Abstract
This study aimed to compare the serum lipid profiles between tenofovir disoproxil fumarate (TDF) and tenofovir alafenamide (TAF) in the long-term treatment of chronic hepatitis B (CHB). We analyzed data from treatment-naïve CHB patients administered with TDF or TAF, collected from electronic medical records between May 2017 and September 2022. Serum lipid indices, including total cholesterol (TC), triglycerides (TG), low-density (LDL) and high-density lipoprotein (HDL), and their ratios (TC/HDL, LDL/HDL), were assessed at baseline, and at 48 and 96 weeks. Propensity score matching (PSM) adjusted for baseline differences between groups. From 2344 patients initially screened, 418 were included for the 48-week analysis (265 on TDF, 153 on TAF) and 292 for the 96-week analysis (238 on TDF, 54 on TAF). At 48 weeks, comparing the serum lipid indicators between the pre- and post-treatment, TDF significantly reduced TC and TC/HDL, whereas TAF induced widespread dyslipidemia, characterized by elevated levels of TC, TG, LDL, LDL/HDL, and TC/HDL, and reduced HDL (P < 0.05). After PSM grouping, TAF remained significantly associated with higher TC, TG, LDL, LDL/HDL, and TC/HDL compared to TDF (P < 0.05). Over 48 weeks, TAF treatment was associated with significant increases in TC, TG, and LDL, whereas TDF treatment led to decreases (P < 0.05). TC/HDL and LDL/HDL increased in both groups, but more significant in TAF (P < 0.05). At 96 weeks, the TAF group continued to exhibit significantly higher levels of TC, LDL, and LDL/HDL compared to the TDF group (P < 0.05). Notably, LDL levels were 115.65 ± 28.07 mg/dL in TAF versus 96.07 ± 23.97 mg/dL in TDF. The increase in TC/HDL ratio in the TAF group was higher than in the TDF group, though not statistically significant. Furthermore, TAF treatment was associated with significant increases in LDL (18.58 ± 24.35 mg/dL) and LDL/HDL ratio (0.41 ± 0.95) over 96 weeks, while TDF treatment showed reductions in TC (-8.13 ± 30.86 mg/dL). Between 48 and 96 weeks, most lipid changes in the TDF group were not statistically significant, except for increases in LDL and LDL/HDL. In the TAF group, an increasing trend of LDL and TC/HDL was noted, although LDL showed a slight turnover after 48 weeks. This real-world study provides new evidence that TAF can induce dyslipidemia, while TDF exhibits a lipid-lowering effect in CHB. Patients at high risk for hepatic steatosis and cardiovascular diseases should consider these effects when choosing between TAF and TDF.
Similar content being viewed by others
Introduction
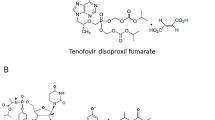
Despite the annual incidence and mortality rate of chronic hepatitis B (CHB) showing a downward trend globally, CHB remains a significant contributor to the global public health burden. According to the latest WHO report, in 2022, 254 million people lived with hepatitis B, and 83% of the 1.3 million deaths due to viral hepatitis were caused by hepatitis B1. Early diagnosis and treatment of CHB is crucial to reduce the incidence of hepatitis B-related complications, such as liver failure, cirrhosis and hepatocellular carcinoma (HCC). However, the diagnosis rate for hepatitis B is only 10%, and the antiviral treatment rate is only 5% worldwide2. To accomplish the goals of the 2030 agenda of WHO for the elimination of CHB, patients are recommended long-term or even life-long antiviral treatment. The first-line antiviral treatment recommended by the guidelines are the nucleo(t)ide analogues (NAs), including enticavir (ETV), tenofovir disoproxil fumarate (TDF) or tenofovir alafenamide (TAF)3.
TDF and TAF are both orally administered prodrugs of tenofovir, extensively used in the treatment of CHB. Approved in 2008, TDF is administered at a daily dose of 300 mg and demonstrates high efficacy, although it is associated with renal and bone side effects due to increased systemic exposure. In contrast, TAF, approved in 2016 and dosed at 25 mg daily, features an improved delivery system that more efficiently targets the liver, minimizing renal and bone toxicity while maintaining comparable antiviral effectiveness. Both drugs effectively suppress viral replication and reduce the risk of cirrhosis and HCC. TAF is often preferred for patients at risk of kidney or bone disease due to its safer profile, while TDF remains a viable option for those without such risks, benefiting from a longer history of use in CHB management3. Nevertheless, previous studies in patients with human immunodeficiency virus (HIV) infection indicated that TDF could improve the serum lipid profiles. Conversely, TAF could induce the dyslipidemia4,5,6,7. In patients with HIV infection, switching from TDF to TAF in the anti-retroviral therapy (ART) regimen significantly elevated the level of total cholesterol (TC) and low-density lipoprotein (LDL)6,7. On the contrary, reversing TAF to TDF could restore the lipid profile8.
