Abstract
Korean chronic kidney disease (CKD) patients have relatively low cardiovascular disease (CVD) and high end stage kidney disease (ESKD) incidence rates. Using the multi-state model this study analyzed the 5- and 10-year cumulative hazard estimates, transition probabilities and risk factors associated with the five clinical transitions; ESKD, CVD, CVD to death, ESKD to death and death. CKD stages 1–4 patients from the KoreaN Cohort Study for Outcome in Patients With Chronic Kidney Disease cohort were included. Multivariable multi-state model analysis was performed to investigate the study outcomes associated with the five transitions. Among the 1502 patients (median age 54 years, male 61.3%), the overall prevalence of clinical events were: ESKD (22.6%), CVD (7.5%), death after ESKD (3.6%), death (3.3%) and death after CVD (1.2%). Patients who experienced intermediate ESKD event had higher risk of death than those who experienced CVD event (10-year cumulative hazard: 0.35; 95% CI: 0.23, 0.48 vs. 0.27; 95% CI: 0.15, 0.40). The 10-year transition probability was highest for enrollment to ESKD (0.27; 95% CI: (0.23, 0.31)) followed by enrollment to CVD (0.08; 95% CI: 0.07, 0.10). Different clinical risk factors were associated with each of the five transitions. Patients who experienced intermediate ESKD event were more exposed to death risk than those who experienced CVD and the highest 10-year progression probability was for enrollment to ESKD followed by death after ESKD. Different risk factors were associated with varying transitions. These findings correlate with the distinctive clinical features of Korean CKD patients.
Similar content being viewed by others
Introduction
Patients with chronic kidney disease (CKD) have increased risks of cardiovascular disease (CVD) due to accelerated vascular calcification and myocardial fibrosis associated with chronic inflammation1. In the western CKD population, CVD is the leading cause of death rather than end stage kidney disease (ESKD) with high incidence of CVD events2,3,4,5. Korean CKD patients have distinctive differences in event outcomes compared to western patients where the CVD incidence is comparably lower, approximately 7% opposed to 33.4% from the Chronic Renal Insufficiency Cohort study, and that of ESKD is higher2,6,7.
Since the KoreaN Cohort Study for Outcome in Patients With Chronic Kidney Disease (KNOW-CKD) is a longitudinal study the enrolled patients are not only exposed to fatal events such as death, but also to intermediate non-fatal events such as CVD and ESKD8. Estimating the survival probability of CKD patients only with the information of whether the patient survived or are censored while ignoring intermediate events may lead to misleading results. In situations where intermediate events may occur during the patient’s disease pathway the multi-state model is used to analyze the effects of intermediate events on patient’s mortality by adding intermediate event states to the two-state model.
It is important to investigate the progression probability and risk factors associated with various clinical events in CKD patients as early surveillance and individualized management of risk factors can reduce the overall morbidity and mortality. Also, it may give clues to the distinctive differences in clinical outcomes between Asian and western CKD patients. Therefore, multi-state model consisting of the five clinical event transitions, including CVD, ESKD, CVD to death, ESKD to death and death, was designed to more adequately explain the disease progression pathway of Korean CKD patients from the KNOW-CKD study. Using this multi-state model, this study compared the effects of ESKD or CVD event experience on patient’s death and analyzed the 5- and 10-year cumulative hazard estimates, transition probabilities and clinical risk factors associated with the five clinical event transitions.
Materials and methods
Study design
The KNOW-CKD study includes Korean non-dialysis CKD patients from nine university hospital affiliated nephrology centers in Korea8. The study exclusion criteria include: 1) history of dialysis or organ transplantation, 2) congestive heart failure (NYHA class 3 or 4), 3) liver cirrhosis (Child–Pugh class 2 or 3), 4) past or current history of cancer, 5) pregnant, or 6) single kidney due to trauma or kidney donation. The CKD subtypes were classified into four categories according to the cause of CKD: diabetes mellitus (DM), hypertension, glomerulonephritis and polycystic kidney disease.
