Abstract
Desmosomes are transmembrane protein complexes that contribute to cell–cell adhesion in epithelia and other tissues. Here, we report the discovery of frequent genetic alterations in the desmosome in human cancers, with the strongest signal seen in cutaneous melanoma, where desmosomes are mutated in more than 70% of cases. In primary but not metastatic melanoma biopsies, the burden of coding mutations in desmosome genes is associated with a strong reduction in desmosome gene expression. Analysis by spatial transcriptomics and protein immunofluorescence suggests that these decreases in expression occur in keratinocytes in the microenvironment rather than in primary melanoma cells. In further support of a microenvironmental origin, we find that desmosome gene knockdown in keratinocytes yields markedly increased proliferation of adjacent melanoma cells in keratinocyte and melanoma cocultures. Similar increases in melanoma proliferation are observed in media preconditioned with desmosome-deficient keratinocytes. Thus, gradual accumulation of desmosome mutations in neighboring cells may prime melanoma cells for neoplastic transformation.
Similar content being viewed by others
Main
Transformation of melanocytes to skin cutaneous melanoma (SKCM) includes interaction with numerous cells in the tumor microenvironment, which can have important roles in progression1,2,3. One important component of this microenvironment is the keratinocyte, which forms the major cellular component of the epidermis, that is, the top layer of the skin. Nascent melanoma cells detach from neighboring keratinocytes, regulating melanocyte homeostasis through paracrine signaling and cell–cell adhesion4,5,6, and impacting tumor proliferation and invasion.
A primary adhesion structure that facilitates the physical interaction between cells in the epithelium is the desmosome, an intercellular junction conserved across vertebrates7. Desmosomes have a transmembrane core consisting of cadherin proteins (desmogleins and desmocollins), which is linked via plakoglobin and plakophilin proteins to keratin filaments in the cytoplasm8 (Fig. 1a). Alterations to desmosome components can impair tissue strength and has both positive and negative effects on cell proliferation and differentiation9. For example, loss of desmoglein-1 (DSG1) is associated with predisposition to skin inflammation10, and increases in expression of desmosome cadherins can upregulate Wnt/β-catenin signaling leading to cell proliferation11. In the context of cancer, loss of DSG1 leads to worse prognosis in head and neck squamous cell carcinomas12; loss of desmocollin-3 (DSC3) is associated with an increase in KRAS-induced skin tumors13; and upregulation of plakophilin-3 (PKP3) has been associated with poor patient survival and advanced disease stage in non-small-cell lung carcinomas11. In contrast, upregulation of plakoglobin (JUP) has been found to suppress proliferation of bladder tumor cells in vitro14,15. The tumor suppressive functions of the desmosome have also been found in pancreatic neuroendocrine cancer16, skin cancer mouse models17 and human lung cancer18. These findings underscore that individual desmosome components have nonredundant functions and impact, not only in cell adhesion and signaling but in tumorigenesis.
a, Illustration of the desmosome complex, which consists of proteins of three different families: cadherins (DSG and DSC); armadillo proteins (PKP and JUP); and the plakin protein DSP. b, Desmosome mutation frequency for each of 32 tumor types, with mutations aggregated across the 15 desmosome genes. Inset: mutation frequency of each desmosome gene in SKCM. ACC, adrenocortical carcinoma (n = 92); BLCA, bladder urothelial carcinoma (n = 413); BRCA, breast invasive carcinoma (n = 1108); CESC, cervical squamous cell carcinoma and endocervical adenocarcinoma (n = 310); CHOL, cholangiocarcinoma (n = 51); COADREAD, colorectal adenocarcinoma (n = 640); DLBC, lymphoid neoplasm diffuse large B cell lymphoma (n = 48); ESCA, esophageal carcinoma (n = 186); GBM, glioblastoma multiforme (n = 619); HNSC, head and neck squamous cell carcinoma (n = 530); KICH, kidney chromophobe (n = 113); KIRC, kidney renal clear cell carcinoma (n = 538); KIRP, kidney renal papillary cell carcinoma (n = 293); LAML, acute myeloid leukemia (n = 200); LGG, brain lower grade glioma (n = 530); LIHC, liver hepatocellular carcinoma (n = 442); LUAD, lung adenocarcinoma (n = 586); LUSC, lung squamous cell carcinoma (n = 511); MESO, mesothelioma (n = 87); OV, ovarian serous cystadenocarcinoma (n = 617); PAAD, pancreatic adenocarcinoma (n = 186); PCPG, pheochromocytoma and paraganglioma (n = 184); PRAD, prostate adenocarcinoma (n = 501); SARC, sarcoma (n = 265); STAD, stomach adenocarcinoma (n = 478); TGCT, testicular germ cell tumor (n = 156); THCA, thyroid carcinoma (n = 516); THYM, thymoma (n = 124); UCEC, uterine corpus endometrial carcinoma (n = 549); UCS, uterine carcinosarcoma (n = 57); UVM, uveal melanoma (n = 80). c, Excess number of tumors with a mutated desmosome gene (colored dots) above the number expected by chance (Online Methods). The horizontal black lines indicate the median value across desmosomal genes. Ten frequently mutated tumor types from b are shown. Significance was determined using bootstrap analysis (q < 10−10, Benjamini–Hochberg-corrected for multiple testing; Methods). The number of samples (n) for each cancer type is described in b. d, Ranked SKCM mutation frequencies of each human gene. Desmosome genes are shown in red; the known SKCM driver genes22 are shown in blue. The PERP gene is not shown in the figure; it is located at the 63.5 percentile.
While these studies focused on desmosome expression, a separate question is whether the desmosome is affected by genetic mutations. Recently, we performed an integrative analysis of protein biophysical interactions and tumor mutations19, resulting in a map of 395 protein complexes under mutational selection in one or more cancer types. One of these complexes pointed to the desmosome as a potential focal point for the accumulation of mutations in melanoma; however, at the time we did not validate or further explore this observation (Extended Data Fig. 1). In this study, we find that desmosome mutations are highly recurrent in melanoma, with over 70% of tumors harboring such alterations. These mutations lead to a reduction in desmosome gene expression in the tumor microenvironment, ultimately promoting melanoma proliferation through paracrine signaling.
Results
Desmosome mutations are highly prevalent in melanoma
To investigate the importance of mutations to the desmosome complex, we began with a comprehensive survey of somatic nonsynonymous mutations affecting any of the 15 desmosome genes in aggregate, across 32 tumor tissue types profiled by The Cancer Genome Atlas (TCGA) (Supplementary Table 1). By far the highest mutation recurrence was observed for SKCM, in which 71% of tumors harbored a desmosome coding mutation. In contrast, desmosome mutation rates were substantially lower in all other tissue types (<40%; Fig. 1b).
As melanomas are one of the tumor types with a generally high genome-wide burden of mutations20, we sought to assess the significance of desmosome mutation rates in several ways. First, we computed the excess mutational load on the 15 desmosome genes using MutSigCV20, which considers the genome-wide mutation burden, the type of mutational signature(s)21 and gene-specific factors such as mRNA expression level and time of replication during the cell cycle. As a group, desmosome genes were mutated significantly more often than expected, again with the strongest signal in melanoma (Fig. 1c). Second, we repeated this analysis in an independent melanoma cohort22, again finding that desmosome genes are highly and significantly mutated (Extended Data Fig. 2a). These patterns did not depend on the particular mutational model for the expected mutational frequency (P < 10−20 using MutSigCV20 and P < 10−9 using OncodriveFML23). Third, ranking human genes by decreasing mutation frequency in melanoma, we found that nearly all desmosome genes were among the top quartile, on a par with the distribution of well-established melanoma cancer genes (Fig. 1d), with the single exception of PERP, which nonetheless was highly mutated in a second independent melanoma cohort we examined (Extended Data Fig. 2a). Notably, none of the desmosome genes had been previously reported to be significantly mutated in melanoma when analyzed individually, perhaps because the mutational signal is spread across the desmosome complex.
