Abstract
Japan’s workplace reforms, including a 60-hour weekly work limit for medical residents, that has been in effect from April 2024, have raised concerns about compliance and its impact on training quality. This study analyzed data from 17,967 residents who participated in the General Medicine In-Training Examination from 2019 to 2022, focusing on weekly duty hours, clinical responsibilities, and training environments. Duty hours increased from 2019 to 2021, before declining in 2022. The proportion of residents working over 60 h per week decreased from 57 to 49%, while those working under 50 h increased from 12 to 19%. Concurrently, the percentage of residents managing zero to four inpatients rose from 18 to 39%. University hospital residents reported shorter duty hours but fewer patient encounters and diminished clinical exposure compared to community hospital residents. These findings underscore the educational consequences of duty-hour restrictions, particularly in university hospitals, where reduced clinical responsibilities may compromise competency-based training. The results highlight the need for balanced policies that ensure compliance while maintaining sufficient clinical exposure. Future reforms should prioritize equitable workload distribution, increased clinical opportunities, and targeted interventions to address disparities between hospital types, thereby ensuring the dual goals of resident well-being and high-quality medical education.
Similar content being viewed by others
Introduction
Over the past two decades, the policy of limiting resident doctors’ working hours has been widely adopted, particularly in the United States and European Union1,2. Resident physicians often work extended hours due to their dual roles in patient care and education. Extensive resident working hours have been linked to compromised patient safety and well-being, prompting a global consensus on the necessity of regulating these hours. Despite the recognition of the need for limits, challenges remain. First, no universal agreement exists on the maximum number of working hours. For instance, the US, Canada, and neighboring Asian countries cap working hours at approximately 80 per week, while the EU imposes a 48-hour limit3. In Japan, many residents are restricted to 60 h per week. These variations complicate the interpretation of evidence regarding the optimal working hour limits due to factors such as roles in patient care, education, and work ethic. Second, non-compliance with duty-hour restrictions is widespread. A large US study found that 84% of residents exceeded the prescribed limits4. This may be due to the demands of patient care, educational commitments, and pressure from programs and supervisors. Additionally, concerns also exist about the impact of hour restrictions on educational opportunities, particularly clinical case exposure. A 2011 systematic review of 37 studies from the US and EU reported that 30% of the studies noted a reduction in case experience5. Although subsequent US reports indicate a recovery in case numbers, it remains unclear whether this is related to the differences in upper limits6,7. Despite these unresolved issues, global collection and evaluation of data on the impacts of duty-hour policies could provide valuable insights in this context.
In Japan, regulations limiting the working hours of residents (and all physicians) were implemented in April 2024, lagging behind other countries1,8. In 2018, Japan introduced work-style reforms in response to its aging population and prolonged working hours for the broader workforce. Given the unique demands of the physician profession, implementing these reforms for doctors was deferred until 2024, and tailored restrictions were set. In 2021, the Ministry of Health, Labour and Welfare (MHLW) set the overtime limit for general physicians at 960 h per year (“Level A,” equivalent to a 60-hour work week). The standard legal working hours are set at 8 h per day and 40 h per week, with any additional hours classified as overtime. Furthermore, physicians in specialized training programs, such as residents, could work up to 1,860 h of overtime annually (“Level C-1,” similar to an 80-hour work week) because of their educational commitments. To ensure well-being, the law restricts continuous working hours to 28 h and mandates nine-hour rest intervals. Level C-1 applies to training hospitals designated by prefectures based on their work practices.
Although not explicitly stated, many residency programs, especially those in university hospitals, are expected to cap resident duty hours at Level A, equivalent to 60 h per week. Only a few programs are expected to apply the Level C-1 limits. Based on the MHLW’s 2016 Physician Work Hours Survey, residents averaged 67.2 h per week, including standby hours, based on a sample size of approximately 400 residents9. In a nationwide cross-sectional study conducted in 2019, 14.4% of 5,593 residents worked for over 80 h per week, while 58.9% reported working for 60 h or more10. Most residency programs have taken steps to reduce residents’ hours worked to address these extended duty hours.
