Abstract
Conventional open laminectomy has long been considered one of the important surgical options for lumbar central stenosis owing to its positive outcomes. However, newer approaches have emerged as alternatives, including full-endoscopic and biportal endoscopic laminectomy. Therefore, a comparison of the outcomes that are associated with each of these surgical methods is warranted. This prospective multicenter trial, initiated in February 2019, compared the outcomes of three lumbar central stenosis surgical approaches: open laminectomy (OPEN), uniportal endoscopy (UNIPORT), and biportal endoscopy (BIPORT). Among 115 participants from seven centers, one-year follow-ups assessed laboratory, radiological, and clinical outcomes. Despite all groups showing adequate decompression and clinical improvement, the OPEN group exhibited less improvement in Visual analog scale (VAS) for back pain scores (p < 0.05) and significant postoperative increases in most laboratory markers. Furthermore, the OPEN group experienced a significant decrease in multifidus muscle cross-sectional area compared to endoscopic groups (p < 0.001). Each surgical techniques produced similar clinical outcomes and dural space expansion. However, endoscopic surgery was associated with better muscle preservation and better relief of back pain. Endoscopic surgery is a reasonable alternative to conventional laminectomy for treating lumbar central stenosis.
This trial was registered on CRIS (Clinical Research Information Service, KCT0004355).
Similar content being viewed by others
Introduction
Lumbar stenosis is an age-related spinal disease that causes pain, impairment, and reduced quality of life (QOL), which contribute to higher socioeconomic costs1,2. Lumbar central stenosis involves narrowing of the vertebral canal, caused by encroachment of bone on the space. Symptoms are caused by compression of nervous system tissue, and include pain, paresthesias, and neurogenic claudication. The condition either may be congenital or may be caused by spinal degeneration3.
There are a variety of non-surgical treatment options available; however, surgical interventions have also been recognized as a method of patient care4,5. In 1954, Verbiest reported on wide laminectomy6. For years, studies named conventional open laminectomy as one of the important surgical options for lumbar central stenosis owing to its satisfactory results. Conventional wide laminectomy was mainly concerned with obtaining sufficient dural space. The importance of the surrounding structures was underestimated7,8. Consequently, problems persist with surgical complications following its use, such as bleeding, extended hospital stays, and soft tissue and muscle injuries. Three columns compose the spine, and their combination ensures stability9. The essential role of the posterior column, including interspinous ligaments and facet joints, has been confirmed by biomechanical investigations10,11,12. These structures are usually injured during the conventional approach. Therefore, surgeons have been exploring optimal approaches to minimize disruption, leading to the development of minimally invasive spine surgery. Spetzger proposed unilateral laminectomy bilateral decompression (ULBD)13, which is a technique that preserves the ligaments and spinous process by including flavectomy on both sides, while entering from one side and leaving the muscle on the other side intact. This technique continues to be the fundamental tool for endoscopic surgery. In the late 1990s, Yeung introduced the first functional endoscopic spine surgery system, featuring a multichannel endoscope with continuous fluid irrigation, which led to successful outcomes in disc herniation14. In 1996, De Antoni et al. published the first technical note on independently inserting endoscopes and instruments through two portals, which later evolved into biportal endoscopic spine surgery15.
Recent advancements in endoscopic instruments, including larger-diameter endoscopes, allow for sufficient lamina excision, the expansion, of which, extends endoscopic surgery from discectomy to central and foraminal decompression16,17. However, endoscopic surgery also possesses some drawbacks. The full endoscopic approach embodies key features, such as minimal soft tissue damage and multilevel observation through a single port18; however, the learning curve involved in its performance is quite steep19,20. Therefore, to compensate, biportal endoscopic surgery was developed, which offers a broad field of view and the use of surgical instruments similar to conventional methods, thereby making endoscopic surgery more accessible15,21. Compared to open laminectomy, controlling bleeding is challenging, and irrigation can raise intracranial pressure, while complications, such as dural tears, root injuries, and epidural hematomas have been consistently reported20,22.
