling of intramuscular AAV doses limit extrapolation to human infants, who may develop different bNAb concentrations in serum, especially as they grow. Third, we did not determine the cellular sources of transgene expression in macaques with sustained bNAb production. However, prior studies46,47 suggest that the majority of bNAb production in vivo originates from long-lived myocytes that were transduced with the AAV vectors at the time of intramuscular dosing. Fourth, AAV-based gene therapies remain prohibitively expensive and largely inaccessible in low- and middle-income countries, due in part to profit-driven regulatory frameworks that influence pricing. Despite this, ongoing advances in AAV vector production48, capsid engineering49 and cell and gene therapy manufacturing capacity in low- and middle-income countries, along with evolving policy initiatives and calls to reform the current business model50, hold promise for making these therapies more affordable and globally available.
Methods
Research animals and procedures
A total of 65 rhesus macaques (M. mulatta) of Indian origin were utilized in this study (Extended Data Tables 1 and 2). All macaques were born and raised at the California National Primate Research Center (CNPRC). The maintenance and handling of the animals adhered to the United States Department of Agriculture (USDA) Animal Welfare Act and regulations, as well as the Guide for the Care and Use of Laboratory Animals. The animal care and use programme of The University of California, Davis, which oversees the CNPRC, is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care, registered with the USDA, and maintains a Public Health Services Assurance. All procedures and experiments conducted for this study received approval from the University of California-Davis’s Institutional Animal Care and Use Committee (protocol numbers 21768, 21884, 20609, and 22373).
The primary criterion for enroling macaques in experiments involving gene therapy with AAV vectors was seronegativity for the relevant AAV capsid. To identify eligible macaques, pregnant adult females were screened for serum IgG antibodies against AAV-1 and/or AAV-8 by ELISA (see ‘Estimation of serum anti-AAV antibodies’ section) and those that were seronegative for the capsid(s) of interest were placed on hold. Dams with a history of prior live births were prioritized. The infants in groups 1–5 were vaginally delivered by dams in the outdoor colony. Those that were assigned to groups requiring AAV vector administrations at birth were removed from their mothers within 48 h of delivery and transferred to the nursery for specialized care and monitoring. Nursery-reared infants were fed a nutritionally balanced formula (Enfamil Lipil + Iron) and provided with surrogate companions, such as soft toys and blankets, to promote social and emotional development. Trained animal care staff closely monitored the infants’ health, growth and behaviour, ensuring that their physical and psychological needs were met. The infants received regular veterinary check-ups and were gradually introduced to solid foods and social housing with age-matched peers as part of their normal developmental process. The CNPRC nursery-rearing standards are designed to minimize stress and maximize the infants’ well-being, in accordance with current best practices for nonhuman primate husbandry and care in research settings. Nursery-reared infants also received high-protein chow as a supplement to formula. The diet converged over time to high-protein chow at the age of six months. All monkeys received seasonal fruits as part of the CNPRC feeding enrichment programme. Group sizes were dictated by the limited availability of AAV-8 seronegative monkeys. At least six AAV-treated and six control macaques were used in each SHIV challenge study. Efforts were made to balance groups for sex, so allocation of monkeys to each group was not random. Animal staff were not blinded to group assignments.
To identify the mothers of the infants that would be assigned to groups 7–11, we used ELISA to screen archived sera and sera collected during bi-annual physical exams for anti-AAV-8 antibodies. AAV-8 seronegative mothers-to-be were identified and their status was confirmed by a second ELISA. Monkeys that remained AAV-8 seronegative after the second ELISA were moved to indoor housing. At the time of this relocation and four weeks later, additional serum samples were collected for confirmatory AAV-8 ELISAs. If a monkey seroconverted during this quarantine screening period, it was excluded from the cohort and returned to the colony. Following three rounds of AAV screening, 16 pregnant dams remained AAV-8 seronegative and were ultimately assigned to groups A–C (Extended Data Table 2). These monkeys were then transferred to an ABSL-2 environment with specific personal protective equipment requirements to avoid transmission of wild-type AAV from the outside.
The 16 AAV-8 seronegative pregnant dams in groups A–C were scheduled to undergo caesarian section when their pregnancies reached term (approximately gestational week 24), but two dams (rhA-1 and rhA-3) delivered their babies vaginally ahead of time (Extended Data Table 2). The remaining 14 dams underwent caesarian section, which was performed by experienced veterinarians boarded by the American College of Laboratory of Animal Medicine. Initially, inhalant anaesthesia was administered, followed by surgical preparation. A laparotomy incision was made at the caudal ventral abdominal midline, and the uterus was then exteriorized. A uterotomy incision was carefully made to avoid placental sites, and the neonate was delivered. Neonatal resuscitative procedures were initiated, and the neonate was transferred to a warm workstation for monitoring. The uterotomy and the abdominal wall were closed using absorbable sutures in layers. Oxytocin was administered as needed during or after uterine closure. Following surgery, the dams were monitored in the recovery room or home cage until they maintained an upright posture. Post-surgical analgesics were administered according to standard protocols.
To deliver the recombinant bNAbs to the pregnant dams in groups B and C, the monkeys were sedated and the site over the vein where the catheter was to be placed was shaved. The area was then cleaned with gauze soaked in alcohol. During this preparation, sterility of the catheter end, which was to be inserted into the vein, was maintained. The catheter, with its stylette-bevel up, was placed on the skin. The skin was punctured with the catheter stylette, which was then introduced into the vein. While holding the stylette stable, the catheter was advanced into the vein. The stylette was then withdrawn while the catheter was held in place. An injection cap or flush syringe was attached to the catheter. The placement of the catheter was checked by flushing with a small volume of flush or fluid solution, and careful observation was made to ensure the fluid flowed into the vein without any leakage into the subcutaneous area. The catheter was then taped to the limb to secure it. For the slow infusion procedure, 30 mg kg−1 of recombinant rh-3BNC117-IgG1 or rh-3BNC117-IgG1-LS proteins was delivered through the intravenous catheter at a rate of approximately 2.0 ml min−1. The intravenous line was flushed with saline at the end of the infusion to ensure the full amount of the bNAbs was delivered.
