Abstract
Atrial fibrillation (AF) is more prevalent in individuals with chronic kidney disease (CKD) compared to the general population. While a potential inverse correlation between lipid levels and AF has been proposed, it remains unclear if this relationship applies to CKD patients. This study examined the connection between the ratio of low-density lipoprotein cholesterol to high-density lipoprotein cholesterol (LDL-C/HDL-C) and the likelihood of AF in CKD patients. Data was gathered from 21,091 consecutive CKD patients between 2006 and December 31, 2015. We examined the link between the LDL-C/HDL-C ratio and AF in CKD patients through binary logistic regression, as well as various sensitivity and subgroup analyses. The dataset that backs up these analyses is available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0230189. Of the 21,091 CKD patients, 211 (1.00%) were diagnosed with AF. The cohort, predominantly male (79.93%), had a mean age of 60.89 ± 10.05 years. The mean LDL-C/HDL-C ratio was 1.39 ± 0.35. After adjusting for covariates, a significant inverse association was observed between the LDL-C/HDL-C ratio and the incidence of AF in CKD patients (OR = 0.422, 95% CI 0.273–0.652, P = 0.00010). The robustness of these findings was confirmed through sensitivity analysis. Subgroup analysis revealed a strong correlation between the LDL-C/HDL-C ratio and incident AF in patients without hypertension (HR = 0.26, 95% CI 0.15–0.45). Conversely, this association was absent in hypertensive patients (HR = 1.09, 95% CI 0.54–2.17). Our research shows an independent inverse correlation between the LDL-C/HDL-C ratio and the risk of AF in CKD patients. It is advised to refrain from excessively aggressive reduction of LDL levels in CKD patients, as this could elevate the risk of developing AF.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is a complex arrhythmia associated with severe complications such as stroke, cognitive impairment, and heart failure, which can significantly diminish quality of life and elevate morbidity and mortality rates1,2,3. The worldwide prevalence of atrial AF is 37,574 million cases (0.51% of worldwide population), increased also by 33% during the last 20 years4. While around 2% of adults in Europe and North America are affected by AF5,6, its prevalence in China is lower, at 0.71% among those over 35 years of age7. The risk of developing AF increases with age, particularly in individuals 55 years and older, with a lifetime risk of 1 in 5.38. The risk of AF increases, especially with hemodynamic or mechanical atrial load due to accompanying diseases or conditions. Cardiovascular risks include hypertension, heart failure, coronary artery disease/myocardial infarction, heart valve disease, cardiomyopathy, sick sinus syndrome, myocarditis/pericarditis, and post-cardiac surgery. Non-cardiovascular risks include thyroid dysfunction, electrolyte imbalances, CKD, diabetes, infections, alcohol consumption (“holiday heart syndrome”), drug use (especially cocaine), Chronic obstructive pulmonary disease, and sleep apnea9.
AF and chronic kidney disease (CKD) share a bidirectional relationship, CKD heightens the risk of AF, while AF can accelerate the progression and onset of CKD10,11,12,13. CKD patients exhibit a 2–3 times higher prevalence of AF compared to the general population5,14. Specifically, AF prevalence is 1.0% in individuals without CKD, 2.8% in those with stages 1–2 CKD, 2.7% in stage 3 CKD, and 4.2% in stages 4–5 CKD15.
Dyslipidemia, characterized by elevated total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) and low high-density lipoprotein cholesterol (HDL-C), is a recognized risk factor for coronary heart disease16. Dyslipidemia frequently occurs in individuals with CKD, with an estimated prevalence of around 40%17. LDL particles and LDL-C contribute to atherosclerotic cardiovascular disease, which is also a risk factor for AF18.
While LDL-C remains the primary target for lipid-lowering therapy, cardiovascular events may still occur despite its reduction19,20. The LDL-C/HDL-C ratio is increasingly recognized as a predictor of ischemic heart disease offering insights beyond LDL-C levels alone21,22,23. This ratio correlates with the thickness of the carotid intima-media24.
Studies on blood lipids and AF risk have yielded inconsistent results. While some research suggests that lower cholesterol levels may increase the risk of AF, a phenomenon known as the cholesterol paradox25,26, longitudinal studies have produced either conflicting outcomes or no significant correlation27,28,29. Notably, a comprehensive study of 88,785 patients found an inverse relationship between TC, LDL-C levels, and incident AF over a seven-year period. However, no substantial association was found between AF and HDL-C or triglycerides (TG)30. A combined analysis of two cohorts indicated that high levels of HDL-C and TG, rather than TC or LDL-C, were linked to a lower risk of AF28. To date, no studies have explored the link between dyslipidemia and AF in individuals with CKD.
Prior investigations have shown an inverse relationship between the LDL-C/HDL-C ratio and the development of AF, particularly in individuals aged 75 and older30,31. Moreover, research involving coronary artery bypass graft (CABG) patients revealed a higher incidence of postoperative AF with elevated LDL-C/HDL-C ratios, notably in women32.
Previous studies have primarily examined the general population or specific subgroups such as post-CABG patients32. Considering the heightened incidence of AF in patients with CKD, it is imperative to identify associated risk factors. Yet, the potential link between the LDL-C/HDL-C ratio and AF in CKD patients remains unexplored. This study, therefore, investigates the association between the LDL-C/HDL-C ratio and AF in a cohort of 21,091 CKD patients, who represent a high-risk cohort with distinct pathophysiological characteristics, positioning our study as a pioneer in this niche but important area of research. This targeted approach contributes valuable insights that are particularly relevant for the management of CKD patients.