Advancements in endoscopic surgery have provided alternatives to open laminectomy. Findings from retrospective research projects indicate that endoscopic surgery might produce better outcomes, perhaps due to less invasiveness, and corresponding muscle preservation23,24. Our project prospectively compared results from three laminectomy methods: conventional open laminectomy, full-endoscopic laminectomy, and biportal endoscopic laminectomy. Our comparisons included biochemical, radiological, and patient-reported outcomes.
Materials and methods
Study design and patient eligibility criteria
This prospective case–control clinical trial was approved by the Institutional Review Board of Yonsei University Gangnam Severance Hospital (IRB number: 3-2018-0361, 25/02/2019) and registered on CRIS (Clinical Research Information Service, KCT0004355, 18/10/2019). All patient data were analyzed anonymously in accordance with relevant guidelines and regulations. This trial has been conducted in compliance with the the Declaration of Helsinki. Informed consent was obtained from 115 patients who underwent surgery between February 2019 and October 2021. Patients were tracked for a minimum of 12 months. Outcomes were assessed by an independent researcher during in-hospital visits at baseline, during surgery, and postoperatively.
This multicenter case–control study included 7 spine surgery centers. Patients were divided into three groups: OPEN (31 patients; surgeons J.P. and J.K.), UNIPORT (37 patients; surgeons H.K. and C.L.), and BIPORT (47 patients; surgeons C.C., J.J., and M.P.). Primary reasons for surgery were mainly uncontrolled back and radiating leg pain. The detailed inclusion criteria were as follows: (1) aged 20–85 years old (2) low back pain or radiating leg pain (more than 3 months); (3) lumbar spinal stenosis observed on MRI; (4) do not respond to analgesics (more than 1 month); (5) general state of health sufficient to withstand anesthesia for surgery; and (6) in good health and able to participate in the study. The exclusion criteria were as follows: (1) unclear or suspicious symptoms; (2) previous spine surgery; (3) grade 2 or higher spondylolisthesis; (4) fractures or dislocations; (5) structural damage or destruction to vertebral bodies; and (6) infections or metastatic diseases. Scheduled procedures and assessments are outlined in Supplementary material.
Surgical techniques
All patients underwent operations in the prone position and general anesthesia was administered in accordance with the institution's protocols. Each operation was conducted by an experienced surgeon. Seven surgeons were involved in this project.
Conventional open laminectomy (OPEN group)6
Patients underwent a 4–5 cm midline skin incision, monopolar cautery to separate the fascia and paraspinal muscle from the spinous process and lamina bilaterally, high-speed drill for subtotal laminectomy, and bilateral spinal lateral recess decompression (Fig. 1a).
Operative image of the three techniques. (a) An image of the operating field applying the retractor after muscle dissection in an open laminectomy, as well as an image of intraoperative level confirmation and a decompressed condition. (b) Appearance of a mounted single portal and the C-arm picture used to examine the surgical level in a full-endoscopic procedure. Endoscopic view of a decompression procedure in uniportal process. (c) Two portals mounted in biportal endoscopic surgery. The C-arm image demonstrated level confirmation and docking of instruments. Endoscopic view of biportal process.
Full-endoscopic laminectomy (UNIPORT group)16
A 1–2 cm skin incision, 0.5–1 cm lateral to the spinous process, followed by dilator insertion to create surgical space and endoscope placement. A partial hemilaminectomy was performed, using the working channel of the endoscope, to decompress the ipsilateral and contralateral sides (Fig. 1b).
Biportal endoscopic laminectomy (BIPORT group)17
A 1 cm skin incision was independently performed above and below the lesion and a dilator was inserted to separate and dissect the muscle unilaterally. It differs from a full-endoscopic laminectomy because it has a viewing endoscope on one side and surgical tools on the other side (Fig. 1c).
Evaluation
Laboratory markers
Creatine phosphokinase (CPK), lactate dehydrogenase (LDH), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) related to muscle and tissue injuries, were assessed preoperatively and 1–3 days postoperatively, with results analyzed in the following units: CPK: U/L (units per liter); LDH: IU/L (international units per liter); ESR: mm/h (millimeters per hour); CRP: mg/L (milligrams per liter). These internationally recognized units were chosen to ensure consistent blood test results across hospitals and enable accurate data representation and comparison.
