Abstract
The objective of the present study was to determine cytokine thresholds derived from predictive models for the diagnosis of chronic periodontitis, differentiating by smoking status. Seventy-five periodontally healthy controls and 75 subjects affected by chronic periodontitis were recruited. Sixteen mediators were measured in gingival crevicular fluid (GCF) using multiplexed bead immunoassays. The models were obtained using binary logistic regression, distinguishing between non-smokers and smokers. The area under the curve (AUC) and numerous classification measures were obtained. Model curves were constructed graphically and the cytokine thresholds calculated for the values of maximum accuracy (ACC). There were three cytokine-based models and three cytokine ratio-based models, which presented with a bias-corrected AUC > 0.91 and > 0.83, respectively. These models were (cytokine thresholds in pg/ml for the median ACC using bootstrapping for smokers and non-smokers): IL1alpha (46099 and 65644); IL1beta (4732 and 5827); IL17A (11.03 and 17.13); IL1alpha/IL2 (4210 and 7118); IL1beta/IL2 (260 and 628); and IL17A/IL2 (0.810 and 1.919). IL1alpha, IL1beta and IL17A, and their ratios with IL2, are excellent diagnostic biomarkers in GCF for distinguishing periodontitis patients from periodontally healthy individuals. Cytokine thresholds in GCF with diagnostic potential are defined, showing that smokers have lower threshold values than non-smokers.
Similar content being viewed by others
Introduction
Periodontitis is a public health problem, as it is highly prevalent and causes disability and social inequality1. In 2010, severe periodontitis was estimated to be the sixth most prevalent disease globally, affecting 743 million people worldwide2. Periodontitis is currently being connected bidirectionally to the pathogenesis of various conditions and systemic diseases of high morbi-mortality such as diabetes, coronary heart disease, metabolic syndrome, chronic respiratory diseases, rheumatoid arthritis, cancer, obstetric complications and cognitive impairment3,4.
It is now widely accepted that, although the initiating factor is a polymicrobial dysbiosis5, the pathogenesis of periodontitis is driven by the development of a chronic inflammatory host immune response6,7. The nature and extent of this response are fundamental determinants of the susceptibility to and progression of periodontitis6,7.
Cytokines are soluble protein ‘messenger’ molecules produced by a variety of cells that transmit signals to other cells8. Cytokines play a crucial role in initiating and sustaining the inflammatory immune response by stimulating the production of secondary mediators. These mediators, in turn, evoke a cascade of events that amplify the inflammatory response and induce the production of enzymes that are responsible for the degradation of connective tissue and osteoclastic bone resorption9.
Cytokines interact and function within a complex and dynamic network of interactions, rather than being dominated by the action of individual cytokines8. In fact, an imbalance between the pro-inflammatory and anti-inflammatory cytokines derived from Th1, Th2, Th17 and Treg lymphocyte subpopulations is suggested as being responsible for periodontal breakdown through cellular and humoral hyper-immune responses10. However, the reductionist approach is predominant in vivo research, as very few authors have analysed the simultaneous presence of more than 10 cytokines11,12,13, or more than four cytokine ratios, in gingival crevicular fluid (GCF) from periodontal patients14,15. Accordingly, more evidence is required from multiple cytokine analyses to increase what is understood of this complex and dynamic network8.
On the other hand, the detection of biomarkers in GCF for predicting the early onset of periodontitis or evaluating the untreated or treated disease activity is a key challenge in periodontology16,17,18. There is, however, limited literature on the development and validation of predictive models based on GCF cytokine levels for the diagnosis or prognosis of periodontitis19,20.
Accordingly, the objectives of this cross-sectional study were:
-
1.
To compare the levels of 16 cytokines detected in GCF, as well as multiple cytokine ratios obtained from them, in periodontally healthy individuals and patients with chronic periodontitis.
-
2.
To determine the diagnostic value thresholds derived from cytokine-based and cytokine ratio-based models in non-smokers and smokers, selecting those models with a high discriminatory capacity to distinguish between periodontal patients and periodontally healthy controls.
-
3.
To validate cytokine-based and cytokine ratio-based models internally using bootstrapping techniques, describing their diagnostic thresholds, as well as apparent and corrected measures of discrimination and classification.
Materials and Methods
Selection of study groups
A sample of 150 eligible participants was recruited among 250 consecutive patients from the general population who were referred to the School of Medicine and Dentistry (Universidade de Santiago de Compostela, Spain) for an evaluation of their oral health status between 2013 and 2015. This sample consisted of all the cases (patients with the target condition, that is, 75 subjects affected by moderate to severe generalised chronic periodontitis -perio group-) and a random sample of the noncases (75 periodontally healthy controls -control group-). Patients were selected if they fulfilled the inclusion criteria, which are detailed in the footnote of Table 1.
