Abstract
Donor-derived fecal microbiota treatments are efficacious in preventing recurrent Clostridioides difficile infection (rCDI), but they have inherently variable quality attributes, are difficult to scale and harbor the risk of pathogen transfer. In contrast, VE303 is a defined consortium of eight purified, clonal bacterial strains developed for prevention of rCDI. In the phase 2 CONSORTIUM study, high-dose VE303 was well tolerated and reduced the odds of rCDI by more than 80% compared to placebo. VE303 organisms robustly colonized the gut in the high-dose group and were among the top taxa associated with non-recurrence. Multi-omic modeling identified antibiotic history, baseline stool metabolites and serum cytokines as predictors of both on-study CDI recurrence and VE303 colonization. VE303 potentiated early recovery of the host microbiome and metabolites with increases in short-chain fatty acids, secondary bile acids and bile salt hydrolase genes after antibiotic treatment for CDI, which is considered important to prevent CDI recurrences. These results support the idea that VE303 promotes efficacy in rCDI through multiple mechanisms.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
VE303 strain genomes are available at the National Center for Biotechnology Information (NCBI) GenBank under study ID PRJNA755324, and the unique markers used to track the strains were previously published10. VE303 strain assignments were assessed using the Genome Taxonomy Database version 220 (2024). Raw stool metagenomics datasets and disaggregated clinical metadata have been uploaded to the NCBI Sequence Read Archive under study ID PRJNA1121316. Other unique biological materials generated in this study will be made available under a material transfer agreement with Vedanta Biosciences. Correspondence should be addressed to legal@vedantabio.com and the corresponding authors and will be addressed within 2 weeks. Source data are provided with this paper.
Code availability
Processed datasets and code associated with this manuscript can be accessed on GitHub: https://github.com/vedantabio/VE303-Ph2-paper. All statistical analyses were carried out using R software (version 4.3.1 or higher). Linear mixed effects models were fit using R packages ‘lme4’ (version 1.1-35.1) and ‘lmertest’ (version 3.1-3) and the Maaslin2 package; recurrence-free survival analysis was conducted using the R package ‘survival’ (version 3.2-12); random forest analysis and feature selection were performed using the R packages ‘randomForest’ (version 4.7-1.1) and ‘Boruta’ (version 8.0.0); and bile acid genes in participant metagenomes were profiled using ShortBRED software (version 0.9.5). Further details on statistical and modeling approaches are described in the Methods section.
References
Finn, E., Andersson, F. L. & Madin-Warburton, M. Burden of Clostridioides difficile infection (CDI)—a systematic review of the epidemiology of primary and recurrent CDI. BMC Infect. Dis. 21, 456 (2021).
Feuerstadt, P., Theriault, N. & Tillotson, G. The burden of CDI in the United States: a multifactorial challenge. BMC Infect. Dis. 23, 132 (2023).
Guh, A. Y. et al. Trends in U.S. burden of Clostridioides difficile infection and outcomes. N. Engl. J. Med. 382, 1320–1330 (2020).
Feuerstadt, P. et al. SER-109, an oral microbiome therapy for recurrent Clostridioides difficile infection. N. Engl. J. Med. 386, 220–229 (2022).
Khanna, S. et al. Efficacy and safety of RBX2660 in PUNCH CD3, a phase III, randomized, double-blind, placebo-controlled trial with a Bayesian primary analysis for the prevention of recurrent Clostridioides difficile infection. Drugs 82, 1527–1538 (2022).
van Nood, E. et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N. Engl. J. Med. 368, 407–415 (2013).
Craven, L. J., Nair Parvathy, S., Tat-Ko, J., Burton, J. P. & Silverman, M. S. Extended screening costs associated with selecting donors for fecal microbiota transplantation for treatment of metabolic syndrome-associated diseases. Open Forum Infect. Dis. 4, ofx243 (2017).