Desmosome expression is localized to keratinocytes
The finding that the desmosome is frequently mutated in melanoma was puzzling because in normal epidermis, desmosome function has been typically associated with keratinocytes rather than melanocytes24. However, this is a point of some confusion as melanocytes cultured in the absence of other cell types have been shown to express the desmosomal cadherin desmoglein-2 (DSG2)25 and leading to increased migration26. To understand the patterns and cell types associated with desmosome expression in melanoma tumors more fully, we performed single-cell RNA sequencing (scRNA-seq) using the inDrop system27 on two human primary melanoma tumor biopsies encapsulating approximately 1,000 cells from each tumor (Fig. 2a). Single-cell transcriptomes were displayed using uniform manifold approximation and projection28 (UMAP), resulting in clusters that matched pre-identified distinct cell types (Online Methods). Analysis against a panel of established expression markers for different human cell types distinguished clear populations of immune, endothelial, muscle, keratinocyte and melanocyte tumor types (Fig. 2b). Examining the expression profile of desmosome genes across these different types, we found desmosomes to be predominantly expressed in keratinocytes (Fig. 2c,d). To extend this analysis to animal models, we analyzed primary transgenic zebrafish tumors29, where we also found that desmosome expression is limited to keratinocytes (Extended Data Fig. 2c) as we had seen in the human melanoma samples. These results were also seen in normal (non-melanoma) skin cells, as indicated by the analysis of a large existing scRNA-seq dataset from normal skin collected by the Human Cell Atlas (HCA) (https://developmental.cellatlas.io/diseased-skin), again showing that desmosomal gene expression is overwhelmingly restricted to keratinocyte cell populations (Extended Data Fig. 2b–f).
a, Tumor biopsies from two patients, one male and one female, processed using scRNA-seq. b, UMAP analysis of 1,109 individual cells from melanoma 1, with the color indicating the inferred cell type. ‘Cancer’ denotes melanoma cells. The two clusters of keratinocyte cells (red) reflect basal versus non-basal types. c, Same UMAP as in b, with the color indicating the expression of desmosome genes as median transcripts per million (TPM) (Online Methods). d, Correspondence of desmosome gene expression to cell types. The color indicates the mean expression per cell (log2). The dot size indicates the fraction of cells in the cell type expressing each desmosome gene.
Desmosome mutations correlate with reduced expression
To investigate the relationship between desmosome expression and mutation, we next examined multi-omics data collected from 472 melanoma tumors by the TCGA30 (104 primary and 368 metastatic; see Extended Data Fig. 3a–g for details about the SKCM cohort analyzed). Analysis of these data indicated that the expression of the desmosome system was significantly higher in primary than metastatic tumors, which is consistent with an elevated keratinocyte presence in primary versus metastatic melanoma (Fig. 3a). Examining the matched somatic mutation data, we found that primary tumors with desmosome mutations had significantly reduced expression of the desmosome complex compared to tumors without such mutations (Fig. 3b). Moreover, in primary melanoma only, there was a strong inverse relationship between the number of mutated desmosome genes in a tumor and overall desmosome expression (Fig. 3c). The most pronounced negative correlation between desmosome expression and desmosome mutations occurred in the early stages of melanoma, specifically in stage I and II tumors (Extended Data Fig. 3h). Further analysis of this TCGA cohort found that desmosome mutation in primary melanoma is associated with significantly higher expression of genes related to cell proliferation (Fig. 3d). To determine if these particular mutations are under evolutionary selection pressure, we calculated the ratio of nonsynonymous (dN) to synonymous (dS) mutations in the desmosome genes. We found that the dN/dS ratio was approximately 2.5 in primary melanoma tumors, indicating strong positive selection, and that this value was significantly larger than for metastatic melanoma tumors (Fig. 3e). Finally, desmosome mutation was associated with a marginal increase in patient overall survival in this TCGA cohort (P = 0.03, false discovery rate = 0.29; Supplementary Table 1). Collectively, these results suggested that accumulation of mutations in the desmosome disrupt its expression in a graded manner, and that these events are selected in primary melanoma.
a, Violin plot of average desmosome gene expression in primary (left, n = 104) or metastatic (right, n = 362) melanoma tumors in the TCGA. Significance was determined using a two-sided, two-sample t-test (****P = 4.9 × 10−27). b, Same as in a, distinguishing wild-type (WT, gray) and desmosome-mutated (pale gray, n = 62 for primary, n = 277 for metastatic) tumors in the TCGA cohort. Significance was determined using a two-sided, two-sample t-test (****P < 10−4; *P = 0.005; NS, not significant). c, Average desmosome gene expression (TPM) as a function of the number of desmosome genes with coding mutations, shown separately for primary (light blue, n = 62) versus metastatic (dark blue, n = 277) melanoma tumor populations. The regression lines for each of these populations are shown: primary melanoma, slope = −0.66; metastatic melanoma, slope = 0.03; the significant difference with P = 0.004 was determined using a two-sided t-test for the Pearson correlation coefficient. The error bars represent the s.d. and the shaded areas capture the 95% confidence intervals. d, Degree of proliferative gene expression (defined previously in ref. 50) in desmosome WT (gray, n = 42) or desmosome mutant (pale gray, n = 62) primary melanoma tumors (points) in the TCGA cohort. Significance was determined using a two-sided, two-sample t-test (*P = 0.005). The boxes in the plot contain the 25th to 75th percentiles, the middle line denotes the 50th percentile and the whiskers mark the 5th and 95th percentiles. e, Ratio of fixed nonsynonymous (dN) to synonymous (dS) mutations (dN/dS) in primary (light blue, n = 12 genes across 104 patients) or metastatic (dark blue, n = 12 genes across 362 patients) melanoma tumors in the TCGA cohort. The distributions of dN/dS across the population of tumors are shown in box plots, using a similar display convention as in d. Significance was determined using a two-sided, two-sample t-test (*P = 0.005).
Keratinocyte-specific reduction in desmosome expression
We reasoned that the distinction between primary and metastatic melanoma could be due to at least two explanations. First was the very different microenvironments of these two tumor locales. Primary melanoma tumor biopsies tend to contain large numbers of surrounding keratinocytes because of their growth within and below the epidermis, in contrast to metastatic tumors that, apart from cutaneous metastases, lack the epidermal component and are typically purer31. By this reasoning, the decrease in desmosome expression could be due to loss of desmosomal expression in keratinocytes. A second explanation was related to cancer-specific transcriptional states of melanoma cells. As melanoma tumors can assume distinct transcriptional programs29,32, the effect on desmosome expression could be caused by a change in transcriptional state of melanoma cells between primary and metastatic cancer.