One previously calibrated, experienced dentist performed all the periodontal examinations. The probing pocket depth (PPD) and clinical attachment level (CAL) were recorded on all teeth at six sites per tooth using a PCP-UNC 15 probe. Bleeding on probing (BOP) and bacterial plaque level (BPL) data were recorded for the full mouth on a binary scale (presence/absence) on six sites per tooth. Standardised radiographs of all teeth were obtained to assess the alveolar bone status.
The presence of periodontal health or moderate to severe generalised chronic periodontitis was established according to the clinical/radiographic information, applying previously published criteria21,22. Smoking histories were obtained using a questionnaire, with information collected on smoking status (never, past or current, the number of months of smoking and the number of cigarettes/day). All the answers were reviewed with the subject by a member of the study team.
This study was conducted according to the principles outlined in the Declaration of Helsinki (as revised in 2000) on experimentation involving human beings23. The TRIPOD guidelines were considered for further predictive analysis24.
Gingival crevicular fluid sampling
The GCF collection took place one week after the initial examination, and the samples were obtained at the same time of day (in the afternoon, approximately 5–7 h after toothbrushing). A paper strip (Periopaper, Amityville, NY, USA) was inserted into the gingival sulcus or periodontal pocket for 30 sec, using a GCF collection protocol previously described25. GCF samples from the controls and periodontal patients were collected and pooled from 20 non-adjacent proximal sites. In the first case, samples were taken from subgingival sites from teeth in quadrants 1 and 3, and in the second case from sites from the most in-depth PPD in each quadrant.
Strips from each subject were inserted into labelled tubes with 300 ml of 0.01 M PBS (pH = 7.2) and a protease inhibitor (Complete Mini, protease inhibitor cocktail tablets, Roche Applied Science, Indianapolis, IN, USA). To ensure sample collection, the GCF volume was determined based on measurements of weighing the tubes and strips before and after sampling using a very sensitive scale26 (readability of 0.01 mg; Explorer Semi Micro Ex125M, OHAUS, Greifensee, Switzerland). All the samples collected had volumes of GCF ≥ 10 µl. After obtaining the supernatant, the GCF samples were frozen at −80 °C until further biochemical analysis.
Quantification of cytokines in gingival crevicular fluid using multiplexed bead immunoassays
GCF cytokine levels were determined using the human cytokine 16-plex Procarta immunoassay (Affymetrix, Inc., Santa Clara, CA, USA). Sixteen mediators were measured: granulocyte-macrophage colony stimulating factor – GMCSF; IFNgamma; IL1alpha; IL1beta; IL2; IL3; IL4; IL5; IL6; IL10; IL12p40; IL12p70; IL13; IL17A; IL17F; and TNFalpha.
A single investigator blinded to the clinical data performed the experimental analyses of the GCF cytokine quantification. The assays were performed in 96-well filter plates following the manufacturer’s instructions and applying an analysis protocol described previously25. The GCF samples were quantified using the Luminex 100™ instrument (Luminex Corporation, Austin, Texas, USA) and all of them were run in duplicate. The concentrations of the unknown samples were estimated from the standard curve using a 5PL algorithm and the Luminex IS 2.3 and xPONENT 3.1 software packages (Luminex Software, Inc.). Values were expressed as pg/ml adjusting for the dilution factor. Samples below the detection limit (DL) of the assay were recorded as DL/227, while those above the upper limit of quantification of the standard curves were assigned the highest value of the curve.
Statistical analysis
The statistical analyses were performed using the R software (version 3.4.3)28. It is available as Free Software under the terms of the Free Software Foundation’s GNU General Public License in source code form. After applying the Shapiro-Wilks test and verifying the non-normal distribution of almost all the clinical variables, the Mann-Whitney U test was used to compare the quantitative variables between the perio and control groups. The Fisher’s exact test was used to assess the association of the qualitative variables between both study groups. The significance level applied was a p-value < 0.05.
Comparison of GCF cytokine levels and cytokine ratio values in periodontally healthy individuals and patients with chronic periodontitis
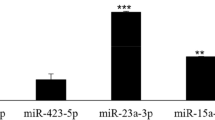
After verifying the non-normal distribution of variables using the Shapiro-Wilks test, the Mann-Whitney U test was used to compare the cytokine levels and cytokine ratios in the control and perio groups. The significance levels applied were adjusted by the Benjamini-Hochberg correction29, with p-values ≤ 1 × 10−3 and <1 × 10−5, respectively. A total of 66 cytokine ratios were evaluated, taking into account exclusively those cytokines that showed significant levels in the periodontal patients compared to the controls (Fig. 1).
