Abstract
Ewing's sarcoma (ES) is the second most common bone tumor in children and adolescents and is highly malignant. Although the new chemotherapy has significantly improved the survival rate for ES from about 10 to 75%, the survival rate for metastatic tumors remains around 30%. This treatment is often associated with various side effects that contribute to the suffering of the patients. Cold physical plasma (CPP), whether used alone or in combination with current chemotherapy, is considered a promising adjunctive tool in cancer treatment. This study aims to investigate the synergistic effects of CPP in combination with cytostatic chemotherapeutic agents that are not part of current ES therapy. Two different ES cell lines, RD-ES and A673, were treated with the determined IC20 concentrations of the chemotherapeutic agents cisplatin and methotrexate (MTX) in combination with CPP. The effects on population doubling, cell viability, and apoptotic processes within these cell lines were assessed. This combination therapy has led to a reduction of population doubling and cell viability, as well as an increase in apoptotic activity in cells compared to CPP monotherapy. The results of this study provide evidence that combining CPP with non-common chemotherapy drugs such as MTX and CIS in the treatment of ES enhances the anticancer effects of these drugs. These findings open up new possibilities for the effective use of these drugs against ES.
Similar content being viewed by others
Introduction
Ewing’s sarcoma (ES) is a rare but highly aggressive bone malignancy1,2. Its incidence is reported to be up to 1 case per 1.2 million population per year3. However, this number can vary depending on the ethnic population. Thus, African populations are significantly less affected by ES than Europeans3,4,5,6. The latest analyses of epidemiological data have shown an incidence of approximately 10 cases per million in white population groups3. Regardless of ethnic differences, the common feature is the manifestation of ES in adolescents at a mean age of 15 years5,7,8,9. Although ES typically occurs in bone tissue and primarily affects the axial skeleton, like pelvis and rips, and also proximal metaphysis of long bones, in about 20% of cases, it can also develop primarily in non-osseous tissue9,10,11,12. Cases of extraosseous ES are then diagnosed much more frequently in adults13,14.
The clinical diagnosis of ES can be challenging due to its non-specific symptoms, such as local pain that aggravates at night and swelling without an obvious cause. Pathologic fractures in the affected bones occur in about 10–15% of ES cases. The radiological analysis is much more meaningful than the diagnostic method. Multiple lytic bone lesions, Codman's triangle, and "onion peel" are typical radiological periosteal signs of proliferative response to bone malignancy15,16. As the disease progresses, other non-specific symptoms may appear, including fever, night sweats, fatigue, and weight loss17. Most laboratory diagnostics of the blood often show non-specific increases in inflammatory parameters and bone turnover, but an increased serum lactate dehydrogenase level correlates with this tumor burden and is, therefore, an important prognostic marker15. However, the most reliable diagnosis is made by identifying characteristic ES chromosomal translocations18,19,20.
Until the 1960s, the diagnosis of ES was fatal for approximately 90% of patients21. Several factors contribute to the prognosis of ES, such as the patient’s age and, histological characteristics, but the most important of these is the presence of metastasis at the time of diagnosis22,23. ES disease metastasis is found mostly in the lung, bone, or bone marrow24. With the introduction of chemotherapeutic agents in the treatment of ES, the survival rate of patients increased25. The current strategies against ES include combinations of chemotherapeutics such as doxorubicin, vincristine, and ifosfamide26,27 led to improvement in the prognosis of ES, raising the survival rates of up to 70%18,26,28,29. Other chemotherapeutics agents such as cisplatin and methotrexate have also been found to increase the prevalence of limb salvage surgery and to improve the 5-year survival rate to over 50% for bone sarcomas30, but those are not a part of the current treatment protocol for ES. Regardless of the positive influence on the survival rate of the patients, chemotherapy drugs have a number of side effects with high toxicity for many organ systems, such as kidneys, liver, heart, and nervous system, that remain a problem in the clinical setting31,32,33.
Looking for ways to solve this problem and to accelerate the arsenal against ES, cold physical plasma (CPP) has been suggested as a powerful tool in local anti-cancer therapy. Numerous studies have reported on the anti-oncological effect of CPP in many different types of cancer34, such as skin cancer35,36, breast cancer37,38,39, brain cancer40,41, and colon cancer42,43,44. On an experimental level, the inhibitory effects of CPP have also been demonstrated in the most common primary bone tumors, osteosarcoma and chondrosarcoma45,46,47,48,49, and also in ES50.
A strong inhibition of cell growth and viability of ES cells after CPP treatment has recently been reported and the advantages of combining CPP and the most commonly used chemotherapeutic agents in a clinically relevant in vitro setup51. The current study aims to evaluate whether CPP treatment leads to enhanced effectiveness of chemotherapeutic agents methotrexate (MTX) and cisplatin52 that have not yet been included in the list of "standard chemotherapy" against ES. Any opportunity to expand efficacy against ES is an advance that may impact patient care in ES therapy in the future.
Materials and methods
Ewing’s sarcoma cells
The Ewing sarcoma cell lines RD-ES (DSMZ-Deutsche Sammlung von Mikroorganismen und Zellkulturen, Braunschweig, Germany) and A673 (American Type Culture Collection, Manassa, VA, USA) were used in this study. Dulbecco’s modified Eagle’s medium (DMEM) and Roswell Park Memorial Institute 1640 medium (RPMI) were used for culturing the ES cells according to the producer's recommendation. DMEM contained 1.0 g/L glucose, 10% fetal bovine serum, 1 mM sodium pyruvate, and 1% penicillin/streptomycin, while RPMI 1640 contained 10% fetal bovine serum and 1% penicillin/streptomycin. The ES cell lines were grown under standardized conditions—(humidified atmosphere with 5% CO2 at 37 °C).
Chemotherapeutic agents
MTX and CIS (both from Cayman Chemical, Ann Arbor, MI, USA) were prepared by dissolving the dry substance in DMSO (Carl Roth, Karlsruhe, Germany). The stock concentrations for the chemotherapeutic agents were as follows: MTX 10 mM and CIS 1 mM. These solutions were then diluted to the final concentrations using DMSO.
