Abstract
The present preliminary study aimed to provide a targeted lipidomic analysis of Hashimoto (HT) and non-HT patients with well-controlled hypothyroidism as well as in healthy adults, and is the first to demonstrate the association of several components of the human lipidome with hypothyroidism in relation to the total plasma selenium content. All the patients and age-, sex-, and BMI-matched healthy controls met the very strict qualification criteria. Se levels were analyzed by ICP-MS, and lipidome studies were conducted using TQ-LC/MS. The 40 acylcarnitines, 90 glycerophospholipids, and 15 sphingomyelins were identified and quantified. PCaaC26:0 and PCaaC40:1 were negatively correlated with Se concentrations. Other lipids that were negatively correlated with Se concentrations but did not present significant differences between the three groups in the Kruskal–Wallis ANOVA test were PCaaC32:0, PCaeC30:0, PCaeC36:5, SMC18:0, and SM C18:1. In the multiple linear regression analyses, Se levels showed negative relationship, whereas different phosphatidylcholines: PCaaC24:0, PCaaC26:0, PCaeC30:1, PCaeC34:0, PCaeC36:4, PCaeC42:0 were positively associated with the presence of (H). Different lipidome components were identified in healthy and hypothyroid patients regardless of the cause of that condition. Studies on larger populations are needed to determine cause-and-effect relations and the potential mechanisms underlying these associations.
Similar content being viewed by others
Introduction
Lipids are diverse and multifunctional molecules integral to cellular structure, signaling, and function. Studying lipid species in biological samples, including human body fluids or tissues, provides valuable insights into biology, physiology, disease mechanisms, and potential ways for therapeutic intervention. Research on human lipidome, i.e., the total lipid content within a cell, organ, or biological system, can be used in risk assessment model development, disease diagnosis, and its monitoring1. Understanding how lipids function and how to control their activity also offers the potential to develop novel treatments for controlling numerous diseases. The involvement of lipids in metabolic pathways and their role in the pathology of diseases related to the endocrine system is increasingly understood2. Hormones modulate every pathway in lipoprotein metabolism, influence the expression of lipoprotein receptors, the production of apolipoproteins, the activity of plasma lipoprotein-modifying enzymes, and the blood concentrations of substrates for triglycerides (TGs) synthesis, such as fatty acids and glucose. Therefore, it is anticipated that endocrine disruption, including hypothyroidism, alters the lipid profile3. Hypothyroidism is a common endocrine disorder resulting from a deficiency of thyroid hormones (TH). Worldwide, iodine deficiency is the most common cause of hypothyroidism; however, in Poland and other areas of adequate iodine intake, chronic autoimmune thyroiditis—the Hashimoto’s disease also known as the Hashimoto thyroiditis is the primary reason for hypothyroidism4,5.
Although it has been suggested that overt hypothyroidism results in elevated levels of low-density lipoprotein (LDL)- cholesterol, high-density lipoprotein (HDL)- cholesterol, and triglycerides (TGs) in serum6, the relationship between subclinical hypothyroidism (SCH) and blood lipid metabolism remains controversial, and the definite association between SCH and routinely measured blood lipid levels such as TC (total cholesterol), LDL-C, and HDL-C has not been confirmed7. In contrary, another study revealed that the total cholesterol level in SCH was positively correlated with the level of TSH8.
Recently, several studies have shown that thyroid hormones can affect incident dyslipidemia in a general euthyroid population9,10. Low but normal FT3 was associated with high dyslipidemia risk, especially for elevated TC and LDL-C, and normal TSH had a weak positive effect on the incidence of reduced HDL-C9. In another study, positive and significant relationships between TSH level and TG level as well as between FT4 level and TC, LDL-C, and HDL-C cholesterol levels were demonstrated10. Since levothyroxine (LT4) replacement therapy reduces levels of TSH, it is well known that the treatment could also reduce TC and LDL-C in hypothyroidic patients, including those with mild SCH11,12.
The current standard of care for hypothyroidism is levothyroxine (LT4) monotherapy to reduce levels of TSH within its reference range. Once a patient’s thyroid hormones are in the normal range, the Endocrine Society clinical practice guideline being the first to focus on lipid management in patients with endocrine disorders, recommends re-evaluating the lipid profile12. Since thyroid hormones modulate a number of pathways involved in lipid metabolism, it is doubtful whether a basic blood lipid profile assessment in hypothyroidic patients with biochemical euthyroidism (i.e. thyroid hormones and TSH within the normal range) brings adequate information on the complexity of lipids activity and turnover. Using a modern lipidomic approach, we intended to find out to what extent and which specific lipid molecules differ quantitatively in healthy and hypothyroid adults with biochemical euthyroidism and without any comorbidities. To the best of our knowledge, human lipidome alterations have not been studied in such patients with well-controlled hypothyroidism (i.e. stable TSH levels within the normal range on the appropriate dose of LT4 replacement therapy).
Furthermore, other factors may mediate the interplay between the action of thyroid hormones and lipid compounds, considering that thyroid hormones play an important role in maintaining energy homeostasis in the body. The essential trace element selenium (Se) is known to influence such a balance13. There are many reports on the disruption of the physiological levels of Se in the body that adversely affect the functioning of cells and tissues, which can lead to the development of hypothyroidism14. Selenium is required for the antioxidant function and the metabolism of thyroid hormones, and its intake has been associated with autoimmune disorders15. Duntas et al.16 investigated the effect of selenium treatment in the form of selenomethionine in patients with autoimmune thyroiditis by affecting the levels of TPOAb and TgAb after 3 and 6 months. In the supplement group TPOAb levels decreased by 46% after 3 months and by 46% after 6 months compared to a decrease of only 21% and 27%, respectively, at 3 and 6 months in the group treated with thyroxine. Nevertheless, there was no statistically significant statistically significant difference in TPOAb levels or in the levels of TSH, free T4 and T3 between the two groups. There were no significant changes of antibodies against thyroglobulin levels between these groups. In turn, another randomized double-blind placebo-controlled trial investigating whether adding selenium to standard LT4 treatment in Hashimoto’s thyroid patients can lead to improved quality of life and reduced autoimmune disease activity did not justify the routine use of selenium supplementation in patients with Hashimoto’s disease, as selenium supplementation for 12 months, compared to placebo, did not improve patients’ quality of life, LT4 dose or FT3I / FT4 ratio17. Despite some inconsistencies presented in the literature regarding either low or high Se status in hypothyroid patients, there is clear evidence of a close relationship between this element and thyroid health and function18,19. Recently, integrated analysis of miRNAs and the proteome in SCH mice highlighted an interesting associations between some miRNAs and proteins, including selenium-binding protein 2, which contributes to a better understanding of lipid metabolism disorders in subclinical hypothyroidism20. Although there are some data indicating that no strong correlation exists between serum selenium levels and lipid profile in humans without any pathology of the thyroid gland21, the associations between Se in plasma and the plasma lipidome in patients with hypothyroidism remain unknown.
Our cohort study aimed to reveal which lipid species are altered in hypothyroidic patients with biochemical euthyroidism who present normal serum lipid profiles (LDL-cholesterol, HDL-cholesterol, total cholesterol, and triglycerides). Furthermore, we intended to investigate whether selenium levels in these patients are associated with the content of individual lipid molecules and whether the possible Se-lipidome association is modified by thyroid status. This may provide a theoretical basis for the better understanding and control of thyroid dysfunctions and related lipid imbalances, as well as it may help to reveal more about human metabolism.