Radiological parameters
Magnetic resonance imaging (MRI) uses a T2-weighted sequence and was applied mainly for radiologic outcome confirmation. Cross-sectional area (CSA) analysis compared muscle injury and dural expansion after surgery. PACS (ZeTTA PACS, TaeYoung Soft. Co., Seoul, Korea) and a computerized area of interest (ROI) were used for measurement. ROI encompassed bilateral multifidus (MF) muscles to estimate lean MF muscle CSA, excluding unwanted adjacent fatty tissue, skeletal structures, and facet joints21. The same method assessed dural decompression, with an ROI drawn outside the dural sac. The CSA sum of bilateral lean MF muscle (muscle CSA) and dural area (dural CSA) was calculated (Fig. 2). The radiologic results were obtained before surgery, immediately after surgery, and six months later. Two highly experienced neurosurgeons performed the measurement procedure independently by selecting the most comparable preoperative and follow-up axial images at the same spinal level for comparison using anatomic landmarks. Initially, we examined the preoperative axial cut exhibiting the most severe stenosis and thoroughly assessed the shape and positioning of the iliac artery and vein, mesenteric artery and vein, and psoas muscle on that cut. After confirming the axial cut showing the most consistent distribution and shape of these structures on postoperative MRI, we measured the dural and muscle CSA on that particular cut. Percentage comparisons were conducted by considering MRI magnification differences.
Measurement of the cross-sectional area of the dural sac and multifidus muscle in axial T2-weighted MR images. The area was estimated automatically by tracing a line (red dotted) along the outer wall of the dural. An additional line (yellow solid) was drawn to identify the deteriorated multifidus muscle after surgery. Lean muscle cross-sectional area (CSA) was the sum of all the areas outlined. These methods allow for the comparison of pre- and postoperative conditions, enabling the confirmation of the muscle and dural CSA.
Clinical outcomes
Visual analog scale (VAS), Oswestry disability index (ODI), and 36-item short-form health survey (SF-36) were used to evaluate the degree of clinical improvement following surgery. Results were reviewed at baseline and 1, 3, 6, and 12 months after surgery. Two or more researchers accomplished patient questionnaires at each institution to verify the data. Phone calls were used to collect as much information as feasible in instances of missing data.
Statistical analysis
We conducted Shapiro–Wilk tests to confirm a normal distribution of data. Continuous variables are presented as mean ± standard deviation (SD) and categorical as percentages (%). Analysis of variance (ANOVA) and Chi-square were applied to evaluate group differences. A p value < 0.05 indicated significance. SAS 9.4 (SAS Institute, Cary, NC, USA) was used to compare the three groups.
Results
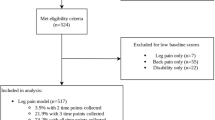
Of the 115 enrolled patients, 106 completed the 1-year follow-up (92.17% follow-up rate). Two OPEN group patients were lost after surgery during the follow-up. Five patients were excluded from the UNIPORT group (two were lost and three underwent revision surgery). Two patients withdrew from the BIPORT group (one was lost and one underwent revision surgery). Thus, the evaluation included 106 participants (29 OPEN, 32 UNIPORT, and 45 BIPORT). The flow diagram in Fig. 3 illustrates the investigation and follow-up. Perioperative changes (Δ, delta value) were used to compare outcomes. Table 1 summarizes baseline characteristics and surgery-related outcomes for patients in the three groups. No significant differences were observed in demographic, baseline radiographic, or clinical characteristics among the three groups. Revision surgery rate was observed as: none (0%) in the OPEN group, 3 cases (8.1%) in the UNIPORT group, and 2 cases (4.2%) in the BIPORT group. These outcomes pertain to all 115 patients enrolled before dropout, and their data are not included in the subsequent analyses. The OPEN group had a longer discharge time (hospital stay: 8.9 ± 3.7 days, p < 0.001).
