Abstract
Given the increasing trend of cholecystectomy, it is imperative to reassess surgical and surveillance strategies in consideration of the potential long-term risks for digestive tract cancers. The objective of this study was to assess the risk of gastrointestinal (GI) and hepato-biliary-pancreatic (HBP) cancer incidence after cholecystectomy. The data for this cohort study was obtained from the National Health Insurance Service database in Korea. 715,872 patients who underwent cholecystectomy between 2004 and 2020 were compared to 1,431,728 individuals who did not underwent cholecystectomy after age, sex, and year of cholecystectomy was matched. The overall incidence rate ratio (IRR) for all GI and HBP cancers was 1.08 (95% C.I., 1.06–1.10). Specifically, the risk of diagnosis of extrahepatic bile duct cancer (IRR 1.92), intrahepatic bile duct cancer (1.78), hepatocellular carcinoma (1.22), and pancreatic cancer (1.13) was significantly increased in the cholecystectomy group. The highest IRR was observed within the 1–3 years following cholecystectomy. Subsequently, the risk of diagnosis gradually decreased and returned to a level comparable to that of the matched control group after 5 to 10 years. In conclusion, hepato-biliary-pancreatic cancer are frequently diagnosed subsequent to cholecystectomy. Too short period of post-cholecystectomy follow-up may hinder monitoring of hepato-biliary-pancreatic cancer occurrence.
Similar content being viewed by others
Introduction
Cholecystectomy is a highly prevalent surgical procedure, with over 1.2 million cases performed annually in the United States and approximately 80,000 cases in Korea1,2. The introduction of laparoscopic surgery has significantly reduced postoperative complications, leading to broader surgical indications especially in younger patients with minimal symptoms. However, the question of whether cholecystectomy increases the long-term risk of cancer development has yielded inconsistent research findings.
Since the 1980s, sporadic reports have suggested that continuous exposure of the gastrointestinal tract to bile after cholecystectomy, coupled with hormonal changes related to gut metabolism and alterations in the gut microbiota, may potentially elevate the incidence of various digestive system cancers3,4,5. However, a systematic literature review in 2015, based on an analysis of 75 previous studies, found no strong evidence of an association between cholecystectomy and an increased risk of digestive system cancers, including esophageal, stomach, liver, bile duct, pancreatic, small intestine, colorectal, and rectal cancers, which were previously thought to have heightened risk5,6. Conversely, other meta-analysis results that analyzed 29 previous studies have indicated a significantly increased risk of pancreatic cancer in cases where cholecystectomy was performed due to gallstones, even after adjusting for factors such as diabetes, obesity, smoking, and follow-up duration7.
Given that the patient group undergoing cholecystectomy differs from the general population in terms of age and gender, this study intends to assess the risk of gastrointestinal and hepato-biliary-pancreatic cancer incidence in the cholecystectomy group by comparing it with a control group matched for age gender, and year of cholecystectomy. The data for this analysis was derived from the National Health Insurance Service database, a comprehensive nationwide health insurance system that covers approximately 97% of the population6.
Methods
Data source
This is a retrospective cohort study using data obtained from the National Health Insurance Service (NHIS) database, Korea. Primary outcome was identifying incidence risk ratio (IRR) of gastrointestinal (GI) and hepato-biliary-pancreatic (HBP) cancer in case group compared to age, sex, and year of cholecystectomy-matched control group.
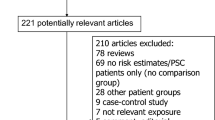
Figure 1a illustrates the patient selection flow chart. We employed a two-year washout period starting from the initial year of available NHIS data, 2002, to exclude patients with a history of GI and HBP cancer or GI and HBP surgery before undergoing cholecystectomy. Subsequently, we analyzed patients from 2004 to 2020. Among patients who had cholecystectomy (identified by insurance claim code Q7380) with diagnosis of cholelithiasis, cholecystitis, or other benign gallbladder conditions (coded as K80–K82 in the 10th International Classification of Diseases8), those who were under 20 years of age at the time of cholecystectomy, those who had two or more records of cholecystectomy, as well as those who died within six months following cholecystectomy were excluded from the analysis9. Afterwards, various exclusion criteria were applied to exclude patients with a history of GI and HBP cancer or GI and HBP surgery before undergoing cholecystectomy or receiving a cancer diagnosis. Furthermore, we excluded all cases with a history of GI and HBP cancer or GI and HBP surgery even after the washout period and before cholecystectomy. Finally, 715,872 patients were included in analysis as the case group.