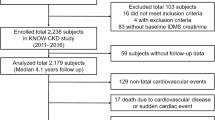
Among the 2237 CKD patients between ages of 20 and 75, 100 patients with initial ESKD diagnosis and 389 patients who dropped out within 6 months of study enrollment were excluded. Also, 246 patients were excluded due to unclassified CKD subtype (n=107), follow-up loss after CVD or ESKD event (n=25), missing information of study variables (n= 83) and study outcomes (n=31). Finally a total of 1502 patients were included for analysis (Fig. 1)
The KNOW-CKD study was conducted according to the principles of the Declaration of Helsinki and supervised by the Korea Disease Control and Prevention Agency. Written informed consents were obtained from all the participants. This study was approved by the Institutional Review Boards of all nine participating hospitals including Seoul National University Hospital in 2011.
Laboratory and clinical variables
Baseline laboratory measurements and clinical information were collected at the study entry. Baseline laboratory measurements included hemoglobin (Hb), blood urea nitrogen (BUN), creatinine, sodium, potassium, calcium, phosphorus, uric acid, fasting glucose, hemoglobin A1C (HbA1C), total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), C-reactive protein (CRP), parathyroid hormone (PTH), fibroblast growth factor-23 (FGF-23) and spot urine protein-to-creatinine ratio. Serum creatinine was measured at one central laboratory (LabGenomics, Seongnam, Korea) using the isotope dilution mass spectrometry-traceable method for consistency. Estimated glomerular filtration rate (eGFR) was calculated using the 2009 Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine equation9. Serum c-terminal FGF-23 was measured using the enzyme-linked immunosorbent assay (ELISA) kit with the intraassay and interassay coefficients of variation of ≤ 2.4% and ≤ 4.7% (Immutopics, California, United States). Other laboratory examinations were conducted in each enrolled hospital laboratory.
Baseline clinical information including sociodemographic data, lifestyle patterns including smoking status (never, former, current), medical history and medication were collected using a self-reported questionnaire with the assistance of a trained staff in each participating hospital. Blood pressure was measured by the trained nurse using an electronic sphygmomanometer after 5 min of rest in sitting position. Hypertension was defined as: (a) systolic blood pressure (SBP) > 140 mmHg or diastolic blood pressure (DBP) > 90 mmHg or (b) previous hypertension diagnosis or (c) on antihypertensive medication. DM was defined as: (a) fasting serum glucose > 126 mg/dL or (b) previous DM diagnosis or (c) on antidiabetic medication.
Multi-state model
The multi-state model consisting of the five transitions is shown in Fig. 2. The five transitions were: enrollment to CVD (transition 1), enrollment to ESKD (transition 2), CVD to death (transition 3), ESKD to death (transition 4) and enrollment to death (transition 5). The above five clinical hard outcomes were selected as these outcomes were particularly associated with increased morbidity and mortality risks in the CKD population. In cases where both CVD and ESKD intermediate events occurred, only the event which occurred first was considered in the current model. CVD event was defined as nonfatal CVD event including acute myocardial infarction, hospitalization for unstable angina or heart failure, receiving percutaneous coronary artery intervention or coronary bypass graft surgery, ischemic stroke, hemorrhagic stroke, carotid artery disease, peripheral artery disease, symptomatic arrhythmia or any other CVD event that required hospitalization or intervention. ESKD event was defined as the initiation of either dialysis or kidney transplantation. Death was defined was death from any cause. The proposed multi-state model with intermediate states can be interpreted as a competing risk model with six mutually exclusive competing risk pathways10.
Statistical analysis
For the analysis of baseline characteristics of study population, continuous variables were expressed as median and interquartile range. Categorical variables were expressed as frequencies and percentages.
