Abstract
New Onset Diabetes After Transplantation (NODAT) is a serious metabolic complication. While β-cell dysfunction is considered the main contributing factor in the development of NODAT, the precise pathogenesis is not well understood. Cytokines are thought to be involved in the inflammation of islet β-cells in diabetes; however, few studies have investigated this hypothesis in NODAT. A total of 309 kidney transplant recipients (KTRs) were included in this study. An association between kidney transplants, and the development of diabetes after transplant (NODAT) was investigated. Comparison was made between KTRs who develop diabetes (NODAT cases) or did not develop diabetes (control), using key cytokines, IL-6 G (− 174)C, macrophage mediator; IL-4 C (− 490)T, T helper (Th)-2 cytokine profile initiator; Th-1 cytokine profile initiator interferon-γ T (+ 874) A gene and TGF β1 C (+ 869) T gene polymorphisms were investigated. The genes were amplified using well-established polymerase chain reaction (PCR) techniques in our laboratory. Compared to the AA and AT genotypes of interferon gamma (IFNG), there was a strong association between the TT genotype of IFNG and NODAT kidney transplant recipients (KTRs) versus non-NODAT KTRs (p = 0.005). The AA genotype of IFNG was found to be predominant in the control group (p = 0.004). Also, significant variations of IL6 G (− 174) C, IL-4 C (− 590) T, interferon-γ T (+ 874) A gene and transforming growth factor β1 C (+ 869) T may contribute to NODAT. Our data is consistent with theTh-1/T-reg pathway of immunity. Further larger pan Arab studies are required to confirm our findings.
Similar content being viewed by others
Introduction
New Onset Diabetes After Transplantation (NODAT) is a serious and common complication following organ transplantation. It is a frustratingly complex disease that is associated with increased mortality and morbidity possibly due to high rates of cardiovascular disease and infection. These factors are the leading causes of death in kidney transplant recipients (KTRs)1,2. The rate of NODAT varies depending on the age and ethnicity of patients at the time of transplant. Also, the usage of immunosuppressive agents plays a role in the development of NODAT3. NODAT is diagnosed typically between three months to one-year post-transplant, when transplant recipients are receiving a stable maintenance dose of immunosuppressive drugs, are free from infection, and have stable graft function1,2,3. Different studies have reported variable rates of NODAT ranging from 2 to 53%4. NODAT was reported to occur in 4–25% of KTRs5,6,7, and is more commonly manifested in African- Americans and Hispanics in comparison to Caucasians and Asians8. Information about NODAT in the Arab populations is scarce, with the exception of few epidemiologic studies9,10,11 suggesting that 25–30% of KTRs eventually develop NODAT9,10,11,12. Specifically, the incidence rate of NODAT, following kidney transplantation, has been found in to be as high as 27% in Saudi Arabia9, 30% in Bahrain10, 22.2% in Egypt11, and 25.6% in Kuwait12,13.
Genetic predisposition to NODAT likely involves an inherited defect in the peripheral tolerance to T-cell infiltration along with inadequate insulin secretion14,15,16. There is clear evidence showing that the different stages of NODAT are discrete entities, and that progression from one stage to the next is dependent on immune regulation16. T-cells are important for orchestrating the immune response and can be categorized into subsets according to their phenotypic characteristics resulting from polarization of naïve T-cells (i.e. Th-1, Th-2 and regulatory T-cell; T-reg)17,18,19. Each T-cell subset has a unique functional role highlighted by their capacity to produce pro-inflammatory and anti-inflammatory cytokines in response to various immune challenges. Cytokines are a group of pharmacologically active polypeptides that possess autocrine, paracrine, and juxtacrine effects with characteristic features19. Given the critical role of cytokines in regulating immune responses, subtle differences in cytokine expression may have a major effect on the outcomes of those responses20. Single nucleotide polymorphisms (SNP) in the regulatory region of the cytokine genes have been shown to correlate with individual variations in cytokine production9,10,11,12,13,14,15,16,17,18,19,20,21,22,23. Thus, variations in susceptibility to NODAT may be influenced by inter-individual genetic variations of cytokine genes19,20,21,22,23. Research on the association of SNPs have now become a potential means not only for better understanding the etiopathogenesis of the disease, but also as a probable marker for disease susceptibility and severity. It has been shown that interleukin-6(IL-6) derived from macrophages play a key role in inflammation19,24. This process is regulated via two major arms of the immune system: intra-cellular suppressor of cytokine signaling (SOCS) and T-reg cells25.
IL-6 gene (Online Mendelian Inheritance in Man #147620) maps to chromosome 7p2126. IL-6 a glycoprotein composed of 212 amino acids with a signal peptide of 27 amino acids and two potential NH2-linked glycosylation sites26. The molecular weight ranges from 21 to 28 kDa. IL-6 is a key cytokine with pleiotropic interactions in different human diseases pathogenesis19. IL-6 activates the immune system and enhances inflammatory response but also carries anti-inflammatory properties27. Understanding such pleiotropic effects of IL-6 in in the pathogenesis of the disease may help determine the progression, severity and duration of the disease. IL-6 is currently considered an important target for clinical interventions28,29. Hence, better understanding of IL-6 role in the pathogenesis of NODAT can provide rational and therapeutic intervention29. The guanine (G)/cytosine (C) polymorphism in the IL-6 proximal promoter region, at position IL-6 G (− 174) C, regulates transcription of the IL-6 gene and subsequently in IL-6 levels of plasma and serum19,30; the same polymorphism was found to be associated with fasting insulin levels,insulin sensitivity, and the integrated area under the curve of serum glucose concentrations30,31.
