Abstract
Previous studies have examined the prevalence of allergic diseases in adolescents 1–2 years after the emergence of the COVID-19 pandemic. However, more data is needed to understand the long-term impact of COVID-19 on allergic diseases. Thus, we aimed to examine the trend of the atopic dermatitis prevalence in Korean adolescents before and during the COVID-19 pandemic across 14 years. Additionally, we analyze the risk factors of atopic dermatitis (AD) based on the results. The Korean Disease Control and Prevention Agency conducted the Korea Youth Risk Behavior Web-based Survey from 2009 to 2022, from which the data for this study were obtained. Prevalence trends were compared across subgroups, and the β difference (βdiff) was calculated. We computed odds ratios to examine changes in the disease prevalence before and during the pandemic. This study included a total of 917,461 participants from 2009 to 2022. The prevalence of atopic dermatitis increased from 6.79% (95% CI 6.66–6.91) in 2009–2011 to 6.89% (95% CI 6.72–7.05) in 2018–2019, then decreased slightly to 5.82% (95% CI 5.60–6.04) in 2022. Across the 14 years, middle school student status, low parent’s highest education level, low household income, non-alcohol consumption, non-smoker smoking status, no suicidal thoughts, and no suicide attempts were associated with increased risk of atopic dermatitis, while female sex, rural residence, high BMI, low school performance, low household income, and no feelings of sadness and despair was associated with a small increase. This study examined the prevalence of atopic dermatitis across an 18-year, and found that the prevalence increased in the pre-pandemic then decreased during the start of the pandemic and remained constant throughout the pandemic. This trend could be explained mainly by the large scale social and political changes that occurred during the COVID-19 pandemic.
Similar content being viewed by others
Introduction
The COVID-19 pandemic has brought about changes in various aspects, including daily life and hospital treatment. Furthermore, the South Korean government recommended the use of masks not only for individuals exhibiting respiratory symptoms but also for healthy members of the general public as part of a nationwide effort to prevent and control the spread of infection. Such changes brought about by COVID-19 may have also impacted the prevalence and condition of skin-related diseases1. Therefore, it is necessary to compare the prevalence of skin-related ailments before and after the COVID-19 pandemic, as well as to analyze prevalence rates during the period of the pandemic2,3. For this reason, it is imperative to focus special attention on the changes in specific diseases, particularly atopic dermatitis (AD), following COVID-19. The prolonged exposure of the skin to warm and humid conditions, as experienced with mask wearing, can exacerbate AD. Among the diseases that have undergone changes after COVID-19, we are particularly interested in AD.
AD is a widely encountered condition, affecting 15–20% of adolescents1,4,5,6. Additionally, although AD is not a fatal disease with a low mortality rate, it can recur and has a negative impact on people’s health and quality of life7,8. Therefore, there is a need for further research about AD including COVID-19 pandemic. However, there has been a lack of studies analyzing and interpreting the prevalence of AD up to 2022. Since the COVID-19 pandemic occurred over a short period starting from 2020, it is essential to conduct detailed analysis including the most recent data9,10,11,12,13. Additionally, whereas previous studies lacked investigation into risk factors or their utilization of invalidated definitions of AD such as claim-based codes11, we identify risk factors influencing AD by analyzing the data including information up to 2022.
Therefore, our study aims to analyze the changing prevalence of AD before and after pandemic and to conduct an analysis considering the changed situation in 2022, including the risk factors. Based on this analysis, we aim to identify risk factors that influence AD and present a new perspective on AD after 2022, including aspects that have not been considered.
Methods
Patient selection and data collection
In this study, we used data from the Korea Youth Risk Behavior Web-based Survey (KYRBS) from 2009 to 202214,15. The KYRBS is an online survey administered to Korean adolescents in computer laboratories at their schools, and it utilizes a self-reporting method that monitors the health and behavior of Korean youths while being supervised by the Korean Disease Control and Prevention Agency (KDCA)9,16. This data includes information about behaviors and health such as smoking, drinking, physical activity, and allergic diseases. To ensure that the survey data reflects the entire Korean population, it employs sample selection methods such as stratified cluster sampling and two-step stratification16,17. And the weighting is calculated by multiplying the inverse of the sampling rate by the inverse of the response rate, and then multiplying this by the post-adjustment weighting rate16. The data collected included all adolescents aged 13–18 years with a response rate over 95% while participants with missing data were excluded. The research protocol received approval from both the Institutional Review Board of Kyung Hee University (KHUH 2022-06-042) and the KDCA. Written informed consent was obtained from all participants prior to their involvement in the study. Additionally, the KYRBS provides public access to its data, making it a valuable resource for conducting various epidemiological investigations. This research adhered to the ethical guidelines established by relevant national, and institutional review boards for human research and followed the 1975 Helsinki Declaration, as amended in 2008.