Laboratory markers
Significant increases were noted for all markers on postoperative day 1 (ΔCPK, p = 0.002, OPEN vs. UNIPORT/BIPORT; ΔLDH, p = 0.031; ΔESR, p = 0.020, UNIPORT vs. BIPORT; ΔCRP, p < 0.001, OPEN vs. UNIPORT/BIPORT), while a marked elevation in ESR and CRP was observed postoperatively in the OPEN group on day 3 (ΔESR, p < 0.001, OPEN vs. UNIPORT/BIPORT and ΔCRP, p < 0.001, OPEN vs. UNIPORT/BIPORT) (Table 2). The mean blood test results before and after surgery are presented in Fig. 4.
Results of laboratory blood tests conducted before surgery and on the first and third days after surgery. (a) Mean creatine phosphokinase (CPK), U/L (units per liter). (b) Mean lactate dehydrogenase (LDH), IU/L (international units per liter). (c) Mean erythrocyte sedimentation rate (ESR), mm/hr (millimeters per hour). (d) Mean C-reactive protein (CRP), mg/L (milligrams per liter).
Radiological parameters
Dural areas expanded postoperatively in all groups, whereas no noticeable differences were observed in dural expansion (Δdural CSA) over six months: OPEN 76.2 ± 22.1 mm2 (203.7 ± 82.8%), UNIPORT 71.0 ± 29.3 mm2 (195.5 ± 104.7%), and BIPORT 78.7 ± 29.8 mm2 (228.5 ± 110.4%). The OPEN group showed significantly greater muscle CSA decreases both immediately after surgery and at 6 months (immediately: 300.1 ± 193.5 mm2, 29.7 ± 12.9%; 6 months postoperation: 285.2 ± 130.5 mm2, 28.9 ± 10.6%) compared to both the UNIPORT (immediately: 92.4 ± 70.3 mm2, 10.1 ± 7.2%; 6 months postoperation: 81.7 ± 65.2 mm2, 8.6 ± 6.3%), and BIPORT groups (immediately: 107.3 ± 74.7 mm2, 11.6 ± 7.0%; 6 months postoperation: 89.9 ± 92.9 mm2, 9.5 ± 9.2%) (Table 2).
Clinical outcomes
Clinical results improved during the 1-year trial period in all groups. However, the VAS scores for back pain in the OPEN group exhibited less relief compared to the UNIPORT and BIPORT groups, especially immediately after surgery. On day 1 postoperation, the OPEN group showed a smaller improvement in VAS back pain (1.31 ± 3.52) compared to the UNIPORT and BIPORT groups (2.91 ± 2.38 and 2.87 ± 2.42) (p = 0.036). Differences between the OPEN and UNIPORT groups were seen on the third day postoperation (1.24 ± 3.84 vs. 3.39 ± 2.33, p = 0.017). The OPEN and UNIPORT groups also differed in the recovery observed at three months (2.09 ± 2.79 vs. 4.34 ± 2.00, p = 0.002), with other results (VAS leg pain, ODI, and SF-36) demonstrating similar improvements (Table 3). The clinical improvement pattern is illustrated in Fig. 5.
Tendency in clinical outcomes among the three groups during the course of a 12-month follow-up. (a) Mean VAS scores for back pain, ranged from 0 (no pain) to 10. (b) Mean VAS scores for leg pain, ranged from 0 (no pain) to 10. (c) Mean Oswestry disability index (ODI) scores, ranged from 0 (no disability) to 100. (d) Mean physical component score (PCS) of 36-item short-form health survey (SF-36), ranged from 0 (severe impairment) to 100. (e) Mean mental component score (MCS) of SF-36, ranged from 0 (severe impairment) to 100.
Discussion
This prospective study compared conventional open laminectomy to full-endoscopic and biportal endoscopic decompression for lumbar stenosis, aiming to explore the potential advantages and disadvantages of each surgical approach.
There were no significant differences observed among the demographics in the three groups. Although differences were in the operational data. The occurrence of revision surgery was as follows: 0 (0%) in the OPEN group, 3 (8.1%) in the UNIPORT group, and 2 (4.2%) in the BIPORT group. This implies the advantages of open laminectomy, which has been practiced for a long time, and is also considered intuitive, for surgeons. However, it is important to note that these figures represent data for all 115 patients enrolled in our study, as revisions were considered drop-out criteria. As a result, we were unable to gather data on the reasons for revision surgery and comprehensive postoperative outcomes in revision patients. The reason for setting revision as the drop-out criterion is to compare them with the laboratory, radiological, and clinical parameters of patients who successfully completed surgery. This raises concerns about potential selection bias, prompting us to conduct additional studies that include data related to revision surgery.