DeFilipp, Z. et al. Drug-resistant E. coli bacteremia transmitted by fecal microbiota transplant. N. Engl. J. Med. 381, 2043–2050 (2019).
Chen, Y. et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J. Med. Virol. 92, 833–840 (2020).
Dsouza, M. et al. Colonization of the live biotherapeutic product VE303 and modulation of the microbiota and metabolites in healthy volunteers. Cell Host Microbe 30, 583–598.e8 (2022).
Louie, T. et al. VE303, a defined bacterial consortium, for prevention of recurrent Clostridioides difficile infection: a randomized clinical trial. JAMA 329, 1356–1366 (2023).
Deshpande, A. et al. Risk factors for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Infect. Control Hosp. Epidemiol. 36, 452–460 (2015).
Song, J. H. & Kim, Y. S. Recurrent Clostridium difficile infection: risk factors, treatment, and prevention. Gut Liver 13, 16–24 (2019).
Britton, R. A. & Young, V. B. Role of the intestinal microbiota in resistance to colonization by Clostridium difficile. Gastroenterology 146, 1547–1553 (2014).
Feuerstadt, P. et al. Healthcare resource utilization and direct medical costs associated with index and recurrent Clostridioides difficile infection: a real-world data analysis. J. Med. Econ. 23, 603–609 (2020).
Feuerstadt, P., Nelson, W. W., Teigland, C. & Dahdal, D. N. Clinical burden of recurrent Clostridioides difficile infection in the medicare population: a real-world claims analysis. Antimicrob. Steward. Healthc. Epidemiol. 2, e60 (2022).
Boulesteix, A.-L., Janitza, S., Kruppa, J. & König, I. R. Overview of random forest methodology and practical guidance with emphasis on computational biology and bioinformatics. WIREs Data Min. Knowl. Discov. 2, 493–507 (2012).
Statnikov, A. et al. A comprehensive evaluation of multicategory classification methods for microbiomic data. Microbiome 1, 11 (2013).
Abujamel, T. et al. Defining the vulnerable period for re-establishment of Clostridium difficile colonization after treatment of C. difficile infection with oral vancomycin or metronidazole. PLoS ONE 8, e76269 (2013).
Thabit, A. K. & Nicolau, D. P. Impact of vancomycin faecal concentrations on clinical and microbiological outcomes in Clostridium difficile infection. Int. J. Antimicrob. Agents 46, 205–208 (2015).
Rybak, M. et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am. J. Health Syst. Pharm. 66, 82–98 (2009).
Bradter, U. et al. Variable ranking and selection with random forest for unbalanced data. Environ. Data Sci. 1, e30 (2022).
Fernández, A. et al. Learning From Imbalanced Data Sets (Springer, 2018).
van Rossen, T. M. et al. Prognostic factors for severe and recurrent Clostridioides difficile infection: a systematic review. Clin. Microbiol. Infect. 28, 321–331 (2022).
Shivashankar, R. et al. Clinical factors associated with development of severe-complicated Clostridium difficile infection. Clin. Gastroenterol. Hepatol. 11, 1466–1471 (2013).
Kelly, C. R. et al. ACG clinical guidelines: prevention, diagnosis, and treatment of Clostridioides difficile infections. Am. J. Gastroenterol. 116, 1124–1147 (2021).
Lesniak, N. A. et al. The gut bacterial community potentiates Clostridioides difficile infection severity. mBio 13, e0118322 (2022).
Crobach, M. J. T. et al. The bacterial gut microbiota of adult patients infected, colonized or noncolonized by Clostridioides difficile. Microorganisms 8, 677 (2020).
Mullish, B. H. & Allegretti, J. R. The contribution of bile acid metabolism to the pathogenesis of Clostridioides difficile infection. Therap. Adv. Gastroenterol 14, 17562848211017725 (2021).
Theriot, C. M. et al. Antibiotic-induced shifts in the mouse gut microbiome and metabolome increase susceptibility to Clostridium difficile infection. Nat. Commun. 5, 3114 (2014).