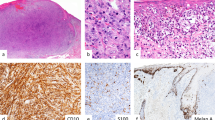
To distinguish between these two possibilities, we performed spatial transcriptomics and protein immunofluorescence (IF) analysis of primary tumor biopsies drawn from a cohort of 18 patients with melanoma (Fig. 4a). All samples were characterized by bulk whole-exome sequencing (WES), identifying nine tumors with desmosome mutations and nine without (Supplementary Table 2). Eight of these samples were analyzed using NanoString GeoMx spatial transcriptomics profiling33, resulting in a deep mRNA expression profile for four to eight regions of interest (ROIs) per tumor. In each case, ROIs were selected to represent melanoma cells, keratinocytes or a combination of both cell types (Fig. 4b). Analysis of these data showed that the ROI expression profiles were well clustered according to cell type and desmosome expression levels (Extended Data Fig. 4a–c). Desmosome expression was very high in keratinocyte-enriched ROIs but barely detectable in melanocyte-enriched ROIs (Fig. 4c), corroborating our earlier findings with scRNA-seq (Fig. 2b,c and Extended Data Fig. 2). Moreover, desmosome expression in keratinocyte ROIs was significantly lower in tumors with desmosome mutations than in tumors lacking such mutations (Fig. 4d; P < 0.05). In contrast, we did not see substantial change in desmosome expression in melanocyte ROIs when comparing mutated versus unmutated samples (Fig. 4d). Finally, we found that tumors with desmosome mutations had significantly increased expression of many genes used as standard markers of cell proliferation, but only in ROIs enriched for melanocytes (Extended Data Fig. 4d and Online Methods).
a, A total of 18 primary melanoma tumors underwent WES. Top, eight tumors were subjected to spatial transcriptomic analysis using NanoString GeoMx, covering a combined total of 48 ROIs. Bottom, the remaining ten tumors were subjected to IF analysis, in which the expression levels of the DSP protein were scored using quantitative fluorescence. b, Tissue cross-section with example ROIs shown. Each ROI is indicated by a circle boundary marked using a lowercase Roman numeral. ROIs are enriched for keratinocytes (i), mixed melanocytes and keratinocytes (ii) or melanocytes (iii). Fluorescent markers have been used to label nuclei (blue), immune cells (red), cancer cells (yellow) or keratinocytes (green). Gene expression profiling was performed once per slide with multiple ROIs. c, Average mRNA expression levels of desmosome genes in each ROI, stratified according to keratinocyte (n = 15) versus melanoma (n = 21) and mixed (n = 12) ROIs. In the box plots, the lower and upper box boundaries delineate the 25th and 75th percentiles, the middle line denotes the 50th percentile and the whiskers mark the 5th and 95th percentiles. Significance was determined using a two-sided, two-sample t-test (**P = 0.001, ****P < 10−13). d, Average mRNA expression levels of desmosome genes in each ROI, stratified according to keratinocyte (n = 15) versus melanoma (n = 21) and further subdivided based on whether ROIs are from tumors with WT (dark gray, n = 24) or mutant desmosomes (light gray, n = 12). In each category, the set of ROI values is summarized using a box plot, according to the convention used in c. Significance was determined using a two-sided, two-sample t-test (*P = 0.033). e, DSP IF of tumor MKD15 (right, desmosome WT) and MKD12 (left, mutated desmosome). Red indicates DSP expression, cyan represents JUP expression serving as a membrane mask and yellow represents SOX10 expression marking melanocytes. Each staining was performed once for ten individual tumor samples. f, Total DSP protein expression levels across ten human melanoma tumor-adjacent epidermis primary tumors. Samples are split according to desmosome mutational status (WT, mutated). Significance was determined using a two-sided Wilcoxon rank-sum test (*P = 0.042). g, Same as in f but for membrane-only DSP protein expression. Significance was determined using a two-sided Wilcoxon rank-sum test (*P = 0.018).
The remaining ten samples were used to perform IF staining with an antibody against desmoplakin (DSP), the central desmosomal protein that provides links to keratin intermediate filaments in the cytosol (Fig. 4a,e). DSP is essential to desmosome structural integrity34; we also found that it had the single largest mutation burden in patients with melanoma (Fig. 1c,d). In addition to DSP, the samples were co-stained with antibodies against SOX10 (a melanocyte nucleocytoplasmic marker) and JUP (a keratinocyte membrane marker). The analysis revealed that samples harboring desmosome mutations exhibited DSP expression levels that were colocalized with JUP and significantly lower than DSP levels in samples without such mutations (Fig. 4f). This difference was significant not only for total DSP intensity but also when quantifying DSP intensity at the cell membrane (Fig. 4g), as most of the DSP was specific to that location (Fig. 4e). Thus, both the earlier spatial profiling and the subsequent IF data supported a model in which desmosome mutation leads to a reduction in desmosome expression specifically in keratinocytes.
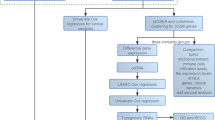
Keratinocyte desmosome loss promotes melanoma cell growth
We next wanted to functionally test whether loss of desmosome expression in keratinocytes can influence the behavior of neighboring melanoma cells. For this purpose, we used a keratinocyte cell line (HaCaT human immortalized keratinocytes), which we demonstrated reliably expresses and localizes the desmosome at cell–cell junctions, with the expected connections to cytokeratins (Fig. 5a). We then subjected this cell line to stable knockdown of DSP gene expression using short hairpin RNA (shRNA), which we confirmed causes marked loss of DSP protein along with the loss of other desmosome components such as DSG2 (Fig. 5b and Extended Data Fig. 5a). Next, we examined the effects of DSP knockdown on cell proliferation in a series of complementary cell culture experiments, including keratinocyte and melanoma monocultures, keratinocyte and melanoma cocultures and keratinocyte-to-melanoma conditioned media transfer assays (Fig. 6a). In monocultures, DSP knockdown led to no change in proliferation in the HaCaT keratinocytes or melanoma cells over several days in culture (Extended Data Fig. 5b). In addition, DSP knockdown did not result in any change in apoptosis in melanoma cells and keratinocytes (Extended Data Fig. 5c,d). In contrast, when keratinocytes and melanoma cells were grown together in coculture, we found that proliferation of melanoma cells increased by more than twofold on DSP knockdown in keratinocytes (Fig. 6b and Extended Data Figs. 5b and 6). Notably, significant increases in melanoma proliferation could also be obtained by transfer of conditioned medium from DSP knockdown keratinocytes to melanoma monocultures (Fig. 6c); this effect was seen in three independent melanoma cell lines, two of which were derived from primary melanoma tumors in the radial growth phase35,36. These results suggested that loss of keratinocyte desmosomes promotes neighboring melanoma growth through secreted factors (Fig. 6d).
a, Representative image from keratinocyte monocultures expressing stable nontargeting control (NTC) shRNA, depicting the staining for keratin (KRT14, cyan), DSP (purple) and DSG2 (yellow). Cell nuclei were stained with DAPI (gray). Each stain is shown separately and in a single image overlay. The images show the robust expression and expected location of desmosome components (DSP, DSG2). b, Same as in a but for keratinocyte monocultures expressing stable DSP shRNA, illustrating the effective knockdown of the desmosome proteins DSP and DSG2. Each experiment was repeated independently three times with similar results, with individual replicate values summarized in Extended Data Fig. 5.
