Abstract
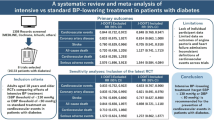
This study pooled data from SPRINT (Systolic Blood Pressure Intervention Trial) and ACCORD-BP (Action to Control Cardiovascular Risk in Diabetes Blood Pressure) trial to estimate the treatment effect of intensive BP on stroke prevention, and investigate whether stroke risk score impacted treatment effect. Of all the potential manifestations of the hypertension, the most severe outcomes were stroke or death. A composite endpoint of time to death or stroke (stroke-free survival [SFS]), whichever occurred first, was defined as the outcome of interest. Participants without prevalent stroke were stratified into stroke risk tertiles based on the predicted revised Framingham Stroke Risk Score. The stratified Cox model was used to calculate the hazard ratio (HR) for the intensive BP treatment. 834 (5.92%) patients had SFS events over a median follow-up of 3.68 years. A reduction in the risk for SFS was observed among the intensive BP group as compared with the standard BP group (HR: 0.76, 95% CI: 0.65, 0.89; risk difference: 0.98([0.20, 1.76]). Further analyses demonstrated the significant benefit of intensive BP treatment on SFS only among participants having a high stroke risk (risk tertile 1: 0.76 [0.52, 1.11], number needed to treat [NNT] = 861; risk tertile 2: 0.87[0.65, 1.16], NNT = 91; risk tertile 3: 0.69[0.56, 0.86], NNT = 50). Intensive BP treatment lowered the risk of SFS, particularly for those at high risk of stroke.
Similar content being viewed by others
Introduction
Elevated blood pressure (BP) has been identified as the major modifiable risk for stroke development with an estimated population-attributable risk of 48%1. Thus, strict and aggressive BP lowering is deemed the most important prevention strategy for both primary and secondary stroke prevention2,3,4,5. A significant benefit of intensive BP lowering the risk of stroke was observed in the ACCORD-BP trial (Action to Control Cardiovascular Risk in Diabetes Blood Pressure Trial)6. On the contrary, this treatment benefit was not found in the SPRINT (Systolic Blood Pressure Intervention Trial) trial with a similar study design but a larger sample size in comparison to the ACCORD-BP trial7.
Although this observed difference could be attributed to the trial population or the study power, treatment heterogeneity on all-cause mortality from the two trials should be otherwise noted. We observed a significant reduction in death from any cause in the SPRINT trial, which contrasted with the ACCORD-BP trial6,7. Clearly, it is known that the occurrence of death would preclude the observation of a stroke. As such, further analyses are needed to account for the presence of this terminal competing risk. Meanwhile, many researchers have identified that individual patients vary from one another in many ways that can affect the potential for benefit, which cannot be captured by conventional one-variable-at-a-time subgroup analyses8,9,10. However, the heterogeneity of treatment effect (HTE) of intensive BP lowering based on individual stroke risk has not been explored.
As such, the aims of this study were (1) to estimate the treatment effect of intensive BP lowering on stroke prevention using the pooled patient data of SPRINT and ACCORD-BP after considering the presence of competing risks from death; (2) to further investigate whether stroke risk score was associated with differential treatment effect.
Methods
Patient population and intervention
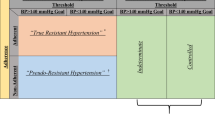
The limited-access SPRINT and ACCORD-BP participant-level data were pooled for the current post-hoc analysis. The design and rationale have been reported previously6,7. Briefly, the SPRINT was a randomized, controlled trial, which was designed to test whether the intensive BP control strategy (lowering systolic BP [SBP] to < 120 mmHg) reduces cardiovascular disease(CVD) compared with standard BP control (lowering SBP to < 140 mmHg) in 9361 high CVD risk participants without diabetes mellitus (DM)7. In contrast, a double 2 × 2 factorial design was used in ACCORD study. All 10,251 high-CVD-risk participants with DM were randomly assigned to intensive or standard glycemic therapy. Additionally, 4733 of 10,251 participants were also randomly allocated to intensive (SBP target to < 120 mmHg) or standard (SBP target to < 140 mmHg) BP therapy (ACCORD-BP trial), which was used for our present analysis6. The population included in the study did not have a prevalent stroke, as SPRINT excluded participants with a history of stroke, and the number of participants with a history of stroke was very low in ACCORD-BP6,7. The flow chart of participant selection was shown in Supplemental Fig. S1.