Sorg, J. A. & Sonenshein, A. L. Bile salts and glycine as cogerminants for Clostridium difficile spores. J. Bacteriol. 190, 2505–2512 (2008).
Foley, M. H., O’Flaherty, S., Barrangou, R. & Theriot, C. M. Bile salt hydrolases: gatekeepers of bile acid metabolism and host-microbiome crosstalk in the gastrointestinal tract. PLoS Pathog. 15, e1007581 (2019).
Thanissery, R., Winston, J. A. & Theriot, C. M. Inhibition of spore germination, growth, and toxin activity of clinically relevant C. difficile strains by gut microbiota derived secondary bile acids. Anaerobe 45, 86–100 (2017).
Kang, J. D. et al. Bile acid 7α-dehydroxylating gut bacteria secrete antibiotics that inhibit Clostridium difficile: role of secondary bile acids. Cell Chem. Biol. 26, 27–34.e4 (2019).
Fachi, J. L. et al. Butyrate protects mice from Clostridium difficile-induced colitis through an HIF-1-dependent mechanism. Cell Rep. 27, 750–761 (2019).
Minot, S. S., Krumm, N. & Greenfield, N. B. One Codex: a sensitive and accurate data platform for genomic microbial identification. Preprint at bioRxiv https://doi.org/10.1101/027607 (2015).
Khanna, S. et al. A novel microbiome therapeutic increases gut microbial diversity and prevents recurrent Clostridium difficile infection. J. Infect. Dis. 214, 173–181 (2016).
Martinez, E., Taminiau, B., Rodriguez, C. & Daube, G. Gut microbiota composition associated with Clostridioides difficile colonization and infection. Pathogens 11, 781 (2022).
Yun, B., Song, M., Park, D.-J. & Oh, S. Beneficial effect of Bifidobacterium longum ATCC 15707 on survival rate of Clostridium difficile infection in mice. Korean J. Food Sci. Anim. Resour. 37, 368–375 (2017).
Khanna, S. et al. Gut microbiome predictors of treatment response and recurrence in primary Clostridium difficile infection. Aliment. Pharmacol. Ther. 44, 715–727 (2016).
Larcombe, S., Hutton, M. L., Riley, T. V., Abud, H. E. & Lyras, D. Diverse bacterial species contribute to antibiotic-associated diarrhoea and gastrointestinal damage. J. Infect. 77, 417–426 (2018).
Motamedi, H. et al. A worldwide systematic review and meta-analysis of bacteria related to antibiotic-associated diarrhea in hospitalized patients. PLoS ONE 16, e0260667 (2021).
Zollner-Schwetz, I. et al. Role of Klebsiella oxytoca in antibiotic-associated diarrhea. Clin. Infect. Dis. 47, e74–e78 (2008).
Theriot, C. M. & Young, V. B. Microbial and metabolic interactions between the gastrointestinal tract and Clostridium difficile infection. Gut Microbes 5, 86–95 (2014).
Brown, J. R.-M. et al. Changes in microbiota composition, bile and fatty acid metabolism, in successful faecal microbiota transplantation for Clostridioides difficile infection. BMC Gastroenterol. 18, 131 (2018).
Seekatz, A. M. et al. Restoration of short chain fatty acid and bile acid metabolism following fecal microbiota transplantation in patients with recurrent Clostridium difficile infection. Anaerobe 53, 64–73 (2018).
Mullish, B. H. et al. Microbial bile salt hydrolases mediate the efficacy of faecal microbiota transplant in the treatment of recurrent Clostridioides difficile infection. Gut 68, 1791–1800 (2019).
Guzior, D. V. & Quinn, R. A. Review: microbial transformations of human bile acids. Microbiome 9, 140 (2021).
