Abstract
We aimed to compare the accuracy performance of the new 2018 periodontitis case definition by the European Federation of Periodontology (EFP)/ American Association of Periodontology (AAP) with Centers for Disease Control (CDC)/AAP 2012 in full-mouth partial recording protocols (PRP). Retrospective data from NHANES 2011-2012 and 2013-2014 were analyzed. For each case definition, full-mouth diagnostic was defined as the reference standard. Patients were diagnosed for the presence of periodontitis and staging for each PRP. Sensitivity, specificity, accuracy and precision, through several indicators, were determined. Performance measurement was assessed through binary and multiclass ROC/AUC analyses. Our performance analysis shows that the new 2018 classification outperforms the 2012 classification regarding the diagnosis and staging of periodontitis on full-mouth PRPs. This recent case definition has strengthened the utility of PRPs and its improvements certainly explain the observed findings. Also, our findings contribute to the reliability of PRPs and its use in future worldwide epidemiological surveys.
Similar content being viewed by others
Introduction
The constant pursuit of improved protocols on how periodontal diseases are diagnosed represents the disease complexity and a scientific community aiming for valid and accurate systems. In 2018, a world consensus from the European Federation of Periodontology (EFP) and the American Academy of Periodontology (AAP) provided a new classification of periodontal diseases1. This new classification revised unsettled points from previous classification2, showing a reliable capacity to reflect patients’ characteristics, disease evolution and tooth loss3.
In 2012, the Centers for Disease Control (CDC) with the AAP proposed a standard case definition for surveillance periodontitis based on measurements of periodontal probing depth (PPD) and clinical attachment loss (CAL) at interproximal sites4. Ever since this case definition has been widely accepted and applied both in epidemiological and clinical research. In the new 2018 classification, in addition to the interproximal sites, mid-buccal and mid-lingual sites were also considered5. Comprehensively, this addition reinforces this new classification with a potential improved ability to transmit the entire periodontal condition.
Furthermore, the 2012 and 2018 case definitions demand circumferential full-mouth inspection, which in large surveys and epidemiological studies it is often difficult to conduct, and time and labour intensive6,7,8. In this sense, several partial recording protocols (PRP) have been proposed for a full and partial mouth, though full-mouth PRPs present much less biasing potential6,9,10,11. Therefore, considering the improvements in the new 2018 case definition, it is reasonable to consider that it could contribute to more reliable and accurate PRPs using this diagnostic framework.
The present study aimed to compare how the new 2018 EFP/AAP classification performs in full-mouth PRPs for presence and staging of periodontitis, in comparison with the 2012 CDC/AAP.
Methods
Source of data and study population
NHANES 2011-2012 and 2013–2014 data were obtained through the CDC and Prevention National Center for Health Statistics (NCHS) website at https://www.cdc.gov/nchs/nhanes/index.htm. The present study was deemed exempt from review by the Egas Moniz Ethics Committee.
It focuses on participants who underwent periodontal health status evaluation. Oral health data collection protocols were approved by the CDC, NCHS Research Ethics Review Board, Atlanta (USA), and all participants gave written informed consent. All the examinations were conducted in a mobile examination centre. In these datasets, participants younger than 30 years of age were excluded due to reason explained elsewhere (see in detail in12). This study follows the Standards for Reporting of Diagnostic Accuracy Studies (STARD) statement13.
Eligibility criteria and periodontal examination
Exclusion criteria accounted for participants with medical exclusion from periodontal exam, non-complete periodontal status and edentulous. Periodontal examination consisted of a circumferential assessment of PPD and CAL around each tooth for all teeth. Third molars were excluded from the analysis.
Periodontitis case definition
For this study, we used the 2018 World Workshop EFP/AAP consensus5 and the 2012 CDC/AAP case definition4.
In the 2018 EFP/AAP case definition, a participant was a periodontitis case if: interdental CAL ≥ 2 non‐adjacent teeth, or Buccal or Oral CAL ≥ 3 mm with PPD > 3 mm is detectable at ≥2 teeth. Then, periodontitis staging was defined according to presence and stage5. For the staging, interdental CAL at the site of greatest loss of 1–2, 3–4 and ≥5 mm were considered as mild (stage 1), moderate (stage 2), and severe (stage 3 and stage 4), respectively5.