Similarly, the effect of TAF on serum lipid levels has been observed in anti-viral treatment for CHB patients. TAF could increase the serum lipid levels including triglyceride (TG), TC, and LDL, compared to other NAs such as ETV and TDF. The incidence of high LDL (defined as ≥ grade 3 fasting LDL levels ) in patients treated with TAF increased from 4% at 48 weeks to 6% at 96 weeks9. In patients switching from TDF to TAF, levels of TG, TC, LDL, and high-density lipoprotein (HDL) were elevated after 48 weeks of follow-up10. A recent meta-analysis, which included 12 studies, demonstrated that TAF worsened lipid profiles after 6 months of treatment11. However, other studies also indicated no significant impact on LDL profile with TAF treatment12,13.
Due to the effective intervention of antiviral treatment, the lifespan of patients with CHB has been extended. Consequently, the risk of non-liver related diseases, such as cardiovascular diseases (CVD) and metabolic syndrome, should also be considered during long-term treatment. Both LDL and TC to HDL ratio (TC/HDL) are recognized as the risk factors for CVD14. In addition to the varied results of LDL level, few studies reported TC/HDL in TAF treatment for CHB. Therefore, the current study aims to investigate the effect of TAF on the serum lipid profile, particularly LDL and TC/HDL, in a real-world setting.
Methods
This study was approved by the Ethics Review Committee of the Mengchao Hepatobiliary Hospital of Fujian Medical University (no. 2024_047_01) and was conducted in accordance with the principles of the Declaration of Helsinki. The Ethics Review Committee of the Mengchao Hepatobiliary Hospital of Fujian Medical University exempted informed consent as the patient information was anonymized.
Study population
We conducted a comprehensive analysis of the electronic medical records (EMR) of treatment-naïve CHB patients treated with TDF or TAF between May 2017 and September 2022 from the outpatient department of the Mengchao Hepatobiliary Hospital of Fujian Medical University, a tertiary hepatobiliary specialist center in Southeast China. The inclusion criteria were: (1) patients aged 18 years or older diagnosed with CHB, defined as serum HBsAg positive, HBeAg positive or negative, HBV-DNA positive, with persistent or recurrent abnormal ALT levels, significant necrosis verified by liver histology, or liver histology/non-invasive indicators suggesting significant liver fibrosis15; (2) administration of branded antiviral agents: TDF (GlaxoSmithKline) or TAF (Gilead Sciences); (3) no interferon therapy; (4) a baseline estimated glomerular filtration rate (eGFR) of ≥ 50 mL/min according to the 2021 updated Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) criteria; and (5) a minimum of 48 weeks of TDF/TAF treatment. Exclusion criteria, based on the EMR information at baseline, encompassed switching to other NAs, coexisting conditions such as Hepatitis C virus infection, alcoholic liver disease, non-alcoholic fatty liver disease, autoimmune liver disease, liver cirrhosis, HCC, other malignant neoplasms, or HIV infection, history of hypertension or diabetes mellitus, and pregnant or lactating patients. Other antiviral agents, such as ETV, were not included in the study because the primary focus was to compare the effects of TAF and TDF, both tenofovir-based treatments, in the management of CHB. Additionally, patients with insufficient clinical data were also excluded.
Data collection
Demographic and clinical data of patients were collected from the EMR. Laboratory examinations, including complete blood count, biochemistry, and virology (hepatitis B virus serological indicators and HBV-DNA), were extracted at baseline and at 48 weeks. Data at 96 weeks were also collected if available. For the current analysis, key fasting serum lipid metabolism indicators were collected, including TG, TC, LDL, and HDL. To comprehensively present the serum lipid profiles, the TC/HDL ratio and the LDL to HDL ratio (LDL/HDL) were also calculated. Since the high-sensitivity quantification method, with a negative criterion of < 20 IU/mL, was not applied to all patients, HBV-DNA levels were categorized as “positive” if they exceeded 500 IU/mL, and “negative” otherwise. Considering the different diagnostic assays used in our hospital, the detection results of HBeAg and HBeAb were also recorded as “positive” or “negative” to facilitate subsequent analysis. We also collected data from patients who had continuous baseline to 96-week follow-up data.
