Abstract
Purpose: Estrogen receptor-positive (ER+), progesterone receptor-negative (PR-) and human epidermal growth factor receptor 2-negative (HER2−) breast cancer (BC) often developed resistance to endocrine treatment (ET). We aimed to explore (1) the different clinicopathological features between ER+/PR+/HER2- and ER+/PR-/HER2- BC, and (2) whether ER+/PR-/HER2- early BC patients could benefit from adjuvant ET. Methods: All patients treated for ER+/HER2- early BC who underwent surgery between 2010 and 2021 from a BC database in China were retrospectively examined. The cases followed up for less than six months were excluded. Results: The records of ER+/PR+/HER2- (n = 10843) and ER+/PR-/HER2- BC (n = 1193) cases were reviewed, with median follow-up times of 35.8 and 47.0 months, respectively. Compared with ER+/PR+/HER2- cases, ER+/PR-/HER2- BC occurred more in postmenopausal women (73.1% vs. 52.9%, p = 0.000) and were more likely to be T > 2 cm (40.6% vs. 37.6%, p = 0.048) and Ki67 > 20%+ (48.1% vs. 36.9%, p = 0.000). However, ER+/PR-/HER2- cases had fewer nodal involvement (32.9% vs. 36.9%, p = 0.000). Approximately 82.2% (981/1193) of ER+/PR-/HER2- patients received ET, while approximately 17.8% (212/1193) did not. Compared to patients did not receive adjuvant ET, the ET group had similar disease-free survival (DFS) (HR = 1.33, 95% confidence interval (CI): 0.68–2.59, p = 0.444) and overall survival (OS) (HR = 1.17, 95%CI: 0.37–3.68, p = 0.799). 65.7% of recurrent ER+/PR-/HER2- patients experienced distant relapse (65.7% vs. 48.2% (for ER+/PR + cases), p = 0.011). By comparison, recurrent ER+/PR+/HER2- patients were more likely to experience only local relapse (31.6% vs. 14.9% (for ER+/PR- cases), p = 0.007). Conclusions: ER+/PR-/HER2- BC was a special subtype with aggressive clinicopathological features and more tend to have distant metastasis rather than nodal involvement or local relapse. ER+/PR-/HER2- early BC did not seem to benefit from adjuvant ET.
Similar content being viewed by others
Introduction
Estrogen receptor-positive (ER+)/ progesterone receptor-negative (PR-) breast cancer (BC) is a special subtype but not rare. According to different studies, it accounts for approximately 6.9–15% of all BC patients1,2,3,4,5. PR is a downstream gene upregulated by ER. Conversely, PR can also modulate the function of ER through the redirection of ERα chromatin binding. The increased expression of gene signature stimulated by PR is associated with better prognosis6. PR loss may be a marker of nonfunctional ER. Hyper-methylation of the PR promoter and genetic loss of PR gene are common in ER+/PR- BC7. Growth factor signaling pathways activate more in this special subtype and may downregulate PR expression7,8,9. Consequently, PR is usually inversely correlated to human epidermal growth factor receptor 2 (HER2) status10. ER+/PR- BC has a higher tumor mutational burden (TMB) than ER+/PR + BC, and exhibits more mutations in TP53 and ERBB25. PR negativity is significantly correlated with worse disease-free survival (DFS) and overall survival (OS) in ER+/HER2- BC11,12,13,14. Although ER+/PR-BC has a higher pathological complete response (pCR) rate, the prognosis is still worse after neoadjuvant treatment15. In HER2- inflammatory BC, ER+/PR- subtype exhibits more aggressive biological features and worse breast cancer-specific survival (BCSS) and OS16. Regardless of HER2 status, ER+/PR- BC is also has a significantly worse prognosis1,3,17,18,19,20.