In the laboratory, a significant increase was observed in the OPEN group for all indicators. An increase in CPK levels correlated with postoperative muscle injury25,26. Similarly, LDH and CPK are related to muscle damage through myosin-heavy chain fragments (i.e., troponin I and myoglobin)27. ESR and CRP were analyzed as inflammatory markers. Elevated levels of inflammatory markers are associated with muscle atrophy and impaired muscle regeneration28. Furthermore, previous studies reported that elevated levels of inflammatory cytokines caused sarcopenia and muscular weakness29. Therefore, by incorporating various blood markers, beyond CPK levels, we enhanced our comprehensive assessment, to provide valuable insights for interpreting clinical and radiological findings.
A radiological review showed sufficient dural expansion in all groups. We measured the dural area using the method employed in previous research30,31. In this study, we opted to establish two indicators for significant decompression. Schonstrom defined absolute lumbar spinal stenosis with a dural sac area < 70 mm2. In Steurer et al.’s review, most authors considered central stenosis if the dural sac area was < 100 mm2. Based on these criteria, postoperative decompression can be considered adequate with a dural sac area of 100 mm2 or more, indicative of sufficient relief. Concerning the dural spaces below 70 mm2 as a state of lumbar stenosis, an increase of 30 mm2 or more postoperatively can be deemed as substantial decompression. The second substantial decompression criterion, which is the more than 50 percentage increase in the dural sac area, is based on the concept of Hermansen et al. and other studies32,33,34. Our patients had a baseline of less than 70 mm2 (41.5, 41.7, and 38.4 mm2, respectively), and the degree of postoperative decompression was over 30 mm2 and 50% in all groups (76.2 mm2, 203.7%; 71.0 mm2, 195.4%; and 78.7 mm2, 228.5%, respectively). Meeting both criteria in all groups indicated that sufficient decompression was achieved. However. the OPEN group exhibited worse postoperative muscle injury compared to the endoscopic groups. Multifidus muscles are widely used, in research, to assess postoperative muscle damage in research24,35,36. Thus, MF was measured in the posterior spinal muscles and was identified in the surgical range. The loss of muscle mass with these procedures would expect to occur from devascularization and denervation during surgical exposure in the OPEN group and potentially some pressure necrosis from retraction. Certainly, this would not be apparent over the relatively short 6-month period following surgery. However, the observed difference in CSA in our study allows us to assess the extent of muscle stripping, and through this, we infer that the degree of muscle atrophy in the OPEN group would likely increase over the long term follow-up. The recent rise in endoscopic surgeries led to numerous comparative studies being conducted on full-endoscopic vs. biportal approaches37,38. Full endoscopic surgery may struggle with dural decompression due to limited instrument movement, which is ultimately attributed to the steep learning curve involved in this procedure. Therefore, since the surgeons in our study possessed over a decade of experience using this technique, some significant discrepancies may have been masked.
Previous retrospective studies found insignificant differences in clinical improvements between groups37,38,39. In our study, all three groups demonstrated clinical improvement in most of the questionnaire areas, whereas the difference in the amount of improvement was not observed. However, in the case of the VAS for back pain, the OPEN group exhibited less improvement than the other endoscopic groups. According to Fan et al.36, the severity of the muscle injury can cause persistent back pain. Muscle and ligament injuries likely affect pain relief; however, our study could not assess site-specific pain. Thus, since the VAS score is involved with general back pain and neurological factors, this interpretation may be limited.