Statistical analysis
In this study, categorical variables were presented as frequencies and proportions, while continuous variables were depicted as means with standard deviations (SD) or medians with interquartile ranges (IQR). The analysis of categorical variables employed the Pearson chi-square test, whereas continuous variables were compared using either a t-test, paired t-test, or Kruskal-Wallis test, as appropriate. The study further implemented propensity score matching (PSM) to compare lipid profiles between the TAF group and the TDF group after treatment, adjusting for baseline characteristics such as gender, age, and serum lipid indicators. This matching was based on the logit of the propensity score with a caliper width of 0.2 SD. Post-PSM, the balance between TAF and TDF groups was verified by standardized differences (SDM) for each baseline variable, all remaining below 0.2 (20%). P-values were two-sided, with values less than 0.05 deemed statistically significant. Data management and statistical analyses, including graph construction, were conducted using R statistical software. (version 4.3.1; R Foundation Inc.; http://cran.r-project.org/).
Results
In the preliminary phase of this investigation, a total of 2344 patients were comprehensive screened. This initial selection was followed by the formation of a focused cohort comprising 418 individuals (265 on TDF, 153 on TAF), each with complete baseline and 48-week follow-up data, warranting their inclusion in this study. According to EMR data, no patients were administered lipid-lowering medications after anti-virus treatment. Additionally, a subset of 292 patients (238 on TDF, 54 on TAF) with baseline and 96-week follow-up data were analyzed. Furthermore, 216 patients with sequential baseline to 96-week data were used to investigate the dynamic changes during the treatment (Fig. 1).
Patient selection and analysis flowchart. A total of 2344 patients were comprehensively screened from electronic medical records. Exclusions included 1916 patients without sufficient data, one patient younger than 18 years old, and nine patients who switched antiviral medication after treatment. A focused cohort comprising 418 individuals (265 on TDF, 153 on TAF) with complete baseline and 48-week follow-up data was analyzed. Additionally, a subset of 292 patients (238 on TDF, 54 on TAF) with baseline and 96-week follow-up data was examined, and 216 patients with sequential baseline to 96-week data were used to investigate dynamic changes during treatment.
Analysis at 48 weeks
The comparative analysis of baseline and 48-week data revealed pronounced differences between the TAF and TDF cohorts (Table 1). These differences spanned a multitude of parameters at baseline, including demographic factors (gender, age), serum lipid profiles (TC, LDL, and LDL/HDL), virological indicators (HBeAg and HBeAb), hepatic function markers [direct/indirect bilirubin, gamma-glutamyl transferase (GGT)], renal function metrics (serum creatinine and eGFR), and the Fibrosis-4 (FIB-4) index. According to FIB-4, seven patients (5%) in the TAF group had fibrosis, compared to two patients (1%) in the TDF group. Notably, during this period, cirrhosis was diagnosed in five patients, with two in the TAF group and three in the TDF group, and no cases of HCC were detected in either group. Comparing the serum lipid indicators between the pre- and post-treatment at 48 weeks, TDF significantly reduced TC and TC/HDL, whereas TAF induced widespread dyslipidemia, including elevated levels of TC, TG, LDL, LDL/HDL, and TC/HDL, and reduced HDL (Table 2).
The PSM process ensured a balanced comparison, aligning patients 1:1 across both groups based on age, sex, and various serum lipid parameters (TG, TC, LDL, and HDL). Subsequent to the PSM, the baseline characteristics exhibited equilibrium across the cohorts (Table 1). The post-PSM cohort included 258 patients, evenly divided with 129 in each group. After 48 weeks of treatment, an examination of clinical parameters revealed that the patients under TAF treatment exhibited significantly lower levels of direct bilirubin (DBIL), alanine aminotransferase (ALT), and alkaline phosphatase (ALP) compared to the TDF group. The respective values were: DBIL (TAF: 2.31 ± 1.16; TDF: 3.11 ± 1.85; P < 0.001) µmol/L, ALT [TAF: 24 (IQR 17, 31); TDF: 27 (IQR 20, 45); P = 0.01] U/L, and ALP (TAF: 78.64 ± 20.68; TDF: 88.38 ± 28.77; P = 0.002) U/L. Moreover, the TAF group showed a noticeable elevation in serum lipid levels in comparison to the TDF group, including TC (TAF: 186.39 ± 37.68; TDF: 167.5 ± 29.44; P < 0.001) mg/dL, TG (TAF: 126.32 ± 70.41; TDF: 102.12 ± 52.69; P = 0.002) mg/dL, LDL (TAF: 118.92 ± 34.23; TDF: 95.07 ± 22.01; P < 0.001) mg/dL, TC/HDL (TAF: 4.23 ± 2.15; TDF: 3.78 ± 0.93; P = 0.033), and LDL/HDL (TAF: 2.69 ± 1.2; TDF: 2.17 ± 0.72; P < 0.001) (Table 3). The changes in these parameters over the 48-week period within the TAF group were marked by significant increases in TC, TG, and LDL, with respective increments of 8.16 ± 28.58 mg/dL, 16.76 ± 68.26 mg/dL, and 17.79 ± 25.63 mg/dL. In contrast, the TDF group exhibited decreases in these values: TC (-7.6 ± 30.47 mg/dL), TG (-3.41 ± 50.25 mg/dL), and LDL (-3.95 ± 20.41 mg/dL), underscoring significant disparities between the two groups (P < 0.05). Both TC/HDL and LDL/HDL increased in both groups, but the increase was more significant in the TAF group (P < 0.05). Despite the TAF group presenting with slightly elevated urea nitrogen levels compared to the TDF group (TAF: 0.4 ± 1.06; TDF: 0.12 ± 1.15 mmol/L; P = 0.044), no notable differences were observed in renal function, as gauged by serum creatinine and eGFR (Table 3).