The role of endocrine treatment (ET) in ER+/PR- BC is still controversial. The ER+/PR- BC with epidermal growth factor receptor (HER1) expression or HER2 overexpression is more likely to resist to tamoxifen in adjuvant treatment10,21. Analysis of data from National Cancer Database (NCDB) demonstrates that hormone blocking therapy benefits OS in ER+/PR- BC22. However, HER2 status are unknown in more than half of study patients. In advanced stage, PR negativity is an independent predictor of worse first-line ET responses for ER+/HER2- BC20. We aim to explore the role of adjuvant ET in early ER+/PR-/HER2- BC and different clinicopathological features from ER+/PR+/HER2- BC.
Materials and methods
Patients
The data of all enrolled patients were from the Shanghai Jiaotong University Breast Cancer Database (SJTU-BCDB) which included the clinicopathological data of patients from 40 breast cancer centers. The inclusion criteria included: (1) patients were initially diagnosed as early breast cancer (pT0-4N0-3M0) and received surgery between 2010 and 2021; (2) breast cancers were pathologically proven and subtyped as ER positive and HER2 negative with immunohistochemistry (IHC) or fluorescence in situ hybridization (FISH, only for HER2 2+) results; (3) follow-up time was longer than six months after surgery. Exclusion criteria were as follows: (1) patients initially diagnosed as stage IV; (2) male or bilateral breast cancer; (3) lack of necessary clinicopathological data. Patients terminated endocrine therapy in 3 months were considered as no-ET. This was a noninterventional study and was approved by the Institutional Review Board of Zhejiang Provincial People’s Hospital (ZPPH). The study was conducted in accordance with the principles set forth in the Declaration of Helsinki. The requirement for informed consent was waived because of the retrospective nature of the study by the Institutional Review Board of ZPPH.
Statistical analysis
DFS was defined as time from surgery to first local or distant relapse, death, last follow-up or secondary cancer diagnosis. OS was defined as intervals from the time of surgery to death of any cause or last follow-up. Differences of distribution were analyzed using χ2 or Fisher exact test and continuous variables were compared using Student’s t-test. Survival analysis was constructed using Kaplan-Meier method and log-rank test. The hazard ratio (HR) and 95% confidence interval (CI) were calculated by Cox proportional hazard regression model. All figures were drawn by Graph Prism 9.3.1. The statistical analyses were performed using IBM SPSS 26.0 and Graph Prism 9.3.1. A two-sided p-value less than 0.05 was considered statistically significant.
Results
According to the inclusion criteria, a total of 10,843 cases of ER+/PR+/HER2-BC and 1193 cases of ER+/PR-/HER2-BC were included in this study. The median follow-up time were 35.8 and 47.0 months, respectively. The PR- BC occurred more in postmenopausal females (PR- vs. PR+: 73.1% vs. 52.9%, p = 0.000) and average age at diagnosis was older in PR- BC patients (PR- vs. PR+: 56.6 vs. 53.2, p = 0.000, Table 1). The PR- BC tended to be more aggressive and more likely to be T > 2 cm (p = 0.048), Ki67 > 20%+ (p = 0.000), AR negative (p = 0.000) and smaller median value of ER expression (80% vs. 90%, p = 0.000). However, PR- BC had less regional nodal metastasis than PR + BC (p = 0.000). 70.1% of PR- BC patients underwent mastectomy, which was higher than PR + BC patients (66%, p = 0.005). The proportion of PR- BC patients receiving chemotherapy was also significantly higher than that of PR + BC patients (81.0% vs. 67.2%, p = 0.000). Of the 1193 PR- BC cases, about 17.8% (n = 212) of patients did not receive ET which was higher than that in PR + patients (14.5%, 1571/10843, p = 0.003). The majority of patients reject ET due to poor compliance, side effects, and unknown reasons. Characteristics of cohort are summarized in Table 1.