The control group, composed of individuals in a 1:4 ratio relative to the case group, consisted of those who had neither undergone cholecystectomy nor had a history of GI and HBP cancer before 2004 (Fig. 1b) and those who were equal or over 20 years of age at the time of cholecystectomy. After applying exclusion criteria, 3,615,461 individuals between 2004 and 2020 were identified. Among these, 1:2 matching was done regarding age, sex, and year of cholecystectomy of the case group. Finally, 1,431,728 individuals were included in analysis as the control group.
Identification of cancer cases
The categories of cancer classification were as follows; esophageal (ICD-10 code C15); stomach (C16); small intestine (C17); colorectum (C18-C20); anus (C21); liver (C22); extrahepatic bile duct (C24, EBDC); pancreas (C25); and other unspecified digestive cancer (C26). Particularly, liver cancer (C22) was subcategorized as intrahepatic bile duct cancer (C22.1, IBDC) and hepatocellular carcinoma and other subtypes (C22 except C22.1, HCC and others). In the early days of cancer registries and cause-of-death statistics, hepatocellular carcinoma and other histologic subtypes, which make up a small fraction of primary liver cancer, were not well distinguished. Therefore, to account for potential diagnostic inaccuracies, statistical calculations were performed by combining hepatocellular carcinoma with other subtypes as HCC and others10.
Ethical statement
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. Prior approval was obtained from the Institutional Review Board, National Cancer Center, Korea (reference number NCC2021-0133). The requirement for written informed consent from participants was waived by the Institutional Review Board due to the retrospective design of the study.
Statistical analysis
A poisson regression model, known as a method which fits countable rare events to given person-times and other demographic covariates, was employed to compare the incidence of digestive tract cancer in the case group with that in the age, sex, and year-matched control group. In our meticulously matched design, which obviated the need for further consideration of covariates in our regression model, the incidence rate was defined by dividing the number of cancer cases by the sum of each person’s contributed years within our follow-up period (2004–2020). The incidence rate ratio (IRR), obtained by exponentiating the regression coefficient, represents the ratio of the incidence rates between the two groups, with values greater than 1 indicating a higher rate.
Starting one year before the individual’s cholecystectomy record date (the matched date for the control group), we applied ICD-10 algorithms11, and calculated the Charlson Comorbidity Index (CCI) score by multiplying the presence or absence of morbidities by their original weights. The obtained CCI was categorized into ‘none,’ ‘moderate,’ and ‘severe,’ with corresponding cutoffs of zero, 1 ≤ CCI < 3, and ≥ 3, respectively.
Univariate and CCI-adjusted multivariate Cox proportional hazard regression models were employed to assess the risk of digestive tract cancer incidence.
Statistical analysis was conducted using R Statistical Software (v4.2.2; R Core Team 2022) and SAS (Release 9.4, SAS Institute Inc., Cary, NC, USA).
Results
Patient characteristics
The mean age of the case group was 53.4 years, with individuals aged between 40 and 59 years constituting 43.3% of all patients (Table 1). The male-to-female ratio was 1:1.2. The number of cholecystectomy procedures consistently increased from 2004 to 2020. As matched control group was matched by age, sex, and year of cholecystectomy of case group, distribution of age group, sex, and year of cholecystectomy was identical to case group. The proportion of individuals with a CCI equal to or higher than 1 was higher in the case group.
Cancers in all sites, not limited to GI and HBP cancers, were diagnosed in 5.5% of the case group and 5.0% of the matched control group. GI and HBP cancers were diagnosed in 2.2% of the case group and 2.0% of the matched control group. Stomach, colorectum, and liver cancers were the most common GI and HBP cancers in both the case and matched control groups.
Incidence rate ratio compared to matched control
The overall IRR of all GI and HBP cancers in the case group compared to the matched control group was 1.08 (Fig. 2a). The IRR for EBDC (1.92), IBDC (1.78), HCC and others (1.22), and pancreatic (1.13) cancer was significantly increased in the case group.
