Abstract
We aimed to investigate the interaction between the transcript levels of taurine-upregulated gene 1 (TUG1) and metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) and the Cholesterol-Saturated Fat Index (CSI) in relation to the visceral adiposity index (VAI) and body adiposity index (BAI). This cross-sectional study involved 346 women classified as obese and overweight, aged between 18 and 48 years. Dietary intake and the quality of dietary fat were assessed using a validated and reliable 147-item semi-quantitative food frequency questionnaire, with the Cholesterol-Saturated Fat Index (CSI) used as an indicator. Transcription levels of MALAT1 and TUG1 were evaluated through real-time polymerase chain reaction following the criteria outlined in the Minimum Information for Publication of Quantitative standards. Serum profiles were measured using standard protocols. We observed a positive association between transcription level of MALAT1 and VAI in both crude (β = 3.646, 95% CI 1.950–5.341, p < 0.001) and adjusted (β = 8.338, 95% CI 6.110–10.566, p < 0.001) models. Furthermore, after adjusting for confounders, a significant positive interaction was noted between MALAT1 expression and CSI on BAI (β: 0.130, 95% CI 0.019, 0.240, p = 0.022), with a marginal positive interaction observed on VAI (β: 0.718, 95% CI − 0.028, 1.463, p = 0.059). It seems that there may be a positive interaction between MALAT1 transcription level and CSI on VAI and BAI among overweight and obese women. However, no associations were seen between TUG1 mRNA level and the above-mentioned outcomes. Further functional studies are still required to elucidate this concept.
Similar content being viewed by others
Introduction
One of the main contributors to global non-communicable diseases and mortality is the rising incidence of obesity1,2,3. Estimates suggest that by 2030, one billion people worldwide, comprising one in seven males and one in five females, will be affected by obesity4. Obesity affects roughly 21.7% of the adult population of Iran5. Additionally, Iranian women (57%) were more likely than men (42.8%) to be overweight or obese6,7,8.
While adipose tissue is widely distributed throughout the body and serves crucial functions in maintaining health, it is essential to recognize it as a highly active endocrine organ9,10. Obese individuals are more prone to metabolic disorders due to the increased susceptibility associated with visceral adipose tissue (VAT) compared to subcutaneous adipose tissue (SAT)11. The VAT is related to the pathogenesis of insulin resistance, dyslipidemia, and cardiovascular diseases (CVDs)11,12. Among obesity indices, visceral adiposity index (VAI) and body adiposity index (BAI) are two novel anthropometric measures that hold the potential to enhance the assessment of obesity, body composition, and the identification of metabolic syndrome13,14. Various factors, including low socioeconomic status, a sedentary lifestyle, environmental influences, genetic variations or expressions, molecular mechanisms, and diet, play a role in the etiology of adiposity15,16,17,18,19.
To develop effective diagnostic and treatment techniques, a comprehensive understanding of the molecular pathways governing the onset of metabolic syndrome and obesity is imperative20. A subclass of non-coding RNAs called long non-coding RNAs (lncRNAs) plays crucial roles in a variety of biological processes because they can regulate gene expression at various levels21,22.
Cutting-edge research has revealed that lncRNA dysregulation plays crucial roles in maintaining homeostasis, and control of lipid metabolism, and fat accumulation20,23,24. Recent research suggests that the lncRNAs; taurine-upregulated gene 1 (TUG1) and metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) may play regulatory roles in the etiology of obesity-related illnesses and the control of lipid metabolism25. There is limited and somewhat conflicting research on the role of MALAT1 in obesity. Recent findings indicate a reduction in MALAT1 expression in white adipose tissue from obese mice. However, the deletion of MALAT1 showed minimal impact on diet-induced growth in adipose tissue and lipid balance in obese animals25. On the contrary, distinct research has revealed a significant increase in MALAT1 expression in the medium released by adipose-derived stem cells and omental depots from obese individuals26. Another study also showed that mesenteric adipose tissue-derived exosomes from mice on a high-fat diet exhibited elevated MALAT1 expression27 Moreover, Ebrahimi et al.28 reported that VAT and SAT from obese women had considerably lower mRNA levels of TUG1 in comparison with the controls.
In addition to lncRNAs, the diet has a crucial role in adiposity29. All facets of fatty acids in the diet should be taken into account to analyze how the quality of dietary fat consumption relates to obesity and body fat percentage30. An innovative dietary self-monitoring tool, proposed by Connor et al., is the Cholesterol-Saturated Fat Index (CSI), which provides information on the cholesterol and saturated fat content of meals31. A low CSI index indicates a reduction in saturated fatty acid (SFA) and cholesterol levels, suggesting a decrease in atherogenicity32. Recent findings suggest that long non-coding RNAs (lncRNAs) can influence metabolic processes in response to shifting nutritional cues. Mounting evidence indicates that tissue-specific long non-coding RNAs (lncRNAs) play a functional role in response to nutritional changes. Certain lncRNAs play a role in coordinating physiological responses to nutrient deprivation, while others contribute to the pathogenesis of diseases influenced by nutrition33. Understanding how lncRNAs respond to changes in nutrition is crucial for comprehending the intricate downstream cascades triggered by dietary shifts. This knowledge can profoundly influence how we approach the treatment of metabolic diseases.