Methods
Patients and control group
The cross-sectional cohort study was initiated in 2021. The study protocol received ethical approval from the Medical University of Lublin Bioethics Committee (KE-0254/7/2021). Informed consent was obtained in writing from each participant. The study was conducted in accordance with the principles of the Declaration of Helsinki. The patients included in the study had a diagnosis of either Hashimoto’s disease or non-autoimmune hypothyroidism (Hypo-non-Hashimoto), according to endocrinological assessment. This study investigated plasma lipidome in 24 HT patients with autoimmune hypothyroidism, 11 non-HT patients with hypothyroidism without autoimmune thyroiditis, and 6 age-, sex-, and body mass index (BMI)-matched healthy controls. Subjects were recruited from a specialized thyroid outpatient unit with higher frequencies of thyroid disorders than in the general population. The control group consisted of individuals with normal thyroid function. Thyroid-stimulating hormone (TSH), free T4 (fT4), free T3 (fT3), serum lipid profile, fasting glucose, and fasting insulin were measured. Thyroid peroxidase antibody (TPOAb) and antithyroglobulin antibody (TgAb) were assessed to confirm autoimmune thyroiditis in patients with Hashimoto’s disease.
Patients with either Hashimoto’s disease or non-autoimmune hypothyroidism were receiving thyroid hormone replacement therapy with levothyroxine (LT4) in tablets (doses of LT4 are shown in Tables 1 and 2).
The doses of levothyroxine were carefully selected (based on information such as patients’ weight, age, and other medical conditions) to maintain euthyreosis in hypothyroidic patients. There were no differences in the euthyroidic levels of TSH, fT4, and fT3 between both the hypothyroidic groups and the healthy control—see the results section.
The study participants were not receiving any other medical treatment. All members of the control and study groups were from the same geographic area (central and south-eastern Poland). Neither the control nor the two groups with hypothyroidism presented any pathologies (except the hypofunction of the thyroid gland), and they had taken no mineral or vitamin supplements for at least 3 months before the samples for analysis were collected.
They were not on any special diets during the tests. Other exclusion criteria included the presence of a chronic condition (particularly affecting the function of the thyroid gland or weight or limiting the patient’s ability to participate in the study), use of lipid-altering drugs, and refusal to give informed consent.
Collection of the samples
Fasting blood specimens for lipidomic studies were collected from the patients and control groups into commercially available sterile anticoagulant-treated tubes, e.g., EDTA-treated (VACUETTE® K2E K2EDTA). For Se measurements blood plasma was obtained by centrifuging heparinized whole blood (VACUETTE® TUBE NH Trace Elements Sodium Heparin (Greiner-Bio-One, Austria). All blood samples were separated for plasma immediately after collection and stored in − 80 °C freezers until laboratory analyses. Serum was used for routine diagnostic measurements (such as cholesterol, insulin, and thyroid hormones). Serum was collected in non-anticoagulant sterile tubes with a serum separator.
Serum levels of TC and TG were determined using enzymatic methods, and HDL-C was measured by immunoassay. The Friedewald formula using determined TC, HDL-C, and TG levels and the adopted TG-to-VLDL-C ratio was used to calculate the LDL-C level (LDL-C = TC – HDL-C – TG/5 (mg/dl))22.
Targeted metabolomic analysis (TMA)
We applied TMA because such an analytical approach has better sensitivity and quantitative abilities than untargeted approaches where the metabolic, including lipid species of interest, are not predefined23. The quantifications of 145 lipids (such as 40 acylcarnitines, 90 glycerophospholipids, and 15 sphingomyelins) were undertaken. AbsoluteIDQ p180 kit (Biocrates Life Sciences AG, Innsbruck, Austria) analyzed metabolites. Sample preparation was performed following the manufacturer’s protocol. Briefly, 10 µl of plasma was pipetted onto the filter plate of the kit. Subsequently, 10 µl internal standards were added, and the plate was dried under a nitrogen stream. The samples were derivatized using phenylisothiocyanate and again dried under a nitrogen stream. Metabolites were extracted using 5 mm ammonium acetate in methanol and further diluted for LC–MS and FIA-MS experiments. Analyses were performed on an Agilent Infinity II 1290 HPLC coupled to an Agilent triple quadrupole mass spectrometer 6470 TQ LC/MS (Agilent Technologies, Santa Clara, CA, USA). Acquisition methods were set as provided by Absolute Biocrates for the p180 kit. Data acquisition was performed by Mass Hunter Acquisition B.10.0 (Agilent Technologies, Santa Clara, CA, USA). Data analysis was performed using MetIDQ (Biocrates, Innsbruck, Austria) and Mass Hunter Quantitative (Agilent Technologies, Santa Clara, CA, USA).
Determination of se in plasma by inductively coupled plasma mass spectrometry (ICP-MS)
The plasma samples were dissolved with the acidic treatment in the microwave-assisted digestion system Ethos Up—Advanced Microwave Digestion Labstation (Milestone Srl, Italy) with user-selectable output power (0–1800W with 1W increment). Microwave-assisted acid digestion of samples was performed using a polypropylene rotor equipped with high-pressure Teflon vessels. The samples after the thawing were homogenized by sonification (15 min) and vortexing (30 s). Next, the plasma samples underwent microwave mineralization with 3.5 mL of 65% HNO3 Suprapur® grade and 1.5 mL of deionized water (DI water, conductivity < 0.08 µS/cm, HLP10 system, Hydrolab, Poland). The samples were dissolved with (DI) water up to a final volume of 7 mL. Solutions were stored at 4 °C prior to ICP-MS measurements.
The selenium standard solution was made from an individual standard (1.000 mg/L, TraceCERT®, Switzerland), and the calibration curves were prepared within range in the range of 0.2–50 µg/L. All solutions were prepared in freshly rinsed vials (with 1:1 nitric acid and deionized water (DI) at least three times). After microwave digestion, the plasma samples were diluted in the solution of 6% HNO3 in deionized water to reduce non-spectral interferences.
The total contents of Se in the plasma samples were measured by XSeries 2 ICP-MS (Thermo Fisher Scientific, Bremen, Germany) with PlasmaLab software, equipped with a collision/reaction cell operated using 7% H2 in He mixture gas (Linde Gaz Polska, Poland), used in conjunction with an ASX-510 autosampler (CETAC, Omaha, Nebraska, USA). The advantage of using ICP-MS is that it detects both organic and inorganic forms of Se in samples. Each sample was analyzed in triplicate, and the FullQuant analysis method was used to quantify the data. The linearity of the calibration curves was evaluated by the respective correlation coefficients (r2) = 0.9999; the LOD of the method was based on a 3 × standard deviation of 100 analytical blanks. To validate the method, the certified reference materials were used. We used both non-matrix matched CRMs – EP-H-2 (EnviroMAT Drinking Water), and EU-H-3 (EnviroMAT Waste Water) (SCP Science, Quebec, ON, Canada), as well as Seronorm™ Serum Seronorm Trace Elements serum L2 (Sero, Billingstad, Norway), where the concentration of Se was within the control range specified by the manufacturer (120–157 µg/L). Recoveries were in the range of 95.00–104.17% (Supplementary Table S1).
Statistical analysis
Descriptive statistics were stratified by the presence of hypothyroidism. As the Kolmogorov–Smirnov and Lilliefors tests indicated that the variables were not normally distributed, the nonparametric Kruskal–Wallis ANOVA test was used for continuous variables. A multiple linear regression analysis was used to evaluate the association between the presence of hypothyroidism and plasma selenium levels as well as lipid species. All analyses were two-tailed, with a significance level of 0.05 and a power of 80%. Statistical analyses were performed using TIBCO Software Inc. (2017) Statistica, version 13.0.0.0 (TIBCO, Tulsa, OK, USA), licensed to the Medical University of Lublin.