Incidence rate ratios of gastrointestinal and hepato-biliary-pancreatic cancers in case group compared to matched control. (a) Overall gastrointestinal and hepato-biliary-pancreatic cancer, entire period, (b) Overall gastrointestinal and hepato-biliary-pancreatic cancer, according to follow-up period, (c) Incidence rate ratios according to cancer site and follow-up period.
According to the follow-up period, IRR for all GI and HBP cancers was highest within the 1 to 3 years following cholecystectomy (Fig. 2b). Subsequently, the IRR gradually decreased and returned to a level comparable to that of the matched control group after a period of 10 years.
In terms of specific cancer sites, the IRR for IBDC showed a significant increase throughout the follow-up period (Fig. 2c). It peaked within 1 to 3 years following cholecystectomy and gradually decreased afterward. EBDC exhibited a similar pattern, but the IRR returned to a level comparable to that of the matched control group after a period of 10 years. The IRR for HCC and others increased continuously after 1 to 3 years following cholecystectomy. The IRRs for stomach and colorectal were mildly elevated within 1 to 3 years, and 1 to 5 years, respectively, following cholecystectomy. The IRR for pancreatic cancer was constantly elevated within 1 to 10 years. Subsequently, the IRRs for stomach, colorectal, and pancreatic cancer returned to a level comparable to that of the matched control group, and in the case of colorectal cancer, even decreased below the level of the matched control group.
The IRR was compared to the matched control group was analyzed according to sex and age group. In male patients, the case group aged 20–39 years exhibited a comparable IRR of cancer when compared to the matched control group (Table 2). For male patients aged 40 years and older, the IRR for HCC and others, IBDC, and EBDC increased, while that for colorectal cancer decreased. Specifically, the IRR of pancreatic cancer was elevated in the 40–64 years age group. In female patients, the case group aged 20–39 years exhibited a comparable IRR of cancer when compared to the matched control group. For female patients aged 40 years and older, the IRR for HCC and others, IBDC, EBDC, and pancreatic cancer was elevated.
CCI adjusted hazard ratio of GI and HBP cancers compared to matched control group
The hazard ratios of GI and HBP cancer in case group, when compared to the age and sex-matched control group and adjusted for CCI are presented in Table 3. The hazard ratios for intra- and extrahepatic bile duct cancer in the case group were significantly increased. In contrast, the hazard ratios for esophagus, stomach, colorectum, anus, and hepatocellular carcinoma and others were significantly decreased when compared to the matched control group.
Discussion
Until now, there were concerns about the long-term increase in cancer occurrence following the rise in cholecystectomy procedures. Particularly, with a high proportion of young patients, a heightened post-operative cancer occurrence would necessitate a more cautious approach to surgical indications. In this population-based study, cholecystectomy was associated with an increased diagnosis of EBDC, IBDC, HCC and others and pancreatic cancer compared to a matched control group. The IRR reached its peak within 1–3 years after cholecystectomy but gradually diminished thereafter, eventually becoming comparable to the level of the control group. Consequently, the study suggests that cholecystectomy does not elevate the long-term risk of cancer occurrence but diagnosis of hepato-biliary-pancreatic cancer is increased after cholecystectomy.
Concerning EBDC, certain studies have documented an increased risk of occurrence shortly after cholecystectomy, which gradually decreases to a nonsignificant level over time12,13. On the contrary, other cohort studies reported nonsignificant risk of EBDC occurrence with reported effect estimate ranging from 0.70 to 2.225,14,15. On the other hand, there has been a scarcity of studies focusing specifically on IBDC, but a previous report revealed increased risk of IBDC following cholecystectomy12. In this study, it was observed that patients who underwent cholecystectomy had an increased diagnosis of EBDC or IBDC starting from the age of 40 years.
The majority of previous studies that reported an elevated risk of liver cancer (C22) after cholecystectomy did not distinguish between IBDC and HCC and others, despite their distinct pathology and epidemiology6,14,15,16,17,18,19. Previous studies have provided inconsistent results, with some indicating an increased risk of HCC after cholecystectomy12,13, while others did not find a significant change in liver cancer risk ranging between 0.91 and 1.1712,14,15,20. In this study, diagnosis of HCC and others increased in both sexes compared to the matched control group in patients with the age of 40 years and older.