Despite our endeavors to understand the roles of lncRNAs MALAT1 and TUG1 in the context of metabolic disorders, the precise role of these lncRNAs in obesity and to understand how they interact with dietary factors remain unclear. In this study, we aimed to explore, the interaction between long non-coding RNA MALAT1 and TUG1 with dietary fatty acid quality indices concerning the visceral adiposity index (VAI) and body adiposity index (BAI) in overweight and obese women.
Subjects and methods
Study population
In this cross-sectional study, 346 healthy overweight and obese women were selected using community-based multi-stage simple random sampling after considering eligibility criteria. The participants were drawn from 20 randomly chosen health centers located throughout West and Central Tehran, Iran. The inclusion criteria comprised a body mass index (BMI) ranging from 25 to 40 kg/m2, and ages between 18 and 48 years. The criteria for not entering the study were individuals with a history of cardiovascular diseases (CVDs), kidney failure, stroke, thyroid disease, liver disease, cancer, inflammatory illnesses, and addiction to alcohol or drugs. Moreover, women undergoing menopause, pregnancy, and lactation, as well as those using weight-loss supplements, engaging in dieting within the previous year, and taking medications to lower blood pressure, glucose, and lipid levels in plasma, were not entering the study. All study participants provided written informed consent before the investigation commenced. The research received approval from the local ethics committee of Tehran University of Medical Sciences (TUMS) with the ethics number IR.TUMS.MEDICINE.REC.1401.073.
Assessment of body composition
We applied a bioelectrical impedance analyzer (BIA) (Inbody 770 Co., Seoul, Korea) following the methods, safety precautions, and instructions outlined in the manufacturer's protocol34. Participants place their bare feet on the balance scale and grasp the BIA handles. The different readings were determined by the BIA using an electric signal that passes through the palms and soles of the feet. Before measuring, participants took off their shoes, excess clothes, and any metal items. It takes 15–20 s to check body composition, weight, trunk fat, body fat mass (BFM), visceral fat, fat-free mass index (FFMI), and fat mass index (FMI).
Assessment of anthropometric indices
Before anthropometric measurements, participants were instructed to refrain from engaging in strenuous physical activity for 72 h and to fast for 12 h. While individuals were shoeless and wearing as minimal garments as possible, we utilized BIA 770 (South Korea) to determine body weight to the closest 100 g. A non-elastic tape was used to measure each participant’s height to the closest 0.5 cm while they were standing next to a wall in a typical stance. To determine the BMI (in square meters), we divided the weight (in kilograms) by the square of the height. According to the World Health Organization (WHO), obesity classes 1, 2, and 3 correspond to BMIs of 30–34.9%, 35–39.9%, and 40 kg/m2, respectively. A BMI of 25 to 29.9 kg/m2 is regarded as overweight. Without exerting any pressure on the body, we measured the waist circumference to the closest 0.5 cm using non-elastic tape at the place where the natural waistline ends. The waist-to-hip ratio (WHR) was estimated by dividing the waist circumference (WC) by the hip circumference (HC). To minimize measurement errors, all measures were performed by a single trained dietician.
VAI and BAI assessment
BAI and VAI were calculated using the following formulas14,35
Assessment of dietary intake
Habitual dietary intake frequency over the past 12 months was assessed using a 147-item semi-quantitative food frequency questionnaire (FFQ), whose validity and reliability have been approved36. Based on this questionnaire, the individuals were asked to indicate whether they consumed each food item on a daily, weekly, monthly, or yearly basis. After being told the typical size of each food item in the FFQ, participants were asked to rate the frequency of intake of each food item according to their standard unit on a daily, weekly, monthly, or yearly basis. The information from this questionnaire was entered into an Excel file that was made to determine the weight (in grams) of each food item. Items reported using standard units and home scales were converted to grams using the home scale conversion guide. So, for every item and every person, the equivalent of consumption was calculated. The dietary consumption data were converted and analyzed using the NUTRITIONIST 4 (N4) food analyzer from Hearst Corporation in San Bruno, California. Total energy, macronutrients, and micronutrients were determined using Hearst Corporation's Nutritionist 4 software in San Bruno, California37.
Dietary fat quality indices
The FFQ was assessed to determine the meals to be included, which were then converted to grams per day using household measures. Cholesterol and saturated fatty acid levels were determined using the Iranian Food Composition Table (FCT) and N4 software. To evaluate the quality of fat, the Cholesterol-Saturated Fat Index (CSI) was employed. CSI provides data on the cholesterol and saturated fat content in various foods. The index is calculated by dividing cholesterol by the quantity of saturated fat in meal items, as assessed by the FFQ38. A low CSI indicates a lower quantity of saturated fat and/or cholesterol, suggesting that a diet with a lower CSI has a hypocholesterolemic and low atherogenic potential31.
Assessment of physical activity and other variables
The duration and frequency of regular daily activities over a week in the preceding year are included in The International Physical Activity Questionnaire (IPAQ). Metabolic equivalent hours (MET-h/week) are used to calculate the participants' weekly quantities of physical activity39. The reliability and validity of the International Physical Activity Questionnaire (IPAQ) have been previously assessed in Iranian adolescents39. A demographic questionnaire was used to collect data on demographic variables such as income and education status, income, and smoking status as well.
