Abstract
Clostridioides difficile infection (CDI) is the leading cause of healthcare- and antibiotic-associated infection and has a 30% recurrence rate1,2,3,4,5. Previous vaccine strategies against CDI failed to reduce pathogen burden, a prerequisite for preventing C. difficile transmission and recurrence6,7,8,9,10,11. These vaccines were administered parenterally, which induced a systemic immune response, rather than a mucosal response in the colon, the site of infection. Here we compare protection and colonization burden between mucosal (rectal) and parenteral (intraperitoneal) administration routes of a multivalent, adjuvanted vaccine combining inactivated C. difficile toxins and novel surface antigens. We found that mucosal immunization, but not parenteral, clears C. difficile from the host. Unique correlates of decolonization included faecal IgG responses to vegetative surface antigens and a colonic, T helper type 17 (TH17)-skewed tissue-resident memory T cell response against spore antigen. Importantly, mucosal vaccination protected against morbidity, mortality, tissue damage and recurrence. Our results demarcate notable differences in correlates of protection and pathogen clearance between vaccine administration routes and highlight a mucosal immunization regimen that elicits sterilizing immunity against CDI.
Similar content being viewed by others
Main
C. difficile is a spore-forming anaerobic bacterium that is a leading cause of nosocomial infections and the primary cause of antibiotic-associated diarrhoea1. In the United States alone, C. difficile infection (CDI) leads to approximately 500,000 cases, 29,000 deaths and US$4.8 billion in healthcare costs each year2,3,4. As such, substantial efforts have been made to develop vaccines against CDI.
Previous vaccine strategies against CDI have targeted the primary virulence factors, toxins TcdA and TcdB6,7,8,9,10. A phase 3 clinical trial of a bivalent TcdA/TcdB vaccine from Pfizer protected against severe infection but did not meet its primary end point of preventing infection (ClinicalTrials.gov: NCT03090191), while one from Sanofi was discontinued after meeting criteria for futility (ClinicalTrials.gov: NCT01887812). Recently, a multivalent mRNA–lipid nanoparticle candidate vaccine against CDI showed promise in preclinical studies by protecting mice against severe infection and death11. However, these strategies and others demonstrated either minimal or no efficacy in clearing the bacterium from the colon6,7,8,9,10,11,12—a crucial end point when considering C. difficile spore transmission through the faecal–oral route. The 30% incidence of recurrent CDI5 and the documented increase in community-acquired CDI cases among otherwise healthy adults3 underscore the need for an immunization strategy that prioritizes C. difficile clearance.
We established a vaccination approach to potentiate C. difficile clearance while promoting protection against CDI symptoms. Our strategy combined (1) selection of novel vegetative and spore antigens to promote clearance of C. difficile; (2) inactivating point mutations of the C. difficile toxin antigens that retain native structure for broad epitope recognition; (3) the double mutant of Escherichia coli heat labile toxin (dmLT) as a mucosal adjuvant; (4) a rectal route of administration that was compared against parenteral vaccination; and (5) the assessment of humoral and cellular indicators of immune responses to identify correlates of symptom reduction and clearance. We demonstrate a protective mucosal vaccine formulation that provides sterilizing immunity to clear C. difficile from the host.
NTAs induce non-canonical clearance
Sixteen candidate C. difficile non-toxin antigens (NTAs) associated with cell-surface functions were predicted to have low allergenicity, high antigenicity, B cell linear epitopes and MHC-II-binding sites, robust conservation across C. difficile strains, and low homology to host (mouse and human) and commensal-microbial proteins in silico13. We recombinantly expressed and purified 13 of these proteins and selected several for antigenicity testing based on the overall yield and solubility of each protein or protein complex (Supplementary Table 1). We prioritized FlgGEK, a ternary complex comprising the FlgG, FlgE and FlgK flagellar basal-body rod components (Supplementary Information); C40 peptidase 2, a cell-wall-modifying enzyme; polysaccharide deacetylase, a peptidoglycan deacetylase; and CspC, a spore-coat-bound germinant receptor14.
Vaccination-induced bacterial clearance from the colon is mediated by mesenteric lymph node responses. We therefore reasoned that immunization with a mixture of the NTAs at the site of infection would induce a mucosal immune response capable of reducing the bacterial burden. We vaccinated mice 3 times over 28 days either by rectal instillation (r.i.; a proxy for mucosal immunization by enema) or intraperitoneal (i.p.) injection (a proxy for parenteral immunization) (Fig. 1a). All immunizations included dmLT as an adjuvant, which elicits systemic and mucosal humoral and TH17 responses in the gut15. Both r.i. and i.p. vaccination of the NTA mixture promoted survival against lethal challenge with wild-type (WT) C. difficile R20291 (Fig. 1b). However, only i.p.-vaccinated mice were significantly protected against weight loss at 2 days after infection (Fig. 1c–e). Separate cohorts of vaccinated mice were challenged with C. difficile R20291 ∆A∆B (hereafter ∆A∆B), a disrupted toxin strain, to enumerate colonization burden without animal mortality. r.i. of the NTA mixture significantly reduced ∆A∆B colonization burden compared with in the dmLT-only controls (Fig. 1f). Within the r.i.-vaccinated group, there were individual mice that decreased colonization to the limit of detection (500 colony-forming units (CFU) per g faeces) beginning at day 5 after infection and remained uncolonized until the experimental end point. By contrast, i.p. vaccination had no effect on colonization burden (Fig. 1g). This demonstrates that mucosal vaccination of NTAs reduces colonization burden while providing modest protection against severe disease and death.
a, Experimental schematic. The diagram was created using BioRender. b–e, The survival (b) and percentage weight loss relative to day 0 (c), and quantification of weight at 2 days post-infection (d.p.i.) (d) and 3 d.p.i. (e). f,g, Enumeration of C. difficile bacteria in the faeces through CFU titrations after r.i. (f) and i.p. (g) vaccination. The limit of detection is indicated by the dotted lines: 500 CFU per g faeces. For c–e, data are mean ± s.e.m. Statistical significance was calculated using log-rank Mantel–Cox tests (b), one-way ANOVA with Tukey’s correction (d and e) and two-sided Student’s t tests (f and g), with each day analysed separately; *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001; NS, not significant. For b–g, n = 10 per group; decreases in n were due to animal mortality during infection. Individual datapoints are represented and were pooled from two independent experiments.
To determine the individual contributions of each NTA to the protective and colonization-reduction effects from r.i. vaccination with the NTA mixture, we immunized mice through either r.i. or i.p. with a single NTA before challenging with either WT R20291 or ∆A∆B (Extended Data Fig. 1a). Each NTA administered by r.i., as well as C40 peptidase 2 administered by i.p., provided a survival benefit (Extended Data Fig. 1b,c). Importantly, r.i. vaccination of CspC, C40 peptidase 2 and FlgGEK significantly reduced the colonization burden in mice challenged with ∆A∆B compared with the dmLT-only controls (Extended Data Fig. 1d). i.p. vaccination with the individual NTAs did not affect colonization (Extended Data Fig. 1e).
Despite the ability of the vaccine to clear bacteria, r.i.-vaccinated mice did not exhibit increased systemic anti-NTA IgG or faecal IgA, discordant with typical dmLT-adjuvanted mucosal humoral responses15. Indeed, i.p.-vaccinated mice had significantly greater anti-NTA serum IgG (Extended Data Fig. 1f) and faecal IgA (Extended Data Fig. 1g) titres compared with the r.i.-vaccinated mice. By contrast, faecal IgG titres against FlgGEK, C40 peptidase 2 and polysaccharide deacetylase increased in r.i.-vaccinated mice (Extended Data Fig. 1h). While there were no statistically significant increases in anti-NTA faecal IgA or serum IgG in r.i.-vaccinated mice compared with i.p.-vaccinated mice, these titres did correlate positively with the ability of single-NTA r.i.-vaccinated mice to reduce C. difficile burden, but did not for i.p.-vaccinated mice (Extended Data Fig. 1i,j).
r.i. vaccination provides sterilizing immunity
Previous C. difficile vaccines included either chemically crosslinked or formalin-inactivated toxoid antigens of C. difficile toxins TcdA and TcdB6,7,8,9,10. Although these methods allow for safe injection, they potentially disrupt pertinent neutralization epitopes on the toxins16,17. To avoid this, we minimally mutated TcdA and TcdB constructs to prevent glucosyltransferase activity of both toxins (GTX)18. To address residual TcdB toxicity, we included additional mutations to abrogate pore formation (L1106K)19 and CSPG4 receptor binding (D1812G)20. These mutant toxins were verified as natively folded, inactive in a cell rounding assay and safe for immunization in vivo when coupled with dmLT (Supplementary Information).
As a third immunization by r.i. and i.p. did not increase mucosal humoral titres (Extended Data Fig. 1f–h), we immunized mice with a combination of NTAs and inactivated C. difficile toxins using a two-dose, prime–boost schedule (Fig. 2a). The amount of dmLT for r.i. and i.p. vaccinations was also optimized to maximize humoral longevity, reducing dmLT to 15 and 1 µg per dose, respectively (Extended Data Fig. 2).
a, Experimental schematic. Mice were infected for 10 or 15 days, with no differences observed between cohorts. The diagram was created using BioRender. b,c, The survival of infected with WT C. difficile R20291 after r.i. (b) and i.p. (c) vaccination. The bracket refers to the lines of both the toxin + dmLT and toxin + NTA + dmLT cohorts. d,e, Weight loss at 2 d.p.i. (d) and 3 d.p.i. (e) relative to day 0. Data are mean ± s.e.m. f–q, Enumeration of total C. difficile R20291 bacteria (vegetative cells and spores (f–h and l–n)) and spores (i–k and o–q) in faeces after vaccination with dmLT only (f,i,l,o), toxins + dmLT (g,j,m,p) and toxins + NTAs + dmLT (h,k,n,q) through the r.i. (f–k) and i.p. (l–q) routes. P values were calculated relative to the control at the same timepoint. Individual lines correspond to individual mice. The limit of detection is shown by the dotted line: 500 CFU per g faeces. Statistical significance was calculated using log-rank Mantel–Cox tests (b and c) and one-way ANOVA with Tukey’s correction (d–g and f–q (each day analysed individually)). For b–q, n = 20 per group; decreases in n are due to animal mortality during infection. Individual datapoints are represented and were pooled from two independent experiments.