In the 2012 CDC/AAP case definition, a participant was a case of: Mild periodontitis − 2 or more interproximal sites with CAL ≥ 3 mm, and 2 or more interproximal sites with PPD ≥ 4 mm (not on the same tooth) or one site with PPD ≥ 5 mm; Moderate periodontitis − 2 or more interproximal sites with CAL ≥ 4 mm (not on the same tooth) or 2 or more interproximal sites with PPD ≥ 5 mm, also not on the same tooth); Severe periodontitis - the presence of 2 or more interproximal sites with CAL ≥ 6 mm (not on the same tooth) and 1 or more interproximal site(s) with PPD ≥ 5 mm; No periodontitis - no evidence of mild, moderate, or severe periodontitis4.
Full-mouth partial recording protocols
For this study, 6-sites PRPs selected were: 1) “Ramfjord teeth”14 on 6-site circumferential inspection (mesio-buccal [MB], mid-buccal [B], distal-buccal [DB], mesio-lingual [ML], mid-lingual [L], distal-lingual [DL]) – right maxillary first molar (16), left maxillary central incisor (21), left maxillary first premolar (24), left mandibular first molar (36), right mandibular central incisor (41) and right mandibular first premolar (44); 2) Community Periodontal Index of Treatment Needs (CPITN) teeth15 on 6-site circumferential inspection – right maxillary first and second molar (16,17), right maxillary central incisor (11), left maxillary first and second molar (26,27), left mandibular first and second molar (36,37), left mandibular central incisor (31) and right mandibular first and second molar (46,47). 3) MB–B measurements in all teeth; 4) MB–B–DB measurements in all teeth; 5) MB–B–DL measurements in all teeth. We decided to use these indexes based on the high bias (Ramfjord and CPITN) and low bias (MB-B, MB-B-DB, MB-B-DL) previously reported9,10,11.
Data management, test methods and analysis
Data were uploaded through SAS Universal Viewer for Windows and handled with Microsoft Office (MO) Excel. For each periodontal case definition, specific MO Excel datasets were derived in order to formulate appropriate algorithms.
In the performance analysis, full-mouth diagnosis was used as the standard reference for each case definition because it represents entirely the periodontal status. To test the index performance, we started by computing the final diagnosis into two variables according to the presence of disease (coded: 0-no, 1-yes) and the staging (coded: 0- non periodontitis, 1-mild, 2-moderate, 3-severe). Then, contingency tables were used to calculate true positive (TP), true negative (TN), false positive (FP) and false negative (FN) values. From this, sensitivity, specificity, accuracy and precision, through several indicators, were determined (Table 1)16. Also, Diagnostic Odds Ratio (DOR) and the respective standard error (SE) and 95% confidence interval (95% CI) were estimated. Performance measurement was assessed through binary and multiclass Area Under the Curve (AUC), through Receiver Operating Characteristics (ROC) analysis. For AUC/ROC analysis, we used the R package “plotROC”17 (by means of “roc” and “multiclass.roc” functions). The evolution of the periodontal status, from the 2012 CDC/AAP to the 2018 EFP/AAP case definition, was assessed through an alluvial diagram using https://app.rawgraphs.io/. Data were analysed as originally recorded, without missing data handling.
Results
Population
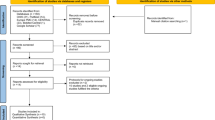
From an initial sample of 9,034 individuals, eligibility criteria were applied resulting in a final sample of 6,940 participants (Fig. 1). The baseline demographic, clinical characteristics of participants and distribution of severity of disease in the target condition were fully described elsewhere (for more details see12,18).
Accuracy performance for the presence of periodontitis
Regarding the presence of periodontitis, the 2018 case definition outperforms the sensitivity analyses of all PRPs, though the 2012 case definition presents excellent specificity results (Table 2). Because of the high specificity rates, the 2012 classification shows higher precision and DOR values. However, when looking for the remaining performance indexes, the 2018 classification clearly outperforms the 2012 one, in particular, the AUC values.