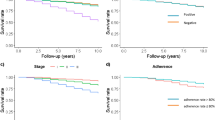
The DFS (HR = 1.394, 95%CI: 1.038–1.873, p = 0.013, Fig. 1A) and OS (HR = 1.824, 95%CI: 1.039–3.203, p = 0.010, Fig. 1B) of ER+/PR-/HER2- BC were worse than those of ER+/PR+/HER2- BC. Adjuvant ET improved DFS (HR = 0.716, 95%CI: 0.514–0.996, p = 0.047, Fig. 2A) and OS (HR = 0.463, 95%CI: 0.231–0.930, p = 0.004, Fig. 2C) in ER+/PR+/HER2- BC, while seemed not benefit DFS (HR = 1.332, 95%CI: 0.685–2.590, p = 0.444, Fig. 2B) and OS (HR = 1.170, 95%CI: 0.372–3.683, p = 0.799, Fig. 2D) in ER+/PR-/HER2- BC. The clinicopathological features of ET and no-ET ER+/PR-/HER2- cohorts were similar, while the no-ET group had more premenopausal (34.1% vs. 25.4%, p = 0.009, Table 2), Ki67 > 20%+ (55.2% vs. 46.6%, p = 0.023, Table 2), post-lumpectomy no RT patients (52.4%(33/63) vs. 13.4%(39/292), p = 0.000, Table 2) and smaller median value of ER expression (50% vs. 80%, p = 0.000, Table 2). Further analysis suggested that adjuvant ET could not improve DFS in each subgroup of ER+/PR-/HER2- BC (Fig. 3). There was no evidence to suggest that adding ovarian function suppression (OFS) to selective estrogen receptor modulator (SERM) or aromatase inhibitor (AI) could improve DFS in PR negative premenopausal chemotherapy patients (p = 0.994, Figure S1A). The DFS of PR negative postmenopausal patients receiving SERM or AI treatment was also similar (p = 0.924, Figure S1B).
The Kaplan–Meier curves of DFS and OS for ER+/PR + and ER+/PR- breast cancer patients with and without adjuvant ET. Adjuvant ET is associated with better DFS (A) and OS (C) in ER+/PR + patients. Adjuvant ET cannot improve DFS (B) and OS (D) in ER+/PR- patients. DFS, disease-free survival; OS, overall survival; ER, estrogen receptor; PR, progesterone receptor; ET, endocrine treatment.
The subgroup analysis of adjuvant ET in ER+/PR- patients. Adjuvant ET cannot improve DFS of ER+/PR- patients in each subgroup. ET, endocrine treatment; HR, hazard ratio; ER, estrogen receptor; HER2, human epidermal growth factor receptor 2; RT, radiation therapy; SLNB, sentinel lymph node biopsy; ALND, axillary lymph node dissection.
The recurrence patterns of PR + and PR- were different. Recurrent PR- BC were more likely to experience distant relapse than PR + BC (65.7% vs. 48.2%, p = 0.011). However, recurrent PR + BC were more likely to experience only local relapse (31.6% vs. 14.9%, p = 0.007). Bone and lung were most common sites of metastasis for both PR+ (bone: 55.0%; lung: 35.6%) and PR- (bone: 43.2%; lung: 40.9%) BC. PR- breast cancer was more prone to brain metastasis (20.5% vs. 6.3%, p = 0.010) (Table 3). The peak of recurrence for PR + BC occurred in the second to third year, while the peak of recurrence for PR- BC occurred in the second and fifth year (Fig. 4).
Discussion
According to current guidelines, all BCs with 1-100% ER nuclear staining are considered ER-positive and should receive adjuvant ET for at least 5 years. The decision of whether accept ET is less referred to PR status. ER+/PR-/HER2- BC commonly accept standard adjuvant ET, but the benefits are still unknown. Limited data suggests that ER+/PR- BC is resistant to adjuvant tamoxifen but more correlated with HER1 and HER2 overexpression10,21. In a ER+/PR- BC cohort with unknown HER2 status, ET is associated with improved outcome in both stages I-III and stage IV patients22. However, compared to ER+/PR + BC, advanced ER+/PR-BC has much smaller clinical benefits from first-line ET20. The role of adjuvant ET in ER+/PR-/HER2- BC was rarely studied.
