Abstract
When treating perimembranous ventricular septal defect, median sternotomy leads to unsightly scar, right subaxillary thoracotomy requires cardiopulmonary bypass, and transcatheter device closure constrained by vascular condition. Using small left intercostal incision, we employed transthoracic device closure to get around these issues. During this study, right subaxillary thoracotomy was used for surgical repair in 117 patients (Surgical group), whereas small left intercostal incision was used for transthoracic device closure in 131 patients (Device group). Retrospective data collection and analysis were conducted. The success rate was comparable (117/117 vs. 130/131, P = 1.000). The device group experienced notably reduced operating time, mechanical ventilation duration, ICU stay, and postoperative hospital stay (All P < 0.001). Given that the device group’s incision was much smaller than the surgical group’s (1.1 ± 0.3 vs. 6.8 ± 1.6 cm, P < 0.001), blood transfusion or drainage tube was not needed. The device group observed a lower frequency of complications, with the exception of small residual shunt. It is feasible and safe to perform transthoracic device closure in children with perimembranous ventricular septal defects via small left intercostal incision. It can be a good minimally invasive substitute for surgical closure when utilized properly.
Similar content being viewed by others
Introduction
Surgical repair using median sternotomy has been the classical approach for treating perimembranous ventricular septal defects (PmVSD) for many years1. While this method allows the full exposure of the cardiac structure, it results in a noticeable scar in the mid-thoracic area that may cause long-term discomfort, both physically and psychologically2. To address this issue, minimally invasive surgical approaches have been developed. Making the incision less noticeable is one strategy, such as performing a right subaxillary thoracotomy where the scar is hidden under the arm3. Minimizing the size of the incision is another strategy, as seen in approaches like transcatheter device closure (TCDC)4 and transthoracic device closure (TTDC)5. These approaches do, however, come with certain drawbacks. Surgical repair through a right subaxillary thoracotomy still requires an open chest and cardiopulmonary bypass (CPB)6. Although TCDC has no CPB, its usage is restricted by vascular constraints and radiographic exposure7,8. While TTDC avoids the aforementioned issues, visible scarring, and potential chest deformity can still occur due to partial sternotomy9. Based on the clinical experience of these three surgical methods, we modified the surgical procedure to conduct TTDC on patients with PmVSD using a small left intercostal incision of only 1 cm, thus obviating concerns related to scarring and the need for CPB.
Recently, right subaxillary thoracotomy has been a widely used minimally invasive approach for the treatment of PmVSD3,10. This study compared the advantages and disadvantages of TTDC utilizing a small left intercostal incision with surgical repair using a right subaxillary thoracotomy, and offered a novel surgical approach for minimally invasive therapy of PmVSD.
Patients and methods
Patients
The study was approved by the Ethics Committee of Fujian Medical University Union Hospital (approval code: 2019KY101), and adhered to the principles of WMA Declaration of Helsinki. Written informed consents were obtained from the guardians of patients.
From January 2021 to December 2022, patients with PmVSD who met inclusion criteria and underwent surgery at our center were all enrolled. The option of the surgical procedure is made by the patient’s guardians. Of them, 117 patients received surgical repair by right subaxillary thoracotomy (surgical group), and 131 patients had TTDC utilizing a small left intercostal incision (device group). Retrospective data collection and analysis were conducted on clinical records obtained during hospitalization, including physical exams, electrocardiograms, chest X-rays, and echocardiograms.
To guarantee comparability, the criteria for inclusion and exclusion were identical for both groups. If the following conditions were satisfied, patients were admitted: ① isolated PmVSD; ② Age greater than 6 months; ③ VSD size more than 3 mm; ④ noticeable clinical manifestations including recurrent respiratory infections, stunted growth, or frequent heart failure; ⑤ significant cardiac enlargement or mild-to-moderate pulmonary hypertension. The following were the exclusion criteria: ① PmVSD that is not restrictive; ② significant prolapse or regurgitation of the aortic valve; ③ lower edge of aortic valve less than 1 mm away from PmVSD; ④ patients with less than 1 year of follow-up.
Surgical closure
For surgical closure under CPB, a right subaxillary thoracotomy was done, and all patients used autologous pericardial patches.
Delivery system and device selection
The occlude system utilized in this study was manufactured in China by Visee Medical Apparatus Co. Ltd, and composed of the occluder, trocar, guidewire, dilator, and delivery sheath (Fig. 1). The occluder is made of nickel-titanium alloy with a shape-memory function. Typically, an occluder is used whose waist diameter is 1 to 2 mm larger than the PmVSD’s maximum diameter. An asymmetric occluder is employed when the gap is more than 1 mm but less than 2 mm between the lower edge of the aortic valve and PmVSD. Otherwise, a symmetrical occluder was used.