In this study, it was assumed that the disease progression of a patient satisfies the Markov property where the transition of a patient from one state to another at the specified time since enrollment depends only on the state to which the patient belongs and does not depend on how long the patient stays in that state. In addition, the Cox proportional hazards model was employed to include the characteristics of patients in the multi-state model. Therefore, the rate of transition from state \(i\) to state \(j\) for a patient with covariate \(z(t)\) at time \(t(>0)\) since enrollment can be written as follows:
where \({\lambda }_{ij0}\left(t\right)\) is an unspecified baseline rate of transition from state \(i\) to state \(j\) and \({\beta }_{ij}\) is a vector of regression coefficients indicating the extent to which the covariate \(z(t)\) affects the transition rate from state \(i\) to state \(j\)11. In long-term follow-up studies, there may be covariates that remain unchanged as well as those that may change with each monitoring period. When defining the model, these were expressed as time-dependent covariates, i.e., z(t). However, in this study, we conducted the analysis using the covariate values at the time of enrollment. First, the baseline transition rate included in the above model was estimated for each of the five transitions using the nonparametric method proposed by Nelson and Aalen11,12. Second, the Aalen-Johansen estimator was used to estimate the probabilities of the transition state within a certain time since enrollment11. Third, univariable and multivariable multi-state model analyses were performed to test whether the effect of each predictor on each of the five transition rates was statistically significant and estimate the marginal effect of each variable on each of the five transitions. Finally, based on the results of the multivariable multi-state model, the 10-year transition probability of the five transitions were predicted. The mstate R package version 0.3.3 (July, 2024) was used for the statistical analyses in this study.
Results
Baseline characteristics of enrolled patients
During the median follow-up duration of 7.17 years, a total of 1502 patients (median age 54 years, male 61.3%) were included. The baseline characteristics of the enrolled patients are described in Table 1. The most common cause of CKD was glomerulonephritis (38%) followed by DM (23.7%), polycystic kidney disease (19.2%) and hypertension (19.1%).
Prevalence of the clinical transition events according to CKD subtype
The majority of enrolled patients experienced no event (61.8%) followed by ESKD (22.6%), CVD (7.5%), death after ESKD (3.6%), death (3.3%) and death after CVD (1.2%). According to the CKD subtype, the most common event experienced by diabetic nephropathy patients was ESKD (37.9%) followed by no event (33.7%) and CVD (12.4%). For hypertensive, glomerulonephritis and polycystic kidney disease patients, the highest number of patients experienced no event followed by ESKD and CVD (Table 2).
Estimation of cumulative hazards of the five transitions
Both the 5- and 10-year cumulative hazards of transition 2 (enrollment to ESKD) (5-year: 0.21; 95% CI: 0.19, 0.24, 10-year: 0.43; 95% CI: 0.37, 0.49) was highest followed by transition 4 (ESKD to death) (5-year: 0.20; 95% CI: 0.09, 0.31, 10-year: 0.35; 95% CI: 0.23, 0.48). Also, the 5- and 10-year cumulative hazards for both transitions 3 (CVD to death) (5-year: 0.19; 95% CI: 0.09, 0.30, 10-year: 0.27; 95% CI: 0.15, 0.40) and 4 (ESKD to death) were higher than that of transition 5 (enrollment to death) (5-year: 0.03; 95% CI: 0.02, 0.04, 10-year: 0.05; 95% CI: 0.03, 0.06). Therefore, the patients who experienced either CVD or ESKD intermediate events were exposed to higher risk of death than those who did not. The 5-year cumulative hazard estimates were similar for transitions 3 (CVD to death) and 4 (ESKD to death). However, the 10-year cumulative hazard estimate was approximately 1.3 fold higher in transition 4 showing that the subjects who experienced intermediate ESKD event were exposed to higher risk of death than those who experienced CVD event at 10 years (Fig. 3).
Transition probabilities of the five transitions
Similar trends of transition probabilities were observed at both 5 and 10 years with the highest being transition 2 (enrollment to ESKD) followed by transition 4 (ESKD to death). The 5-year transition probability was highest in transition 2 (enrollment to ESKD) (0.16; 95% CI: 0.15, 0.18) followed by transition 1 (enrollment to CVD) (0.06; 95% CI: 0.04, 0.07), transition 4 (ESKD to death) (0.02; 95% CI: 0.01, 0.02), transition 5 (enrollment to death) (0.02; 95% CI: 0.02, 0.03) and transition 3 (CVD to death) (0.01; 95% CI: 0.00, 0.01). The 10-year transition probability was also highest in transition 2 (0.27; 95% CI: 0.23, 0.31) followed by transition 1 (0.08; 95% CI: 0.07, 0.10), transition 4 (0.05; 95% CI: 0.03, 0.06), transition 5 (0.04; 95% CI: 0.03, 0.05) and transition 3 (0.01; 95% CI: 0.01, 0.02) (Fig. 4).