Both r.i. and i.p. vaccination of the toxin and NTA formula promoted survival during challenge with WT C. difficile R20291 (Fig. 2b,c). Vaccination of the toxins alone or in combination with the NTAs by both administration routes protected against weight loss at critical disease timepoints (Fig. 2d,e). Importantly, r.i. vaccination protected against colonic and caecal epithelial injury (Extended Data Fig. 3a,b) on day 3 after infection in comparison to naive unvaccinated mice.
To determine whether the addition of the toxins to a NTA formula reduces colonization in r.i.- and i.p.-vaccinated mice, total CFUs (reflecting both spores and vegetative bacteria) or heat-resistant spores alone were enumerated in the faeces for 10 or 15 days after infection. Vaccination with the toxin and NTA formula by r.i. allowed mice to clear C. difficile by day 9 after infection (Fig. 2f–h) and spores by day 8 (Fig. 2i–k). No spores or vegetative bacteria were present in macerated colons and caeca from these animals (Extended Data Fig. 4a-d), nor did they contain C. difficile as determined by 16S PCR (Extended Data Fig. 4e) and quantitative PCR (qPCR; Extended Data Fig. 4f,g). These results contrasted with i.p.-vaccinated mice, which did not clear C. difficile (Fig. 2l-q and Extended Data Fig. 4a-g) and remained colonized at levels similar to naive infection (Extended Data Fig. 4h). These data demonstrate that r.i., but not i.p., delivery of the inactive toxin and NTA formula eliminates C. difficile at both the faecal and tissue level while protecting against weight loss, epithelial damage and death.
The ability of the inactive toxin + NTA formula to eliminate CDI in r.i.-vaccinated mice led us to next examine whether this administration route and formula could prevent recurrent infection in a vancomycin-induced relapse model (Fig. 3a). Mice r.i.-administered with the toxin + NTA formula were significantly protected against death during CDI relapse compared with the dmLT-only and toxin + dmLT formulas (Fig. 3b). Toxin + NTA-vaccinated mice were also significantly protected against weight loss and diarrhoea during primary and recurrent infection (Fig. 3c,d). These mice also cleared C. difficile during vancomycin treatment and did not relapse for 30 days after infection (Fig. 3i,j), in contrast to the control groups (Fig. 3e-h). Thus, r.i.-vaccination-induced clearance of C. difficile from the host protects against relapse by providing sterilizing immunity.
a, Experimental schematic. The diagram was created using BioRender. b, Survival of mice 30 days after infection and relapse with WT C. difficile R20291. c, Weight loss. d, Stool score. e–j, Enumeration of total C. difficile R20291 bacteria (vegetative cells and spores; e,g,i;) and spores in faeces (f,h,j) after vaccination with dmLT only (e,f), toxins + dmLT (g,h) and toxins + NTAs + dmLT (i,j). P values were calculated relative to the control at the same timepoint. Individual lines correspond to individual mice. The limit of detection is shown by the dotted line: 500 CFU per g faeces. For c and d, data are mean ± s.e.m. Statistical significance was calculated using log-rank Mantel–Cox tests (b) and one-way ANOVA with Tukey’s correction (c and d, and e–j, with each day analysed individually). For b–j, n = 15 per group; decreases in n are due to animal mortality during infection.
Faecal IgG clears vegetative C. difficile
Mucosal and systemic antibody responses to the vaccines were assessed in the sera and faeces before C. difficile challenge to examine the humoral mechanisms of bacterial clearance. While both administration routes induced anti-TcdA serum IgG, systemic humoral responses for all other antigens were elicited only after i.p. injection (Fig. 4a–e). r.i. vaccination did not induce faecal IgA responses against the antigens, apart from TcdA (Fig. 4f–j). However, r.i. vaccination did significantly increase anti-TcdA, anti-C40 peptidase 2 and anti-FlgGEK faecal IgG (Fig. 4k,n,o).
a–e, Sera IgG responses against antigens before challenge at day 28. f–j, Faecal IgA responses against antigens before challenge at day 28. k–o, Faecal IgG responses against antigens before challenge at day 28. p–s, Percentages of T cells in the IEL and LPL compartments of the colon at day 3 after infection. t–v, Enumeration of cytokines produced by ex vivo T cells from vaccinated mice that were co-cultured with CspC-primed dendritic cells in vitro. For a–v, data are mean ± s.e.m. Statistical significance was calculated using one-way ANOVA with Tukey’s correction (a–v). Individual datapoints are represented and were pooled from two independent experiments. For a–o, n = 5–15 per group (dependent on ability to collect samples); p–s, n = 4–10 per group (dependent on whether there was death at day 3 after infection); t–v, n = 3 replicates per group/condition. C40 pep 2, C40 peptidase 2; N, naive/no antigen mice.
Vaccinated mice were euthanized at 3 days after infection with C. difficile and assessed for cellular correlates of humoral immunity. Notably, r.i. of the toxin + NTA formula increased anti-C40 peptidase 2 and anti-FlgGEK memory B cells (Extended Data Fig. 5b) and plasma cells (Extended Data Fig. 5c) in the gut-draining mesenteric lymph nodes. Thus, r.i. vaccination increases mucosal IgG responses and memory against the vegetative antigens C40 peptidase 2 and FlgGEK.
To further gauge the role of anti-vegetative mucosal IgG in C. difficile clearance, as well as determine whether these IgG can transudate from serum to the site of infection, we performed a passive transfer experiment. Donor mice were immunized through r.i. with either dmLT alone or C40 peptidase 2, FlgGEK and dmLT to elicit anti-vegetative antigen mucosal IgG. Faeces was collected 2 weeks after boost, and faecal IgG was isolated and filter-sterilized. Donor faecal IgG was administered through either i.p. or r.i. three times during C. difficile challenge to recipient mice that were previously vaccinated against the inactivated toxins and CspC (Extended Data Fig. 6a).
There were no differences in survival or weight loss between the groups administered control or anti-vegetative antigen faecal IgG from either route (Extended Data Fig. 6c,d). However, mice that had received anti-vegetative antigen faecal IgG through r.i. had significantly less severe diarrhoea than those that had received the control (Extended Data Fig. 6e). These mice also had significantly decreased total C. difficile burden compared with their respective r.i. dmLT-only controls (Extended Data Fig. 6f,g). Total CFU burden was unaffected in mice that were i.p. injected with either group’s mucosal IgG (Extended Data Fig. 6j,k). None of the groups showed statistical differences in C. difficile spore counts, suggesting that the variances in total CFU burden were due to effects on vegetative C. difficile (Extended Data Fig. 6h,i,l,m). A functional in vitro analysis revealed that anti-C40 peptidase 2 and anti-FlgGEK mucosal IgG disrupted C. difficile swimming motility (Extended Data Fig. 6b). Taken together, these data illustrate that anti-C40 peptidase 2 and -FlgGEK faecal IgG reduce vegetative C. difficile burden and impede bacterial movement. These results further demonstrate that anti-vegetative faecal IgG administered through the i.p. route do not reduce colonization burden, suggesting that any contribution of systemic circulating IgG to C. difficile clearance is minimal.
r.i. elicits anti-spore TH17 responses
Although cellular mechanisms of protection against C. difficile have not been studied in the context of rectal immunization, other mucosal vaccines induce tissue-resident memory (TRM; CD103+CD69+) cells at the site of infection21,22. As such, we hypothesized that the immune memory generated by r.i. would also enable TRM cell responses in intraepithelial (IEL) and lamina propria (LPL) lymphocytes.
There were significant increases in CD8+ TRM cells in the IEL (Fig. 4p) and LPL (Fig. 4q) compartments of mice that were r.i. administered the toxin-only or toxin + NTA formulas. Moreover, r.i. administration significantly induced CD4+ TRM cells in both the IEL and LPL compartments (Fig. 4r,s). To define the molecular TRM cell response to specific antigens, we co-cultured colonic CD4+ or CD8+ TRM cells isolated from i.p.- and r.i.-immunized mice with bone-marrow-derived dendritic cells (BMDCs) from naive mice that were primed with a single vaccine antigen. Cytokine profiles from co-cultures were analysed after 3 days. CspC induced a significant increase in TH17-cell-response-associated cytokines, including IL-1β, IL-6 and IL-1α, in T cells from r.i.-vaccinated mice (Fig. 4t–v). These cytokine responses were not produced by CD4+ and CD8+ T cells co-cultured with BMDCs that were primed with the other vaccine antigens (Extended Data Fig. 7a–c). No other notable cytokine responses against the other antigens were observed, including those canonical in the TH1 and TH2 pathways (Extended Data Fig. 7).
To determine whether the inclusion of CspC in the vaccine formula is necessary to clear C. difficile, mice were r.i.-vaccinated with either a formula of inactivated toxins, CspC and dmLT, or a formula of inactivated toxins, C40 peptidase 2, FlgGEK and dmLT. While vaccination with the toxins and CspC significantly protected against death and weight loss (Extended Data Fig. 8a–c), the formula without resulted in a 40% mortality rate and significant weight loss. The CFU burden in mice vaccinated without CspC was significantly increased compared with in the dmLT-only controls (Extended Data Fig. 8e,g). Conversely, mice immunized with the toxin + CspC formula cleared C. difficile spores by day 10 after infection but did not clear total bacterial burden (Extended Data Fig. 8d,f).