Predictive modelling of chronic periodontitis based on cytokine levels and cytokine ratios: model selection; discrimination and classification measures; determination of diagnostic thresholds; and internal validation
To obtain specific diagnostic thresholds differentiating by smoking status, we decided to develop different models for non-smokers and smokers (n = 93 and 54, respectively). Models were constructed by selecting one cytokine or cytokine ratio as a predictor variable, which was treated in its original scale.
The statistical criterion applied for the model selection was the ability of each cytokine- or cytokine ratio-based model to determine the presence of chronic periodontitis using the value of the area under the curve (AUC)30. The AUC values and their corresponding 95% confidence intervals (CIs) obtained by bootstrapping were calculated using the pROC package (version 1.10.0)31. Only those models that presented an apparent AUC ≥ 0.85 in both types of model for smokers and non-smokers were selected32.
The best cut-off value or optimal classification threshold for each model was defined as that which provides the maximum percentage of correct predictions (accuracy, ACC), and was calculated using the PresenceAbsence package (version 1.1.9)33. By setting this optimal value, various classification measures such as the ACC, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV), as well as their corresponding 95% CIs acquired by bootstrapping, were obtained using the pROC package31. The respective cytokine levels or cytokine ratios were calculated for all the periodontitis probability values of each model, and the model curves were constructed graphically using the ggplot package (version 2.2.1)34.
Regarding internal validation, bootstrapping was used to test for possible overfitting by determining the optimism values on the discrimination and classification measures. The bootstrap analysis was replicated on 10,000 random samples of the same sample size, drawn with replacements from the original sample35,36. Bias-corrected (bc) AUC and all other classification measures (bc-sensitivity, bc-specificity, bc-PPV, bc-NPV) were calculated as their corresponding apparent measures derived from the entire original sample minus optimism35,36. This technique was also used to define the cytokine thresholds for the median ACC values derived from 10,000 samples from each model selected, as well as the thresholds for the 90% CIs of the ACC values (Fig. 1).
Ethics approval and consent to participate
The study’s protocol was approved by the Clinical Research Ethics Committee of Galicia (number 2015/006). Patients who agreed to participate in the research provided written informed consent.
Results
The mean age of the study group was 48.37 ± 11.55 years; 62 individuals were male and 85 female. The perio group had significantly higher BPL, BOP, PPD and CAL values than the control group at both the full mouth and sampling site levels (p < 0.001; Table 1). The number of smokers was significantly higher in the perio group than in the control group (41 and 13 patients, respectively, p < 0.001; Table 1).
Comparison of GCF cytokine levels and cytokine ratio values in periodontally healthy individuals and patients with chronic periodontitis
All the pro-inflammatory cytokines analysed (GMCSF, IL1alpha, IL1beta, IL6, IL12p40, IL17A, IL17F and TNFalpha), as well as four cytokines with anti-inflammatory effects (IFNgamma, IL2, IL3 and IL4), had significantly higher levels in the perio group than in the control group (adjusted p-value ≤ 1 × 10−3). Nineteen cytokine ratios showed significant differences between the control and perio groups (adjusted p-value < 1 × 10−5). Of these ratios, nine were based on the combination of two pro-inflammatory cytokines, which were: IL1alpha combined with GMCSF, IL12p40 and TNFalpha; and IL1beta combined with GMCSF, IL12p40, IL17F or TNFalpha, GMCSF/IL17A and IL17A/IL17F. The remaining 10 ratios were based on the combination of one pro-inflammatory cytokine and one cytokine with anti-inflammatory effects. These were: IL1alpha/IL2; IL1alpha/IL3; IL1alpha/IFNgamma; ILbeta/IL2; ILbeta/IL3; ILbeta/IL4; ILbeta/IFNgamma; IL17A/IL2; IL17A/IL3; and IL17A/IFNgamma. All these cytokine ratios, except for GMCSF/IL17A, had significantly higher values in the perio group than in the control group (Table 2).
Predictive modelling of chronic periodontitis based on GCF cytokine levels and cytokine ratios: model selection; discrimination and classification measures; determination of diagnostic thresholds; and internal validation
There were three cytokine-based models and three cytokine ratio-based models, which had an apparent AUC ≥ 0.85 for both non-smokers and smokers. These models were IL1alpha, IL1beta, IL17A, IL1alpha/IL2, IL1beta/IL2 and IL17A/IL2.