Interferon-gamma (IFN-γ), also known as type II interferon or macrophage-activating factor32, is a multipotent cytokine with an approximate molecular weight of 17 kDa. IFN-γ is secreted by activated T-cells and natural killer cells (NK), and it modulates many facets of the hosts immune response33. It enhances the hosts defense and innate immune response through promoting inflammation via the JAK-STAT1 signaling pathway and inhibiting both interleukin (IL)-4 (the initiator of the Th-2 cytokine cascade) and the promoter of the Th-1 cytokine profile22. TheDNA sequence of the human IFN‐γ gene (GenBank AF330164) shows the presence of a variable‐length CA repeat in the first intron of the gene where allele 2 (12 CA repeats) produces a high level of IFN‐γ protein18. This sequence is immediately adjacent and correlated with allele T for thiamine of the polymorphism at position + 87434. It is well established that the IFN-γ gene polymorphism T (+ 874) A (IFNG) of the first intron is correlated with serum level of IFN-γ production and mRNA expression in vitro and in vivo; the TT genotype correlates with high levels of IFN-γ production, and TA and AA are correlated with intermediate and low production level18,22,34,35,36,37,38. This polymorphism coincides with a putative NF-κB binding site that may mediate high production of IFN-γ39,40. Importantly, IFN-γ is believed to play an important role in the autoimmune pathogenesis of type 1 diabetes22,41. Inhibition of the IFN-γ function in non-obese diabetic (NOD) mice using either IFN-γ-specific antibodies42 or soluble IFN-γ receptors (IFN-γ-R)43 reduced the incidence of spontaneous diabetes and also prevented the transfer of diabetes via splenocytes from NOD donor mice44. Furthermore, transgenic expression of IFN-γ by β-cells induced autoimmunity, resulting in overt diabetes in otherwise diabetes-resistant mice44. The resistance of IFN-γ-R deficient animals to CD4+ T-cell mediated diabetes was shown to be primarily due to a lack of IFN-γ-R expression by β-cells. Kuriya et al. demonstrated that IFN-γ-R deficiency has distinct effects on CD4+ compared with CD8+ T-cell mediated diabetes, and that IFN-γ may play a critical role in CD4+ T-cell mediated destruction of β-cells45.
IL-4 is a 20-KDa glycoprotein encoded by the IL-4 gene on chromosome 5q23.31. It is secreted by helper T-cells (CD4) type 2 (Th-2), by NK cells, and by cells of the innate immune system: mast cells, basophils, and eosinophils46. IL-4 regulates proliferation, apoptosis, gene expression, and differentiation in many hematopoietic cells; it directs the immunoglobulin (Ig0) class switch to IgG1 and IgE, downregulates the production of Th-1 cells and is a critical mediator of the Th 1/ Th-2 cytokine milieu counterbalance22,46. IL-4 appears to protect human islets from cytotoxic damage induced by proinflammatory and Th-1 cytokines. Another study showed that long-term exposure of rat pancreatic islets to IL-4 resulted in an inhibitory action to certain islet functions47. These phenomena occur by the modulation of the homing of autoreactive cells to inflammatory sites and the stabilization of a protective Th-2-mediated environment in the thymus, spleen, and pancreatic islets. Thus, IL-4 treatment favors the expansion of regulatory CD4+ Th-2 cells in vivo and prevents the onset of insulitis and type 1 diabetes mediated by autoreactive Th-1 cells22,48. It has been suggested that IL-4 protects human islets from cytotoxic damage induced by proinflammatory and Th-1 cytokines. The local expression of IL-4 in the pancreatic islets of NOD mice (ins-IL-4 mice) restricted the activation of autoreactive T-cells and promoted complete protection against spontaneous diabetes49. IL-4 T (− 590) C, rs2243250, is a functional promoter of gene polymorphism, where C is substituted by T22. It is well established that TT genotype of IL-4 T (− 590) C corresponds to high level of IL-4 serum and mRNA production in vivo as well as in vitro. The same is true for IL-4 C (− 590) C for low levels, and TC for putative intermediate protein levels22,50.
Transforming growth factor-β1 (TGF-β1) belongs to a family of multifunctional growth factors which have profound regulatory effects on many developmental and physiological processes51.The human TGF-β1 gene is located on chromosome 19q13.1–13.352, and more than ten polymorphic loci are presently known that are distributed across exons, introns, and the 5′flanking region53. A single nucleotide polymorphism (SNP) of codon 10 in the TGF-β1 T (+ 869) C gene(TFGB), T (proline) to C (leucine) is associated with different diseases including type 1 and type 2 diabetes54. There is well-established evidence regarding the association of codon 10 with varying levels of TGF-β1 synthesis in vitro and in vivo23. Increases or decreases in the production of TGF-β1 have been linked to numerous diseases including atherosclerosis, and fibrotic diseases of the kidney, liver, and lung23.
There is increasing evidence to show that SOCS proteins may be involved in the development of diabetes and its associated complications55. In addition, SOCS-modulating properties have been attributed to pharmacological agents that are currently used for the treatment of diabetes56.
Our results indicate that susceptibility to NODAT might be monitored by genotyping KTRs who developed diabetes compared with KTRs who did not develop diabetes for selected major Th 1(IFNG)/ Th-2 (IL-4)/TGFB, T-reg in addition to IL-6, macrophage derived cytokines. We have investigated well-established SNPs in major cytokines, according to their site of origin, in order to identify our future line of research.