Pancreatic cancer also had conflicting reports with effect estimate ranging from 0.80 to 2.435. Some cohort studies reported an elevated risk of pancreatic cancer following cholecystectomy12,13,15,21, while others could not find a significant association14,20. However, more recent meta-analysis including some of the aforementioned references revealed increased risk of pancreatic cancer following cholecystectomy7. In this study, pancreatic cancer showed an elevated diagnosis when compared to a matched control group, especially within the age group of 40–64.
This study also noted that the IRR of diagnosis peaked during the first 1 to 3 years following cholecystectomy and gradually decreased afterward, particularly for IBDC and EBDC. The secular trend was in line with previous studies, wherein the risk of cancer occurrence peaks immediately following cholecystectomy and subsequently diminishes over time12,13. The absence of a cumulative increase in the IRR of cancer occurrence after cholecystectomy over time does not provide conclusive evidence for a causal relationship between cholecystectomy and cancer development. While chronic bile exposure is often considered a contributing factor to inflammation and cellular repair processes resulting in tumorigenesis22, this explanation seems less plausible in the context of our data, given the relatively short duration of exposure before the observed peak. Therefore, we hypothesize that the increased incidence of hepato-biliary-pancreatic cancer after cholecystectomy is likely attributable to enhanced diagnostic detection rather than actual cancer development.
On the other hand, gallstones are recognized as a significant risk factor for biliary cancer, particularly cholangiocarcinoma22. Furthermore, based on the observation that the increased risk of cholangiocarcinoma decreases to baseline levels within ten years of cholecystectomy—a finding consistent with this study—it has been suggested that the elevated risk may be attributable to gallstone disease rather than the cholecystectomy procedure itself23. As this study did not examine cancer incidence based on the presence or absence of gallstones, it is difficult to draw definitive conclusions. However, this possibility should be considered. Additionally, we would like to suggest that the symptoms prompting cholecystectomy in patients with gallstones may have been induced by subtle changes in the bile ducts, which are challenging to detect through imaging or blood tests.
Nevertheless, it is important to consider the phenomenon observed where the diagnosis of cancer increases within 1–3 years after surgery and took 5 to 10 years for the IRR to decrease to the levels observed in the control group from an observational perspective. Particularly, patients aged 40–64 are younger than the typical age of onset for hepato-biliary-pancreatic cancers which might make it less intuitive to focus on the risk of cancer. Therefore, if individuals in these age groups have undergone cholecystectomy, it would advisable to exercise caution when determining the follow-up duration after surgery, as setting it too short may not allow for adequate monitoring of the diagnosis of these cancers.
In this study, the diagnosis of stomach cancer in female and colorectal cancer in male following cholecystectomy were found to be lower compared to the matched control group. It is worth noting that previous studies on these cancers have reported conflicting results, with the reported risks being either elevated or not significantly different5,14,24,25, but not as significantly low as observed in this study. Although fully explaining the mechanisms behind this phenomenon may have its limitations, lifestyle modification after cholecystectomy might have had an impact. Additionally, we can hypothesize that the extensive healthcare access and utilization in Korea, where individuals receive medical care both before and after cholecystectomy, including examinations for other organs, might contribute to the early detection and removal of precursor lesions. This, in turn, could potentially explain the observed lower incidence of cancer in these cases12.
The strengths of our study are that the dataset used in this study spans 17 years from 2004 to 2020 and encompasses a large-scale, nationwide dataset that includes all cholecystectomy data that doesn’t meet the exclusion criteria. Notably, it excludes not only the history of GI and HBP cancer but also GI and HBP surgical history. Moreover, a distinctive feature of this study is the exclusion of prior cancer diagnoses or surgeries, extending beyond the defined washout period (from January 2002 to December 2003) to encompass cancer diagnoses and surgeries conducted prior any cholecystectomy but after January 2004. Additionally, the control group was meticulously constructed to match the case group in terms of age, sex, and year of cholecystectomy, allowing for a comparable person-years comparison.