In comparison of the transition probabilities according to the baseline CKD stages (1, 2, 3a vs. 3b, 4) similar trends were observed as the overall analysis, but the transition probabilities for each clinical transitions were higher in the higher baseline CKD stage group (Supplementary Fig. 1).
Risk factors associated with each of the five transitions
The Cox proportional hazard models were used to analyze the various clinical risk factors associated with the five transitions. (Tables 3 and 4). The reference group for smoking status was never-smokers and that for the CKD subtype was glomerulonephritis. Both CRP and FGF-23 were transformed into log[(FGF-23) + 1] and log(CRP) as the distributions were highly skewed. There was no polycystic kidney disease patient who experienced transition 3. Therefore, the values corresponding to this are missing in both univariable and multivariable analysis.
Different clinical variables were associated with different transition states in both univariable and multivariable analysis. In the multivariable analysis, transition 1 (enrollment to CVD) was associated with older age (HR: 1.07; 95% CI: 1.05, 1.09), male (HR: 1.71; 95% CI: 1.17, 2.50), eGFRcreatinine (HR: 0.99; 95% CI: 0.98, 0.99), CRP (HR: 1.13; 95% CI: 1.00, 1.28), proteinuria (HR: 1.15; 95% CI: 1.06, 1.25), current or former smoking status (HR: 1.58; 95% CI: 1.12,2.24) and CVD history (HR: 4.56; 95% CI: 3.04, 6.84). In comparison to glomerulonephritis, diabetic nephropathy (HR: 4.71; 95% CI: 2.97, 7.49) and hypertensive nephropathy (HR: 1.20; 95% CI: 1.41, 3.97) were associated with increased transition risks. For transition 2 (enrollment to ESKD) older age (HR: 1.02; 95% CI: 1.01, 1.02), higher systolic blood pressure (HR: 1.02; 95% CI: 1.01, 1.03), eGFRcreatinine (HR: 0.92; 95% CI: 0.91, 0.93), FGF-23 (HR: 1.42; 95% CI: 1.32, 1.53), CRP (HR: 1.09; 95% CI: 1.01, 1.17), proteinuria (HR: 1.41; 95% CI: 1.36, 1.46), current or former smoking status (HR: 1.27; 95% CI: 1.04, 1.54), CVD history (HR: 1.84; 95% CI: 1.33, 2.54) and diabetic nephropathy (HR: 3.53; 95% CI: 2.78, 4.48) were associated with transition risk. For transition 3 (CVD to death) only increased age (HR: 1.10; 95% CI: 1.02, 1.18) was associated with increased risk and for transition 4 (ESKD to death) older age (HR: 1.12; 95% CI: 1.08, 1.16), higher CRP (HR: 1.24; 95% CI: 1.02, 1.50) and CVD history (HR: 2.69; 95% CI: 1.37, 5.26) were associated with increased transition risk. Finally, for transition 5 (enrollment to death) older age (HR: 1.06; 95% CI: 1.04, 1.09), male (HR: 2.18; 95% CI: 1.14, 4.16), higher systolic blood pressure (HR: 1.03; 95% CI: 1.01, 1.04), eGFRcreatinine (HR: 0.98; 95% CI: 0.97, 0.99), FGF-23 (HR: 1.25; 95% CI: 1.02, 1.52), CRP (HR: 1.22; 95% CI: 1.01, 1.48), proteinuria (HR: 1.28; 95% CI: 1.15, 1.43), current or former smoking status (HR: 1.97; 95% CI: 1.11, 3.49) and CVD history (HR: 4.33; 95% CI: 2.21, 8.49) were associated with transition risk. Also, in comparison to glomerulonephritis, diabetic nephropathy (HR: 7.79; 95% CI: 3.10, 19.56), hypertensive nephropathy (HR: 4.83; 95% CI: 1.29, 9.47) and PKD (HR: 4.43; 95% CI: 1.60, 12.25) were all associated with higher risks for enrollment to death transition.