Apparent and bc-percentages of discrimination and classification of the six predictive models are described in Table 3. The cytokine-based models had AUC and bc-AUC values ≥ 0.940 and ≥ 0.912, respectively, and the cytokine ratio-based model values were ≥ 0.857 and ≥ 0.834, respectively. The bc-ACC range derived from the cytokine-based models was 86.8–94.1% and that of the cytokine ratio-based models was 72.9–88.7%, with IL17A and IL17A/IL2 being the biomarkers with the lowest bc-ACC values in both smokers and non-smokers. The 95% CIs of the model coefficients and those of the performance measures are detailed in Supplementary Dataset 1.
The periodontitis probability range for the median ACC values varied between 23 and 51%. The cytokine thresholds in pg/ml for the median ACC values (and those for the 95% CIs of the ACC values) for smokers and non-smokers were, respectively: IL1alpha model: 46099 (37495–64161) and 65644 (51310–76700); IL1beta model: 4732 (3705–6459) and 5827 (4721–7532); IL17A model: 11.03 (7.28–15.22) and 17.13 (13.10–22.53); IL1alpha/IL2 model: 4210 (3164–5648) and 7118 (4798–10166); IL1beta/IL2 model: 260 (63–487) and 628 (348–897); and IL17A/IL2 model: 0.810 (0.707–1.132) and 1.919 (1.073–3.489). The range of cytokine thresholds represented around 9–13% of the cytokine or ratio measurement range, except for IL17/IL2 for non-smokers (30%). Compared to the non-smokers, the smokers had lower diagnostic thresholds on all the predictive models for both apparent ACC values and ACC values obtained by bootstrapping (Figs 2–4).
Discussion
High cytokine concentrations and cytokine ratios in the gingival crevicular fluid of patients with chronic periodontitis
As mentioned in the Introduction, there has been a failure to study a broader spectrum of cytokines that may directly influence the local inflammatory response in different types of periodontitis37. The present series is the first comparative analysis of more than 50 cytokine ratios derived from the simultaneous quantification of 16 cytokines with different roles in the pathophysiology of chronic periodontitis7,8.
It should be noted that a particularly strict corrected significance value was applied (adjusted p-value < 1 × 10−5) in order to select the cytokine ratios with the most significant impact on chronic periodontitis. This statistical decision conditioned the ratios considered to be non-significant and significant. As a consequence, comparisons with the contributions of other authors must be interpreted with caution.
Although very few authors have investigated the ratios between pro-inflammatory cytokines in periodontitis38,39,40, up to eight pro-inflammatory cytokine ratios showed significant differences in periodontal patients. Although we detected significantly elevated levels of all the pro-inflammatory cytokines analysed, IL1alpha and IL1beta were the most important biomarkers in terms of increased concentration associated with the disease. This resulted that the ratios based on IL1alpha combined with GMCSF, IL12p40 or TNFalpha, and IL1beta combined with GMCSF, IL12p40, IL17F or TNFalpha, showed significantly higher values in the periodontal patients. Coinciding with the results reported by Azman et al.41, we also obtained a significantly elevated IL17A/IL17F ratio in the patients with chronic periodontitis. Interestingly, in this series, and unlike the other pro-inflammatory cytokine ratios, the GMCSF/IL17A ratio had significantly lower values in the periodontal patients, representing the first evidence of the impact of this ratio in the pathogenesis of periodontitis.
Most previous studies have focused on the analysis of ratios between pro-inflammatory and anti-inflammatory cytokines, or vice versa, in periodontal diseases, with IL1beta/IL10 and IL11/IL17 being the most evaluated14,38,42,43,44,45. In the present series, up to nine ratios based on the combination of one pro-inflammatory cytokine (IL1alpha, ILbeta or IL17A) and one cytokine with anti-inflammatory effects (IFNgamma, IL2, IL3 or IL4) showed significantly higher values in the periodontal patients. These results were due to the higher mean concentrations of pro-inflammatory cytokines compared to the levels presented by anti-inflammatory cytokines. In contrast to the findings of Stadler et al.46, these mediators also showed a significant mean increase associated with chronic periodontitis. On the other hand, applying multivariate predictive modelling techniques, we have previously demonstrated that the extent of the periodontitis-associated imbalance between IL1alpha, ILbeta or IL17A (acting as enhancers) and IFNgamma, IL2, IL3 or IL4 (acting as protectors) was associated with a particular probability of having chronic periodontitis25.