Ascertainment of AD
Our research aimed to confirm the trend in the prevalence of AD among adolescents from 2009 to 202216,18. Additionally, the objective of our study was to investigate the risk factors associated with atopic dermatitis. Patients with AD were defined by positive responses to two questions: “Have you ever been diagnosed AD by a doctor within the past 12 months?” and “Have you ever been diagnosed AD by a doctor throughout life?” In addition, the questions were used the same during the study11,19,20.
Covariates
The data was divided into time periods before and during the COVID-19 pandemic. Since the first case of COVID-19 in South Korea was reported in January 2020, the year 2020 was defined as the first year of the pandemic21,22. Before COVID-19, 2009–2019, was subdivided into intervals of 2 to 3 years to obtain a stable estimate of the prevalence of allergic diseases (2009 to 2011, 2012–2013, 2014–2015, 2016–2017, and 2018–2019). Prevalence of AD was further by stratified variables including grade, sex, region of residence (rural and urban)23,24,25,26,27,28, body mass index (BMI; underweight, normal, overweight, obese, and unknown), school performance (low, lower-middle, middle, upper-middle, and high), parent’s highest educational level (middle school graduated or under, high school graduated, university graduated or higher, and unknown), household income (lower or middle lower, middle, and middle higher or higher), alcohol consumption (non-drinker, 1–2, 3–5, 6–9, and ≥ 10 day/month), smoking status (non-smoker and smoker), stress status (none, mild, moderate, high, and severe), sadness and despair, suicidal thoughts, and suicide attempts. BMI was calculated with body height, weight, sex, and age with reference to the 2017 Korean National Growth Charts for children and adolescents29.
Statistical analysis
We included demographic characteristics of the study participants as covariates30. We analyzed secondary data from KYRBS spanning a total of 14 years, from 2009 to 2022. Only records with complete data were included in the study. Analysis was conducted using composite sampling linear and logistic regression models. The term “composite sampling linear regression” refers to a method of conducting linear regression analysis by amalgamating data obtained from multiple sampling sources31. To investigate the trends in prevalence before and during the COVID-19 pandemic, we utilized a weighted linear regression model, deriving a β coefficient along with a 95% confidence interval (CI)32. The βdiff was used to emphasize the difference between the pre-pandemic (2009–2020) and the pandemic (2020 and 2022). This method was chosen to examine changes over time and to contrast the effects before and during the pandemic. We used a binary logistic regression model to calculate the odds ratio for the 2009–2019 and 2020–2022. We also employed this method to identify risk factors of AD and calculate the ratio of odds ratio (OR) by using odds ratios from before and during the pandemic. We further determined risk factors for the years 2020, 2021 and 2022, to deepen our understanding of the pandemic’s impact33,34,35. Categorical data were presented as frequencies and percentages, whereas numerical data were presented as means along with their corresponding 95% CIs. All statistical analyses were performed using SAS version 9.4 software (SAS Institute, Cary, NC, USA) and GraphPad Prism version 9.5.0 (GraphPad, San Diego, CA, USA)35,36,37.
Ethics approval
The study protocol was approved by the Institutional Review Board of KDCA (2014-06EXP-02-P-A).
Informed consent
All participants provided written informed consent.