Mucosal vaccination has longevity
Although current parenteral C. difficile vaccines elicit long-term protective antitoxin immunity, the longevity of such responses in a colonic mucosal vaccine model have not been investigated. To test whether r.i. administration would durably protect against disease and clear C. difficile, we vaccinated and challenged mice with WT C. difficile R20291 either 60 or 200 days after the final dose (Fig. 5a). Immunization with the toxin and NTA formula protected against death and weight loss at both elongated infection timepoints (Fig. 5b–e). These immunized mice also cleared vegetative C. difficile and spores (Fig. 5k,n,q,t) at both timepoints compared with the dmLT-only (Fig. 5i,l,o,r) and toxin + dmLT-only (Fig. 5j,m,p,s) formulas.
a, Experimental schematic. The diagram was created using BioRender. b,c, Survival of WT mice after infection with C. difficile R20291 at 60 (b) and 200 (c) days after boost. d,e, Weight loss at 2 d.p.i. (d) and 3 d.p.i. (e) after infection at 60 and 200 days after boost. f–h, Percentages of T cells (CD8+ (f), CD8+ TRM (g) and CD4+ TRM (h) LPLs) in the LPL compartment of the colon. i–t, Enumeration of total C. difficile R20291bacteria (vegetative cells and spores; i–k and o–q) and spores (l–n and r–t) in the faeces of mice 60 (i–n) and 200 (o–t) days after boosting, for the dmLT only (i,l,o,r), toxins + dmLT (j,m,p,s) and toxins + NTAs + dmLT (k,n,q,t) groups. For i–t, P values were calculated relative to the control at the same timepoint. Individual lines correspond to individual mice. The limit of detection is shown by the dotted line: 500 CFU per g faeces. For d–h, data are mean ± s.e.m. Statistical significance was calculated using log-rank Mantel–Cox tests (b and c) and one-way ANOVA with Tukey’s correction (d–t; for i–t, each day was analysed individually). For b–e, n = 15 per group; f–h, n = 5 per group; i–t, n = 10 per group; decreases in n were due to animal mortality during infection. Individual datapoints are represented and were pooled from two independent experiments. FACS, fluorescence-activated cell sorting.
To address whether the humoral phenotypes were durable, we measured antigen-specific antibody titres in the sera and faeces at days 14, 74, 134 and 214 (Fig. 5a). There were significant increases in anti-TcdA and anti-TcdB serum IgG, faecal IgA and faecal IgG at 60 and 120 days after boost (day 74 and 134, respectively) (Extended Data Fig. 9a–c). Serum IgG increased against CspC and C40 peptidase 2 at 120 days after boost, and anti-FlgGEK titres trended similarly (Extended Data Fig. 9a). Faecal IgG increased against C40 peptidase 2 and FlgGEK (Extended Data Fig. 9c) at 74 days before waning at 120 days after boost. Thus, there is an expansion of anti-NTA and antitoxin humoral responses, in particular faecal IgG, months after r.i. boost.
We further compared cellular responses at 3 days after infection to determine whether the TRM cells were present at the 60- and 200-day post-r.i.-boost timepoints. Total T cell responses, but not TRM cells, increased in the IEL compartment of vaccinated mice at these elongated timepoints (Extended Data Fig. 10c,e–h). We also found significant increases in CD8+ T cells among LPLs of vaccinated mice (Fig. 5f), as well as CD8+ TRM (Fig. 5g) and CD4+ TRM (Fig. 5h) cells. Taken together, these data highlight the persistence and longevity of r.i.-induced anti-NTA faecal IgG and TRM cells in the lamina propria—responses that correlate with sterilizing immunity against C. difficile.
Discussion
Here we describe the preclinical development of a multivalent, mucosal vaccine comprising inactivated toxins, novel surface-associated NTAs and the dmLT adjuvant, which elicits sterilizing immunity against acute and recurrent CDI. Along with decreasing disease severity, rectal administration of this vaccine reduces tissue damage caused by the C. difficile toxins (Extended Data Fig. 3a,b)—a protection not garnered by other preclinical vaccines11 and antitoxin therapeutics23,24. We expect this strategy to have strong translational value in the effort to develop a human vaccine for CDI, as well as other enteric pathogens. We envision deploying an effective r.i. vaccine as an enema, similar to the original administration route of faecal microbiota transplantation. A recent survey highlighted the willingness of the public to receive a C. difficile vaccine, regardless of administration route, provided that it is effective25.
Given that CDI is primarily a disease of the elderly26, we wanted to evaluate whether the age of immunization or challenge had an impact on the sterilizing immunity inculcated by r.i. We vaccinated mice at both 6- and 12-weeks of age and noted no difference in the responses to C. difficile challenge (combined data are represented in Fig. 2). We also examined the longevity of the immune response and challenged mice with C. difficile at 14, 60 and 200 days after the final r.i. boost. The observation that mice retain TRM cell responses and the ability to clear the pathogen when challenged 200 days after boost (Fig. 5g,h,q,t) provides a positive indication for clinical translation into older populations. A key next step will be to conduct r.i. immunization trials in aged mice (>18 months)27.
Previous C. difficile toxin vaccines were parenterally administered6,7,8,9,10,11. Our results align with these studies in demonstrating that parenteral vaccination decreases morbidity and mortality (Fig. 2b-e), but not bacterial burden, even with the inclusion of C. difficile surface antigens (Fig. 2n,q). Canonical mucosal IgA responses were upregulated in these mice (Fig. 4f–j) but did not correlate with bacterial clearance (Fig. 2n,q). Studies focusing on why the mucosal IgA garnered by parenteral vaccination does not imbue sterilizing immunity may elucidate strategies to overcome these shortcomings in future iterations of preclinical C. difficile vaccines.
Our results highlight that r.i., but not i.p., vaccination elicits robust faecal IgG against the C. difficile NTAs C40 peptidase 2 and FlgGEK (Fig. 4n,o), which clear the vegetative bacterium (Extended Data Fig. 6f,g) and restrict motility (Extended Data Fig. 6b). Other enteric pathogens have been shown to be eliminated from the gut in a faecal-IgG-dependent manner28,29. Although faecal IgG tends to be less abundant than faecal IgA, the concentration does increase in response to enteric infection30. Intestinal IgG-secreting plasma cells can home to the bone marrow31, further suggesting a mechanism for sustained immunological memory. Together, these data implicate a localized anti-surface antigen faecal IgG response, as elicited by r.i., as a key factor in constraining vegetative C. difficile colonization.
We included CspC as a vaccine antigen with the intention of targeting spores during infection. r.i. of formulas including CspC reduce the total colonization burden (Fig. 2h,k and Extended Data Fig. 8d–g) faster than the toxin + dmLT formula alone (Fig. 2g). However, the lack of anti-CspC antibody responses (Fig. 4c,h,m) suggests a cellular mechanism of spore clearance. Indeed, CspC-primed BMDCs elicited TH17-cell-response-associated cytokines from CD4+ and CD8+ TRM cells during co-culture (Fig. 4t–v). Notably, IL-17a was lacking from our cytokine assay responses (Extended Data Fig. 7g). Previous reports have highlighted difficulties with low limits of IL-17a quantification in human sera samples using Luminex analysis, which may explain our results32,33.
Alternatively, a reduction in or lack of IL-17a in a TH17-cell-driven response has been linked to intracellular bacterial infections in the gut34. This, coupled with the significant increase in CD8+ TRM in r.i.-vaccinated mice (Fig. 4p,q), was interesting, as C. difficile is an extracellular pathogen. Two recent studies have implicated spore internalization by intestinal epithelial cells as a possible mechanism for recurrent CDI35,36. This idea is bolstered by the facts that carriage of toxigenic C. difficile among otherwise healthy individuals can go undetectable by 16S rRNA stool sequencing37, and that 83–88% of those who experience recurrent CDI are reinfected by their original strain38,39. Taken together, these data may suggest that hidden spore reservoirs in the gut can germinate and reseed infection in susceptible hosts.
As such, we speculate that CD8+ TRM cells are promoting the elimination of hidden spore reservoirs in the host. This theory may explain the oscillation in spore and vegetative cell counts observed in r.i.-vaccinated mice that clear infection (Fig. 2h,k and Fig. 5k,n,q,t), as spores may germinate in response to the clearance of vegetative bacteria until all reservoirs are eliminated. Colonic-resident CD8+ TRM cells are maintained with minimal homeostatic turnover and do not repopulate from circulation40, which validates the long-lived CD8+ TRM cells (Fig. 5g,h) and clearance phenotypes (Fig. 5k,n,q,t) in our model. Future studies that define the mechanism of spore clearance are important for C. difficile immunization endeavours to halt transmission and recurrence.
Methods
Protein expression and purification
Point mutations were made in WT VPI10463 TcdA and WT TcdB2 as described previously18,19,20. Primer information can be found in Supplementary Table 2. TcdA, TcdB and CspC were recombinantly expressed and purified as previously described18,41. Plasmid information for all antigens is provided in Supplementary Table 2. Plasmids encoding NTAs were codon-optimized versions of the candidate NTAs from the C. difficile R20291 background which were synthesized at Genscript into a pET47b(+) vector and included a C-terminal 6×-histidine tag for protein purification. C40 peptidase 2, FlgG, FlgE, FlgK, CspC and polysaccharide deacetylase were transformed into E. coli BL21 (DE3) STARs (Supplementary Table 2). To express each NTA, 12 l of lysogeny broth medium supplemented with 50 mg l−1 kanamycin were inoculated with an overnight culture to an optical density at 600 nm (OD600) of 0.1. Cells were grown at 37 °C and 220 rpm. Expression was induced with 1 mM Isopropyl-β-D-1-thiogalactopyranoside (IPTG) once cells reached an OD600 of 0.4–0.6. After 4 h, cells were centrifuged and the pellets were resuspended in 20 mM Tris (pH 8.0), 500 mM NaCl, 2% lysis mix (phenylmethylsulfonyl fluoride (0.1 mM), leupeptin (2 mg ml−1), pepstatin (2 mg ml−1), 2% DNase (2 mg ml−1) and 2% lysozyme (10 mg ml−1)). Bacterial suspensions were lysed three times using an EmulsiFlex C3 microfluidizer (Avestin) at 15,000 lb in−2. Lysates were centrifuged at 40,000g for 45 min at 4 °C. NTAs were initially isolated from supernatant using a Ni2+-affinity column (HisTrap FastFlow Crude; GE Healthcare). NTA eluents were further purified using an S-200 size-exchange column (GE Healthcare) in 20 mM HEPES (pH 6.9) with 50 mM NaCl on the ÄKTA Pure fast protein liquid chromatography system (Cytiva). All of the samples were treated using an endotoxin removal kit (Thermo Fisher Scientific) and sterile filtered through a 0.22-µm filter before being aliquoted for immunization studies and stored at −80 °C.