Despite the new duty-hour limits, several issues remain unresolved. First, ascertain whether residents’ actual duty hours have decreased based on the mandated limits is vital. After the US implemented the 80-hours-per-week limit, studies indicated that the average weekly duty hours for residents dropped from 80 h to 75 h4. Similarly, in Korea, it decreased from 114 h to 88 h11. Conversely, Japan has a more stringent limit, restricting many residents to a 60-hour work week. This raises concerns about whether training programs in Japan could reduce these hours. Second, there exist some unintended educational consequences of the duty-hour restriction policy, such as a disproportionate reduction in duty hours and training opportunities for some residents. From an educational perspective, we have previously shown that a certain amount of work contributes to higher in-training examination scores and increased self-study time10,12,13. Hence, excessively curtailing duties and learning hours for certain groups might be detrimental to their education. However, this perspective has received limited attention in the duty-hour studies conducted in other countries. Finally, the factors contributing to residents’ prolonged duty hours remain poorly understood. The type of teaching hospital—whether community hospital or university hospital—may influence residents’ duty hours and their constraints. Identifying these factors could help determine which residents stand to benefit the most from protective policies.
In this study, we collected comprehensive data on resident duty hours in Japan from 2019 to 2022. The primary aim was to evaluate changes in resident duty hours and the educational environment in Japan toward implementing duty hour restrictions. To assess the training environment, we inquired about the average number of inpatients under residents’ care and the number of emergency department duties, which reflected the number of patient cases handled during residency. The secondary aim was to analyze the influence of different hospital types on these metrics. Finally, the third aim was to identify the determinants of prolonged resident duty hours. This study provides important evidence for medical educators and policymakers in Japan and globally to assess the impact of duty-hour restrictions and consider necessary policy adjustments.
Methods
Study setting
This multicenter survey study involved postgraduate residents who participated in the General Medicine In-training Examination (GM-ITE) over four years, that is, the 2019–2022 academic period. Educational environment surveys were administered every January immediately after the examination and accompanied by a research consent form. The informed consent form specified that participation was voluntary and that the responses were anonymous. All the participants gave their informed consent. This study was approved by the Ethical Review Committee of the Japanese Institute for Advancement of Medical Education Program (JAMEP) under Reference No. 22 − 14, and adhered to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines. Additionally, this study was conducted in accordance with the Declaration of Helsinki.
The GM-ITE is a residency-in-training examination designed for first- and second-year postgraduate residents (PGY-1 and -2) in Japan14. It assesses general clinical knowledge, and its application uses multiple-choice questions. The examination is annually curated by the Specified Nonprofit Corporation of JAMEP. Until the 2020 academic year, it comprised 60 questions. However, this number increased to 80 in 2021 to enhance its validity and reliability. Each training program could be used to participate in the GM-ITE. Examinations have been conducted annually since 2012. Participation in the examination increased significantly, reaching one-third of all medical residents in Japan by 2018.
Study population
The study participants were PGY-1 and PGY-2 residents in Japan who took the GM-ITE in the 2019, 2020, 2021, and 2022 academic years. To prevent data from being obtained from the same individual multiple times, e.g., if a resident took the examination in two consecutive years, data from their PGY-1 year were excluded from the analysis. Residents who either did not complete the educational environment survey or omitted duty-hour questions from the survey were excluded.
After completing their six-year medical education and passing the national examination in Japan, most medical graduates commence a two-year residency15. The training is provided by accredited community and university hospitals. Although the number of training hospitals and residents remained consistent, by 2022, 8,995 residents had been enrolled in programs at 1,024 hospitals16. To attain general medical proficiency, these training programs require residents to train in departments such as internal medicine, emergency medicine, surgery, pediatrics, obstetrics and gynecology, psychiatry, and community medicine, with additional elective training.
Measurements
The educational environment survey investigated residents’ average weekly duty hours throughout their residency training. As questions related to weekly duty hours varied each year (Appendix 1), the categorization was adjusted to ensure comparability as follows: < 50 h, 50 h to 60 h, 60 h to 70 h, 70 h to 80 h, and ≥ 80 h.