Results
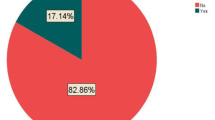
Table 1, Tables S1 and S2 show the data collected from KYRBS. The survey included a total of 917,461 participants aged 13–18 years from 2009 to 2022. The number of participants in each period was as follows: 223,947 from 2009 to 2011, 146,621 from 2012 to 2013, 140,103 from 2014 to 2015, 127,804 from 2016 to 2017, and 117,343 from 2018 to 2019 (Fig. 1). During the pandemic, there were 54,948 participants in 2020, 54,848 in 2021, and 51,847 in 2022. In terms of participant demographics, 471,306 (51.37%) of the participants were male, 446,155 (48.63%) female, and 502,419 (54.76%) lived in rural areas. 106,900 (11.65%) were people with obese, 765,939 (83.48%) were non-drinkers and 749,053 (81.64%) non-smokers. 30,765 (3.35%) of participants reported suicide attempts while 137,537 (14.99%) reported suicidal thoughts.
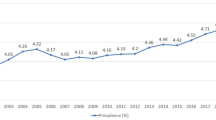
Table 2 and Fig. 2 shows the weighted prevalence of AD from 2009 to 2022, further stratified against socioeconomic factors. The weighted prevalence of AD increased from 6.79% (95% CI 6.66–6.91) in 2009–2011 to 7.22% (95% CI 7.06–7.38) in 2016–2017. However, there was a slight decrease immediately preceding the pandemic, from 2018–2019 (6.89%, 95% CI 6.72–7.05) to 2022 (5.82%, 95% CI 5.60–6.04). There was no significant difference between the pre-pandemic and pandemic in prevalence (βdiff − 0.041, 95% CI − 0.124 to 0.042) showing that the prevalence decreased since the start of the pandemic. Table 3 was analyzed to more closely examine the changes in AD prevalence during the pandemic period. The prevalence consistently showed a decreasing trend. Notably, from 2021 to 2022, there was a significant decrease (weighted OR 0.93, 95% CI 0.88 to 0.98). Table 4 shows the odds ratios of the socioeconomic factors of AD. Overall, from 2009 to 2022, high school grade, female sex, urban, high BMI group, lower-middle school performance, university graduated or higher parent’s highest educational level, middle household income, current alcohol consumption, smoker, severe stress, sadness and despair, suicidal thoughts, and suicidal attempts are observed as risk factor of AD. In addition, we calculated the ratio of OR for the pandemic/pre-pandemic period to analyze vulnerable groups during the pandemic. AD vulnerable groups during the pandemic were followed by; high school grade (ratio of OR 95% CI 1.07 [1.01 to 1.12]), middle household income (ratio of OR 95% CI 1.18 [1.09 to 1.27]), ≥ 10 days alcohol consumption (ratio of OR, 95% CI 1.25 [1.05 to 1.49]), and current smoker (ratio of OR 95% CI 1.10 [1.02 to 1.19]).
In Table S3, risk factors such as high school grade, female sex, high BMI group, low school performance, high school graduated parent’s highest educational level, current alcohol consumption, smoker, severe stress, sadness and despair, suicidal thoughts, and suicidal attempts were identified during the pandemic in 2020–2022, respectively.
Discussion
Key results
In this study we found the prevalence of AD to be 5.82% in 2022 among adolescents aged 13 to 18 years. Analyzing the prevalence of AD is important because this allergic disease has a significant impact on the quality of life, particularly among adolescents. The prevalence of AD continued to increase prior to the pandemic. However, the most significant decline in prevalence occurred after the COVID-19 pandemic began, with a smaller decline observed during the pandemic. Examining this prevalence contributes to understanding the scope of the COVID-19 pandemic and its influences on allergic disease trends. Additionally, current alcohol consumption, smoker, severe stress, sadness and despair, suicidal thoughts, and suicidal attempts are observed as risk factors of AD. These results could also provide a new perspective on coping with AD.
Global epidemiology and mechanism
In South Korea, the first cases of COVID-19 were discovered in January 2020, and the severity of the pandemic increased over time37. One hypothesis for this phenomenon could be the reduced exposure to allergens due to the changes during COVID-19. Several significant social and political changes occurred during this period, which could have influenced the level of allergen exposure. Because the most drastic of measures included social distancing, lockdowns, closures of public places, decreased physical interaction, mask mandates, and other self-isolating actions38,39,40. Furthermore, during the COVID-19, there was a decrease in air pollution in South Korea41, which is consistent with decreased smoking and automobile traffic resulting from decreased socialization42. Air pollution has previously been linked to AD as air particulates can damage the skin barrier through oxidative stress, thus triggering immune dysregulation which can potentially increase inflammation of AD43,44. Heavy metals exposure (a factor of air pollution) has similarly been associated with allergic diseases, acting as a direct activator of Th2 cells as well as an adjuvant, increasing the effect of other allergens42. In addition, the use of face masks has further enhanced the protective effect as studies have shown that they reduce allergic diseases, particularly AD45,46. While face masks could have an inflammatory effect on facial dermatoses due to increased skin hydration, temperature, and sebum secretion, it has been found that in patients with AD, facial eczema is deceased due to covering sensitive areas46. In 2022, many COVID-19 regulations began to be rescinded, with South Korea removing the mask mandate and other social restrictions as the pandemic started to wind down. This return to pre-pandemic action could partially explain the decreased trend of AD during 202213. However, although there is a decreasing trend, it is too early to determine the impact of reducing social restrictions in 2022, so future research is required.