Materials and methods
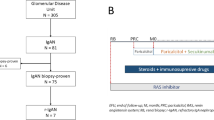
This piece of research was conducted following written approval from Dasman Diabetes Institute Research and Ethical Committee reference: RA 2015-013. Oral and written informed consent was obtained from all participants prior to data collection. The methods were performed in accordance with the relevant rules and regulations. This work was conducted in collaboration between Dasman Diabetes Institute and Hamed Al-Essa Organ Transplant Center of Kuwait. KTRs with NODAT and non-NODAT were recruited from May 2015 until March 2017. A total of 309 KTRs were recruited: 155 patients in the non-diabetic, non-NODAT cohort and 154 patients who developed NODAT following kidney transplantation (Table 1).
Genomic DNA was extracted from a 5 ml sample of fresh peripheral blood using the QIAamp DNA Mini Kit (QIAGEN) according to the manufacturer’s instructions. Extracted DNA sample had a final concentration of 55–365 ng/ml, and samples were stored at −20°C prior to use. Allele-specific sequence primers were used to amplify IL-6G, IFNG, IL4G and TGFG using well-established techniques available in our laboratories (Table 2)22, and PCR products were separated on a 2% agarose gel. To ensure the quality of the experiments, 10% of all samples were genotyped twice, producing 100% reproducibility.
Diagnosis of NODAT
All kidney transplant recipients were screened for fasting plasma glucose and glycated hemoglobin, according to Kidney Disease: Improving Global Outcomes (KDIGO) guidelines57. Abnormal results were confirmed using an oral glucose tolerance test. In these cases, diabetes management was introduced immediately that included diet, exercise, oral agents and/or insulin, in addition to regular blood glucose monitoring at home.
Immunosuppression protocol
The immunosuppression protocol consisted of five doses of anti-thymocyte globulin (Sanofi US, Bridgewater, NJ, USA) for high-risk patients (re-transplants, prior pregnancy, blood transfusion, HLA-antibody positive, and/or more than four HLA mismatches), or two doses of IL-2 receptor blocker (Basiliximab, Novartis, Inc., Switzerland) for low-risk patients. Maintenance therapy consisted of prednisolone, mycophenolic acid, and a calcineurin inhibitor (CNI). The dose of CNI was gradually decreased over 12 months guided by a 12-h trough level.
Acute cellular rejection was treated using intravenous methylprednisolone sodium succinate (solumedrol, 1 g daily for 3 days) or thymoglobulin (1 mg/kg for 7–10 days) for steroid-resistant rejection. Antibody-mediated rejection was treated using plasma exchange, intravenous immunoglobulin (2 g/kg), and rituximab. All rejection episodes were biopsy-proven according to the Banff criteria (2015)58. Patients who received thymoglobulin as anti-rejection therapy were managed by universal chemoprophylaxis for both cytomegalovirus (CMV) and Pneumocystis Jirovecii Pneumonia (PJP). Valganciclovir was used as CMV secondary prophylaxis for one month, while those who developed CMV viremia during this period were managed with a therapeutic dose for three weeks, followed by three months prophylaxis. Trimethoprim was used for one month as a prophylaxis for PJP. Associated infections were recorded if patients required hospital admission. Details of the patients who developed CMV infection or rejection episodes during the study period were recorded. Clinical data were collected with special emphasis on patient age, sex, donor type, immunosuppressive therapy, dialysis type and duration, primary kidney disease, pretransplant comorbidities, details of rejection episodes, post-transplant infections and graft and patient outcome.
Statistical analysis
The Hardy–Weinberg equilibrium was assessed using a chi-square test based on a comparison of the observed and expected genotypes. Statistical analyses were performed using SPSS software (SPSS, version 20.0, IBM Corporation, Armonk, NY, USA). The sample size was calculated to accept a marginal error of 6.6% (95% confidence interval) in a normally-distributed population. Allelic and genotypic distribution of IL6G, IFNG, IL-4G and TGFBG between both cohorts were compared using a paired-sample t-test, independent sample t-test, chi-square test, Fisher’s exact test, and ANOVA, as appropriate. Results are expressed as mean ± standard deviation, and differences were considered significant at p < 0.05.
Results
Phenotypic features
The participants age ranged between 20 and 80 years, the mean age for recipients who developed NODAT was 52.85 ± 11.4 years compared to 38.97 ± 13.1years in the control group. Younger patients(<40years) were more prevalent in the control group, while patients older than 40 years were predominant in NODAT, p < 0.0001. All patients received grafts from donors aged 30–40 years. The mean donor age was 34.4 ± 9.1 in cases versus 34.7 ± 8.8 for controls (Table 1). We noticed that the two groups were homogenous in variability of original kidney disease, dialysis type, donor type, and type of immunosuppression (both induction and maintenance). As well as that, all subjects had no history of diabetes as demonstrated by normal fasting and postprandial blood glucose levels prior to transplantation.
There were no differences in ethnicity of our cohorts, 55% Kuwaiti, 45% non-Kuwaiti (Table 3). Moreover, no statistically significant differences were noticed in pre-transplant comorbidities in both cohorts, especially hypertension, history tuberculosis treatment, ischemic heart disease, bone disease, anemia, and hyperlipidemia, HLA class 1 -A and -B and class II DR, p > 0.05, Table 3. There was a significantly higher prevalence of patients with chronic hepatitis C virus (HCV) infection in NODAT (12 cases in NODAT compared to two cases in control, p = 0.006, Table 3). In addition, there were significantly more CMV IgG positive patients for in NODAT than control (153 vs. 148, respectively; p = 0.02). However, the two groups were comparable regarding pre transplant CMV IgM (p > 0.05). Evaluation of immediate post-transplant graft function showed that the number of patients with slow graft function was significantly higher in control (p = 0.03). Overweight, as measured by mean basal body mass index (BMI), was significantly higher in the NODAT group compared to the control group (28.07 ± 5.5 vs. 26.11 ± 7, respectively; p = 0.01), while follow-up mean BMI was comparable in both cohorts irrespective of age, p = 0.21, see (Table 3).