While our study is a secondary analysis, and the data was originally collected by the Kailuan cohort, the research design, statistical analysis, and interpretation of results are entirely our contributions, ensuring the originality of the findings. We employed binary logistic regression, sensitivity analysis, and subgroup analysis to rigorously examine the relationship between the LDL-C/HDL-C ratio and AF. These advanced statistical methods substantiate the robustness, reliability, and minimized susceptibility to confounding factors of our findings.
Subjects and methods
Data source
The data used in our research was obtained from the publicly available repository: (https://journals.plos.org/plosone), by Zhang et al.33 Reference: Association of atrial fibrillation and clinical outcomes in adults with chronic kidney disease: A propensity score-matched analysis. https://doi.org/10.1371/journal.pone.0230189. This open-access article was published under the Creative Commons Attribution License, which allows for unrestricted use, distribution, and reproduction in any medium, as long as the original author and source are properly credited.
Study design
The cross-sectional study extensively utilized healthcare data from the KAILUAN Health and Wellness Registry (Registration number: ChiCTR-TNRC-11001489). In our rigorous examination, we focused on the pivotal independent variable: the ratio of LDL-C to HDL-C. The dependent variable under study was AF, categorized dichotomously as either AF present or AF absent (AF, non-AF).
Study population
The Kailuan study is a prospective cohort investigation within the Kailuan community of Tangshan, a modern city. Managed by the Kailuan Group, this self-contained community features 11 hospitals overseeing residents’ healthcare. Between June 2006 and October 2007, the study invited all 155,418 employees and retirees aged 18 and over from the Kailuan Group, drawing a 65.3% participation rate with informed consent. The participants’ average age (51.93 years) closely mirrored that of the general employee population (51.92 years), though there was a notable gender disparity (79.9% men compared to 85.9% in the company). Ultimately, the study recruited 101,510 individuals (81,110 men and 20,400 women, aged 18–98), who completed questionnaires and underwent medical and lab assessments across the 11 hospitals. Biennial follow-ups from 2006 through December 31, 2015, tracked potential risk factors and new disease occurrences. The study was conducted in line with the Helsinki Declaration and jointly approved by the Ethics Committees of Kailuan General Hospital, Beijing Chaoyang Hospital, and TianTan Hospital, with all participants providing written informed consent. Clinical Trial Registration—URL: http://www.chictr.org.cn/proj/show.aspx?proj=1441. Unique identifier: ChiCTR-TNC-1100148934,35,36,37.
Eligibility for initial recruitment required individuals to be at least 45 years old, with an estimated glomerular filtration rate (eGFR) below 60 mL/min/1.73 m2, and/or displaying proteinuria levels from 1+ to 4+ as determined by urine dipstick analysis. Exclusion criteria included a history of kidney treatments such as transplantation or dialysis, incomplete or invalid initial data, or an eGFR above 60 mL/min/1.73 m2 in the absence of proteinuria. Following exclusions, the study population comprised 21,587 adult men and women aged 45 and older diagnosed with CKD, as cited in reference33.
For the current study, we implemented several steps to ensure data quality and integrity. We first eliminated cases with missing LDL-C (N = 303) and HDL-C (N = 2) values. We also identified and excluded LDL-C/HDL-C ratio outliers, defined as values more than ± 3 standard deviations from the mean (N = 191). After these exclusions and quality control measures, our final analysis included a total of 21,091 cases, as shown in Fig. 1.
Flowchart of study participants. The inclusion of participants. 101,150 participants were assessed for eligibility in the original study. We excluded participants less than 45 years old (N = 22,512), eGFR ≥ 60mL/min per 1.73 m2 and proteinuria negative (N = 56,379), missing or invalid baseline data (N = 630), previous dialysis or transplant (N = 42), missed LDL-C (n = 303), missed HDL-C (n = 2), unreasonable abnormal values of LDL-C/HDL-C (n = 191). The final analysis included 20,191 subjects in the present study.
Variables
Low-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio
In our analysis, we regarded the LDL-C/HDL-C ratio as a continuous variable, which was calculated as follows: LDL-C/HDL-C ratio = low-density lipoprotein cholesterol by high-density lipoprotein cholesterol.
Atrial fibrillation
To guarantee accuracy and consistency, all subjects underwent standard 12-lead electrocardiograms (ECGs) following strict protocols. Skilled electrocardiographers at the reading center of Kailuan General Hospital assessed these ECGs using the Minnesota ECG classification system33.
Covariates
Drawing on clinical expertise and prior research, we identified the following covariates for our study14,30,38: (1) Continuous variables included diastolic blood pressure (DBP), systolic blood pressure (SBP), age, waist circumference (WC), triglycerides (TG), C-reactive protein (CRP), and eGFR; (2) Categorical variables consisted of gender, education level, and clinical history of smoking, alcohol intake, diabetes mellitus (DM), hypertension, myocardial infarction (MI), peripheral artery disease (PAD), and proteinuria.
Baseline data were collected upon enrollment, with participants providing socio-demographic information and medical histories to skilled interviewers during clinical assessments. Anthropometric measurements and blood pressure readings were taken accurately. Hypertension was defined as having an SBP of 140 mmHg or higher, a DBP of 90 mmHg or more, or current use of antihypertensive medication. DM was determined by a fasting glucose level of 126 mg/dl or greater, a random glucose level of 200 mg/dl or higher, or the use of insulin or other glucose-lowering medications.
Blood samples were uniformly collected and analyzed at the Kailuan General Hospital Laboratory, which included serum creatinine and other assays such as TC, LDL-C, HDL-C, TG, and C-reactive protein (CRP)35. The eGFR was calculated using the CKD-EPI creatinine equation, adjusted with a 1.1 coefficient for the Asian population, and categorized to reflect different levels of renal function. Proteinuria was assessed through urine dipstick tests, with results ranging from none to 4+33. An eGFR below 60 mL/min/1.73 m2 denoted impaired renal function39. WC cut-offs for overweight were established at more than 94 cm for men and 80 cm for women40. Additional details are provided in previous studies33,34,35.