The ternary complex of FlgGEK was produced by co-purifying FlgG, FlgE and FlgK. In brief, supernatants of the three proteins were mixed in a 1:1:1 ratio after lysis and centrifugation, before purification by Ni2+-affinity and S-200 size-exchange chromatography and subsequent endotoxin removal, filtration and freezing, as described above.
dmLT was provided by PATH (Acknowledgements and Data Availability) in 1× PBS supplemented with 0.05% Tween-20 (0.6 mg ml−1).
Animals and study design
Male and female C57BL/6J mice (Jackson Laboratories, 000664) were used in all studies. Mice were assimilated to the new facility 1 week before immunization. Mice were maintained at Vanderbilt University Medical Center under 12 h–12 h light–dark cycles under an ambient temperature of 23 °C (±3 °C) and 50% humidity (±20%), with ad libitum access to chow pellets and water. These studies were approved by the Institutional Animal Care and Use Committee at Vanderbilt University Medical Center and were performed using protocol M2200087-00. All animals were randomly assigned to experimental groups. Researchers were not blinded to groups throughout the animal experiments to properly monitor individual weight loss and morbidity during C. difficile infection according to institutional euthanasia guidelines.
For NTA-cocktail and individual NTA studies, 6-week-old male and female mice were immunized three times over the course of 28 days, with 14 days spanning between injections. Intraperitoneally injected mice received 5 µg of dmLT adjuvant with 5 µg of FlgGEK, C40 peptidase 2, CspC and/or polysaccharide deacetylase in sterile PBS in a total volume of 100 µl per injection. r.i.-treated mice received 25 µg of dmLT adjuvant with 5 µg of FlgGEK, C40 peptidase 2, CspC and/or polysaccharide deacetylase suspended in 200 µl of PBS. Mice were rectally instilled after faecal collection to empty the colon. r.i. occurred under anaesthesia using a sterilized metal ball-end gavage needle that was inserted into the rectum. The vaccine formula was pulsed into the colon, and the rectum was manually squeezed shut for 15 s after administration to prevent leakage, as described previously42. All vaccinations were administered within 2 h of antigen thaw. Faecal and serum samples were obtained before each vaccination and challenge. Mice were challenged 14 days after the final boost, as previously described43,44. Antibiotic treatment was administered by providing 0.5 mg ml−1 cefoperazone in the drinking water ad libitum for 5 days, followed by a 2-day recovery period where normal water was provided before CDI through oral gavage. Two different C. difficile strains were used where indicated: WT R20291 and R20291 ∆A∆B45, both administered at a dose of 1 × 103 spores per mouse. Mice were monitored daily for survival and weight loss. Animal cages were kept the same (left unchanged) for the entirety of the infection. Mice were humanely euthanized when weight loss exceeded 20% of their original body weight. Faecal samples were obtained daily during challenge for CFU enumeration.
For studies to analyse the toxicity of various TcdA and TcdB point mutants, 6-week-old mice were intraperitoneally injected as described above with 5 µg of dmLT and either 1 or 5 µg of the following toxins/toxin combinations: TcdAGTX; TcdB2GTX,L1106K; TcdAGTX + TcdB2GTX,L1106K; TcdB2GTX,L1106K,D1812G; or TcdB2GTX,L1106K + TcdB2GTX,L1106K,D1812G. For combination vaccines with two antigens, 1 or 5 µg of each antigen was injected for a combined total antigenic amount of 2 or 10 µg. The mice were monitored for signs of morbidity and mortality for 7 days after injection.
For studies to optimize the amount of dmLT to include in vaccination, 6-week-old mice were either i.p. injected or rectally instilled with varying amounts of dmLT. Mice were intraperitoneally injected twice over 2 weeks with 0, 0.5, 1, 2.5 or 5 µg of dmLT alongside 5 µg of TcdAGTX or rectally instilled twice over 2 weeks with 0, 10, 15, 20 and 25 µg dmLT with 5 µg of TcdAGTX. Sera and faeces were collected at days 0 (first dose), 14 (second dose), 28, 58 and 88 for enzyme-linked immunosorbent assays (ELISA) analysis of vaccine-induced humoral immune responses.
For studies comparing vaccination of dmLT adjuvant alone to toxin mutants with dmLT and toxin mutants with the NTA cocktail and dmLT, 2 cohorts of 6- and 12-week-old mice were immunized twice with vaccinations spaced 14 days apart. Intraperitoneally injected mice received 1 µg dmLT; 1 µg dmLT with 5 µg each of TcdAGTX, TcdB2GTX,L1106K, TcdB2GTX,L1106K,D1812G; or 1 µg dmLT alongside 5 µg each of TcdAGTX, TcdB2GTX,L1106K, TcdB2GTX,L1106K,D1812G, CspC, C40 peptidase 2 and FlgGEK. r.i.-treated mice received: 15 µg dmLT; 15 µg dmLT with 5 µg each of TcdAGTX, TcdB2GTX,L1106K and TcdB2GTX,L1106K,D1812G; or 15 µg dmLT alongside 5 µg each of TcdAGTX, TcdB2GTX,L1106K, TcdB2GTX,L1106K,D1812G, CspC, C40 peptidase 2 and FlgGEK. Serum and faecal samples were collected as described above. Mice were challenged as stated above with WT C. difficile R20291. Mice were either euthanized for histopathological analysis and flow cytometry analysis on day 3 after infection or were monitored for 10 (6-week-old mice) or 15 (12-week-old mice) days after infection as described above.
For relapsing infection studies, 6 week-old mice were immunized by r.i. with the same experimental groups and same amounts of adjuvant and antigens as noted above. Then, 2 weeks after the final boost, the mice were challenged as stated above with WT C. difficile R20291. Two days after infection, the mice received 0.5 mg ml−1 vancomycin ad libitum in the drinking water for 10 days to clear infection, as described elsewhere46,47. After receiving vancomycin for 10 days, the mice were returned to regular drinking water and monitored for 30 days to document relapsing infection. Stool samples were scored on a 1–5 scale for colour and composition, similar to our previous work48, and were determined as follows: 5, normal, well-formed stool; 4, well-formed, slightly moist or slightly discoloured stool; 3, moist and discoloured stool; 2, soft diarrhoea without wet tail; and 1, wet tail, watery diarrhoea and empty rectum. Animal cages, food and water bottles were changed daily for the entirety of the infection to reduce cross-contamination risk.
For passive transfer studies, 6-week-old donor mice were immunized by rectal instillation with either 15 µg dmLT; or 15 µg of dmLT alongside 5 µg each of C40 peptidase 2 and FlgGEK. Then, 2 weeks after boost, faecal samples were collected from donor mice, as were colonic and caecal contents post-mortem. Faecal and caecal contents were pooled per group and homogenized in 1:1 (w/v) PBS with 2% lysis mix (described above) before centrifugation for 10 min at 10,000g. The resultant supernatant was removed, sterile-filtered with 0.22 µm filters and incubated with anti-mouse IgG MicroBeads (Miltenyi Biotech) for extraction of faecal IgG using an LS Column (Miltenyi Biotech) and MidiMACS magnet system (Miltenyi Biotech). A total of 3.8 mg ml−1 and 3.3 mg ml−1 of faecal IgG were obtained from dmLT-only and C40 peptidase 2- and FlgGEK-vaccinated donors, respectively. Concentrations were obtained on a Nanodrop One C Microvolume UV Spectrophotometer (Thermo Fisher Scientific). Meanwhile, a cohort of 6-week-old recipient mice were r.i.-vaccinated with 15 µg of dmLT alongside 5 µg each of TcdAGTX, TcdB2GTX,L1106K, TcdB2GTX,L1106K,D1812G and CspC. The recipient mice were challenged as stated above with WT C. difficile R20291. At days 1, 4 and 7 after infection, mice received a passive transfer of isolated, sterile-filtered faecal IgG from donor mice either by i.p. (100 µl) or r.i. (200 µl). Recipient mice were monitored for 10 days after infection, as noted above. The animal cages were changed daily for the entirety of the infection.
For studies comparing vaccination formulas with and without the inclusion of CspC, 6-week-old mice were rectally instilled with 15 µg dmLT; 15 µg dmLT alongside 5 µg each of TcdAGTX, TcdB2GTX,L1106K, TcdB2GTX,L1106K,D1812G and CspC; or 15 µg dmLT alongside 5 µg each of TcdAGTX, TcdB2GTX,L1106K, TcdB2GTX,L1106K,D1812G, C40 peptidase 2 and FlgGEK. The mice were challenged as stated above with WT C. difficile R20291. The animals were monitored for 10 days after infection as described above, and the cages were changed daily for the entirety of the infection.
For longevity studies, two cohorts of 6-week-old mice were immunized by r.i. with the same experimental groups and same amounts of adjuvant and antigens as noted above. One cohort of mice was challenged as previously stated with WT C. difficile R20291 60 days after boost, whereas the other was challenged 200 days after boost. Mice were either euthanized for flow cytometry analysis on day 3 after infection or were monitored for 10 days after infection as described above. Animal cages were changed daily for the entirety of both infections.
Antigen-specific antibody measurements
ELISAs were performed. Nunc MaxiSorp 384-Well Plates (Thermo Fisher Scientific) were coated with 30 µl per well of 1 µg ml−1 recombinant TcdA, TcdB2, CspC, C40 peptidase 2, FlgGEK or polysaccharide deacetylase. After overnight incubation at 4 °C, the plates were washed three times with PBS with 0.1% Tween-20 (PBS-T) (100 µl per well per cycle) and replaced with blocking solution (PBS with 0.1% Tween-20 and 2% (w/v) BSA). The plates were then incubated, rocking for 1 h at room temperature. Faeces were homogenized in 1:1 (w/v) PBS with 2% lysis mix (described above) and centrifuged for 10 min at 10,000g. Serum samples were diluted 1:100 in PBS with 2% lysis mix. Plates were washed three times with PBS-T before incubating with 20 µl per well of diluted samples for 2 h, rocking at room temperature. The plates were washed thrice with PBS-T before incubating for an hour with 30 µl per well of horseradish peroxidase (HRP) F(ab’)2-specific goat anti-mouse IgG (Jackson ImmunoResearch; 1:2,000) or goat anti-mouse IgA-HRP (Southern Biotech; 1:2,000) in PBS-T with 2% BSA. Plates were washed four times with PBS-T. Then, 30 µl of TMB substrate reagent (Thermo Fisher Scientific) was added to plates and 30 µl of 2 M sulfuric acid was added after 3 min of substrate development. Plates were recorded at wavelengths of 450 nm using a BioTek Cytation 5 plate reader (Agilent). Faecal antibody titres were normalized to milligram of faeces. Graphs were generated using GraphPad Prism v.10.4.2, and statistical differences between groups were assessed using one-way ANOVA and Tukey’s HSD test.