Additionally, we collected the following data from the educational environment survey and examination application form: average number of assigned inpatients (0 to 4, 5 to 9, 10 to 14, ≥ 15, and unknown), number of emergency department (ED) duties per month (0, 1 to 2, 3 to 5, ≥ 6, and unknown), and daily self-study duration (none, 0 min to 30 min, 31 min to 60 min, 61 min to 90 min, and ≥ 91 min). The average number of assigned inpatients refers to the number of patients assigned to each resident at a given time, averaged across all rotations. Moreover, information regarding the hospital, e.g., type (community, university, university-affiliated hospital), area (urban or non-urban), and number of annual ambulance volumes, was obtained from the Foundation for the Promotion of Medical Training website and the Healthcare Market Analysis Platform17,18.
In this study, training hospitals are categorized into three types: university hospitals, community hospitals, and university-affiliated hospitals. A university hospital refers to a general hospital that is affiliated with a university. A community hospital is located within a community and not operated by a university. In contrast, a university-affiliated hospital is situated in a community but operated by a university. Since university-affiliated hospitals have characteristics of both, university and community hospitals, they are classified as a distinct category.
Statistical analysis
We summarized the characteristics of residents and their work environments for the 2019 to 2022 academic year and categorized the same by hospital type. Linear trends in these characteristics were assessed using the Cuzick trend test where appropriate. The association between weekly duty hours and hospital type was analyzed using a proportional odds regression model, with community hospitals set as the reference for the analyses. To account for the clustering of residents within teaching hospitals, which violates the assumption of independent observations, we adjusted the estimated odds ratios (OR) and 95% confidence intervals (CI) using generalized estimating equations. We adjusted for academic year, age, sex, postgraduate year, monthly emergency duties, number of assigned inpatients, daily self-study time, hospital area, and the annual ambulance volume. Residents who did not provide information on adjusted factors were excluded from the multivariable analysis. All analyses were performed using the STATA software version 15 (STATA Corporation, College Station, Texas, USA).
Results
Between 2019 and 2022, the residents took the exam a total of 30,657 times. Of these, 24,621 provided consent to participate in the study and responded to the training environment questionnaire. After excluding 5,487 data entries from PGY-1 residents who had taken the exam for two consecutive years, we identified 19,134 residents. Subsequently, we excluded those who did not provide data on hours worked, resulting in a final sample of 17,967 participants (Fig. 1).
Flowchart of study participants. Note: Study participants were postgraduate year-1 (PGY-1) and − 2 (PGY-2) residents in Japan took the GM-ITE between 2019 and 2022. To avoid repeated data, if a resident took the exam in two successive years, their PGY-1 data was excluded. Residents who did not complete the duty hours question were omitted.
The participants’ demographics revealed that 63% were in their PGY-2 years, 68% were male, and the predominant age was 26 years (Table 1). Regarding hospital affiliation, 83% of residents were at community hospitals, 11% at university hospitals, and 6% at university-affiliated hospitals. Overall, 32% of the hospitals were located in urban areas. The most frequent number of ED shifts per month was three to five, reported by 70% of residents. On average, 56% of the residents were responsible for five to nine inpatients. The most common self-study duration was between 31 min and 60 min daily, as indicated by 40% of the participants.
When analyzed on the basis of hospital category, residents in university hospitals reported fewer ED shifts and shorter self-study times compared to those in community hospitals or university-affiliated hospitals (Table 1). Moreover, among university hospital types, residents in public university hospitals have significantly fewer monthly ED shifts, assigned inpatients, and self-study time compared to their private university hospital counterparts (Supplementary Table 1).
Annual trends
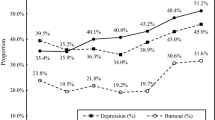
Figure 2 shows the annual trends in the self-reported resident duty hours. In the 2019 academic year, 57% of the residents reported having worked more than 60 h per week. This percentage increased to 60% in the 2021 academic year and began to decline in the 2022 academic year, reaching 49% (Fig. 2A). Contrastingly, from 2019 to 2022, the percentage of residents working fewer than 50 h per week rose from 12 to 19%.