Monkeys had to weigh at least 0.5 kg to be eligible for AAV vector inoculations. The group 1 infants were injected intramuscularly with a phosphate buffered saline (PBS) solution containing weight-adjusted amounts of two AAV-1 vectors: one expressing rh-eCD4-IgG2-LS (2.0 × 1012 genome copies (GC) per kg; VCAV-05105) and the other encoding rhesus tyrosine-protein sulfotransferase-2 (TPST-2; 5.0 × 1011 GC kg−1; VCAV-05102). TPST-2 is needed during cellular synthesis of eCD4-Ig to sulfate the tyrosines in its co-receptor mimetic peptide. The sulfopeptide in the AAV-encoded rh-eCD4-IgG2-LS molecule was mim6 (GGGGGDYYDYDGGYYYDGD). Each monkey received 400 μl of this vector inoculum, which was split evenly between 2 injections into each quadriceps muscle. The group 1 infants were treated with the aforementioned AAV-1 vectors within 24 h after birth.
The group 2 infants were treated intravenously with an AAV-8-rh-eCD4-IgG2-LS (5.0 × 1012 GC kg−1; VCAV-05106) vector within 24 h of birth. Because the majority of intravenously administered AAV particles end up in the liver, where TPST-2 is constitutively expressed, no TPST-2-expressing AAV vector was delivered at this stage. The AAV-8-rh-eCD4-IgG2-LS inoculum consisted of 500 μl of PBS containing a weight-adjusted dose of the vector. At postnatal week 4, the group 2 infants were treated intramuscularly with the same doses of the same AAV-1-rh-eCD4-IgG2-LS and AAV-1-TPST-2 vectors given to the group 1 infants. This AAV-1 inoculum was formulated and administered as described above for group 1.
The group 3 infants were treated intramuscularly with 400 µl of a PBS solution containing 2.0 × 1012 GC kg−1 of an AAV-8-rh-3BNC117-IgG1-LS (VCAV-04757) vector within 24 h of birth. The AAV-8-rh-3BNC117-IgG1-LS inoculum was formulated and administered as described above for group 1. The group 3 monkey rh3-3 was euthanized at postnatal week 21 so that the remaining infants in groups 1–3 could be transitioned to paired housing.
Beginning at postnatal weeks 30–34, the monkeys in groups 1–4 (except for rh3-3) were subjected to weekly oral challenges with escalating doses of a SHIV-AD8EO stock produced in HEK293T cells. The concentration of this SHIV-AD8EO stock was 6.6 × 105 pg ml–1 of Gag p27. For the first oral challenge, each macaque was exposed to 129 pg Gag p27, which corresponded to a 5,000-fold dilution of the stock. The appropriately diluted virus inoculum was loaded into syringes without needles in a final volume of 0.5 to 1.0 ml. The challenge dose was doubled after each exposure. Beginning at the 12th exposure, the challenge inoculum consisted of 0.5 ml of the undiluted SHIV-AD8EO stock. Plasma was collected at the time of each challenge and tested for the presence of viral RNA (vRNA). Monkeys that remained aviraemic continued to be re-challenged in the next week. However, once a macaque experienced two consecutive episodes of positive viraemia, it was deemed to be infected and did not receive additional virus challenges. Plasma viral loads were then monitored for up to ten weeks post-infection.
The macaques in groups 5 and 6 were treated intramuscularly with the same dose of AAV-8-rh-3BNC117-IgG1-LS given to the group 3 infants, but the vector lot was different (VCAV-06302). The AAV-8-rh-3BNC117-IgG1-LS inoculum was formulated in PBS as described above and split into four and eight separate muscle sites for the group 5 and group 6 monkeys, respectively. Of note, the group 5 infant rh5-6 was born below the pre-specified weight criterion (≥0.5 kg) to be inoculated with an AAV vector. It took four weeks for monkey rh5-6 to gain enough weight to meet this criterion, so rh5-6 was treated with AAV-8-rh-3BNC117-IgG1-LS one month after its group 5 counterparts.
The macaques in groups 7–11 were treated intramuscularly with 2.5 × 1012 GC kg−1 of the same lot of AAV-8-rh-3BNC117-IgG1-LS (VCAV-06302) given to groups 5 and 6. The AAV-8-rh-3BNC117-IgG1-LS inoculum was formulated in PBS and split into four separate muscle injections, as described above.
When the group 5 macaques reached ~2.5 years of age, they were subjected to weekly intrarectal challenges with a peripheral blood mononuclear cell (PBMC)-derived stock of SHIV-AD8EO. The six rhesus macaques in group 12 served as controls for this experiment. The SHIV-AD8EO stock used for this experiment was amplified in concanavalin A-activated rhesus PBMCs for 7 days. The Gag p27 concentration of the resulting stock was 96 ng ml–1 and each monkey in groups 5 and 12 was challenged intrarectally with 3.8 ng of Gag p27 of this stock. The challenge inoculum for each macaque consisted of 1.0 ml of PBS containing 0.5% of fetal bovine serum and 1:25 dilution of the aforementioned SHIV-AD8EO stock. This volume was loaded into 3-ml syringes and applied intrarectally (without needle) to each macaque. Plasma was collected at the time of each challenge and tested for the presence of vRNA. Monkeys that remained aviraemic continued to be re-challenged in the next week. However, once a macaque experienced two consecutive episodes of positive viraemia or a single episode with a viral load greater than 1,000 vRNA copies ml–1 of plasma, it was deemed to be infected and did not receive additional virus challenges. Plasma viral loads were then monitored for 10 weeks after infection.
SHIV RNA viral load measurements
Three hundred and fifty-microliter EDTA plasma samples were collected from the infant macaques in groups 1–4 during the oral SHIV-AD8EO challenge phase. These samples were diluted 1:1 with TRIS buffer and then RNA was extracted and analysed as previously described51. The threshold of detection on an input volume of 0.35 ml of plasma was 29 vRNA copies ml–1.
Plasma viral loads from rhesus macaques in groups 5 and 12 were measured using 0.5 ml of EDTA-anticoagulated plasma based on a modification of a previously published method51. The threshold of detection on an input volume of 0.5 ml of plasma was 15 vRNA copies ml–1.