Biochemical parameters assessment
Participants provided a morning blood sample between 8:00 and 10:00 AM following an overnight fasting period. The collected blood sample was then centrifuged, divided into smaller aliquots, and stored at − 80 °C. Subsequently, all samples underwent analysis using a standardized testing method. A glucose oxidase-phenol 4-aminoantipyrine peroxidase (GOD-PAP) test was used to determine fasting blood glucose (FBG). Triglycerides (TG) and total cholesterol (TC) were quantified using an enzyme endpoint called glycerol-3-phosphate oxidase-phenol 4-aminoantipyrine peroxidase (GPOPAP). The levels of low-density lipoprotein (LDL-c) and high-density lipoprotein (HDL-c) cholesterol were assessed using a direct enzymatic clearance test (Pars Azmoon Inc, Tehran, Iran). The minimum detectable level of insulin was 1.76 mIU/mL, with intra- and inter-class correlation coefficients of 2.11 and 4.4%, respectively. To determine the HOMA-IR, the homeostasis model assessment (HOMA) was computed as [(fasting plasma glucose fasting serum insulin)/22.5]40. At the School of Nutrition and Dietetics at TUMS, the Nutrition and Biochemistry Laboratory evaluated each sample using standardized procedures.
Real-time quantitative polymerase chain reaction (PCR)
The concentration of the extracted RNA was assessed using NanoDrop at an absorbance of 260 nm. For optimal RNA purity, the A260/A280 ratio was maintained between 1.80 and 2.05, while the A260/A230 ratio fell within the range of 2.00–2.50. The integrity of the RNA was verified through agarose gel electrophoresis. For the subsequent step, the first-strand complementary DNA (cDNA) synthesis was conducted using 1000 ng of RNA that had undergone DNase treatment. This process utilized a cDNA synthesis kit from AnaCell, Tehran, Iran, following the manufacturer's instructions.
Quantitative real-time PCR was then carried out using the Step-One-Plus TM real-time PCR system by ABI Applied Biosystems, in conjunction with Bio FACTTM 2X Real-Time PCR Master Mix (for SYBR Green I), following the MIQE (Minimum Information for Publication of Quantitative Real-Time PCR Experiments) recommendations41. Following the real-time PCR, a melting curve analysis was conducted, involving a gradual temperature increase from 60 to 95 °C, followed by a return to 60 °C for 1 min. The SYBR Green fluorescence signal was continuously monitored, and the presence of single peaks, denoting a unique melting temperature (Tm), confirmed the success of the amplification process.
To assess gene alterations at the long non-coding RNA (lncRNA) level, we utilized the Schmittgen and Livak method, which calculates relative expression (2 − ΔCT) based on the ΔCT values obtained from real-time PCR. The reference gene used was 18s rRNA, and the expression of each sample was normalized to its corresponding reference gene value.
It is noteworthy that all samples exhibited Ct (Cycle threshold) values below 35. Calibration curves were employed to evaluate the amplification efficiency for both the target genes and reference genes, with the amplification efficiency (E) ranging from 95 to 100% for all genes. Since there was only one group under investigation (overweight and obese women), the 2-∆CT formula was applied to all measurements. For specific primer sequences used in the examination of MALAT1 and TUG1 gene expression, please refer to Table S1 for details.
Statistical analyses
Based on the cross-sectional study sample size calculation (β = 0.95, α = 0.05, power = 90%, effect size = 0.05, and number of predictive parameters = 7), a sample size of 346 has been determined42. The normality of quantitative variables was assessed using the Kolmogorov–Smirnov technique, and the histogram curve was evaluated (P > 0.05). Mean and standard deviation (SD) were used to report quantitative and number (percent) for categorical variables. Participants’ characteristics among tertiles of transcript levels of MALAT1 TUG1 and CSI were analyzed using one-way analysis of variance (ANOVA) for continuous variables and chi-squared for categorical variables. Analysis of covariance (ANCOVA) was performed for adjustment models. All associations were reported in the crude model and after adjustment for age, BMI, energy intake, and physical activity. Generalized linear models (GLMs) as linear regression were exerted to analyze the interaction between mRNA expression of MALAT1, TUG1, and CSI on VAI and BAI indexes in the crude and adjusted model. The adjustment was applied based on age, energy intake, smoking, income, and physical activity in Model 1. Analysis output was reported as β, standard error (SE) and 95% confidence interval (CI). SPSS version 26.0 (SPSS, Chicago, IL, USA) was used for all statistical analyses. All published P-values were two-sided, with a significance level set at less than 0.05 to be considered statistically significant. P-values less than 0.1 were deemed marginally significant.
Ethical approval and consent to participate
The study protocol has been approved by the ethics committee of Tehran University of Medical Sciences (TUMS) with the following identification: IR.TUMS.MEDICINE.REC.1401.073. Each participant was completely informed about the study protocol and provided a written and informed consent form before taking part in the study. All methods were carried out under relevant guidelines and regulations or the declaration of Helsinki.