Results
A detailed characterization of the patients with Hashimoto’s disease or non-autoimmune hypothyroidism (Hypo-non-Hashimoto), as well as control, is presented in Tables 1, 2, and 3, respectively. As the variables were not normally distributed and nonparametric median tests were used to compare samples, the mean and standard deviation values are presented only to completely characterize the study groups. All the groups were age-, sex-, and BMI-matched. There were no significant differences in TSH or free thyroid hormone (fT4 and fT3) levels between the two hypothyroid groups (which included patients adequately treated with levothyroxine to maintain euthyreosis) and the healthy control. Furthermore, there were no significant differences in lipid profile, including total cholesterol (p = 0.13), LDL-cholesterol (p = 0.94), HDL-cholesterol (p = 0.09), and triglycerides (p = 0.16), as well as fasting glucose (p = 0.23), fasting insulin (p = 0.79), and HOMA-IR (p = 0.87) values between the Hashimoto’s disease group, non-autoimmune hypothyroidism (Hypo-non-Hashimoto) group and the healthy control (data not shown graphically).
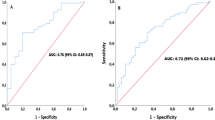
There were significant differences in selenium plasma levels between all hypothyroid patients (lower levels) and control (p = 0.005). However, there were no differences in selenium plasma levels between the two groups of patients with hypothyroidism (multiple comparisons of mean ranks are available in Fig. 1 and Table 4).
Interestingly, lysoPC a C20:3 was lower (p = 0.04) in the Hypo-non-Hashimoto group than in the Hashimoto’s disease group and the control group (CG). PC aa C26:0 (p = 0.002), PC ae C30:1 (p = 0.025), PC ae C34:0 (p = 0.03), as well as PC aa C24:0 (p = 0.04), were higher in the group with Hashimoto’s disease than in the CG. There were no significant differences in the two hypothyroid groups for these lipids. PC aa C40:1 (p = 0.0004), as well as PC ae C42:0 (p = 0.0006), were higher in all hypothyroid patients in comparison to CG, and PC ae C36:4 was higher (p = 0.02) in the group with the Hashimoto’s disease than in the group Hypo-non-Hashimoto, but not in CG, as it is seen in Fig. 1 and Table 4.
All values, both significant and not significant regarding the multiple comparison p values (two-sided) of plasma selenium levels and selected lipid species in the three groups are presented in supplementary Table S2.
As it is seen in Table 5, PC aa C26:0 and PC aa C40:1 were negatively correlated with plasma selenium concentrations. These lipid species also presented significant differences in the Kruskal–Wallis ANOVA test (see above). Other lipids that were negatively correlated with plasma selenium concentrations but did not present any significant differences between the three groups in the Kruskal–Wallis ANOVA test were PC aa C32:0, PC ae C30:0, PC ae C36:5, SM C18:0, and SM C18:1.
In the multiple linear regression analyses (Table 6), plasma selenium levels showed a negative relationship with the presence of hypothyroidism. PC aa C24:0, PC aa C26:0, PC ae C30:1, PC ae C34:0, PC ae C36:4, PC ae C42:0 were positively associated with the presence of hypothyroidism.
Discussion
It is known that a wide range of hormones regulate lipid metabolism simultaneously in a time-specific manner. Thyroid hormones regulate and affect both cholesterol and fatty acid metabolism. They stimulate fatty acid synthesis (lipogenesis), triglyceride breakdown (lipolysis), fatty acid oxidation, cholesterol synthesis, and low-density lipoprotein (LDL) receptors. Genes involved in lipogenesis in the liver and positively regulated by HT include fatty acid synthase (FAS), acetyl-CoA carboxylase (ACC), spot14 protein, and malate enzyme (ME) genes. Fatty acid oxidation-related genes positively regulated by HT include carnitine acyltransferase (CPT), acyl-CoA translocase (TAC), and long-chain fatty acid oxidase (AOX) genes. Cholesterol synthesis is influenced by T3 by stimulating the expression of the hydroxymethylglutaryl-CoA reductase (RHMG) gene and the activity of this enzyme. Inhibition by T3 of the expression of cholesterol 7α-hydroxylase (CYP7A1) contributes to the reduction of bile acid synthesis24. Very recently, Zhang et al.25 provided new insight into hormones regulating lipid metabolism and highlighted the role of thyroid hormone receptors (THR) in lipid metabolism. Although the effect of THRs and subsequent pathways in lipid metabolism is still under investigation, this research, citing animal studies, emphasizes that THs not only directly regulate lipogenic gene expression but also affect the activity of other transcription factors, such as sterol regulatory element binding protein-1c (SREBP1c) and carbohydrate-responsive element-binding protein (ChREBP), indirectly influencing hepatic lipogenesis26. THs promote the lipolysis of white adipose tissue, which is a source of circulating free fatty acids (FFAs), induces the protein transporter expression such as fatty acid transporter proteins (FATPs), liver fatty acid-binding proteins (L-FABPs) and fatty acid translocase27.
Thyroid hormones, such as thyroxine (T4) and triiodothyronine (T3), exert their effects by binding to specific nuclear receptors, which then modulate gene expression24. Proper membrane structure is essential for the function and localization of these receptors. Its integrity and fluidity are precisely ensured by, for example, glycerophospholipids28. The membrane of thyrocytes contains thyroid peroxidase (TPO), an enzyme involved in the synthesis of thyroid hormones, and proteins involved in the processes of iodine uptake, incorporation of this element into thyroglobulin, as well as the release of thyroid hormones into the bloodstream and their transport29. In addition, glycerophospholipids may play a role in immune system recognition and response, so changes in membrane composition could potentially affect antigen presentation and immune responses, contributing to the development of autoimmune diseases such as Hashimoto’s30.
The imbalance between free radical production and antioxidant defense, is associated with damage to a wide range of molecular species, including lipids, proteins and nucleic acids31. Oxidative damage affecting glycerophospholipids, among others, leads to lipid peroxidation and the release of inflammatory molecules, exacerbating thyroid dysfunction30. Lipid peroxidation occurs when a hydroxyl radical strips an electron from an unsaturated fatty acid. The unstable lipid radical that forms can then react with oxygen to form a fatty acid peroxyl radical can react with another unsaturated fatty acid. As a result, the generated fatty acid hydroperoxide and new lipid radical promote damage to cell membranes32. Free radicals play a very important role in the functioning and regulation of the immune system33. They intensify the activation of T lymphocytes and cause leukocyte cells to fuse with the endothelium, allowing them to move from the circulatory system to the site of the inflammatory response. Reactive oxygen species are signaling molecules, in their action very similar to hormone messengers and hormones themselves34. Oxidative stress is implicated in multiple diseases, including diabetes, obesity, neurological diseases, cardiovascular disease and cancer35.
Research on oxidative stress indicates associations of thyroid diseases, including thyroid gland tumors, as well as autoimmune thyroid disease36,37. Hashimoto’s thyroiditis is likely related to iodide-mediated oxidative stress and inflammation38. Thyroid disorders may initiate or increase ROS release and oxidative stress, enhancing oxidative damage, which appears to be involved in both the initiation and progression of carcinogenesis37.