In this study, we found that alcohol consumption and smoking are both associated with an increased risk of AD, which is consistent with the literature9. However, in Korean adolescents, we found a minor negative association between high BMI and AD, which is in contrasts with other sources, as overweight or obese individuals have been found to have an increased risk of AD through a small but important causal relationship47. Having suicidal thoughts was the only factor that demonstrated an increased risk of AD across the pandemic, 2020–2022. However, further research is necessary to fully understand the underlying mechanism behind this association. Falling rates of AD during COVID-19 may also be due to other factors. Firstly, the common allergens for AD have been found to be changing as patients are less sensitized to them and new allergens emerge48. Secondly, in the United States, it has been postulated that falling rates of allergic disease could be due to the changes in measurements49, but the KYRBS has remained consistent in its measurement and questions. Finally, a study in Colombia found that leading up to 2019, there was an increasing utilization of healthcare resources and healthcare visits, which correlated with an increased in the incidence and prevalence of AD50. The COVID-19 pandemic saw a decrease in healthcare utilization, including for allergic disease, as fewer people reported to hospitals during COVID-19 for fear of contracting SARS-CoV-251. Furthermore, many patients with AD are treated by specialists, and data from other countries data outpatient dermatological visits during the COVID-19 pandemic, with AD being the most common reason for visits52,53. However, specific studies conducted in South Korea found no decrease in incidence in adolescent AD from 2019 to 2020, so changes in incidence may not fully explain the decreasing trend of AD during this period54.
Strengths and limitations
We utilized the KYRBS, which serves as both the greatest strength and limitation of this study. The KYRBS is the only national database for the prevalence of allergic disease since the COVID-19 pandemic, with over one million Korean adolescents included in the study. The KYRBS is also integrated with the public school system in South Korea, as it is administered to most school-age adolescents via computers with anonymous online self-reporting9. However, this poses several limitations. First, the KYRBS excludes any student not in the Korean public education system, potentially excluding a segment of the adolescent population. Second, the KYRBS is a self-reporting questionnaire, which, although considered reliable based on a kappa coefficient of 0.78–0.8055, still yields subjective data that lacks objective measures. Third, in our study, we analyzed the data without considering the sensitivity and specificity of AD. Therefore, there is a limitation that the numbers may change when considering this. However, even if we consider this limitation, it is unlikely to significantly alter the overall trend of the results. Fourth, this study has limitations due to the lack of use of validated questionnaires, impacting the reliability and accuracy of its results. This common issue in self-report studies necessitates caution in interpreting data and may restrict the generalizability of the findings. Fifth, while the results of this study show an overall decreasing trend in the number of AD patients, this may be attributed to a reduction in doctor visits during the pandemic. However, our dataset lacks information on doctor visits, making this difficult to ascertain. Finally, the data is confined to one country, South Korea. Primary healthcare is highly valued worldwide56. However, contrary to this, according to statistics from the World Health Organization, many countries suffer from poor access to primary healthcare57,58. On the other hand, South Korea boasts excellent accessibility to primary healthcare59. This disparity may be attributed to cultural differences, the presence or absence of social insurance, among other factors, which could result in the trends in other countries being different.