Production of monoclonal antibodies for in vivo studies
The recombinant rh-3BNC117-IgG1 and rh-3BNC117-IgG1-LS proteins used in groups B and C were expressed by Chinese hamster ovary (CHO)-K1SP cell lines stably expressing each molecule. Both cell lines were developed and authenticated by Genscript, but they were not tested for Mycoplasma contamination. In sum, linearized plasmids encoding each molecule were transfected into CHO-K1SP cells, followed by cell pool screening and selection. The selected pools were then subjected to single clone screening using the limiting dilution method, followed by single clone batching in six-well plates. After the first batch of single clones was identified, the top six were selected for fed-batch. Based on their growth performance and productivity, the top three clones were selected for final delivery. Both molecules were purified from supernatant by affinity chromatography, followed by cation exchange and ultrafiltration–diafiltration. Both molecules were formulated in citrate buffer (20 mM sodium citrate, 150 mM sodium chloride, pH 6.0, 0.02% Tween-80) at a concentration of ~10.5 mg ml–1. The endotoxin level was less than 1.0 endotoxin units per mg of protein, as determined by the limulus amoebocyte lysate (LAL)/tachypleus amebocyte lysate (TAL) assay. The rh-3BNC117-IgG1-LS molecule (lot U086PGG21009/202201) was produced and purified by Genscript, and the rh-3BNC117-IgG1 protein (RRID: AB_2895627, lot JH21-08) was produced and purified by MassBiologics.
AAV vectors
Three single-stranded AAV transfer plasmids were used to produce the recombinant AAV vectors described in this study. The first one encoded rh-3BNC117-IgG1-LS and was used to prepare the AAV-8 vector used in group 3 and groups 5–11. Transgene expression was under the control of the cytomegalovirus (CMV) promoter. A simian virus 40 (SV40) intron was placed between the promoter and the rh-3BNC117-IgG1-LS transgene. To reduce the immunogenicity of this vector, the promoter and transgene sequences lacked CpG motifs that can serve as ligands for TLR952. The rh-3BNC117-IgG1-LS transgene was bicistronic; that is, both heavy and light chains of IgG1 were expressed from one open reading frame using an F2A ‘self-processing’ peptide from foot-and-mouth disease virus. The cleavage sequence RKRR for the cellular protease furin is added for removal of amino acids that were left on the heavy chain C-terminus following F2A self-processing. The peptide linker SGSG is added for improved furin enzyme-mediated cleavage. Additionally, the 3′ untranslated region contains multiple binding sites for conserved endogenous microRNAs (miRNAs) that are specifically expressed in professional antigen-presenting cells (pAPCs). These miRNA binding sites were included to render the monoclonal antibody transcripts sensitive to translational inhibition by the miRNAs expressed in pAPCs. The second AAV expression cassette encoded a rh-eCD4-IgG2-LS molecule and was used to prepare the AAV-1 and AAV-8 vectors used in groups 1 and 2. Additional relevant features about the rh-eCD4-IgG2-LS protein include an I39N substitution in the CD4 domains intended to increase HIV neutralization potency and the use of mim6 (GGGGGDYYDYDGGYYYDGD) as the carboxyl-terminus co-receptor mimetic peptide. Transgene expression was under the control of the chicken β-actin promoter with a CMV enhancer and an SV40 intron. Downstream from the rh-eCD4-IgG2-LS transgene was the woodchuck hepatitis virus posttranscriptional regulatory element, which was intended to increase transgene expression. The third AAV expression cassette encoded rh-TPST-2 and was used to prepare the AAV-1-rh-TPST-2 construct that was co-delivered with the AAV-1-rh-eCD4-IgG2-LS vector during the intramuscular inoculations of the group 1 and group 2 monkeys. The promoter structure of this vector consisted of the CMV promoter and CMV enhancer, followed by the SV40 intron. All AAV expression cassettes used in this study contained the SV40 poly-adenylation signal and were flanked by AAV-2 inverted terminal repeats. All recombinant AAV vectors used in this study were produced at the Horae Gene Therapy Center and Vector Core at the UMass Chan Medical School as described previously53. In brief, HEK293T cells (American Type Culture Collection, authenticated and tested negative for Mycoplasma contamination) were co-transfected with each transfer plasmid, a plasmid co-expressing the AAV-2 Rep protein with the AAV-1 or AAV-8 capsid, and a helper plasmid encoding adenovirus genes. After collecting lysates of transfected cells, AAV was purified through three sequential CsCl centrifugation steps. The vector GC number per ml was determined by quantitative PCR. The purity of the AAV preparations was verified by silver-stained SDS–PAGE.
RNA-seq analysis
Following collection of peripheral blood (~0.5 ml per time point) in BD PAXgene tubes, the tubes were gently inverted 8–10 times and stored vertically at room temperature for a minimum of 2 h. The tubes were then transferred to a −80 °C freezer where they were stored until the time of the RNA extraction. Total RNA was extracted using a Paxgene Blood miRNA kit (Qiagen 763134), following the manufacturer’s instructions. The purified RNA was eluted in buffer BR5 (supplied in the kit), incubated at 65 °C for 5 min for RNA denaturation, and stored immediately at −80 °C. RNA samples were shipped on dry ice to Novogene for RNA quality control, library preparation and RNA sequencing. cDNA libraries were prepared at Novogene from total RNA using the NEBNext Ultra II RNA Library Prep Kit for Illumina (NEB E7770L). Sequencing was performed on a Novaseq 6000 instrument (Illumina).
After initial quality control, the sequence data were quantified using Kallisto54, to obtain transcript level abundances using Mmul_10 (Ensembl) as reference. Following quantification, DEGs and differentially expressed transcripts (DETs) were identified using Sleuth55. The DETs were identified in samples collected on day 3 and week 4 vs. baseline (day 0) post-AAV vector administration in group 5 and group 6, respectively. We performed a similar analysis in infants in group 7 and in those in groups 8 and 9. Significant DETs were defined using a q-value (Benjamini–Hochberg adjusted P value) threshold of <0.05. Over-representation analysis was performed using the Clusterprofiler56,57 tool to identify enrichment of the genes in specific pathways described in Kyoto Encyclopedia of Genes and Genomes (KEGG)58 and Reactome59 databases. The gene counts for groups 5–9 in Extended Data Figs. 6 and 7 ranged from 20,515 to 28,321.