In general, although the two trials share a similar trial design and are not powered to examine the reduction in CVD subtypes, including stroke, it is of note that differences in BP measurement protocol existed between trials. Unlike the SPRINT trial, an observer remained present during the BP measurements in the ACCORD-BP trial.
Study outcomes
Since participants who die cannot subsequently experience events, Zachary et al., recommended a clinically interpretable method by combing information from occurrences of the terminal event (death) for assessing the treatment effect on the event of interest11, which has been widely used in cancer trials12,13. Of all the potential manifestations of the hypertension, the most severe outcomes were stroke or death. In our study, we defined the outcome of interest as the stroke-free survival (SFS), which was a composite endpoint of time to death or stroke, whichever occurred first.
Statistical analysis
For this analysis, we merged the SPRINT and ACCORD-BP trial data after harmonizing the study duration by censoring it to the longest follow-up duration of SPRINT (4.77 years). Baseline characteristics of the pooled SPRINT and ACCORD-BP participants were described by SBP treatment strategies and expressed as mean ± standard deviation and n (%) for continuous and categorical variables, respectively.
The cumulative incidence rates of SFS in the intensive and standard BP treatment groups were estimated using Kaplan–Meier (KM) curve and compared by the log-rank test. We calculated the number of events and incidence rate per 100 person-years across treatments. Hazard ratios (HRs) and 95% confidence intervals (CIs) for the intensive BP treatment were calculated using the stratified Cox proportional hazards model to account for the clustering of patients from the same trial (i.e., SPRINT or ACCORD-BP). Statistical tests based on the Scaled Schoenfeld residuals were used to identify whether the assumption of proportional hazards has been met.
Apart from the subgroup analyses by individual covariates of interest, we also assessed the HTE across the tertiles of the individual probability of stroke based on the published equations of the revised Framingham Stroke Risk Score (R-FSRS)14. This risk score combines 7 covariates (i.e., age, current smoking, prevalent CVD, prevalent atrial fibrillation, Diabetes mellitus, anti-hypertension treatment, SBP), which would narrow the reference class for each individual to more granular and similar patients and have indicated better prediction in current stroke risks14,15. We also estimated the risk difference and number needed to treat (NNT) of SFS across each R-FSRS strata and overall participants. Available information on serious adverse events across each R-FSRS strata in the SPRINT trial was also summarized. All analyses were performed using STATA version 15.0 (Stata Corporation).
Ethical approval and consent to participate
The data have been made publicly available and can be requested at https://biolincc.nhlbi.nih.gov upon approval. The U.S. National Heart, Lung, and Blood Institute (NHLBI) initiated the SPRINT trial, with co-sponsorship from the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the National Institute on Aging. The trial was designed and conducted by five Clinical Center Networks, which included 102 clinical sites, under the guidance of the Steering Committee. Similarly, the ACCORD trials, sponsored by the NHLBI, were carried out at 77 clinical sites organized into seven networks. Detailed information about the funding agencies and study locations has been previously reported6,7. SPRINT and ACCORD-BP trials and related experimental protocols received approval from the institutional review boards of the participating study sites. We confirm that all methods were performed in the present study are in accordance with the relevant guidelines and regulations. Both trials adhered to the International Conference on Harmonization guidelines, and were registered on http://www.clinicaltrials.gov (Identifier: NCT01206062 for SPRINT and NCT00000620 for ACCORD-BP). The objective of the study was explained, and written informed consent was obtained from study participants. The data used in this study were anonymized before use. Access to the raw data used in this study required permissions from NHLBI. The present analysis received approval from the Xi 'an Medical University ethics approval committee (XYLS2023077).
Results
The baseline characteristics for the individual trial and the pooled participants of SPRINT and ACCORD-BP per treatment allocation are shown in Supplemental Table S1 and Table 1, respectively. 14,094 patients were included, with an average age of 66.18 ± 8.94 years, the proportion of females was 39.66%, 22.39% had clinical CVD, 89.65% received hypertension treatment, and the average systolic blood pressure was 139.51 ± 15.67 mmHg. The average Framingham stroke risk was 9.29 ± 8.00%. In general, baseline characteristics differed between studies, such as the presence of clinical CVD and R-FSRS. However, the baseline characteristics were similar between intensive and standard BP groups except for dyslipidemia and LDL-C.