a, Keratinocytes were engineered to stably express either NTC shRNA or DSP shRNA constructs; melanoma cells were not genetically engineered. These cell types were grown and characterized independently or as cocultures (first three plates). Alternatively, melanoma cells were characterized in keratinocyte-conditioned medium (final plate). Cells were stained using specific antibodies and characterized using proliferation assays. b, 5-Ethynyl-2′-deoxyuridine (EdU) assay of melanoma cell proliferation (A375), shown for keratinocyte and melanocyte cocultures in which keratinocytes stably expressed NTC shRNA (dark gray) versus DSP shRNA (light gray) for 2, 4, 6 or 8 days. Each violin plot summarizes five distinct fields per well × three biological replicates for n = 15 replicate measurements. Significance was determined using a two-sided, two-sample t-test, Bonferroni-corrected for multiple testing (****P < 6 × 10−5). c, CyQUANT assay of melanoma cell proliferation when grown in conditioned medium from keratinocytes stably expressing either NTC shRNA (dark gray) or DSP shRNA (light gray). Results for three different melanoma cell lines are shown (A375, metastatic; WM1862 and WM1552C, nonmetastatic). Each violin plot summarizes six conditioned-medium measurements. Significance was determined using a two-sided, two-sample t-test, Bonferroni-corrected for multiple testing (*P = 0.020, **P = 0.009, ****P = 1.08 × 10−8). d, Suggested model in which desmosome mutations in keratinocytes lead to decoupling of keratinocyte-melanoma cells and decreased keratinocyte adhesion, which in turn promotes melanocyte proliferation.
Discussion
Typically, studies of the cancer genome have focused on identifying frequent genetic alterations in single genes or associations between individual gene alterations and tumor functional outcomes37,38. The main challenge of these gene-by-gene approaches is that most cancer mutations are rare. However, consideration of groups of genes, corresponding to discrete cellular components such as protein complexes and signaling pathways, provides an expanded means of understanding mutational effects19,39,40. Using such a strategy, we have shown that the desmosome complex is frequently affected by coding mutations in primary melanoma samples, which are associated with a substantial decrease in expression of desmosome components. Spatial transcriptomic profiling and protein IF indicate that these decreases in expression occur predominantly in keratinocytes in the tumor local microenvironment rather than in melanoma tumor cells. These observations are corroborated by genetic disruptions showing that loss of the DSP desmosome subunit in keratinocytes has the effect of amplifying the proliferation of adjacent melanoma cells in coculture.
It is notable that some tumors show coding mutations in several desmosome genes, not just one (Fig. 3c and Extended Data Fig. 3). One way to explain this finding is that some genes in the desmosome system are paralogs, for example, the cadherins DSG1, DSG2 and DSG3, where studies have shown that loss of DSG3 function can be compensated by DSG2 (ref. 41). Similarly, desmocollins can undergo expression pattern switching, in which loss of expression of one isoform can cause upregulation of alternative isoforms, thus retaining desmosome activity42. Another explanation is complementarity between subunits, for instance, PERP deficiency compromises desmoplakin localization such that there may be selection for mutations in only one or the other gene43. Thus, loss of single desmosome genes may not always provide a selective advantage in melanoma because of functional redundancy or complementarity with alternate desmosome members.
We also observed differences in desmosome mutation patterns across melanoma cohorts (Fig. 1c and Extended Data Fig. 2). While these may relate to underlying differences in the biology of the tumor populations analyzed (TCGA SKCM versus Conway et al.22), it is clear that at least part of the difference can be attributed to variations in the two data processing pipelines. In particular, Conway et al.22 describe a more stringent process than that of the TCGA SKCM study, for instance, using an ‘expression filter’ based on a human scRNA-seq dataset among other criteria. Despite these differences, our system-level approach identified the desmosome system as significantly mutated in both cohorts.
The observed interplay between keratinocytes and melanoma cells stands in contrast to the usual mode according to which somatic mutations are thought to promote cancer by direct selection in a clonal population of tumor cells. It is unclear whether desmosome mutant keratinocytes are actually selected by the melanoma tumor or merely serve as a pre-existing condition that increases the risk of tumor formation. A recent study using organotypic skin cultures highlighted that melanoma cells can transcriptionally repress the expression of a desmosomal cadherin subunit, DSG1, in keratinocytes, via paracrine signaling44. Further, loss of DSG1 expression is correlated with increased migration of melanoma tumor cells, suggesting that downregulation of desmosome gene expression is pro-tumorigenic in melanoma, independent of mutations44. If selection occurs, one mechanism could be that desmosome mutant keratinocytes and proliferating melanocytes synergistically amplify one another’s growth. We do not yet know how ‘large’ a patch of mutant keratinocytes would need to be to affect a nearby melanoma. Regardless of clone size, our data suggest that the keratinocyte-melanoma interaction may occur through secreted factors, the nature of which will need to be identified in future studies.
More generally, our results are consistent with earlier findings that non-tumor cells can indeed carry cancer-causing mutations, predominantly in genes associated with tumor initiation rather than clonal expansion45,46. For example, a study of melanocyte transformation identified that non-tumor cells close to a melanoma tumor have significantly greater numbers of mutations than those farther away, including mutations in oncogenes such as BRAF47. Our findings not only support the notion that tumors arise from a collection of cells rather than a clonal population48,49, but they also extend that notion to other cell types, which are not necessarily the cell type of origin. By such a model, mutations in complementary cellular communities may alter expression programs and growth profiles, which in turn help determine the order in which specific mutations arise within the complex cancer tissue.
Methods
Ethics
This study was conducted in accordance with ethical guidelines and received approval from the New York University Institutional Review Board (IRB) (no. s16-00122) for the scRNA-seq experiment. Consent was obtained from all participants before sample collection. The requirement for ethical approval was waived for the GeoMx and IF experiments because these analyses were conducted on de-identified archival tissue samples. No potentially identifiable data are included in this manuscript.
Statistical framework for assessing desmosome mutation
The enrichment analysis of coding mutations in the desmosome system was conducted for each TCGA cancer cohort following the method of Zheng et al.19. First, we used the MutSigCV20 tool to estimate the expected number of tumor samples with somatic coding mutations in each human gene, assuming no positive selection pressure. In estimating this expected number for each gene, MutSigCV accounts for an array of features, including gene length, local mutational signatures, DNA replication timing and mRNA expression level. Second, for each gene we computed the difference between the actual and expected counts of mutated tumor samples. Genes were ranked according to decreasing value of this difference in an ordered gene list. Third, this list was examined for the significance of the rankings of desmosome genes using permutation testing (similar to Mann–Whitney U-test). For the permutation test, the average rank of the desmosome genes in the ordered list was compared to their average rank in each of 100,000 permuted lists of all human genes. This test generated a P value for each TCGA cancer cohort. To account for multiple hypothesis testing (that is, due to multiple cohorts), P values were adjusted using the Benjamini–Hochberg procedure, resulting in q values.
scRNA-seq of primary melanoma tumors
Melanoma tumors were collected postoperatively from two patients who consented to participate in this IRB-approved study. To obtain single-cell suspensions, samples were washed in PBS and cut into small pieces (4–5 mm3) followed by dissociation using the Miltenyi Biotec human tumor dissociation kit according to the manufacturer’s instructions. Red blood cells were depleted using ACK lysing buffer for 3 min. If needed, dead cells were removed using the Miltenyi Biotec dead cell separator. Single-cell encapsulation and library preparation were performed using the inDrop platform27,51 and were followed by sequencing on an Illumina NextSeq system. Sequencing reads were demultiplexed, aligned and counted using a custom pipeline as described previously29 to produce a raw count matrix for each tumor. Quality control was performed as described previously52. The raw matrix count was first transformed to unique molecular identifiers (UMIs) to correct for library preparation duplication53. Cells with more than 750 distinct UMIs, less than 20% mitochondrial transcripts and less than 30% ribosomal transcripts were selected for analysis. UMI counts for the selected cells were normalized by the total number of transcripts per cell; a scale factor equivalent to the median number of transcripts across all cells was applied (median TPM). Expression was transformed using the Freeman–Tukey transformation as described previously54.