We have not found any articles that would enable us to compare our findings on ratios between IL1alpha and different anti-inflammatory cytokines. Regarding the ratios between ILbeta and other anti-inflammatory cytokines, some authors have observed that: the ILbeta/IL10 ratio was increased in the GCF or gingival tissue of patients with aggressive periodontitis or chronic periodontitis14,42,43; this ratio was significantly reduced after periodontal therapy43. However, after studying these papers in detail, these results can be attributed mainly to significantly higher mean levels of IL1beta, while the levels of IL10 showed non-significant individual variations. These results obtained in vivo call into question the importance of this ratio in the pathogenesis of periodontitis. Likewise, in the present study, no significant differences in IL10 levels between the controls and periodontal patients were detected, and so the IL1beta/IL10 ratio was not evaluated. However, it should be noted that IL10 acquired a greater protagonism as an anti-inflammatory cytokine within a two-biomarker predictive model, as this increased the capacity of IL1beta to discriminate the chronic periodontitis state25. In contrast, in the present series, we observed that other ratios, such as IL1beta/IFNgamma, ILbeta/IL2, ILbeta/IL3 and ILbeta/IL4, may play an essential role in quantitative terms in chronic periodontitis. Several studies have revealed that the IL11/IL17 ratio was reduced in patients with chronic and aggressive periodontitis44,45,47, although other authors have described conflicting findings38. In the present study, other ratios such as IL17A/IFNgamma, IL17A/IL2, IL17A/IL3 and IL17A/IL4 had significantly higher values in the periodontal patients, reflecting their impact on chronic periodontitis.
Consequently, this study is the first time that evidence is provided on a high number of ratios between pro-inflammatory cytokines or pro-inflammatory and anti-inflammatory cytokines that, due to their performance in GCF samples, could be biomarkers associated with chronic periodontitis. Future research is required to clarify the relevance of these ratios in the chronic periodontitis pathogenesis.
High predictive ability of GCF cytokine levels and cytokine ratios for the diagnosis of chronic periodontitis
Due to the characteristics of cytokine networks48, whether cytokines in GCF may show an acceptable ability to discriminate chronic periodontitis from periodontal health is questioned. However, this affirmation is supported by little evidence, as there are very few studies that have evaluated the predictive properties of cytokines in chronic and aggressive periodontitis using an appropriate experimental design19,20. The current series reveals the first results on the predictive ability of cytokines and cytokine ratios for the diagnosis of chronic periodontitis, differentiating between smokers and non-smokers. Moreover, internal validation was carried out for the first time on the predictive parameters obtained, as recommended in the TRIPOD guidelines24.
In this study, in relation to individual cytokines, and corroborating observations published previously by our research group25, there were three models consisting of IL1alpha, IL1beta and IL17A, which presented a bc-AUC > 0.90 for both smokers and non-smokers. According to experts in the field32, these high AUC values indicate that these pro-inflammatory cytokines have a great capacity to discriminate the disease condition. Consequently, these pro-inflammatory cytokines were associated with elevated bc-ACC percentages: 90.7% (for IL1beta), 90.3% (for IL17A) and 89.4% (for IL1alpha) in smokers; and 94.1%, 86.8% and 92.4%, respectively, in non-smokers. Findings on IL1’s high predictive ability are consistent with those previously described by Baeza et al.20, while IL17’s findings represent the first evidence of a strong diagnostic capability. In our opinion, our results on the high predictive potential of these cytokines are comparable to those found for other well-known biomarkers, such as different metalloproteinases20.
We evaluated the cytokine ratios using predictive modelling techniques, with the aim being to identify a set of biomarkers that guarantee a high diagnostic predictability16. In this sense, we obtained three ratio-based models consisting of IL1alpha/IL2, IL1beta/IL2 and IL17A/IL2, which presented a bc-AUC > 0.80 for both smokers and non-smokers. These bc-AUC values, although lower than those detected in individual cytokines, were also very high, revealing that these cytokine ratios were associated with an excellent ability to discriminate periodontitis patients32.
For the first time in the literature, we have defined specific thresholds with diagnostic potential for each smoking status. These were derived from cytokine- and cytokine ratio-based predictive models, and their validity was verified given that the apparent ACC and median ACC values derived from the bootstrap approaches were similar. On the other hand, the range of thresholds obtained by bootstrapping represented only around 9–13% of the measurement range of the biomarkers (except for the IL17A/IL2 ratio in non-smokers). Accordingly, the upper and lower thresholds of these ranges would ensure optimal diagnostic classification.
In line with the trend of attempting to discover biomarkers to improve the clinical diagnosis of periodontal diseases16,17,18, the determination of these specific thresholds could represent a first step in the design and construction of chronic periodontitis diagnostic kits for use in clinical practice.
As smoking is a well-established traditional risk factor for chronic periodontitis49,50, we demonstrated previously from a predictive perspective that smoking status increases the probability of having chronic periodontitis by 15–20%25. Interestingly, in the present series, smokers had lower diagnostic thresholds than non-smokers. At a biochemical level, this justifies what is observed at a clinical level, i.e. the presence of a less intense inflammatory reaction in smoking-associated periodontitis, indicating that smoking may have an immunosuppressant effect49. Secondly, it reveals the convenience of designing biomarker studies for predicting periodontal diseases differentiating by smoking status, especially if the diagnostic thresholds are to be defined.