Results
Study population characteristics
The statistical analysis included a total of 346 women.The transcript levels of MALAT1, TUG1, and CSI mean and standard deviation (SD) in this study were 1.520 (6.010), 1.700 (6.024), and 13.244 (5.714), respectively. Individuals’ average age, weight, and BMI were 36.568 ± 8.978 years, 80.762 ± 10.518 kg, and 31.215 ± 4.182 kg/m2 respectively. The mean (SD) of anthropometric and body composition such as BFM, WC, and WHR were 33.990 (8.085), 99.533 (9.993), and 1.159 (4.486) respectively.
General characteristics of participants among MALAT1, TUG1 mRNA expression, and CSI tertiles
Table 1 shows the characteristics of the participants, their socioeconomic status, and anthropometric and biochemical assessments before and after adjustment for cofounders. In the crude model and after adjustments for age, physical activity, BMI, and total energy consumption, there were no statistically significant mean differences observed for social characteristics, anthropometrics, biochemical assessment, and categorical variables between MALAT1 and TUG1 expression tertiles. However, there was a marginally significant mean difference for total cholesterol among tertiles of MALAT1 transcript levels before adjustment (p = 0.056), and after controlling for confounders, it remained significant (p = 0.046).
Furthermore, there was a significant mean difference among tertiles of CSI for education status (p = 0.007) and smoking (p = 0.009), and a marginally significant mean difference for income (p = 0.069) after controlling confounders.
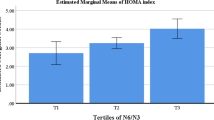
The difference in means of BAI and VAI among tertiles of MALAT1 and TUG1 transcript levels and CSI in obese and overweight women
There was no significant mean difference among the tertiles of MALAT1, TUG1 transcript levels, and CSI for VAI and BAI (p > 0.05) (Table 2).
Dietary intake of study population over MALAT1 and TUG1 expression tertiles
Table 3 shows the participants' intake of specific nutrients and food groups across MALAT1 and TUG1 expression tertiles. After controlling energy intake, lower intakes of carbohydrates (p = 0.038), fat (p = 0.019), oleic acid (p = 0.037), vitamin B5 (p = 0.040), and legumes (p = 0.031) were found in participants in the highest tertile of MALAT 1 transcript level. Meanwhile, linolenic acid (p = 0.095), vitamin A (p = 0.064), vitamin B1 (p = 0.086), and poultry (p = 0.073) intake were marginally significant mean differences among tertiles of MALAT 1 mRNA expression. Participants with lower mRNA expression of TUG1 showed a significantly lower intake of fruits (p = 0.007), and dietary vitamin K (p = 0.026) was lower in the top tertiles of the TUG1 transcript level. Additionally, there was a marginally significant difference in omega-3 intake (p = 0.071), vitamin B1 (p = 0.079), and high-fat dairy intake (p = 0.058).
The association of MALAT1 and TUG1 mRNA expression with BAI and VAI
The association between MALAT1 and TUG1 mRNA expression and BAI and VAI was presented in Table 4. The crude model revealed a significant positive relationship between the transcript level of MALAT1 and VAI (β = 3.646, 95%CI 1.950–5.341, p < 0.001) (Table 4). After adjusting for confounding factors such as age, BMI, energy intake, and physical activity, a significant positive association persisted between MALAT1 transcript level and VAI (β = 8.338, 95%CI 6.110 to 10.566, p < 0.001). However, no significant association of the mRNA level of TUG1 with BAI and VAI was observed in both the crude and adjusted models (Table 4).
The interaction between MALAT1 and TUG1 mRNA expression and CSI on BAI and VAI
The interaction between MALAT1 expression and CSI on BAI and VAI in the crude model and after adjustment for age, energy intake, smoking, income, and physical activity in model 1 is presented in Table 5. In the crude model, a significant positive interaction was observed between MALAT1 expression and CSI on VAI (β: 1.287, 95%CI 0.806, 1.769, p < 0.001), and a marginally significant positive interaction was noted between MALAT1 expression and CSI on BAI (β: 0.105, 95%CI − 0.015, 0.226, p = 0.088). After controlling for confounding variables in model 1, a significant positive interaction between MALAT1 expression and CSI was observed on BAI (β: 0.130, 95%CI 0.019, 0.240, p = 0.022), and a marginal positive interaction was seen on VAI (β: 0.718, 95%CI − 0.028, 1.463, p = 0.059). There was no significant interaction between CSI and TUG1 expression on BAI and VAI in both crude and adjustment models.
Discussion
To the best of our knowledge, this is the first study investigating the interactions between mRNA expression of lncRNAs, MALAT1, and TUG1, with dietary fat quality index (CSI) on VAI and BAI in overweight and obese women. Our study can provide evidence regarding positive interactions between increased CSI and MALAT1 expression on VAI and BAI. However, no substantially significant interactions between TUG1 and CSI were identified in terms of the above-mentioned markers.
VAI, a novel sex-specific index, is focused on BMI, WC, TG, and HDL-c.