With advances in analytical methodologies and techniques for determining compounds of indisputable relevance in health and disease states, such as lipids, there has been an increased interest in individual metabolites. Lipidomics, belonging to the field of metabolomics, may be used to investigate metabolic changes in various diseases39. Recent studies have shown an association between the results of lipidomic profiling and selected disease onset and progression40,41. Lipidomics involves complex lipidome analysis and is quite challenging due to the vast number of lipid species. Owing to their considerable structural diversity, lipids are important players in various complex physiological processes where they execute important functions, acting as cellular membrane components, signaling mediators, energy reserve molecules, and endocrine regulators42. It has been revealed that not only the main “clinical” lipids (TG, CHOLs) are useful during routine diagnostics and treatment, but there is also a great hope among scientists that analysis of the human lipidome will help in detecting and monitoring an increasing number of human diseases.
An essential advantage of lipidomics is the ability to identify specific plasma lipid abnormalities, e.g., changes in molecular species containing particular-chain-length fatty acids. The specific molecular changes would remain undetected if one were using the enzymatic lipid assays that are routinely applied in clinical laboratories to determine total lipid (TL) content in serum. In our study, the following lipid classes: acylcarnitines (more specifically, a plasma acylcarnitine profile can aid in the diagnosis of organic acidemias in addition to fatty acid oxidation disorders), glycerophospholipids (structural components of biological membranes, important constituents of lipoproteins, performing functions in other cellular processes such as signal induction and transport), and sphingomyelins (having significant structural and functional roles in the cell, as plasma membrane components and as participants in many signaling pathways) were identified and quantified. Our results suggest that among almost two hundred metabolites, which we could quantify using targeted metabolomics analysis, only a few correlated with hypothyroidism and Hashimoto disease (see Tables 4, 5, and 6).
Although glycerophospholipids are known to dominate cell membranes, providing stability, fluidity and permeability, are required for the proper function of membrane proteins, receptors and ion channels, and act as reservoirs of second messengers and their precursors, not all species of this broad class of lipids are well understood in the context of interactions with thyroid hormones. The different combinations of glycerophospholipid head groups and fatty acyl chains give rise to thousands of molecular species43. Among them are glycerophospholipids such as PC ae C30:1, PC ae C36:5, and PC ae C42:0. According to our best knowledge, no studies describe a significant association of these molecules in any disease. Due to the complexity of metabolism and insufficient research, there is a lack of thorough information on the function of these specific lipids in the human body. There is no conclusive data that glycerophospholipids have a direct effect on the onset and development of thyroid diseases, such as hypothyroidism or Hashimoto’s, which are complex and often multifactorial, involving factors such as genetics, immune responses, hormonal imbalances, and also environmental factors44,45.
Although PC ae C34:0 has not been previously linked to hypothyroidism or Hashimoto’s, this lipid has been linked to other diseases. PC ae C34:0 levels have been characterized in three papers on Alzheimer’s disease (AD), colorectal cancer (CRC), and VZV (chickenpox and hemiplegia virus) meningitis. In a study performed by Huo et al.46 concerning Alzheimer’s disease, elevated serum levels of this lipid measured prior to diagnosis (AD) predicted a faster decline in global cognition and three cognitive domains (episodic memory, perceptual speed, semantic memory). At the same time, it showed protective effects on neuropathology in brain tissue samples. It is also suggested that this lipid may be a predictor of high risk of colorectal cancer recurrence in the next 6 months after hepatectomy47.
Furthermore, PC ae C34:0 can be considered as a biomarker in the diagnosis of meningitis resulting from VZV since, in addition to the other lipids mentioned, its concentration characterized inflammation and pathological processes in parenchymal cells of the central nervous system, without a clear effect on the number of leukocytes in the cerebrospinal fluid48. PC ae C36: 4 was characterized in the study on determining metabolic changes after metformin use to treat type 2 diabetes mellitus (T2DM)49. A significant decrease in phosphatidylcholine PC ae C36:4 was demonstrated not with the first dose of this drug but with its prolonged use in the 4–6 weeks range. PC aa C36:4 was also demonstrated to be positively associated with BMI50.
Interestingly, in our study the analyses of the association between the presence of hypothyroidism and plasma selenium levels as well as selected lipid species revealed significant values for phosphatidylcholines (PCs) which are among the major constituents of cell membranes and represent important components of lipoproteins51. Out of 145 different lipid molecules analyzed qualitatively by TLA in the present study for only six PCs, i.e. PC aa C24:0, PC aa C26:0, PC ae C30:1, PC ae C34:0, PC ae C36:4, PC ae C42:0 (aa indicating two acyl-bound and ae indicating one acyl- and one alkyl-bound fatty acids) the mentioned significant associations were found.
Most research on sphingomyelin (SM) has focused on its role in cell membrane structure, myelin sheath formation, neurological functions, and various cell signaling pathways52,53,54,55. Although sphingolipids, including sphingomyelins, are known to be involved in cell signaling and membrane functions, their specific involvement in thyroid diseases, such as hypothyroidism or Hashimoto’s thyroiditis, has not been thoroughly studied or established. Sphingolipids, like glycerophospholipids, are major components of cell membranes, contributing to their structural integrity and fluidity. They are particularly abundant in the outer layer of the plasma membrane, where they help form lipid rafts—microdomains that play a role in signaling, protein transport, and membrane organization. They participate in intracellular membrane transport and vesicle formation during endocytosis, exocytosis, and vesicular transport. Sphingolipids are involved in various signaling pathways that regulate cell growth, differentiation, survival, and apoptosis (programmed cell death). They can modulate immune responses by affecting immune cell activity and cytokine secretion56. Both the de novo synthesis of sphingolipids and the sphingomyelinase pathway are important in the pathogenesis of some auto-immune disorders, e.g., autoimmune encephalomyelitis57 or arthritis58.
SMs are major components of cell membranes, particularly abundant in the outer layer of the plasma membrane. Along with cholesterol, SMs contribute to membrane stability, fluidity, and lipid raft formation. This interaction is vital for maintaining the proper balance between rigidity and elasticity of cell membranes. It is also a key component of myelin sheaths in neurons. Contributing to the insulation and integrity of nerve fibers, it enables efficient transmission of nerve signals. Sphingomyelin can act as a reservoir of enzymes involved in sphingolipid metabolism, such as sphingomyelinases. As a result of their action, bioactive lipid molecules can be formed, including ceramides, which are involved in cell signaling59. Disruption of sphingomyelin metabolism is associated with various diseases, including Niemann-Pick disease, lysosomal storage disorder, and arteriosclerosis, in which the accumulation of sphingomyelin in blood vessels can contribute to the formation of atherosclerotic plaques60,61.
Research revealed a significant association of C18:1 sphingomyelin (SM) with multisite musculoskeletal pain (MSMP)62 with alcohol use and smoking63, liver cirrhosis64, and also in association with other sphingomyelins, contribute to T2D through effects on BMI50. Elevated levels of SM C18 have been reported as a probable predictor of Alzheimer’s disease65, diagnosis of insulin-related disorders, and especially type 1 diabetes mellitus (T1DM) and latent autoimmune diabetes in adults (LADA)66. In addition, increased levels of this sphingomyelin were detected in a study group with endocrine hypertension (EHT)67, hyperglycemic patients were more likely to develop chronic kidney disease (CKD)68, and in patients with polycystic ovary syndrome (PCOS)69. Significantly reduced levels of SM C18:1 were reported in studies70 concerning only peritoneal fluid samples from patients diagnosed with endometriosis.
To the best of our knowledge, the present study is the first to demonstrate the possible association of several components of the human lipidome with hypothyroidism. Our finding is significant as it may provide a basis for further investigation to clarify the role of selected lipid molecules in hypothyroidism.