Our research has some limitations. Although we are in a scenario of small data, the sample size used allowed certain metrics of model performance were estimated with an acceptable precision24; in addition, a strict model selection criterion (apparent AUC value ≥ 0.85) was applied for both non-smokers and smokers. An internal validation process was carried out using bootstrap techniques, with the aim being to counteract the prediction that the study’s accuracy is only measured in the samples that generated the model equations24. Although the results derived from the internal validation were quite optimal, the predictive parameters and diagnostic thresholds obtained from our models should be evaluated in an external cohort of patients (including using calibration analyses) to verify whether our findings are applicable universally.
In conclusion, a high number of previously undescribed GCF cytokine ratios are elevated in patients with chronic periodontitis, evidencing disease-associated imbalances between cytokines with pro-inflammatory and anti-inflammatory effects. IL1alpha, IL1beta and IL17A, and their ratios with IL2, are excellent diagnostic biomarkers in GCF for distinguishing periodontitis patients from periodontally healthy individuals. Cytokine thresholds in GCF with diagnostic potential are defined, showing that smokers have lower threshold values than non-smokers.
Availability of Data and Material
All results obtained in this study are included in this manuscript and in the supplementary information file.
References
Baehni, P. & Tonetti, M. S., Group of the European Workshop on Periodontology. Conclusions and consensus statements on periodontal health, policy and education. Eur. J. Dent. Educ. 14(Suppl 1), 2–3, https://doi.org/10.1111/j.1600-0579.2010.00619.x (2010).
Kassebaum, N. J. et al. Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J. Dent. Res. 93, 1045–1053, https://doi.org/10.1177/0022034514552491 (2014).
Linden, G. J. & Herzberg, M. C., Working Group 4 of the Joint EFP/AAP Workshop. Periodontitis and systemic diseases. J. Periodontol. 84(4 Suppl), S20–3, https://doi.org/10.1902/jop.2013.1340020 (2013).
Cardoso, E. M., Reis, C. & Manzanares-Céspedes, M. C. Chronic periodontitis, inflammatory cytokines, and interrelationship with other chronic diseases. Postgrad. Med. 130, 98–104, https://doi.org/10.1080/00325481.2018.1396876 (2018).
Camelo-Castillo, A. J. et al. Subgingival microbiota in health compared to periodontitis and the influence of smoking. Front. Microbiol. 6, 119, https://doi.org/10.3389/fmicb.2015.00119 (2015).
Ebersole, J. L. et al. Periodontal disease immunology: ‘double indemnity’ in protecting the host. Periodontol. 2000 62, 163–202, https://doi.org/10.1111/prd.12005 (2013).
Jaedicke, K. M., Preshaw, P. M. & Taylor, J. J. Salivary cytokines as biomarkers of periodontal diseases. Periodontol. 2000 70, 164–183, https://doi.org/10.1111/prd.12117 (2016).
Preshaw, P. M. & Taylor, J. J. How has research into cytokine interactions and their role in driving immune responses impacted our understanding of periodontitis. J. Clin. Periodontol. 38(Suppl 11), 60–84, https://doi.org/10.1111/j.1600-051X.2010.01671.x (2011).
Korte, D. L. & Kinney, J. Personalized medicine: an update of salivary biomarkers for periodontal diseases. Periodontol. 2000 70, 26–37, https://doi.org/10.1111/prd.12103 (2016).
Garlet, G. P. Destructive and protective roles of cytokines in periodontitis: a re-appraisal from host defense and tissue destruction viewpoints. J. Dent. Res. 89, 1349–63, https://doi.org/10.1177/0022034510376402 (2010).
Tymkiw, K. D. et al. Influence of smoking on gingival crevicular fluid cytokines in severe chronic periodontitis. J. Clin. Periodontol. 38, 219–228, https://doi.org/10.1111/j.1600-051X.2010.01684.x (2011).
Shimada, Y., Tabeta, K., Sugita, N. & Yoshie, H. Profiling biomarkers in gingival crevicular fluid using multiplex bead immunoassay. Arch. Oral Biol. 58, 724–730, https://doi.org/10.1016/j.archoralbio.2012.11.012 (2013).
Zhou, J. et al. Relationship between gingival crevicular fluid microbiota and cytokine profile in periodontal host homeostasis. Front. Microbiol. 8, 2144, https://doi.org/10.3389/fmicb.2017.02144 (2017).