Compared to the effect of a single factor, VAI provides more comprehensive estimates of overall variables, thus better identifying visceral adiposity dysfunction associated with cardio-metabolic risk factors43. BAI is a useful established indicator of % fat in both men and women, and it has also been considered to serve as a better predictor of health outcomes than BMI itself44. Nevertheless, the interaction of these two novel indicators of obesity has been scarcely investigated in the context of lncRNAs45,46. The possible role of lncRNAs in pathogenesis and underlying mechanisms of obesity and related abnormalities have recently started to emerge47,48. However, no previous research has been conducted directly on lncRNAs-CSI interaction and lncRNAs-VAI/BAI, and even less has looked at the association of these molecules pertinent to metabolic disorders49,50; therefore, our results shed light on an unknown relationship between MALAT1 and TUG1 expression with CSI on VAI and BAI. A recent study among patients with atherosclerosis reported the involvement of MALAT1 in cholesterol accumulation in oxidized low-density lipoprotein (ox-LDL)-stimulated macrophages51. Jia et al. also demonstrated that MALAT1 transcript level was statistically upregulated in cardiomyocytes by saturated fatty acids (SFAs) during palmitic acid-induced hepatic steatosis treatment52. The contribution of lncRNAs in obesity-related research has been mostly performed in vitro and animal model study more than in human tissues53,54,55 and several lncRNAs were mapped to genetic loci that influence fat deposition regulation and lipid homeostasis49,56,57. Among these, increased expression of MALAT1 in pig fat tissue of the obese group revealed the direct role of MALAT1 expression in an obesity-related context57. The precise mechanisms explaining positive interactions between increased CSI and MALAT1 expression on VAI and BAI cannot be definitively determined based on the current study. Nonetheless, it is important to consider various possibilities derived from experimental investigations. Based on an animal model study, increased expression of MALAT1 in the livers of genetically leptin-deficient obese (ob/ob) mice exposed to palmitate was demonstrated to result in hepatic lipid accumulation49. Certainly, under conditions characterized by fatty acid overload, such as with palmitate, there is an observed elevation in intracellular levels of triglycerides and cholesterol in primary mouse hepatocytes58. It has also been suggested that high-fat diets in obese mice trigger a set of dysregulated lncRNAs in adipocytes which increases fat mass through decreasing plasma leptin59. Another possible mechanism for lipid profile incremental changes depends on the direct link between MALAT1 expression with peroxisome proliferator-activated receptor γ (PPARγ) and PPARγ coactivator 1-α (PGC1α)60. PPARγ is a nuclear receptor, which is activated by PGC1α, and displays tendencies for lipid synthesis and fat accumulation61,62,63. Furthermore, the occurrence of metabolic disorders seems to be attributed to the elevated expression of PPARγ induced by a high-fat diet.64. On the other hand, gene silencing of MALAT1 in mice significantly attenuated the palmitate-induced lipid accumulation of both intracellular levels of triglycerides and cholesterol49. Another possible explanation accounting for the observed interaction might be attributed to the absence of MALAT1, which seems to reduce 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, the rate-limiting enzyme of cholesterol synthesis49. Notably, reducing MALAT1 expression in the liver of ob/ob mice did not exhibit any impact on body weight49. Moreover, a recent study revealed that suppressing MALAT1 did not influence the accumulation of adipose tissue in mice induced by either age or dietary factors65. Regarding TUG1, our study did not identify any links between TUG1 expression and CSI affecting VAI and BAI. The possible candidate explaining our findings could be microRNA-204 (miR-204), a key tumor-suppressor microRNA that engages in the process of obesity66. It has been documented that miR-204 was abnormally up-regulated in obese mice and its overexpression is more likely to inhibit the expression of TUG167.
Consistent with our results, no notable correlation was observed between TUG1 and obesity-related parameters in VAT when accounting for age and HOMA-IR50. However, obese mice on a high-fat diet exhibited multiple essential functions of TUG1 in reducing weight and lipid accumulation. This effect was accomplished by stimulating the expression of leptin and adiponectin67.
Until recently, the extent to which long non-coding RNAs (lncRNAs) are implicated in the genetic mechanisms governing metabolic homeostasis and disorders, particularly in the context of addressing obesity and influencing the aforementioned outcomes, remained largely unexplored. It is also noteworthy that the majority of the studies are conducted on animal models and it can be proposed as one possible reason for these contradictory results. As such, our study along with others could uncover the possible role of MALAT1 and TUG1 associated with CSI on VAI and BAI among overweight/obese women. However, several limitations deserve to be mentioned. Firstly, the use of cross-sectional study design precludes the extrapolation of the results. Furthermore, environmental factors such as physical activity and nutrient status affecting lncRNAs have not been explored. The use of FFQ for recording the individual's food, which is subjected to recall bias, can also be regarded as a limitation. Given the significant roles of adipokines, particularly leptin and adiponectin, in the pathogenesis of obesity and related disorders, it is crucial to assess their connections with the two studied lncRNAs. As this study exclusively involved women, the generalizability of our findings to all genders is limited. Consequently, it is strongly recommended to conduct further studies with larger sample sizes encompassing both men and women to comprehensively address this issue.
Conclusion
In summary, this study represents the inaugural attempt to assess the interplay of the long non-coding RNAs (lncRNAs), MALAT1 and TUG1, in relation to CSI and its impact on VAI and BAI. The findings suggest a positive correlation between MALAT1 expression and CSI, potentially influencing VAI and BAI. Conversely, no robust associations were detected between TUG1 and the aforementioned outcomes. Nonetheless, further investigations in human studies are imperative to validate and expand upon these concepts in this field.