Estimating monoclonal antibody concentrations in serum
Concentrations of rh-3BNC117-IgG1-LS in macaque serum were quantified by ELISA as follows: 384-well high binding polystyrene plates (Corning 3700) were coated with 4.0 μg ml–1 of the anti-idiotype antibody 1F1 (Protein Production Facility, The Duke Human Vaccine Institute, Duke University, NC) diluted in Dulbecco’s PBS without Ca2+ or Mg2+ (DPBS) for 1.5 h at 37 °C. The plate was washed twice with 10× diluted commercial 0.5% Tween-20 solution (BioWorld 40120769-3) and blocked with 5.0% (w/v) bovine serum albumin (BSA) in DPBS (blocking buffer) for 1 h at 37 °C. The blocking buffer was aspirated off the plate and serum samples, serially diluted in the blocking buffer, were loaded onto the plate. Each assay contained serial dilutions of recombinant rh-3BNC117-IgG1-LS to generate a standard curve. These serial dilutions were performed with blocking buffer and the first well of the series was spiked with macaque serum to a final dilution of 1:2,000. The samples and the standard curve dilutions were incubated in the plate for 1.5 h. The plate was then washed five times. Next, a (Fab)2 fragment conjugated to horseradish peroxidase (HRP) specific for the human Fcγ domain (Jackson Immuno 109-036-008) was diluted 1:5,000 in blocking buffer. This solution was added to the plate and incubated at 37 °C for 1 h. The plate was washed 10 times and developed using 1-step Ultra TMB-ELISA Substrate solution (Thermo Fisher 34028). The reaction was stopped using Liquid Stop Solution for TMB (Surmodics LTSP-1000-01). Absorbance was measured at a wavelength of 450 nm using a BioTek Synergy LX spectrophotometer (Agilent Technologies). To obtain an ELISA standard curve, the recorded absorbance values were plotted on the y axis, while the concentrations of the standard protein, namely rh-3BNC117-IgG1-LS, were plotted on the x axis. Data analysis and curve fitting were performed with GraphPad Prism software, employing a four-parameter logistic or sigmoidal curve model. Subsequently, this model was used for the estimation of unknown concentrations of the analyte within the serum samples via interpolation. Interpolated values derived from the linear region typically in mid to low concentration ranges of the standard curve were utilized for further analyses. The same methodology was used to determine serum concentrations of rh-eCD4-IgG2-LS, except that plates were coated with 4.0 μg ml–1 of a mouse anti-CD4 monoclonal antibody (clone MEM-241; Millipore Sigma SAB4700059) and serial dilutions of recombinant rh-eCD4-IgG2-LS were used to generate the standard curve of the assay.
Estimation of ADA responses in serum
Serum reactivity to rh-3BNC117-IgG1-LS was monitored by ELISA using 384-well high binding polystyrene plates (Corning 3700). These plates were coated with a DPBS solution containing 2.0 μg ml–1 of purified recombinant rh-3BNC117-IgG1-LS, which uses a κ light chain. Each plate was washed twice with 10× diluted commercial 0.5% Tween-20 solution and blocked with 5.0% (w/v) BSA in DPBS for 1 h at 37 °C. The blocking buffer was aspirated off the plate and serum samples, diluted 1:200 in the blocking buffer, were loaded onto the plate. Samples were incubated in the plate for 1.5 h. The plate was then washed five times. Next, a goat polyclonal antibody preparation specific for human IgG λ light chain and conjugated to HRP (Southern Biotech 2070-05) was diluted 1:5,000 in blocking buffer. This solution was added to the plate and incubated at 37 °C for 1 h. The plate was washed 10 times and developed using 1-step Ultra TMB-ELISA Substrate solution (Thermo Fisher 34028). The reaction was stopped using Liquid Stop Solution for TMB (Surmodics LTSP-1000-01). The same 384-well ELISA plate was used to screen all the group 5 and group 6 samples for anti-rh-3BNC117-IgG1-LS antibodies. A separate plate was used for groups 7–11.
The same methodology was used to measure anti-rh-eCD4-IgG2-LS antibody responses. However, because rh-eCD4-IgG2-LS does not have light chains, reactivity was assayed with detector antibodies against both κ (Southern Biotech 2060-05) and λ light chains, both diluted 1:5,000 in blocking buffer. All serum samples from monkeys in groups 1 and 2 were tested at a fixed serum dilution of 1:20. Reactivity against each AAV-delivered molecule was plotted as background- and baseline-subtracted absorbance values measured in each assay.
SHIV neutralization assay
TZM-bl neutralization assays were performed as described60. In brief, rhesus serum was serially diluted, mixed with SHIV-AD8EO Env-pseudotyped SG3.1 pseudovirus, and incubated at 37 °C, 5% CO2 for 1 h. TZM-bl cells (NIH AIDS Reagent Program; not authenticated) were then added to each well and the plate was incubated for an additional 48 h. DEAE dextran was added to the cell containing media before its addition to the plate, such that the final concentration in each well was 15 μg ml–1. Plates were developed using Britelite reagent (PerkinElmer 6066761) and luciferase activity, measured as total luminescence, was quantified using a Synergy LX plate reader (Agilent Technologies). Raw luminescence values were converted to ‘per cent neutralization’ using the formula [1 − (sample luminescence − background luminescence)/(virus control − background luminescence)] × 100 and plotted in GraphPad Prism software. ID50 titres were calculated by fitting each neutralization curve with a 4-parameter logistic non-linear regression, and then interpolating 50% neutralization onto each curve. The TZM-bl cell line tested negative for Mycoplasma contamination.