Discussion
During the median follow-up duration of 7.17 years, 61.8% of Korean CKD patients did not experience any clinical event followed by 22.6% of patients who only experienced ESKD event. Both 5- and 10-year cumulative hazard estimates and transition probabilities were highest in transition 2 (enrollment to ESKD). This finding correlates with that of previous studies where the incidence rate of ESKD was higher and that of CVD was relatively lower in Asian CKD patients compared to the western patients6,7,13.
Both the 5- and 10-year cumulative hazard estimates of transitions 3 (CVD to death) and 4 (ESKD to death) were higher than that of transition 5 (enrollment to death) meaning that the patients who experienced intermediate events had increased risk of death than those who didn’t. In comparison of the cumulative hazard estimates of transitions 3 and 4, patients experienced intermediate ESKD event were exposed to a higher risk of death than those who experienced intermediate CVD event. A previous study which analyzed the mortality causes in Korean CKD patients showed that the most common cause was kidney-related disease followed by DM-related and CVD-related14. Asian CKD patients tend to experience more rapid kidney function decline compared to the western patients possibly due to higher prevalence of comorbid metabolic complications including anemia, hypoalbuminemia, hyperparathyroidism, hyperphosphatemia and hypocalcemia.15,16 Also, the differences in susceptibility of CVD event, traditional cardiovascular risk factors and lifestyle patterns may be associated with low risk of CVD and CVD-associated death in Asian CKD patients7,17,18,19. These factors may have attributed to the relatively higher risk of death in Korean CKD patients who experienced intermediate ESKD event compared to those who experienced CVD event.
The 5- and 10-year transition probabilities of the five clinical transitions states were similar with the highest being transition 2 (enrollment to ESKD) followed by transition 1 (enrollment to CVD). In particular, in comparison to the 5-year transition probability, the 10-year transition probabilities for transition 4 (ESKD to death) was 2.5 fold higher, that of transition 5 (enrollment to death) was twofold higher and that of transition 2 (enrollment to EKSD) was 1.6 fold higher meaning that the risk of ESKD and death was highly increased at relatively 10 years. On the contrary, the 10-year transition probabilities for transitions 1 (enrollment to CVD) and 3 (CVD to death) were relatively stable compared to that of 5-years. Also, since the cause of CKD is an important predictor of clinical outcomes, subgroup analysis of transition probabilities according to the CKD subtype was conducted (Supplementary Fig. 2). Similar patterns observed in all CKD subtypes compared to that of the overall CKD population. However, the 10-year transition probabilities for both transitions 1 (enrollment to CVD) and 2 (enrollment to ESKD) were particularly high in the diabetic nephropathy subtype. As diabetic nephropathy is the leading cause of CKD and diabetic nephropathy patients are likely to have other metabolic comorbidities, including obesity and dyslipidemia, the probability that the patient will experience ESKD and CVD event will be higher than the other CKD subtypes. 20,21 Also, the 10-year transition probabilities for both transitions 2 (enrollment to EKSD), 4 (ESKD to death) and 5 (enrollment to death) were particularly high in the PKD subtype as PKD patients generally experience more rapid kidney function decline and are at higher risk of experiencing fatal events associated with cyst infection and hemorrhage complications. 22,23 Therefore, CKD patients need different risk management and prediction strategies at different sites of the disease progression timeline and the cause of CKD is important in predicting the disease course that the patient will experience.
Different risk factors were associated with each clinical transition. In particular, variables associated with ESKD, which are of particular importance in Korean CKD patients, were older age, higher SBP, CRP, FGF-23 and proteinuria levels, current or former smoking status, CVD history and diabetic nephropathy. For ESKD to death, older age, higher CRP level and CVD history were associated with increased risks. As older age was significantly associated with increased risks in all five transitions it may be one of the most important risk factors associated with clinical outcomes. Different clinical risk factors including age, CVD history and CKD subtype must be carefully evaluated in stratifying clinical event and outcome risks in CKD patients.