Conclusion
This study observed the prevalence of AD over a 14-year from 2009 to 2022, analyzing both the differences before and during the COVID-19 pandemic, as well as within the pandemic itself. The prevalence of AD increased before the pandemic, then decreased at the start of the pandemic and remained stable throughout the pandemic. This prevalence helps us understand the scope of the COVID-19 pandemic and its effects on allergic disease trends. In addition, risk factors of AD include alcohol consumption, smoking, severe stress, feelings of sadness and despair, suicidal ideation, and suicide attempts. Further research is necessary to understand whether these results are specific to the COVID-19 pandemic and whether the trend of AD will revert to pre-pandemic levels as the COVID-19 pandemic ends.
Data availability
Data are available on reasonable request. Study protocol, statistical code: available from DKY (email: yonkkang@gmail.com). Data set: available from the Korea Disease Control and Prevention Agency (KDCA) through a data use agreement.
References
Lim, S., Yoon, H. I., Song, K. H., Kim, E. S. & Kim, H. B. Face masks and containment of COVID-19: Experience from South Korea. J. Hosp. Infect. 106, 206–207. https://doi.org/10.1016/j.jhin.2020.06.017 (2020).
Choi, S. Y. et al. Mask-induced dermatoses during the COVID-19 pandemic: A questionnaire-based study in 12 Korean hospitals. Clin. Exp. Dermatol. 46, 1504–1510. https://doi.org/10.1111/ced.14776 (2021).
Rudd, E. & Walsh, S. Mask related acne (“maskne”) and other facial dermatoses. BMJ 373, n1304. https://doi.org/10.1136/bmj.n1304 (2021).
Nutten, S. Atopic dermatitis: Global epidemiology and risk factors. Ann. Nutr. Metab. 66(Suppl 1), 8–16. https://doi.org/10.1159/000370220 (2015).
Abuabara, K., Yu, A. M., Okhovat, J. P., Allen, I. E. & Langan, S. M. The prevalence of atopic dermatitis beyond childhood: A systematic review and meta-analysis of longitudinal studies. Allergy 73, 696–704. https://doi.org/10.1111/all.13320 (2018).
Kim, M. S. et al. Efficacy and safety of topical Streptococcus postbiotic emollient in adolescents and adults with mild-to-moderate atopic dermatitis: A randomized, double-blind, vehicle-controlled trial. Allergy. https://doi.org/10.1111/all.16077 (2024).
Yew, Y. W., Thyssen, J. P. & Silverberg, J. I. A systematic review and meta-analysis of the regional and age-related differences in atopic dermatitis clinical characteristics. J. Am. Acad. Dermatol. 80, 390–401. https://doi.org/10.1016/j.jaad.2018.09.035 (2019).
Kumar, R., Seibold, M. A. & Burchard, E. G. Atopic dermatitis, race, and genetics. J. Allergy Clin. Immunol. 145, 108–110. https://doi.org/10.1016/j.jaci.2019.11.008 (2020).
Lee, K. H., Yon, D. K. & Suh, D. I. Prevalence of allergic diseases among Korean adolescents during the COVID-19 pandemic: Comparison with pre-COVID-19 11-year trends. Eur. Rev. Med. Pharmacol. Sci. 26, 2556–2568. https://doi.org/10.26355/eurrev_202204_28492 (2022).
Ha, J., Lee, S. W. & Yon, D. K. Ten-year trends and prevalence of asthma, allergic rhinitis, and atopic dermatitis among the Korean population, 2008–2017. Clin. Exp. Pediatr. 63, 278–283. https://doi.org/10.3345/cep.2019.01291 (2020).
Koo, M. J. et al. National trends in the prevalence of allergic diseases among Korean adolescents before and during COVID-19, 2009–2021: A serial analysis of the national representative study. Allergy 78, 1665–1670. https://doi.org/10.1111/all.15600 (2023).
Shin, Y. H. et al. Global, regional, and national burden of allergic disorders and their risk factors in 204 countries and territories, from 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Allergy 78, 2232–2254. https://doi.org/10.1111/all.15807 (2023).
Park, K. & Baek, H. J. Contextual response to the COVID-19 pandemic from the experience of South Korea. Public Health 222, e7–e8. https://doi.org/10.1016/j.puhe.2022.07.015 (2023).
Kim, Y. et al. Data resource profile: The Korea youth risk behavior web-based survey (KYRBS). Int. J. Epidemiol. 45, 1076. https://doi.org/10.1093/ije/dyw070 (2016).