To our knowledge, we conducted the first multicenter prospective study. Our results were compared between conventional open laminectomy and endoscopic approaches as well as between different types of endoscopic surgery. By combining an MRI follow-up along with laboratory analysis, it was feasible to assess muscle damage more precisely than in previous studies. Furthermore, by incorporating the clinical outcomes, we intended to provide overall guidance in the selection of surgical procedures for lumbar central stenosis. This study has some limitations, whereby it was not randomized or blinded. Selection bias was judged to be modest because every institution performed its most frequently conducted procedure using identical indications. This was a non-matched case–control study, which aimed to include all prospective data. Unfortunately, we could not use the initially planned data from surgery for a tubular retractor since the preference of MIS surgeons in South Korea has rapidly shifted from tubular retractors to endoscopic surgery. Due to the regional prevalence of endoscopic surgery, few surgeons were assigned to perform tubular decompression. Recruiting enough patients proved challenging, meaning necessitating plan modifications was inevitable. We believe conducting multinational studies would be beneficial, as it is a globally performed approach for preserving posterior elements (supraspinous ligaments, interspinous ligaments) and muscles on the opposite side during surgery. It is unfortunate that we could not achieve uniformity in pre-, intra-, and post-operative protocols among the participating hospitals, which can be considered a limitation of our multicenter study. There was variability in the hospital environment, including staffing in the operating room and system configurations. Moreover, protocols for preoperative antibiotic types and administration, anesthesia methods, as well as postoperative medication and dressing methods, were not standardized across all centers. There were also limitations regarding the measurements. Assessing the extent of decompression through 3D measurements could have been more beneficial. The lack of standardization of MRI equipment across hospitals posed a challenge in multicenter studies. The variability in the interval of axial cuts, ranging from 3 to 5 mm, meant that areas with relatively less severe stenosis could be more prevalent depending on the hospital, potentially introducing bias into the results. To address this, we identified the narrowest site of stenosis preoperatively and assessed stationary anatomical structures without movement, which were less related to the surgical range, to determine the postoperative cut. Using this approach, we aimed to enhance representativeness while reducing bias by conducting measurements using 2D axial cuts. Furthermore, if stenosis-specific outcome scales such as the Swiss Spinal Stenosis Questionnaire40, Oxford Claudication Score41, or Quebec Back Pain Disability Questionnaire42 had been used for comparison of clinical outcomes, it would have provided a more specific comparison of functional recovery in patients post-surgery. Due to language validation issues with the questionnaires, the already validated versions of VAS, ODI, and SF-36 were employed. Lastly, the sample size was small, and the follow-up period was limited. Thus, a larger, more long-term randomized trial is required.
Conclusion
The findings of this prospective multicenter research focusing on lumbar central stenosis supported the non-inferiority of endoscopic surgery over conventional open laminectomy. Both conventional and endoscopic approaches can provide satisfactory outcomes for postoperative dural expansion, as well as similar QOL improvements. However, endoscopic surgery excels in muscle preservation and rapid postoperative back pain relief. Therefore, endoscopic spine surgery, whether full-endoscopic or biportal endoscope, is a promising option for treating lumbar central stenosis.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request. We can share the final Excel data without patient identification.
References
Deyo, R. A. et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303, 1259–1265 (2010).
Parker, S. L. et al. Two-year comprehensive medical management of degenerative lumbar spine disease (lumbar spondylolisthesis, stenosis, or disc herniation): A value analysis of cost, pain, disability, and quality of life. J. Neurosurg. Spine 21, 143–149 (2014).
Benoist, M. The natural history of lumbar degenerative spinal stenosis. Jt. Bone Spine 69, 450–457 (2002).
Malmivaara, A. et al. Surgical or nonoperative treatment for lumbar spinal stenosis?: A randomized controlled trial. Spine (Phila Pa 1976) 32, 1–8 (2007).
Weinstein, J. N. et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N. Engl. J. Med. 358, 794–810 (2008).
Verbiest, H. A radicular syndrome from developmental narrowing of the lumbar vertebral canal. J. Bone Joint Surg. Br. 36, 230–237 (1954).
Guiot, B. H., Khoo, L. T. & Fessler, R. G. A minimally invasive technique for decompression of the lumbar spine. Spine (Phila Pa 1976) 27, 432–438 (2002).
Ikuta, K. et al. Short-term results of microendoscopic posterior decompression for lumbar spinal stenosis. J. Neurosurg. Spine 2, 624–633 (2005).
Denis, F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin. Orthop. Relat. Res. 189, 65–76 (1984).
Haher, T. et al. The contribution of the three columns of the spine to spinal stability: A biomechanical model. J. Spinal Disord. 27, 432–439 (1989).