Treatment with cold physical plasma
The kINPen® med device (neoplas tools, Greifswald, Germany) was used for CPP treatment. The plasma flame is generated in a plasma jet that is suitable for manual use. Argon (Alphagaz 1 AIR LIQUIDE, Düsseldorf, Germany) is used as the carrier gas with a flow rate of 3.5 standard liters/minute (slm). The CPP application took place after the cells had been seeded in a 24-well plate with 2 × 104 cells per 200 µL. The plasma flame was passed over this cell suspension with pendulum-like hand movements for different periods (5 s, 10 s, and 20 s). The control treatment of the cells was performed in the same way but without switching on the plasma device, i.e., only with the carrier gas argon.
Application of chemotherapeutic agents
The addition of chemotherapeutics was done as previously described54. Briefly, or each cell line, 2 × 104 cells per 200 µL of full medium were transferred to 6 wells of a 24-well plate. Subsequently, 800 µL of warm, fully-supplemented medium containing the corresponding cytostatic agent (MTX or CIS), dissolved at their determined IC20 values, was added to each well and incubated at 37 °C. As a control, a similar treatment with the carrier solution DMSO was carried out.
Combination treatment with cold physical plasma and chemotherapeutic agents
Both cell lines were seeded separately with 2 × 104 cells in 200 µL of full medium and directly exposed to CPP in the wells of a 24-well plate. After 5 s CPP exposure, 800 µL of warm, fully-supplemented medium containing the corresponding IC20 concentration of each cytostatic agent (MTX or CIS) was added to each well prior to incubation at 37 °C. Control cells were treated only with cytostatic agents.
Quantification of the population doublings
After performing a single treatment (either 2.3. isolated 5 s CPP application; or 2.4. exposure to chemotherapeutic agents; or 2.5. combined treatment), cells were incubated over a 120 h period. The number of living cells was determined using the CASY cell counter and analyzer (Roche Applied Science, Mannheim, Germany). The population doublings were calculated using the following formula: PDL = PDL0 + 3.322 (logCf − logCi).
CellTiter-Blue cell viability assay
The CellTiter-Blue cell viability assay (Promega, Walldorf, Germany) was utilized according to the assay protocol to determine the cell viability of cells after being treated either only with a chemotherapeutic agent or after a combined treatment of CPP and chemotherapeutic agent.
After incubation for 24 h, the ES cells were treated with MTX or CIS in different concentrations from 10–11 to 10–4 M. The cytostatic drug preparations were performed by diluting to the desired concentrations in DMSO. The solutions were further diluted 1:100 in fully-supplemented medium before being administered to the cells. The cells were then incubated for 72 h at 37 °C before cell viability quantification with the CellTiter-Blue reagent.
As a second experiment, a total of 100 µL of cell suspension containing 1 × 104 cells was seeded into 96-well plates and incubated for 24 h prior to the combination therapy. CPP treatment was carried out indirectly by transferring 200 µL of the full medium into the wells of a 24-well plate and treating each well with CPP for 5 s, 10 s, and 20 s. Then, 100 µL of the treated medium was added to the cells in the 96-well plates, followed by the addition of 100 µL of warm complete medium containing the cytostatic drug, and subsequently incubated at 37 °C for 72 h, followed by the determination of the cell viability using CellTiter-Blue reagent.
The CellTiter-Blue reagent was incubated for 1 h, and the formation of resorufin in living cells was detected using a multimode plate reader at 560 nm excitation and 590 nm emission wavelengths (TECAN, Männedorf, Switzerland). The fluorescence signals of the cells treated with the cytostatic drugs were then normalized to the signals of cells treated with DMSO (control) to determine their respective cell viability.
TUNEL assay
A total of 5.0 × 104 (24 h) and 2.0 × 104 (48 h) from the A673 cells and 4.0 × 104 (24 h) and 2.0 × 104 (48 h) RD-ES were seeded in 100 µL. This cell suspension was transferred to a 96-well plate for the respective treatments. After a 5 s CPP treatment was performed indirectly by treating 200 µL of a full medium, 100 µL of the treated medium was added to the seeded cells. An argon treatment for 5 s served as control. In the next step, an IC20 concentration of MTX or CIS was added to the cells. As a control, a combination of an argon treatment and cytostatic drugs was performed. Controls with untreated cells (1 negative and 1 positive; nuclease treated) were included on each plate. A corresponding second plate was treated in parallel to normalize the absorption values to cell numbers. The TUNEL assay (R&D Systems, Minneapolis, MN, USA) was performed 24 h or 48 h after treatment according to the manufacturer’s protocol using the TECAN multimode plate reader. The relative TUNEL signals of cells treated with CPP, cytostatic or combination therapy were normalized to the mean relative TUNEL signals of cells treated with argon gas alone (control).
Caspase assay
The CellEvent Caspase 3/7 green Detection Reagent (Thermo Fisher Scientific, Waltham, MA, USA) was used to detect apoptosis by performing the Caspase 3/7 assay. The detection reagent binds fluorescently to DNA, and DEVD peptide inhibits this binding. Upon activation of Caspases 3 and 7, the peptide is cleaved, allowing the binding to occur. The treatments were performed similarly to 2.8. After the incubation period (24 h and 48 h), the medium was carefully aspirated, and 100 µL of Caspase 3/7 detection solution was added to the wells of the 96-well plate. The plate was then incubated for 45 min at 37 °C. Following the 45-min incubation, fluorescence was measured using the TECAN multimode plate reader at 495 nm excitation and 535 nm emission wavelengths. The fluorescence per well was used to calculate the fluorescence per cell by deviding by the cell numbers determined using counting with the CASY device.. The relative Caspase 3/7 signals of cells treated with CPP, cytostatic, or combination therapy were normalized to the mean relative Caspase 3/7 signals of cells treated with argon gas only (control).