C. difficile enumeration
C. difficile burden in the stool was quantified by counting CFU from serially diluted stool in 1× PBS (pH 7.4) and plated on taurocholate-cycloserine-cefoxitin-fructose agarose (TCCFA) semi-selective medium49. Faeces was heat treated for 20 min at 75 °C to kill vegetative cells before plating on TCCFA to enumerate spores50. Similarly, bacterial burden in caecal and colonic tissue were quantified by macerating dissected tissues in 1× PBS until slurries were created and plating on TCCFA agar to enumerate total bacterial and spore burdens. Graphs were generated using GraphPad Prism v.10.4.2, and statistical differences between groups were assessed for each day using one-way ANOVA and Tukey’s HSD test.
For PCR analyses, DNA from caecal and colonic tissues (macerated for bacterial burden above) was extracted using the QIAamp PowerFecal Pro DNA Kit (Qiagen). The C. difficile-specific 16S rRNA-encoding gene PCR was used to verify the presence of the bacterium in tissue samples. The PCR set-up was identical to previous published protocols51,52, with template DNA normalized to 50 ng among all of the samples. The following primers were used (ordered from IDT): forward primer 5′-TTGAGCGATTTACTTCGGTAAAGA-3′ (25 nmol, standard desalt purification); reverse primer 5′-CCATCCTGTACTGGCTCACCT-3′ (25 nmol, standard desalt purification)53. PCR products were run on a 1% agarose gel and imaged using a ChemiDoc MP (Bio-Rad).
For qPCR analyses, reactions were set up precisely as outlined elsewhere53, using the same primers as listed above for PCR and TaqMan Fast Advanced Master Mix for qPCR (Thermo Fisher Scientific). Template DNA extracted above from the caecal and colonic tissues were normalized to 50 ng among all samples. Primer amplifications was identified using a C. difficile-specific 16S probe (ordered from IDT): 5′-6-FAM-CGGCGGACGGGTGAGTAACG-MBG-3′ (100 nmol, HPLC purification). Reactions were run on the QuantStudio 6 Flex qPCR system (Thermo Fisher Scientific). Graphs were generated using GraphPad Prism v.10.4.2, and statistical differences between groups were assessed using one-way ANOVA and Tukey’s HSD.
Differential scanning fluorometry
0.1 mg ml−1 each of recombinant WT VPI TcdA, VPI TcdAGTX, WT TcdB2, TcdB2GTX,L1106K and TcdB2GTX,L1106K,D1812G were loaded into glass capillaries and tested using a Tycho differential scanning fluorometer (NanoTemper) according to the manufacturer’s instructions.
Cell rounding assay
Vero–GFP cells54 were seeded in a black, clear-bottom 96-well plate at a concentration of 25,000 cells per well and incubated overnight. Recombinant WT TcdB2, TcdB2GTX, TcdB2L1106K, TcdB2GTX,L1106K, TcdB2GTX,L1106K and TcdB2GTX,L1106K,D1812G were serially diluted tenfold in culture medium, and 100 μl of each sample was added to individual wells in technical duplicate. The plates were statically incubated in a BioTek Cytation 5 plate reader (Agilent) at 37 °C under 5% CO2 and imaged under the bright-field and GFP channels every 45 min at ×20 magnification for 24 h. This experiment was performed twice. The normalized number of rounded cells versus the number of total cells per image was calculated and analysed for concentrations of 1 pM at selected timepoints as previously described54. Graphs were generated using GraphPad Prism v.10.4.2, and statistical differences between groups were assessed using two-way ANOVA and Tukey’s HSD test.
Histopathology
Caeca and colons were fixed in 10% neutral-buffered formalin, dehydrated in graded ethanol series, cleared with xylenes and embedded in paraffin. Tissue blocks were sectioned at a thickness of 5 µm on the HM 335E microtome (Microm) onto Superfrost Plus microscope slides (Thermo Fisher Scientific). To assess histopathology, caecum and colon sections were stained with haematoxylin and eosin (Vector Labs), and conditions were masked for a board-certified gastrointestinal pathologist and a board-certified veterinary pathologist to separately score oedema, inflammation and epithelial damage based on published criteria (n = 5 per treatment)55,56. The averages of the scores from the two pathologists were reported. Histological scores were graphed using GraphPad Prism v.10.4.2, and statistical differences were determined using one-way ANOVA and Tukey’s HSD test. Presented images were captured using a BioTek Cytation 5 automated digital image system (Agilent). Whole slides were imaged at ×10 magnification to a resolution of 0.25 µm px−1.
C. difficile motility assay
WT C. difficile R20291 was grown at 37 °C in BHIS (37 g l−1 brain–heart infusion broth supplemented with 5 g l−1 yeast extract) anaerobic conditions using a COY anaerobic gas chamber (COY Laboratory Products) until mid-log phase. 1 ml of C. difficile was centrifuged at 10,000g for 5 min and the supernatant was removed. The bacterial pellet was either resuspended in 1 ml of 1× PBS (pH 7.4), sterile-filtered dmLT faecal IgG, or sterile-filtered anti-FlgGEK and -C40 peptidase 2 faecal IgG (obtained as noted in the passive transfer mouse experiment, above) and incubated for 30 min. Then, 10 µl of bacterial–faecal IgG mixture was then spotted onto BHIS plates containing 0.3% agar, as previously described57. The plates were incubated at 37 °C for 8 h and room temperature for 16 h under anaerobic conditions. Measurements of the diameter of the widest point of bacterial growth were taken for each spotted colony with a ruler. PBS-incubated C. difficile grew a lawn on BHIS plates, so measurements were taken until the edge of swimming motility, before lawn growth.
Spleen and mesenteric lymph node collection
Spleens were collected, macerated into single-cell suspensions, and filtered using 70 µm cell strainers in 1× Hank’s buffered saline solution (1× HBSS) (Thermo Fisher Scientific). Red blood cells were lysed using ACK lysis buffer (Thermo Fisher Scientific) to obtain a single-cell suspension. Cells were centrifuged and resuspended in 500 µl 1× HBSS, counted and used immediately. Gut-draining mesenteric lymph nodes were collected and processed as described above (without ACK).
Preparations of colons to obtain IELs and LPLs
IEL and LPL fractions were obtained and validated as previously described58,59. In brief, colons were collected, cleaned of fat residue and faeces, and cut open longitudinally before two sequential washes with cold 1× HBSS. The colons were cut into ~0.7 cm chunks and added to 15 ml conical vials with 2 ml of ice-cold HBSS. To these, 5 ml of DTT mix (1× HBSS supplemented with 20 mM HEPES, pH 8.0, 1 mM sodium pyruvate and 1 mM DTT) was added before a 15 min incubation at 37 °C. The conical vials were then shaken by hand for 2 min. The supernatant was transferred to a new 15 ml conical vial containing 5 ml cRPMI-10% FCS (RPMI-GlutaMax supplemented with 10% FBS and 10 mM HEPES, pH 8.0), whereas the tissue was reserved for LPL extraction (below). IELs in the supernatant were further enriched using a Percoll density gradient (Sigma-Aldrich). IELs were centrifuged for 20 min at 4 °C and 650g. The supernatant was aspirated, and IELs were resuspended in 250 µl of 1× PBS supplemented with 0.5% BSA and 1 mM EDTA (constituting PBE buffer). Cells were immediately stained for flow cytometry analyses.
For the LPL compartment, the remaining colonic tissue was kept in the original 15 ml conical vial. Then, 5 ml of EDTA-only mix (1× HBSS supplemented with 20 mM HEPES, pH 8.0, 1 mM sodium pyruvate and 0.5 mM EDTA) was added. The samples were incubated for 10 min at 37 °C. Next, the vials were shaken by hand for 2 min and the supernatant was discarded. Tissue was removed with tweezers and finely minced with scissors into a new 15 ml conical vial containing 3 ml digest mix (1× HBSS supplemented with 20% FBS, 3 mg collagenase D and 0.06 mg DNase I). Samples were then incubated at 37 °C for 30 min. Tubes were shaken by hand for 1 min before pipetting supernatant into new 15 ml conical vials containing 2 ml cRPMI-10% FCS (RPMI-GlutaMax supplemented with 10% FBS and 10 mM HEPES, pH 8.0). LPL cells were centrifuged 20 min at 4 °C and 650g. The supernatant was aspirated, and LPLs were resuspended in 250 µl of 1× PBE. Cells were immediately stained for flow cytometry analyses.
Production of fluorescently labelled recombinant proteins for antigen-specific B cells
Fluorescently labelled recombinant TcdA, TcdB, CspC, C40 peptidase 2, and FlgGEK were prepared by biotinylation using a EZ-Link Sulfo-NHS-LC-Biotinylation kit (Thermo Fisher Scientific, 21435) and conjugated to Streptavidin-linked BV650 (BioLegend, 405231), Alexa Fluor 568 (Thermo Fisher Scientific, S11226), FITC (BioLegend, 405201), APC-Cy7 (BioLegend, 405208) and Alexa Fluor 680 (Thermo Fisher Scientific, S32358). Labelling reactions were calculated to produce a 1:1 ratio of fluorophore:protein. Labelled proteins were flash-frozen in liquid N2 and stored at −80 °C until use to prevent degradation.