Resident Weekly Duty Hours Trends: 2019–2022. Note: Fig. 2 illustrates the self-reported weekly duty hours of residents from 2019 to 2022. Weekly duty hours are categorized as: < 50 h, 50–60 h, 60–70 h, 70–80 h, and ≥ 80 h. Panel A depicts overall trends, whereas Panel B differentiates by hospital type: community, university, or university-affiliated.
Duty hours by the type of residency hospital (Fig. 2B) showed an upward trend through 2021, followed by a decline from 2022. Overall, community hospital residents exhibited longer duty hours than university hospital residents. In 2022, 51% of community hospital residents worked over 60 h per week, compared to 34% at university hospitals, highlighting a disparity. Furthermore, the proportion of residents at university hospitals working fewer than 50 h per week has increased, rising from 19% in 2019 to 32% in 2022. This trend was more pronounced at public universities than private universities (Supplementary Fig. 1).
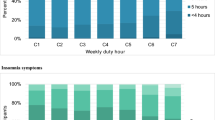
Table 2 illustrates the annual trends of educational metrics. The number of inpatients, monthly ED shifts, and daily self-study time decreased annually, and each item showed a negative trend (p < 0.001). In particular, the number of residents assigned to only zero to four inpatients had increased from 17.7% in 2019 to 38.6% in 2022.
Factors associated with weekly duty hours
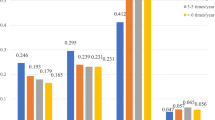
Table 3 shows the estimates of ORs for weekly duty hours based on the univariate and multivariate proportional odds models for hospital type. Compared to community hospital residents, university hospital residents exhibited fewer weekly duty hours (OR: 0.55; 95% CI: 0.40 to 0.76). Nonetheless, after adjusting for the academic year, age, sex, postgraduate year, monthly emergency duties, assigned inpatients, daily self-study time, hospital area, and annual ambulance volume, it was observed that the weekly duty hours of university hospital residents did not show a reduction (OR, 0.86; 95% CI: 0.67 to 1.10).
Table 4 presents the distributions of other variables along with the rest of the multivariate model estimates to evaluate the factors associated with duty hours. PGY-2 residents had reduced duty hours (OR, 0.93). Resident educational metrics, such as the number of inpatients assigned, monthly emergency duty shifts, and daily self-study duration, were directly correlated with extended work hours. For every 1,000 increases in the annual ambulance volume at the training hospital, resident work hours increased by an ORs of 1.26. Duty hours showed no discernible association with age, sex, or hospital location.
Discussion
Japan has been undergoing nationwide workplace reforms that began in 2019, with specific reforms targeting resident duty hours ahead of the introduction of working-hour restrictions in 2024. In this context, we analyzed historical data from 17,967 residents over four years (2019–2022), focusing on weekly duty hours and training environment, particularly by hospital type. Overall, residents’ duty hours were found to increase from 2019 to 2021, before declining in 2022. Of particular concern was the growing number of residents working fewer than 50 h per week, alongside reductions in their self-study hours and the number of inpatients under care. By 2022, the proportion of residents responsible for managing zero to four hospitalized patients had risen by over 20%. These findings highlight significant changes in residents’ workload as Japan progresses toward duty-hour restrictions.
Trends of resident duty hours
The observed pattern in resident duty hours indicated an increase from 2019 to 2021, followed by a decrease in 2022. The escalation in duty hours during the initial three years deviated from expectations with multiple potential explanations. First, a redefinition of resident duty hours emerged because of work-style reforms. The MHLW stated that self-learning—jiko-kensan, characterized by residents’ autonomy and exemption from work obligations – did not qualify as working hours19. As a result of these reform guidelines, activities formerly regarded as self-learning (jiko-kensan) may have been reclassified as duty hours if conducted under the direction of supervisors, potentially contributing to an apparent increase in reported working hours19. Second, heightened precision in tracking duty hours might have increased residents’ awareness of their working hours, resulting in a potential recall bias. Third, the COVID-19 pandemic, which emerged in 2020, might have placed additional demands on healthcare institutions, hindering the advancement of workstyle reforms. While reports indicated that Japanese residents were minimally engaged in the direct care of COVID-19 patients, residents’ actual work hours might have been extended due to increased demands on their supervising physicians20,21.