To our knowledge, this is the first study to incorporate multi-state model in a large CKD cohort to analyze the crude hazard estimate and transitional probability of the five transition states in the CKD patient’s disease progression pathway. Through our proposed model, we were able to eliminate the bias that could be produced by disregarding intermediate events when predicting the survival function of CKD patients and predict the patient-specific transition probability at any state of time since enrollment. Also, the relatively proportionate number of patients in each CKD subgroup allowed accurate statistical analysis. The limitations of this study include the relatively small number of CVD events compared to other large CKD cohort studies and that the results of this study may be limited to that of the Korean CKD population4,24. However, as the overall CVD incidence is similar to that of other Asian CKD cohort studies and the results of this study consistently show low crude hazard estimate and transition probability of CVD risks, this finding may be a distinctive clinical characteristic of Asian CKD patients7,13,25. Also, the intermediate events, CVD and ESKD, are mutually transitional; however, as shown in Fig. 2, the relevant transitions were not incorporated into the model as although there were 33 patients who experienced ESKD event after CVD event there was no patient who experienced CVD event after ESKD event. Therefore, the regression parameters for the corresponding transitions could not be calculated.
In conclusion, Korean CKD patients showed distinctive clinical characteristic where the risk of ESKD was highest and those who experienced intermediate ESKD event were exposed to a higher risk of death than those who experienced CVD. Also, the highest 5- and 10-year progression probability was ESKD followed by ESKD to death and varying risk factors were associated with each clinical transition state. Therefore, individualized clinical event risk management and prediction are needed at different timeline of the patient’s disease progression pathway. Also, various clinical variables must be taken into account for accurate outcome risk assessment.
Data availability
The data used in this study are available from the KNOW-CKD investigator team upon reasonable request. For data requirement, please contact Kook-Hwan Oh (khoh@snu.ac.kr), the head of KNOW-CKD investigator team.
Change history
22 April 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41598-025-98168-9
References
Jankowski, J. et al. Cardiovascular disease in chronic kidney disease: Pathophysiological insights and therapeutic options. Circulation 143(11), 1157–1172 (2021).
Shah, R. et al. Serum fractalkine (CX3CL1) and cardiovascular outcomes and diabetes: Findings from the chronic renal insufficiency cohort (CRIC) study. Am. J. Kidney Dis. 66(2), 266–273 (2015).
Sarnak, M. J. et al. Kidney disease as a risk factor for development of cardiovascular disease: A statement from the american heart association councils on kidney in cardiovascular disease, high blood pressure research, clinical cardiology, and epidemiology and prevention. Circulation 108(17), 2154–2169 (2003).
Martínez-Castelao, A. et al. Baseline characteristics of patients with chronic kidney disease stage 3 and stage 4 in Spain: the MERENA observational cohort study. BMC Nephrol. 12(1), 1–11 (2011).
Iimori, S. et al. Anaemia management and mortality risk in newly visiting patients with chronic kidney disease in J apan: The CKD-ROUTE study. Nephrology 20(9), 601–608 (2015).
Oh, K. H. et al. The KNOW-CKD Study: What we have learned about chronic kidney diseases. Kidney Res. Clin. Pract. 39(2), 121–135 (2020).
Ryu, H. et al. Incidence of cardiovascular events and mortality in Korean patients with chronic kidney disease. Sci. Reports 11(1), 1131 (2021).
Oh, K.-H. et al. KNOW-CKD (KoreaN cohort study for Outcome in patients With Chronic Kidney Disease): design and methods. BMC Nephrol. 15(1), 80 (2014).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150(9), 604–612 (2009).
Geskus, R. Data analysis with competing risks and intermediate states 1–245 (Chapman and Hall/CRC, 2015).
Nelson, W. Theory and applications of hazard plotting for censored failure data. Technometrics 14(4), 945–966 (1972).
Aalen, O. Nonparametric inference for a family of counting processes. Ann. Stat. 6(4), 701–726 (1978).
Tanaka, K. et al. Cardiovascular events and death in Japanese patients with chronic kidney disease. Kidney Int. 91(1), 227–234 (2017).
Lee, M. J. et al. Trends in the incidence, prevalence, and mortality of end-stage kidney disease in south korea. Diabetes Metab. J. 44(6), 933–937 (2020).