Data availability
The data supporting the findings of this study are not publicly available due to restrictions imposed by the license under which they were used for the current study. However, interested parties may request access to the data from the authors, with permission from the corresponding author, and subject to reasonable conditions.
References
Troeger, C. et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis 18(11), 1211–1228 (2018).
Suara, S. B., Siassi, F., Saaka, M., Foroshani, A. R. & Sotoudeh, G. Association between carbohydrate quality index and general and abdominal obesity in women: A cross-sectional study from Ghana. BMJ Open 9(12), e033038 (2019).
Rasaei, N. et al. The association between healthy beverage index and quality of life among overweight and obese women: A cross-sectional study. BMC Public Health. 23(1), 176 (2023).
Lobstein, T., Brinsden, H., & Neveux, M. World Obesity Atlas 2022 (2022).
Senobari, M., Azmoude, E. & Mousavi, M. The relationship between body mass index, body image, and sexual function: A survey on Iranian pregnant women. Int. J. Reprod. BioMed. 17(7), 503 (2019).
Al Kibria, G. M., Swasey, K., Hasan, M. Z., Sharmeen, A. & Day, B. Prevalence and factors associated with underweight, overweight and obesity among women of reproductive age in India. Global Health Res. Policy 4, 1–12 (2019).
Inoue, Y., Qin, B., Poti, J., Sokol, R. & Gordon-Larsen, P. Epidemiology of obesity in adults: Latest trends. Curr. Obes. Rep. 7, 276–288 (2018).
Barak, F., Falahi, E., Keshteli, A. H., Yazdannik, A. & Esmaillzadeh, A. Adherence to the dietary approaches to stop hypertension (DASH) diet in relation to obesity among Iranian female nurses. Public Health Nutr. 18(4), 705–712 (2015).
Schleinitz, D., Böttcher, Y., Blüher, M. & Kovacs, P. The genetics of fat distribution. Diabetologia 57, 1276–1286 (2014).
Rohm, T. V., Meier, D. T., Olefsky, J. M. & Donath, M. Y. Inflammation in obesity, diabetes, and related disorders. Immunity 55(1), 31–55 (2022).
Kissebah, A. Central obesity: Measurement and metabolic effects. Diabetes Rev. 5, 8–20 (1997).
Després, J.-P. et al. Role of deep abdominal fat in the association between regional adipose tissue distribution and glucose tolerance in obese women. Diabetes 38(3), 304–309 (1989).
Saqlain, M. et al. Body mass index versus other adiposity traits: Best predictor of cardiometabolic risk. Iran. J. Public Health 48(12), 2224 (2019).
Bergman, R. N. et al. A better index of body adiposity. Obesity 19(5), 1083–1089 (2011).
Hadi, A., Sepandi, M., Marx, W., Moradi, S. & Parastouei, K. Clinical and psychological responses to synbiotic supplementation in obese or overweight adults: A randomized clinical trial. Complement. Ther. Med. 47, 102216 (2019).
Mozaffarian, D. et al. Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Circulation. 131 (2015).
Tobore, T. O. Towards a comprehensive theory of obesity and a healthy diet: The causal role of oxidative stress in food addiction and obesity. Behav. Brain Res. 384, 112560 (2020).
Mohamadi, A. et al. Circulating inflammatory markers may mediate the relationship between healthy plant-based diet and metabolic phenotype obesity in women: A cross-sectional study. Int. J. Clin. Pract. 2022, 8099382 (2022).
Gholami, F., Naghshi, S., Samadi, M., Rasaei, N. & Mirzaei, K. Dietary acid load and bone health: a systematic review and meta-analysis of observational studies. Front. Nutr. 9, 869132 (2022).
Ji, E., Kim, C., Kim, W. & Lee, E. K. Role of long non-coding RNAs in metabolic control. Biochim. Biophys. Acta (BBA)-Gene Regul. Mech. 1863(4), 194348 (2020).
Eddy, S. R. Non-coding RNA genes and the modern RNA world. Nat. Rev. Genetics 2(12), 919–929 (2001).
Ulitsky, I. & Bartel, D. P. lincRNAs: Genomics, evolution, and mechanisms. Cell 154(1), 26–46 (2013).
Kim, J. et al. 2016 Long noncoding RNAs in diseases of aging. Biochim. Biophys. Acta (BBA)-Gene Regul. Mech. 1, 209–221 (1859).
Wei, S. et al. Long noncoding RNAs in regulating adipogenesis: New RNAs shed lights on obesity. Cell. Mol. Life Sci. 73, 2079–2087 (2016).
Carter, S., Miard, S., Boivin, L., Salle-Lefort, S. & Picard, F. Loss of Malat1 does not modify age-or diet-induced adipose tissue accretion and insulin resistance in mice. PLoS ONE 13(5), e0196603 (2018).
Patel, R. S. et al. Adipose-derived stem cells from lean and obese humans show depot specific differences in their stem cell markers, exosome contents and senescence: role of protein kinase C delta (PKCδ) in adipose stem cell niche. Stem Cell Investig. 3, 2 (2016).