After this upward trajectory, the post-2022 period showed a decline in work hours, which may be attributable to implemented strategies aimed at reducing prolonged work durations among residents, such as the redistribution and reduction of tasks22. However, data from 2022 revealed that approximately 25% of residents are still working over 60 h weekly, exceeding the limits set by the “A-level” work hour regulations. This underscored the need for several residents to further reduce their duty hours in compliance with the new regulations.
Educational impact
This study also highlighted the potential educational consequences of duty-hour restrictions. Over the past four years, reductions were observed in the average number of inpatients assigned to residents, frequency of ED shifts, and duration of daily self-study time. The decline in the number of inpatients under residents’ care is particularly concerning, as clinical exposure is a cornerstone of medical training. The proportion of residents responsible for zero to four inpatients increased from 18% in 2019 to 39% in 2022, with the trend being most pronounced in public university hospitals. By 2022, 50% of residents in public university hospitals reported managing only zero to four inpatients, compared to smaller increases in other hospital types.
While this reduction may alleviate the workload, it also reduces opportunities for clinical skill development and competency-based education. Similar trends have been observed globally, with duty-hour limitations associated with decreased case volumes, particularly in surgical specialties1. However, this contrasts findings from the US, where an 80-hour weekly cap has not significantly affected the caseloads of surgical and internal medicine residents6,23. In Europe, where stricter 48-hour weekly limits are in place, reports of maintained caseloads were less frequent. Japan’s 60-hour cap places its residency programs between the US and European models, underscoring the need for careful monitoring to ensure sufficient clinical exposure while adhering to regulations.
Differences by hospital type
This study examined the duty hours of resident physicians in Japan, specifically by comparing those in university hospitals with their counterparts in community hospitals. While the initial findings indicated shorter duty hours at university hospitals, a trend confirmed by the regression analysis, this discrepancy was not evident when adjusting for resident background and training environment metrics in the multivariate analysis. The primary factors influencing duty hours were the number of inpatients assigned and the number of ED duty shifts per month. This suggests that differences in patient volume may be a key factor contributing to the variation in duty hours between university and community hospitals. Prior studies in Japan have shown that residents in community hospitals typically manage more patients and gain broader clinical exposure compared to those in university hospitals, where the focus tends to be more research-oriented and subspecialized24. These differences are reflected in educational outcomes, with community hospital residents scoring higher on national in-training examinations25. Additionally, Tokuda et al. (2023) reported that, during the COVID-19 pandemic, community hospitals admitted significantly more internal medicine patients per 100 beds than university hospitals, despite similar facility sizes26. Given that university hospitals also tend to have a higher number of residents under Japan’s training system, the combination of greater patient volume and fewer residents per institution in community hospitals may contribute to a higher clinical burden per resident, potentially explaining the observed differences in duty hours.
Implications and future directions
This study identifies two key challenges associated with work-style reforms for medical residents: inadequate reductions in working hours for some groups and potential negative impacts on education, particularly a decrease in the number of assigned patients. Moreover, these issues vary, depending on the hospital type. Community hospitals may struggle to enforce adequate working hour limits, while university hospitals may excessively reduce working hours, potentially failing to maintain the training intensity required for effective education. Particularly, concerns have been raised regarding insufficient training opportunities in public university hospitals.
Several policy recommendations can be adopted, based on this study’s findings. First, monitoring the number of patients assigned to residents is crucial. Adequate clinical experience is a cornerstone of successful medical training, yet Japan currently lacks a nationwide system to measure and monitor case volumes27,28. Beyond merely comparing working hours, evaluating whether residents are acquiring sufficient clinical experience and engaging in meaningful educational activities is also essential. Policymakers should consider establishing minimum standards for training intensity, including benchmarks for case volumes and working hours. Second, residents should be optimally utilized in clinical roles. This is particularly pertinent in university hospitals, where residents often report being assigned excessive non-clinical tasks, leading to dissatisfaction with their training experience and reduced clinical exposure29. Furthermore, during the COVID-19 pandemic, it was reported that only about 10% of residents in Japan had sufficient opportunities to provide care to COVID-19 patients, highlighting a missed opportunity for meaningful clinical training20. Third, Japan’s attempt to limit residents’ working hours to 60 h per week represents a unique regulatory approach, positioned between the United States (80 h per week) and European Union (48 h per week) models. Policymakers must acknowledge the limited evidence supporting the appropriateness of this regulation. While it may offer benefits for residents’ health and well-being, the educational consequences of these restrictions must be carefully and thoroughly evaluated. Balancing work hour limitations with adequate clinical exposure is critical to maintaining the quality of medical education and ensuring that reforms achieve their intended goals.