Mehrotra, R. et al. Racial differences in mortality among those with CKD. J. Am. Soc. Nephrol. https://doi.org/10.1681/ASN.2007070747 (2008).
Barbour, S. J. et al. Differences in progression of CKD and mortality amongst Caucasian, Oriental Asian and South Asian CKD patients. Nephrol. Dialysis. Transplant. 25(11), 3663–3672 (2010).
Lu, X. et al. Genome-wide association study in Han Chinese identifies four new susceptibility loci for coronary artery disease. Nat. Genetics 44(8), 890–894 (2012).
Kuller, L. H. Ethnic differences in atherosclerosis, cardiovascular disease and lipid metabolism. Curr. Opin. Lipidol. 15(2), 109–113 (2004).
Kao, W. H. et al. MYH9 is associated with nondiabetic end-stage renal disease in African Americans. Nat. Genet. 40(10), 1185–1192 (2008).
Pálsson, R. & Patel, U. D. Cardiovascular complications of diabetic kidney disease. Adv. Chronic. Kidney Dis. 21(3), 273–280 (2014).
Huxley, R., Barzi, F. & Woodward, M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. Bmj 332(7533), 73–78 (2006).
Ryu, H. et al. Comparison of outcomes of chronic kidney disease based on etiology: a prospective cohort study from KNOW-CKD. Sci. Rep. 13(1), 3570 (2023).
Haynes, R. et al. Evaluating the contribution of the cause of kidney disease to prognosis in CKD: results from the Study of Heart and Renal Protection (SHARP). Am. J. Kidney Dis. 64(1), 40–48 (2014).
Denker, M. et al. Chronic Renal Insufficiency Cohort Study (CRIC): Overview and Summary of Selected Findings. Clin. J. Am. Soc. Nephrol. 10(11), 2073–2083 (2015).
Kim, J. H. et al. Comparison of cardiovascular event predictability between the 2009 and 2021 Chronic Kidney Disease Epidemiology Collaboration equations in a Korean chronic kidney disease cohort: the KoreaN Cohort Study for Outcome in Patients With Chronic Kidney Disease. Kidney Res. Clin. Pract. https://doi.org/10.2876/j.krcp.22.206 (2023).
Acknowledgements
The institutional review board of each participating clinical center approved the study protocol as follows: Seoul National University Hospital (1104-089-359), Seoul National University Bundang Hospital (B-1106/129-008), Yonsei University Severance Hospital (4-2011- 0163), Kangbuk Samsung Medical Center (2011-01-076), Seoul St. Mary’s Hospital (KC11OIMI0441), Gil Hospital (GIRBA2553), Eulji General Hospital (201105-01), Chonnam National University Hospital (CNUH-2011-092), and Pusan Paik Hospital (11-091). The authors thank the clinical research coordinators of each participating center for their dedication during patient recruitment and data acquisition.
Funding
The KNOW-CKD study was supported by Research Programs funded by the Korea Disease Control and Prevention Agency (2011E3300300, 2012E3301100, 2013E3301600, 2013E3301601, 2013E3301602, 2016E3300200, 2016E3300201, 2016E3300202, 2019E320100, 2019E320101, 2019E320102, and 2022‐11‐007). Also, this research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (No. NRF-2020R1F1A1A01048397; RS-2023-00239958) (Jinheum Kim). This work was supported (50%) by the New Faculty Startup Fund from Seoul National University.
Author information
Authors and Affiliations
Contributions
J.H Kim, J Kim, and K-H Oh assisted with conception or design, drafting the article, analysis and interpretation of data, revising the article and final approval of the article. J Kim, J.Y Jung, J.C Jeong and S.H Han assisted with analysis and interpretation of data.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article Affiliation 1 was incomplete and was given as ‘Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Republic of Korea’. The correct affiliation is listed in the correction notice.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, J.H., Kim, J., Kim, J. et al. Risk factors and transitional probability of clinical events in Korean CKD patients using the multistate model. Sci Rep 15, 8582 (2025). https://doi.org/10.1038/s41598-024-82426-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-82426-3