Abumi, K. et al. Biomechanical evaluation of lumbar spinal stability after graded facetectomies. Spine (Phila Pa 1976) 15, 1142–1147 (1990).
Bresnahan, L., Ogden, A. T., Natarajan, R. N. & Fessler, R. G. A biomechanical evaluation of graded posterior element removal for treatment of lumbar stenosis: Comparison of a minimally invasive approach with two standard laminectomy techniques. Spine (Phila Pa 1976) 34, 17–23 (2009).
Spetzger, U., Bertalanffy, H., Reinges, M. T. & Gilsbach, J. Unilateral laminotomy for bilateral decompression of lumbar spinal stenosis part II: Clinical experiences. Acta Neurochir. 139, 397–403 (1997).
Yeung, A. T. The evolution and advancement of endoscopic foraminal surgery: One surgeon’s experience incorporating adjunctive techologies. SAS J. 1, 108–117 (2007).
De Antoni, D. J., Claro, M. L., Poehling, G. G. & Hughes, S. S. Translaminar lumbar epidural endoscopy: Anatomy, technique, and indications. Arthroscopy 12, 330–334 (1996).
Kim, H. S. et al. Percutaneous full endoscopic bilateral lumbar decompression of spinal stenosis through uniportal-contralateral approach: Techniques and preliminary results. World Neurosurg. 103, 201–209 (2017).
Heo, D. H., Son, S. K., Eum, J. H. & Park, C. K. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: Technical note and preliminary clinical results. Neurosurg. Focus 43, E8 (2017).
Lim, K. T. et al. Therapeutic feasibility of full endoscopic decompression in one-to three-level lumbar canal stenosis via a single skin port using a new endoscopic system, percutaneous stenoscopic lumbar decompression. Asian Spine J. 13, 272 (2019).
Morgenstern, R., Morgenstern, C. & Yeung, A. T. The learning curve in foraminal endoscopic discectomy: Experience needed to achieve a 90% success rate. Int. J. Spine Surg. 1, 100–107 (2007).
Tenenbaum, S. et al. Percutaneous posterolateral transforaminal endoscopic discectomy: Clinical outcome, complications, and learning curve evaluation. Surg. Technol. Int. 21, 278–283 (2011).
Park, S.-M. et al. Learning curve for lumbar decompressive laminectomy in biportal endoscopic spinal surgery using the cumulative summation test for learning curve. World Neurosurg. 122, e1007–e1013 (2019).
Joh, J.-Y. et al. Comparative study of neck pain in relation to increase of cervical epidural pressure during percutaneous endoscopic lumbar discectomy. Spine (Phila Pa 1976) 34, 2033–2038 (2009).
Arai, Y. et al. A prospective comparative study of 2 minimally invasive decompression procedures for lumbar spinal canal stenosis: Unilateral laminotomy for bilateral decompression (ULBD) versus muscle-preserving interlaminar decompression (MILD). Spine (Phila Pa 1976) 39, 332–340 (2014).
Bresnahan, L. E. et al. Assessment of paraspinal muscle cross-sectional area after lumbar decompression. Clin. Spine Surg. 30, E162–E168 (2017).
Kawaguchi, Y., Matsui, H. & Tsuji, H. Back muscle injury after posterior lumbar spine surgery: A histologic and enzymatic analysis. Spine (Phila Pa 1976) 21, 941–944 (1996).
Arts, M. P., Nieborg, A., Brand, R. & Peul, W. C. Serum creatine phosphokinase as an indicator of muscle injury after various spinal and nonspinal surgical procedures. J. Neurosurg. Spine 7, 282–286 (2007).
Brown, S. J., Child, R. B., Day, S. H. & Donnelly, A. E. Exercise-induced skeletal muscle damage and adaptation following repeated bouts of eccentric muscle contractions. J. Sports Sci. 15, 215–222 (1997).
Sanchez-Ramirez, D. C. et al. Association of serum C-reactive protein and erythrocyte sedimentation rate with muscle strength in patients with knee osteoarthritis. Rheumatology 52, 727–732 (2013).