UMAP two-dimensional projection and annotation of scRNA-seq data
We selected genes with both above-mean mRNA expression level and above-mean Fano factor (a standardized measure of variance). These genes were then used as features to project cells onto two dimensions using the UMAP technique with default parameters28. Ten communities of cells were clearly discernible in the resulting UMAP projection (Fig. 2b,c). To label the cell type represented by each community, we identified the top differentially expressed genes in each (P < 10−6, Kolmogorov–Smirnov test; effect size > 0.2, Cohen’s d). These genes were cross-referenced against a collection of published gene expression markers of known cell types29,32,55,56,57, allowing unambiguous assignment of each community to one of five types: immune (markers: CD45, CD4, CD8A); endothelial (EPCAM); muscle (MYH11); melanocyte (SOX10, SOX2, S100B); or keratinocyte (KRT4, KRT5, KRT17, KRT19). To further annotate a subset of melanocytes as malignant, we inferred copy number variants (CNVs) from the RNA-seq profiles with inferCNV (https://github.com/broadinstitute/inferCNV), using all other cells from the same tumor sample as a reference. All three melanocyte communities had a common pattern of aneuploidy in their CNV profiles, indicating cancer.
Reanalysis of scRNA-seq from the HCA dataset
The HCA skin dataset was reanalyzed using the CellAtlas.io application. The analysis focused on key relevant cell types, including melanocytes, undifferentiated keratinocytes and differentiated keratinocytes. Of the 15 desmosome genes evaluated, 11 were detected in the dataset (Extended Data Fig. 2e,f).
Spatial transcriptomics using the GeoMx platform
After IRB approval (no. 756049-26), formalin-fixed paraffin-embedded samples of eight primary melanomas were chosen and sectioned (clinical information provided in Supplementary Table 2). The sections were processed for WES to determine desmosome mutation status, using the GATK pipeline with default settings, and for the digital spatial profiling workflow to determine desmosome expression. Digital spatial profiling was performed using the GeoMx system as described previously58. IF visualization markers for keratinocytes (PanCK), melanoma cells (S100B, PMEL) and immune cells (CD45) were used to guide the selection of ROIs containing either pure or mixed areas of each cell type (keratinocyte, melanocyte) followed by RNA profiling using the GeoMx human whole assay.
Melanoma proliferative signature
To calculate the expression level of the proliferative gene program across the datasets presented in this study, we used a predefined gene set used previously50 representing the melanoma proliferation signature. This gene set includes ACP5, CEACAM1, HPS4, NR4A3, RRAGD, WDR91, ADCY2, DAPK1, INPP4B, OCA2, SEMA6A, ZFYVE16, APOE, DCT, IRF4, PHACTR1, SIRPA, ASAH1, FAM174B, IVNS1ABP, PIR, SLC45A2, BIRC7, GALNT3, KAZ, PLXNC1, ST3GAL6, C21orf91, GNPTAB, MBP, PMEL, STX7, CAPN3, GPM6B, MICAL1, RAB27A, TNFRSF14, CDH1, GPR143, MITF, RAB38, TRPM1, CDK2, GPRC5B, MLANA, RGS20, TYR, CDK5R1, GYG2, MYO1D, RHOQ and TYRP1. For each dataset, the expression levels of these genes were aggregated and log-scaled to infer the activity of the proliferation program.
Cell lines (melanoma and keratinocytes)
The melanoma cell line A375 was obtained from ATCC, authenticated using short tandem repeat profiling and tested for Mycoplasma contamination using a MycoAlert Mycoplasma Detection Kit (cat. no. LT07-318, Lonza). The authenticated (using short tandem repeat profiling) and tested primary radial growth phase melanoma cell lines WM1862 and WM1552C were obtained from Rockland. A375 cells were maintained in DMEM (cat. no. 11965, Gibco) supplemented with 10% FCS (Gemini Bio) and 1× penicillin-streptomycin (cat no. 15140122, Gibco). The WM1862 and WM1552C cells lines were maintained in tumor-specialized medium with 2% FCS according to the manufacturer’s instructions. The HaCaT cell line (immortalized keratinocyte cell line) was obtained from AddexBio and authenticated by the Memorial Sloan Kettering Cancer Center Molecular Cytogenetics Core. Keratinocyte lines were maintained in DMEM supplemented with 10% FCS and 1× penicillin-streptomycin.
Lentiviral shRNA cell lines
For the DSP knockdown studies, we used Dharmacon SMARTvector lentiviral shRNA constructs (n = 3 distinct DSP-targeting shRNAs). Of these shRNAs, two showed more than 80% knockdown and were pooled for subsequent studies (sh1: AAGAATCCAACTCCACTGC; sh2: AGCCCTCTTATATGCTAT). Stable knockdown cell lines (HaCaT and A375) were created using puromycin selection for 1 week. HaCaT cells stably expressing NTC (CACACAACATGTAAACCAGGGA) shRNA or DSP-targeting shRNA were then cocultured with the indicated melanoma cell lines for the time points indicated. HaCaT and A375 cells in monoculture stably expressing NTC shRNA or DSP-targeting shRNA were subsequently plated in 96-well plates and used for plate-based proliferation assays.
Immunostaining
For immunostaining, melanoma and keratinocyte monocultures or cocultures were fixed in 4% paraformaldehyde for 15–30 min at room temperature followed by three PBS washes. Cells were permeabilized in 0.1% Triton X-100 for an additional 15–30 min, followed by three PBS washes. For the EdU stain, click-chemistry-based EdU detection was performed using an Abcam kit (cat. no. ab219801) according to the manufacturer’s instructions. To stain for cell-specific markers, cells were treated overnight with primary antibodies at 4 °C then washed with PBS and incubated with secondary antibodies and a nuclear stain (cat. no. H3570, Invitrogen). Imaging was performed on an LSM880 high-resolution confocal microscope (ZEISS) with a ×63 objective using AiryScan imaging. The following primary antibodies were used: mouse anti-human KRT14 (1:1,000 dilution, cat. no. ab7800, Abcam); rabbit anti-human SOX10 (1:500 dilution, cat. no. PA5-84795, Thermo Fisher Scientific); rabbit anti-human S100A6 conjugated to Alexa Fluor 647 (1:100 dilution, cat. no. ab204028, Abcam); anti-DSP1 guinea pig (1:100 dilution, cat. no. DP-1, Progen); and mouse anti-human DSG2 (1:100 dilution, cat. no. 32-6100, Thermo Fisher Scientific). The percentage of EdU+ cells was quantified by calculating double-positive cells (SOX10+S100A6+ or KRT14+ and EdU+) as a fraction of the total number of SOX10 S100A6+ or KRT14+ cells in each field. Image analysis was performed using FIJI. For DSP IF with IRB approval, ten different primary melanoma tissue sections of 5-μm thickness were cut from formalin-fixed, paraffin-embedded tissue blocks. Immunostaining was performed using standard deparaffinization, followed by heat-induced epitope retrieval in a pressure cooker for 10 min at 95 °C as described previously3. Immunostained slides were counterstained with Hoechst 33342 (cat. no. H3570, Invitrogen) and mounted with ProLong Glass Antifade Mountant (cat. no. P36984, Thermo Fisher Scientific). The following primary antibodies were used: anti-rabbit SOX10 (1:100 dilution, clone E6B6I, cat. no. 69661, Cell Signaling Technology); anti-mouse JUP (1:50 dilution, sc514115, Santa Cruz Biotechnology); and anti-DSP1 guinea pig. For DSP membrane signal intensity quantification, JUP staining was used as a membrane mask and quantifications were performed using ImageJ. All sections were imaged on an LSM880 high-resolution confocal microscope with a ×20 objective.