DNA damage detection
A total of 1.0 × 105 cells was seeded in 100 µL medium into a 96-well plate. The next day, cells were either treated with CPP followed by the addition of IC20 concentrations of CIS or MTX, or CPP, or cytostatic drugs alone, as described above (2.8). After 24 h incubation, the medium was discarded, and cells were washed carefully with DPBS. For fixation and permeabilization, cells were covered with ice-cold methanol for 30 min. After washing, cells were stained with PE-conjugated anti-ATM phospho and AF647-conjugated anti-H2A.X phospho antibodies (both Biolegend, Amsterdam, The Netherlands) for 30 min. Cells were washed again, and finally, 100 µL of PBS containing 4ʹ,6-diamidino-2-phenylindole (DAPI, 1 µM) were added to the cells to stain whole nuclei. Images were acquired using the high-content imaging system Operetta CLS (PerkinElmer, Hamburg, Germany) with a 20× objective, and quantification was performed using Harmony 4.9 software (PerkinElmer, Hamburg, Germany).
Statistical analysis
For data analysis and visualization, GraphPad Prism Version 9.1.2 (GraphPad Software Inc., La Jolla, CA, USA) was used. The results of p ≤ 0.05 of at least three independent experiments were considered significant, and data were given as the mean ± SD. Differences were examined using an ANOVA test or t-test, as indicated in the figure captions.
Results
Impact of chemotherapeutic agents on cell viability and proliferation
In order to investigate the influence of the chemotherapeutic agents CIS and MTX on ES cells A673 and RE-ED, these were incubated for 72 h with the chemotherapeutics in concentrations ranging from 10–11 M to 10–4 M. Cell viability (2.7) was determined after that. Both chemotherapeutic agents have inhibited the cell viability of A673 and RE-ED (Fig. 1). However, the chemotherapeutic agents had varying impacts on both ES cell lines. Using the maximum concentration of 100 µM of CIS, cell viability was reduced by approximately 50% in the cell line A673, and a 30% reduction in viability was observed in the cell line RD-ES. Using MTX in the same concentration, stronger inhibitory effects on the cell viability were achieved. For A673 cells, a reduction in cell viability of 80%, and for the RD-ES cell line, a reduction of 60% was shown. These effects and correlations have also been found by determination of the IC20 concentration of these chemotherapeutic agents. There were significant differences between the IC20 concentrations of CIS and MTX in both cell lines (p < 0.0001). IC20 of CIS was about 1000-fold higher than the IC20 of MTX (Fig. 1C,F).
Inhibitory effect of cisplatin and methotrexate on Ewing’s sarcoma cells. The Ewing’s sarcoma cell lines A673 (A–C) and RD-ES (D–F) were treated with cisplatin and methotrexate (MTX). After 72 h, the cell viability was determined, and the IC20 was calculated. Individual values are shown with a dose–response curve and the IC20 calculated from this (A,B,D,E) as well as mean values of the calculated IC20 (C,F). The mean values were examined with the t-test for significant differences, which were presented as follows: ****p < 0.0001.
Impact of combination of cold physical plasma and chemotherapeutic agents
A combined treatment of the cell lines with CPP and MTX or CIS led to a stronger inhibitory effect on the cell viability. These effects were dependent on the treatment time with CPP (Fig. 2). A combination of chemotherapeutics and CPP treatment for 10 s led to a shift in the dose–response curve towards lower cell viability. In cell line A673, the 10 s CPP treatment in combination with CIS and MTX below the effective threshold led to a reduction in cell viability of over 20%. In general, the additive effects were significantly milder in this cell line. In contrast, the additive effects of CPP and chemotherapeutics agents were observed in the cell line RD-ES over the entire concentration range investigated. While a single CIS treatment of the RD-ES cells, even at a concentration of 100 µM, led to a reduction of about 80%, the combination with CPP achieved a reduction in cell viability of less than 40%. A combination of the chemotherapeutic agents with 20 s CPP led to a further reduction in cell viability in all cell lines. In the RD-ES cell line, the 20 s CPP treatment was already so effective below the threshold of the chemotherapeutics that the cells were almost completely obliterated. Thus, no further effect could be observed by increasing the concentration of chemotherapeutic agents. Experiments to cell population doubling confirm these results. A combination of CPP and chemotherapeutic agents can improve the effectiveness compared to treatment alone (Fig. 3). Thus, the population doublings of A673 cells were reduced from 4.4 to 3.7 after 5 s CPP treatment. Reductions to − 0.952 or 0.67 (MTX) could be achieved through the combination of CPP and chemotherapeutics. The effects on the RD-ES cells were similar. CPP treatment alone reduced the population doublings from 5.13 to 3.66, the combination with CIS to 0.59, and the combination with MTX to 0.76.
Effect of a combined treatment of ES cell lines with CPP and chemotherapeutics. The Ewings sarcoma cell lines A673 (A,B) and RD-ES (C,D) were treated with CPP combined with the chemotherapeutic agents cisplatin and methotrexate (MTX). Cell viability was determined after 72 h. Shown are individual values with dose–response curves.
Effects of CPP treatment combined with chemotherapeutic agents on cell population doubling. A673 cells (A,B) and RD-ES cells (C,D) were treated with CPP and a combination of CPP and cytostatics. The number of living cells was determined after 120 h of incubation and the population of doublings was calculated. Mean values are shown. Significant differences were determined using ANOVA and Tukey's multiple comparisons test and are reported as follows (*p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001, ****p ≤ 0.0001).
Cell apoptosis and DNA damage after combined treatment of cold physical plasma and chemotherapeutic agents
To examine the mechanism of cell death, apoptosis assays (caspase 3/7 activation, and TUNEL) were performed. The cells were treated with CPP for 5 s prior to cytostatic treatment at the determined IC20 (Fig. 4). In A673 cells, CPP treatment alone led to a significant increase in the caspase 3/7 activity and TUNEL signal both after 24 h and after 48 h compared to the control treatment (Fig. 4A,B). The combination of CPP and MTX treatment led to a significantly increased caspase 3/7 activity after 48 h (Fig. 4I,J). The CPP treatment of the RD-ES cells only increased the caspase 3/7 activity after 24 h. After 48 h, no significant increase in the signal could be detected. In the TUNEL assay, we could detect a significant increase in the signal both after 24 h and 48 h (Fig. 4C,D). A combination of CPP and MTX led to a significant increase in caspase activity and relative TUNEL signal after 24 h in RD-ES cells (Fig. 4K,L). The combination of CPP and CIS led to increased apoptotic signals in both cell lines;, however, this was not statistically significant (Fig. 4E–H).