Subgroup analyses revealed that TDF reduced TC and TC/HDL in HBeAg-positive patients but not in those who were HBeAg-negative. In contrast, TAF increased LDL and LDL/HDL in HBeAg-positive patients and significantly increased TC, TG, LDL, LDL/HDL, and TC/HDL, while reducing HDL in those who were HBeAg-negative (Fig. S1-2; Table S2).
Analysis at 96 weeks
For patients with complete 96-week follow-up data, an additional analysis was performed to elucidate the long-term impact of TAF and TDF treatment on serum lipid profiles. This subset included 54 patients in the TAF group and 238 in the TDF group. Consistent with the results at 48 weeks, TDF significantly reduced TC and TC/HDL, while increasing LDL, compared to baseline. Conversely, TAF continued to elevate LDL and LDL/HDL levels, though the fluctuations in TC, TG, HDL, and TC/HDL appeared to be neutralized (Table 2).
Following a 1:2 ratio PSM adjustment, the comparative analysis included 52 patients in the TAF group and 101 in the TDF group. The findings revealed that TC, LDL, and LDL/HDL levels in the TAF group were significantly higher than those in the TDF group at 96 weeks (P < 0.05; Table S1). Notably, LDL levels were 115.65 ± 28.07 mg/dL in TAF versus 96.07 ± 23.97 mg/dL in TDF. The level of TC/HDL was higher in patients treated with TAF compared to TDF, although the difference was not significant (TAF: 4.19 ± 1.14; TDF: 3.84 ± 1.2; P = 0.082). Analyzing serum lipid fluctuations from baseline to 96 weeks, there was an elevation in TC, LDL, and LDL/HDL in the TAF group, with increases of 6.24 ± 32.37 mg/dL, 18.58 ± 24.35 mg/dL, and 0.41 ± 0.95, respectively. In contrast, TDF treatment was associated with a reduction in TC, showing changes of -8.13 ± 30.86 mg/dL after 96 weeks. The differences in TC, LDL, and LDL/HDL between the TAF and TDF groups were significant (P < 0.05; Table S1).
A total of 216 patients (174 in the TDF group and 42 in the TAF group) with continuous follow-up data were analyzed for serum lipid changes between 48 weeks and 96 weeks. In the TDF group, most changes in serum lipid indicators from 48 to 96 weeks were not statistically significant, except for increases in LDL and LDL/HDL (Fig. 2). However, a continuous decrease was observed in TC and TC/HDL (Fig. 2-A and -F). Similarly, in the TAF group, the majority of the changes were not statistically significant, except for an increase in TC/HDL from 48 to 96 weeks (Fig. 3). The increasing trend of LDL in the TAF group showed a slight turnover after 48 weeks (Fig. 3-C).
The continuous changes of serum lipid after TAF treatment. Comparison of serum lipid levels from 48 to 96 weeks shows no significant changes in TC, TG, LDL, HDL, and LDL/HDL ratio, except for a significant increase in the TC/HDL (P < 0.05). The increasing trend of LDL showed a slight reversal after 48 weeks.