Accuracy performance for staging
Multiclass ROC analyses, through AUC values, show that 2018 EFP/AAP outperforms 2012 CDC/AAP in all PRPs (Table 3). In terms of precision, 2012 CDC/AAP has excellent predictive values for non periodontitis patients and very low values for mild periodontitis patients. The 2018 EFP/AAP improved the precision for mild periodontitis patients in all PRPs, though for moderate and severe cases the results are similar to the 2012 CDC/AAP. Interestingly, the 2018 case definition has improved remarkably the precision performance of Ramfjord and CPITN teeth.
Comparison of classifications
We further assessed how patients classified according to the 2012 classification were re‐classified in the 2018 classification (Fig. 2). Most patients with periodontitis were re‐classified in non periodontitis cases. Mostly, moderate and mild periodontitis patients were re-classified as non periodontitis. Also, a set of non periodontitis patients had their status updated to periodontitis, and several patients had their severity downgraded or even diagnosed as non periodontitis.
Discussion
In our investigation, we hypothesized that the 2018 EFP/AAP periodontal classification could improve the performance on PRPs comparing to the 2012 CDC/AAP classification. To examine this hypothesis, we compiled a significant dataset from the NHANES between 2011 and 2014 and we performed several diagnostic performance indicators in a comparative analysis. Our results confirmed that the new 2018 classification outperforms the 2012 classification regarding the diagnosis of periodontitis and its staging on full-mouth PRPs.
Our findings have significant wide implications. (1) From a perspective of population-based surveillance of periodontitis, the 2018 case definition has strengthened the utility of PRPs comparing to the 2012 classification. (2) The 2012 case definition has excellent specificity properties. (3) The comparison of classifications provided interesting re-classification findings. (4) Considering the challenges of performing full-mouth protocols in large studies, the 2018 EFP/AAP classification on full-mouth PRPs might contribute to enhance the number of population-based surveillance studies on periodontal diseases.
The inclusion of central surfaces (mid-buccal and mid-lingual sites) in the 2018 case definition1,5 has endowed it with a holistic view of the periodontal situation. In other words, by considering all circumferential sites we increase the likelihood of correctly diagnosing periodontitis, rather than the 2012 classification that only uses interproximal locations (maximum of four sites). Moreover, both case definitions evidenced cases whose final diagnosis did not coincide, with several periodontitis patients in the 2012 classification being re-classified as non periodontitis patients in the 2018 case definition.
On the one hand, the new 2018 EFP/AAP case definition is a reliable tool in depicting patients’ characteristics, disease progression and tooth loss3. On the other hand, our findings emphasize its reliability on future epidemiological studies using PRPs, considering that more surveys are warranted to improve surveillance of periodontitis, a pandemic disease with worldwide prevalence and worrisome socio-economic impact19,20,21,22,23,24.
A periodontal diseases surveillance system has intrinsic limitations, in particular, time, number of examiners and complexity of the measurement tool25. Therefore, we consider relevant to seek reliable alternatives with current case definitions for the purpose of minimizing these limitations. Regarding the complexity of the measurement strategy, the challenge of the number of teeth and sites to be examined were addressed through the tested indexes. In indexes with a lower number of teeth, the current 2018 case definition endowed CPITN has a more reliable tool in both detecting and staging periodontitis, comparing to the 2012 scenario. For the “Ramfjord teeth”, the 2018 classification provided slight surveillance improvements, though it was the index with less favorable performance. While the indexes with all teeth but with a lower number of sites, the MB-B-DL and MB-B-DB sites had very pleasant results for both diagnosis and staging of periodontitis, unlike the MB-B sites. Interestingly, these results are in agreement with past studies on previous case definitions showing the bias potential of “Ramfjord teeth” and MB-B approaches to estimate the prevalence of periodontitis9,10,11. Besides, several studies have shown excellent predictive results of MB-B-DL and MB-B-DB for PD and CAL periodontal measures6,9,11. A possible explanation for the better performance of these three-sites approaches relies on the fact that they encompass the interproximal sites and one central face of all teeth, which provides them with a more comprehensive surveillance ability. However, a possible shortcoming of these three-sites indexes is that we only reduce the periodontal inspection by the halved, though from the epidemiological perspective can be very significative. Henceforth, these full-mouth three-sites PRPs might be of high epidemiological relevance, considering the requirements of the surveillance surveys in periodontal diseases26.