Flow cytometry analysis of B and T cells
Single-cell suspensions were incubated with Zombie Near-IR cell viability dye (BioLegend, 423105) for 30 min at room temperature. Cells were washed with 1× PBE, centrifuged at 650g for 10 min and then resuspended in 1× PBE with 5% normal goat serum (60 mg ml−1, Thermo Fisher Scientific) for blocking at room temperature for 30 min. For T cell analysis, cells were stained with anti-CD45 (eFluor 450, 30-F11, 1:600, Thermo Fisher Scientific, 50-112-9409), anti-∆yTCR (PerCP-Cy5.5, GL3, 1:600, BioLegend, 118117), 5-OP-RU tetramer (PE, 1:1,500, NIH Tetramer Core Facility; Data availability), anti-TCRb (Alexa Fluor 594, H57-597, 1:600, BioLegend, 109238), anti-B220 (FITC, RA3-6B2, 1:600, BioLegend, 103205), anti-CD4 (BV570, RM4-5, 1:150, BioLegend, 100541), anti-CD8 (Alexa Fluor 532, 53-6.7, 1:300, Thermo Fisher Scientific, 58-0081-80), anti-CD69 (APC, H1.2F3, 1:300, BioLegend, 104513), and anti-CD103 (PE-Fire 810, QA17A24, 1:300, BioLegend, 156919) for 30 min at room temperature. For B cell analysis, cells were stained with anti-CD45 (eFluor 450, 30-F11, 1:600, Thermo Fisher Scientific, 50-112-9409), anti-B220 (BV480, RA3-6B2, 1:300, BD Biosciences, 565631), anti-CD27 (BV510, LG.3A10, 1:300, BD Biosciences, 563605), anti-CD138 (BV785, 281-2, 1:300, BioLegend, 142534) and the fluorescently labelled recombinant vaccine antigens noted above for 30 min at room temperature. Cells were washed with 1× PBE and centrifuged at 650g for 10 min before fixation in 4% paraformaldehyde fixation for 30 min at room temperature. Cells were then centrifuged, washed with 1× PBE and resuspended in 250 µl of 1× PBE. Flow cytometry data were acquired on a Cytek Aurora Spectral Flow Cytometer (Cytek) and analysed using SpectroFlow Software (v.3.3.0, Cytek). Before flow cytometry analysis, gating of cell populations was determined using Fluorescence Minus One (FMO) controls. FMO controls were prepared by staining replicate cellular samples and beads (Thermo Fisher Scientific, U20250) with all fluorophore-conjugated antibodies in a panel with the exception of one to be analysed for a given control. This accounted for fluorescence spillover and spread across channels and allowed for the precise determination of the positive and negative populations. The gating strategy is provided in the Supplementary Information. Graphs were generated using GraphPad Prism v.10.4.2, and statistical differences between groups were assessed using one-way ANOVA and Tukey’s HSD test.
Priming of naive dendritic cells with antigens and co-culture with TRM cells
BMDCs were isolated from naive C57BL/6J mice and differentiated using GM-CSF (Thermo Fisher Scientific, 315-03-50UG), IL-4 (Thermo Fisher Scientific, 214-14-50UG) and Flt3L (Thermo Fisher Scientific, 250-31L-50UG) as described previously60,61. The day before co-culture with TRM cells, BMDCs were activated with 10 ng ml−1 of lipopolysaccharide (LPS, Thermo Fisher Scientific) and 1 µM of individual antigens or LPS alone. BMDCs were incubated with antigens for 24 h at 37 °C and 5% CO2.
On the day of co-culture, colons from mice vaccinated by i.p. or r.i. with dmLT only or dmLT, toxins and NTAs were collected (n = 3 per group). LPLs were extracted from colons as stated above, pooled within groups, and stained for T cell markers. CD4+ and CD8+ TRM cells were flow-sorted using the Cytek Aurora CS Cell Sorter (Cytek) following the gating strategy provided in the Supplementary Information.
BMDCs were resuspended, washed to remove LPS and growth factors and seeded into 12-well tissue culture plates (Thermo Fisher Scientific) at 5,000 cells per well in 2 ml medium. Based on the counts obtained from the cell sorter, 1,000 CD4+ or CD8+ TRM cells were added to each well of DCs. Cells were incubated together at 37 °C for 72 h before 1 ml of co-culture supernatant was removed and flash-frozen at −80 °C for liquid bead cytokine analysis.
Liquid bead cytokine array
Two custom 12-plex Mouse Luminex Discovery Assay kits (BioTechne) were used to quantify IL-7, IL-12 p70, IL-1β/IL-1F2, IL-2, IL-4, IL-5, IL-6, IL-10, IL-13, IL-17/IL-17a, IFNγ and IL-1α/IL-1F1. Assays were run in triplicate according to manufacturer’s protocol. Acquisition was on a Luminex FlexMap 3D (Luminex). Data were analysed using Millipore Belysa (v.1.0.19) using a four-parameter logistic regression model for calculating concentrations from each standard curve. Graphs were generated using GraphPad Prism v.10.4.2, and statistical differences between groups were assessed using one-way ANOVA and Tukey’s HSD test.
Statistics and reproducibility
Data are presented as mean ± s.e.m. where applicable. Quantitative variables were tested for normal distribution using D’Agostino–Pearson normality tests. If normality was not indicated, then nonparametric statistical tests were used. Statistical tests, parametric or nonparametric, are listed in the figure legends for each experiment and in the corresponding Methods section. Sample variances were also similar between groups unless otherwise mentioned. The range of n within experiments varies based on when samples are taken; for example, lower n values on days 2–3 after infection may be due to animals succumbing to disease or sickness, resulting in an inability to provide faecal samples. Graph schematics were generated using GraphPad Prism v.10.4.2.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data supporting the findings of this study are available in the Article and its Supplementary Information. The dmLT adjuvant was provided by PATH under the terms of a materials transfer agreement. PE-labelled 5-OP-RU tetramer was obtained through the NIH Tetramer Core Facility under the terms of a materials transfer agreement. Source data are provided with this paper.
References
Kordus, S. L., Thomas, A. K. & Lacy, D. B. Clostridioides difficile toxins: mechanisms of action and antitoxin therapeutics. Nat. Rev. Microbiol. 20, 285–298 (2022).
C. diff (Clostridioides difficile) (CDC, 2022).
Guh, A. Y. et al. Emerging Infections Program Clostridioides difficile Infection Working Group. Trends in U.S. burden of Clostridioides difficile infection and outcomes. N. Engl. J. Med. 382, 1320–1330 (2020).
McDonald, L. C. et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin. Infect. Dis. 66, e1–e48 (2018).
Stevens, V. W. et al. Comparative effectiveness of vancomycin and metronidazole for the prevention of recurrence and death in patients with Clostridium difficile infection. JAMA Intern. Med. 177, 546–553 (2017).
Quemeneur, L. et al. Clostridium difficile toxoid vaccine candidate confers broad protection against a range of prevalent circulating strains in a nonclinical setting. Infect. Immun. 86, e00742-17 (2018).
Gribenko, A. et al. Development of a subunit vaccine for prevention of Clostridium difficile associated diseases: biophysical characterization of toxoids A and B. Biochem. Biophys. Rep. 9, 193–202 (2017).
Donald, R. G. K. et al. A novel approach to generate a recombinant toxoid vaccine against Clostridium difficile. Microbiology 159, 1254–1266 (2013).
de Bruyn, G. et al. Safety, immunogenicity, and efficacy of a Clostridioides difficile toxoid vaccine candidate: a phase 3 multicentre, observer-blind, randomised, controlled trial. Lancet Infect. Dis. 21, 252–262 (2021).
Donskey, C. J. et al. CLOVER (Clostridium difficile Vaccine Efficacy Trial) study: a phase 3, randomized trial investigating the efficacy and safety of a detoxified toxin A/B vaccine in adults 50 years and older at increased risk of Clostridioides difficile infection. Clin. Infect. Dis. 79, 1503–1511 (2024).
Alameh, M. G. et al. A multivalent mRNA-LNP vaccine protects against Clostridioides difficile infection. Science 386, 69–75 (2024).
Glover, R. C., Peritore-Galve F. C., Lacy, B. & Zackular, J. P. Immune aspects of Clostridioides difficile infection and vaccine development. Infect. Dis. Clin. North Am. 39, 801–820 (2025).
Noori Goodarzi, N. et al. Subtractive genomic approach toward introduction of novel immunogenic targets against Clostridioides difficile: thinking out of the box. Microb. Pathog. 162, 105372 (2022).
Francis, M. B., Allen, C. A., Shrestha, R. & Sorg, J. A. Bile acid recognition by the Clostridium difficile germinant receptor, CspC, is important for establishing infection. PLoS Pathog. 9, e1003356 (2013).
Clements, J. D. & Norton, E. L. The mucosal adjuvant LT(R192G/L211A) or dmLT. mSphere 3, e00215-18 (2018).
Wang, B. et al. Detecting and preventing reversion to toxicity for a formaldehyde-treated C. difficile toxin B mutant. Vaccine 33, 252–259 (2015).
Vidunas, E. et al. Production and characterization of chemically inactivated genetically engineered Clostridium difficile toxoids. J. Pharm. Sci. 105, 2032–2041 (2016).
Chumbler, N. M., Farrow, M. A., Lapierre, L. A., Franklin, J. L. & Lacy, D. B. Clostridium difficile toxins TcdA and TcdB cause colonic tissue damage by distinct mechanisms. Infect. Immun. 84, 2871–2877 (2016).
Zhang, Z. et al. Translocation domain mutations affecting cellular toxicity identify the Clostridium difficile toxin B pore. Proc. Natl Acad. Sci. USA 111, 3721–3726 (2014).
Chen, P. et al. Structural basis for CSPG4 as a receptor for TcdB and a therapeutic target in Clostridioides difficile infection. Nat. Commun. 12, 3748 (2021).
Correa, V. A., Portilho, A. I. & De Gaspari, E. Vaccines, adjuvants and key factors for mucosal immune response. Immunology 167, 124–138 (2022).
Mao, T. et al. Unadjuvanted intranasal spike vaccine elicits protective mucosal immunity against sarbecoviruses. Science 378, eabo2523 (2022).
Peritore-Galve, F. C. et al. The monoclonal antibody AZD5148 confers broad protection against TcdB-diverse Clostridioides difficile strains in mice. PLoS Pathog. 21, e1013651 (2025).
Mileto, S. J. et al. Bezlotoxumab prevents extraintestinal organ damage induced by Clostridioides difficile infection. Gut Microbes 14, 2117504 (2022).
Vietri, J. et al. Preferences for a Clostridioides difficile vaccine among adults in the United States. Vaccine. 42, 126261 (2024).