Limitations
This study had some limitations. First, it did not examine the potential benefits of duty-hour restrictions in critical areas such as medical safety, patient outcomes, mental health, and gender equality. While it highlighted the potential educational drawbacks of these restrictions for Japanese residents, a comprehensive assessment incorporating these areas would provide a more holistic view of the impact of the policy. Second, the methodology employed in this study relied on self-reported surveys on duty hours and training environments, which are susceptible to response bias, including recall error and social desirability bias30,31. Residents might report hours that they perceive as socially acceptable rather than their actual duty hours, a tendency previously reported among residents concerned about institutional consequences32. However, previous research has shown negligible differences between self-reported duty hours and those measured by electronic tracking systems or objective logs33. Third, the study’s reporting of outcomes did not account for variability in duty hours across different clinical rotations, instead averaging data over the entire training period. Prior research has shown that resident working hours in Japan vary considerably by specialty, with longer hours and heavier clinical burdens in fields such as surgery, neurosurgery, emergency medicine, and obstetrics/gynecology compared to others34. Therefore, this approach may obscure important differences in workload and training experiences between rotations. Fourth, there is a possibility of selection bias, as the study included only one-third to one-half of all residents in Japan. The participants were candidates for the GM-ITE, and it is likely that participating facilities are more committed to education than nonparticipating ones. Moreover, only 11% of the participants were affiliated with university hospitals, despite nearly one-third of Japan’s medical residents being associated with such institutions35.
Conclusion
This study, using four years of national data, evaluated shifts in residents’ work styles and training environments in anticipation of the duty-hour restrictions that have been in effect since April 2024. While duty hours initially increased, a decline was observed in 2022, although many residents continued to exceed the stipulated limits. The educational consequences of these reforms were particularly evident in university hospitals, where reduced patient loads and limited clinical exposure raised concerns regarding the adequacy of training. Moving forward, striking a balance between enforcing duty-hour limits and ensuring that residents receive sufficient clinical exposure to maintain the quality of medical education is essential. Comprehensive monitoring and targeted interventions are critical to address disparities across hospital types and optimize the impact of duty-hour restrictions on both training and patient care.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to privacy reasons but are available from the corresponding author on reasonable request.
References
Nagasaki, K. & Kobayashi, H. The effects of resident work hours on well-being, performance, and education: A review from a Japanese perspective. J. Gen. Fam Med. 24, 323–333. https://doi.org/10.1002/jgf2.649 (2023).
Temple, J. Resident duty hours around the Globe: where are we now? BMC Med. Educ. 14, S8. https://doi.org/10.1186/1472-6920-14-s1-s8 (2014).
Breuer, R. M. et al. Work like a doc: A comparison of regulations on residents’ working hours in 14 high-income countries. Health Pol. 130, 104753. https://doi.org/10.1016/j.healthpol.2023.104753 (2023).
Landrigan, C. P., Barger, L. K., Cade, B. E., Ayas, N. T. & Czeisler, C. A. Interns’ compliance with accreditation Council for graduate medical education work-hour limits. JAMA 296, 1063–1070. https://doi.org/10.1001/jama.296.9.1063 (2006).
Moonesinghe, S. R., Lowery, J., Shahi, N., Millen, A. & Beard, J. D. Impact of reduction in working hours for Doctors in training on postgraduate medical education and patients’ outcomes: systematic review. BMJ (Clinical Res. ed) 342, d1580–d1580. https://doi.org/10.1136/bmj.d1580 (2011).