Statistical analysis
Continuous variables were presented as mean ± standard deviation for those with a normal distribution, or as median with interquartile ranges for non-normally distributed data. Categorical variables were expressed as frequencies and percentages. Participants were categorized into quartiles based on their LDL-C/HDL-C ratio31. Differences in categorical variables between LDL-C/HDL-C ratio quartiles were evaluated using the χ2 test, one-way ANOVA for normally distributed continuous variables, and the Kruskal–Wallis H test for skewed continuous data. Participants were also categorized based on the presence of AF. The χ2 test was used for categorical variables, independent samples t-test for normally distributed variables, and the Mann–Whitney test for variables with a skewed distribution.
Our dataset had missing values, including smoking history for 131 participants (0.62%), alcohol intake history for 574 (2.72%), hypertension history for 574 (2.72%), DM history for 573 (2.71%), education level for 334 (1.58%), SBP for 71 (0.34%), DBP for 71 (0.34%), WC for 507 (2.40%), CRP for 157 (0.74%), TC for 2 (0.0000948%), and proteinuria for 1737 (8.23%). To address these missing entries, we utilized multiple imputation, considering variables like age, gender, WC, DBP, SBP, TC, CRP, proteinuria, TG, eGFR, history of alcohol intake, smoking, education level, DM, hypertension, MI, congestive heart failure, PAD, and prior strokes. We conducted a missing data analysis assuming data were missing at random (MAR)41,42.
To analyze the independent linear relationship of the LDL-C/HDL-C ratio and AF
Adhering to the STROBE guidelines43, we utilized both univariate and multivariate binary logistic regression to construct three distinct models: the unadjusted Crude model without covariate adjustment; the minimally adjusted Model I, which considers sociodemographic factors like age, gender, WC, DBP, SBP, education level, and history of alcohol intake, smoking, DM, hypertension, MI, and PAD; and the fully adjusted Model II, which expands on Model I by further adjusting for covariates outlined in Table 3, including proteinuria, CRP, TG, eGFR. We provided the odds ratios and their 95% confidence intervals for each model.
The selection of covariates was guided by an assessment of collinearity. To assess potential collinearity among covariates, we calculated the variance inflation factor (VIF)44. The VIF was computed using the formula VIF = 1/(1-R2), with the R-squared value obtained from the linear regression equation. The variable of interest was treated as the dependent variable, while all other variables were considered independent. If the VIF value exceeded 5, we eliminated the corresponding variables from the multivariate regression analysis to address significant collinearity concerns (Table S1).
Sensitivity analysis
To bolster the credibility of our study’s findings, we conducted a comprehensive range of sensitivity assessments45. Initially, we divided the LDL-C/HDL-C ratio into four quartiles and analyzed patterns to confirm its effectiveness as a continuous variable and explore potential non-linear relationships. Recognizing that a history of DM, hypertension, MI, and PAD could elevate the risk of AF9,30, we performed additional sensitivity analyses. These analyses were limited to individuals without such medical conditions to examine the relationship between the LDL-C/HDL-C ratio and AF risk. Furthermore, we employed E-values46 to assess the potential impact of unmeasured confounding factors on the observed association between the LDL-C/HDL-C ratio and the likelihood of AF.
Subgroup analysis
We conducted subgroup analyses using stratified binary logistic regression to explore the associations between outcomes and subgroups defined by gender, age, WC, kidney function, proteinuria, educational level, and histories of alcohol consumption, smoking, DM and hypertension. Initially, continuous variables were grouped based on established clinical thresholds: age (< 64, 64–74, ≥ 75 years); kidney function (< 60, ≥ 60 mL/min/1.73 m2); proteinuria (yes, no); and WC (normal: < 94 cm for men, < 80 cm for women; overweight: ≥ 94 cm for men, ≥ 80 cm for women)30,31,38,40. Subsequently, we accounted for relevant covariates along with the stratification variable itself, including gender, age, WC, education level, alcohol intake and smoking histories, DM, hypertension, MI, PAD, SBP, DBP, proteinuria, CRP, TG, and eGFR. Finally, likelihood ratio tests were used to compare models with and without interaction terms among subgroups, allowing for the assessment of potential effect modification47,48.
Ethical approval and consent to participate
The previously published article has stated that ethical approval was jointly obtained from the Ethics Committees of Kailuan General Hospital, Beijing Chaoyang Hospital, and TianTan Hospital, which adhered to the ethical principles outlined in the Declaration of Helsinki. Informed consent was secured in writing from all participants before their enrollment 33,34,35,36,37.
Results
Characteristics of patients
Table 1 displays the demographic and clinical characteristics of the 210,191 adult participants in the study. Among them, 79.93% (16,857) were male, with an average age of 60.89 ± 10.05 years. The average LDL-C/HDL-C ratio was 1.39 ± 0.35, and the mean eGFR was 67.23 ± 20.22 mL/min/1.73 m2. AF was present in 1.00% of the cohort (211 individuals).
Participants were categorized into quartiles based on their LDL-C/HDL-C ratios (< 1.105, ≥ 1.105 to < 1.350, ≥ 1.350 to < 1.590, ≥ 1.590). Compared to the reference group with an LDL-C/HDL-C ratio below 1.105, those in the highest quartile exhibited higher mean SBP, DBP, WC, TC, TG, and CRP levels. This group also showed a higher percentage of females, individuals with over nine years of education, and increased rates of hypertension, DM, and proteinuria, along with lower eGFR. In contrast, they had a lower occurrence of AF, MI, male gender, and smoking and alcohol use (Table1).