Estimation of serum anti-AAV antibodies
ELISA plates (384-well high binding polystyrene plates; Corning 3700) were coated with rAAV-8 viral particles by adding 30 µl of AAV-8, diluted to 1.55 × 1010 GC ml–1 in DPBS without Ca2+ or Mg2+, to each well. Coating was allowed to proceed overnight at 4 °C. Plates were then washed twice with a commercial wash buffer (BioWorld 40120769-3) and blocked by adding 90 µl of 5.0% Blotto (Rockland Immunochemicals B5010500) in DPBS followed by incubation at 37 °C for 1 h. The plate was aspirated and serum samples, diluted by a factor of 200 in the same blocking buffer, were loaded onto the plate. The plate was incubated at 37 °C for 1 h and then washed 5 times. A Fab fragment conjugated to HRP, specific for human Fcγ (Jackson Immuno 109-036-008) was added to each well and the plate was incubated at 37 °C for 1 h. The plate was then washed 10 times and developed using 1-step Ultra TMB-ELISA Substrate solution (Thermo Fisher 34028) and Liquid Stop Solution for TMB (Surmodics LTSP-1000-01). All samples in the study were measured on the same ELISA plate, so that valid relative comparisons could be made using raw absorbance values.
Statistics
Kaplan–Meier survival analysis was used to determine whether the rate of SHIV-AD8EO acquisition differed between AAV-treated and control macaques following oral or intrarectal challenges with SHIV-AD8EO. The P values for these comparisons were calculated using the log-rank (Mantel-Cox) test. Differences between serum concentrations of rh-3BNC117-IgG1-LS, anti-rh-3BNC117-IgG1-LS antibody responses (that is, ADAs) and other immune parameters were assessed using the Mann–Whitney U-test.
For comparisons of ADAs between groups, we determined the cumulative levels of these responses for each monkey. Specifically, we calculated the AUC of absorbance values measured during the 20 weeks of follow-up after the AAV vector administration. To avoid confounders related to inter-assay variability in ADA values, only absorbance values measured in the same 384-well ELISA plate were used to calculate AUC values. For these assays, the developing reagents were added to the plates within seconds using an automated 96-channel pipette in order to minimize time differences in well development.
The Spearman rank correlation method was used to search for associations between the age of monkeys at the time of AAV-bNAb vector administration and bNAb serum concentrations and the cumulative levels of anti-bNAb antibody responses measured over time. The incidence of macaques that developed persistent bNAb expression following AAV-bNAb therapy was compared between experimental or age groups using Fisher’s exact test. A significance threshold of 0.05 was used for all statistical tests. All P values reported here are two-tailed.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All the RNA-seq data used for the whole blood transcriptomics analysis are available at https://github.com/CIG-Core/HIV_bnAbs_delivery_Mauricio/tree/main. The other data that support the findings of this study are available from the corresponding author upon reasonable request. Source data are provided with this paper.
Code availability
All code and documentation are available at https://github.com/jishnu-lab/HIV_bnAbs_delivery. A corresponding stable release is available at https://doi.org/10.5281/zenodo.15660098 (ref. 61).
Change history
19 November 2025
In the version of this article initially published, the Acknowledgements did not include thanks for funding from the HIV/AIDS and Emerging Infectious Diseases Institute at the University of Miami through the State of Florida Funding Initiative, as is now amended in the HTML and PDF versions of the article.
References
UNAIDS. The Urgency of Now: AIDS at a Crossroads. 2024 Global AIDS Update (Joint United Nations Programme on HIV/AIDS, 2024).
Corey, L. et al. Two randomized trials of neutralizing antibodies to prevent HIV-1 acquisition. N. Engl. J. Med. 384, 1003–1014 (2021).
Billingham, R. E., Brent, L. & Medawar, P. B. Actively acquired tolerance of foreign cells. Nature 172, 603–606 (1953).
Billingham, R. E., Brent, L. & Medawar, P. B. Quantitative studies on tissue transplantation immunity. III. Actively acquired tolerance. Phil. Trans. R. Soc. B 239, 357–414 (1956).
Women and HIV. A Spotlight on Adolescent Girls and Young Women (UNAIDS, 2019).
World Health Organization. HIV Drug Resistance Report (2019).
Clarke, D. F. et al. Prevention and treatment of HIV infection in neonates: evidence base for existing WHO dosing recommendations and implementation considerations. Expert Rev. Clin. Pharmacol. 11, 83–93 (2018).
Abrams, E. J., Capparelli, E., Ruel, T. & Mirochnick, M. Potential of long-acting products to transform the treatment and prevention of human immunodeficiency virus (HIV) in infants, children, and adolescents. Clin. Infect. Dis. 75, S562–S570 (2022).
Cockbain, B., Fidler, S. & Lyall, H. Preventing perinatal HIV acquisition; current gaps and future perspectives. Curr. Opin. HIV AIDS 19, 293–304 (2024).
Hessell, A. J. et al. Early short-term treatment with neutralizing human monoclonal antibodies halts SHIV infection in infant macaques. Nat. Med. 22, 362–368 (2016).
Ng, C. T. et al. Passive neutralizing antibody controls SHIV viremia and enhances B cell responses in infant macaques. Nat. Med. 16, 1117–1119 (2010).
Shapiro, R. L. et al. Broadly neutralizing antibody treatment maintained HIV suppression in children with favorable reservoir characteristics in Botswana. Sci. Transl. Med. 15, eadh0004 (2023).
Hahn, P. A. & Martins, M. A. Adeno-associated virus-vectored delivery of HIV biologics: the promise of a “single-shot” functional cure for HIV infection. J. Virus Erad. 9, 100316 (2023).
Wang, D., Tai, P. W. L. & Gao, G. Adeno-associated virus vector as a platform for gene therapy delivery. Nat. Rev. Drug. Discov. 18, 358–378 (2019).
Sender, R. & Milo, R. The distribution of cellular turnover in the human body. Nat. Med. 27, 45–48 (2021).
Kollmann, T. R. et al. Neonatal innate TLR-mediated responses are distinct from those of adults. J. Immunol. 183, 7150–7160 (2009).
Levy, O. et al. The adenosine system selectively inhibits TLR-mediated TNF-alpha production in the human newborn. J. Immunol. 177, 1956–1966 (2006).
Upham, J. W. et al. Development of interleukin-12-producing capacity throughout childhood. Infect. Immun. 70, 6583–6588 (2002).
Mold, J. E. et al. Maternal alloantigens promote the development of tolerogenic fetal regulatory T cells in utero. Science 322, 1562–1565 (2008).