The number of cases with post-transplant CMV viremia was significantly higher in control compared to NODAT (p = 0.01, Table 4). Moreover, there was no significant difference between NODAT and control groups regarding both graft and patient outcome (p > 0.05).
Frequencies of cytokine genotypes according to protein production
Patients with of IL-6(CC), IFN-G (AA), and TGF-B (CC), corresponding to low protein production, were significantly higher in control (p = 0.05, p = 0.01, and p = 0.001, respectively, Fig. 1). IL-6(GG), IFN-G (TT), and TGF-B (TT) genotypes, correlating to high protein production, were significantly higher in NODAT (p = 0.05, p = 0.003 and p = 0.002, respectively). On the other hand, patients with IL-4 genotype (TT) that correspond to high IL-4 production were significantly higher in the control group while the low producers were significantly higher in NODAT, p = 0.001.
Genotypic frequencies of cytokines in NODAT and controls. Genotypes of cytokines are illustrated as homozygote (corresponded to high protein producer), heterozygote (corresponded to intermediate protein producer) and homozygote (corresponded to low protein producer). IL-6, IFNG and TGFB high producer genotypes were strongly associated with the disease, p = 0.05, 0.01 and 0.007; while, IL-4 high producer corresponded genotype was strongly associated with control cases, p = 0.001. In all cytokines intermediate protein level genotype did not show any significant association. Low protein producer corresponded genotypes were strongly associated with control group in IL-6, IFNG and TGFB, p = 0.05, 0.003 and 0.002; while, low protein level corresponded genotype in IL-4 was significantly associated with the disease, p = 0.001.
Frequencies of cytokine genotypes and virology
Genotype frequencies of IL-6(CG), IL-4(TC) and IFNG (AA, AT) were found to be significantly more prevalent among HCV positive patients in NODAT group (p = 0.013, p = 0.006, p = 0.05 and p = 0.007 respectively, Table 4). Genotype frequencies of IL-6(GG), IL-4(TC), TGF-B(TC) were found to be significantly more prevalent amongst patients with post-transplant CMV viremia in the control group (p = 0.02, p = 0.009 and p = 0.02 respectively, Table 4). Importantly, no significant association was noticed with IFNG genotypes, Table 4.
Age specificity and genotypic frequency
The allelic distribution of the IL-6, IL-4, IFNG and TGFB among both studied cohorts were significant, p = 0.006, p < 0.0001, p = 0.0002 and p < 0.0001 (Fig. 2) however, these effects were only observed when the alleles were paired in genotypes.
Genotype frequencies of IL-6, IL-4, IFNG and TGFB did not show any statistical gender specificity among NODAT versus control. IL-6 GG gene frequency was predominant in control participants < 40 years of age, p < 0.0001, while it was most frequent in patients 40-60 years of age in the NODAT group, p = 0.02. Although its distribution was greater in patients > 60 years of age in the NODAT group, this data did not rank to significance, p = 0.06 (Table 5). IL-6 GC was predominantly more frequent in control patients > 40 years of age versus NODAT, p=0.003 (Table 5), while its frequency was shifted towards NODAT in patients > 60 years of age, p = 0.002. The same was true for IL-6 CC genotype distribution. Its frequency was more in the controls among > 40 years of age patients, p = 0.0001, and significantly increased in > 60 years of age NODATs, p = 0.005, Table 5. IL-4 TT was more abundant in the controls among patients < 40 years of age when compared to NODAT, p = 0.01. However, TT distribution was comparable in 40-60 years of age groups. No statistically significant results were found between control and NODAT in the > 60 years of age group and this is likely due to the small number of cases, Table 4.
Likewise, IL-4 TC was more frequent among older participants than 40 years in control, p < 0.0001, while its distribution was shifted in older age groups towards NODAT, p = 0.04, (among 40–60 years of age) and p < 0.0001 among > 60 years of age, Table 5. FNG AA, AT, TT was more dominant in controls less than 40 years, p = 0.0002, p < 0.0001, p < 0.0001 respectively. Its genotype frequencies were shifted towards NODAT in 40–60 years of age groups, p = 0.04, 0.01, 0.04 respectively (Table 5). In the same order, the genotype distributions of IFNG were predominantly more in NODAT than the control with > 60 years of age, p = 0.02, p = 0.02, p = 0.009 respectively (Table 5).
The distribution of TGFB followed almost the same pattern as IFNG. The distribution of all genotypes were predominantly more in control among those older than 40 years, p < 0.0001, p = 0.001, p < 0.0001. The distributions were shifted towards dominance in NODAT among older age groups, p = 0.03, p = 0.4, p = 0.0007 in 40–60 years of age and p = 0.002, p = 0.001and p = 0.03 among > 60 years of age groups (Table 5). The frequency of the above cytokines was investigated according to their HLA class I -A and -B and class II DR but no statistical association was noted.