AF patients tended to be older with elevated SBP, DBP, WC, and lower LDL-C/HDL-C ratio, TC, TG, and LDL-C. They also had a higher prevalence of proteinuria, congestive heart failure, and prior strokes, as well as hypertension. No significant differences were observed in HDL-C, CRP, eGFR, gender, alcohol intake, education level, MI, PAD, and DM between the AF and non-AF groups (see Table2).
Results of a binary logistic regression model used in univariate analyses
Our univariate analysis revealed an inverse relationship between AF incidence and several lipid metrics, notably the LDL-C/HDL-C ratio (OR = 0.39, 95% CI 0.25–0.61), LDL-C (OR = 0.60, 95% CI 0.47–0.75), TG (OR = 0.80, 95% CI 0.69–0.93), and TC (OR = 0.69, 95% CI 0.59–0.80). In contrast, positive correlations were observed between AF likelihood and age (OR 1.08; 95% CI 1.06–1.09), DBP (OR = 1.01, 95% CI 1.00–1.02), SBP (OR = 1.01, 95% CI 1.00–1.01), proteinuria (OR = 1.43, 95% CI 1.08–1.88) and WC (OR = 1.03, 95% CI 1.02–1.04), all reaching statistical significance (P < 0.05; Table 3). However, non-significant associations were found between AF and factors such as gender, hypertension, alcohol intake, education level, MI, PAD, DM, HDL-C, CRP or eGFR.
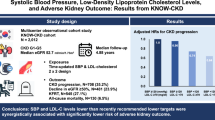
Analysis of multivariate data using binary logistic regression
Using binary logistic regression, the researchers examined the association between the LDL-C/HDL-C ratio and the risk of AF. The initial model indicated a significant inverse correlation; a one-unit increase in the LDL-C/HDL-C ratio was linked to a 61.1% decrease in the probability of AF (OR = 0.389, 95% CI 0.25–0.607, P = 0.00003). This protective effect remained consistent even after accounting for demographic and clinical variables such as age, gender, WC, education level, alcohol consumption, smoking habits, diabetes, and cardiovascular events in Model I (OR = 0.427, 95% CI 0.277–0.660, P = 0.00013). Importantly, the fully-adjusted Model II, which also included variables like age, gender, WC, education level, history of alcohol intake, smoking, DM, hypertension, MI, PAD, DBP, SBP, BMI, proteinuria, TG, eGFR, maintained a consistent effect size with a 57.8% reduction in AF risk per unit increase in the LDL-C/HDL-C ratio (OR = 0.422, 95% CI 0.273–0.652, P = 0.00010). The consistent confidence intervals across the models highlight the reliability of the regression analyses in illustrating the inverse association between the LDL-C/HDL-C ratio and AF risk, as outlined in Table 4.
Sensitivity analysis
To validate the strength of our results, we performed a set of sensitivity analyses. The researchers transformed the original continuous LDL-C/HDL-C ratio into quartiles and reinserted this modified variable into the statistical model. The results showed a consistent pattern in effect sizes among the quartiles, with a P-value for trend that matched the findings from the initial continuous variable. (see Tables 4 and 5).
We further evaluated the robustness by excluding participants with pre-existing PAD and hypertension, then re-conducted the adjusted analysis. The inverse correlation between the LDL-C/HDL-C ratio and AF risk remained significant in both scenarios (OR 0.392, 95% CI 0.251–0.613 and OR 0.252, 95% CI 0.144–0.442, see Table 5). Recognizing the potential confounding impact of DM and MI on AF, we repeated the analysis after excluding individuals with these conditions. The negative relationship between the LDL-C/HDL-C ratio and AF risk persisted (Table 5).
Lastly, we computed an E-value to assess the impact of potential unmeasured confounders. With an E-value of 4.58 exceeding the relative risk attributed to both hidden confounders and the LDL-C/HDL-C ratio, this robust E-value indicates that the association between the LDL-C/HDL-C ratio and AF risk is resilient to unmeasured confounding factors.
The results of subgroup analyses
A subgroup analysis investigated potential confounders such as eGFR and proteinuria that might influence the link between the LDL-C/HDL-C ratio and AF risk. We categorized by factors like gender, age, WC, proteinuria status, education, smoking, DM, hypertension, eGFR, and alcohol consumption to assess trends in effect size.
Table 6 shows that factors such as gender, age, WC, proteinuria status, education, smoking, DM, hypertension, eGFR, and alcohol consumption did not have a significant impact on the relationship between the LDL-C/HDL-C ratio and AF risk (all P-interaction > 0.05). This suggests that the association remains consistent and unaffected by these variables. Specifically, a strong correlation between the LDL-C/HDL-C ratio and incident AF was observed in the patients without hypertension (HR = 0.26, 95% CI 0.15–0.45). In contrast, no association was probed in those with hypertension (HR = 1.09, 95% CI 0.54–2.17).
Discussion
In our study of 210,191 CKD patients, 211 (1.00%) were diagnosed with AF, a lower incidence than the previously reported 2.7% to 4.2% in similar groups15. This discrepancy might be due to biennial ECG follow-ups underestimating AF’s true frequency. Notably, AF prevalence here was higher than the general population’s 0.71%7, emphasizing the need to identify AF risk factors. Patients with AF were older, with higher SBP, DBP, WC, but lower TC, TG, LDL-C, and LDL-C/HDL-C ratios. They also had higher rates of heart failure, strokes, hypertension, and proteinuria.