To the best of our knowledge, this is the first study examining the performance of the new 2018 classification on PRPs and its epidemiological potential. Previously, data from the NHANES 2009–2010 was used to test several full-mouth and half-mouth PRPs performance on 2012 CDC/AAP case definition6,10. Due to the fact that the 2012 classification only accounts for interproximal sites,the authors did not include central surfaces, hence, these results are not comparable to our findings. Similarly to our results, MB-DB and MB-DL presented the most promising results10.
This study has strengths and limitations worth mentioning. In contrast to NHANES III that used half-mouth data6, full-mouth values were provided minimizing the underestimation of periodontitis in these patients. Also, the dataset is originated from a very significant national health survey, with substantial representativeness and generalizability. Furthermore, measures of interest were assessed by trained and calibrated examiners and the most up-to-date definitions of periodontitis were used making these results current and of high scientific interest, though having multiple examiners may result in variability in the analysis and determination of the stage. Nevertheless, despite AUC, there is high variability of performance indicators that may contribute to less certainty in the interpretation of the results. Additionally, these indicators were developed for less complex clinical diagnostic tests and multiclass assessment on staging accuracy has limited analyses available. Also, we were unable to assess how the disease level influences PRP performance, though this was already reported27. From these results, the advantages of applying this case definition on full-mouth PRPs might be the decrease of time and effort invested in diagnosing large representative samples. In particular, the MB-B-DL approach seems to be the PRP with the most potential for prevalence and staging purposes. Interestingly, there apparent a low difference in the therapeutic attitude according to the staging with the new classification compared to the old one, though this was recently addressed ().Future studies should investigate the impact of employing this type of PRPs on epidemiologic settings and how the variation of disease prevalence could affect the performance of such indexes.
Conclusion
The new 2018 classification outperforms the 2012 classification regarding the diagnosis and staging of periodontitis on full-mouth PRPs. This recent case definition has strengthened the utility of PRPs and its improvements certainly explain the observed findings. Also, our findings contribute to the reliability of PRPs and its use in future epidemiological surveys.
Data availability
References
Caton, G. J. et al. A new classification scheme for periodontal and peri-implant diseases and conditions – Introduction and key changes from the 1999 classification. J. Clin. Periodontol. 45, S1–S8 (2018).
Armitage, G. Development of a Classification System for Periodontal Diseases and Conditions. Ann. Periodontol. 4, 1–6 (1999).
Graetz, C. et al. Comparison of periodontitis patients’ classification in the 2018 versus 1999 classification. J. Clin. Periodontol. 46, 908–917 (2019).
Eke, P. I., Page, R. C., Wei, L., Thornton-Evans, G. & Genco, R. J. Update of the Case Definitions for Population-Based Surveillance of Periodontitis. J. Periodontol. 83, 1449–1454 (2012).
Tonetti, M. S., Greenwell, H. & Kornman, K. S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Periodontol. 45, S149–S161 (2018).
Kingman, A., Susin, C. & Albandar, J. M. Effect of partial recording protocols on severity estimates of periodontal disease. J. Clin. Periodontol. 35, 659–667 (2008).
Kingman, A. & Albandar, J. Methodological aspects of epidemiological studies of periodontal disease. Periodontol. 2000 29, 11–30 (2002).
Susin, C., Kingman, A. & Albandar, J. M. Effect of Partial Recording Protocols on Estimates of Prevalence of Periodontal Disease. J. Periodontol. 76, 262–267 (2005).
Tran, D. T. et al. Assessing periodontitis in populations: A systematic review of the validity of partial-mouth examination protocols. J. Clin. Periodontol. 40, 1064–1071 (2013).
Tran, D. T. et al. Assessment of partial-mouth periodontal examination protocols for periodontitis surveillance. J. Clin. Periodontol. 41, 846–852 (2014).
Machado, V. et al. Partial recording protocols performance on the assessment of periodontitis severity and extent: Bias magnitudes, sensibility, and specificity. Rev. Port. Estomatol. Med. Dent. e Cir. Maxilofac. 59, 145–153 (2018).