CyQUANT proliferation assay in monocultures
For plate-based measurement of proliferation, 2,000 or 5,000 cells per well (melanoma cells or keratinocytes) were plated in a 96-well plate followed by 24–96 h incubation. Proliferation was measured using a CyQUANT Cell Proliferation Assay (cat. no. C7026, Invitrogen) according to the manufacturer’s instructions. For the conditioned media experiments, equal cell numbers of NTC or DSP shRNA-expressing keratinocytes were cultured in fresh medium; this medium was then collected after 48 h and used to treat the melanoma cells. Fluorescence was ascertained using a BioTek Synergy 96-well plate reader, with all values normalized to the control conditions.
Statistics and reproducibility
For the in vitro validations, statistical analysis was performed on three biological replicates measured five times. No statistical method was used to predetermine sample size for the human tumor cohorts included in this study. No data were excluded from the analyses. The experiments were not randomized and the investigators were not blinded to allocation during the experiments and outcome assessment.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Processed scRNA-seq, GeoMx and annotated mutations from the WES of primary melanoma tumors are available on Figshare (https://figshare.com/projects/Baron_Tagore_2025_Desmosomes/234914). Additionally, the scRNA-seq and GeoMx raw data from this paper have been submitted to the Gene Expression Omnibus under accession nos. GSE291160 and GSE291159, respectively.
Code availability
All code used for this work, including custom algorithms and analysis scripts, has been distributed on Zenodo (https://doi.org/10.5281/zenodo.14880581)59 and GitHub (http://github.com/MaayanBaron/desmosome_paper.git).
References
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011).
Chen, F. et al. New horizons in tumor microenvironment biology: challenges and opportunities. BMC Med. 13, 45 (2015).
Tagore, M. et al. GABA regulates electrical activity and tumor initiation in melanoma. Cancer Discov. 13, 2270–2291 (2023).
Kim, I. S. et al. Microenvironment-derived factors driving metastatic plasticity in melanoma. Nat. Commun. 8, 14343 (2017).
Kunisada, T. et al. Keratinocyte expression of transgenic hepatocyte growth factor affects melanocyte development, leading to dermal melanocytosis. Mech. Dev. 94, 67–78 (2000).
Haass, N. K. & Herlyn, M. Normal human melanocyte homeostasis as a paradigm for understanding melanoma. J. Investig. Dermatol. Symp. Proc. 10, 153–163 (2005).
Green, K. J., Jaiganesh, A. & Broussard, J. A. Desmosomes: essential contributors to an integrated intercellular junction network. F1000Res. 8, F1000 (2019).
Garcia, M. A., Nelson, W. J. & Chavez, N. Cell–cell junctions organize structural and signaling networks. Cold Spring Harb. Perspect. Biol. 10, a029181 (2018).
Chidgey, M. & Dawson, C. Desmosomes: a role in cancer? Br. J. Cancer 96, 1783–1787 (2007).
Godsel, L. M. et al. Translational implications of Th17-skewed inflammation due to genetic deficiency of a cadherin stress sensor. J. Clin. Invest. 132, e144363 (2022).
Furukawa, C. et al. Plakophilin 3 oncogene as prognostic marker and therapeutic target for lung cancer. Cancer Res. 65, 7102–7110 (2005).
Wong, M. P. et al. Loss of desmoglein 1 expression associated with worse prognosis in head and neck squamous cell carcinoma patients. Pathology 40, 611–616 (2008).
Chen, J., O’Shea, C., Fitzpatrick, J. E., Koster, M. I. & Koch, P. J. Loss of desmocollin 3 in skin tumor development and progression. Mol. Carcinog. 51, 535–545 (2012).
Rieger-Christ, K. M. et al. Restoration of plakoglobin expression in bladder carcinoma cell lines suppresses cell migration and tumorigenic potential. Br. J. Cancer 92, 2153–2159 (2005).
Canes, D. Histone deacetylase inhibitors upregulate plakoglobin expression in bladder carcinoma cells and display antineoplastic activity in vitro and in vivo. Int. J. Cancer 113, 841–848 (2005).
Chun, M. G. H. & Hanahan, D. Genetic deletion of the desmosomal component desmoplakin promotes tumor microinvasion in a mouse model of pancreatic neuroendocrine carcinogenesis. PLoS Genet. 6, e1001120 (2010).
Beaudry, V. G. et al. Loss of the p53/p63 regulated desmosomal protein Perp promotes tumorigenesis. PLoS Genet. 6, e1001168 (2010).
Yang, L. et al. Desmoplakin acts as a tumor suppressor by inhibition of the Wnt/β-catenin signaling pathway in human lung cancer. Carcinogenesis 33, 1863–1870 (2012).
Zheng, F. et al. Interpretation of cancer mutations using a multiscale map of protein systems. Science 374, eabf3067 (2021).
Lawrence, M. S. et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499, 214–218 (2013).
Alexandrov, L. B. et al. The repertoire of mutational signatures in human cancer. Nature 578, 94–101 (2020).
Conway, J. R. et al. Integrated molecular drivers coordinate biological and clinical states in melanoma. Nat. Genet. 52, 1373–1383 (2020).
Mularoni, L., Sabarinathan, R., Deu-Pons, J., Gonzalez-Perez, A. & López-Bigas, N. OncodriveFML: a general framework to identify coding and non-coding regions with cancer driver mutations. Genome Biol. 17, 128 (2016).
Barbieri, J. S., Wanat, K. & Seykora, J. in Pathobiology of Human Disease (eds McManus, L. M. & Mitchell, R. N.) 1134–1144 (Academic Press, 2014).
Rickelt, S. Subtypes of melanocytes and melanoma cells distinguished by their intercellular contacts: heterotypic adherens junctions, adhesive associations, and dispersed desmoglein 2 glycoproteins. Cell Tissue Res. 334, 401–422 (2008).
Peitsch, W. K. et al. Desmoglein 2 depletion leads to increased migration and upregulation of the chemoattractant secretoneurin in melanoma cells. PLoS ONE 9, e89491 (2014).
Klein, A. M. et al. Droplet barcoding for single-cell transcriptomics applied to embryonic stem cells. Cell 161, 1187–1201 (2015).
McInnes, L., Healy, J., Saul, N. & Großberger, L. UMAP: uniform manifold approximation and projection. J. Open Source Softw. 3, 861 (2018).
Baron, M. et al. The stress-like cancer cell state is a consistent component of tumorigenesis. Cell Syst. 11, 536–546 (2020).