Discussion
Both TDF and TAF are the recommended as first-line NAs for CHB treatment. TAF is suitable for elderly patients and those with renal dysfunction due to its lower renal and bone toxicity compared to TDF. In addition, clinical evidence indicated that TAF could induce serum dyslipidemia while TDF could have lipid-lowering effect16,17. This real-world study revealed significant differences in serum lipid profiles between patients treated with TAF and TDF over 48 and 96 weeks. From baseline to 48 weeks, TAF was associated with elevated levels of TG, TC, HDL, LDL, TC/HDL, and LDL/HDL, whereas TDF was associated with reduced TC and TC/HDL. From baseline to 96 weeks, TAF continued to increase LDL and LDL/HDL levels, while TDF continued to reduce TC and TC/HDL levels. These findings were consistent with a recent meta-analysis of 12 studies involving 6127 patients, which demonstrated that TAF significantly increased the the levels of TG, TC, HDL and LDL compared to TDF or other NAs11. In contrast, a real-world study by Zhang et al., which included 126 patients treated with TAF, reported increases only in TC and TG after 48 weeks, without a significant rise in LDL. The discrepancy may be explained by the imbalance in group sizes, with a ratio of 4:1 between the TAF and control groups18. Another real-world study comparing serum lipid levels between TAF and ETV found that only TC levels were significantly higher in the TAF group after one year of treatment12. Moreover, switching from TDF to TAF could increase the TC and LDL levels in CHB patients after one year17. A multi-center, prospective, observational study also showed that switching from TDF or ETV to TAF significantly increased body weight, serum lipids, fasting glucose, glycosylated hemoglobin, insulin, and insulin resistance10. In contrast, a retrospective cohort study reported significant changes in body weight, but did not observe glucose levels, or serum lipids after switching to TAF19. Despite these variations, most studies support that TAF treatment leads to dyslipidemia in CHB patients. Our study strengthens this evidence, providing real-world data showing TAF’s effect in elevating LDL levels in CHB patients. Furthermore, the current study also analyzed the impact of TAF and TDF on serum lipid in CHB patients with different HBeAg status. The results indicated that, TAF had a more pronounced impact on serum lipids in HBeAg negative patients, leading to significant increases in TC, TG, LDL, TC/HDL, and LDL/HDL levels. Conversely, TDF primarily reduced TC and TC/HDL levels in HBeAg positive patients.
In 2019, an estimated 17.9 million people died from CVD, accounting for 32% of all global deaths20. Serum LDL is recognized as the risk factor of CVD; for every 1 mmol/L reduction in LDL, the incidence of major CVD significantly decreases by 21%21. High TC/HDL is another risk factor for ischemic heart diseases22,23. In the current study, TAF increased LDL and TC/HDL from baseline to 96 weeks. Although LDL levels showed a slightly downturn after 48 weeks, TC/HDL continued to trend upward. Conversely, TDF exhibited a downturn trend in TC/HDL over 96 weeks of treatment. Previous large multi-center randomized clinical trials showed that among HBeAg-positive CHB patients (581 on TAF and 292 on TDF), the proportion with LDL > 300 mg/dL was 4% and 0%, respectively24. Among HBeAg-negative CHB patients (285 on TAF and 140 on TDF), the proportions were 5% and 1%, respectively25. However, a retrospective study including 6631 patients treated with TAF or TDF reported different results, showing no significant changes in LDL compared to TDF from baseline to 12, 24, or 36 months26. Few studies have reported on TC/HDL levels in CHB patients treated with TAF or TDF. According to unpublished data, TC/HDL increased minimally (≤ 5-fold) during TAF treatment over 8 years27. Although the long-term effect of TAF and TDF on LDL and TC/HDL remain unclear, the potential risk of dyslipidemia and CVD should be aware during the long-term TAF treatment. As serum lipid management is crucial in controlling CVD, TDF should be considered for the patients at high risk of CVD, such as metabolic syndrome, high body mass index (BMI) or a history of ischemic heart diseases, due to its lipid-lowering effect.
The high prevalence of co-existing with hepatic steatosis (HS) and CHB is approximately 32.8%28. The association between HS and disease progress is controversial. It has been reported that the co-existent with HS and CHB can suppress the activity of the virus, including lower proportions of HBeAg positive, reduced HBV-DNA level, and higher rates of HBsAg seroclearance28,29. A recent meta-analysis of 19 studies involving 13,262 patients indicated that CHB patients with fatty liver have significantly lower risks of cirrhosis, HCC, and mortality compared to those without fatty liver. Liver biopsy is the gold standard for diagnosing fatty liver. Notably, studies on CHB patients with histologically proven fatty liver have shown a high incidence of disease progression. In a retrospective study of 1089 CHB patients with liver histological evaluation, patients with concurrent non-alcoholic steatohepatitis (NASH) had a higher degree of liver fibrosis30; similarly, HS was associated with fibrosis and cirrhosis in another biopsy-proven cohort of 270 CHB patients31. Compared to those with NASH, CHB patients without NASH had prolonged event-free survival (defined as the absence of liver decompensation events such as jaundice, ascites, hepatic encephalopathy, or variceal bleeding) and prolonged non-HCC survival after 10 years of follow-up30. These findings suggest that fatty liver may have diverse effects on the clinical manifestations of CHB. It is necessary to manage serum lipids and educate patients on appropriate lifestyle modifications when using TAF.
