Abstract
To evaluate the effects of an endoscopic aqueous environment on the viability and differentiation capacity of autologous bone marrow mesenchymal stem cells (MSCs) enriched with β-tricalcium phosphate (β-TCP). A screening-enrichment-combination circulating system (SECCS) was used to prepare MSCs/β-TCP from a patient. A simulated aqueous flushing environment for spinal endoscopic surgery was established with different flushing times (0–60 min). Scanning electron microscopy (SEM) was employed to determine the adhesion and condition of MSCs/β-TCP. CCK-8 was used to determine the viability of adherent MSCs. The osteogenic, adipogenic, and chondrogenic differentiation potentials of adherent MSCs were assessed with alizarin red, alkaline phosphatase, Oil Red O, and toluidine blue staining. A subcutaneous implantation mouse model was utilized to evaluate the osteogenic capacity of MSCs/β-TCP under different aqueous flushing conditions using micro-CT, haematoxylin–eosin staining, and Von Kossa staining. SEM revealed sustained MSC adhesion on β-TCP across all irrigation durations (0–60 min), with no differences in adhesion density. However, cell viability declined significantly after 30 min(P < 0.05). Differentiation assays demonstrated time-dependent impairments: osteogenic and adipogenic potentials decreased significantly at 30 min (P < 0.05), chondrogenic morphology disorganized after 15 min, while ALP activity declined only at 60 min (P < 0.05). In vivo, irrigation > 15 min markedly reduced bone formation (P < 0.05) and parallel reductions in mineralized matrix(P < 0.05). In summary, prolonged irrigation (> 15 min) in the spinal endoscopic aqueous environment compromises MSC/β-TCP adhesion and osteogenic capacity. Optimizing surgical efficiency and strictly controlling the irrigation time and pressure are critical in preserving graft performance for successful bone fusion.
Similar content being viewed by others
Introduction
Lumbar interbody fusion (LIF) is a widely recognized surgical method utilized for addressing various degenerative spinal conditions1. In an effort to reduce surgical trauma, researchers have concentrated on endoscopic techniques for performing lumbar fusion, which include transforaminal endoscopic LIF (TE-LIF), endoscopic assisted LIF (Endo-ALIF), and unilateral biportal endoscopy-TLIF (UBE-TLIF)2,3,4,5. These methods have been developed as minimally invasive options compared to conventional open surgery for degenerative spinal issues, resulting in less tissue trauma and faster recovery times. A defining feature of these procedures is the application of continuous aqueous irrigation, which facilitates better visualization and preparation of the endplates, an essential component for achieving successful fusion6. Nonetheless, this aquatic environment may unintentionally compromise the bone graft materials inserted into the intervertebral space.
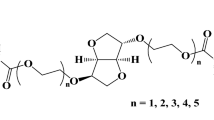
Autologous bone is widely regarded as the premier graft material for lumbar fusion; however, it frequently proves inadequate in endoscopic procedures due to its limited capacity for decompression. Common alternatives include allogeneic bone, xenogeneic bone, and synthetic bone. Scaffolds made from β-tricalcium phosphate (β-TCP) exhibit both osteoconductivity and biocompatibility, although they require osteogenic augmentation. The integration of mesenchymal stem cells (MSCs) with β-TCP helps to meet this requirement7,8. Nonetheless, stem cells make up a very small portion of the bone marrow, and acquiring adequate amounts of these cells is a major challenge limiting their use in clinical settings. Presently, strategies for MSC enrichment mainly involve harvesting autologous bone marrow, followed by techniques like centrifugation, flow cytometry sorting, or in vitro culture expansion9,10. However, these methods present considerable difficulties, as they typically demand advanced equipment and specialized skills while also carrying risks of contamination, genetic variability, and ethical concerns11.
Our cooperative group has developed a screening-enrichment-combination circulating system (SECCS) that rapidly enrich autologous MSCs through a closed-loop, nonculture process12,13. Preclinical data have confirmed that SECCS-enriched MSCs/β-TCP retain multipotency and enhance β-TCP-mediated bone regeneration in bone defects12,14,15,16. Recently, Zhao et al. further confirmed that SECCS-derived MSCs/β-TCP achieved superior 3-month fusion rates versus local bone grafts in TLIF procedures (53.8% vs. 28.0%), with the equivalent 12-month fusion of 100% and functional outcomes13. Nevertheless, whether dynamic irrigation inherent to endoscopic surgery poses risks to MSC/β-TCP scaffold integrity remains uncharacterized.