Drake, F. T., Horvath, K. D., Goldin, A. B. & Gow, K. W. The general surgery chief resident operative experience: 23 years of National ACGME case logs. Jama Surg. 148, 841–847. https://doi.org/10.1001/jamasurg.2013.2919 (2013).
Kansier, N., Varghese, T. K., Verrier, E. D., Drake, F. T. & Gow, K. W. Accreditation Council for graduate medical education case log: general surgery resident thoracic surgery experience. Ann. Thorac. Surg. 98, 459–465. https://doi.org/10.1016/j.athoracsur.2014.04.122 (2014).
Fujikawa, H., Son, D. & Eto, M. Are residents learners or workers? A historical perspective in Japan. Asia Pac. Schol. 6, 122–124. https://doi.org/10.29060/taps.2021-6-1/pv2339 (2021).
Ministry of Health. Labour and Welfare. Survey on physicians’ working conditions and working style intents (2024). https://www.mhlw.go.jp/file/05-Shingikai-10801000-Iseikyoku-Soumuka/0000161146.pdf (in Japanese).
Nagasaki, K. et al. Impact of the resident duty hours on in-training examination score: A nationwide study in Japan. Med. Teach. 21, 1–8. https://doi.org/10.1080/0142159x.2021.2003764 (2021).
Sohn, S. et al. Changes in the working conditions and learning environment of medical residents after the enactment of the medical resident act in Korea in 2015: A National 4-year longitudinal study. J. Educ. Eval. Heal Prof. https://doi.org/10.3352/jeehp.2021.18.7 (2021).
Nagasaki, K., Nishizaki, Y., Shinozaki, T., Kobayashi, H. & Tokuda, Y. Association between resident duty hours and self-study time among postgraduate medical residents in Japan. JAMA Netw. Open. 4, e210782–e210782. https://doi.org/10.1001/jamanetworkopen.2021.0782 (2021).
Nagasaki, K. et al. Association between prolonged weekly duty hours and self-study time among residents: A cross-sectional study. Postgrad. Méd J. 9, 1080–1087. https://doi.org/10.1093/postmj/qgad044 (2023).
Nagasaki, K. et al. Validation of the general medicine in-training examination using the professional and linguistic assessments board examination among postgraduate residents in Japan. Int. J. Gen. Med. 14, 6487–6495. https://doi.org/10.2147/ijgm.s331173 (2021).
Kozu, T. Medical education in Japan. Acad. Med. 81, 1069–1075. https://doi.org/10.1097/01.acm.0000246682.45610.dd (2006).
Japan Residency Matching Program. Matching results of FY2022. (2022). https://www.mhlw.go.jp/content/10803000/001005268.pdf (2022). (in Japanese).
Promotion of Medical Training. Foundation for the Promotion of Medical Training (2024). http://guide.pmet.jp/web2024/php/hosp_srch_input.php (in Japanese).
Healthcare market analysis platform. https://caremap.jp (2024). (in Japanese).
Ministry of Health. Labour and Welfare. Perspectives on physicians’ self-improvement and working hours. (2017). https://www.mhlw.go.jp/content/10800000/000404613.pdf (in Japanese).
Nishizaki, Y. et al. Relationship between COVID-19 care and burnout among postgraduate clinical residents in Japan: A nationwide cross-sectional study. BMJ Open. 13, e066348. https://doi.org/10.1136/bmjopen-2022-066348 (2022).
Hamada, S. et al. Association between hospital internal medicine physician workforce and patient admissions during the COVID-19 pandemic in Japan. BMC Heal Serv. Res. 23, 65. https://doi.org/10.1186/s12913-023-09043-0 (2023).
Koike, S. et al. Working hours of full-time hospital physicians in Japan: a cross-sectional nationwide survey. BMC Public. Health. 24, 164. https://doi.org/10.1186/s12889-023-17531-5 (2024).
Leafloor, C. W. et al. Time-motion studies of internal medicine residents’ duty hours: A systematic review and meta-analysis. Adv. Med. Educ. Pract. 6, 621–629. https://doi.org/10.2147/amep.s90568 (2015).
Yano, E. et al. Comparing postgraduate medical education at university and non-university hospitals in Japan. Acad. Med. 67, 54–58. https://doi.org/10.1097/00001888-199201000-00011 (1992).