The mechanism of TAF on serum lipid metabolism remains uncertain. The lipid-lowering effect of TDF has reached common agreement of researchers, potentially related to the serum TFV levels and involving in the peroxisome proliferator-activated receptor alpha (PPAR-α) mediated carnitine palmitoyltransferase 1 (CPT1) and CD36 signalling32. Although both TAF and TDF are prodrugs of TFV, they have different metabolic process. Unlike TDF, which is primarily hydrolyzed into TFV by plasma esterases, TAF is mainly hydrolyed into TFV by carboxulesterase1 (CES1) in the liver33. CES1, also known as cholesteryl ester hydrolase (CEH), is highly expressed in the liver and mediates the metabolism of endogenous substances, such as the hydrolysis of cholesterol and triglycerides, playing an important role in lipid metabolism balance. CES1 is a key target in the regulation of ester metabolism, obesity, and diabetes treatment34. In a mouse model, over-expression of hepatic CES1 reduced TG levels and improved glucose homeostasis, while knockdown of hepatic CES1 elevated serum lipid levels (TC and LDL) and induced HS35. Therefore, it is speculated that the lipid dysfunction of TAF could be linked to the low serum level of TFV and the consumption of hepatic CES1. However, more experimental studies are needed to confirm these mechanisms.
There are several limitations in this study. First, due to the shortage of our EMR data, information on smoking habits, alcohol consumption, BMI, and the history of lipid-lowering medications was lacking. Nevertheless, previous prospective cohort studies and real-world research have demonstrated that TAF and TDF affect blood lipid levels, consistent with our findings, even when baseline BMI is comparable between the two groups27,36. Although the history of lipid-lowering medication use in our cohort was unavailable, none of the patients received lipid-lowering treatment during the observation period. Second, the sample size was relatively small. Third, the study was conducted in a single center with an East Asian population, limiting the generalizability of the results. Fourth, HS was not verified in this study due to insufficient information. For patients experiencing dyslipidemia during TAF treatment, the use of statins would be an optimal choice due to their benefits in chronic liver disease. Although high doses of statins can induce liver injury, their use is still noteworthy37. Moreover, a recent real-world study based on EMR compared serum lipid profiles between patients on TAF treatment and healthy controls, showing no significant differences and suggesting that TAF may not worsen serum lipid profiles36. Similarly, our study showed that LDL level decreased from 48 weeks to 96 weeks during TAF treatment. Therefore, more well-designed clinical trials should be conducted to clarify this topic.
In this real-world study, we investigated the serum lipid profiles in the CHB treated with TAF, and compared to those treated with TDF over long-term observation period. The result showed the TAF could induce dyslipidemia, while the TDF had lipid-lowering effect. LDL and TC/HDL levels increased in patients with TAF group, suggesting that clinicians should monitor patients with high risk of HS and CVD when using TAF. Future research should explore the association between HS and long-term cardiovascular outcomes in CHB patients treated with TAF, the safety and efficacy of combining TAF with lipid-lowering medications, and the mechanisms behind TAF-induced dyslipidemia.
Data availability
The data supporting our findings are available from the corresponding author, HaiBing Gao. They are not publicly available due to containing clinical information of patients. All relevant R scripts used for data processing and analysis in this study are publicly available on GitHub (https://github.com/AlongLin/TAF_TDF_Lipid).
Abbreviations
- ALT:
-
Alanine aminotransferase
- ALB:
-
albumin
- ALP:
-
alkaline phosphatase
- AST:
-
aspartate aminotransferase
- BMI:
-
body mass index
- BUN:
-
blood urea nitrogen
- CHB:
-
chronic hepatitis B
- CPT1:
-
carnitine palmitoyltransferase 1
- CR:
-
creatinine
- CVD:
-
cardiovascular diseases
- DBIL:
-
direct bilirubin
- eGFR:
-
estimated glomerular filtration rate
- EMR:
-
electronic medical record
- ETV:
-
entecavir
- FIB4:
-
fibrosis-4 index
- GGT:
-
gamma-glutamyl transferase
- HBsAg:
-
hepatitis B surface antigen
- HBV:
-
hepatitis B virus
- HBeAb:
-
hepatitis B envelope antibody
- HBeAg:
-
hepatitis B envelope antigen
- HCC:
-
hepatocellular carcinoma
- HDL:
-
high-density lipoprotein
- HIV:
-
human immunodeficiency virus
- HS:
-
hepatic steatosis
- IBIL:
-
indirect bilirubin
- LDL:
-
low-density lipoprotein
- LDL/HDL:
-
low-density lipoprotein to high-density lipoprotein ratio
- NAs:
-
nucleo(t)ide analogues
- NASH:
-
non-alcoholic steatohepatitis
- PPAR-α:
-
peroxisome proliferator-activated receptor alpha
- PSM:
-
propensity score matching
- TAF:
-
tenofovir alafenamide
- TC:
-
total cholesterol
- TC/HDL:
-
total cholesterol to high-density lipoprotein ratio
- TDF:
-
tenofovir disoproxil fumarate
- TG:
-
triglycerides
- TFV:
-
tenofovir
- WHO:
-
World Health Organization
References
World Health Organization. Global Hepatitis Report 2024: Action for Access in Low- and Middle-Income Countries (World Health Organization, 2024).