Apoptosis induction by the combination of CPP and cytostatic agents. To evaluate the apoptotic effect of combination therapy of the cell lines A673 and RD-ES Caspase 3/7 activity assay and TUNEL assay were used. The relative Caspase 3/7 signals and TUNEL signals of cells treated with CPP and combination therapy were normalized to the relative Caspase 3/7 signals and TUNEL signals of cells treated with Argon (control). The mean values ± SD are depicted in the graphs and were assessed for statistically significant differences using paired t-tests (*p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001).
To further investigate toxic effects of CPP and cytostatic treatment, A673 cells were stained against the DNA damage markers pATM and yH2AX 24 h after IC20 single treatment or combination treatment (Fig. 5A). Formation of pATM or yH2AX foci in the nuclei (Fig. 5B) was quantified as mean fluorescence intensity (MFI) over all detected nuclei (Fig. 5C,D). In A673 cells, a significant increase of nuclear pATM was detected after CPP and CIS treatment, while MTX did not increase pATM (Fig. 5C). The combination of CPP and cytostatic drugs did not cause an additional increase in pATM. Significant formation of yH2AX foci was observed upon CPP as well as CIS and MTX single treatments (Fig. 5D). No additional increase of yH2AX but rather a decrease was visible in the case of combination treatments.
DNA damage marker formation upon CPP and chemotherapeutics treatment. A673 cells were stained 24 h after treatment with CPP, CIS, MTX, or combinations of these (A) to investigate the formation of nuclear pATM and yH2AX foci (B). Images were quantified by calculating the mean fluorescence intensity (MFI) of pATM (C) and yH2AX (D) in all detected nuclei of treated cells against untreated controls. The mean values ± SD are depicted in the graphs and were assessed for statistically significant differences using one-way ANOVA and Šídák's multiple comparisons test (*p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001).
Discussion
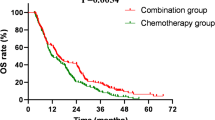
Since its introduction in the 1970s, chemotherapy has significantly improved the outcomes of patients with ES and is now an integral part of their treatment. A clear advantage over monotherapy has been shown in combination therapy with different drugs53,54. Besides the use of doxorubicin and vincristine, the use of ifosfamide, alone or in combination with etoposide, showed very good results in patients with ES and is currently part of the standard protocol for ES treatment55,56,57,58. The current 5-year survival rate varies and is 75% for patients with localized ES manifestations, around 50% for patients with isolated lung metastases, and less than 30% for people with primary metastases59,60,61.
The use of high doses of chemotherapeutic agents is associated with increasing their toxic effects on the patient62,63. A dose reduction with a constant effect of the chemotherapeutic agent would, therefore, be desirable. Such a dose reduction with the same effect on ES cell lines has been demonstrated with the combination of chemotherapeutic agents doxorubicin or vincristine and CPP51.
CPP treatment seems to be considered a possible anti-cancer tool that supports the effects of chemotherapy, not least because of its selective effect on tumor cells39,64,65. CPP treatment alone can significantly impact the viability of Ewing sarcoma cells by inducing apoptosis, disrupting cell proliferation, and inhibiting tumor growth50. While CPP treatment shows promising results in targeting cancer cells locally, its efficacy as a stand-alone therapy may not surpass that of chemotherapy in all cases. Despite its systemic nature, chemotherapy often remains a cornerstone of cancer treatment due to its ability to reach metastatic sites and eradicate disseminated tumor cells. The effect of the chemotherapeutic agents unfolds through binding to DNA and the production of ROS in the cells66. The action of CPP on various cancer cells unfolds in different ways—some of them, like apoptosis and DNA damage46,50, are very similar to the anti-oncogenic mechanism of action of chemotherapeutic agents. Thus, these two methods are able to complement their effects so that the dosage of the cytostatic can be reduced in order to achieve the desired effects45. A number of studies with different tumor entities have demonstrated the high efficiency of the combination of CPP and different chemotherapy agents67,68,69,70,71,72. The current study raised the question of whether the spectrum of anti-ES chemotherapy drugs can be expanded by combining them with CPP. MTX and CIS were frequently chosen for this in the treatment of other bone sarcomas. MTX is an effective therapeutic agent not only for treating many solid tumors but also autoimmune diseases. However, its use is limited by poor pharmacokinetics73. Among many chemotherapy drugs that are widely used for cancer, CIS is one of the most compelling ones74. It is effective against various types of cancer, including various sarcomas. Its mode of action has been linked to its ability to cross-link with the purine bases on DNA, causing damage to the cancer cells66,75. CPP also builds up its effect against cancer cells via similar mechanisms of action, so their combination can likely have a synergistic effect46,50.
This study showed that the isolated CPP treatment of the ES cells inhibited their proliferation capacity. A limitation of tumor treatment with CPP is its local intraoperative application. Disseminated individual cells or metastases cannot be addressed during tumor resection. Thus, CPP treatment only achieves a local effect. Therefore, it is of particular importance to consider CPP as a potential complementary therapeutic option in combination with established treatment modalities such as resection and systemic chemotherapy. Incorporating CPP into a multimodality treatment approach may more effectively target heterogeneous cancer cell populations, which could lead to better long-term outcomes for patients with Ewing's sarcoma. While CPP treatment alone is promising, combining it with chemotherapy is a rational strategy to maximize therapeutic efficacy and minimize adverse effects in the treatment of ES. The treatment of both cell lines A673 and RD-ES with CCP combined with MTX or CIS significantly increased their antiproliferative effect. The combination treatment also reduced cell viability, as these effects were CPP treatment time-dependent. Thus, a CPP treatment of 20 s CPP treatment even led to a complete reduction in cell viability of the ES cells. These results can be compared with the effects of the combined treatment of ES cells by CPP and the conventional chemotherapeutic agents typically used in clinical settings for these sarcomas, such as doxorubicin and vincristine51.