Transthoracic device closure
After tracheal intubation with general anaesthesia, the patient was placed in the left slope position. The location of the trans-intercostal incision was determined by TTE following the direction of trans-PmVSD blood flow and the position of the PmVSD, with the left fourth intercostal incision was the most commonly used. When an incision was made, it should be a minimum of 1 cm from the sternum11. The right ventricle was exposed by bluntly separating the intercostal muscles, incising and suspending the pericardium (Fig. 2). The right ventricle was gently compressed with tweezers with TTE guidance, and the puncture spot was chosen based on the spot that had the shortest distance and the same direction as the trans-PmVSD blood flow. After systemic heparinization, the purse string was sewn at the previously identified puncture spot, and the right ventricle was accessed via a central puncture through the purse string. Under guidance of TEE, the guidewire was passed through the PmVSD into the left ventricle (Fig. 3), and subsequently, a delivery sheath was implanted along the guidewire to establish the delivery pathway (Fig. 4). The occluder was delivered into the left ventricle through the delivery sheath, and the left ventricular disc was unrolled. The right ventricular disc was released after the TEE confirmed that the occluder did not affect the surrounding cardiac structure (Fig. 5). Routine chest closure without chest tube placement. At the end of the surgery, the incision was usually only 1 cm in length (Fig. 6). Closure was considered successful in the absence of significant residual shunt (width was less than 2 mm and velocity was less than 2 m/s), severe valve regurgitation, or complete atrioventricular block (CAVB).
Statistical analysis
All data were processed by SPSS version 26.0 (IBM, Armonk, NY). Since this was a retrospective study, to reduce the effects of selection bias and confounders, propensity score matching was performed between the device group and the surgical group. Common confounders as well as factors associated with the severity of VSD patients such as age, sex, weight, VSD size and pulmonary artery pressure were included in the propensity score model12,13. The patients were matched using the nearest neighbor matching (1:1) with a caliper value of 0.02 and no replacement sampling14. Standardized mean differences were used to evaluate the variables balance after matching, and the standardized mean differences of age, sex, weight, VSD size and pulmonary artery pressure after PSM were all within 0.1.
All continuous variables were confirmed to be normally distributed by the Shapiro-Wilk test and were expressed as mean ± standard deviation. Categorical variables were represented as numbers with percentages (n, %). Continuous variables were compared using independent samples t test, while categorical variables were compared using chi-square test or Fisher’s exact test when necessary. P-value (two-tailed) less than 0.05 was regarded as statistically significant.
Result
By using PSM, 108 patients were matched in each of the two groups. The comparisons of the clinical data in both groups did not change before and after the utilization of PSM.
Table 1 shows that there are no notable differences (all P > 0.05) between the two groups’ preoperative clinical data, suggesting that the patients are homogeneous and comparable between the two groups.
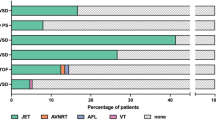
Table 2 shows the perioperative clinic data. Not a single patient died in either group. In the device group, closure was achieved in 130 patients (99.2%), using 107 symmetric occluders and 23 asymmetric occluders. Only one patient experienced closure failure as a result of a significant residual shunt. This patient was transferred for surgical repair through a right subaxillary thoracotomy. In the surgical group, all 117 patients were operated successfully, and the success rates in the two groups did not differ significantly (P = 1.000). As CPB is not required in the device group and the incision is only about 1 cm, no blood transfusion (0/131 vs. 9/117, P = 0.001) or drainage tube were needed. Operation times, ICU stays and mechanical ventilation times were shorter in the device group (all P < 0.001), resulting in a shorter postoperative hospital stay than in the surgical group (P < 0.001).
Table 3 shows the comparison of the two groups’ postoperative complications. Major complications such as hemolysis, CAVB, and occluder dislodgement did not happen in either group. Eleven patients in the surgical group and ten in the device group experienced transient arrhythmias (P = 0.618), which were treated with antiarrhythmic medication before discharge. In the device group, there was a greater prevalence of small residual shunts (≤ 2 mm) compared to the surgical group (13/131 vs. 3/117, P = 0.019). Ten patients in the device group and seven in the surgery group experienced new-onset tricuspid regurgitation (P = 0.608), but it was mild and did not need to be treated.