Discussion
The presence of NODAT has increasingly emerged as an important factor in the long-term outcome of KTRs, including mortality59. In the current study, the patient demographics of NODAT and control cohorts were indistinguishable. There were more males than females in both cohorts. This was similar to several other studies which reported that organ-recipients were mainly males. It is possible this reflects a gender bias in the incidence of transplant-related pathologies60,61. However, some differences were noted, patients with chronic HCV and CMV infections were significantly more prevalent amongst the NODAT group. Furthermore, in our study, age appears to be an important contributing factor in the development of NODAT. More KTRs < 40 years of age were found in the control group, while those > 40 years of age were more susceptible to NODAT. These findings are in line with several reports from Europe and the USA1,2,3,62,63. There was a 90% increase of relative risk in kidney transplant patients aged 45–59 years and a 160% increase in patients older than 60 years compared to patients between 18–44 years old63. However, our data did not support findings concluded from studies from Egypt, Bahrain, Saudi Arabia, and Iran9,10,11,64. This could be explained by transracial differences or a lack of large systematic studies.
Associations of IL6 GG, IL-4 CC, IFNG TT and TGFB TT genotypes were superseded by age group and bio-physiology of patients. This might confirm identified differences in innate immune system in older KTRs compared to younger ones65.
Interestingly, patients with IL-6(GG), IFN-G (TT), and TGFB (TT) genotypes, which were associated with high protein production, were significantly higher in the NODAT cohort. While, IL-4(CC), related to low protein production, was significantly associated with the disease. On the contrary, HCV infection has been shown to be associated with IFNG and the development of type 2 diabetes mellitus in general population66.
Previous studies have suggested that asymptomatic CMV infection and CMV disease are independently associated with the development of NODAT67, while other studies reported that CMV was not a risk factor for NODAT62,63,68. In pretransplant evaluation we found a significantly higher number of patients with positive CMV IgG in NODAT cohort, while CMV IgM was comparable between both cohorts. Interestingly, there were significantly more patients with post-transplantation CMV viremia in control cohort, especially among IL-6 (GG), IL-4 (TC) and TGFB (TC), but no statistical association was found between IFNG and CMV in either cohorts. This could be explained by the use of routine antiviral chemoprophylaxis among our patients after transplant which nullified CMV as a risk for NODAT in our cohort. The significant association of genetic polymorphisms in IL-6, IFNG, TGFB in NODAT could be due to Th1 mediated immunity which occurs as a result of deviation of SOCS/T-reg Fox P3 balance. Our results support a previously reported deviation in SOCS/T-reg Fox P3 balance causing immune dysregulation by IFN-γ. The association of IL-6 (GG), IFNG (TT) and TGFB (TT) high protein producers and IL4 (CC), low IL-4 protein producer might go some way to explain these findings.
KTRs gender did not appear to effect genetic susceptibility of either IL-6 G (− 147) C, IL-4 C (− 590) T, IFNG, and TGFB genotypes. However, there was a clear association with age and the distribution of IL-6 G (− 147) C, IL-4 C (− 590) T, IFNG, and TGFB genotypes among NODAT and control groups. The associations of IL6 G (− 147) G, IL-4 C (− 590) C, IFNG TT and TGFB TT were superseded by age group and bio-physiology of patients. In short, IL6 G (− 147) G, IL-4C (− 590) C, IFNG TT and TGFB TT were not independently associated to NODAT. The current data might indicate that the latter immune signature complex can provide a clue to the pathogenesis of NODAT. Although throughout our induction procedure, we aimed to suppress T-cells, thereby reducing the chance of kidney rejection.
Conclusion
The ability to perform noninvasive testing to transplant recipients will provide tools to identify patient risk of NODAT and the individualization of immune suppression regimens to improve outcomes after transplantation. The pathogenesis of NODAT is Th-1 cell-mediated variations, while IFNG, IL-4, TGF-β1 and IL-6may play a crucial role in that mechanism. Interestingly no association was found between the above cytokine genes and well-established HLA loci for NODAT. The latter rules out the autoimmune nature of NODAT.
Tailoring of immunosuppressive agents may be used to target patients according to their genetic makeup. The results of our research might provide a suitable platform for a larger multicenter study, focusing on the Arab population, to evaluate the role of cytokine genes in NODAT to confirm our findings and better understand the prevalence of NODAT in KTR patients.
References
Rocha, R. V. et al. Long-term patient and allograft outcomes of kidney transplant recipients undergoing cardiac surgery. J. Thorac. Cardiovasc. Surg. 147, 270–275. https://doi.org/10.1016/j.jtcvs.2012.10.037 (2014).
Prakash, J., Ghosh, B., Singh, S., Soni, A. & Rathore, S. S. Causes of death in kidney transplant recipients with functioning allograft. Indian J. Nephrol. 22, 264–268. https://doi.org/10.4103/0971-4065.101245 (2012).
Juan Khong, M. & Ping Chong, C. Prevention and management of new-onset diabetes mellitus in kidney transplantation. Neth. J. Med. 72, 127–134 (2014).
Davidson, J. A., Wilkinson, A. & International Expert Panel on New-Onset Diabetes After Transplantation. New-Onset Diabetes After Transplantation 2003. International consensus guidelines: an endocrinologist’s view. Diabetes Care 27, 805–812 (2004).
Chadban, S. New-onset diabetes after transplantation—should it be a factor in choosing an immunosuppressant regimen for kidney transplant recipients. Nephrol. Dial. Transplant. 23, 1816–1818. https://doi.org/10.1093/ndt/gfn052 (2008).
Chadban, S. et al. Immunosuppression in kidney transplantation: some aspects for the modern era. Transplant. Rev. 22, 241–251. https://doi.org/10.1016/j.trre.2008.05.003 (2008).
Marcen, R. et al. Ischemic heart disease after kidney transplantation in patients on cyclosporine in Spain. J. Am. Soc. Nephrol. JASN 17, S286–S290. https://doi.org/10.1681/ASN.2006080928 (2006).
Sulanc, E. et al. New-onset diabetes after kidney transplantation: an application of 2003 international guidelines. Transplantation 80, 945–952 (2005).