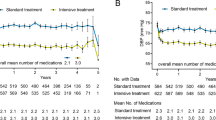
After a median follow-up of 3.68 years, 834 of 14,094 patients (5.92%) had SFS events. The incidence rate for SFS was 1.51 per 100 patient-years in the intensive BP group and 1.79 per 100 patient-years in the standard BP group (Log-rank test: P = 0.018; HR: 0.76, 95%CI: 0.65, 0.89, risk difference: 0.98 [95%CI: 0.20, 1.76]) (Table 2 and Fig. 1). Results from the subgroup analysis in the combined (Fig. 2) or separate data of SPRINT (Supplemental Fig. S2) and ACCORD-BP (Supplemental Fig. S3) generally confirmed the findings of the effect of intensive BP treatment on SFS. The interaction between intensive blood pressure lowering and T2DM was nonsignificant (P = 0.90) (Fig. 2).
Forest plot of stroke-free survival according to subgroups. Incidence rate per 100 patient-years and HRs of intensive blood pressure treatment effect, compared with patients in the standard blood pressure control group. HRs were calculated by adjusting the analysis by adding the interaction term of the BP treatment group and glycemic treatment group (the SPRINT are treated as standard glycemic) to adjust for the influence of factorial design in the ACCORD study. The interaction term of the BP treatment group and each subgroup was also added to the Cox model among the subgroup analyses.
Further analyses demonstrated the heterogeneity of intensive BP treatment on SFS across the tertiles of stroke risk (HR: 0.76 [95%CI: 0.52, 1.11]; 0.87[0.65, 1.16]; 0.69[0.56, 0.86] for low, intermediate and high-risk categories, respectively) (Table 2). Similar results were found in the SPRINT trial and the ACCORD-BP participants (Supplemental Table S2). We also identified that patients in the high-risk categories have the largest risk difference between groups (2.00 [95%CI: 0.33, 3.68]), although this estimate was not statistically significant for low (0.12 [− 0.85, 1.08]) or intermediate (1.10[− 0.18, 2.37]) categories. Correspondingly, for individuals in the high-risk category, the NNT was estimated to be 50 (95% CI, 25, 232), which is much lower than the low (861) and intermediate-risk categories (91). Meanwhile, we also identified that any or related serious adverse events were more frequent among individuals in the intensive versus standard BP groups across all levels of stroke risk based on the available safety data from the SPRINT trial (Supplemental Table S3).
Discussions
Our pooled analysis of the ACCORD-BP and SPRINT trials demonstrated that patients in the intensive BP treatment group (target SBP < 120 mmHg) had a lower relative and absolute risk of SFS compared with those from the standard BP control group (target SBP < 140 mmHg). Additionally, our study indicated that the heterogeneity of intensive BP treatment benefit existed across the tertiles of stroke risk, with a significant reduction in SFS among the group at the highest stroke risk based upon the R-FSRS.
Many observational studies have documented a progressive increase in CVD risk as SBP rises above 115 mm Hg16,17. According to the estimation from the INTERSTROKE study, high BP is the most important contributor among the 10 most commonly identified major modifiable risk factors, which accounts for 48% of the population attributable risk for stroke development1. Thus, BP lowering is regarded as the important strategy for stroke prevention, which has been proven by several randomized trials4,18. However, previous analyses for the SPRINT and ACCORD-BP trials found inconsistent results on the stroke risk reduction from the intensive BP treatment, where a significant treatment benefit was found in the ACCORD-BP trial but not in the SPRINT trial. On the contrary, it is noteworthy that a significant death reduction in the SPRINT trial but not in the ACCORD-BP trial6,7. This brought us attention to the presence of so-called “terminal competing risks” in both trials as a stroke could not be observed if the patient dies before its occurrence19,20. Meanwhile, investigators argued that studies treating the death as censoring in traditional survival analyses can have a depletion of susceptible issue, especially when one of the treatments has a strong effect on the occurrence of a terminal event (eg. death)21,22,23. Therefore, our study, following the recommendation from Zachary R. McCaw et al.11 re-analyzed the two trial data using SFS as the outcome of interest. We consistently found that intensive BP treatment could improve SFS in the pooled and individual trials.