Follow-up
The median follow-up time in this study was 12.7 months. After surgery, all patients had a physical examination, TTE, and electrocardiogram three and twelve months later, and then again as needed. Table 4 shows the Clinical data during follow-up. In both groups, postoperative tricuspid regurgitation did not change. Only 1 patient in the surgical group and 5 patients in the device group still had a small residual shunt at 3 months postoperatively (P = 0.218), and twelve months after surgery, all small residual shunts vanished. Both groups showed no occluder dislodgement, new-onset aortic or tricuspid regurgitation, CAVB, infective endocarditis, thrombus, or hemolysis.
Discussion
In recent years, surgical trauma and cosmetic effects have become important determining factors in the selection of surgical methods15. TTDC has achieved satisfactory clinical results and has become a commonly used minimally invasive surgical method for PmVSD5,16. Compared with surgical repair, TTDC does not require whole sternotomy and CPB, and is therefore much less traumatic. Compared with TCDC, TTDC avoids the limitation of vascular conditions, can be performed without radiographic exposure, providing an alternative minimally invasive surgical method, especially in hospitals that are ill-equipped to perform TCDC or in which the patient does not tolerate CPB. However, TTDC requires a lower sternotomy, and the risk of bleeding and chest deformity is inevitable7. More importantly, once device closure has failed, the PmVSD can only be repaired by extending the incision using a median sternotomy9, which may cause considerable trauma and aesthetic problems. For superior esthetic outcomes, our department performed TTDC on PmVSD patients utilizing a small left intercostal incision without opening the sternum.
Comparison of incision between right subaxillary and left intercostal
The size and location of the incision are usually the key factor in determining surgical trauma and cosmetic results. Because the incision of right subaxillary thoracotomy is hidden under the resting arm, it has a better cosmetic outcome than median thoracotomy and has become another common approach for surgical repair of PmVSD in recent years10. While surgical repair inevitably requires the exposure of the cardiac structure to establish CPB, the incision of the right subaxillary thoracotomy is still 5 to 8 cm6,17. During the TTDC procedure, we used a chest X-ray to establish the left lung’s border and used TTE to determine the direction of blood flow across the PmVSD to find the optimal location for the intercostal incision. Since just the right ventricle’s puncture spot needs to be exposed, the incision can typically be made close to the optimal puncture spot and shortened to almost 1 cm. Furthermore, the incision would be concealed during breast growth, making it more tolerable for female patients.
Safety and effectiveness of left intercostal incision
In addition to surgical trauma and cosmetic results, the safety and effectiveness of the surgery are also crucial. Generally, minimally invasive techniques have better cosmetic outcomes, but such surgeries are also limited in surgical scope and is therefore more difficult. However, no patient died during this study, and there was no difference in the two groups’ surgical success rates. We believe that left intercostal incision can achieve a good balance between adequate surgical scope and incision aesthetics. Firstly, TTE can accurately localize the projection point of blood flow across the PmVSD on the body surface in order to select the best incision location. Subsequently, by suspending the pericardium, the right ventricle is closer to the incision, and the vision is clearer than expected. Furthermore, the surgeon and assistant can lift the purse string suture together to raise the puncture spot closer to the body surface and keep it relatively fixed, which makes the subsequent operation easier and more visible. Finally, the most critical part of the procedure — the adjustment of the guidewire orientation — is performed completely outside the body and is therefore not limited by the small incision.
Because sternotomy and CPB were not required, patients in the device group experienced significantly less trauma compared to those in the surgical group. This led to shorter operation times, mechanical ventilation times, ICU stays, and postoperative hospital stays.
Comparison of complication between right subaxillary and left intercostal
With the exception of residual shunt, the device group’s complication rate was either the same or lower than the surgical group’s. Significant residual shunt is usually due to a mismatch between the occluder and PmVSD18. This is because the size of the PmVSD is often underestimated due to aortic valve interference. Therefore, when selecting an occluder, the distance from the lower margin of aortic valve to the true upper margin of the PmVSD should be measured. The appearance of a small residual shunt is usually due to the gaps between the occluder and the PmVSD19. Replacing with a larger occluder can reduce the incidence of the small residual shunt, but it may compress the conducting tissue, leading to CAVB, or affect the aortic valve, leading to aortic regurgitation. Generally, residual shunts with diameters less than 2 mm and velocities less than 2 m/s can be observed. Within weeks to months following surgery, small residual shunts may gradually vanish due to the occluder’s progressive deployment and intimalization20. Our follow-up results confirmed this, which showed that one year after surgery, there was no significant different prevalence of residual shunts between the two groups.