Chen, D. et al. High-fat diet aggravates colitis via mesenteric adipose tissue derived exosome metastasis-associated lung adenocarcinoma transcript 1. World J. Gastroenterol. 28(29), 3838–3853 (2022).
Ebrahimi, R. et al. Adipose tissue gene expression of long non-coding RNAs; MALAT1, TUG1 in obesity: is it associated with metabolic profile and lipid homeostasis-related genes expression?. Diabetol. Metab. Syndr. 12, 1–13 (2020).
Speakman, J. R. Use of high-fat diets to study rodent obesity as a model of human obesity. Int. J. Obes. 43(8), 1491–1492 (2019).
Barbieiri, P. et al. Indices of dietary fat quality during midpregnancy is associated with gestational diabetes. Nutrition 32(6), 656–661 (2016).
Connor, S. L. et al. The cholesterol/saturated-fat index: an indication of the hypercholesterolaemic and atherogenic potential of food. Lancet (London, England) 1(8492), 1229–1232 (1986).
Mitchell, D. T., Korslund, M. K., Brewer, B. K. & Novascone, M. A. Development and validation of the cholesterol-saturated fat index (CSI) Scorecard: a dietary self-monitoring tool. J. Am. Diet. Assoc. 96(2), 132–136 (1996).
Lovell, C. D. & Anguera, M. C. Long noncoding rnas that function in nutrition: lnc-ing nutritional cues to metabolic pathways. Annu. Rev. Nutr. 42, 251–274 (2022).
A. T. Body Composition Analyzer;. BC-418 Instruction manual 2015.
Amato, M. C. et al. Visceral adiposity index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 33(4), 920–922 (2010).
Esmaillzadeh, A., Mirmiran, P. & Azizi, F. Whole-grain intake and the prevalence of hypertriglyceridemic waist phenotype in Tehranian adults. Am. J. Clin. Nutr. 81(1), 55–63 (2005).
Hearst C FDNIdaSB, CA: First DataBank (1995).
Mitchell, D. T. K. M., Brewer, B. K. & Novascone, M. A. Development and validation of the cholesterol-saturated fat index (CSI) scorecard: A dietary self-monitoring tool. J. Am. Diet. Assoc. 96, 132–136 (1996).
Craig, C. L. et al. International physical activity questionnaire: 12-Country reliability and validity. Med. Sci. Sports Exerc. 35(8), 1381–1395 (2003).
Mirzaei, K. et al. Insulin resistance via modification of PGC1α function identifying a possible preventive role of vitamin D analogues in chronic inflammatory state of obesity. A double blind clinical trial study. Minerva Med. 105(1), 63–78 (2014).
Bustin, S. A. et al. The MIQE guidelines: Minimum information for publication of quantitative real-time PCR experiments. Clin. Chem. 55(4), 611–622 (2009).
Cohen, J., Cohen, P., West, S. G. & Aiken, L. S. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences (Routledge, 2013).
Amato, M. C. G. C. et al. Visceral adiposity index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 33(4), 920–922 (2010).
Bergman, R. N. S. D. et al. A better index of body adiposity. Obesity (Silver Spring) 19(5), 1083–1089 (2011).
Blus, E.W.-K.A., Majewska, E. & Baj, Z. Usefulness of new indicators of obesity (BAI and VAI) in estimation of weight reduction. J. Am. Coll. Nutr. 39(2), 171–7 (2020).
Jabłonowska-Lietz, B. W. M., Włodarczyk, M. & Nowicka, G. New indexes of body fat distribution, visceral adiposity index, body adiposity index, waist-to-height ratio, and metabolic disturbances in the obese. Kardiol. Pol. 75(11), 1185–1191 (2017).
Wapinski, O. C. H. Long noncoding RNAs and human disease. Trends Cell Biol. 21(6), 354–361 (2011).
Latorre, J.F.-R.J. LncRNAs in adipose tissue from obese and insulin-resistant subjects: New targets for therapy?. EBioMedicine 30, 10–11 (2018).
Yan, C. C. J. & Chen, N. Long noncoding RNA MALAT1 promotes hepatic steatosis and insulin resistance by increasing nuclear SREBP-1c protein stability. Sci. Rep. 6, 22640 (2016).
Ebrahimi, R. T. K. et al. Adipose tissue gene expression of long non-coding RNAs; MALAT1, TUG1 in obesity: Is it associated with metabolic profile and lipid homeostasis-related genes expression?. Diabetol. Metab. Syndr. 12, 1–13 (2020).
Liu, L., Tan, L., Yao, J. & Yang, L. Long non-coding RNA MALAT1 regulates cholesterol accumulation in ox-LDL-induced macrophages via the microRNA-17-5p/ABCA1 axis. Mol. Med. Rep. 21, 1761–1770 (2020).
Jia, P., Wu, N., Jia, D. & Sun, Y. Downregulation of MALAT1 alleviates saturated fatty acid-induced myocardial inflammatory injury via the miR-26a/HMGB1/TLR4/NF-κB axis. Diabetes Metab. Syndr. Obes. Targets Ther. 12, 655–665 (2019).