In our current study, we were interested in whether Se, a micronutrient whose excess is just as problematic as deficiency, may be associated with particular lipid species linked to hypothyroidism. The relationship between hypothyroidism and selenium levels is complex and bidirectional—hypothyroidism is associated with an increased risk of selenium deficiency. In contrast, selenium deficiency can exacerbate thyroid dysfunction because selenium is required to convert the inactive thyroid hormone T4 (thyroxine) into the active form T3 (triiodothyronine). Without sufficient selenium, this conversion process may be impaired, contributing to the symptoms of hypothyroidism. In individuals with hypothyroidism, the body’s metabolic rate is decreased, leading to reduced absorption of nutrients, including selenium, from the gastrointestinal tract—this can result in a feedback loop, further lowering selenium levels in the bloodstream. Selenium is thus regarded as one of the most potent antioxidants. The role of Se-containing selenoenzymes and selenoproteins is to speed up the oxidation reaction of proteins scavenging reactive oxygen species. Se protects the body from oxidative stress, which can cause immune disorders, cardiovascular disease, and cancer. Selenium deficiencies can lead to a significant weakening of the immune response. This is due to, among other things, a decrease in the activity of T lymphocytes, macrophages, and NK cells. Studies indicate that selenium supplementation causes a decrease in anti-thyroid peroxidase antibodies (anti-TPO) and also an increase in the ratio between FT3 and FT4 (selenium is an important component of the enzyme that converts thyroxine T4 into triiodothyronine T3)71. Khorasani et al.71 investigated Se status in patients categorized into two groups depending on the type of diagnosis, i.e., hypothyroidism and autoimmune thyroiditis, and found significant differences in serum concentrations of Se between hypothyroid patients (with a lower concentration of Se) and controls. However, no relationship was found between the type of thyroid disease and a pronounced selenium deficiency. The findings of Stojsavljević et al.72 indicated apparent differences in Se profiles between hypothyroidism and healthy subjects. However, in contrast to studies of Khorasani et al.71 significantly higher concentrations of selenium in the group of respondents suffering from hypothyroidism compared with healthy subjects were found.
Studies on the relationship between body selenium levels and hyperlidpidemia emphasize the role of oxidative stress and the inflammatory response73. This is not the only possible pathway, as selenium may interact with other elements and this may cause dyslipidaemia by encouraging the release of lipids from the liver and adipose tissues, resulting in decreased activity of antioxidant enzymes such as superoxide dismutase and catalase, increased lipid peroxide levels in the liver and kidneys and markers of abnormal liver function. Oxidation of cell membranes can potentially cause hepatotoxic effects that affect liver function and reduce lipid production in hepatocytes74. Studies showed that selenium deficiency increases lipid peroxidation in the membranes, and clearly leads to the cell death. Research confirmed that the lipid hydroperoxides, play a causative role in the oxidative damage to cells induced by selenium deficiency75.
Recent animal studies revealed that selenium deficiency in diet may adversely influence the fatty acid profile (e.g., conversion of linolenic acid (ALA) to eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), resulting in the unbeneficial n-6/n-3 ratio in tissue lipids)76. A meta-analysis based on human studies that explored Se levels and the effect of Se supplementation on lipid profile (including total cholesterol (TC), triglyceride (TG), low-density lipoprotein (LDL), high-density lipoprotein (HDL), very low-density lipoprotein (VLDL)) measurements) suggested that the effect of selenium supplementation on the serum levels of TG and VLDL was marginally significant and that the effect of selenium supplementation on lipid profile was negative77. While it has been reported that Se may be associated with lipid levels, the available data seem to be conflicting78. Examining the relation of serum selenium concentrations with serum lipids in large, Se-replete men and women from the US revealed the association of Se and TC, LDL-C, HDL-C, TGs, apo B, and apo A-I. However, the cause-and-effect relations and the potential mechanisms underlying these associations remain unknown79. About two decades ago, a considerable number of Polish inhabitants had a relatively low concentration of Se in blood plasma—about 50–55 μg/l, and the calculated daily dietary intake was about 30–40 μg/day80. Selenium deficiency was diagnosed by measuring the serum or plasma selenium level, which should be at least 85 μg/L81. Recent studies on the Polish population report Se levels of approximately 79 μg/L in healthy adults82. Although various national and international guidelines often provide reference ranges, there is no specific data on Se levels in compensated (well-controlled) hypothyroidism in the Polish population of adults.
Strong and weak points of the study
The great advantage of our work is that we follow very strict criteria for qualifying patients for the research. It is rare in patients suffering from hypothyroidism for the lipid profile—usually routinely prescribed for patients (total cholesterol, LDL, HDL, TG)- for glucose and insulin levels to be within the accepted norms. The exclusion of the most common fluctuations in biochemical parameters and the well-controlled levels of thyroid hormones in the study group is the basis for suspecting that individual species of the lipidome are typical of hypothyroidism itself, perfectly compensated without comorbidities. Both studied, and the control groups were age- and BMI-matched. Moreover, there were no statistically significant differences in TC, LDL-C, HDL-C, TGs, glucose/insulin, and degree of insulin resistance. We ensured that all participants in the study were not taking any medication, and dietary supplements that could affect the lipid profile. The project participants came from the same geographical region and were on a similar diet.
We indicated that the hypothyroid group had lower levels of Se than the controls (the normal concentration in adult human blood serum is between 110 and 165 mcg/L). There is a lack of such current data on this specific human population. In the state of selenium deficiency associated with loss of glutathione peroxidase activity, the serum concentration is usually below 40 mcg/L83. We assessed selenium status by measuring plasma selenium, which responds to changes in intake. It is essential to note that while selenium plays a role in thyroid function, not everyone with hypothyroidism will have its deficiency, and the relationship between the two can vary from person to person. In our study, we eliminated the results of patients whose selenium levels would have indicated a severe deficiency.
The study’s weakness is the small sample size, especially the control group. During recruitment for the study, many volunteers had to be excluded due to the diagnosis of other diseases. It also turned out that it was challenging to select a group of people who would meet the rigorous qualification criteria for our project. The power of our study is relatively low. However, the data acquired here may be considered preliminary for broader research. Interactions with other nutrients, such as vitamins and some minerals, may also influence the effects of selenium on plasma lipids. We will examine this in the next stage of our project.
Completing our future studies with the identified limitations may contribute to a deeper understanding of the complex relationship between Se and lipids’ metabolism and its modification by various thyroid pathologies. Moreover, considering that the biological effects and bioavailability of Se may strongly depend on its chemical forms and their amounts in diet84,85, our research could be extended to investigate speciation forms of that element and their distribution in different tissues, as well as their response to varying dietary selenium content.
Conclusions
The present preliminary study is the first to demonstrate the association of several components of the human lipidome with hypothyroidism in relation to the total plasma selenium content. Different lipidome profiles were identified in healthy and hypothyroid patients regardless of the cause of that condition. Our studies emphasize the contributing role of Se in altered lipid metabolism in patients with hypothyroidism. The association between Se and particular lipid molecules was modified by thyroid pathology. Out of 145 different lipid molecules analyzed qualitatively by TLA in the present study only six PCs, i.e. PC aa C24:0, PC aa C26:0, PC ae C30:1, PC ae C34:0, PC ae C36:4, PC ae C42:0 were positively associated with the presence of hypothyroidism. Plasma selenium levels showed a negative relationship with the presence of hypothyroidism. Subsequent studies are required to elucidate the mechanisms of such association and clarify the role of particular lipid species in hypothyroidism.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Medical University of Lublin.