Global & national burden of hepatitis B. 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 7, 796–829 (2022).
Yim, H. J. et al. Comparison of clinical practice guidelines for the management of chronic hepatitis b: when to start, when to change, and when to stop. Clin. Mol. Hepatol. 26, 411–429 (2020).
Brunet, L. et al. Switch from Tenofovir Disoproxil Fumarate to Tenofovir Alafenamide in people living with HIV: lipid changes and statin underutilization. Clin. Drug Invest. 41, 955–965 (2021).
Kauppinen, K. J., Aho, I. & Sutinen, J. Switching from tenofovir alafenamide to tenofovir disoproxil fumarate improves lipid profile and protects from weight gain. Aids. 36, 1337–1344 (2022).
Kauppinen, K. J., Kivelä, P. & Sutinen, J. Switching from Tenofovir Disoproxil Fumarate to Tenofovir Alafenamide significantly worsens the lipid Profile in a Real-World setting. AIDS Patient Care STDS. 33, 500–506 (2019).
Schafer, J. J. et al. Changes in body Mass Index and atherosclerotic disease risk score after switching from Tenofovir Disoproxil Fumarate to Tenofovir Alafenamide. Open. Forum Infect. Di. 6, ofz414 (2019).
Milinkovic, A., Berger, F., Arenas-Pinto, A. & Mauss, S. Reversible effect on lipids by switching from tenofovir disoproxil fumarate to tenofovir alafenamide and back. AIDS. 33, 2387–2391 (2019).
Agarwal, K. et al. 96 weeks treatment of tenofovir alafenamide vs. tenofovir disoproxil fumarate for hepatitis B virus infection. J. Hepatol. 68, 672–681 (2018).
Cheng, P. N. et al. Body weight increase and metabolic derangements after tenofovir disoproxil fumarate switch to tenofovir alafenamide in patients with chronic hepatitis B. Aliment. Pharm. Ther. https://doi.org/10.1111/apt.17765 (2023).
Eg, H., Ea, J., Jj, Y., Sg, K. & Ys, K. Risk of dyslipidemia in chronic hepatitis B patients taking tenofovir alafenamide: a systematic review and meta-analysis. Hep. Intl. 17, (2023).
Rm, L. et al. Tenofovir alafenamide significantly increased serum lipid levels compared with entecavir therapy in chronic hepatitis B virus patients. World J. Hepatol. 15, (2023).
Peng, W. T. et al. Tenofovir amibufenamide vs tenofovir alafenamide for treating chronic hepatitis B: a real-world study. World J. Gastroentero. 29, 5907–5918 (2023).
Sun, T. et al. Predictive value of LDL/HDL ratio in coronary atherosclerotic heart disease. Bmc Cardiovasc. Disor. 22, 273 (2022).
Chinese Society of Hepatology, Chinese Medical Association & Chinese Society of Infectious Diseases, Chinese Medical Association. [Guidelines for the prevention and treatment of chronic hepatitis B (version 2022)]. Zhonghua Gan Zang Bing Za Zhi. 30, 1309–1331 (2022).
Jeong, S., Shin, H. P. & Kim, H. I. Real-world single-center comparison of the Safety and Efficacy of Entecavir, Tenofovir Disoproxil Fumarate, and Tenofovir Alafenamide in patients with chronic Hepatitis B. Intervirology. 65, 94–103 (2022).
K, S. et al. Effect of switching from tenofovir disoproxil fumarate to tenofovir alafenamide on lipid profiles in patients with hepatitis B. PloS One 17, (2022).
Zhang, Y. et al. Changes in blood lipids in patients with chronic hepatitis B after 48 weeks of tenofovir alafenamide treatment: a prospective real-world clinical study. Antivir Ther. 27, 13596535221082399 (2022).