Clinical trials provide average treatment effects across participants with variable patient characteristics. However, patients are likely to receive treatment benefits differently. Risk-based treatments to inform treatment decisions of CVD prevention have been recognized for decades18,24 and were included in some guidelines25,26. Unlike the conventional approach which poorly defined disease risk by individual clinical variables such as age, body mass index, and baseline SBP, risk scores could give a better assessment of risk after integrating all relevant variables simultaneously14,26,27. Our study observed the heterogeneity of intensive BP treatment effect across different levels of baseline stroke risk. Specifically, a significant improvement in SFS and lowest NNT (largest absolute risk difference) from intensive BP treatment was observed in subjects at high stroke risk. These findings highlighted that intensive BP treatment targeting those at greatest stroke risk is likely to be more cost-effective for stroke prevention.
This study has notable strengths, including that SPRINT and ACCORD-BP trials are both large randomized controlled trials evaluating the clinical effectiveness of intensive BP treatment and had similar study design and adjudicated outcomes. In addition, our secondary analysis used a clinically interpretable endpoint that combined information from occurrences of death and stroke simultaneously and naturally accounted for differences in terminal event rates when comparing treatments concerning the time to an undesirable outcome. Nevertheless, some limitations are worthy of comment. First, both trials enrolled high-risk populations and results may not be generalizable to healthier populations. Second, our analysis included the relatively short duration of follow-up in each study. The long-term implications of increased risk of serious adverse events like kidney disease are unclear, which prevented us to assess the net benefit given that the existing safety concerns arise from intensive BP control28,29. Third, data were not available for either study regarding stroke subtype (i.e., ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage), which prevented us to assess potential differences from intensive BP treatment in these subtypes. The cause of stroke and hemodynamic consequences are heterogeneous across stroke subtypes and timing of disease presentation, though the number of hemorrhagic and ischemic stroke subtypes were similar across the intensive and standard BP arms of SPRINT30.
Conclusions
Our analysis confirmed the benefit of intensive BP treatment on SFS. Strick BP treatment could be recommended for the primary prevention of strokes, particularly for those at the highest predicted stroke risk.
Data availability
The data that support the findings of this study are available from NHLBI Biologic Specimen and Data Repository (BioLINCC) (http://www.biolincc.nhlbi.nih.gov/home, https://biolincc.nhlbi.nih.gov) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of NHLBI.
References
O’Donnell, M. J. et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study. Lancet 388, 761–775 (2016).
Appleton, J. P., Sprigg, N. & Bath, P. M. Blood pressure management in acute stroke. Stroke Vasc. Neurol. 1, 72–82 (2016).
Mukete, B. N., Cassidy, M., Ferdinand, K. C. & Le Jemtel, T. H. Long-term anti-hypertensive therapy and stroke prevention: A meta-analysis. Am. J. Cardiovasc. Drugs 15, 243–257 (2015).
Ettehad, D. et al. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet 387, 957–967 (2016).
Katsanos, A. H. et al. Blood pressure reduction and secondary stroke prevention: A systematic review and metaregression analysis of randomized clinical trials. Hypertension 69, 171–179 (2017).
Group AS et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N. Engl. J. Med. 362, 1575–1585 (2010).
Group SR et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 373, 2103–2116 (2015).
Kent, D. M., Steyerberg, E. & van Klaveren, D. Personalized evidence based medicine: Predictive approaches to heterogeneous treatment effects. BMJ 363, k4245 (2018).
Kent, D. M. et al. The predictive approaches to treatment effect heterogeneity (PATH) statement. Ann. Intern. Med. 172, 35–45 (2020).
Dahabreh, I. J., Hayward, R. & Kent, D. M. Using group data to treat individuals: Understanding heterogeneous treatment effects in the age of precision medicine and patient-centred evidence. Int. J. Epidemiol. 45, 2184–2193 (2016).
McCaw, Z. R. et al. Practical recommendations on quantifying and interpreting treatment effects in the presence of terminal competing risks: A review. JAMA Cardiol. 7, 450–456 (2022).
Locatelli, F. et al. Effect of blinatumomab vs chemotherapy on event-free survival among children with high-risk first-relapse B-cell acute lymphoblastic leukemia: A randomized clinical trial. JAMA 325, 843–854 (2021).