Lee, H. et al. Machine learning-based prediction of suicidality in adolescents with allergic rhinitis: Derivation and validation in 2 independent nationwide cohorts. J. Med. Internet Res. 26, e51473. https://doi.org/10.2196/51473 (2024).
Choi, Y. et al. National prevalence and trends in food labeling awareness, comprehension, usage, and COVID-19 pandemic-related factors in South Korea, 2014–2022. Sci. Rep. 14, 2617. https://doi.org/10.1038/s41598-024-51948-1 (2024).
Noh, H. et al. Sleep problems increase school accidents related to allergic diseases. Pediatr. Allergy Immunol. 31, 98–103. https://doi.org/10.1111/pai.13132 (2020).
Kang, J. et al. National trends and prevalence of atopic dermatitis and pandemic-related factors among Korean adults, 2007–2021. Int. Arch. Allergy Immunol. https://doi.org/10.1159/000535666 (2024).
Lee, H. et al. National trends in allergic rhinitis and chronic rhinosinusitis and COVID-19 pandemic-related factors in South Korea, from 1998 to 2021. Int. Arch. Allergy Immunol. https://doi.org/10.1159/000535648 (2024).
Yon, D. K. et al. Indoor exposure and sensitization to formaldehyde among inner-city children with increased risk for asthma and rhinitis. Am. J. Respir. Crit. Care Med. 200, 388–393. https://doi.org/10.1164/rccm.201810-1980LE (2019).
Park, S. et al. National trends in physical activity among adults in South Korea before and during the COVID-19 pandemic, 2009–2021. JAMA Netw. Open 6, e2316930. https://doi.org/10.1001/jamanetworkopen.2023.16930 (2023).
Oh, J. et al. Hand and oral hygiene practices of South Korean adolescents before and during the COVID-19 pandemic. JAMA Netw. Open 6, e2349249. https://doi.org/10.1001/jamanetworkopen.2023.49249 (2023).
Yoo, I. K., Marshall, D. C., Cho, J. Y., Yoo, H. W. & Lee, S. W. N-Nitrosodimethylamine-contaminated ranitidine and risk of cancer in South Korea: A nationwide cohort study. Life Cycle 1, e1. https://doi.org/10.54724/lc.2021.e1 (2021).
Park, J. et al. National trends in rheumatoid arthritis and osteoarthritis prevalence in South Korea, 1998–2021. Sci. Rep. 13, 19528. https://doi.org/10.1038/s41598-023-46279-6 (2023).
Lee, S. W. et al. Estimating COVID-19 infection and severity risks in patients with chronic rhinosinusitis: A Korean nationwide cohort study. J. Allergy Clin. Immunol. Pract. 9, 2262–2271. https://doi.org/10.1016/j.jaip.2021.03.044 (2021).
Yoo, H. W. et al. Non-alcoholic fatty liver disease and COVID-19 susceptibility and outcomes: A Korean nationwide cohort. J. Korean Med. Sci. 36, e291. https://doi.org/10.3346/jkms.2021.36.e291 (2021).
Lee, S. W. et al. Association between mental illness and COVID-19 in South Korea: A post-hoc analysis. Lancet Psychiatry 8, 271–272. https://doi.org/10.1016/s2215-0366(21)00043-2 (2021).
Lee, S. W. et al. Proton pump inhibitors and the risk of severe COVID-19: A post-hoc analysis from the Korean nationwide cohort. Gut 70, 2013–2015. https://doi.org/10.1136/gutjnl-2020-323672 (2021).
Kim, J. H. et al. The 2017 Korean National Growth Charts for children and adolescents: Development, improvement, and prospects. Korean J. Pediatr. 61, 135–149. https://doi.org/10.3345/kjp.2018.61.5.135 (2018).
Park, J. et al. National trends in asthma prevalence in South Korea before and during the COVID-19 pandemic, 1998–2021. Clin. Exp. Allergy 53, 1291–1294. https://doi.org/10.1111/cea.14394 (2023).
Kang, J. et al. National trends in depression and suicide attempts and COVID-19 pandemic-related factors, 1998–2021: A nationwide study in South Korea. Asian J. Psychiatr. 88, 103727. https://doi.org/10.1016/j.ajp.2023.103727 (2023).