However, this study has several limitations. One significant limitation of this study is the lack of risk adjustment for various clinical risk factors and the absence of sensitivity analysis. Accurately identifying individual clinical risk factors from a population-level database proved challenging due to the unavailability or incomplete capture of relevant data. Furthermore, we reasoned that clinical risk factors such as inflammatory disorders, metabolic conditions, and infections would not significantly influence the decision to undergo cholecystectomy. Consequently, the study was conducted on the assumption that constructing a large matched control cohort with comparable age and gender distributions would result in similar distributions of clinical risk factors. While the risk estimates remained unchanged after adjusting for the CCI, it is important to note that we cannot completely rule out the possibility of confounding by other unmeasured risk factors. Another limitation of this study is the inability to account for the specific underlying causes of cholecystectomy, which may influence cancer risk differently. While we examined cancer risk in a broad cohort, the diverse etiologies of cholecystectomy may have introduced unmeasured confounding factors that could affect the observed outcomes. Future research incorporating these variables could provide a more nuanced understanding of this relationship. Additionally, while previous studies have suggested an increased incidence of various non-abdominal cancers following cholecystectomy, with evidence of a potential link to an elevated risk of certain non-gastrointestinal cancers, the mechanisms underlying this association remain unclear and the risks have been controversial, with the exact biological pathways not yet fully understood6,26,27,28. Therefore, this study focused on GI and HBP cancers, given the stronger biological plausibility and more established epidemiological evidence for these malignancies. However, future research incorporating broader datasets, ideally including both abdominal and non-abdominal cancers, would be valuable in addressing this gap in the data. Furthermore, this study examined only the diagnosis of HBP cancer following cholecystectomy, without investigating the causal relationship between cholecystectomy and HBP cancer.
In conclusion, hepato-biliary-pancreatic cancers revealed an increased diagnosis following cholecystectomy when compared to a matched control group even in the age group 40–64 years. The IRR peaked during the first 1 to 3 years following cholecystectomy and gradually decreased afterward, and it took 5 to 10 years for the IRR to decrease to the levels observed in the control group. Special attention should be paid to the age group of 40–64 years, as it is a period when individuals may not pay significant attention to the risk of developing hepato-biliary-pancreatic cancer. Therefore, if cholecystectomy has been performed, it would be advisable to focus more on monitoring the occurrence of these cancers during follow-up, and not to set the follow-up duration too short, as this may not allow for adequate monitoring of potential risks.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to restrictions imposed by the National Health Insurance Service database, which only allows data analysis within controlled environments, but are available from the corresponding author on reasonable request.
References
Jones, M. W., Guay, E. & Deppen, J. G. Open Cholecystectomy. StatPearls, Treasure Island (FL) Ineligible Companies. Disclosure: Evan Guay Declares no Relevant Financial Relationships with Ineligible Companies. Disclosure: Jeffrey Deppen declares no relevant financial relationships with ineligible companies. (2023).
Health Insurance Review & Assessment Service. HIRA Bigdata Open portal. (2023).
Giovannucci, E., Colditz, G. A. & Stampfer, M. J. A meta-analysis of cholecystectomy and risk of colorectal cancer. Gastroenterology 105(1), 130–141 (1993).
Mahid, S. S. et al. Meta-analysis of cholecystectomy in symptomatic patients with positive hepatobiliary iminodiacetic acid scan results without gallstones. Arch. Surg. 144(2), 180–187 (2009).
Coats, M. & Shimi, S. M. Cholecystectomy and the risk of alimentary tract cancers: a systematic review. World J. Gastroenterol. 21(12), 3679–3693 (2015).
Jung, Y. K. et al. De Novo Cancer incidence after Cholecystectomy in Korean Population. J. Clin. Med. 10, 7 (2021).
Fan, Y. et al. Increased risk of pancreatic Cancer related to gallstones and cholecystectomy: a systematic review and Meta-analysis. Pancreas 45(4), 503–509 (2016).
World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 10th rev. (World Health Organization, 1994).
Kim, Y. I. et al. Effect of Helicobacter pylori treatment on long-term mortality in patients with hypertension. Gut Liver 14(1), 47–56 (2020).
Park, H. M. et al. Trend Analysis and Prediction of Hepatobiliary Pancreatic Cancer incidence and mortality in Korea. J. Korean Med. Sci. 37(28), e216 (2022).
Quan, H. et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 43(11), 1130–1139 (2005).