Schaap, L. A., Pluijm, S. M., Deeg, D. J. & Visser, M. Inflammatory markers and loss of muscle mass (sarcopenia) and strength. Am. J. Med. 119, 526 (2006).
Hamanishi, C., Matukura, N., Fujita, M., Tomihara, M. & Tanaka, S. Cross-sectional area of the stenotic lumbar dural tube measured from the transverse views of magnetic resonance imaging. Clin. Spine Surg. 7, 388–393 (1994).
Steurer, J., Roner, S., Gnannt, R. & Hodler, J. Quantitative radiologic criteria for the diagnosis of lumbar spinal stenosis: A systematic literature review. BMC Musculoskelet. Disord. 12, 1–9 (2011).
Schönström, N. & Willén, J. Imaging lumbar spinal stenosis. Radiol. Clin. North Am. 39, 31–53 (2001).
Mannion, A. et al. Dural sac cross-sectional area and morphological grade show significant associations with patient-rated outcome of surgery for lumbar central spinal stenosis. Eur. Spine J. 26, 2552–2564 (2017).
Hermansen, E. et al. Comparable increases in dural sac area after three different posterior decompression techniques for lumbar spinal stenosis: Radiological results from a randomized controlled trial in the NORDSTEN study. Eur. Spine J. 29, 2254–2261 (2020).
Kim, D.-Y., Lee, S.-H., Chung, S. K. & Lee, H.-Y. Comparison of multifidus muscle atrophy and trunk extension muscle strength: Percutaneous: Versus: Open pedicle screw fixation. Spine (Phila Pa 1976) 30, 123–129 (2005).
Fan, S. et al. Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: Minimally invasive procedure versus conventional open approach. Eur. Spine J. 19, 316–324 (2010).
Heo, D. H., Lee, D. C. & Park, C. K. Comparative analysis of three types of minimally invasive decompressive surgery for lumbar central stenosis: Biportal endoscopy, uniportal endoscopy, and microsurgery. Neurosurg. Focus. 46, E9 (2019).
Hua, W. et al. Clinical outcomes of uniportal and biportal lumbar endoscopic unilateral laminotomy for bilateral decompression in patients with lumbar spinal stenosis: A retrospective pair-matched case-control study. World Neurosurg. 161, e134–e145 (2022).
Park, S.-M. et al. Biportal endoscopic versus microscopic lumbar decompressive laminectomy in patients with spinal stenosis: A randomized controlled trial. Spine J. 20, 156–165 (2020).
Stucki, G. et al. Measurement properties of a self-administered outcome measure in lumbar spinal stenosis. Spine (Phila Pa 1976) 21, 796–803 (1996).
Makan, P. Clinical assessment of lumbar spinal stenosis. J. Bone Joint Surg. Br. 30, 158 (1998).
Kopec, J. A. et al. The Quebec back pain disability scale: Measurement properties. Spine (Phila Pa 1976) 20, 341–352 (1995).
Author information
Authors and Affiliations
Contributions
Y.H. wrote the main manuscript text and prepared figures and tables. J.P. conceptualized the study, and J.K., C.C., J.C., H.K., J.J., C.L, and M.P. collected clinical data. All authors reviewed the manuscript, and J.P. approved the final version on behalf of all authors.
Corresponding author
Ethics declarations
Competing interests
The study was supported primarily by research funds from the Korean Spinal Neurosurgery Society (KSNS). The funding organization was not involved in any aspect of the trial, including study design, data analysis, or results interpretation. Partial support for patient follow-up examination expenses. All authors declare no personal conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hwang, Y.H., Kim, JS., Chough, CK. et al. Prospective comparative analysis of three types of decompressive surgery for lumbar central stenosis: conventional, full-endoscopic, and biportal endoscopic laminectomy. Sci Rep 14, 19853 (2024). https://doi.org/10.1038/s41598-024-65923-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65923-3
This article is cited by
-
The usefulness and utilisation of Lu’s retractor for unilateral biportal endoscopic discectomy: a retrospective cohort study
Journal of Orthopaedic Surgery and Research (2025)
-
How I do it—tubular trans-spinous process muscle-sparing approach for bilateral lumbar microdiscectomy: surgical technique with illustrative video
Acta Neurochirurgica (2025)