Eke, P. I. et al. Update on Prevalence of Periodontitis in Adults in the United States: NHANES 2009 − 2012. J. Periodontol. 1–18. https://doi.org/10.1902/jop.2015.140520 (2015)
Bossuyt, P. M. et al. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. BMJ 351, 1–9 (2015).
Ramfjord, S. P. Indices for Prevalence and Incidence of Periodontal Disease. J. Periodontol. 30, 51–59 (1959).
Baelum, V., Fejerskov, O., Manji, F. & Wanzala, P. Influence of CPITN partial recordings on estimates of prevalence and severity of various periodontal conditions in adults. Community Dent. Oral Epidemiol. 21, 354–359 (1993).
Glas, A. S., Lijmer, J. G., Prins, M. H., Bonsel, G. J. & Bossuyt, P. M. M. The diagnostic odds ratio: A single indicator of test performance. J. Clin. Epidemiol. 56, 1129–1135 (2003).
Sachs, M. C. Plotroc: A tool for plotting ROC curves. J. Stat. Softw. 79, 1–19 (2017).
Beydoun, H. A. et al. Periodontal disease, sleep duration, and white blood cell markers in the 2009 to 2014 National Health and Nutrition Examination Surveys. J. Periodontol. 1–14. https://doi.org/10.1002/jper.19-0055 (2019)
Tonetti, M. S., Jepsen, S., Jin, L. & Otomo-Corgel, J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J. Clin. Periodontol. 44, 456–462 (2017).
Kassebaum, N. J. et al. Global Burden of Severe Tooth Loss: A Systematic Review and Meta-analysis. J. Dent. Res. 93, 20S–28S (2014).
Richards, D. et al. Review finds that severe periodontitis affects 11% of the world population. Evid. Based. Dent. 15, 70–71 (2014).
Petersen, P. E. & Ogawa, H. The global burden of periodontal disease: Towards integration with chronic disease prevention and control. Periodontol. 2000. 60, 15–39 (2012).
Pihlstrom, B. L., Michalowicz, B. S. & Johnson, N. W. Periodontal diseases. Lancet 366, 1809–1820 (2005).
Chapple, I. L. C. et al. Primary prevention of periodontitis: Managing gingivitis. J. Clin. Periodontol. 42, S71–S76 (2015).
Beltrán-Aguilar, E. D., Malvitz, D. M., Lockwood, S. A., Rozier, R. G. & Tomar, S. L. Oral health surveillance: past, present, and future challenges. J. Public Health Dent. 63, 141–149 (2003).
Beltrán-Aguilar, E. D., Eke, P. I., Thornton-Evans, G. & Petersen, P. E. Recording and surveillance systems for periodontal diseases. Periodontol. 2000 60, 40–53 (2012).
Kingman, A., Morrison, E., Löe, H. & Smith, J. Systematic errors in estimating prevalence and severity of periodontal disease. J. Periodontol. 59, 707–713 (1988).
Acknowledgements
We declare that the authors have no competing interests as defined by Nature Research, or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Author information
Authors and Affiliations
Contributions
João Botelho, Vanessa Machado and Luís Proença have conceived the project, conducted data analysis, interpreted data and wrote the manuscript. José João Mendes has interpreted data and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Botelho, J., Machado, V., Proença, L. et al. The 2018 periodontitis case definition improves accuracy performance of full-mouth partial diagnostic protocols. Sci Rep 10, 7093 (2020). https://doi.org/10.1038/s41598-020-63700-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-020-63700-6
This article is cited by
-
Association between cardiometabolic index (CMI) and periodontitis in US adults: analysis of NHANES data (2009–2014)
BMC Oral Health (2024)
-
Hepatitis B infection is associated with periodontitis: the national health and nutrition examination survey (2009–2014)
BMC Oral Health (2024)
-
Association between brominated flame retardants (BFRs) and periodontitis: Results from a large population-based study
BMC Oral Health (2024)
-
The PocketPerio application significantly increases the accuracy of diagnosing periodontal conditions in didactic and chairside settings
Scientific Reports (2024)
-
Association between muscle quality index and periodontal disease among American adults aged ≥ 30 years: a cross-sectional study and mediation analysis
BMC Oral Health (2023)