Abbreviations
- a:
-
Acyl residue
- aa:
-
Diacyl resid
- ae:
-
Acyl-alkyl residue
- BMI:
-
Body mass index
- FG:
-
Fasting plasma glucose
- FINS:
-
Fasting plasma insulin
- FT3:
-
Free triiodothyronine
- FT4:
-
Free thyroxine
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- HT:
-
Hashimoto thyroiditis
- ICP-MS:
-
Inductively coupled plasma mass spectrometry
- LDL-C:
-
Low-density lipoprotein cholesterol
- LT4:
-
Levothyroxine
- lysoPC:
-
Lysophosphatidylcholine
- PC:
-
Phosphatidylcholine
- Se:
-
Selenium
- SM:
-
Sphingomyelin
- SM (OH):
-
Hydroxysphingomyelin
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- TgAb:
-
Antithyroglobulin antibody
- TLA:
-
Targeted lipidomic analysis
- TQ-LC/MS:
-
Triple quadrupole liquid chromatography/mass spectrometry
- TPOAb:
-
Thyroid peroxidase antibody
- TSH:
-
Thyrotropin
References
Wang, J., Wang, C. & Han, X. Tutorial on lipidomics. Anal. Chim. Acta. 1061, 28–41. https://doi.org/10.1016/j.aca.2019.01.043 (2019).
Płaczkiewicz-Jankowska, E. & Jankowski, P. Diagnostyka i leczenie zaburzeń lipidowych u chorych z zaburzeniami endokrynnymi. Podsumowanie wytycznych the Endocrine Society 2020 z odniesieniem do wytycznych European Society of Cardiology (2019) i zaleceń Polskiego Towarzystwa Kardiologicznego, Polskiego Towarzystwa Lipidologicznego i Kolegium Lekarzy Rodzinnych w Polsce. Med. Prakt. 5, 12–36 (2021).
Newman, C. B. et al. Lipid management in patients with endocrine disorders: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 105, 1–70. https://doi.org/10.1210/clinem/dgaa674 (2020).
Płaczkiewicz-Jankowska, E. Leczenie niedoczynności tarczycy: podsumowanie wytycznych American thyroid association task force on thyroid hormone replacement. Med. Prakt. 5, 12–26 (2014).
Jonklaas, J. et al. American thyroid association task force on thyroid hormone replacement. Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid. 12, 1670–1751. https://doi.org/10.1089/thy.2014.0028 (2014).
Duntas, L. H. Thyroid disease and lipids. Thyroid 12, 287–293. https://doi.org/10.1089/10507250252949405 (2002).
Luo, Y. et al. Assessment of the relationship between subclinical hypothyroidism and blood lipid profile: reliable or not?. Lipids Health Disease 21, 137. https://doi.org/10.1186/s12944-022-01749-0 (2022).
Monzani, F. et al. Effect of levothyroxine replacement on lipid profile and intima-media thickness in subclinical hypothyroidism: A double-blind, placebo-controlled study. J. Clin. Endocrinol. Metab. 89(5), 2099–2106. https://doi.org/10.1210/jc.2003-031669 (2004).
Gu, Y. et al. Thyroid function and lipid profile in euthyroid adults: the TCLSIH cohort study. Endocrine 70(1), 107–114. https://doi.org/10.1007/s12020-020-02312-6 (2020).
Chin, K. Y. et al. The relationships between thyroid hormones and thyroid-stimulating hormone with lipid profile in euthyroid men. Int J Med Sci. 11(4), 349–355. https://doi.org/10.7150/ijms.7104 (2014).
Li, X., Wang, Y., Guan, Q., Zhao, J. & Gao, L. The lipid-lowering effect of levothyroxine in patients with subclinical hypothyroidism: A systematic review and meta-analysis of randomized controlled trials. Clin Endocrinol. 87, 1–9. https://doi.org/10.1111/cen.13338 (2017).
Newman, C. B. et al. Lipid management in patients with endocrine disorders: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metabolism https://doi.org/10.1210/clinem/dgaa674 (2020).
Toh, P., Nicholson, J. L., Vetter, A. M., Berry, M. J. & Torres, D. J. Selenium in bodily homeostasis: Hypothalamus, hormones, and highways of communication. Int. J. Mol. Sci. 23, 15445. https://doi.org/10.3390/ijms232315445 (2022).
Błażewicz, A., Wiśniewska, P. & Skórzyńska-Dziduszko, K. Selected essential and toxic chemical elements in hypothyroidism—A literature review (2001–2021). Int. J. Mol. Sci. 22, 10147. https://doi.org/10.3390/ijms221810147 (2021).
Ventura, M., Melo, M. & Carrilho, F. Selenium and thyroid disease: from pathophysiology to treatment. Int. J. Endocrinol. https://doi.org/10.1155/2017/1297658 (2017).
Duntas, L. H., Mantzou, E. & Koutras, D. A. Effects of a 6 month treatment with selenomethionine in patients with autoimmune thyroiditis. Eur. J. Endocrinol. 148, 389–393 (2003).
Larsen, C. B. et al. Selenium supplementation and placebo are equally effective in improving quality of life in patients with hypothyroidism. Eur. Thyroid J. https://doi.org/10.1530/ETJ-23-0175 (2024).
Gorini, F., Sabatino, L., Pingitore, A. & Vassalle, C. Selenium: An element of life essential for thyroid function. Molecules 23, 7084. https://doi.org/10.3390/molecules26237084 (2021).
Leonidas, H. D. Selenium and the thyroid: A close-knit connection. J. Clin. Endocrinol. Metabol. 95(12), 5180–5188. https://doi.org/10.1210/jc.2010-0191 (2010).
Zhang, L. et al. Integrated microRNA and proteome analysis reveal a regulatory module in hepatic lipid metabolism disorders in mice with subclinical hypothyroidism. Exper. Therapeutic Med. 19, 897–906 (2020).
Mazaheri-Tehrani, S. et al. Serum selenium levels and lipid profile: A systematic review and meta-analysis of observational studies. Biol. Trace Elem. Res. https://doi.org/10.1007/s12011-024-04365-4 (2024).
Solnica, B. et al. Guidelines of the polish society of laboratory diagnostics (PSLD) and the polish lipid association (PoLA) on laboratory diagnostics of lipid metabolism disorders. Arch. Med. Sci. 16(2), 237–252. https://doi.org/10.5114/aoms.2020.93253 (2020).
Swinnen, J. V. & Rueda, N. A beginner’s guide to lipidomics. The Biochemist 44, 1. https://doi.org/10.1042/bio_2021_181 (2022).
Liu, Y. Y. & Brent, G. A. Thyroid hormone crosstalk with nuclear receptor signaling in metabolic regulation. Trends Endocrinol. Metab. 21, 166–173 (2010).
Zhang, D. et al. Important hormones regulating lipid metabolism. Molecules 27(20), 7052. https://doi.org/10.3390/molecules27207052 (2022).
Wang, Y., Viscarra, J., Kim, S. J. & Sul, H. S. Transcriptional regulation of hepatic lipogenesis. Nat. Rev. Mol. Cell Biol. 16, 678–689. https://doi.org/10.1038/nrm4074 (2015).
Santana-Farre, R. et al. Influence of neonatal hypothyroidism on hepatic gene expression and lipid metabolism in adulthood. PLoS One https://doi.org/10.1371/journal.pone.0037386 (2012).
Sinha, R., Yen, P.M., Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., Kalra, S., Kaltsas, G., Kapoor, N., Koch, C., Kopp, P., Korbonits, M., Kovacs, C.S., Kuohung, W., Laferrère, B., Levy, M., McGee, E.A., McLachlan, R., New, M., Purnell, J., Sahay, R., Shah, A.S., Singer, F., Sperling, M.A., Stratakis, C.A., Trence, D.L. & Wilson, D.P. (2018) Cellular Action of Thyroid Hormone.