Górska, R. et al. Relationship between clinical parameters and cytokine profiles in inflamed gingival tissue and serum samples from patients with chronic periodontitis. J. Clin. Periodontol. 30, 1046–52, https://doi.org/10.1046/j.0303-6979.2003.00425.x.
Mohamed, H. G. et al. Influence of type 2 diabetes on local production of inflammatory molecules in adults with and without chronic periodontitis: a cross-sectional study. BMC Oral Health 15, 86, https://doi.org/10.1186/s12903-015-0073-z (2015).
Zhang, L., Henson, B. S., Camargo, P. M. & Wong, D. T. The clinical value of salivary biomarkers for periodontal disease. Periodontol. 2000 51, 25–37, https://doi.org/10.1111/j.1600-0757.2009.00315.x (2009).
Buduneli, N. & Kinane, D. F. Host-derived diagnostic markers related to soft tissue destruction and bone degradation in periodontitis. J. Clin. Periodontol. 38, 85–105, https://doi.org/10.1111/j.1600-051X.2010.01670.x (2011).
Barros, S. P., Williams, R., Offenbacher, S. & Morelli, T. Gingival crevicular fluid as a source of biomarkers for periodontitis. Periodontol. 2000 70, 53–64, https://doi.org/10.1111/prd.12107 (2016).
Shaddox, L. M. et al. Local inflammatory markers and systemic endotoxin in aggressive periodontitis. J. Dent. Res. 90, 1140–1144, https://doi.org/10.1177/0022034511413928 (2011).
Baeza, M. et al. Diagnostic accuracy for apical and chronic periodontitis biomarkers in gingival crevicular fluid: an exploratory study. J. Clin. Periodontol. 43, 34–45, https://doi.org/10.1111/jcpe.12479 (2016).
Armitage, G. C. Development of a classification system for periodontal diseases and conditions. Ann. Periodontol. 4, 1–6 (1999).
Page, R. C. & Eke, P. I. Case definitions for use in population-based surveillance of periodontitis. J. Periodontol. 78, 1387–1399 (2007).
World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. J. Am. Med. Assoc. 310, 2191–2194, https://doi.org/10.1001/jama.2013.281053 (2013).
Moons, K. G. M. et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann. Intern. Med. 162, W1–W74, https://doi.org/10.7326/M14-0698 (2015).
Tomás, I. et al. Cytokine-based predictive models to estimate the probability of chronic periodontitis: development of diagnostic nomograms. Sci. Rep. 7, 11580, https://doi.org/10.1038/s41598-017-06674-2 (2017).
Griffiths, G. S. Formation, collection and significance of gingival crevice fluid. Periodontol. 2000 31, 32–42 (2003).
Uh, H.-W., Hartgers, F. C., Yazdanbakhsh, M. & Houwing-Duistermaat, J. J. Evaluation of regression methods when immunological measurements are constrained by detection limits. BMC Immunol. 9, 59, https://doi.org/10.1186/1471-2172-9-59 (2008).
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, http://www.R-project.org/ (2018).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B 57, 289–300 (1995).
Steyerberg, E. W. et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21, 128–138, https://doi.org/10.1097/EDE.0b013e3181c30fb2 (2010).
Robin, X. et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics 12, 77, https://doi.org/10.1186/1471-2105-12-77 (2011).
Hosmer, D. W., Lemeshow, J. S. & Sturdivant, R. X. Applied Logistic Regression. (John Wiley & Sons, 2013).
Freeman, E. A. & Moisen, G. PresenceAbsence: an R package for presence absence analysis. J. Stat. Softw. 23, 1–31 (2008).
Wickham, H. ggplot2. Wiley Interdiscip. Rev. Comput. Stat. 3, 180–185 (2011).
Efron, B. & Tibshirani, R. An Introduction to the Bootstrap. (CRC Press, 1994).
Steyerberg, E. W. et al. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J. Clin. Epidemiol. 54, 774–81 (2001).
Duarte, P. M. et al. Do subjects with aggressive and chronic periodontitis exhibit a different cytokine/chemokine profile in the gingival crevicular fluid? A systematic review. J. Periodontal Res. 50, 18–27, https://doi.org/10.1111/jre.12180 (2015).
Johnson, R. B., Wood, N. & Serio, F. G. Interleukin-11 and IL-17 and the pathogenesis of periodontal disease. J. Periodontol. 75, 37–43, https://doi.org/10.1902/jop.2004.75.1.37 (2004).
Ikezawa-Suzuki, I. et al. Effects of treatment on soluble tumour necrosis factor receptor type 1 and 2 in chronic periodontitis. J. Clin. Periodontol. 35, 961–8, https://doi.org/10.1111/j.1600-051X.2008.01317.x (2008).