Aleid, H. et al. New-onset diabetes after kidney transplantation: Incidence, risk factors, and outcomes. Saudi J. Kidney Dis. Transplant. 27, 1155–1161 (2016).
Al-Ghareeb, S. M., El-Agroudy, A. E., Al Arrayed, S. M., Al Arrayed, A. & Alhellow, H. A. Risk factors and outcomes of new-onset diabetes after transplant: single-centre experience. Exp. Clin. Transplant. 10, 458–465. https://doi.org/10.6002/ect.2012.0063 (2012).
Nagib, A. M. et al. New onset diabetes mellitus after living donor kidney transplantation: a unique pattern in the Egyptian population. J. Diabetes Metab. 6, 1–5. https://doi.org/10.4172/2155-6156.1000519 (2015).
Johny, K. V. et al. High incidence of post-transplant diabetes mellitus in Kuwait. Diabetes Res. Clin. Pract. 55, 123–130 (2002).
Tarek, M. et al. Post transplant diabetes mellitus in Kuwait. Nephrol. Dial. Transplant. 32, III275. https://doi.org/10.1093/ndt/gfx149.SP451 (2017).
Chakkera, H. A. et al. Pilot study: association of traditional and genetic risk factors and new-onset diabetes mellitus following kidney transplantation. Transpl. Proc. 41, 4172–4177. https://doi.org/10.1016/j.transproceed.2009.08.063 (2009).
Tang, Q. & Bluestone, J. A. Regulatory T-cell therapy in transplantation: moving to the clinic. Cold Spring Harb. Perspect. Med. https://doi.org/10.1101/cshperspect.a015552 (2013).
Zwang, N. A. & Leventhal, J. R. Cell therapy in kidney transplantation: focus on regulatory T cells. J. Am. Soc. Nephrol. JASN 28, 1960–1972. https://doi.org/10.1681/ASN.2016111206 (2017).
Prasad, P. et al. Differential expression of circulating Th1/Th2/Th17 cytokines in serum of Chlamydia trachomatis-infected women undergoing incomplete spontaneous abortion. Microb. Pathog. 110, 152–158. https://doi.org/10.1016/j.micpath.2017.06.031 (2017).
Cartwright, N., Demaine, A., Jahromi, M., Sanders, H. & Kaminski, E. R. A study of cytokine protein secretion, frequencies of cytokine expressing cells and IFN-G gene polymorphisms in normal individuals. Transplantation 68, 1546–1552 (1999).
Jahromi, M. M., Millward, B. A. & Demaine, A. G. A polymorphism in the promoter region of the gene for interleukin-6 is associated with susceptibility to type 1 diabetes mellitus. J. Interferon Cytokine Res. 20, 885–888. https://doi.org/10.1089/10799900050163253 (2000).
Ro, H. et al. Association of polymorphisms of interleukin-8, CXCR1, CXCR2, and selectin with allograft outcomes in kidney transplantation. Transplantation 91, 57–64 (2011).
Weng, S. C. et al. Gene polymorphisms are associated with posttransplantation diabetes mellitus among Taiwanese kidney transplant recipients. Transpl. Proc. 44, 667–671. https://doi.org/10.1016/j.transproceed.2011.11.011 (2012).
Jahromi, M., Millward, A. & Demaine, A. A CA repeat polymorphism of the IFN-gamma gene is associated with susceptibility to type 1 diabetes. J. Interferon Cytokine Res. 20, 187–190. https://doi.org/10.1089/107999000312595 (2000).
Jahromi, M. M., Millward, B. A. & Demaine, A. G. Significant correlation between association of polymorphism in codon 10 of transforming growth factor-beta1 T (29) C with type 1 diabetes and patients with nephropathy disorder. J. Interferon Cytokine Res. 30, 59–66. https://doi.org/10.1089/jir.2009.0026 (2010).
Koh, T. J. & DiPietro, L. A. Inflammation and wound healing: the role of the macrophage. Expert Rev. Mol. Med. 13, e23. https://doi.org/10.1017/S1462399411001943 (2011).
Hayase, H. et al. Aberrant gene expression by CD25 + CD4 + immunoregulatory T cells in autoimmune-prone rats carrying the human T cell leukemia virus type-I gene. Int. Immunol. 17, 677–684. https://doi.org/10.1093/intimm/dxh238 (2005).
Liao, W. C. et al. Serum interleukin-6 level but not genotype predicts survival after resection in stages II and III gastric carcinoma. Clin. Cancer Res. 14, 428–434. https://doi.org/10.1158/1078-0432.CCR-07-1032 (2008).
Scheller, J., Chalaris, A., Schmidt-Arras, D. & Rose-John, S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim. Biophys. Acta 878–888, 2011. https://doi.org/10.1016/j.bbamcr.2011.01.034 (1813).
Herder, C. & Hermanns, N. Subclinical inflammation and depressive symptoms in patients with type 1 and type 2 diabetes. Semin. Immunopathol. https://doi.org/10.1007/s00281-019-00730-x (2019).
Meng, Y. et al. Genetic polymorphisms near IL-21 gene associated with Th17 cytokines confer risk for systemic lupus erythematosus in Chinese Han population. Lupus https://doi.org/10.1177/0961203319829821 (2019).
Lorente, L. et al. Association between interleukin-6 promoter polymorphism (− 174 G/C), serum interleukin-6 levels and mortality in severe septic patients. Int. J. Mol. Sci. https://doi.org/10.3390/ijms17111861 (2016).