Johnson, J. L. & Johnson, L. A. Homeostasis of Lipid Metabolism in Disorders of the Brain Encyclopedia of Behavioral Neuroscience 2nd edn, 372–382 (Elsevier, 2022). https://doi.org/10.1016/B978-0-12-819641-0.00146-8.
Sorrenti, S. et al. Iodine: Its role in thyroid hormone biosynthesis and beyond. Nutrients 13(12), 4469. https://doi.org/10.3390/nu13124469 (2021).
McCord, J. M. The evolution of free radicals and oxidative stress. Am. J. Med. 108, 652–659 (2000).
McGill, M. R. & Jaeschke, H. Chapter 4 - Oxidant Stress, Antioxidant Defense, and Liver Injury. in Drug-Induced Liver Disease (Third Edition) (eds. Kaplowitz, N. & DeLeve, L. D.) 71–84 (Academic Press, Boston, 2013). https://doi.org/10.1016/B978-0-12-387817-5.00004-2.
Ahsan, H., Hasan, M. Y. & Ahmad, R. Chapter 16 - Role of free radicals in autoimmune diseases. In Translational autoimmunity (ed. Rezaei, N.) (Academic Press, 2022). https://doi.org/10.1016/B978-0-12-822564-6.00016-1.
Lobo, V., Patil, A., Phatak, A. & Chandra, N. Free radicals, antioxidants and functional foods: Impact on human health. Pharmacogn Rev. 4, 118–126. https://doi.org/10.4103/0973-7847.70902 (2010).
Reddy, V. P. Oxidative stress in health and disease. Biomedicines 11, 2925 (2023).
Halliwell, B. & Gutteridge, J. M. C. Cellular responses to oxidative stress: adaptation, damage, repair, senescence and death. Free Radic. Biol. Med. 4(1), 187–267 (2007).
Kochman, J., Jakubczyk, K., Bargiel, P. & Janda-Milczarek, K. The influence of oxidative stress on thyroid diseases. Antioxidants 10, 1442 (2021).
Sugawara, M. Reactive Oxygen Species and Thyroid Diseases. in Systems Biology of Free Radicals and Antioxidants (ed. Laher, I.) 3521–3538 (Springer, Berlin, Heidelberg, 2014). https://doi.org/10.1007/978-3-642-30018-9_150.
Hubler, M. J. & Kennedy, A. J. Role of lipids in the metabolism and activation of immune cells. J. Nutr. Biochem. 34, 1–7. https://doi.org/10.1016/j.jnutbio.2015.11.002 (2016).
Cengiz, H., Demirci, T., Varim, C. & Tamer, A. The effect of thyroid autoimmunity on dyslipidemia in patients with euthyroid hashimoto thyroiditis. Pak. J. Med. Sci. 37(5), 1365–1370. https://doi.org/10.12669/pjms.37.5.3883 (2021).
Ahluwalia, K. et al. Lipidomics in understanding pathophysiology and pharmacologic effects in inflammatory diseases: considerations for drug development. Metabolites 12(4), 333. https://doi.org/10.3390/metabo12040333 (2022).
Zandl-Lang, M., Plecko, B. & Köfeler, H. Lipidomics—paving the road towards better insight and precision medicine in rare metabolic diseases. Int. J. Mol. Sci. 24, 1709. https://doi.org/10.3390/ijms24021709 (2023).
Johnson, J. L. & Johnson, L. A. Homeostasis of Lipid Metabolism in Disorders of the Brain. In Encyclopedia of Behavioral Neuroscience 2nd edn (ed. Della Sala, S.) 372–382 (Elsevier, 2022). https://doi.org/10.1016/B978-0-12-819641-0.00146-8.
Li, L., Zhang, M., Men, Y., Wang, W. & Zhang, W. Heavy metals interfere with plasma metabolites. Including lipids and amino acids. in patients with breast cancer. OncolLett. 19, 2925–2933. https://doi.org/10.3892/ol.2020.11402 (2020).
Franco, J.S., Amaya-Amaya, J. & Anaya, J.M. (2013) Thyroid disease and autoimmune diseases. Autoimmunity: From Bench to Bedside [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459466/
Huo, Z. et al. Brain and blood metabolome for Alzheimer’s dementia: findings from a targeted metabolomics analysis. Neurobiol Aging. 86, 123–133. https://doi.org/10.1016/j.neurobiolaging.2019.10.014 (2020).
Jonas, J. P. et al. Circulating metabolites as a concept beyond tumor biology determining disease recurrence after resection of colorectal liver metastasis. HPB 24(1), 116–129. https://doi.org/10.1016/j.hpb.2021.06.415 (2022).
Kuhn, M. et al. Mass spectrometric profiling of cerebrospinal fluid reveals metabolite biomarkers for CNS involvement in varicella - zoster virus reactivation. J. Neuroinflammation. 15(1), 20. https://doi.org/10.12669/pjms.37.5.3883 (2018).
Breier, M. et al. Immediate reduction of serum citrulline but no change of steroid profile after initiation of metformin in individuals with type 2 diabetes. J. Steroid Biochem. Molecular Biol. 174, 114–119. https://doi.org/10.1016/j.jsbmb.2017.08.004 (2017).
Dong, Q. et al. Metabolic signatures elucidate the effect of body mass index on Type 2 diabetes. Metabolites 13(2), 227. https://doi.org/10.3390/metabo13020227 (2023).
Quell, J. D. et al. Characterization of bulk phosphatidylcholine compositions in human plasma using side-chain resolving lipidomics. Metabolites 9(6), 109. https://doi.org/10.3390/metabo9060109 (2019).
Signorelli, P., Conte, C. & Albi, E. The multiple roles of sphingomyelin in Parkinson’s Disease. Biomolecules 11(9), 1311. https://doi.org/10.3390/biom11091311 (2021).
Varma, V. R. et al. Brain and blood metabolite signatures of pathology and progression in Alzheimer disease: A targeted metabolomics study. PLoS Med. 15(1), e1002482. https://doi.org/10.1371/journal.pmed.1002482 (2018).
Olsen, A. S. B. & Færgeman, N. J. Sphingolipids: membrane microdomains in brain development function and neurological diseases. Open Biol. 7(5), 170069. https://doi.org/10.1098/rsob.170069 (2017).
Podbielska, M., Ariga, T. & Pokryszko-Dragan, A. Sphingolipid players in multiple sclerosis: Their influence on the initiation and course of the disease. Int. J. Mol. Sci. 23, 5330. https://doi.org/10.3390/ijms23105330 (2022).
Lee, M., Lee, S. Y. & Bae, Y. S. Functional roles of sphingolipids in immunity and their implication in disease. Exp Mol Med 55, 1110–1130. https://doi.org/10.1038/s12276-023-01018-9 (2023).
Walter, S. et al. Pharmacological inhibition of acid sphingomyelinase ameliorates experimental autoimmune encephalomyelitis. Neurosignals 27, 20–31. https://doi.org/10.33594/000000183 (2019).
Beckmann, N. et al. Regulation of arthritis severity by the acid sphingomyelinase. Cell Physiol. Biochem. 43, 1460–1471. https://doi.org/10.1159/000481968 (2017).
Grassi, S., Chiricozzi, E., Mauri, L., Sonnino, S. & Prinetti, A. Sphingolipids and neuronal degeneration in lysosomal storage disorders. J. Neurochem. 148, 600–611. https://doi.org/10.1111/jnc.14540 (2019).
Carsana, E. V. et al. Massive accumulation of sphingomyelin affects the lysosomal and mitochondria compartments and promotes apoptosis in Niemann-Pick disease type A. J. Mol. Neurosci. 72(7), 1482–1499. https://doi.org/10.1007/s12031-022-02036-4 (2022).