Actually, ER+/PR- BC tends to overexpress the growth factor associated pathways like HER1, HER2, fibroblast growth factor receptor 4 (FGFR4) and insulin like growth factor-1 (IGF-1)8,9,21,23,24. ER+/PR- BC with HER2 negative seems to be more special and may be in an intermediate transition state with up-regulated expression of other growth factor pathways. In our study, we found that the IHC results of HER2 1+/2 + proportion in ER+/PR + and ER+/PR- BC were similar. There is no evidence indicates that adjuvant ET can improve survival in subgroup and overall cohorts. Consistent with previous studies, premenopausal patients who received the most SERM treatment did not benefit from it10,21. The ATAC trial compared the 5-years tamoxifen, AI and combination in early postmenopausal HR + patients. Early analysis showed that the majority of ER+/PR- BC patients who experienced recurrence were in tamoxifen only and combination arms, indicating that ER+/PR- BC was more sensitive to AI. On the contrary, AI only showed a trend to be superior to tamoxifen in ER+/PR + BC. These results indicated that AIs had greater benefits in ER+/PR- patients than ER+/PR + patients7. However, neither SERM nor AIs can improve survival in our study. Subgroup analysis also indicates that ER+/PR-/HER2- BC with different clinicopathological features cannot benefit from adjuvant ET.
ER+/PR-/HER2- BC seems to have some special features. The average diagnosed age is older than ER+/PR+/HER2- BC and so more patients are in postmenopausal status. ER+/PR-/HER2- BC also more likely to be T > 2 cm and Ki67 > 20%+. Besides, ER+/PR-/HER2- BC tends to have less lymphatic metastasis. Bae et al.1 also reported similar tendency. We further explore the recurrence patterns of both PR + and PR- BC and find that ER+/PR-/HER2- BC is inclined to distant recurrence especially visceral metastasis. Brain metastasis also occurred more in ER+/PR-/HER2- BC which is closely related to worse prognosis. The main recurrence pattern for majority of patients are distant metastasis. As a consequence, we assume ER+/PR-/HER2- BC have more aggressive biological features and more prone to hematogenous and distant metastasis. The ER+/PR-/HER2- BC is with a peak of recurrence in year 2 and 5. Beyond 5 years, it also maintains a significant recurrence rate which suggests the necessity of extended follow-up.
ER+/PR-/HER2- BC exhibits heterogeneity. Xie et al.27 identified five immune subtypes based on the immune-related gene expression profiles. Among them, the immune-hot subtype showed favorable prognosis compared to the immune-cold subtype. Liu et al.8 evaluated data from five cohorts and found that nearly 20% of ER+/PR-/HER2- BC belonged to the PAM50-defined non-luminal-like subgroup featured with ET resistance. Hence, ER+/PR-/HER2- BC needs further classification to predict prognosis and sensitivity to ET which is also a limitation of our study. The median follow-up duration is another limit of our study. It has been reported that ER + BC can experience recurrence in 5 to 15 years after 5-years ET with tamoxifen28. And also, the treatment effect of ET can carry out for long time after termination. These factors may interfere with the results. Consequence, further follow-up is needed to confirm our research conclusions.
Conclusions
ER+/PR-/HER2- BC has more aggressive clinicopathological features and worse prognosis than ER+/PR+/HER2- BC. ER+/PR-/HER2- BC seems cannot benefit from adjuvant ET and the ET strategy needs further study in the future. The recurrence pattern of ER+/PR-/HER2- BC tends to be distant metastasis rather than local recurrence.
Data availability
The data supporting the conclusions of this article are available from the corresponding author on reasonable request.
References
Bae, S. Y. et al. Poor prognosis of single hormone receptor- positive breast cancer: Similar outcome as triple-negative breast cancer. BMC Cancer. 15, 138. https://doi.org/10.1186/s12885-015-1121-4 (2015).