Genctoy, G. et al. The role of proinflammatory cytokine gene polymorphisms for development of insulin resistance after kidney transplantation. Transpl. Proc. 38, 521–528. https://doi.org/10.1016/j.transproceed.2006.01.041 (2006).
Kang, K. et al. Interferon-gamma represses M2 gene expression in human macrophages by disassembling enhancers bound by the transcription factor MAF. Immunity 47, 235e234-250e234. https://doi.org/10.1016/j.immuni.2017.07.017 (2017).
Kelker, H. C. et al. Three molecular weight forms of natural human interferon-gamma revealed by immunoprecipitation with monoclonal antibody. J. Biol. Chem. 259, 4301–4304 (1984).
Pravica, V., Perrey, C., Stevens, A., Lee, J. H. & Hutchinson, I. V. A single nucleotide polymorphism in the first intron of the human IFN-gamma gene: absolute correlation with a polymorphic CA microsatellite marker of high IFN-gamma production. Hum. Immunol. 61, 863–866 (2000).
Peixe, R. G. et al. Single nucleotide polymorphisms in the interferon gamma gene are associated with distinct types of retinochoroidal scar lesions presumably caused by Toxoplasma gondii infection. Mem. Inst. Oswaldo Cruz 109, 99–107. https://doi.org/10.1590/0074-0276140539 (2014).
Rolandelli, A. et al. The IFNG rs1861494 single nucleotide polymorphism is associated with protection against tuberculosis disease in Argentina. Genes https://doi.org/10.3390/genes9010046 (2018).
Biolo, G. et al. Association of interferon-gamma + 874A polymorphism with reduced long-term inflammatory response in haemodialysis patients. Nephrol. Dial. Transplant. 21, 1317–1322. https://doi.org/10.1093/ndt/gfk033 (2006).
Shiu, K. Y. et al. Graft dysfunction in chronic antibody-mediated rejection correlates with B-cell-dependent indirect antidonor alloresponses and autocrine regulation of interferon-gamma production by Th1 cells. Kidney Int. 91, 477–492. https://doi.org/10.1016/j.kint.2016.10.009 (2017).
Pfeffer, L. M. The role of nuclear factor kappaB in the interferon response. J. Interferon Cytokine Res. 31, 553–559. https://doi.org/10.1089/jir.2011.0028 (2011).
Liu, T., Zhang, L., Joo, D. & Sun, S. C. NF-kappaB signaling in inflammation. Signal Transduct. Target Ther. https://doi.org/10.1038/sigtrans.2017.23 (2017).
Yi, Z. et al. IFN-gamma receptor deficiency prevents diabetes induction by diabetogenic CD4+, but not CD8+, T cells. Eur. J. Immunol. 42, 2010–2018. https://doi.org/10.1002/eji.201142374 (2012).
Rasche, S. S., Phillips, M., McInerney, M. F., Sercarz, E. E. & Quinn, A. IL-13Ralpha1 expression on beta-cell-specific T cells in NOD mice. Diabetes 60, 1716–1725. https://doi.org/10.2337/db10-1229 (2011).
Haicheur, N. et al. Cytokines and soluble cytokine receptor induction after IL-12 administration in cancer patients. Clin. Exp. Immunol. 119, 28–37 (2000).
Shi, X. Y., Zhang, K. & Zhang, L. Type 1 diabetes millitus following short-term recombinant interferon therapy in patient with chronic hepatitis C. Zhonghua Nei Ke Za Zhi 57, 524–525. https://doi.org/10.3760/cma.j.issn.0578-1426.2018.07.012 (2018).
Kuriya, G. et al. Double deficiency in IL-17 and IFN-gamma signalling significantly suppresses the development of diabetes in the NOD mouse. Diabetologia 56, 1773–1780. https://doi.org/10.1007/s00125-013-2935-8 (2013).
Zhu, J. T helper 2 (Th2) cell differentiation, type 2 innate lymphoid cell (ILC2) development and regulation of interleukin-4 (IL-4) and IL-13 production. Cytokine 75, 14–24. https://doi.org/10.1016/j.cyto.2015.05.010 (2015).
Sandler, S. & Sternesjo, J. Interleukin 4 impairs rat pancreatic islet function in vitro by an action different to that of interleukin 1. Cytokine 7, 296–300. https://doi.org/10.1006/cyto.1995.0036 (1995).
Cameron, M. J. et al. IL-4 prevents insulitis and insulin-dependent diabetes mellitus in nonobese diabetic mice by potentiation of regulatory T helper-2 cell function. J. Immunol. 159, 4686–4692 (1997).
Leslie, K. A., Russell, M. A., Taniguchi, K., Richardson, S. J. & Morgan, N. G. The transcription factor STAT6 plays a critical role in promoting beta cell viability and is depleted in islets of individuals with type 1 diabetes. Diabetologia 62, 87–98. https://doi.org/10.1007/s00125-018-4750-8 (2019).
Sobhanifard, M. et al. Effect of extremely low frequency electromagnetic fields on expression of T-bet and GATA-3 genes and serum interferon-gamma and interleukin-4. J. Interferon Cytokine Res. 39, 125–131. https://doi.org/10.1089/jir.2018.0105 (2019).
Mao, S., Zhang, J., Zhao, M. & Zhang, Y. Association of transforming growth factor-beta1 polymorphisms with the risk of diabetes mellitus. Int. J. Clin. Exp. Med. 8, 21886–21892 (2015).
Hamaguchi, T. et al. Association of a polymorphism of the transforming growth factor-beta1 gene with cerebral amyloid angiopathy. J. Neurol. Neurosurg. Psychiatry 76, 696–699. https://doi.org/10.1136/jnnp.2003.034454 (2005).