Yeh, M. L. et al. Body weight changes in treated hepatitis B patients switching to tenofovir alafenamide. J. Formos. Med. Assoc. 121, 1273–1282 (2022).
Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
Baigent, C. et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 366, 1267–1278 (2005).
Lemieux, I. et al. Total Cholesterol/HDL Cholesterol Ratio vs LDL Cholesterol/HDL Cholesterol Ratio as indices of ischemic heart Disease Risk in men: the Quebec Cardiovascular Study. Arch. Intern. Med. 161, 2685–2692 (2001).
Calling, S., Johansson, S. E., Wolff, M., Sundquist, J. & Sundquist, K. The ratio of total cholesterol to high density lipoprotein cholesterol and myocardial infarction in women’s health in the Lund area (WHILA): a 17-year follow-up cohort study. Bmc Cardiovasc. Disor. 19, 239 (2019).
Chan, H. L. Y. et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate for the treatment of HBeAg-positive chronic hepatitis B virus infection: a randomised, double-blind, phase 3, non-inferiority trial. Lancet Gastroenterol. Hepatol. 1, 185–195 (2016).
Buti, M. et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate for the treatment of patients with HBeAg-negative chronic hepatitis B virus infection: a randomised, double-blind, phase 3, non-inferiority trial. Lancet Gastroenterol. Hepatol. 1, 196–206 (2016).
J, L. et al. Efficacy and safety of tenofovir alafenamide versus tenofovir disoproxil fumarate in treatment-naïve chronic hepatitis B. Liver Int. 42, (2022).
Young-Suk Lim. Long-term Safety Profile of Tenofovir Alafenamide in Chronic Hepatitis B patients: final 8-Year results of 2 phase 3 studies. (2023). https://www.natap.org/2023/EASL/EASL_117.htm
Zheng, Q. et al. Systematic review with meta-analysis: prevalence of hepatic steatosis, fibrosis and associated factors in chronic hepatitis B. Aliment. Pharm. Ther. 54, 1100–1109 (2021).
Huang, S. C. & Liu, C. J. Chronic hepatitis B with concurrent metabolic dysfunction-associated fatty liver disease: challenges and perspectives. Clin. Mol. Hepatol. 29, 320–331 (2023).
Choi, H. S. J. et al. Nonalcoholic steatohepatitis is Associated with Liver-related outcomes and all-cause Mortality in Chronic Hepatitis B. Hepatology. 71, 539–548 (2020).
Chan, A. W. H. et al. Concurrent fatty liver increases risk of hepatocellular carcinoma among patients with chronic hepatitis B. J. Gastroen Hepatol. 32, 667–676 (2017).
Kazuharu, S. Tenofovir-disoproxil-fumarate modulates lipid metabolism via hepatic CD36/PPAR-alpha activation in hepatitis B virus infection. J. Gastroenterol. https://doi.org/10.1007/s00535-020-01750-3 (2021).
Aloy, B. et al. Is Tenofovir Alafenamide Safer than Tenofovir Disoproxil Fumarate for the kidneys? AIDS Rev. 18, 184–192 (2016).
Xu, J. et al. Hepatic carboxylesterase 1 is essential for both normal and farnesoid X receptor-controlled lipid homeostasis. Hepatology. 59, 1761–1771 (2014).
Quiroga, A. D. et al. Deficiency of carboxylesterase 1/esterase-x results in obesity, hepatic steatosis, and hyperlipidemia. Hepatology. 56, 2188–2198 (2012).
Jeong, J., Shin, J. W., Jung, S. W., Park, E. J. & Park, N. H. Tenofovir alafenamide treatment may not worsen the lipid profile of chronic hepatitis B patients: a propensity score-matched analysis. Clin. Mol. Hepatol. 28, 254–264 (2022).
Bosch, J., Gracia-Sancho, J. & Abraldes, J. G. Cirrhosis as new indication for statins. Gut. 69, 953–962 (2020).
Funding
This study was supported by Science Foundation of the Fujian Province (No.2021J010289; No.2023J011473).
Author information
Authors and Affiliations
Contributions
HB Gao, DF Huang and ML Lin designed the study; SL Lin and WL Huang performed the analyses and wrote the manuscript jointly; ZY Liao screened and validated the data; HX Ma and WJ Wu collected the data; HB Gao and DF Huang reviewed the final data; SL Lin and WL Huang contributed equally to this study and should be considered as the co-first authors. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lin, S., Huang, W., Liao, Z. et al. Comparison of lipid profile alterations in chronic hepatitis b patients receiving tenofovir alafenamide or tenofovir disoproxil fumarate. Sci Rep 14, 27369 (2024). https://doi.org/10.1038/s41598-024-78656-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-78656-0