Limited research exists on the link between LDL-C/HDL-C ratio and AF risk in CKD patients. The Kailuan Study, with 88,785 participants initially without AF, found an inverse relationship between higher LDL-C/HDL-C ratio and lower AF risk after a 7.12-year median follow-up (HR: 0.77, 95% CI 0.66–0.91)30. Our recent study supports these findings, indicating lower LDL-C/HDL-C ratios in CKD patients with existing AF. Utilizing thorough logistic regression analysis to adjust for various possible confounding factors such as age, gender, WC, alcohol consumption history, smoking, DM, hypertension, MI, PAD, DBP, SBP, CRP, proteinuria, TG, eGFR, we discovered a significant inverse correlation between the LDL-C/HDL-C ratio and the risk of AF in CKD patients.
A Polish study on lipid profiles and AF risk revealed that, after adjusting for demographics and medications, the highest LDL-C/HDL-C quartile showed a significantly lower AF prevalence (OR 0.75, 95% CI 0.61–0.94, P = 0.010). However, this association was only significant for individuals aged 75 and above. No significant variances were observed for those aged 50–64 and 65–74 (OR = 0.78, 95% CI 0.53–1.14; OR = 0.74, 95% CI 0.52–1.05), suggesting that lipid ratios might mainly impact AF risk in the elderly31.
Our broader study somewhat supports these findings, indicating a negative correlation between the LDL-C/HDL-C ratio and AF risk, consistent with previous research. Nevertheless, our results differ in that this association was consistent across all age groups, not just individuals over 75. This discrepancy could be attributed to our focus on a CKD population and a more thorough adjustment for confounding factors.
Through detailed subgroup analyses, we ascertained potential confounders like gender, eGFR, proteinuria, age, WC, education, DM, hypertension, smoking, and alcohol consumption had minimal impact on the LDL-C/HDL-C ratio and AF association. These investigations have strengthened the validity and reliability of the connection between the LDL-C/HDL-C ratio and AF risk. We confirmed the consistent protective effect of the LDL-C/HDL-C ratio against AF in CKD individuals with comorbidities like DM, obesity, and varying lifestyles (smoke and alcohol intake). This suggests the LDL-C/HDL-C ratio could be a predictor of AF in CKD patients, and modifying this ratio might reduce AF risk.
However, hypertension modifies this relationship. The LDL-C/HDL-C ratio showed a stronger association with AF in CKD participants without hypertension, while no association was found in those with hypertension. Since hypertension is a major AF risk factor9, it can obscure the LDL-C/HDL-C ratio’s impact on AF in CKD, making the relationship statistically nonsignificant. Thus, lipid levels should be managed in CKD patients without hypertension to reduce AF risk. For CKD patients with hypertension, the primary focus should be on blood pressure management to decrease AF risk.
To our knowledge, this study is the first to explore the inverse relationship between the LDL-C/HDL-C ratio and AF in patients with CKD, who are at an increased risk of cardiovascular events. Elucidating the role of lipid profiles in AF is crucial for developing effective primary and secondary prevention strategies for the disorder. By specifically targeting the CKD population, applying meticulous statistical adjustments, and conducting sensitivity analyses, our research significantly advances the understanding of lipid ratios and AF risk in this high-risk group. The insights gained may lead to better risk stratification and more precise interventions to reduce the incidence of AF and its complications in individuals with CKD.
In cardiovascular research, the complex interplay between lipoprotein dynamics and AF is yet to be fully elucidated. The LDL-C/HDL-C ratio’s role in AF pathogenesis is multifaceted. Firstly, previous studies have indicated that higher levels of HDL-C are inversely associated with the risk of AF28. The hypothesized mechanisms linking HDL-C to AF involve its anti-inflammatory and antioxidant effects, which may reduce the risk of cardiovascular diseases and subsequently decrease the formation of arrhythmic tissue substrates that lead to AF49. Secondly, cholesterol, crucial for cellular membrane composition, can alter membrane fluidity and permeability50, and affect ion channels like Kv1.5 K+, Kir2.1 K+, and Na+ channels, which are vital for maintaining atrial rhythm, can induce prolongation of QT interval. That was a mechanism of AF development51,52,53. Thirdly, experimental cholesterol depletion disrupts calcium handling, adrenergic signaling, and myofibrillar integrity, impairing cardiomyocyte contractility54.
Additionally, reports suggested that lipoproteins possess anti-inflammatory properties and Kim et al.55 found that patients with AF exhibited significantly impaired lipoprotein functionality, leading to elevated levels of oxidation and inflammation. AF is associated with inflammation, indicated by increased endothelial activation markers, tissue factor, platelet activation, and fibrinogen56. This inflammation is linked to lower TC, LDL-C, HDL-C levels but higher TG, indicating that lower cholesterol levels might signal the inflammatory processes contributing to AF development57. During systemic inflammation, lipoproteins mitigate by neutralizing endotoxins58. Previous studies indicate that lipoprotein effects on AF go beyond cholesterol levels, involving LDL and particles size; notably, smaller particles are inversely associated with AF risk59. AF patients have smaller, more oxidized, glycated, and TG-rich lipoproteins that promote foam cell formation and diminish HDL’s antioxidant defense60, exacerbating the inflammatory processes leading to AF61,62.
Study strengths and limitations
This cross-sectional study presents several strengths and some limitations. A significant strength is the relatively large sample size (21091 CKD patients), which allows for analyses that were not possible in previous smaller studies. To our knowledge, this is the first study to examine the association between the LDL-C/HDL-C ratio and AF risk among Chinese patients with CKD. We also employed multiple imputation to enhance statistical power and reduce bias from missing covariate data.