Takahata, Y. et al. CD25+CD4+ T cells in human cord blood: an immunoregulatory subset with naive phenotype and specific expression of forkhead box p3 (Foxp3) gene. Exp. Hematol. 32, 622–629 (2004).
Fan, X. et al. Donor-specific B-cell tolerance after ABO-incompatible infant heart transplantation. Nat. Med. 10, 1227–1233 (2004).
Gardner, M. R. et al. AAV-expressed eCD4-Ig provides durable protection from multiple SHIV challenges. Nature 519, 87–91 (2015).
Scheid, J. F. et al. Sequence and structural convergence of broad and potent HIV antibodies that mimic CD4 binding. Science 333, 1633–1637 (2011).
Gardner, M. R. et al. Anti-drug antibody responses impair prophylaxis mediated by AAV-delivered HIV-1 broadly neutralizing antibodies. Mol. Ther. 27, 650–660 (2019).
Martinez-Navio, J. M. et al. Host anti-antibody responses following adeno-associated virus-mediated delivery of antibodies against HIV and SIV in rhesus monkeys. Mol. Ther. 24, 76–86 (2016).
Casazza, J. P. et al. Safety and tolerability of AAV8 delivery of a broadly neutralizing antibody in adults living with HIV: a phase 1, dose-escalation trial. Nat. Med. 28, 1022–1030 (2022).
Priddy, F. H. et al. Adeno-associated virus vectored immunoprophylaxis to prevent HIV in healthy adults: a phase 1 randomised controlled trial. Lancet HIV 6, e230–e239 (2019).
Nduati, R. et al. Effect of breastfeeding and formula feeding on transmission of HIV-1: a randomized clinical trial. JAMA 283, 1167–1174 (2000).
World Health Organization (eds). Guideline: Updates on HIV and Infant Feeding: The Duration of Breastfeeding, and Support from Health Services to Improve Feeding Practices Among Mothers Living with HIV (WHO & UNICEF, 2016).
Cournil, A. et al. Relationship between mortality and feeding modality among children born to HIV-infected mothers in a research setting: the Kesho Bora study. AIDS 27, 1621–1630 (2013).
Mattison, J. A. & Vaughan, K. L. An overview of nonhuman primates in aging research. Exp. Gerontol. 94, 41–45 (2017).
Kinder, J. M., Stelzer, I. A., Arck, P. C. & Way, S. S. Immunological implications of pregnancy-induced microchimerism. Nat. Rev. Immunol. 17, 483–494 (2017).
Immunization, Vaccines and Biologicals (eds) WHO Preferred Product Characteristics for Monoclonal Antibodies for HIV Prevention (WHO, 2022).
Ridge, J. P., Fuchs, E. J. & Matzinger, P. Neonatal tolerance revisited: turning on newborn T cells with dendritic cells. Science 271, 1723–1726 (1996).
Leventhal, J. et al. Tolerance induction in HLA disparate living donor kidney transplantation by donor stem cell infusion: durable chimerism predicts outcome. Transplantation 95, 169–176 (2013).
Chaigne, B. & Watier, H. Monoclonal antibodies in excess: a simple way to avoid immunogenicity in patients. J. Allergy Clin. Immunol. 136, 814–816 (2015).
Maini, R. N. et al. Therapeutic efficacy of multiple intravenous infusions of anti-tumor necrosis factor alpha monoclonal antibody combined with low-dose weekly methotrexate in rheumatoid arthritis. Arthritis Rheum. 41, 1552–1563 (1998).
Steinman, L., Ho, P. P., Robinson, W. H., Utz, P. J. & Villoslada, P. Antigen-specific tolerance to self-antigens in protein replacement therapy, gene therapy and autoimmunity. Curr. Opin. Immunol. 61, 46–53 (2019).
Calcedo, R., Vandenberghe, L. H., Gao, G., Lin, J. & Wilson, J. M. Worldwide epidemiology of neutralizing antibodies to adeno-associated viruses. J. Infect. Dis. 199, 381–390 (2009).
Calcedo, R. et al. Adeno-associated virus antibody profiles in newborns, children, and adolescents. Clin. Vaccine Immunol. 18, 1586–1588 (2011).
Scallan, C. D. et al. Human immunoglobulin inhibits liver transduction by AAV vectors at low AAV2 neutralizing titers in SCID mice. Blood 107, 1810–1817 (2006).
Greig, J. A. et al. Intramuscular administration of AAV overcomes pre-existing neutralizing antibodies in rhesus macaques. Vaccine 34, 6323–6329 (2016).
Bennett, A. et al. Thermal stability as a determinant of AAV serotype identity. Mol. Ther. Methods Clin. Dev. 6, 171–182 (2017).
GGBD 2019 Child and Adolescent Communicable Disease Collaborators. The unfinished agenda of communicable diseases among children and adolescents before the COVID-19 pandemic, 1990-2019: a systematic analysis of the Global Burden of Disease Study 2019. Lancet 402, 313–335 (2023).
Mundel, T. The quest for transformative tools to eradicate malaria. N. Engl. J. Med. 390, 1620–1621 (2024).
Penaud-Budloo, M. et al. Adeno-associated virus vector genomes persist as episomal chromatin in primate muscle. J. Virol. 82, 7875–7885 (2008).
Toromanoff, A. et al. Safety and efficacy of regional intravenous (RI) versus intramuscular (IM) delivery of rAAV1 and rAAV8 to nonhuman primate skeletal muscle. Mol. Ther. 16, 1291–1299 (2008).
Merten, O. W. Development of stable packaging and producer cell lines for the production of AAV vectors. Microorganisms 12, 384 (2024).
Tabebordbar, M. et al. Directed evolution of a family of AAV capsid variants enabling potent muscle-directed gene delivery across species. Cell 184, 4919–4938.e22 (2021).
Kliegman, M. et al. A roadmap for affordable genetic medicines. Nature 634, 307–314 (2024).
Li, H. et al. Envelope residue 375 substitutions in simian-human immunodeficiency viruses enhance CD4 binding and replication in rhesus macaques. Proc. Natl Acad. Sci. USA 113, E3413–E3422 (2016).