Valve damage and CAVB are the main reasons for the limited use of transcatheter closure in PmVSD21. However, no patient in the device group experienced CAVB and valve damage. This is because the delivery access is established through the direct puncture of the right ventricular surface without the need to traverse the tricuspid and aortic valves. Not only that, during the surgery, the TEE can display the sheath and crucial nearby structures, including the tricuspid and aortic valves, in real-time to avoid injury. Moreover, due to the short operating distance, the hard and straight delivery sheath is easy to control accurately and pass through the PmVSD almost perpendicularly, which minimizes the influence of surgery on the conduction system. Nevertheless, we believe that in certain cases, surgical correction is still irreplaceable.
Prevention of pneumothorax and left internal mammary artery injury
Special vigilance for pneumothorax and left internal thoracic artery injury is required when using a small left intercostal incision. The preoperative clarification of the boundaries of the left lung using chest X-ray, and an intraoperative brief cessation of respiration before entering the chest cavity to allow the left lung to atrophy as much as possible help avoid pneumothorax. In this study, to make the intercostal incision as far away from the sternum as possible (at least 1 cm), we move the heart leftward by using the left slope posture, and therefore, no left internal thoracic artery injury occurred. Furthermore, in certain children, TTE can assist prevent injury by detecting the blood flow of the internal thoracic artery.
Limitation
There are several limitations on this study. First off, as this was a retrospective investigation and the grouping of patients was not randomized; therefore, selectivity bias is inevitable. Its findings required to be validated by a multicenter prospective randomized controlled trial. Second, to assess the long-term outcomes, a long-term follow-up is required.
Conclusion
Transthoracic device closure in children with PmVSD via a small left intercostal incision guided by echocardiography is safe and feasible. It does not require median sternotomy or CPB, has no vascular diameter restriction or radiographic exposure, and can be a good alternative to surgery for minimally invasive treatment if used appropriately. We will refine the long-term postoperative follow-up as well as conduct prospective randomized controlled trials to provide more comprehensive clinical information.
Data availability
The data from this study will not be shared publicly. All data included in this study are available upon request by contact with the corresponding author.
References
Lozier, J. S., Sati, M., Cheifetz, I. M. & Bocks, M. L. Update on percutaneous and perventricular device closure of congenital ventricular septal defect. Expert Rev. Cardiovasc. Ther. 21(5), 337–345. https://doi.org/10.1080/14779072.2023.2206566 (2023).
Guan, G., Liu, H., Wang, Y., Han, B. & Jin, Y. Behavioural and emotional outcomes in school-aged children after surgery or transcatheter closure treatment for ventricular septal defect. Cardiol. Young. 24(5), 910–917. https://doi.org/10.1017/S104795111300142X (2014).
An, G., Zhang, H., Zheng, S., Wang, W. & Ma, L. Mid-term outcomes of common congenital heart defects corrected through a right subaxillary thoracotomy. Heart Lung Circ. 26(4), 376–382. https://doi.org/10.1016/j.hlc.2015.05.028 (2017).
Turner, M. E., Bouhout, I., Petit, C. J. & Kalfa, D. Transcatheter closure of atrial and ventricular septal defects: JACC focus seminar. J. Am. Coll. Cardiol. 79(22), 2247–2258. https://doi.org/10.1016/j.jacc.2021.08.082 (2022).
Song, X. et al. Transthoracic device closure of juxtaarterial ventricular septal defects: Midterm follow-up results. Ann. Thorac. Surg. 104(3), 841–846. https://doi.org/10.1016/j.athoracsur.2017.01.042 (2017).
An, G. et al. Minimally invasive surgical closure for doubly committed subarterial ventricular septal defects through a right subaxillary thoracotomy. Interact. Cardiovasc. Thorac. Surg. 23(6), 924–928. https://doi.org/10.1093/icvts/ivw255 (2016).
Hongxin, L. et al. Peratrial device closure of perimembranous ventricular septal defects through a right parasternal approach. Ann. Thorac. Surg. 98(2), 668–674. https://doi.org/10.1016/j.athoracsur.2014.03.029 (2014).
Andreassi, M. G. et al. Cardiac catheterization and long-term chromosomal damage in children with congenital heart disease. Eur. Heart J. 27(22), 2703–2708. https://doi.org/10.1093/eurheartj/ehl014 (2006).
Xu, F. et al. Intraoperative device closure of perimembranous ventricular septal defects another safe and feasible alternative to surgical repair in infants. Eur. J. Cardiothorac. Surg. 42(5), 800–805. https://doi.org/10.1093/ejcts/ezs186 (2012).