One of the main anti-oncogenic factors generated by CPP is the reactive species, which leads to apoptosis in cancer cells71,72. This mechanism of action has also been demonstrated specifically in bone cancer cells such as osteosarcoma and chondrosarcoma48,49,76,77, but also in ES cells50. The cytotoxic effect of CIS can also be explained by the inhibition of replication by cisplatin–DNA adducts and the induction of apoptosis78.
The combination of CPP treatment with chemotherapy may lead to increased tumor cell toxicity through several mechanisms. One possible mechanism is that the combination of CPP with cytostatic agents may lead to additive effects in cancer cells by enhancing drug uptake and increasing intracellular ROS induction71. In particular, CPP has been shown to increase the permeability of cell membranes, facilitating the entry of chemotherapeutic agents into cancer cells50. Furthermore, CPP treatment may synergize with specific chemotherapy drugs. For example, CPP-induced reactive oxygen and nitrogen species (ROS/RNS) production can interfere with DNA repair mechanisms, thereby sensitizing cancer cells to DNA-damaging agents like CIS. Similarly, CPP may modulate cellular signaling pathways involved in folate metabolism, potentiating the cytotoxic effects of MTX. Overall, the combination of CPP with chemotherapy can lead to increased toxicity of tumor cells by improving drug uptake, disrupting metabolic pathways that promote survival and achieving synergistic effects with specific chemotherapeutic agents. These effects ultimately lead to better treatment outcomes and can help to overcome the resistance mechanisms that often occur in cancer therapy. In-virto studies using mouse models were used to investigate the toxicity of individual CPP and chemotherapy treatments by analyzing biochemical markers in the liver and kidney. The results show that cold plasma significantly reduces the side effects of cytostatics (DOX)79. The combination treatment with CPP and cytostatics led to varying degrees of activation of apoptosis in each of the ES cell lines. In an in vitro study80, similar effects were found when combining CPP with low-dose CIS in head and neck squamous cell carcinomas cells, evaluating the cell viability, DNA damage, and apoptosis after this treatment58. The results of the current study indicate that concomitant treatment of CPP and chemotherapeutic drugs, like MTX and CIS, not included in the current ES treatment protocol, is promising in ES therapy.
Although the use of MTX and CIS in this study was effective against ES at the cellular level, these results cannot be prematurely extrapolated to the clinical treatment of ES. While there are reports of the use of CIS in the clinical setting, the use of CIS is part of a combination with other chemotherapeutic agents or as anecdotal reports81. The recommendation for the clinical use of chemotherapeutic agents does not only depend on the response of the specific cancer cell lines but also requires the consideration of many other factors, such as pharmacological properties, side effects, and interactions with other drugs in the treatment protocol. A number of preclinical and clinical studies are necessary to make such recommendations. However, an important finding from this study is the efficacy and interaction of chemotherapeutic agents and CPP in ES cells.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
van Oosterwijk, J. G., Anninga, J. K., Gelderblom, H., Cleton-Jansen, A. M. & Bovée, J. V. Update on targets and novel treatment options for high-grade osteosarcoma and chondrosarcoma. Hematol. Oncol. Clin. N. Am. 27, 1021–1048. https://doi.org/10.1016/j.hoc.2013.07.012 (2013).
Chow, W. A. Chondrosarcoma: Biology, genetics, and epigenetics. F1000Research 7, 25. https://doi.org/10.12688/f1000research.15953.1 (2018).
Spector, L. G. et al. Comparative international incidence of Ewing sarcoma 1988 to 2012. Int. J. Cancer 149, 1054–1066. https://doi.org/10.1002/ijc.33674 (2021).
Worch, J. et al. Racial differences in the incidence of mesenchymal tumors associated with EWSR1 translocation. Cancer Epidemiol. Biomark. Prev. 20, 449–453. https://doi.org/10.1158/1055-9965.Epi-10-1170 (2011).
Nakata, K. et al. Childhood cancer incidence and survival in Japan and England: A population-based study (1993–2010). Cancer Sci. 109, 422–434. https://doi.org/10.1111/cas.13457 (2018).
Fraumeni, J. F. Jr. & Glass, A. G. Rarity of Ewing’s sarcoma among US Negro children. Lancet 1, 366–367. https://doi.org/10.1016/s0140-6736(70)90754-3 (1970).
Li, F. P., Tu, J. T., Liu, F. S. & Shiang, E. L. Rarity of Ewing’s sarcoma in China. Lancet 1, 1255. https://doi.org/10.1016/s0140-6736(80)91719-5 (1980).
Glass, A. G. & Fraumeni, J. F. Jr. Epidemiology of bone cancer in children. J. Natl. Cancer Inst. 44, 187–199 (1970).
Grünewald, T. G. P. et al. Ewing sarcoma. Nat. Rev. Dis. Primers 4, 5–5. https://doi.org/10.1038/s41572-018-0003-x (2018).
Romeo, S. & Dei Tos, A. P. Soft tissue tumors associated with EWSR1 translocation. Virch. Arch. 456, 219–234. https://doi.org/10.1007/s00428-009-0854-3 (2010).
Fisher, C. The diversity of soft tissue tumours with EWSR1 gene rearrangements: A review. Histopathology 64, 134–150. https://doi.org/10.1111/his.12269 (2014).
Agaram, N. P., Zhang, L., Sung, Y. S., Singer, S. & Antonescu, C. R. Extraskeletal myxoid chondrosarcoma with non-EWSR1-NR4A3 variant fusions correlate with rhabdoid phenotype and high-grade morphology. Hum. Pathol. 45, 1084–1091. https://doi.org/10.1016/j.humpath.2014.01.007 (2014).
Lynch, A. D. et al. Extraskeletal versus skeletal ewing sarcoma in the adult population: Controversies in care. Surg. Oncol. 27, 373–379. https://doi.org/10.1016/j.suronc.2018.05.016 (2018).