Lucas, L. N. et al. Dominant bacterial phyla from the human gut show widespread ability to transform and conjugate bile acids. mSystems 6, e0080521 (2021).
Barrasa, J. I., Olmo, N., Lizarbe, M. A. & Turnay, J. Bile acids in the colon, from healthy to cytotoxic molecules. Toxicol. In Vitro 27, 964–977 (2013).
Winston, J. A. et al. Ursodeoxycholic acid (UDCA) mitigates the host inflammatory response during Clostridioides difficile infection by altering gut bile acids. Infect. Immun. 88, e00045-20 (2020).
Chen, J. et al. Targeting Clostridioides difficile: new uses for old drugs. Drug Discov. Today 27, 1862–1873 (2022).
Smith, A. B. et al. Enterococci enhance Clostridioides difficile pathogenesis. Nature 611, 780–786 (2022).
Bosnjak, M. et al. Multi-omics analysis of hospital-acquired diarrhoeal patients reveals biomarkers of enterococcal proliferation and Clostridioides difficile infection. Nat. Commun. 14, 7737 (2023).
Aguirre, A. M. & Sorg, J. A. Gut associated metabolites and their roles in Clostridioides difficile pathogenesis. Gut Microbes 14, 2094672 (2022).
Ouyang, Z.-R., Niu, X.-R., Wang, W.-G. & Zhao, J.-H. The role of short-chain fatty acids in Clostridioides difficile infection: a review. Anaerobe 75, 102585 (2022).
Pensinger, D. A. et al. Butyrate differentiates permissiveness to Clostridioides difficile infection and influences growth of diverse C. difficile isolates. Infect. Immun. 91, e00570-22 (2023).
Collins, S. L., Stine, J. G., Bisanz, J. E., Okafor, C. D. & Patterson, A. D. Bile acids and the gut microbiota: metabolic interactions and impacts on disease. Nat. Rev. Microbiol. 21, 236–247 (2023).
Sorg, J. A. & Sonenshein, A. L. Inhibiting the initiation of Clostridium difficile spore germination using analogs of chenodeoxycholic acid, a bile acid. J. Bacteriol. 192, 4983–4990 (2010).
Theriot, C. M., Bowman, A. A. & Young, V. B. Antibiotic-induced alterations of the gut microbiota alter secondary bile acid production and allow for Clostridium difficile spore germination and outgrowth in the large intestine. mSphere 1, e00045-15 (2016).
Hofmann, J. D. et al. Metabolic reprogramming of Clostridioides difficile during the stationary phase with the induction of toxin production. Front. Microbiol. 9, 1970 (2018).
Carr, A., Baliga, N. S., Diener, C. & Gibbons, S. M. Personalized Clostridioides difficile engraftment risk prediction and probiotic therapy assessment in the human gut. Preprint at bioRxiv https://doi.org/10.1101/2023.04.28.538771 (2024).
Mallick, H. et al. Multivariable association discovery in population-scale meta-omics studies. PLoS Comput. Biol. 17, e1009442 (2021).
Chen, E. Z. & Li, H. A two-part mixed-effects model for analyzing longitudinal microbiome compositional data. Bioinformatics 32, 2611–2617 (2016).
Murphy, J. I., Weaver, N. E. & Hendricks, A. E. Accessible analysis of longitudinal data with linear mixed effects models. Dis. Model. Mech. 15, dmm048025 (2022).
Therneau, T. M. & Grambsch, P. M. Modeling Survival Data: Extending the Cox Model (Springer, 2000).
Kursa, M. B. & Rudnicki, W. R. Feature selection with the Boruta package. J. Stat. Softw. 36, 1–13 (2010).
Kaminski, J. et al. High-specificity targeted functional profiling in microbial communities with ShortBRED. PLoS Comput. Biol. 11, e1004557 (2015).
Heinken, A. et al. Systematic assessment of secondary bile acid metabolism in gut microbes reveals distinct metabolic capabilities in inflammatory bowel disease. Microbiome 7, 75 (2019).