Lee, S. W. Methods for testing statistical differences between groups in medical research: Statistical standard and guideline of Life Cycle Committee. Life Cycle 2, e1. https://doi.org/10.54724/lc.2022.e1 (2022).
Oh, J. et al. Prenatal and postnatal exposure to antibiotics and risk of food allergy in the offspring: A nationwide birth cohort study in South Korea. Pediatr. Allergy Immunol. 35, e14114. https://doi.org/10.1111/pai.14114 (2024).
Lee, H. J. et al. National trends in Rotavirus Enteritis among infants in South Korea, 2010–2021: A nationwide cohort. Children 10, 1436. https://doi.org/10.3390/children10091436 (2023).
Woo, H. G. et al. Global burden of vaccine-associated multiple sclerosis, 1967–2022: A comprehensive analysis of the international pharmacovigilance database. J. Med. Virol. 96, e29591. https://doi.org/10.1002/jmv.29591 (2024).
Kang, J. et al. Prenatal opioid exposure and subsequent risk of neuropsychiatric disorders in children: Nationwide birth cohort study in South Korea. BMJ 385, e077664. https://doi.org/10.1136/bmj-2023-077664 (2024).
Kim, M. S. et al. Long-term autoimmune inflammatory rheumatic outcomes of COVID-19: A binational cohort study. Ann. Intern. Med. 177, 291–302. https://doi.org/10.7326/m23-1831 (2024).
Papadopoulos, N. G. et al. Childhood asthma outcomes during the COVID-19 pandemic: Findings from the PeARL multi-national cohort. Allergy 76, 1765–1775. https://doi.org/10.1111/all.14787 (2021).
Papadopoulos, N. G. et al. Impact of COVID-19 on pediatric asthma: Practice adjustments and disease burden. J. Allergy Clin. Immunol. Pract. 8, 2592–2599. https://doi.org/10.1016/j.jaip.2020.06.001 (2020).
Han, E. et al. Lessons learnt from easing COVID-19 restrictions: An analysis of countries and regions in Asia Pacific and Europe. Lancet 396, 1525–1534. https://doi.org/10.1016/s0140-6736(20)32007-9 (2020).
Ju, M. J., Oh, J. & Choi, Y. H. Changes in air pollution levels after COVID-19 outbreak in Korea. Sci. Total Environ. 750, 141521. https://doi.org/10.1016/j.scitotenv.2020.141521 (2021).
Koh, H. Y. et al. Serum heavy metal levels are associated with asthma, allergic rhinitis, atopic dermatitis, allergic multimorbidity, and airflow obstruction. J. Allergy Clin. Immunol. Pract. 7, 2912–2915. https://doi.org/10.1016/j.jaip.2019.05.015 (2019).
Pan, Z. et al. Impact of air pollution on atopic dermatitis: A comprehensive review. Clin. Rev. Allergy Immunol. 65, 121–135. https://doi.org/10.1007/s12016-022-08957-7 (2023).
Fadadu, R. P. et al. Air pollution and global healthcare use for atopic dermatitis: A systematic review. J. Eur. Acad. Dermatol. Venereol. 37, 1958–1970. https://doi.org/10.1111/jdv.19193 (2023).
Dror, A. A. et al. Reduction of allergic rhinitis symptoms with face mask usage during the COVID-19 pandemic. J. Allergy Clin. Immunol. Pract. 8, 3590–3593. https://doi.org/10.1016/j.jaip.2020.08.035 (2020).
Vanessa, M. et al. Facial dermatoses and use of protective mask during Covid-19 pandemic: A clinical and psychological evaluation in patients affected by moderate-severe atopic dermatitis under treatment with dupilumab. Dermatol. Ther. 35, e15573. https://doi.org/10.1111/dth.15573 (2022).
Budu-Aggrey, A. et al. Assessment of a causal relationship between body mass index and atopic dermatitis. J. Allergy Clin. Immunol. 147, 400–403. https://doi.org/10.1016/j.jaci.2020.04.050 (2021).
Han, Y. et al. Allergic sensitization pattern in the Korean dermatologic patients. Ann. Dermatol. 34, 431–441. https://doi.org/10.5021/ad.21.260 (2022).
Frey, S. M., Rowe, R. K. & Halterman, J. S. The prevalence of childhood asthma: Interpreting falling rates in the context of shifting measurement and the COVID-19 pandemic. Curr. Opin. Pulm. Med. 29, 197–201. https://doi.org/10.1097/mcp.0000000000000959 (2023).