Dauphine, C., Moazzez, A., Neal, J. C., Chlebowski, R. T. & Ozao-Choy, J. Single hormone receptor-positive breast cancers have distinct characteristics and survival. Ann. Surg. Oncol. 27, 4687–4694. https://doi.org/10.1245/s10434-020-08898-5 (2020).
Ng, C. H. et al. Do clinical features and survival of single hormone receptor positive breast cancers differ from double hormone receptor positive breast cancers? Asian Pac. J. Cancer Prev. 15, 7959–7964. https://doi.org/10.7314/apjcp.2014.15.18.7959 (2014).
Li, Z., Wei, H., Li, S., Wu, P. & Mao, X. The role of progesterone receptors in breast cancer. Drug Des. Dev. Ther. 16, 305–314. https://doi.org/10.2147/DDDT.S336643 (2022).
Dai, D. et al. Genetic and clinical landscape of ER + /PR- breast cancer in China. BMC Cancer. 23, 1189. https://doi.org/10.1186/s12885-023-11643-2 (2023).
Mohammed, H. et al. Progesterone receptor modulates ERalpha action in breast cancer. Nature. 523, 313–317. https://doi.org/10.1038/nature14583 (2015).
Cui, X., Schiff, R., Arpino, G., Osborne, C. K. & Lee, A. V. Biology of progesterone receptor loss in breast cancer and its implications for endocrine therapy. J. Clin. Oncol. 23, 7721–7735. https://doi.org/10.1200/JCO.2005.09.004 (2005).
Liu, X. Y. et al. Genomic landscape and endocrine-resistant subgroup in estrogen receptor-positive, progesterone receptor-negative, and HER2-negative breast cancer. Theranostics. 8, 6386–6399. https://doi.org/10.7150/thno.29164 (2018).
Hu, T. et al. Classification of PR-positive and PR-negative subtypes in ER-positive and HER2-negative breast cancers based on pathway scores. BMC Med. Res. Methodol. 21, 108. https://doi.org/10.1186/s12874-021-01297-8 (2021).
Moon, Y. W. et al. Clinical significance of progesterone receptor and HER2 status in estrogen receptor-positive, operable breast cancer with adjuvant tamoxifen. J. Cancer Res. Clin. Oncol. 137, 1123–1130. https://doi.org/10.1007/s00432-011-0976-2 (2011).
Zong, Y. et al. Progesterone receptor status and Ki-67 index may predict early relapse in luminal B/HER2 negative breast cancer patients: A retrospective study. PLoS One. 9, e95629. https://doi.org/10.1371/journal.pone.0095629 (2014).
Park, C. et al. Prognostic values of negative estrogen or progesterone receptor expression in patients with luminal B HER2-negative breast cancer. World J. Surg. Oncol. 14, 244. https://doi.org/10.1186/s12957-016-0999-x (2016).
Van Asten, K. et al. Prognostic value of the progesterone receptor by subtype in patients with estrogen receptor-positive, HER-2 negative breast cancer. Oncologist. 24, 165–171. https://doi.org/10.1634/theoncologist.2018-0176 (2019).
Feeley, L. P., Mulligan, A. M., Pinnaduwage, D., Bull, S. B. & Andrulis, I. L. Distinguishing luminal breast cancer subtypes by Ki67, progesterone receptor or TP53 status provides prognostic information. Mod. Pathol. 27, 554–561. https://doi.org/10.1038/modpathol.2013.153 (2014).
van Mackelenbergh, M. T. et al. Outcome after neoadjuvant chemotherapy in estrogen receptor-positive and progesterone receptor-negative breast cancer patients: A pooled analysis of individual patient data from ten prospectively randomized controlled neoadjuvant trials. Breast Cancer Res. Treat. 167, 59–71. https://doi.org/10.1007/s10549-017-4480-5 (2018).
Luo, Y. et al. ER+/PR- phenotype exhibits more aggressive biological features and worse outcome compared with ER+/PR + phenotype in HER2-negative inflammatory breast cancer. Sci. Rep. 14, 197. https://doi.org/10.1038/s41598-023-50755-4 (2024).