According to the literature and our clinical experience, the average operative duration for full endoscopic spinal fusion procedures typically ranges from 140 to 210 min, influenced by surgical complexity and operator proficiency17,18. In endoscopic LIF, the bone graft materials and cage are typically implanted after discectomy and before the final irrigation19,20,21. Post-implant irrigation durations vary, but average 20–40 min for debris clearance and further decompression. We hypothesized that prolonged irrigation, as encountered in endoscopic spinal surgeries, would mechanically disrupt MSC adhesion to β-TCP and impair their osteogenic potential, thereby contributing to suboptimal bone fusion outcomes. This study aimed to evaluate whether simulated spinal endoscopic irrigation affects the adhesion, viability, and osteogenic capacity of MSC/β-TCP scaffolds and to define time-dependent thresholds for fluid exposure in surgical protocols to optimize graft performance.
Methods
Material preparation
A screening-enrichment-combination circulating system (SECCS) (Shanghai Ninth People’s Hospital Affiliated with Shanghai Jiao Tong University) was used to prepare β-TCP bone material enriched with bone marrow MSCs (MSCs/β-TCP) according to a previously published protocol13. Three healthy male (44–55 years old) surgical donors were selected. Under general anaesthesia, 100 mL of autologous bone marrow was extracted from the anterior superior iliac spine. The SECCS system comprises three main components: (1) a detachable columnar double-layer filter box, which holds the porous biomaterial and facilitates hemofiltration; (2) a sealed pipeline for fluid circulation; and (3) a peristaltic pump that drives the continuous circulation of the bone marrow (Fig. 1A). During the procedure, 10 g of β-TCP particles were loaded into the inner filter box, which was then secured to the outer box. The 100 mL of bone marrow was introduced into the pipeline, and the peristaltic pump was activated to circulate the bone marrow through the porous β-TCP. After 15 min of circulation (60 r/min, 50 Hz), the MSC-enriched β-TCP particles (MSCs/β-TCP composites) were prepared and ready for the experiment. This study was approved by the Medical Ethics Committee of Fujian Medical University Affiliated with Mindong Hospital (2021032503H). All methods were carried out in accordance with relevant guidelines and regulations including the Declaration of Helsinki and local data protection laws and informed consent was obtained from all participants and/or their legal guardians.
Experimental setup, SEM analysis and the viability of MSCs/β-TCP after water medium irrigation. (A) A SECCS system was used to prepare β-TCP bone material enriched with bone marrow MSCs (MSCs/β-TCP), and the experimental setup for water medium irrigation with MSCs/β-TCP is shown. (B) SEM images of β-TCP alone (NC), enriched MSC/β-TCP(PC/0), MSC/β-TCP particles after irrigation for different durations (5, 15, 30, and 60 min), arrows showing MSC cell adhesion and surface morphology. The scale bars represent 5 μm in the top images, 20 μm in the middle images, and 100 μm in the bottom images. (C) Results of the CCK-8 assay of MSC/β-TCP particles after irrigation for different durations (0, 5, 15, 30, and 60 min), showing cell viability (n = 3). *P < 0.05 versus the 0-min group, #P < 0.05 versus the 30-min group.
Experimental treatment and grouping
As shown in Fig. 1A, a 3000 ml saline bag was suspended at a height of approximately 1.7 m to ensure sufficient water flow, generating an irrigation pressure of approximately 2.66–3.99 kPa (flow rate: 100 mL/min, approximately 20–30 mmHg) under operating room temperatures (22–25 °C). The MSC/β-TCP particles were placed in a cup, which was sealed with a rubber membrane, and the inlet and outlet were opened to mimic the water medium irrigation environment under spinal endoscopy. To systematically evaluate the effects of prolonged irrigation, the MSC/β-TCP constructs were categorized into six groups: (1) Negative Control (NC): β-TCP scaffolds alone (without MSCs), irrigated for 0 min to assess the baseline scaffold properties. (2) Positive Control (PC/0): MSC/β-TCP constructs irrigated for 0 min to establish the baseline cellular viability and adhesion. (3) Experimental Groups: MSC/β-TCP constructs irrigated for 5, 15, 30, or 60 min, representing clinically relevant intraoperative exposure periods and extended scenarios to comprehensively assess irrigation-induced impacts.
Assessment of the residual efficacy of BMSCs
For determination of the presence and residual rate of MSCs in MSCs/β-TCP after irrigation in a saline environment, the MSCs/β-TCP from the different groups were gently washed with PBS and then fixed with glutaraldehyde overnight at 4 °C. Following gradual dehydration and metal spraying, cell adhesion was directly observed by scanning electron microscopy (SEM)13.