Jump, R. L. Clostridium difficile infection in older adults. Aging Health 9, 403–414 (2013).
Shin, J. H., Pawlowski, S. W. & Warren, C. A. Teaching old mice new tricks: the utility of aged mouse models of C. difficile infection to study pathogenesis and rejuvenate immune response. Gut Microbes 13, 1966255 (2021).
Kamada, N. et al. Humoral immunity in the gut selectively targets phenotypically virulent attaching-and-effacing bacteria for intraluminal elimination. Cell Host Microbe 17, 617–627 (2015).
Zeng, M. Y. et al. Gut microbiota-induced immunoglobulin G controls systemic infection by symbiotic bacteria and pathogens. Immunity 44, 647–658 (2016).
Rath, T., Baker, K., Pyzik, M. & Blumberg, R. S. Regulation of immune responses by the neonatal Fc receptor and its therapeutic implications. Front. Immunol. 5, 664 (2014).
Fadlallah, J. et al. Synergistic convergence of microbiota-specific systemic IgG and secretory IgA. J. Allergy Clin. Immunol. 143, 1575–1585 (2019).
Nechansky, A., Grunt, S., Roitt, I. M. & Kircheis, R. Comparison of the calibration standards of three commercially available multiplex kits for human cytokine measurement to WHO standards reveals striking differences. Biomark. Insights. 3, 227 (2008).
Tamarozzi, F., Wright, H. L., Thomas, H. B., Edwards, S. W. & Taylor, M. J. A lack of confirmation with alternative assays questions the validity of IL-17A expression in human neutrophils using immunohistochemistry. Immunol. Lett. 162, 194–198 (2014).
Pappu, R., Ramirez-Carrozzi, V. & Sambandam, A. The interleukin-17 cytokine family: critical players in host defense and inflammatory diseases. Immunology. 134, 8–16 (2011).
Castro-Córdova, P. et al. Entry of spores into intestinal epithelial cells contributes to recurrence of Clostridioides difficile infection. Nat. Commun. 12, 1140 (2021).
Castro-Cordova, P. et al. Clostridioides difficile major toxins remodel the intestinal epithelia, affecting spore adherence/internalization into intestinal tissue and their association with gut vitronectin. Preprint at bioRxiv https://doi.org/10.1101/2025.01.29.635439 (2025).
Miles-Jay, A. et al. Longitudinal genomic surveillance of carriage and transmission of Clostridioides difficile in an intensive care unit. Nat. Med. 29, 2526–2534 (2023).
Figueroa, I. et al. Relapse versus reinfection: recurrent Clostridium difficile infection following treatment with fidaxomicin or vancomycin. Clin. Infect. Dis. 55, S104–109 (2012).
Kamboj, M. et al. Relapse versus reinfection: surveillance of Clostridium difficile infection. Clin. Infect. Dis. 53, 1003–1006 (2011).
Masopust, D. et al. Dynamic T cell migration program provides resident memory within intestinal epithelium. J. Exp. Med. 207, 553–564 (2010).
Rohlfing, A. E. et al. The CspC pseudoprotease regulates germination of Clostridioides difficile spores in response to multiple environmental signals. PLoS Genet. 15, e1008224 (2019).
Markham, N. O. et al. Murine intrarectal instillation of purified recombinant Clostridioides difficile toxins enables mechanistic studies of pathogenesis. Infect. Immun. 89, e00543-20 (2021).
Mizrahi, A. et al. A mouse model of mild Clostridioides difficile infection for the characterization of natural immune responses. Microorganisms 12, 1933 (2024).
Johnston, P. F., Gerding, D. N. & Knight, K. L. Protection from Clostridium difficile infection in CD4 T cell- and polymeric immunoglobulin receptor-deficient mice. Infect. Immun. 82, 522–531 (2014).
Kuehne, S. A. & Minton, N. P. ClosTron-mediated engineering of Clostridium. Bioengineered 3, 247–254 (2012).
Sun, X. et al. Mouse relapse model of Clostridium difficile infection. Infect. Immun. 79, 2856–2864 (2011).
Warren, C. A. et al. Vancomycin treatment’s association with delayed intestinal tissue injury, clostridial overgrowth, and recurrence of Clostridium difficile infection in mice. Antimicrob. Agents Chemother. 57, 689–696 (2013).
Peritore-Galve, F. C. et al. Glucosyltransferase-dependent and independent effects of Clostridioides difficile toxins during infection. PLoS Pathog. 18, e1010323 (2022).
Wilson, K. H., Kennedy, M. J. & Fekety, F. R. Use of sodium taurocholate to enhance spore recovery on a medium selective for Clostridium difficile. J. Clin. Microbiol. 15, 443–446 (1982).
Koenigsknecht, M. J. et al. Dynamics and establishment of Clostridium difficile infection in the murine gastrointestinal tract. Infect. Immun. 83, 934–941 (2015).
Martinson, J. N. et al. Evaluation of portability and cost of a fluorescent PCR ribotyping protocol for Clostridium difficile epidemiology. J. Clin. Microbiol. 53, 1192–1197 (2015).
Walk, S. T. et al. Clostridium difficile ribotype does not predict severe infection. Clin. Infect. Dis. 55, 1661–1668 (2012).
Mutters, R. et al. Quantitative detection of Clostridium difficile in hospital environmental samples by real-time polymerase chain reaction. J. Hosp. Infect. 71, 43–48 (2009).
Childress, K. O., Cencer, C. S., Tyska, M. J. & Lacy, D. B. Nectin-3 and shed forms of CSPG4 can serve as epithelial cell receptors for Clostridioides difficile TcdB. mBio 14, e0185723 (2023).
Theriot, C. M. et al. Cefoperazone-treated mice as an experimental platform to assess differential virulence of Clostridium difficile strains. Gut Microbes 2, 326–334 (2011).
Manion, J. et al. C. difficile intoxicates neurons and pericytes to drive neurogenic inflammation. Nature 622, 611–618 (2023).
Purcell, E. B., McKee, R. W., McBride, S. M., Waters, C. M. & Tamayo, R. Cyclic diguanylate inversely regulates motility and aggregation in Clostridium difficile. J. Bacteriol. 194, 3307–3316 (2012).
Bilate, A. M. et al. Tissue-specific emergence of regulatory and intraepithelial T cells from a clonal T cell precursor. Sci. Immunol. 1, eaaf7471 (2016).
Reis, B. S., Rogoz, A., Costa-Pinto, F. A., Taniuchi, I. & Mucida, D. Mutual expression of the transcription factors Runx3 and ThPOK regulates intestinal CD4+ T cell immunity. Nat. Immunol. 14, 271–280 (2013).
Sauter, M. et al. Protocol to isolate and analyze mouse bone marrow derived dendritic cells (BMDC). STAR Protoc. 3, 101664 (2022).
Wölfl, M. & Greenberg, P. Antigen-specific activation and cytokine-facilitated expansion of naive, human CD8+ T cells. Nat. Protoc. 9, 950–966 (2014).
Acknowledgements
We thank J. White, M. Estrada and A. Bzami with the Center for Vaccine Innovation and Access at PATH for providing the dmLT adjuvant; A. Kruse for help with protein validation; and A. Louis Bourgeois, I. Georgiev and E. Skaar for their feedback on this study. dmLT production at PATH is funded by a grant from the Bill & Melinda Gates Foundation (INV-008763). The views expressed here are solely those of the authors and do not necessarily reflect the views of the Bill & Melinda Gates Foundation. The Vanderbilt Flow Cytometry Shared Resource is supported by the Vanderbilt Ingram Cancer Center (P30 CA068485) and the Vanderbilt Digestive Disease Research Center (P30 DK058404). Paraffin embedding of tissue was performed by the Vanderbilt Translational Pathology Shared Resource, which is supported by NCI/NIH Cancer Center Support Grant (P30CA068485) and the Shared Instrumentation Grants S10 OD023475-01A1 (Leica Bond RX), S10 OD016355 (Tissue MicroArray (TMA)) and IS1BX003154 (LCM). Funding was provided by National Institutes of Health grant U19 AI174999 (D.B.L., B.W.S., C.B.C. and M.R.N.).
Author information
Authors and Affiliations
Contributions
A.K.T., F.C.P.-G. and D.B.L. conceptualized this story. A.K.T., B.B.C.L., J.C., R.S., R.C.R., H.K.K., B.W.S. and D.B.L. produced reagents for this work. A.K.T. performed all experiments with assistance from F.C.P.-G., A.G.E. and E.J.B.; A.K.T. and S.M.Y. curated data with guidance from D.O.-V. Formal data analysis was performed by A.K.T. Blinded analysis and scoring of histopathological data were performed by M.K.W. and K.N.G.-C.; A.K.T. visualized all data and created figures. A.K.T. and J.C. validated data. D.B.L. supervised this work. The original draft of this manuscript was written by A.K.T. and reviewed and edited by A.K.T., F.C.P.-G. and D.B.L. with input from all of the authors. Funding was acquired by D.B.L., B.W.S., C.B.C. and M.R.N.
Corresponding author
Ethics declarations
Competing interests
A.K.T. and D.B.L. are listed as inventors on a patent application filed by Vanderbilt University Medical Center containing data published in this manuscript and covering multiple C. difficile vaccines and immunogens (US patent application 18/671,007). D.B.L. has research collaborations with AstraZeneca and Pfizer that are unrelated to this work and serves as a consultant to GSK. B.W.S. is a co-founder and owner at Turkey Creek Biotechnology, which was not involved in this work. C.B.C. receives grant support from Moderna, Pfizer, and Vedanta; serves as a consultant to GSK, Merck, CommenseBio, TDCowen, Guidepoint Global, AstraZeneca and Delbiopharm; and serves on the data and safety monitoring boards for studies sponsored by GSK and Bavarian Nordic—each unrelated to this work. The other authors declare no competing interests.