Akbani, R. et al. Genomic classification of cutaneous melanoma. Cell 161, 1681–1696 (2015).
Aran, D., Sirota, M. & Butte, A. J. Corrigendum: systematic pan-cancer analysis of tumour purity. Nat. Commun. 7, 10707 (2016).
Tirosh, I. et al. Dissecting the multicellular ecosystem of metastatic melanoma by single-cell RNA-seq. Science 352, 189–196 (2016).
Beechem, J. M. in Biomarkers for Immunotherapy of Cancer: Methods and Protocols (eds Thurin, M., Cesano, A. & Marincola, F. M.) 563–583 (Humana Press, 2020).
Wanuske, M.-T. et al. Clustering of desmosomal cadherins by desmoplakin is essential for cell–cell adhesion. Acta Physiol. 231, e13609 (2021).
Masters, J. & Palsson, B. Ø. Human Cell Culture: Cancer Cell Lines Part 1 (Springer Netherlands, 2006).
Hsu, M.-Y., Elder, D. E. & Herlyn, M. in Human Cell Culture (eds Masters, J. R. W. & Palsson, B.) 259–274 (Kluwer Academic Publishers, 2002).
McLendon, R. et al. Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455, 1061–1068 (2008).
Stransky, N. et al. The mutational landscape of head and neck squamous cell carcinoma. Science 333, 1157–1160 (2011).
Hofree, M., Shen, J. P., Carter, H., Gross, A. & Ideker, T. Network-based stratification of tumor mutations. Nat. Methods 10, 1108–1115 (2013).
Olcina, M. M. et al. Mutations in an innate immunity pathway are associated with poor overall survival outcomes and hypoxic signaling in cancer. Cell Rep. 25, 3721–3732 (2018).
Hartlieb, E., Rötzer, V., Radeva, M., Spindler, V. & Waschke, J. Desmoglein 2 compensates for desmoglein 3 but does not control cell adhesion via regulation of p38 mitogen-activated protein kinase in keratinocytes. J. Biol. Chem. 289, 17043–17053 (2014).
Khan, K. et al. Desmocollin switching in colorectal cancer. Br. J. Cancer 95, 1367–1370 (2006).
Ihrie, R. A. et al. Perp is a p63-regulated gene essential for epithelial integrity. Cell 120, 843–856 (2005).
Burks, H. E. et al. Melanoma cells repress desmoglein 1 in keratinocytes to promote tumor cell migration. J. Cell Biol. 222, e202212031 (2023).
Kakiuchi, N. & Ogawa, S. Clonal expansion in non-cancer tissues. Nat. Rev. Cancer 21, 239–256 (2021).
Martincorena, I. et al. Tumor evolution. High burden and pervasive positive selection of somatic mutations in normal human skin. Science 348, 880–886 (2015).
Tang, J. et al. The genomic landscapes of individual melanocytes from human skin. Nature 586, 600–605 (2020).
McGranahan, N. & Swanton, C. Clonal heterogeneity and tumor evolution: past, present, and the future. Cell 168, 613–628 (2017).
Batlle, E. & Clevers, H. Cancer stem cells revisited. Nat. Med. 23, 1124–1134 (2017).
Hoek, K. S. et al. In vivo switching of human melanoma cells between proliferative and invasive states. Cancer Res. 68, 650–656 (2008).
Zilionis, R. et al. Single-cell barcoding and sequencing using droplet microfluidics. Nat. Protoc. 12, 44–73 (2017).
Baron, M. et al. A single-cell transcriptomic map of the human and mouse pancreas reveals inter- and intra-cell population structure. Cell Syst. 3, 346–360 (2016).
Grün, D. & van Oudenaarden, A. Design and analysis of single-cell sequencing experiments. Cell 163, 799–810 (2015).
Wagner, F., Yan, Y. & Yanai, I. K-nearest neighbor smoothing for high-throughput single-cell RNA-Seq data. Preprint at bioRxiv https://doi.org/10.1101/217737 (2017).
Nieto, P. et al. A single-cell tumor immune atlas for precision oncology. Genome Res. 31, 1913–1926 (2021).
Jerby-Arnon, L. et al. A cancer cell program promotes T cell exclusion and resistance to checkpoint blockade. Cell 175, 984–997 (2018).
Barkley, D. et al. Cancer cell states recur across tumor types and form specific interactions with the tumor microenvironment. Nat. Genet. 54, 1192–1201 (2022).
Merritt, C. R. et al. Multiplex digital spatial profiling of proteins and RNA in fixed tissue. Nat. Biotechnol. 38, 586–599 (2020).
Baron, M. Desmosome mutations impact the tumor microenvironment to promote melanoma proliferation. Zenodo https://zenodo.org/records/14880581 (2025).
Acknowledgements
We gratefully acknowledge funding support from the National Institutes of Health (NIH) under grant nos. NCI U54 CA274502 and NIGMS P41 GM103504 to T.I., grant no. R03CA277645 to M.K. and grant no. 5U01CA260432 to I.Y. and R.M.W. We thank L. Yu and A. Gasper for technical assistance with histology and S. Liu and R. Davis for assistance with WES, supported by a UC Davis Comprehensive Cancer Center Support Grant awarded by the National Cancer Institute (no. P30CA093373); a Cancer Center Support Grant no. P30 CA008748; the Melanoma Research Alliance; the Debra and Leon Black Family Foundation; and NIH grant nos. R01CA229215 and R01CA238317.
Author information
Authors and Affiliations
Contributions
M.B. and T.I. conceived and initiated the study, with important feedback from R.M.W. Most of the bioinformatics data analysis was performed by M.B. where M.T. and R.M.W. designed and performed the functional experimental studies. D.B., M.B. and I.Y. performed and analyzed the scRNA-seq data. F.Z. and T.I performed the initial analysis on the NeST hierarchy. M.B. and M.K. collected and analyzed the spatial transcriptomics data. F.Z., P.W. and J.Y. provided critical interpretation. M.B., R.M.W. and T.I. wrote the paper. The paper was critically reviewed and approved by all authors.
Corresponding authors
Ethics declarations
Competing interests
T.I. is a co-founder, member of the advisory board and has an equity interest in Data4Cure and Serinus Biosciences. T.I. is a consultant for and has an equity interest in IDEAYA BioSciences. The terms of these arrangements have been reviewed and approved by UC San Diego in accordance with its conflict of interest policies. R.M.W. is a paid consultant to N-of-One, a subsidiary of QIAGEN. The other authors declare no competing interests.
Peer review
Peer review information
Nature Genetics thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Interactions defining desmosome and context in NeST hierarchy.
(a) Nested Systems in Tumors (NeST) map showing all mutated systems identified across TCGA cohorts, published previously19. Nodes represent protein systems, identified in the previous study from dense communities of interacting proteins. Node size indicates the size of the system in number of proteins. Red intensity scale indicates significance of system mutation frequency in the skin cutaneous melanoma (SKCM) cohort. Gray arrows represent hierarchical containment (that is system 1 → system 2 denotes that system 1 is contained by system 2). For systems contained by multiple others (pleiotropy), each additional containment relation is connected by a dashed arrow. (b) Zoom detail of NeST hierarchy relevant to the desmosome system and its larger containing compartments (left). Adjacent is the specific protein interaction network that defines the desmosome system (right). Colors denote interaction types: Red: physical protein-protein interactions; green: correlation in mRNA expression; purple: correlation in protein abundance; cyan: protein sequence similarity; brown: co-dependency interactions, connecting proteins for which loss-of-function gene knockouts result in similar patterns of growth dependency across cell lines. See original publication19 for more details. (c) Systems under mutational pressure (defined as mutated systems with FDR < 0.25 as determined in previous study, see Zheng et al. for details) in melanoma TCGA-SKCM.