Acknowledgements
We thank the Multiplex Core at the Forsyth Institute, which provided all multiplex protein analysis services. This project was supported in whole or in part with federal funds from the US Department of Health and Human Services, Administration for Strategic Preparedness and Response, Biomedical Advanced Research and Development Authority (BARDA), under contract number 75A50120C00177. As the trial sponsor, Vedanta Biosciences designed the study, collected and analyzed data and wrote the manuscript. BARDA provided partial reimbursement for the costs of the VE303 program and reviewed the manuscript before submission. V.B. and S.K.B. are supported by a sponsored research agreement with Vedanta Biosciences.
Author information
Authors and Affiliations
Contributions
R.M., E.C., A.L.P., B.O., J.L.S., J.F. and J.M.N. conceptualized and designed the study. R.M., S.K.B. and V.B. developed the methodology for statistical and computational analysis. R.M., S.K.B. and E.C. curated and analyzed the data. R.M., S.K.B., E.C., A.L.P., V.B. and J.M.N. contributed to investigation and interpretation of the data. R.M. and J.M.N. drafted the manuscript. All authors contributed to substantial revisions of the manuscript. All authors critically reviewed the manuscript for intellectual content. All authors approved the final version of the submitted manuscript, agree to be accountable for all aspects and vouch for data accuracy and completeness.
Corresponding authors
Ethics declarations
Competing interests
R.M., E.C., A.L.P., B.O., J.L.S. and J.M.N. are employees of Vedanta Biosciences and have an equity interest in the company. Vedanta Biosciences holds patents related to this work. J.F. and V.B. are members of the scientific advisory board of Vedanta Biosciences; J.F. has an equity interest in the company. The other authors declare no competing interests. This content is solely the responsibility of the authors and does not necessarily represent the official views of the US Department of Health and Human Services, Administration for Strategic Preparedness and Response.
Peer review
Peer review information
Nature Medicine thanks Ed Kuijper, Benjamin Mullish and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editors: Liam Messin and Alison Farrell, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
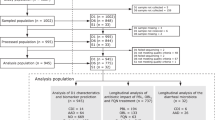
Extended Data Fig. 1 Clinical Study Design and Summary of Data Collection.
A, Clinical study design. Participants were treated with VE303 or placebo after being randomized 1:1:1 into treatment groups. CDI recurrence was evaluated at Week 8, with additional efficacy and safety follow-up through Week 24. B, Metagenomic, metabolomic, and immune datasets examined in the study. C, Sample collection summary (N = total samples, R = samples from recurrent individuals, NR = samples from non-recurrent individuals) for VE303-dosed groups up to Day 14.
Extended Data Fig. 2 Detection of VE303 Strains in All Participants Over Time.
Stacked-bar charts showing detection of individual VE303 strains over time, presented for each participant by treatment group: A, VE303 high-dose, B, VE303 low-dose, and C, placebo. Data are shown for all analyzed samples. D, Exposure to individual VE303 strains after screening and through Day 28. The mean relative abundance per participant over the indicated period is shown across the three treatment groups; VE303 high-dose n = 26; VE303 low-dose n = 26; placebo n = 20. The box-and-whisker plots depict the median, inter-quartile range [IQR] (at the top and bottom of the boxes), and reasonable extreme values at 1.5x IQR in the dataset.
Extended Data Fig. 3 Random Forest Classification Model Schematic and Performance.