Goodwin, P. J. et al. Effect of metformin vs placebo on invasive disease-free survival in patients with breast cancer: The MA32 randomized clinical trial. JAMA 327, 1963–1973 (2022).
Dufouil, C. et al. Revised Framingham Stroke risk profile to reflect temporal trends. Circulation 135, 1145–1159 (2017).
Flueckiger, P., Longstreth, W., Herrington, D. & Yeboah, J. Revised Framingham stroke risk score, nontraditional risk markers, and incident stroke in a multiethnic cohort. Stroke 49, 363–369 (2018).
Lewington, S. et al. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913 (2002).
Lacey, B. et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 05 million adults in China: A prospective cohort study. Lancet Glob. Health 6, e641–e649 (2018).
Collaboration, B. P. L. T. T. Blood pressure-lowering treatment based on cardiovascular risk: A meta-analysis of individual patient data. The Lancet 384, 591–598 (2014).
Austin, P. C., Lee, D. S. & Fine, J. P. Introduction to the analysis of survival data in the presence of competing risks. Circulation 133, 601–609 (2016).
Wolkewitz, M., Cooper, B. S., Bonten, M. J., Barnett, A. G. & Schumacher, M. Interpreting and comparing risks in the presence of competing events. BMJ 349, g5060 (2014).
Austin, P. C. & Fine, J. P. Accounting for competing risks in randomized controlled trials: A review and recommendations for improvement. Stat. Med. 36, 1203–1209 (2017).
Zhao, L. et al. Estimating treatment effect with clinical interpretation from a comparative clinical trial with an end point subject to competing risks. JAMA Cardiol. 3, 357–358 (2018).
McCaw, Z. R. et al. Selecting appropriate endpoints for assessing treatment effects in comparative clinical studies for COVID-19. Contemp. Clin. Trials 97, 106145 (2020).
Jackson, R., Lawes, C. M., Bennett, D. A., Milne, R. J. & Rodgers, A. Treatment with drugs to lower blood pressure and blood cholesterol based on an individual’s absolute cardiovascular risk. Lancet 365, 434–441 (2005).
Stone, N. J. et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129, S1-45 (2014).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 71, 2199–2269 (2018).
Chien, K. L. et al. Constructing the prediction model for the risk of stroke in a Chinese population: Report from a cohort study in Taiwan. Stroke 41, 1858–1864 (2010).
Bress, A. P. et al. Patient selection for intensive blood pressure management based on benefit and adverse events. J. Am. Coll. Cardiol. 77, 1977–1990 (2021).
Leasure, A. C. et al. Association of intensive blood pressure reduction with risk of hematoma expansion in patients with deep intracerebral hemorrhage. JAMA Neurol. 76, 949–955 (2019).
Wright, C. B. et al. Effect of intensive versus standard blood pressure control on stroke subtypes. Hypertension 77, 1391–1398 (2021).
Acknowledgements
This research uses participant-level data from Action to Control Cardiovascular Risk in Diabetes Blood Pressure Trial (ACCORD-BP) and The Systolic Blood Pressure Intervention Trial (SPRINT). The authors would like to acknowledge the ACCORD-BP and SPRINT Investigators and the National Heart, Lung, and Blood Institute investigators greatly acknowledged for conducting the trials and making both data sets publicly available.
Funding
This work was supported by the Shaanxi Provincial Philosophy and Social Science Research Project (2024QN271), the Shaanxi Provincial Sports Bureau Regular Project (2023108), two school-level scientific research fund from Xi’an Medical University (2023BS21 and 2023B27), and the Teacher Education Reform and Development Research Project of Xi’an Medical University (2023JFY-31). The funding body played no role in the design of the study and the collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
ZZ and ZN conducted the formal analysis and contributed to the original draft writing. KC and RS handled visualization, data curation, and reviewed and edited the writing. ZW participated in visualization and the review and editing process. CL and SZ were responsible for conceptualization, review and editing, with SZ also overseeing supervision. TC contributed to conceptualization, review, editing, and supervision. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Z., Nie, Z., Chen, K. et al. Association between intensive blood pressure lowering and stroke-free survival among patients with and without Diabetes. Sci Rep 14, 21551 (2024). https://doi.org/10.1038/s41598-024-72211-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72211-7