Edsfeldt, A. et al. sphingolipids contribute to human atherosclerotic plaque inflammation. Arteriosclerosis Trombosis Vascular Biol. https://doi.org/10.1161/ATVBAHA.116.305675 (2016).
Pan, F. et al. Sphingomyelin is involved in multisite musculoskeletal pain: evidence from metabolomic analysis in 2 independent cohorts. Pain 162(6), 1876–1881. https://doi.org/10.1097/j.pain.0000000000002163 (2021).
Assi, N. et al. Do metabolic signatures mediate the association between lifestyle factors and hepatocellular carcinoma risk? Results from a nested case-control study in EPIC. Cancer Epidemiol Biomarkers Prev. 27(5), 531–540. https://doi.org/10.1158/1055-9965.EPI-17-0649 (2018).
Meyer, J. J. et al. Blood-based targeted metabolomics discriminate patients with alcoholic liver cirrhosis from those with non-cirrhotic liver damage: An explorative study. Dig Dis. 40(2), 223–231. https://doi.org/10.1159/000516488 (2022).
Varma, V. R. et al. Brain and blood metabolite signatures of pathology and progression in Alzheimer disease: A targeted metabolomics study. PLoS Med. 15(1), e1002482. https://doi.org/10.1371/journal.pmed.1002482 (2018).
Sokolowska, E. et al. Sphingomyelin profiling in patients with diabetes could be potentially useful as differential diagnostics biomarker: A pilot study. Adv. Med. Sci. 67(2), 250–256. https://doi.org/10.1016/j.advms.2022.06.001 (2022).
Erlic, Z. et al. Targeted metabolomics as a tool in discriminating endocrine from primary hypertension. J. Clin. Endocrinol. Metab. 106(4), 1111–1128. https://doi.org/10.1210/clinem/dgaa954 (2021).
Huang, J. et al. Validation of candidate phospholipid biomarkers of chronic kidney disease in hyperglycemic individuals and their organ-specific exploration in leptin receptor-deficient db/db mouse. Metabolites 11(2), 89. https://doi.org/10.3390/metabo11020089 (2021).
Ożegowska, K., Plewa, S., Mantaj, U., Pawelczyk, L. & Matysiak, J. Serum metabolomics in PCOS women with different body mass index. J. Clin. Med. 10(13), 2811. https://doi.org/10.3390/jcm10132811 (2021).
Vouk, K., Ribič-Pucelj, M., Adamski, J. & Lanišnik Rižner, T. Altered levels of acylcarnitines. phosphatidylcholines. and sphingomyelins in peritoneal fluid from ovarian endometriosis patients. J. Steroid Biochem. Molecular Biol. 159, 60–69. https://doi.org/10.1016/j.jsbmb.2016.02.023 (2016).
Khorasani, E., Mirhafez, S. R. & Niroumand, S. Assessment of the selenium status in hypothyroid children from north east of Iran. J. Biol. Today’s World 6, 21–26 (2017).
Stojsavljević, A. et al. Significance of arsenic and lead in hashimoto’s thyroiditis demonstrated on thyroid tissue, blood, and urine samples. Environ. Res. 186, 109538 (2020).
Soujanya, K. V. & Jayadeep, A. P. Obesity-associated biochemical markers of inflammation and the role of grain phytochemicals. J. Food Biochem. 46, e14257 (2022).
Saito, Y., Yoshida, Y., Akazawa, T., Takahashi, K. & Niki, E. Cell death caused by selenium deficiency and protective effect of antioxidants. JBC 278(41), 39428–39434 (2003).
Finelli, C. Molecular mechanisms and mediators of hepatotoxicity resulting from an excess of lipids and non-alcoholic fatty liver disease. Gastrointest. Disord. 5, 243–260. https://doi.org/10.3390/gidisord5020020 (2023).
Bień, D., Michalczuk, M., Szkopek, D., Kinsner, M. & Konieczka, P. Changes in lipids metabolism indices as a result of different form of selenium supplementation in chickens. Sci. Rep. 12(1), 13817. https://doi.org/10.1038/s41598-022-18101-2 (2022).
Hasani, M. et al. Effect of selenium supplementation on lipid profile: A systematic review and meta-analysis. Horm Metab Res. 50(10), 715–727. https://doi.org/10.1055/a-0749-6655 (2018).
Christensen, K., Werner, M. & Malecki, K. Serum selenium and lipid levels: Associations observed in the National Health and Nutrition Examination Survey (NHANES) 2011–2012, Environmental Research, 140. ISSN 76–84, 0013–9351. https://doi.org/10.1016/j.envres.2015.03.020 (2015).
Bleys, J. et al. Serum selenium and serum lipids in US adults. Am. J. Clin. Nutr. 88, 416–423. https://doi.org/10.1093/ajcn/88.2.416 (2008).
Wasowicz, W., Gromadzinska, J., Rydzynski, K. & Tomczak, J. Selenium status of low-selenium area residents: Polish experience. Toxicol. Lett. 137, 95–101. https://doi.org/10.1016/S0378-4274(02)00383-1 (2003).
Rayman, M. The importance of selenium to human health. Lancet 356, 233–241. https://doi.org/10.1016/S0140-6736(00)02490-9 (2000).
Janowska, M. et al. An assessment of serum selenium concentration in women with endometrial cancer. Nutrients, MDPI 14(5), 958. https://doi.org/10.3390/nu14050958 (2022).
Muntau, A. C. et al. Age-related reference values for serum selenium concentrations in infants and children. Clin Chem. 48(3), 555–560. https://doi.org/10.1093/clinchem/48.3.555 (2002).
Vinceti, M. et al. Selenium speciation in human serum and its implications for epidemiologic research: a cross-sectional study. J. Trace Elements Med. Biol. 31, 1–10. https://doi.org/10.1016/j.jtemb.2015.02.001 (2015).
Pyrzynska, K. & Sentkowska, A. selenium species in diabetes mellitus type 2. Biol. Trace Elem. Res. https://doi.org/10.1007/s12011-023-03900-z (2023).
Acknowledgements
The authors thank the study participants for their time and effort to participate in the study and gratefully acknowledge the use of the services and facilities of the Center for Interdisciplinary Research of The John Paul II Catholic University of Lublin, Poland, co-funded by the European Union from the European Regional Development Fund in the frame of the Operational Programme Development of Eastern Poland 2007-2013 (POPW.01.03.00-06-003/09-00).
Funding
This work was supported by the Medical University of Lublin (internal grant: DS53/2021–2023/ Anna Błażewicz- “Investigation of endocrine disruptors, elemental and lipid profiles in biological fluids and tissues in people with endocrine and/or metabolic disorders”).
Author information
Authors and Affiliations
Contributions
Author contributions: Conceptualization: AB, KSD; Methodology: AB, KSD, PS, AT, AKP, KS, AS; Formal analysis and investigation: JW, PS, AT, AKP, KS, AS ; Writing—original draft preparation: AB, KSD, AMG; Writing—review and editing: AB, KSD; Funding acquisition: AB, EG; Resources: AB, KSD, JW, AMG; Supervision: KSD.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the Medical University of Lublin (approval number KE-0254/7/2021).
Informed consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Błażewicz, A., Wojnicka, J., Grabrucker, A.M. et al. Preliminary investigations of plasma lipidome and selenium levels in adults with treated hypothyroidism and in healthy individuals without selenium deficiency. Sci Rep 14, 29140 (2024). https://doi.org/10.1038/s41598-024-80862-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-80862-9