A, Schematic of random forest model used to predict features of CDI recurrence and VE303 colonization. Participants were classified into recurrent/non-recurrent and VE303 colonized/non-colonized using a combination of continuous and categorical independent variables including metagenomics, immunological and metabolite datasets, and patient-level metadata such as demographics and medical history. Random forest classification across different data modalities is used to predict B, the colonization status of VE303 strains across all dosed participants; diamonds and error bars represent the mean area under the receiver operating characteristic curve [AUC] ± standard error (se) over n = 10 model iterations C, on-study CDI recurrence status including all VE303 recipients; diamonds and error bars represent the mean AUC ± standard error (se) over n = 100 model iterations and D, on-study CDI recurrence status excluding subjects who recurred later than Day 14; diamonds and error bars represent the mean AUC ± standard error (se) over n = 100 model iterations. Leave-one-out cross-validation was performed to assess the model performance. AUC was computed for all models; an AUC of ≤0.5 (dashed red line) indicates random classification or unreliable model performance. Number labels on each graph indicate the total number of samples available per timepoint and dataset; brackets convey class sizes for (B) colonized/non-colonized and (C, D) recurrent/non-recurrent classes. Missing values indicate lack of sample availability with fewer than 3 recurrent participants available for analysis and unreliable results in the corresponding model.
Extended Data Fig. 4 Random Forest Model Summary for Features Linked to CDI Recurrence.
Random forest model results for microbial, metabolic, and immune features predicting CDI recurrence (at screening) or associated with CDI recurrence (post-screening) in VE303 recipients A, including all participants and B, excluding participants who recurred later than Day 14. The heatmaps represent the frequency with which the feature was selected to be important across 100 model iterations. Features are plotted if permutation importance < 0.1 and frequency > 0.25. Boxes show feature associations with recurrence or non-recurrence identified by the model at the corresponding timepoint.
Extended Data Fig. 5 Increased Age and Inflammation at Screening and CDI Recurrence Prediction.
A, Concentration of cytokines predictive of on-study CDI recurrence at Screening in VE303 recipients with recurrence (n = 12) and without recurrence (n = 32); permutation importance < 0.1, frequency > 0.25 over 100 iterations of a random forest regression model. B, Box-and-violin plots showing age of participants in the VE303-dosed groups; with recurrence (n = 14) and without recurrence (n = 42). C, Correlations between MIP-1β concentrations at baseline and participant age. The blue line indicates the fit from a linear model, while the shaded region indicates the 95% confidence interval for predictions from a linear model. The box-and-whisker plots depict the median, inter-quartile range [IQR] (at the top and bottom of the boxes), and reasonable extreme values at 1.5x IQR.
Extended Data Fig. 6 Associations of Endogenous Taxa at Species, Genus, Family, Order and Class Level with CDI Recurrence and VE303 Abundance.
Effect-size bar plots for all organisms associated with CDI recurrence or non-recurrence (linear mixed effects [LME] model, Results are shown for taxa with un-adjusted p-value < 0.05 computed using the t-statistic.) at the level of A, species, B, genus, C, family, D, order, and E, class. Taxa in the right half of each plot are associated with non-recurrence; those in the left half are associated with recurrence. Bars depict the model effect size estimates for taxa-outcome correlations. Vertical annotations on the right indicate whether taxa were correlated with total VE303 abundance up to Day 14 (LME model); boxes indicate the model estimates for positive or negative correlation with VE303; stars show the level of significance level of correlation with p-values computed using the t-statistic and adjusted for multiple hypotheses by the Benjamini-Hochberg procedure.
Extended Data Fig. 7 Concentration of Primary Bile Acids, Secondary Bile Acids, and Short-chain Fatty Acids Over Time and Differences by Recurrence Status.
Log-transformed total stool concentrations (ng/mg) in individuals with or without a CDI recurrence of A, primary bile acids [BA], B, secondary BA, and C, short-chain fatty acids over time; n samples represented (recurrent/non-recurrent) from Screening to Day 56 are as follows: placebo [9/11, 10/12, 9/11, 8/12, 2/8]; VE303 low-dose [8/16, 10/17, 9/17, 7/14, 1/13]; VE303 high-dose [4/22, 4/25, 3/23, 0/22, 0/22]. The primary BAs include CA, CDCA, TCA, TCDCA, GCA, GCDCA. The secondary BAs include DCA, LCA, DHLCA, TLCA, TDCA, GLCA, GDCA, UDCA, TUDCA, GUDCA, Iso-DCA, and Isoallo- + IsoLCA. The box-and-whisker plots depict the median, inter-quartile range [IQR] (at the top and bottom of the boxes), and reasonable extreme values at 1.5x IQR of the log-transformed metabolite concentrations at each timepoint. D, the heatmap shows the mean log-transformed metabolite concentration per participant during Day 1 through Day 14. Participants are grouped to illustrate differences by recurrence outcomes.