Londoño, A. M., Castro-Ayarza, J. R., Kronfly, A., Buitrago, D. C. & Samacá, D. F. Epidemiology and healthcare resource utilization in atopic dermatitis in Colombia: A retrospective analysis of data from the National Health Registry from 2015 to 2020. Biomedica 43, 107–120. https://doi.org/10.7705/biomedica.6666 (2023).
Kenyon, C. C., Hill, D. A., Henrickson, S. E., Bryant-Stephens, T. C. & Zorc, J. J. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J. Allergy Clin. Immunol. Pract. 8, 2774–2776. https://doi.org/10.1016/j.jaip.2020.05.045 (2020).
Gao, C., Liu, B., Xie, Y. & Wu, Z. Change of dermatological practice after the COVID-19 outbreak resolves. J. Dermatol. Treat. 33, 996–998. https://doi.org/10.1080/09546634.2020.1799920 (2022).
Al Hammadi, A. et al. Healthcare resource utilization and direct cost of patients with atopic dermatitis in Dubai, United Arab Emirates: A retrospective cohort study. Dermatol. Ther. (Heidelb.) 12, 1859. https://doi.org/10.1007/s13555-022-00769-z (2022).
Choi, H. G. & Kong, I. G. Asthma, allergic rhinitis, and atopic dermatitis incidence in Korean adolescents before and after COVID-19. J. Clin. Med. 10, 446. https://doi.org/10.3390/jcm10153446 (2021).
Bae, J. et al. Test–retest reliability of a questionnaire for the Korea youth risk behavior web-based survey. J. Prev. Med. Public Health 43, 403–410. https://doi.org/10.3961/jpmph.2010.43.5.403 (2010).
Allen, L. N. et al. The role of primary health care, primary care and hospitals in advancing Universal Health Coverage. BMJ Glob. Health 8, 442. https://doi.org/10.1136/bmjgh-2023-014442 (2023).
Rao, M. & Pilot, E. The missing link—The role of primary care in global health. Glob. Health Act. 7, 23693. https://doi.org/10.3402/gha.v7.23693 (2014).
Gulliford, M. Access to primary care and public health. Lancet Public Health 2, e532–e533. https://doi.org/10.1016/s2468-2667(17)30218-9 (2017).
Partyka, O. et al. Influence of selected indicators of healthcare system functioning evaluation on the health result. Int. J. Environ. Res. Public Health 19, 4618. https://doi.org/10.3390/ijerph192114618 (2022).
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korean government (RS-2023-00248157), a Grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant Number: HV22C0233), and a Grant (21153MFDS601) from Ministry of Food and Drug Safety in 2024. The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
Dr Dong Keon Yon had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final version before submission. Study concept and design: Mafaz Kattih and Dong Keon Yon; Acquisition, analysis, or interpretation of data: Hojae Lee; Drafting of the manuscript: Mafaz Kattih, Hyesu Jo, Jinyoung Jeong, and Hyejun Kim; Critical revision of the manuscript for important intellectual content: Mafaz Kattih, Hojae Lee, Hyesu Jo, Jinyoung Jeong, Hyejun Kim, Hwi Yang, Ann Nguyen, Hyeon Jin Kim, Hyeri Lee, Minji Kim, Myeongcheol Lee, Rosie Kwon, Sunyoung Kim, Ai Koyanagi, Lee Smith, Min Seo Kim, Masoud Rahmati, Ju Hee Kim, Seung Won Lee, Selin Woo, Jaeyu Park, Seong H. Cho, and Dong Keon Yon; Statistical analysis: Hojae Lee; Study supervision: Dong Keon Yon. Mafaz Kattih, Hojae Lee, Hyesu Jo, Jinyoung Jeong, Jaeyu Park and Hyejun Kim contributed equally as first authors. Lee Smith, Seong H. Cho, and Dong Keon Yon contributed equally as corresponding authors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kattih, M., Lee, H., Jo, H. et al. National prevalence of atopic dermatitis in Korean adolescents from 2009 to 2022. Sci Rep 14, 12391 (2024). https://doi.org/10.1038/s41598-024-62475-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62475-4