As an observational study, the potential for residual confounding exists. Nonetheless, we utilized rigorous statistical adjustments to mitigate the effects of measurable confounders. Our findings’ robustness was further tested through sensitivity analyses, which included independent variable transformation, subgroup analyses, E-value calculations for assessing potential unmeasured confounding, and re-analysis among participants without significant comorbidities, all contributing to the reliability of our results.
However, some limitations must be acknowledged. The cross-sectional design precludes definitive causal inferences. The study centers on a predominantly male occupational cohort from Northern China, with 65.31% of the 155,418 invited employees participating. The “employee records” from Kailuan Company indicate a notable sex distribution discrepancy (85.93% men in the company versus 79.90% in the cohort)36,37. This suggests a potential for selection bias, as healthier individuals might opt out of the free medical examination, affecting the findings’ generalizability. Despite this, the regional focus aids in controlling unmeasured socioeconomic variables. Future research would benefit from a broader design and a more diverse participant base. While we accounted for known confounders, the impact of uncontrolled or unmeasured factors, particularly concerning medications, cannot be ruled out, which is a common limitation in observational studies. Lipid-lowering treatment is common among CKD patients. For instance, many CKD patients use omega-3 fatty acids. The association between omega-3 fatty acids and increased AF risk has been thoroughly researched63. Moreover, lipid-lowering therapy can significantly impact the levels of LDL-C/HDL-C ratio in the bloodstream. Although the initial studies lacked information about the medication. Nevertheless, the E-value analysis indicates that unmeasured confounding is unlikely to account entirely for our findings. Incorporating additional variables, such as medication data, would enhance the depth of future analyses.
Conclusion
In conclusion, our study confirms the LDL-C/HDL-C ratio as an independent predictor of AF in individuals with CKD. An inverse association emerges between the LDL-C/HDL-C ratio and AF risk. These conclusions imply that targeted optimization of the LDL-C/HDL-C ratio could confer protective benefits against AF onset in CKD cohorts. However, we advise judicious caution against pursuing overly aggressive LDL-C reductions in these patients, as excessively low LDL levels may inadvertently heighten AF susceptibility. Moving forward, research should define optimal lipid profiles that balance AF and cardiovascular risk in the setting of CKD.
Data availability
The datasets generated and/or analysed during the current study utilized in our study were obtained from the publicly available repository: (https://journals.plos.org/plosone), courtesy of Zhang et al.33 Reference: Association of atrial fibrillation and clinical outcomes in adults with chronic kidney disease: A propensity score-matched analysis. https://doi.org/10.1371/journal.pone.0230189.
References
Chugh, S. S. et al. Worldwide epidemiology of atrial fibrillation: A global burden of disease 2010 study. Circulation 129, 837–847 (2014).
Vermond, R. A. et al. Incidence of atrial fibrillation and relationship with cardiovascular events heart failure, and mortality: A community-based study from the Netherlands. J. Am. Coll. Cardiol. 66, 1000–1007 (2015).
Ding, W. Y., Protty, M. B., Davies, I. G. & Lip, G. Y. H. Relationship between lipoproteins, thrombosis, and atrial fibrillation. Cardiovasc. Res. 118, 716–731 (2022).
Lippi, G., Sanchis-Gomar, F. & Cervellin, G. Global epidemiology of atrial fibrillation: An increasing epidemic and public health challenge. Int. J. Stroke 16, 217–221 (2021).
Zoni-Berisso, M., Lercari, F., Carazza, T. & Domenicucci, S. Epidemiology of atrial fibrillation: European perspective. Clin. Epidemiol. 6, 213–220 (2014).
Pistoia, F. et al. the epidemiology of atrial fibrillation and stroke. Cardiol. Clin. 34, 255–268 (2016).
Wang, Z. et al. The disease burden of atrial fibrillation in China from a national cross-sectional survey. Am. J. Cardiol. 122, 793–798 (2018).
Guo, Y. et al. Prevalence, incidence, and lifetime risk of atrial fibrillation in China: New insights into the global burden of atrial fibrillation. Chest 147, 109–119 (2015).
Rosemann, A. [Atrial Fibrillation]. Praxis (Bern 1994). 111, 640–652 (2022).
Guo, Y. et al. Comparison of atrial fibrillation in CKD and non-CKD populations: A cross-sectional analysis from the Kailuan study. Int. J. Cardiol. 277, 125–129 (2019).
Bansal, N. et al. Incident atrial fibrillation and risk of end-stage renal disease in adults with chronic kidney disease. Circulation 127, 569–574 (2013).
Carrero, J. J. et al. Incident atrial fibrillation and the risk of stroke in adults with chronic kidney disease: The Stockholm CREAtinine measurements (SCREAM) project. Clin. J. Am. Soc. Nephrol. 13, 1314–1320 (2018).
Watanabe, H. et al. Metabolic syndrome and risk of development of atrial fibrillation: The Niigata preventive medicine study. Circulation 117, 1255–1260 (2008).
Adderley, N. J., Ryan, R., Nirantharakumar, K. & Marshall, T. Prevalence and treatment of atrial fibrillation in UK general practice from 2000 to 2016. Heart 105, 27–33 (2019).
Baber, U. et al. Association of chronic kidney disease with atrial fibrillation among adults in the United States: Reasons for geographic and racial differences in stroke (Regards) study. Circ. Arrhythm. Electrophysiol. 4, 26–32 (2011).
Hedayatnia, M. et al. Dyslipidemia and cardiovascular disease risk among the MASHAD study population. Lipids Health Dis. 19, 42 (2020).
Pan, L., Liao, Y. H., Mo, M. Q., Zhang, Q. H. & Yin, R. X. CMIP SNPs and their haplotypes are associated with dyslipidaemia and clinicopathologic features of IgA nephropathy. Biosci. Rep. 40, BSR20202628 (2020).