Watanabe, Y. et al. A catalog of 106 single-nucleotide polymorphisms (SNPs) and 11 other types of variations in genes for transforming growth factor-beta1 (TGF-beta1) and its signaling pathway. J. Hum. Genet. 47, 478–483. https://doi.org/10.1007/s100380200069 (2002).
Bazzaz, J. T. et al. TNF-alpha and IFN-gamma gene variation and genetic susceptibility to type 1 diabetes and its microangiopathic complications. J. Diabetes Metab. Disord. 13, 46. https://doi.org/10.1186/2251-6581-13-46 (2014).
Feng, X., Tang, H., Leng, J. & Jiang, Q. Suppressors of cytokine signaling (SOCS) and type 2 diabetes. Mol. Biol. Rep. 41, 2265–2274. https://doi.org/10.1007/s11033-014-3079-8 (2014).
Suchy, D., Labuzek, K., Machnik, G., Kozlowski, M. & Okopien, B. SOCS and diabetes—ups and downs of a turbulent relationship. Cell Biochem. Funct. 31, 181–195. https://doi.org/10.1002/cbf.2940 (2013).
Kidney Disease: Improving Global Outcomes Transplant Work. GKDIGO clinical practice guideline for the care of kidney transplant recipients. Am. J. Transplant. 9(Suppl 3), S1–S155. https://doi.org/10.1111/j.1600-6143.2009.02834.x (2009).
Loupy, A. et al. The Banff 2015 kidney meeting report: current challenges in rejection classification and prospects for adopting molecular pathology. Am. J. Transplant. 17, 28–41. https://doi.org/10.1111/ajt.14107 (2017).
Ramesh Prasad, G. V. et al. Pre-transplantation glucose testing for predicting new-onset diabetes mellitus after kidney transplantation. Clin. Nephrol. 71, 140–146 (2009).
Puoti, F. et al. Organ transplantation and gender differences: a paradigmatic example of intertwining between biological and sociocultural determinants. Biol. Sex Differ. 7, 35. https://doi.org/10.1186/s13293-016-0088-4 (2016).
Kim, Y. G. et al. Association of genetic polymorphisms of interleukins with new-onset diabetes after transplantation in kidney transplantation. Transplantation 93, 900–907. https://doi.org/10.1097/TP.0b013e3182497534 (2012).
Sinangila, A. et al. The incidence of new onset diabetes after transplantation and related factors: single center experience. Nefrologia 37, 181–188. https://doi.org/10.1016/j.nefro.2016.11.022 (2017).
Dedinska, I. et al. Correlation between CMV Infection and post-transplantation new-onset diabetes mellitus. Int. J. Organ Transplant. Med. 7, 173–182 (2016).
Khalili, N., Rostami, Z., Kalantar, E. & Einollahi, B. Hyperglycemia after kidney transplantation: frequency and risk factors. Nephro-urol. Mon. 5, 753–757. https://doi.org/10.5812/numonthly.10773 (2013).
Tarnowski, M., Sluczanowska-Glabowska, S., Pawlik, A., Mazurek-Mochol, M. & Dembowska, E. Genetic factors in pathogenesis of diabetes mellitus after kidney transplantation. Ther. Clin. Risk Manag. 13, 439–446. https://doi.org/10.2147/TCRM.S129327 (2017).
Mukhtar, N. A., Ayala, C., Maher, J. J. & Khalili, M. Assessment of factors associated with pre-diabetes in HCV infection including direct and dynamic measurements of insulin action. J. Viral Hepat. 19, 480–487. https://doi.org/10.1111/j.1365-2893.2011.01568.x (2012).
Hjelmesaeth, J. et al. Asymptomatic cytomegalovirus infection is associated with increased risk of new-onset diabetes mellitus and impaired insulin release after kidney transplantation. Diabetologia 47, 1550–1556. https://doi.org/10.1007/s00125-004-1499-z (2004).
Marin, M., Renoult, E., Bondor, C. I. & Kessler, M. Factors influencing the onset of diabetes mellitus after kidney transplantation: a single French center experience. Transpl. Proc. 37, 1851–1856. https://doi.org/10.1016/j.transproceed.2005.03.140 (2005).
Acknowledgements
This work has been performed by funding from our local institution RA 2015-013, as well as Kuwaiti Ministry of Health MOH for our educational clinic. We would like to appreciate them for their generous award. The authors would be delighted to acknowledge initial support and encouragement of Dr Narayanam Nampoory and Dr Adel Ahmad. Meanwhile, we would like to thank Dr Mohamed Hasan Sayegh Executive Vice President, American university of Beirut for his guidance. As we would be pleased to thank Rashid Ahmad for his support. We would like to acknowledge Ms Hidaia Abdullah for her data handling. Authors would like to acknowledge Ms Kawthar Jahrami’s efforts in proof reading.
Author information
Authors and Affiliations
Contributions
M.J. was involved in research planning, management, data analyses and writing manuscript, O.G. oversaw clinical issues, data analysis and editing, N.O. oversaw educational clinic, T.A.O., T.M., P.N., M.A.H. were in nephrology clinics on Hamed Al Essa Center, J.R.A., S.A.D.S. reviewed critically the design and the analysis of the data, P.C., G.M. contributed in data interpretation and editing, P.A. conducting lab work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jahromi, M., Al-Otaibi, T., Ashry Gheith, O. et al. Analysis of the frequency of single nucleotide polymorphisms in cytokine genes in patients with New Onset Diabetes After Transplant. Sci Rep 11, 6014 (2021). https://doi.org/10.1038/s41598-021-84400-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-021-84400-9