Extended Data Fig. 8 Bile Acid Pathways and Correlation with Bacterial Abundance in Study Participants.
Bile acid genes with differential detection in A, VE303 HD and VE303 LD groups versus placebo group and B, recurrent versus non-recurrent individuals. Only genes with significant differences are shown (false discovery rate [FDR] < 0.1, Linear mixed effects [LME] model). C, Associations between BA genes and the endogenous microbiota (FDR < 0.05, LME), boxes indicate positive or negative correlations between the indicate pairs. VE303 organisms are highlighted on the x-axis; endogenous bacteria with a previously validated role in BA modification are indicated with an asterisk49.
Extended Data Fig. 9 Detection of VE303 Strains in VE303 Recipients at Day 14.
Brick plot showing detection of individual VE303 strains at Day 14 in participants dosed with VE303.
Supplementary information
Supplementary Table 2
Summary of VE303 strain detection in study participants at scheduled timepoints
Source data
Source Data Fig. 1
Source data for plotting VE303 colonization.
Source Data Fig. 2
Statistical source data for plotting features predictive of VE303 colonization.
Source Data Fig. 3
Source data for vancomycin concentrations and VE303 colonization.
Source Data Fig. 4
Statistical source data for plotting features predictive of clinical outcome.
Source Data Fig. 5
Source data for plotting diversity indices and statistical source data for plotting bacterial species associated with clinical outcome.
Source Data Fig. 6
Source data for plotting BAs and SCFAs and statistical source data for plotting host bacteria associations with gut metabolites.
Source Data Extended Data Fig./Table 1
Source data for plotting sample collection schedules for data types collected in study.
Source Data Extended Data Fig./Table 2
Source data for plotting VE303 strain detection in individual subjects.
Source Data Extended Data Fig./Table 3
Statistical source data for RF model performance for predicting VE303 colonization, recurrence and early (by day 14) recurrence.
Source Data Extended Data Fig./Table 4
Statistical source data for RF model importance summaries of features predicting recurrence and early (by day 14) recurrence.
Source Data Extended Data Fig./Table 5
Source data for plotting serum cytokines.
Source Data Extended Data Fig./Table 6
Statistical source data for plotting bacterial taxa at all levels associated with clinical outcome.
Source Data Extended Data Fig./Table 7
Source data for plotting BAs and SCFAs.
Source Data Extended Data Fig./Table 8
Statistical source data for plotting BA genes associated with dose, recurrence and host bacterial taxa.
Source Data Extended Data Fig./Table 9
Source data for plotting VE303 strain detection in individual subjects.
Source Data Extended Data Fig./Table 10
Source data for plotting VE303 strain detection in individual subjects.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Menon, R., Bhattarai, S.K., Crossette, E. et al. Multi-omic profiling a defined bacterial consortium for treatment of recurrent Clostridioides difficile infection. Nat Med 31, 223–234 (2025). https://doi.org/10.1038/s41591-024-03337-4
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41591-024-03337-4
This article is cited by
-
Harnessing the microbiome for cancer therapy
Nature Reviews Microbiology (2026)
-
The impact of an oral purified microbiome therapeutic on the gastrointestinal microbiome
Nature Medicine (2026)
-
Detecting microbial engraftment after FMT using placebo sequencing and culture enriched metagenomics to sort signals from noise
Nature Communications (2025)