Ikezawa, I. et al. Imbalance between soluble tumour necrosis factor receptors type 1 and 2 in chronic periodontitis. J. Clin. Periodontol. 32, 1047–54, https://doi.org/10.1111/j.1600-051X.2005.00832.x (2005).
Azman, R. et al. Clinical associations between IL-17 family cytokines and periodontitis and potential differential roles for IL-17A and IL-17E in periodontal immunity. Inflamm. Res. 63, 1001–12, https://doi.org/10.1007/s00011-014-0776-7 (2014).
Teles, R. P. et al. Relationships between subgingival microbiota and GCF biomarkers in generalized aggressive periodontitis. J. Clin. Periodontol. 37, 313–23, https://doi.org/10.1111/j.1600-051X.2010.01534.x (2010).
Oliveira, D. L. A. P. et al. Effects of periodontal therapy on GCF cytokines in generalized aggressive periodontitis subjects. J. Clin. Periodontol. 39, 295–302, https://doi.org/10.1111/j.1600-051X.2011.01817.x (2012).
Shaker, O. G. & Ghallab, N. A. IL-17 and IL-11 GCF levels in aggressive and chronic periodontitis patients: relation to PCR bacterial detection. Mediators Inflamm. 2012, 174764, https://doi.org/10.1155/2012/174764 (2012).
Yetkin, A. Z., Sütçü, R., Uskun, E., Bozkurt, F. Y. & Berker, E. The impact of the IL-11:IL-17 ratio on the chronic periodontitis pathogenesis: a preliminary report. Oral Dis. 15, 93–9, https://doi.org/10.1111/j.1601-0825.2008.01497.x (2009).
Stadler, A. F. et al. Gingival crevicular fluid levels of cytokines/chemokines in chronic periodontitis: a meta-analysis. J. Clin. Periodontol. 43, 727–745, https://doi.org/10.1111/jcpe.12557 (2016).
Ay, Z. Y. et al. The gingival crevicular fluid levels of interleukin-11 and interleukin-17 in patients with aggressive periodontitis. J. Periodontol. 83, 1425–31, https://doi.org/10.1902/jop.2012.110585 (2012).
Fine, D. H. et al. Macrophage inflammatory protein-1α shows predictive value as a risk marker for subjects and sites vulnerable to bone loss in a longitudinal model of aggressive periodontitis. PLoS One 9, e98541, https://doi.org/10.1371/journal.pone.0098541 (2014).
Johannsen, A., Susin, C. & Gustafsson, A. Smoking and inflammation: evidence for a synergistic role in chronic disease. Periodontol. 2000 64, 111–126, https://doi.org/10.1111/j.1600-0757.2012.00456.x (2014).
Kinane, D. F., Stathopoulou, P. G. & Papapanou, P. N. Periodontal diseases. Nat. Rev. Dis. Primers 3, 17038, https://doi.org/10.1038/nrdp.2017.38 (2017).
Acknowledgements
This work was supported by the Instituto de Salud Carlos III (General Division of Evaluation and Research Promotion, Madrid, Spain) and co-financed by FEDER (“A way of making Europe”) under Grant ISCIII/PI17/01722, and the Consellería de Cultura, Educación e Ordenación Universitaria da Xunta de Galicia (Spain) under Grant ED431B 2017/029 and A. Regueira-Iglesias support ED481A-2017. The funders had no role in the study’s design, data collection and analysis, the decision to publish, or the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
A.B.N., R.I.A., G.P.M.M., M.A. and T.I. participated in the recruitment and diagnosis of patients, the collection of oral samples, in reviewing the literature and writing the paper. A.S.M. participated in the quantification of cytokines in G.C.F. using multiplexed bead immunoassays and in the interpretation of the obtained results. B.C.C. participated in the development design of the models, in the internal validation analysis and the development of the graphics. All authors made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) the review and approval of the manuscript in its submitted form.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arias-Bujanda, N., Regueira-Iglesias, A., Alonso-Sampedro, M. et al. Cytokine Thresholds in Gingival Crevicular Fluid with Potential Diagnosis of Chronic Periodontitis Differentiating by Smoking Status. Sci Rep 8, 18003 (2018). https://doi.org/10.1038/s41598-018-35920-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-35920-4
This article is cited by
-
Oral biofluid levels of Activin-A and interleukin-1beta in stage III periodontitis
Clinical Oral Investigations (2024)
-
Gingival crevicular fluid galectin-3 and interleukin-1 beta levels in stage 3 periodontitis with grade B and C
Clinical Oral Investigations (2023)