Ference, B. A. et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European atherosclerosis society consensus panel. Eur. Heart J. 38, 2459–2472 (2017).
Valensi, P. et al. Atherogenic dyslipidemia and risk of silent coronary artery disease in asymptomatic patients with type 2 diabetes: A cross-sectional study. Cardiovasc. Diabetol. 15, 104 (2016).
Bhanpuri, N. H. et al. Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: An open label, non-randomized, controlled study. Cardiovasc. Diabetol. 17, 56 (2018).
Ridker, P. M., Rifai, N., Cook, N. R., Bradwin, G. & Buring, J. E. Non-HDL cholesterol, apolipoproteins AI and B100, standard lipid measures, lipid ratios, and CRP as risk factors for cardiovascular disease in women. Jama-J. Am. Med. Assoc. 294, 326–333 (2005).
Sun, T. et al. Predictive value of LDL/HDL ratio in coronary atherosclerotic heart disease. BMC Cardiovasc. Disord. 22, 273 (2022).
Gao, P., Wen, X., Ou, Q. & Zhang, J. Which one of LDL-C/HDL-C Ratio and non-HDL-C can better predict the severity of coronary artery disease in STEMI patients. BMC Cardiovasc. Disord. 22, 318 (2022).
Lou, Y. et al. LDL-cholesterol to HDL-cholesterol ratio discordance with lipid parameters and carotid intima-media thickness: A cohort study in China. Lipids Health Dis. 19, 141 (2020).
Xue, Y. et al. Lipid profile and new-onset atrial fibrillation in patients with acute ST-segment elevation myocardial infarction (an observational study in southwest of China). Am. J. Cardiol. 124, 1512–1517 (2019).
Mourtzinis, G. et al. Relation between lipid profile and new-onset atrial fibrillation in patients with systemic hypertension (from the Swedish primary care cardiovascular database [SPCCD]). Am. J. Cardiol. 122, 102–107 (2018).
Watanabe, H. et al. Association between lipid profile and risk of atrial fibrillation. Circ. J. 75, 2767–2774 (2011).
Alonso, A. et al. Blood lipids and the incidence of atrial fibrillation: The multi-ethnic study of atherosclerosis and the Framingham heart study. J. Am. Heart Assoc. 3, e1211 (2014).
Lopez, F. L. et al. Blood lipid levels, lipid-lowering medications, and the incidence of atrial fibrillation: The atherosclerosis risk in communities study. Circ. Arrhythm. Electrophysiol. 5, 155–162 (2012).
Li, X. et al. Lipid profile and incidence of atrial fibrillation: A prospective cohort study in China. Clin. Cardiol. 41, 314–320 (2018).
Harrison, S. L. et al. Lipid levels, atrial fibrillation and the impact of age: Results from the Lipidogram 2015 study. Atherosclerosis 312, 16–22 (2020).
Yu, M. H., Zhang, R. J., Yu, X. Y., Shi, J. W. & Liu, Z. G. Association of LDL to HDL ratio with new-onset atrial fibrillation after on-pump coronary artery bypass graft surgery. BMC Cardiovasc. Disord. 22, 564 (2022).
Zhang, C. et al. Association of atrial fibrillation and clinical outcomes in adults with chronic kidney disease: A propensity score-matched analysis. Plos One 15, e230189 (2020).
Jin, C. et al. Prospective study of fasting blood glucose and intracerebral hemorrhagic risk. Stroke 49, 27–33 (2018).
Wu, Y. et al. Longitudinal fasting blood glucose patterns and arterial stiffness risk in a population without diabetes. Plos One 12, e188423 (2017).
Wu, S. et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a Northern Chinese industrial city. Circ. Cardiovasc. Qual. Outcomes 5, 487–493 (2012).
Zhang, Q. et al. Ideal cardiovascular health metrics and the risks of ischemic and intracerebral hemorrhagic stroke. Stroke 44, 2451–2456 (2013).
Lim, W. H. et al. Proteinuria detected by urine dipstick test as a risk factor for atrial fibrillation: A nationwide population-based study. Sci. Rep. 7, 6324 (2017).
Rifkin, D. E. et al. Albuminuria, impaired kidney function and cardiovascular outcomes or mortality in the elderly. Nephrol. Dial. Transplant. 25, 1560–1567 (2010).
Obirikorang, Y. et al. Knowledge and lifestyle-associated prevalence of obesity among newly diagnosed type II diabetes mellitus patients attending diabetic clinic at Komfo Anokye teaching hospital, Kumasi, Ghana: A hospital-based cross-sectional study. J. Diabetes Res. 2016, 9759241 (2016).
Groenwold, R. H. et al. Missing covariate data in clinical research: When and when not to use the missing-indicator method for analysis. Can. Med. Assoc. J. 184, 1265–1269 (2012).
White, I. R., Royston, P. & Wood, A. M. Multiple imputation using chained equations: Issues and guidance for practice. Stat. Med. 30, 377–399 (2011).
von Elm, E. et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ-Br. Med. J. 335, 806–808 (2007).
Wax, Y. Collinearity diagnosis for a relative risk regression analysis: An application to assessment of diet-cancer relationship in epidemiological studies. Stat. Med. 11, 1273–1287 (1992).
Sun, D., Li, W., Zhang, H., Li, Y. & Zhang, Q. Inverted U-shaped relationship between body mass index and multivessel lesions in Chinese patients with myocardial infarction: A cross-sectional study. J. Int. Med. Res. 48, 1220732372 (2020).