Hu, C. X., Tan, J., Chen, S., Ding, H. & Xu, Z. W. Comparison of clinical outcomes and postoperative recovery between two open heart surgeries: Minimally invasive right subaxillary vertical thoracomy and traditional median sternotomy. Asian Pac. J. Trop. Med. 7(8), 625–629. https://doi.org/10.1016/S1995-7645(14)60105-X (2014).
Gao, Q. et al. A study on eccentric occluder via ultra minimal incision of doubly committed subarterial ventricular septal defects. J. Card Surg. 36(6), 2055–2060. https://doi.org/10.1111/jocs.15484 (2021).
Shi, G., Chen, H., Sun, Q., Zhang, H. & Zheng, J. Mattress Stitch—A modified shallow stitching in the surgical closure of large perimembranous ventricular septal defect in infants. Ann. Thorac. Cardiovasc. Surg. 21(3), 282–288. https://doi.org/10.5761/atcs.oa.14-00217 (2015).
Lenoir, M. et al. Pulmonary atresia with ventricular septal defect and tetralogy of Fallot: Transannular path augmentation versus systemic to pulmonary artery shunt for first-stage palliation. Cardiol. Young. 30(11), 1679–1687. https://doi.org/10.1017/S1047951120002553 (2020).
Zhang, Z. Y. et al. The prognostic value of prognostic nutritional index in postoperative onset of PAH in children with isolated VSD: A prospective cohort study based on propensity score matching analysis. Front. Pediatr. 18, 121292786. https://doi.org/10.3389/fped.2024.1292786 (2024).
Ma, J., Shangguan, W., Chen, L. W. & Liao, D. S. Comparison of the clinical effect between the lower sternal incision and the left parasternal fourth intercostal incision in the transthoracic closure of ventricular septal defect. J. Cardiothorac. Surg. 16(1), 165. https://doi.org/10.1186/s13019-021-01543-6 (2021).
Chen, Q. et al. Intraoperative device closure of isolated ventricular septal defects: Experience on 1,090 cases. Ann. Thorac. Surg. 105(6), 1797–1802. https://doi.org/10.1016/j.athoracsur.2018.02.059 (2018).
Zhu, J., Zhang, Y., Bao, C., Ding, F. & Mei, J. Individualized strategy of minimally invasive cardiac surgery in congenital cardiac septal defects. J. Cardiothorac. Surg. 17(1), 5. https://doi.org/10.1186/s13019-022-01753-6 (2022).
Ou-Yang, W. B. et al. Perventricular device closure of perimembranous ventricular septal defect: effectiveness of symmetric and asymmetric occluders. Eur. J. Cardiothorac. Surg. 51(3), 478–482. https://doi.org/10.1093/ejcts/ezw352 (2017).
Wu, L. et al. Hybrid transthoracic periventricular device closure of ventricular septal defects: Single-center experience. Braz J. Cardiovasc. Surg. 36(1), 48–56. https://doi.org/10.21470/1678-9741-2020-0115 (2021).
Sun, Y., Zhu, P., Zhou, P. Y., Guo, Y. L. & Zheng, S. Y. Intra-operative device closure of perimembranous ventricular septal defect without cardiopulmonary bypass under guidance of trans-epicardial echocardiography: A single center experience. J. Cardiothorac. Surg. 11(1), 87. https://doi.org/10.1186/s13019-016-0483-2 (2016).
Shahanavaz, S., Winlaw, D. S. & Opotowsky, A. R. What is blocking transcatheter ventricular septal defect closure. J. Am. Heart Assoc. 11(7), e024963. https://doi.org/10.1161/JAHA.122.024963 (2022).
Acknowledgements
The authors thank the patients’ guardians who participated in the study and the research assistants and study coordinators who assisted during data collection, figure acquisition and the management of the study, including Linfeng Xie and Jian He. The authors also acknowledge assistance from medical writers, proof-readers and editors.
Funding
This work was supported by Natural Science Foundation of Fujian Province, China (Grant Number: 2020J011032, 2022J01696); Joint Funds for the innovation of Science and Technology, Fujian province, China (grant number: 2018Y9047); Fujian Provincial health technology project, China (Grant Number: 2019-1-29).
Author information
Authors and Affiliations
Contributions
DL and CF designed the study; FX and XZ drafted the manuscript; LX and QH collected the clinical data and performed the data analysis, YS made the table and ZL got the Figure. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, F., Zeng, X., Xie, L. et al. Device closure via minimally invasive left intercostal incision in children with perimembranous ventricular septal defect. Sci Rep 14, 26454 (2024). https://doi.org/10.1038/s41598-024-77810-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-77810-y