Jahanseir, K. et al. Ewing sarcoma in older adults: A clinicopathologic study of 50 cases occurring in patients aged ≥ 40 years, with emphasis on histologic mimics. Int. J. Surg. Pathol. 28, 352–360. https://doi.org/10.1177/1066896919893073 (2020).
Biswas, B. et al. Evaluation of outcome and prognostic factors in extraosseous Ewing sarcoma. Pediatr. Blood Cancer 61, 1925–1931. https://doi.org/10.1002/pbc.25095 (2014).
Perlman, E. J. et al. Ewing’s sarcoma–routine diagnostic utilization of MIC2 analysis: A Pediatric Oncology Group/Children’s Cancer Group Intergroup Study. Hum. Pathol. 25, 304–307. https://doi.org/10.1016/0046-8177(94)90203-8 (1994).
Widhe, B. & Widhe, T. Initial symptoms and clinical features in osteosarcoma and Ewing sarcoma. J. Bone Jt. Surg. Am. 82, 667–674. https://doi.org/10.2106/00004623-200005000-00007 (2000).
Riggi, N. & Stamenkovic, I. The biology of Ewing sarcoma. Cancer Lett. 254, 1–10. https://doi.org/10.1016/j.canlet.2006.12.009 (2007).
Sankar, S. & Lessnick, S. L. Promiscuous partnerships in Ewing’s sarcoma. Cancer Genet. 204, 351–365. https://doi.org/10.1016/j.cancergen.2011.07.008 (2011).
Gargallo, P. et al. Review: Ewing sarcoma predisposition. Pathol. Oncol. Res. 26, 2057–2066. https://doi.org/10.1007/s12253-019-00765-3 (2020).
Cripe, T. P. Ewing sarcoma: An eponym window to history. Sarcoma 2011, 457532. https://doi.org/10.1155/2011/457532 (2011).
Heck, R. K. Jr., Peabody, T. D. & Simon, M. A. Staging of primary malignancies of bone. CA Cancer J. Clin. 56, 366–375. https://doi.org/10.3322/canjclin.56.6.366 (2006).
Cotterill, S. J. et al. Prognostic factors in Ewing’s tumor of bone: Analysis of 975 patients from the European Intergroup Cooperative Ewing’s Sarcoma Study Group. J. Clin. Oncol. 18, 3108–3114. https://doi.org/10.1200/jco.2000.18.17.3108 (2000).
Cangir, A. et al. Ewing’s sarcoma metastatic at diagnosis Results and comparisons of two intergroup Ewing’s sarcoma studies. Cancer 66, 887–893. https://doi.org/10.1002/1097-0142(19900901)66:5%3c887::aid-cncr2820660513%3e3.0.co;2-r (1990).
Fisher, B. & Wolmark, N. The current status of systemic adjuvant therapy in the management of primary breast cancer. Surg. Clin. N. Am. 61, 1347–1360. https://doi.org/10.1016/S0039-6109(16)42589-2 (1981).
Grier, H. E. et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumor of bone. N. Engl. J. Med. 348, 694–701. https://doi.org/10.1056/NEJMoa020890 (2003).
Rosen, G. et al. Combination chemotherapy (T-6) in the multidisciplinary treatment of Ewing’s sarcoma. Natl. Cancer Inst. Monogr. 20, 289–299 (1981).
Paulussen, M. et al. Localized Ewing tumor of bone: Final results of the cooperative Ewing’s Sarcoma Study CESS 86. J. Clin. Oncol. 19, 1818–1829. https://doi.org/10.1200/jco.2001.19.6.1818 (2001).
Womer, R. B. et al. Randomized controlled trial of interval-compressed chemotherapy for the treatment of localized Ewing sarcoma: A report from the Children’s Oncology Group. J. Clin. Oncol. 30, 4148–4154. https://doi.org/10.1200/jco.2011.41.5703 (2012).
Han, G., Bi, W. Z., Xu, M., Jia, J. P. & Wang, Y. Amputation versus limb-salvage surgery in patients with osteosarcoma: A meta-analysis. World J. Surg. 40, 2016–2027. https://doi.org/10.1007/s00268-016-3500-7 (2016).
Crona, D. J. et al. A systematic review of strategies to prevent cisplatin-induced nephrotoxicity. Oncologist 22, 609–619. https://doi.org/10.1634/theoncologist.2016-0319 (2017).
Al-malky, H. S., AlHarthi, S. E. & Osman, A.-M.M. Major obstacles to doxorubicin therapy: Cardiotoxicity and drug resistance. J. Oncol. Pharm. Pract. 26, 434–444. https://doi.org/10.1177/1078155219877931 (2020).
Ghosh, S. Cisplatin: The first metal based anticancer drug. Bioorg. Chem. 88, 102925. https://doi.org/10.1016/j.bioorg.2019.102925 (2019).
Bekeschus, S. Medical gas plasma technology: Roadmap on cancer treatment and immunotherapy. Redox. Biol. 65, 102798. https://doi.org/10.1016/j.redox.2023.102798 (2023).
Binenbaum, Y. et al. Cold atmospheric plasma, created at the tip of an elongated flexible capillary using low electric current, can slow the progression of melanoma. PLoS One 12, e0169457. https://doi.org/10.1371/journal.pone.0169457 (2017).
Miebach, L. et al. Medical gas plasma technology combines with antimelanoma therapies and promotes immune-checkpoint therapy responses. Adv. Sci. 10, e2303183. https://doi.org/10.1002/advs.202303183 (2023).
Xiang, L., Xu, X., Zhang, S., Cai, D. & Dai, X. Cold atmospheric plasma conveys selectivity on triple negative breast cancer cells both in vitro and in vivo. Free Radic. Biol. Med. 124, 205–213. https://doi.org/10.1016/j.freeradbiomed.2018.06.001 (2018).
Mahdikia, H. et al. Gas plasma irradiation of breast cancers promotes immunogenicity, tumor reduction, and an abscopal effect in vivo. Oncoimmunology 10, 1859731. https://doi.org/10.1080/2162402X.2020.1859731 (2020).