Nishizaki, Y. et al. Difference in the general medicine in-training examination score between community-based hospitals and university hospitals: a cross-sectional study based on 15,188 Japanese resident physicians. BMC Med. Educ. 21, 255. https://doi.org/10.1186/s12909-021-02649-0 (2021).
Tokuda, Y. et al. Association between hospital internal medicine physician workforce and patient admissions during the COVID-19 pandemic in Japan. BMC Health Serv. Res. 23, 65. https://doi.org/10.1186/s12913-023-09043-0 (2023).
Kinoshita, K. et al. Impact of inpatient caseload, emergency department duties, and online learning resource on general medicine in-training examination scores in Japan. Int. J. Gen. Med. 8, 355–360. https://doi.org/10.2147/ijgm.s81920 (2015).
Nomura, K. et al. The shift of residents from university to non-university hospitals in Japan: A survey study. J. Gen. Intern. Med. 23, 1105. https://doi.org/10.1007/s11606-008-0644-7 (2008).
McCoy, C. P., Stenerson, M. B., Halvorsen, A. J., Homme, J. H. & McDonald, F. S. Association of volume of patient encounters with residents’ in-training examination performance. J. Gen. Int. Med. 28, 1035–1041. https://doi.org/10.1007/s11606-013-2398-0 (2013).
Althubaiti, A. Information bias in health research: definition, pitfalls, and adjustment methods. J. Multidiscip Healthc. 9, 211–217. https://doi.org/10.2147/JMDH.S104807 (2016).
Podsakoff, P. M. et al. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 88, 879–903. https://doi.org/10.1037/0021-9010.88.5.879 (2003).
Drolet, B. C. et al. Residents’ response to duty-hour regulations—a follow-up National survey. N Engl. J. Med. 368, e33. https://doi.org/10.1056/NEJMsr1214912 (2013).
Todd, S. R. et al. Use of a computerized database to monitor compliance with work-hour regulations. J. Surg. Educ. 67, 182–186. https://doi.org/10.1016/j.jsurg.2010.02.005 (2010).
Takata, A. et al. Work style of junior residents in Japanese red cross hospitals: analysis by specialty and lifestyle controllability. J. Hosp. Admin. 6, 28–36. https://doi.org/10.5430/jha.v6n6p28 (2017).
Council of Matching Program. Statistics of Matching for Post-graduate Training for Physician 2019. https://www.jrmp2.jp/koho/2019/2019kekka_koho.pdf (2006). (in Japanese).
Acknowledgements
We thank members of the JAMEP, the question development committee, and the peer-review committee of the GM-ITE for their assistance. The authors would like to thank Editage (https://www.editage.jp) for the English language editing.
Funding
This work was supported by the Health, Labour and Welfare Policy Grants of Research on Region Medical (21IA2004) from the MHLW.
Author information
Authors and Affiliations
Contributions
Dr Nagasaki had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.Study concept and design: Nagasaki, NishizakiAcquisition, analysis, or interpretation of data: Shimizu, Yamamoto, Shikino, KataokaManuscript drafting: NagasakiCritical revision of the manuscript for important intellectual content: Nishizaki, KobayashiStatistical analysis: NagasakiAdministrative, technical or material support: Nishizaki, TokudaSupervision: Nishizaki, Kobayashi, Tokuda.
Corresponding author
Ethics declarations
Competing interests
Dr. Nishizaki received an honorarium from JAMEP as GM-ITE project manager. Dr. Tokuda is the JAMEP director, and he received an honorarium as a speaker of the JAMEP lecture. Dr. Kobayashi and Dr. Shikino received an honorarium as a speaker of the JAMEP lecture. Dr. Shimizu, Dr. Yamamoto, and Dr.Shikino received honorariums from JAMEP as exam preparers of GM-ITE. Dr. Nagasaki and Dr. Kataoka have no conflicts of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nagasaki, K., Nishizaki, Y., Shimizu, T. et al. Educational environment changes toward resident duty hour restrictions in Japan. Sci Rep 15, 16925 (2025). https://doi.org/10.1038/s41598-025-00347-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-00347-1