Huang, D. et al. Gallstones, Cholecystectomy and the risk of Hepatobiliary and Pancreatic Cancer: a Nationwide Population-based Cohort Study in Korea. J. Cancer Prev. 25(3), 164–172 (2020).
Nogueira, L. et al. Gallstones, cholecystectomy, and risk of digestive system cancers. Am. J. Epidemiol. 179(6), 731–739 (2014).
Chen, Y. K. et al. Cancer risk in patients with cholelithiasis and after cholecystectomy: a nationwide cohort study. J. Gastroenterol. 49(5), 923–931 (2014).
Chow, W. H. et al. Gallstones, cholecystectomy and risk of cancers of the liver, biliary tract and pancreas. Br. J. Cancer. 79(3–4), 640–644 (1999).
Kao, W. Y. et al. Risk of hepato-biliary cancer after cholecystectomy: a nationwide cohort study. J. Gastrointest. Surg. 17(2), 345–351 (2013).
Kang, M. J. et al. Distinct prognosis of biliary tract cancer according to tumor location, stage, and treatment: a population-based study. Sci. Rep. 12(1), 10206 (2022).
Kang, M. J. et al. Incidence, mortality and survival of gallbladder, extrahepatic bile duct, and pancreatic cancer using Korea central cancer registry database: 1999–2019. Ann. Hepatobiliary Pancreat. Surg. 26(3), 220–228 (2022).
Hong, S. Y. et al. Incidence, mortality, and survival of liver cancer using Korea central cancer registry database: 1999–2019. Ann. Hepatobiliary Pancreat. Surg. 26(3), 211–219 (2022).
Goldacre, M. J. et al. Cancer after cholecystectomy: record-linkage cohort study. Br. J. Cancer 92(7), 1307–1309 (2005).
Ekbom, A. et al. Risk of pancreatic and periampullar cancer following cholecystectomy: a population-based cohort study. Dig. Dis. Sci. 41(2), 387–391 (1996).
Labib, P. L., Goodchild, G. & Pereira, S. P. Molecular Pathogenesis of Cholangiocarcinoma. BMC Cancer 19(1), 185 (2019).
Nordenstedt, H. et al. Gallstones and cholecystectomy in relation to risk of intra- and extrahepatic cholangiocarcinoma. Br. J. Cancer 106(5), 1011–1015 (2012).
Lee, J. et al. The risk of Colorectal Cancer after Cholecystectomy or Appendectomy: a Population-based Cohort Study in Korea. J. Prev. Med. Public. Health 51(6), 281–288 (2018).
Shao, T. & Yang, Y. X. Cholecystectomy and the risk of colorectal cancer. Am. J. Gastroenterol. 100(8), 1813–1820 (2005).
Choi, Y. J. et al. Increased risk of Cancer after Cholecystectomy: a Nationwide Cohort Study in Korea including 123,295 patients. Gut Liver 16(3), 465–473 (2022).
Chen, C. H., Lin, C. L. & Kao, C. H. Association of Cholecystectomy with the risk of prostate Cancer in patients with gallstones. Cancers (Basel) 12(3). (2020).
Kharazmi, E. et al. Gallstones, Cholecystectomy, and kidney Cancer: observational and mendelian randomization results based on large cohorts. Gastroenterology 165(1), 218–227e218 (2023).
Funding
The funding for this study was provided by the National Cancer Center, Republic of Korea (grant number: 2131660 and 2432270). The funding source has no role in the design, practice or analysis of this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: PSJ and KMJ. Data curation: KHJ and KYA. Methodology: KYA, KHJ, and KMJ. Visualization: KHJ and KMJ. Writing – original draft: KMJ, KYA, and KHJ. Writing, review, and editing: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, Y.A., Kim, H., Kang, M.J. et al. Increased diagnosis of hepato-biliary-pancreatic cancer after cholecystectomy: a population-based study. Sci Rep 15, 411 (2025). https://doi.org/10.1038/s41598-024-84781-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-84781-7
Keywords
This article is cited by
-
Persistent Global Associations Between Gallbladder-Biliary Diseases and Pancreatic Cancer: Evidence from 204 Countries and Territories Over 32 years
Digestive Diseases and Sciences (2025)