Peer review
Peer review information
Nature thanks Vincent Young and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 RI of CspC, C40 Peptidase 2, and FlgGEK reduce C. difficile colonization burden.
a, Experimental schema. The diagram was created using BioRender. b,c, Survival of WT C. difficile R20291 infection. d,e, Enumeration of C. difficile R20291 ∆A∆B bacteria in faeces. P value relative to dmLT control at the same time point. Individual lines correspond to individual mice. Limit of detection shown by dotted line, 500 CFU/g faeces. f–h, Sera IgG (f), faecal IgA (g), and faecal IgG (h) responses against antigens at days 28 and 42. Mean +/− SEM. i, Pearson’s R correlation coefficient and j, corresponding p-value heat maps comparing colonization burden with humoral titres in IP or RI mice that were either colonized or uncolonized 10 days post-infection with C. difficile. Negative Pearson’s R values correspond to colonization burden decrease. Statistical significance was calculated by means of [(b-c)] log-rank Mantel-Cox test, [(d-h), (d-e) each day analysed individually] one-way ANOVA with Tukey’s correction; *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001. 1b-e: n = 10 per group, decreases in n due to animal mortality during infection; 1f-j: n = 5-15 per group, dependent on ability to collect sample. Individual data points are represented and are pooled from two independent experiments in 1b-e. CFU, colony forming units; d.p.i., days post-infection; IP, intraperitoneal injection; RI, rectal instillation; C40 Pep 2, C40 peptidase 2; PD, polysaccharide deacetylase.
Extended Data Fig. 2 Rectal instillation and intraperitoneal injection of TcdAGTX with either > 10 µg or > 1 µg of dmLT, respectively, increases anti-TcdA serum IgG and faecal IgA.
a, Experimental schema for intraperitoneal injection. The diagram was created using BioRender. b,c, Sera IgG (b) and faecal IgA (c) titres against TcdA and dmLT in intraperitoneally-injected mice. d, Experimental schema for rectal instillation. The diagram was created using BioRender. e,f, Sera IgG (e) and faecal IgA (f) titres against TcdA and dmLT in rectally-instilled mice. All data shown as mean +/− SEM. n = 3-5 per group. Statistical significance was calculated by means of [(b-c), (e,f)] two-way ANOVA with Tukey’s correction; *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001.
Extended Data Fig. 3 Mice vaccinated with toxins and NTAs by RI have less epithelial damage to colons and ceca.
a,b, Histopathology scores of colons (a) and caeca (b). c, Representative haematoxylin & eosin (H&E) images of colons and caeca from each group of vaccinated mice at 3 days post infection with C. difficile R20291. Scale bar, 40 μm at 10x magnification. [3a-b] shown as mean +/− SEM. n = 5 per group. Statistical significance was calculated by means of [(a-b)] one-way ANOVA with Tukey’s correction; *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001. n = 5 per group. Total histology score is the summation of oedema, inflammation, and epithelial injury scores.
Extended Data Fig. 4 RI-vaccination with the toxin and NTA formula eliminates C. difficile from tissue.
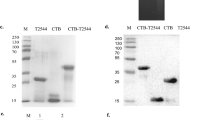
a–d, Enumeration of total C. difficile R20291 bacteria (vegetative cells and spores) (a,c) and spores (b,d) from macerated colons and caeca of vaccinated mice fifteen days post-R20291 infection. Limit of detection (dotted line) is 500 CFU/g faeces. e, PCR of C. difficile 16S gene from bulk DNA extracted from macerated colons and caeca from a–e, with each lane representing one mouse. Desired amplicon is 175 bp (expected size indicated by red arrow; solid line indicates bands are present whereas dotted shows lack of bands). Distinct bands can be noted for certain mice; smeared bands are background DNA from extracted tissues. f, Normalized reporter values from C. difficile 16S qPCR of bulk DNA extracted from macerated colons and caeca from a–d. qPCR was performed in triplicate per sample. Data reported as the mean of all samples’ experimental averages, normalized from baseline. Standard threshold (dotted line) is 30 cycles. g, Cycle threshold from C. difficile 16S qPCR of bulk DNA extracted from macerated colons and caeca from a–d. qPCR was performed in triplicate per sample. Mean +/− SEM. Standard threshold (dotted line) is 30 cycles. h, Total colonization burden (vegetative and spore counts combined; closed circle) versus spore counts (open circle) in faeces of naive, unvaccinated mice infected with WT C. difficile R20291. Limit of detection (dotted line) is 500 CFU/g faeces. 4a-g: n = 2-10 per group, dependent on survival at 15 days post-infection; 4h: n = 3 per group. CFU, colonization forming units; RI, rectal instillation; IP, intraperitoneal injection; L, ladder; bp, base-pairs; ∆Rn, normalized reporter signal above baseline; gDNA, C. difficile R20291 genomic DNA. For source gel data, see Supplementary Information.
Extended Data Fig. 5 Flow cytometric results of vaccinated mesenteric lymph nodes.
a–c, Percent parent of gated mesenteric lymph node total (a), memory (b, B220+, CD27+), and plasma (c, B220+, CD138+) B cells with affinity for each vaccine antigen. All data shown as mean +/− SEM. n = 3–10 per group, dependent on infection survival. Roughly 150,000 events were recorded. Statistical significance was calculated by means of [(a-c)] one-way ANOVA with Tukey’s correction; *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001. Individual data points are represented and are pooled from two independent experiments. Bmem, memory B cells; C40 Pep 2, C40 peptidase 2.
Extended Data Fig. 6 Passive transfer of anti-C40 peptidase 2 and -FlgGEK faecal IgG by RI reduces vegetative bacterial burden.
a, Passive transfer schematic. The diagram was created using BioRender. Recipient mice were RI-vaccinated with inactivated toxins, CspC, and dmLT before undergoing challenge. On days 1, 4, and 7 post-infection, recipient mice were passively transferred faecal IgG by either IP or RI, which was isolated by donor mice that had been RI-vaccinated with either dmLT alone or C40 peptidase 2, FlgGEK, and dmLT. b, C. difficile R20291 motility with or without faecal IgG pre-incubation. c, Survival of WT C. difficile R20291 infection. d, Weight loss. e, Stool scores. j–m, Enumeration of total C. difficile R20291 bacteria (vegetative cells and spores) (f to g, j to k) and spores (h to i, l to m) in faeces. P value relative to control at the same time point. Individual lines correspond to individual mice. Individual lines correspond to individual mice. Limit of detection shown by dotted line, 500 CFU/g faeces. Mean +/− SEM shown for [b-e]. Statistical significance was calculated by means of [c] log-rank Mantel-Cox test, and [(b),(d-e), (f-m, each day analysed individually)] one-way ANOVA with Tukey’s correction; *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001. 6b: n = 21 per group; 6c-m: n = 10 per group, decreases in n due to animal mortality during infection. IP, intraperitoneal injection; RI, rectal instillation; CFU, colony forming units; C40 pep 2, C40 peptidase 2; Veg. Ant., vegetative antigens.
Extended Data Fig. 7 CspC-primed dendritic cells activate Th17-skewed cytokine responses from CD4+ and CD8+ tissue-resident memory T cells from RI-vaccinated mice during co-culture.
a–i, Bone marrow derived dendritic cells were primed individually with TcdA, TcdB, CspC, C40 peptidase 2, or FlgGEK in vitro and incubated for three days with T cells from mice vaccinated by RI or IP with dmLT alone or the toxins, NTAs, and dmLT. Cytokines in the supernatants were quantified by liquid bead array. All data shown as mean +/− SEM. n = 3 per group. Statistical significance was calculated by means of [(a-i)] one-way ANOVA with Tukey’s correction; *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001. n = 3 per group. C40 Pep 2, C40 peptidase 2.
Extended Data Fig. 8 Immunization of inactivated toxins and CspC is sufficient to protect against death but does not fully clear C. difficile.
a, Survival of WT C. difficile R20291 infection. b,c, Weight loss. Mean +/− SEM. d–g, Enumeration of total C. difficile R20291 bacteria (vegetative cells and spores) (d,e) and spores (f,g) in faeces. P value relative to RI dmLT-only control at the same time point (shown in Fig. 2). Individual lines correspond to individual mice. Limit of detection shown by dotted line, 500 CFU/g faeces. 8b-g: n = 10 per group, decreases in n due to animal mortality during infection. Weight loss and survival data for other groups taken from Fig. 2 (n = 10-15 per group). Statistical significance was calculated by means of [(a)] log-rank Mantel-Cox test, and [(b-g), (d-g, each day analysed individually)] one-way ANOVA with Tukey’s correction; *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001. RI, rectal instillation; d.p.i., days post-infection; CFU, colony forming units; NTAs, non-toxin antigens.
Extended Data Fig. 9 Toxin and NTA-vaccinated mice exhibit significantly increased sera and faecal humoral titres against antigens 60- and 120-days post-boost.
a–c, Sera IgG (a), faecal IgA (b), and faecal IgG (c) responses. n = 10-15 per group, based on ability to obtain sample. All data shown as mean +/− SEM. Statistical significance was calculated by means of [(a-c)] two-way ANOVA with Tukey’s correction; *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001.
Extended Data Fig. 10 Flow cytometric results of colonic intraepithelial and lamina propria lymphocytes 60- and 200-days post-immunization.
a–p, Enumeration and percent parent of gated intraepithelial lymphocyte (a–h) and lamina propria lymphocyte (i–p) populations in the colon taken at day 3 post-infection. All data shown as mean +/− SEM. n = 3-5 per group, depending on survival at time of harvest. Statistical significance was calculated by means of [(a-p)] one-way ANOVA with Tukey’s correction; *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001. IEL, intraepithelial lymphocytes; LPL, lamina propria lymphocytes; TRM, tissue resident-memory (CD103 + , CD69 + ); MAIT, mucosal-associated invariant T cells.
Supplementary information
Supplementary Information
Further information: antigen quality control for FlgGEK and TcdB2 mutants; raw gel images corresponding to Extended Data Fig. 4; and flow cytometry gating schemes.
Supplementary Table 1
Expression and purification conditions of the 16 putative C. difficile non-toxin antigens. /, non-applicable; ””, same conditions as above; Y, yes, able to express; N, no, unable to express
Supplementary Table 2
Plasmids and primers used in this study.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thomas, A.K., Peritore-Galve, F.C., Ehni, A.G. et al. Mucosal vaccination clears Clostridioides difficile colonization. Nature (2026). https://doi.org/10.1038/s41586-026-10138-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41586-026-10138-x