Chupradit, S. et al. Recent advances in cold atmospheric plasma (CAP) for breast cancer therapy. Cell Biol. Int. 47, 327–340. https://doi.org/10.1002/cbin.11939 (2023).
Chen, Z. et al. A novel micro cold atmospheric plasma device for glioblastoma both in vitro and in vivo. Cancers (Basel) https://doi.org/10.3390/cancers9060061 (2017).
Adhikari, M. et al. Cold atmospheric plasma as a novel therapeutic tool for the treatment of brain cancer. Curr. Pharm. Des. 26, 2195–2206. https://doi.org/10.2174/1381612826666200302105715 (2020).
Miebach, L. et al. Gas plasma-oxidized sodium chloride acts via hydrogen peroxide in a model of peritoneal carcinomatosis. Proc. Natl. Acad. Sci. USA 119, e2200708119. https://doi.org/10.1073/pnas.2200708119 (2022).
Vandamme, M. et al. ROS implication in a new antitumor strategy based on non-thermal plasma. Int. J. Cancer 130, 2185–2194. https://doi.org/10.1002/ijc.26252 (2012).
Ishaq, M., Evans, M. D. & Ostrikov, K. K. Atmospheric pressure gas plasma-induced colorectal cancer cell death is mediated by Nox2–ASK1 apoptosis pathways and oxidative stress is mitigated by Srx–Nrf2 anti-oxidant system. Biochim. Biophys. Acta Mol. Cell Res. 1843, 2827–2837 (2014).
Mateu-Sanz, M., Tornín, J., Ginebra, M. P. & Canal, C. Cold atmospheric plasma: A new strategy based primarily on oxidative stress for osteosarcoma therapy. J. Clin. Med. https://doi.org/10.3390/jcm10040893 (2021).
Nitsch, A. et al. New approach against chondrosoma cells—cold plasma treatment inhibits cell motility and metabolism, and leads to apoptosis. Biomedicines 10, 688 (2022).
Ermakov, A. M., Ermakova, O. N., Afanasyeva, V. A. & Popov, A. L. Dose-dependent effects of cold atmospheric argon plasma on the mesenchymal stem and osteosarcoma cells in vitro. Int. J. Mol. Sci. 22, 6797 (2021).
Mateu-Sanz, M. et al. Cold plasma-treated ringer’s saline: A weapon to target osteosarcoma. Cancers 12, 227 (2020).
Haralambiev, L. et al. Cold atmospheric plasma treatment of chondrosarcoma cells affects proliferation and cell membrane permeability. Int. J. Mol. Sci. 21, 2291 (2020).
Jacoby, J. M. et al. An innovative therapeutic option for the treatment of skeletal sarcomas: Elimination of osteo-and Ewing’s sarcoma cells using physical gas plasma. Int. J. Mol. Sci. 21, 4460 (2020).
Nitsch, A. et al. Enhancing the impact of chemotherapy on Ewing sarcoma cells through combination with cold physical plasma. Int. J. Mol. Sci. 24, 8669 (2023).
Tabares, F. L. & Junkar, I. Cold plasma systems and their application in surface treatments for medicine. Molecules 26, 1903 (2021).
Pomeroy, A. E., Schmidt, E. V., Sorger, P. K. & Palmer, A. C. Drug independence and the curability of cancer by combination chemotherapy. Trends Cancer 8, 915–929. https://doi.org/10.1016/j.trecan.2022.06.009 (2022).
Haveman, L. M. et al. High-dose chemotherapy followed by autologous haematopoietic cell transplantation for children, adolescents, and young adults with primary metastatic Ewing sarcoma. Cochrane Database Syst. Rev. 9, Cd011405. https://doi.org/10.1002/14651858.CD011405.pub2 (2021).
Nesbit, M. E. Jr. et al. Multimodal therapy for the management of primary, nonmetastatic Ewing’s sarcoma of bone: A long-term follow-up of the First Intergroup study. J. Clin. Oncol. 8, 1664–1674. https://doi.org/10.1200/jco.1990.8.10.1664 (1990).
Greene, W. et al. High-dose daunorubicin therapy for acute nonlymphocytic leukemia: Correlation of response and toxicity with pharmacokinetics and intracellular daunorubicin reductase activity. Cancer 30, 1419–1427. https://doi.org/10.1002/1097-0142(197212)30:6%3c1419::AID-CNCR2820300602%3e3.0.CO;2-I (1972).
Antman, K. H., Ryan, L., Elias, A., Sherman, D. & Grier, H. E. Response to ifosfamide and mesna: 124 previously treated patients with metastatic or unresectable sarcoma. J. Clin. Oncol. 7, 1369–1369 (1989).
Jürgens, H. et al. High-dose ifosfamide with mesna uroprotection in Ewing’s sarcoma. Cancer Chemother. Pharmacol. 24, S40–S44 (1989).
Gorlick, R., Janeway, K., Lessnick, S., Randall, R. L. & Marina, N. Children’s Oncology Group’s 2013 blueprint for research: Bone tumors. Pediatr. Blood Cancer 60, 1009–1015. https://doi.org/10.1002/pbc.24429 (2013).
Ladenstein, R. et al. Primary disseminated multifocal Ewing sarcoma: Results of the Euro-EWING 99 trial. J. Clin. Oncol. 28, 3284–3291. https://doi.org/10.1200/jco.2009.22.9864 (2010).
Dirksen, U. et al. High-dose chemotherapy compared with standard chemotherapy and lung radiation in Ewing sarcoma with pulmonary metastases: Results of the european ewing tumour working initiative of national groups, 99 trial and EWING 2008. J. Clin. Oncol. 37, 3192–3202. https://doi.org/10.1200/jco.19.00915 (2019).
Zraik, I. M. & Heß-Busch, Y. Management von Nebenwirkungen der Chemotherapie und deren Langzeitfolgen. Der Urologe 60, 862–871 (2021).
Schirrmacher, V. From chemotherapy to biological therapy: A review of novel concepts to reduce the side effects of systemic cancer treatment. Int. J. Oncol. 54, 407–419 (2019).