Faust, S. M. et al. CpG-depleted adeno-associated virus vectors evade immune detection. J. Clin. Invest. 123, 2994–3001 (2013).
Mueller, C., Ratner, D., Zhong, L., Esteves-Sena, M. & Gao, G. Production and discovery of novel recombinant adeno-associated viral vectors. Curr. Protoc. Microbiol. 14, 14D.1 (2012).
Bray, N. L., Pimentel, H., Melsted, P. & Pachter, L. Near-optimal probabilistic RNA-seq quantification. Nat. Biotechnol. 34, 525–527 (2016).
Pimentel, H., Bray, N. L., Puente, S., Melsted, P. & Pachter, L. Differential analysis of RNA-seq incorporating quantification uncertainty. Nat. Methods 14, 687–690 (2017).
Wu, T. et al. clusterProfiler 4.0: a universal enrichment tool for interpreting omics data. Innovation 2, 100141 (2021).
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS 16, 284–287 (2012).
Kanehisa, M. & Goto, S. KEGG: Kyoto Encyclopedia of Genes and Genomes. Nucleic Acids Res. 28, 27–30 (2000).
Gillespie, M. et al. The reactome pathway knowledgebase 2022. Nucleic Acids Res. 50, D687–D692 (2022).
Montefiori, D. C. Measuring HIV neutralization in a luciferase reporter gene assay. Methods Mol. Biol. 485, 395–405 (2009).
Mehta, I. & jishnu-lab. jishnu-lab/HIV_bnAbs_delivery: v2 (Version v2). Zenodo https://doi.org/10.5281/zenodo.15660099 (2025).
Acknowledgements
The authors thank J. M. McCune for discussion and insights into the project; M. D. Alpert for comments and assistance on matters related to eCD4-Ig; M. Caskey and the Duke Human Vaccine Institute for providing reagents related to 3BNC117; I. M. Castro and M. J. Ricciardi; R. Shoemaker, K. Oswald and R. Fast for plasma viral load analyses; S. L. O’Connor and D. H. O’Connor for sequencing the HEK293T-derived SHIV-AD8EO challenge stock used in this study; J. Watanabe, J. Usachenko and the animal staff of the California National Primate Research Center for technical assistance; and J. Xie and R. He for assistance in preparing AAV vector preps. This work was supported in part by a National Institutes of Health (NIH) supplement grant issued to the Miami Center for AIDS Research (P30AI073961); by Bill and Melinda Gates Foundation investment OPP1196704 (M.A.M.); and by Public Health Service grants (PHS) R01HD102252 (M.A.M.) and R01HD103494 (M.A.M.) from the National Institute of Child Health and Human Development. Additional support came from PHS grants U19AI149646 (M.F.), R01AI175007 (M.A.M.) and U24AI126683 (D.M.M.) from the National Institute of Allergy and Infectious Diseases. Additional support was provided from the National Cancer Institute, NIH, under contract 75N91019D00024/HHSN261201500003I, and from the Office of Research Infrastructure Program, Office of the Director, NIH, through awards P51OD011107 to the California National Primate Research Center and P51OD011104 (RRID: SCR_008167) to the Tulane National Primate Research Center. The study was further supported by a pilot award by the HIV/AIDS and Emerging Infectious Diseases Institute (HEIDI) at the University of Miami through the State of Florida Funding Initiative (to M. Martins) sponsored by the State of Florida, Department of Health (award contract #CODVD to M. Stevenson). The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government.
Author information
Authors and Affiliations
Contributions
A.A., D.O. and M.A.M. conceived the study and designed experiments. D.O., S.S., L.L.J.H., L.A., P.A.H., L.A.B.d.C., S.P.F. and M.A.M. processed biological samples and conducted laboratory work. A.A., M.J.K., J.D.L., K.K.A.V.R. and M.A.M. managed data collection. I.M. and J.D. conducted bioinformatic analysis. S.P.F., J.M.M.-N., M.R.G., K.K.A.V.R., D.M.M., J.D.L., G.G., M.F., R.C.D. and M.A.M. provided technical support and advice on data analysis and interpretation. M.A.M. wrote the manuscript with help and input from A.A., I.M., D.O. and J.D.
Corresponding author
Ethics declarations
Competing interests
M.A.M., M.R.G. and M.F. have significant financial interests in Emmune Inc., a company that is developing HIV immunotherapies based on the immunoadhesin eCD4-Ig. These potential conflicts of interest are being managed by the authors’ respective institutions. The other authors declare no competing interests.
Peer review
Peer review information
Nature thanks Joris Hemelaar and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer review reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Layout of AAV vector inoculations and timing of oral SHIV challenges in Groups 1–4.
a, The three infants in Group 1 were treated intramuscularly (IM) at birth with the indicated dose of an AAV-1 vector expressing rh-eCD4-IgG2-LS. b, The three infants in Group 2 were treated intravenously (IV) at birth with the indicated dose of an AAV-8 vector expressing rh-eCD4-IgG2-LS. Four weeks later, the Group 2 macaques were injected IM with the same dose of the same AAV-1/rh-eCD4-IgG2-LS vector administered to the Group 1 animals. c, The three infants in Group 3 were injected IM at birth with the indicated dose of an AAV-8 vector expressing rh-3BNC117-IgG1-LS. As the nine infants in Groups 1–3 approached 20 weeks of age, a per-protocol transition to paired housing necessitated the removal of one animal from the study. Because serum concentrations of rh-3BNC117-IgG1-LS had fallen below detection limits after week 12 in the Group 3 infant rh3-3, this animal was removed from the study. d, The six AAV vector-naïve infants in Group 4 were matched in age to those in Groups 1–3. Beginning at postnatal weeks 30–34, all the AAV-treated RMs in Groups 1–3 (except for rh3-3) and the Group 4 controls were subjected to weekly oral challenges with escalating doses of SHIV-AD8EO.
Extended Data Fig. 2 Kinetics of weight gain through the first year of life in macaques in Groups 1–3.
Weight (kg) increased at an expected rate in the AAV vector-treated infant macaques in Group 1 (a), Group 2 (b), and Group 3 (c) during the first year of life. The timing of each AAV vector inoculation is indicated by vertical dotted lines and color-coded hexagons.