Haneuse, S., VanderWeele, T. J. & Arterburn, D. Using the E-value to assess the potential effect of unmeasured confounding in observational studies. JAMA-J. Am. Med. Assoc. 321, 602–603 (2019).
Mullee, A. et al. Association between soft drink consumption and mortality in 10 European countries. JAMA Intern. Med. 179, 1479–1490 (2019).
Keidel, D. et al. The role of socioeconomic status in the association of lung function and air pollution-a pooled analysis of three adult escape cohorts. Int. J. Environ. Res. Public Health 16, 1901 (2019).
Haywood, L. J. et al. Atrial fibrillation at baseline and during follow-up in ALLHAT (antihypertensive and lipid-lowering treatment to prevent heart attack trial). J. Am. Coll. Cardiol. 54, 2023–2031 (2009).
Subczynski, W. K., Pasenkiewicz-Gierula, M., Widomska, J., Mainali, L. & Raguz, M. High cholesterol/low cholesterol: Effects in biological membranes: A review. Cell Biochem. Biophys. 75, 369–385 (2017).
Balse, E. et al. Cholesterol modulates the recruitment of Kv1.5 channels from Rab11-associated recycling endosome in native atrial myocytes. Proc. Natl. Acad. Sci. USA 106, 14681–14686 (2009).
Epshtein, Y. et al. Identification of a C-terminus domain critical for the sensitivity of Kir2.1 to cholesterol. Proc. Natl. Acad. Sci. USA 106, 8055–8060 (2009).
Lundbaek, J. A. et al. Regulation of sodium channel function by bilayer elasticity: The importance of hydrophobic coupling. Effects of Micelle-forming amphiphiles and cholesterol. J. Gen. Physiol. 123, 599–621 (2004).
Hissa, B., Oakes, P. W., Pontes, B., Ramírez-San, J. G. & Gardel, M. L. Cholesterol depletion impairs contractile machinery in neonatal rat cardiomyocytes. Sci. Rep. 7, 43764 (2017).
Kim, S. M., Kim, J. M., Shin, D. G., Kim, J. R. & Cho, K. H. Relation of atrial fibrillation (AF) and change of lipoproteins: Male patients with AF exhibited severe pro-inflammatory and pro-atherogenic properties in lipoproteins. Clin. Biochem. 47, 869–875 (2014).
Guo, Y., Lip, G. Y. & Apostolakis, S. Inflammation in atrial fibrillation. J. Am. Coll. Cardiol. 60, 2263–2270 (2012).
Khovidhunkit, W. et al. Effects of infection and inflammation on lipid and lipoprotein metabolism: Mechanisms and consequences to the host. J. Lipid Res. 45, 1169–1196 (2004).
Berbée, J. F., Havekes, L. M. & Rensen, P. C. Apolipoproteins modulate the inflammatory response to lipopolysaccharide. J. Endotoxin. Res. 11, 97–103 (2005).
Mora, S., Akinkuolie, A. O., Sandhu, R. K., Conen, D. & Albert, C. M. Paradoxical association of lipoprotein measures with incident atrial fibrillation. Circ. Arrhythm. Electrophysiol. 7, 612–619 (2014).
Kim, S. M. et al. Female patients with atrial fibrillation have increased oxidized and glycated lipoprotein properties and lower apolipoprotein AI expression in HDL. Int. J. Mol. Med. 27, 841–849 (2011).
Maguire, E. M., Pearce, S. & Xiao, Q. Foam cell formation: A new target for fighting atherosclerosis and cardiovascular disease. Vasc. Pharmacol. 112, 54–71 (2019).
Wang, D. et al. Targeting foam cell formation in atherosclerosis: Therapeutic potential of natural products. Pharmacol. Rev. 71, 596–670 (2019).
Lombardi, M. et al. Omega-3 fatty acids supplementation and risk of atrial fibrillation: An updated meta-analysis of randomized controlled trials. Eur. Heart J. Cardiovasc. Pharmacother. 7, e69–e70 (2021).
Acknowledgements
As this secondary analysis builds on prior research, our methodology and data interpretations are extensively informed by the study authored by Zhang et al.33: Association of atrial fibrillation and clinical outcomes in adults with chronic kidney disease: A propensity score-matched analysis. PLoS One. 2020-01-01;15(3): e0230189 https://doi.org/10.1371/journal.pone.0230189. We express our gratitude to all the study authors for their pioneering research, which has informed key aspects of the present analysis.
Funding
Funding for this research was provided through the Shenzhen Second People’s Hospital Clinical Research Fund of Guangdong Province High-level Hospital Construction Project (Grant No. 20203357012), Sanming Project of Medicine in Shenzhen (Grant No. SZSM202211013) and Shenzhen Key Medical Discipline Construction Fund (Grant No. SZXK009).
Author information
Authors and Affiliations
Contributions
M.G., H.H., conceived the research, drafted the manuscript, and did the statistical analysis. D.Q., X.Q., Q.W. revised the manuscript and designed the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guan, M., Hu, H., Qi, D. et al. Inverse relationship between LDL-C/HDL-C ratio and atrial fibrillation in chronic kidney disease patients. Sci Rep 14, 17721 (2024). https://doi.org/10.1038/s41598-024-67100-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-67100-y
Keywords
This article is cited by
-
Association between the triglyceride to high-density lipoprotein cholesterol ratio and diabetes mellitus likelihood in patients with chronic kidney disease
BMC Nephrology (2025)
-
Novel predictive role of glomerular filtration rate in atrial fibrillation development among chronic heart failure patients
BMC Cardiovascular Disorders (2025)
-
L-shaped association of plasma low-density lipoprotein cholesterol with atrial fibrillation recurrence after catheter ablation: a prospective cohort study
Scientific Reports (2024)