Li, Y. et al. Clinicopathological characteristics and breast cancer-specific survival of patients with single hormone receptor-positive breast cancer. JAMA Netw. Open. 3, e1918160. https://doi.org/10.1001/jamanetworkopen.2019.18160 (2020).
Li, Z. et al. Clinical characteristics and outcomes of single versus double hormone receptor-positive breast cancer in 2 large databases. Clin. Breast Cancer. 20, e151–e163. https://doi.org/10.1016/j.clbc.2019.07.002 (2020).
Fei, F., Siegal, G. P. & Wei, S. Characterizing clinicopathologic features of estrogen receptor-positive/progesterone receptor-negative breast cancers. Clin. Breast Cancer. 22, e788–e797. https://doi.org/10.1016/j.clbc.2022.07.001 (2022).
Zhang, M., Yan, M., Lv, H., Niu, L. & Zeng, H. Clinical study of first-line endocrine therapy for type ER+/PR + and ER+/PR- advanced breast cancer. Ann. Palliat. Med. 10, 238–243. https://doi.org/10.21037/apm-20-2180 (2021).
Arpino, G. et al. Estrogen receptor-positive, progesterone receptor-negative breast cancer: Association with growth factor receptor expression and tamoxifen resistance. J. Natl. Cancer Inst. 97, 1254–1261. https://doi.org/10.1093/jnci/dji249 (2005).
Dembinski, R. et al. Estrogen receptor positive and progesterone receptor negative breast cancer: The role of hormone therapy. Horm. Cancer. 11, 148–154. https://doi.org/10.1007/s12672-020-00387-1 (2020).
Cui, X. et al. Insulin-like growth factor-I inhibits progesterone receptor expression in breast cancer cells via the phosphatidylinositol 3-kinase/Akt/mammalian target of rapamycin pathway: Progesterone receptor as a potential indicator of growth factor activity in breast cancer. Mol. Endocrinol. 17, 575–588. https://doi.org/10.1210/me.2002-0318 (2003).
Kim, H. J., Cui, X., Hilsenbeck, S. G. & Lee, A. V. Progesterone receptor loss correlates with human epidermal growth factor receptor 2 overexpression in estrogen receptor-positive breast cancer. Clin. Cancer Res. 12, 1013s–1018s. https://doi.org/10.1158/1078-0432.CCR-05-2128 (2006).
Baum, M. et al. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early-stage breast cancer: Results of the ATAC (arimidex, tamoxifen alone or in combination) trial efficacy and safety update analyses. Cancer. 98, 1802–1810. https://doi.org/10.1002/cncr.11745 (2003).
Cuzick, J. et al. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol. 11, 1135–1141. https://doi.org/10.1016/S1470-2045(10)70257-6 (2010).
Xie, P., An, R., Yu, S., He, J. & Zhang, H. A novel immune subtype classification of ER-positive, PR-negative and HER2-negative breast cancer based on the genomic and transcriptomic landscape. J. Transl. Med. 19, 398. https://doi.org/10.1186/s12967-021-03076-x (2021).
Kwong, D. et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: Patient-level meta-analysis of randomised trials. Lancet. 378, 771–784. https://doi.org/10.1016/S0140-6736(11)60993-8 (2011).
Funding
This study was supported by the Public Welfare Technology Application Research Project of Zhejiang Province under Grant No. LGF21H160030, and Medical and Health Science and Technology Project of Zhejiang Province (No.2023KY046 and 2023KY543).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Miaochun Zhong, Xiaoqiu Ren, Wenjie Xia and Yangyang Qian; The first draft of the manuscript was written by Jun Wu and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhong, M., Ren, X., Xia, W. et al. The role of adjuvant endocrine treatment in ER+, PR−, HER2− early breast cancer: a retrospective study of real-world data. Sci Rep 14, 26377 (2024). https://doi.org/10.1038/s41598-024-78341-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-78341-2