Extended Data Fig. 3 Serological neutralizing activity against SHIV-AD8EO in macaques in Groups 1–3.
Sera from the macaques in Group 1 (a-c), Group 2 (d-f), and Group 3 (g,h) were tested for their ability to neutralize the in vitro infectivity of SHIV-AD8EO in TZM-bl cells. Neutralizing titers [i.e., inhibitory dilutions at which 50% of neutralization (ID50) was observed] were derived from these assays and plotted against the right y-axis of each panel. As a reference, the serum concentrations of rh-eCD4-IgG2-LS (a-f) or rh-3BNC117-IgG1-LS (g,h) were plotted against the left y-axis. Sera from the Group 3 macaque rh3-3 were not assayed for anti-SHIV-AD8EO neutralizing antibodies because this animal was euthanized before the start of the oral SHIV challenge phase (gray shaded boxes).
Extended Data Fig. 4 Kinetics of AAV-8 seroconversion in Groups 5 and 6.
Total IgG reactivity to the AAV-8 capsid was measured by ELISA using a fixed dilution (1:1,000) of serum collected at baseline (day 0) and every two weeks thereafter until the last follow up at week 20. All samples from the Group 5 (n = 6; a) and Group 6 (n = 6; b) animals were tested in the same 384-well ELISA plate and the absorbance values measured at 450 nm for each sample were plotted against time. c, Geometric means of absorbance values measured for Group 5 (yellow hexagons) and Group 6 (gray hexagons) were plotted against time. The two-sided P value was calculated using the Mann-Whitney U test and resulted from comparing Groups 5 and 6 in terms of their cumulative levels of anti-AAV-8 IgG reactivity (area under curve analysis of absorbance values) measured over the 20 weeks of follow-up.
Extended Data Fig. 5 Layout and timeline of experiments for the pregnant females in Groups A–C and their offspring in Groups 7–11.
Sixteen pregnant female rhesus macaques at similar gestational stages were selected on the basis of having little or no serum reactivity to AAV-8 by ELISA. These animals were then divided into three groups depending on whether they were treated with recombinant forms of rh-3BNC117-IgG1. The Group A dams (n = 8) received no bNAb infusion and underwent cesarean (c)-section when their pregnancies reached term at gestational week 24. The only exceptions were dams rhA-1 and rhA-3, which delivered their babies vaginally ahead of schedule. The dams in Groups B and C (n = 4 each) were treated intravenously with 30 mg/kg of recombinant rh-3BNC117-IgG1-LS or rh-3BNC117-IgG1, respectively, at gestational week 22 and then underwent c-section two weeks later. The offspring of the dams in Groups A-C were transferred to the nursery after birth and then assigned to Groups 7–11. The infants in Groups 7–11 were treated intramuscularly (IM) with 2.0 × 1012 genome copies ml–1 of an AAV-8/rh-3BNC117-IgG1-LS vector at postnatal weeks 4, 8, or 12, as depicted.
Extended Data Fig. 6 Univariate differential expression analysis of whole blood transcripts in Groups 5 and 6.
a-d, Volcano plots depicting the statistical significance (y-axes; negative log10-transformed P values) and fold change (FC) in gene expression (x-axes; log2-transformed FC) in differentially expressed genes (DEGs) measured in Group 5 (a,c) or Group 6 (b,d) on day 3 vs baseline (day 0) (a,b) or at week 4 vs baseline (c,d). Each data point represents one DEG. Those colored in red have both an adjusted P value < 0.1 and a log2 FC ± 0.5. DEGs colored in blue and green meet either the P value or the log2 FC criterion, respectively, but not both. Gray DEGs meet neither criterion and, therefore, are not significant (NS). The Wald test default method in Sleuth was used to assess whether the estimated coefficients (i.e., FCs) for each DEG was significantly different from zero. All P values are two-sided e,f, Heatmaps depicting differences in expression of top significant differentially expressed genes in Group 5 (e) and Group 6 (f) in week 4 vs baseline (day of AAV inoculation) comparisons. The color gradient from blue to red is obtained using z-transformed transcript per million values, where negative (blue) and positive (red) identify low and highly expressed genes, respectively. g,h, Dot plots showing overrepresented pathways by genes that are upregulated at week 4 in Group 5 (g) and Group 6 (h), as annotated in the Reactome database.
Extended Data Fig. 7 Univariate differential expression analysis of whole blood transcripts in Groups 7–9.
For this analysis, Groups 8 and 9 were pooled, whereas Group 7 was examined separately. a,b, Volcano plots, as described in Extended Data Fig. 6, depicting the statistical significance and fold change (FC) in gene expression in differentially expressed genes measured at baseline (day 0) in Group 7 (a) and Groups 8 + 9 (b). The Wald test default method in Sleuth was used to assess whether the estimated coefficients (i.e., FCs) for each DEG was significantly different from zero. All P values are two-sided. NS, not significant. c,d, Dot plots showing overrepresented pathways by genes that are upregulated at week 4 in Group 7 (c) and Groups 8 + 9 (d), as annotated in the Reactome database.
Extended Data Fig. 8 Pharmacokinetics of recombinant forms of rh-3BNC117-IgG1 administered to the pregnant dams in Groups B and C.
a-h, Serum concentrations of rh-3BNC117-IgG1-LS or rh-3BNC117-IgG1 in the Group B (a-d) and Group C (e-h) dams following passive infusion of 30 mg/kg these molecules at gestational week 22 (vertical dotted lines). Two weeks later, pregnancies reached term and the animals underwent cesarean (c)-section (vertical solid line). The last two weeks of pregnancy are indicated by a gray box. i, Table listing the concentrations of rh-3BNC117-IgG1-LS or rh-3BNC117-IgG1 in maternal, cord blood, or newborn serum at the time of c-section.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ardeshir, A., O’Hagan, D., Mehta, I. et al. Determinants of successful AAV-vectored delivery of HIV-1 bNAbs in early life. Nature 645, 1020–1028 (2025). https://doi.org/10.1038/s41586-025-09330-2
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41586-025-09330-2
This article is cited by
-
Structural basis for childhood antibody recognition of the human metapneumovirus fusion protein
Nature Communications (2025)