Yu, L. T. L., Zhang, L., Chu, Y., Li, Y. & Zhou, L. Comparative analyses of long noncoding RNA in lean and obese pig. Oncotarget 8(25), 41440–41450 (2017).
Lo, K. A. H. S. et al. Adipocyte long-noncoding RNA transcriptome analysis of obese mice identified Lnc-Leptin, which regulates leptin. Diabetes 67(6), 1045–1056 (2018).
Huang, Y. J. C. et al. Knockdown of lncRNA MIR31HG inhibits adipocyte differentiation of human adipose-derived stem cells via histone modification of FABP4. Sci. Rep. 7(1), 8080 (2017).
Chen, Z. Progress and prospects of long noncoding RNAs in lipid homeostasis. Mol. Metab. 5(3), 164–170 (2016).
Piórkowska, K., Żukowski, K., Ropka-Molik, K., Tyra, M. Long-non Coding RNAs Related to Fat Deposition in Pigs Included lncRNA Corresponding to Human MALAT1. Preprints 2021.
Nea, Y. Absence of sterol regulatory element-binding protein-1 (SREBP-1) ameliorates fatty livers but not obesity or insulin resistance in Lep(ob)/Lep(ob) mice. J. Biol. Chem. 277, 19353–19357 (2002).
Dallner, O. S. M. J. et al. Dysregulation of a long noncoding RNA reduces leptin leading to a leptinresponsive form of obesity. Nat. Med. 25(3), 507–516 (2019).
Ee, A. Adipose tissue gene expression of long noncoding RNAs; MALAT1, TUG1 in obesity: Is it associated with metabolic profile and lipid homeostasisrelated genes expression?. Diabetol. Metab. Syndr. 12, 36 (2020).
Fajas, L. S. K. G. L. et al. Regulation of peroxisome proliferator-activated receptor gamma expression by adipocyte differentiation and determination factor 1/sterol regulatory element binding protein 1: Implications for adipocyte differentiation and metabolism. Mol. Cell. Biol. 19(8), 5495–5503 (1999).
Kersten, S. Mechanisms of nutritional and hormonal regulation of lipogenesis. EMBO Rep. 2(4), 282–286 (2001).
Beaven, S. W. et al. Reciprocal regulation of hepatic and adipose lipogenesis by liver X receptors in obesity and insulin resistance. Cell Metab. 18(1), 106–17 (2013).
Sikder, K. S. S. P. N., Singh, H. & Rafiq, K. High fat diet upregulates fatty acid oxidation and ketogenesis via intervention of PPAR-γ. Cell Physiol. Biochem. 48(3), 1317–1331 (2018).
Carter, S., Miard, S., Boivin, L., Sallé-Lefort, S. & Picard, F. Loss of Malat1 does not modify age- or diet-induced adipose tissue accretion and insulin resistance in mice. PLOS ONE 13(5), e0196603 (2018).
Yu, S. Y. D. B. F. Z., Hu, X. Q., Tang, L. & Zhou, S. H. Knockdown of lncRNA AK139328 alleviates myocardial ischaemia/reperfusion injury in diabetic mice via modulating miR-204-3p and inhibiting autophagy. J. Cell Mol. Med. 22, 4886–4898 (2018).
Zhang, Y. G. M. M. Y. & Peng, Y. LncRNA TUG1 reduces inflammation and enhances insulin sensitivity in white adipose tissue by regulating miR-204/SIRT1 axis in obesity mice. Mol. Cell Biochem. 475(1–2), 171–183 (2020).
Acknowledgements
The authors thank the Laboratory of Nutrition Sciences and Dietetics at Tehran University of Medical Sciences (TUMS). We are grateful to all of the participants for their contribution to this research. This study was approved by the Research Ethics Committee of the Tehran University of Medical Sciences (TUMS), Tehran, Iran with ethics number IR.TUMS.MEDICINE.REC.1401.073. All participants signed a written informed consent that was approved by this committee before enrollment in the study.
Funding
This study was supported by grants from the Tehran University of Medical Sciences, Tehran, Iran (Grant Number: 1400-3-212-56212).
Author information
Authors and Affiliations
Contributions
N.R., S.E., K.M. designed the search; N.R. and K.M. conducted the sampling; N.R. performed statistical analysis; N.R., F.G., M.S., F.S., A.K., M.S.Y., S.E. and K.M. wrote the paper, K.M. primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rasaei, N., Gholami, F., Samadi, M. et al. The interaction between MALAT1 and TUG1 with dietary fatty acid quality indices on visceral adiposity index and body adiposity index. Sci Rep 14, 12 (2024). https://doi.org/10.1038/s41598-023-50162-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-023-50162-9
This article is cited by
-
Lycium barbarum glycopeptide mitigates retinal ischemia-reperfusion injury through its anti-inflammatory, anti- senescence, and anti-apoptosis properties
Scientific Reports (2025)
-
lncRNA TUG1 transcript levels and psychological disorders: insights into interplay of glycemic index and glycemic load
BMC Medical Genomics (2024)
-
Investigation of the interaction between genetic risk score (GRS) and fatty acid quality indices on metabolic syndrome among overweight and obese women
BMC Medical Genomics (2024)