Faramarzi, F. et al. Cold physical plasma in cancer therapy: Mechanisms, signaling, and immunity. Oxid. Med. Cell Longev. 2021, 9916796. https://doi.org/10.1155/2021/9916796 (2021).
Nitsch, A. et al. Selective effects of cold atmospheric plasma on bone sarcoma cells and human osteoblasts. Biomedicines 11, 25 (2023).
Ibañez, I. L., Notcovich, C., Catalano, P. N., Bellino, M. G. & Durán, H. The redox-active nanomaterial toolbox for cancer therapy. Cancer Lett. 359, 9–19 (2015).
Boeckmann, L. et al. Synergistic effect of cold gas plasma and experimental drug exposure exhibits skin cancer toxicity in vitro and in vivo. J. Adv. Res. https://doi.org/10.1016/j.jare.2023.06.014 (2023).
Murillo, D., Huergo, C., Gallego, B., Rodríguez, R. & Tornín, J. Exploring the use of cold atmospheric plasma to overcome drug resistance in cancer. Biomedicines 11, 208 (2023).
Daeschlein, G. et al. Enhanced Anticancer efficacy by drug chemotherapy and cold atmospheric plasma against melanoma and glioblastoma cell lines in vitro. IEEE Trans. Radiat. Plasma Med. Sci. 2, 153–159. https://doi.org/10.1109/TRPMS.2018.2789659 (2018).
Gandhirajan, R. K. et al. The amino acid metabolism is essential for evading physical plasma-induced tumour cell death. Br. J. Cancer 124, 1854–1863. https://doi.org/10.1038/s41416-021-01335-8 (2021).
Pefani-Antimisiari, K. et al. Synergistic effect of cold atmospheric pressure plasma and free or liposomal doxorubicin on melanoma cells. Sci. Rep. 11, 14788. https://doi.org/10.1038/s41598-021-94130-7 (2021).
Sagwal, S. K., Pasqual-Melo, G., Bodnar, Y., Gandhirajan, R. K. & Bekeschus, S. Combination of chemotherapy and physical plasma elicits melanoma cell death via upregulation of SLC22A16. Cell Death Dis. 9, 1179. https://doi.org/10.1038/s41419-018-1221-6 (2018).
Abolmaali, S. S., Tamaddon, A. M. & Dinarvand, R. A review of therapeutic challenges and achievements of methotrexate delivery systems for treatment of cancer and rheumatoid arthritis. Cancer Chemother. Pharmacol. 71, 1115–1130. https://doi.org/10.1007/s00280-012-2062-0 (2013).
Kelland, L. The resurgence of platinum-based cancer chemotherapy. Nat. Rev. Cancer 7, 573–584. https://doi.org/10.1038/nrc2167 (2007).
Dasari, S. & Tchounwou, P. B. Cisplatin in cancer therapy: Molecular mechanisms of action. Eur. J. Pharmacol. 740, 364–378. https://doi.org/10.1016/j.ejphar.2014.07.025 (2014).
Utsumi, F. et al. Effect of indirect nonequilibrium atmospheric pressure plasma on anti-proliferative activity against chronic chemo-resistant ovarian cancer cells in vitro and in vivo. PLoS One 8, e81576–e81576. https://doi.org/10.1371/journal.pone.0081576 (2013).
Sarangapani, C. et al. Degradation kinetics of cold plasma-treated antibiotics and their antimicrobial activity. Sci. Rep. 9, 1–15 (2019).
Siddik, Z. H. Cisplatin: Mode of cytotoxic action and molecular basis of resistance. Oncogene 22, 7265–7279. https://doi.org/10.1038/sj.onc.1206933 (2003).
Dezhpour, A., Ghafouri, H., Jafari, S. & Nilkar, M. Effects of cold atmospheric-pressure plasma in combination with doxorubicin drug against breast cancer cells in vitro and in vivo. Free Radic. Biol. Med. 209, 202–210. https://doi.org/10.1016/j.freeradbiomed.2023.10.405 (2023).
Brunner, T. F. et al. Primary cold atmospheric plasma combined with low dose cisplatin as a possible adjuvant combination therapy for HNSCC cells-an in-vitro study. Head Face Med. 18, 21. https://doi.org/10.1186/s13005-022-00322-5 (2022).
Trizzino, A. et al. Dramatic response to Cisplatin window therapy in a boy with advanced metastatic ewing sarcoma. J. Pediatr. Hematol. Oncol. 35, 478–481. https://doi.org/10.1097/MPH.0b013e31829d452c (2013).
Funding
Open Access funding enabled and organized by Projekt DEAL. We acknowledge support for the Article Processing Charge from the DFG (German Research Foundation, 393148499) and the Open Access Publication Fund of the University of Greifswald. A.N. and J.S. receive the Domagk Master Class (DMC) scholarship funded by the University Medicine Greifswald. S.Q. receives the Domagk scholarship funded by the University Medicine Greifswald.
Author information
Authors and Affiliations
Contributions
Conceptualization and methodology, L.H., M.V.T., A.N., A.E. and. G.I.W.; investigation and formal analysis, S.R., L.H., A.N., D.S., and S.Q.; resources, M.V.T., G.I.W., A.E., S.B., J.S., and L.H.; data curation, M.V.T., L.H., S.Q, A.N., D.S., S.B., S.R., and G.I.W.; writing—original draft preparation, A.N., S.Q., S.R., and L.H.; writing—review and editing, M.V.T., J.S., G.I.W., D.S., S.B., and A.E. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nitsch, A., Qarqash, S., Römer, S. et al. Effective combination of cold physical plasma and chemotherapy against Ewing sarcoma cells in vitro. Sci Rep 14, 6505 (2024). https://doi.org/10.1038/s41598-024-56985-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-56985-4
Keywords
This article is cited by
-
Atopic dermatitis: diagnosis, molecular pathogenesis, and therapeutics
Molecular Biomedicine (2025)
-
Small round cell sarcoma tumoroid biobank reveals CIC::DUX4 sarcoma vulnerability to MCL-1 inhibition
Nature Communications (2025)