Extended Data Fig. 2 Desmosome mutation frequencies in multiple melanoma cohorts and scRNA-Seq analysis of desmosome gene expression in skin tissues.
(a) Related to Fig. 1. Counts of mutated tumors per each desmosome gene (colored points) in the largest published melanoma cohort (Conway22, left) are compared to the SKCM-TCGA cohort (right). The set of desmosome genes has an above-expected number of mutations in both cohorts, with significance determined using bootstrap analysis (*, P < 10–10 Benjamani-Hochberg correction for multiple testing, see Methods). Desmosome subunits with consistently high mutation frequencies in both cohorts include PKP1, PKP2, DSC1, DSC2 and JUP. DSP has high mutation frequency in TCGA but not Conway. DSG1, DSG3 and DSC3 exhibit a low mutation frequency in both cohorts. Loss of these desmosome cadherins may not provide a selective advantage in melanoma due to functional redundancy with alternate cadherin genes. (b) t-distributed stochastic neighbor embedding (tSNE) analysis of approximately 7500 individual cells from zebrafish melanoma cells. Reanalysis of data published previously29. Color indicates inferred cell type. (c) Same tSNE plot as panel (b), colored by the expression of desmosome genes. (d) Uniform Manifold Approximation and Projection (UMAP) analysis of 239,045 individual cells from healthy human skin, with colors representing inferred cell types of interest (undifferentiated keratinocytes, differentiated keratinocytes and melanocytes). Uncolored (gray) dots correspond to other cell types found in skin including fibroblasts, vascular cells, and lymphocytes. (e) Heatmap showing the average expression levels of desmosome genes in melanocytes as well as differentiated and undifferentiated keratinocytes. (f) Grid of UMAPs from (d), each colored by expression of a different desmosome gene.
Extended Data Fig. 3 TCGA-SKCM cohort summary information. Shown for N = 472 samples in the TCGA-SKCM cohort.
(a) Pie chart describing clinical staging distribution. (b) Pie chart describing sample type distribution. (c) Pie chart describing sex distribution. (d) Histogram describing diagnosis age distribution. (e) Lower: Pie chart describing tumor site distribution. Upper: Tumor site distribution is divided in separate bar plots shown for high desmosome mutation burden (MUT) versus low desmosome mutation burden (WT). MUT and WT are defined by whether the desmosome mutation count is above or below the median value across all patients, respectively. (f) Bar plot depicting the distribution of the number of mutated desmosome genes across primary melanoma tumor samples in the SKCM-TCGA cohort. (g) Bar plot depicting the distribution of primary tumors with multiple coding mutations across desmosome genes in the SKCM-TCGA cohort. (h) Relationship of desmosome expression to number of desmosome mutations across tumor stages. Average desmosome gene expression (TPM, log2) is shown as a function of the number of desmosome genes with coding mutations. Plots are shown separately for each stage of melanoma tumor populations. Regression lines for each of these populations are shown. Shaded areas capture 95% confidence intervals.
Extended Data Fig. 4 Principal Component Analysis of spatial transcriptomic data and association between DSP mutations and proliferative gene expression program.
(a) Profiles of mRNA expression for each ROI (covering 18,695 genes total) are reduced to the first two principal components (PC1 versus PC2). A total of 48 ROIs are drawn from 8 tumor specimens. Color indicates average expression of desmosome genes. (b) Same PCA as (a), color indicates tumor ID. (c) Same PCA as (a), color indicates cell type identified by antibody staining. (d) Degree of proliferative gene expression (as defined previously50, see Methods) in desmosome WT (dark gray, N = 32) or desmosome mutant (light gray, N = 16) regions of interest (ROI) from primary melanoma tumors in the spatial transcriptomics cohort. Significance determined by two sample t-test (*, P = 0.04). The boxes contain the 25th to 75th percentile, the middle line denotes the 50th percentile, and the whiskers mark the 5th and 95th percentiles.
Extended Data Fig. 5 Effects of DSP knockdown on desmosome protein abundance and proliferation using primary melanoma lines.
(a) DSP (left) and DSG2 (right) relative protein expression levels in keratinocytes stably expressing NTC (dark gray, N = 9 replicates) or DSP shRNA (light gray, N = 9 replicates). Significance determined based on two-sample t-test, Bonferroni corrected for multiple testing (****, P < 10−9). (b) EdU proliferation measurements involving additional melanoma cell lines and keratinocytes, shown for co-cultures in which keratinocytes stably express NTC shRNA (dark gray) versus DSP shRNA (light gray) for 2, 4, 6 or 8 days, or 3, 5 or 7 days (indicated on x-axis). Each box summarizes 5 distinct fields per well × 3 biological replicates for N = 15 replicate co-culture measurements. Significance based on two sample two-sided t-test, Bonferroni corrected for multiple testing (**** P < 0.0001, ns - not significant). The boxes contain the 25th to 75th percentile, the middle line denotes the 50th percentile, and the whiskers mark the 5th and 95th percentiles. The cell type (melanoma cell line or HaCaT keratinocyte) measured for proliferation is shown above each plot. For keratinocytes, the co-cultured melanoma cell line is shown in parentheses. (c) Caspase Glo assay for measurement of apoptosis in melanoma cells (A375, left) or keratinocytes (HaCaT, right). Significance based on two sample two-sided t-test (ns - not significant). (d) Cyquant assay of melanoma and keratinocyte cell proliferation measurements at 24, 48, 72 and 96 hours. Error bars represent SEM.
Extended Data Fig. 6 Effects of DSP gene disruption in melanoma/keratinocyte co-cultures.
(a) Representative images from the melanoma/keratinocyte co-cultures with keratinocytes expressing stable NTC shRNA, depicting staining for SOX10 (yellow, melanoma marker), KRT14 (cyan, keratinocyte marker) and EdU (purple, proliferation marker). Grey color represents all cell nuclei (DAPI). First four panels display each staining individually, while the final right-most panel presents a merged image overlay. The white asterisk indicates proliferating melanoma cells (SOX10+,EDU+). (b) Same as (a) but from the melanoma/keratinocyte co-cultures with keratinocytes expressing stable DSP shRNAs. Each experiment was independently repeated 3 times with similar results, with individual replicate values summarized in Fig. 6b.
Supplementary information
Supplementary Tables 1 and 2
Supplementary Table 1. TCGA cohorts and association of desmosome mutation with survival. Supplementary Table 2. Clinical and assay information on the 18 primary melanoma tumors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baron, M., Tagore, M., Wall, P. et al. Desmosome mutations impact the tumor microenvironment to promote melanoma proliferation. Nat Genet 57, 1179–1188 (2025). https://doi.org/10.1038/s41588-025-02163-9
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41588-025-02163-9
This article is cited by
-
Desmosome mutations in keratinocytes fuel melanoma development
Nature Genetics (2025)
-
Desmosome mutations impact the tumor microenvironment to promote melanoma proliferation
Nature Genetics (2025)