Assessment of the viability of residual BMSCs
Following aqueous irrigation, MSC/β-TCP particles were gently rinsed with phosphate-buffered saline (PBS; Gibco) to remove nonadherent cells. Adherent cells were then cultured for 24 h before CCK-8 analysis. The cultured cells were quantified by using the CCK-8 assay (Beyotime Biotechnology). Briefly, cells were incubated with 10 μL of the CCK-8 reagent for 2 h at 37 °C, and absorbance of the supernatant was measured at 450 nm on a microplate reader (Tecan Infinite M Nano). Data were normalized to untreated control cells (0-min irrigation group) to calculate relative cell viability.
Determination of the multidimensional differentiation potentials of adherent MSCs/β-TCP
After the MSC/β-TCP particles were rinsed with water, the adherent cells were digested with trypsin (Sigma) and repeatedly washed with PBS. The collected cells were centrifuged to obtain adherent cells, which were then cultured and subjected to osteogenic, adipogenic, and chondrogenic induction assays. Osteogenic differentiation was induced using DMEM supplemented with 10% FBS, 100 nM dexamethasone, 10 mM β-glycerophosphate, and 50 μM ascorbic acid-2-phosphate. For adipogenic differentiation, DMEM supplemented with 10% FBS, 1 μM dexamethasone, 0.5 mM IBMX, 10 μg/mL insulin, and 200 μM indomethacin was utilized. Chondrogenic differentiation was achieved using DMEM supplemented with 1% ITS, 100 nM dexamethasone, 50 μM ascorbic acid-2-phosphate, 40 μg/mL proline, and 10 ng/mL TGF-β3.
-
(1)
Osteogenic induction and staining procedure Cells were incubated in 12-well plates with osteogenic induction medium (HUXMX-90021, Cyagen Biosciences). On the seventh day, after washing with PBS, the cells were fixed with 4% paraformaldehyde for 30 min and subsequently stained with alkaline phosphatase (ALP) staining solution (Solarbio, China) at 37 °C for 30 min, followed by examination under a microscope. On the twenty-first day, similarly, after washing with PBS, the cells were fixed with 4% paraformaldehyde for 30 min and then stained with Alizarin Red S (Cyagen Biosciences) as per the manufacturer’s instructions, followed by microscopic observation. The relative area of staining in the images was assessed via ImageJ software.
-
(2)
Adipogenic induction Cells were seeded into 12-well plates, cultured with adipogenic induction solution A for 3 days, and then switched to adipogenic induction solution B for 1 day (HUXXC-90031, Cyagen Biosciences). On day 21, the cells were washed with PBS, fixed with 4% paraformaldehyde for 15 min, and then washed three times with PBS. The cells were subsequently stained with 0.5 ml of Oil Red O working solution (Cyagen Biosciences) for 30 min, followed by three washes with PBS. The relative staining area of the images was analysed using ImageJ software.
-
(3)
Chondrogenic induction Cells were placed in a 15 ml tube and subjected to centrifugation at 1500 rpm for 5 min to eliminate the supernatant. Following this, 1 ml of chondrogenic induction medium (HUXMX-90041, Cyagen Biosciences) was added, and the cells were incubated for 48 h. The resulting cell pellet was then moved to a fresh tube, with the culture medium being replaced biweekly. On the 28 day, the cell pellet underwent fixation using 4% paraformaldehyde for 15 min, was stained at room temperature for another 15 min with toluidine blue staining solution, and rinsed two times with PBS, retaining a small volume of the PBS for subsequent microscopic examination.
Animal experiment
After the MSCs/β-TCP were irrigated with the water medium for different durations, equal volume samples of MSCs/β-TCP were collected and implanted subcutaneously into the subdermal area of the backs of mice to evaluate the effects of bone fusion. All animal experiments were conducted in strict accordance with protocols approved by the Animal Ethics Committee of Fujian Medical University and followed the ARRIVE guidelines for experimental design. Immunodeficient NOD/SCID mice (n = 30, 12-week-old) received subcutaneous implants of human MSC/β-TCP after the mice were assigned to groups using a random number table. No perioperative mortality occurred. All mice were anesthetized via intraperitoneal injection of 3% sodium pentobarbital (50 mg/kg) and euthanized by cervical dislocation four weeks following subcutaneous implantation. The samples were harvested and scanned by micro-CT. Subsequently, three-dimensional (3D) image reconstruction was carried out to observe new bone formation. Micro-CT scanning software (Bruker SkyScan 1272) was used to determine the percentage of new bone formation.
Histological and histomorphometric analysis
After scanning, samples were obtained after confirming the absence of pain reflexes, and stained with Von Kossa and haematoxylin–eosin (HE) as previously reported22. Non-decalcified samples were embedded at low temperature in PMMA and serial 54 µm sections were stained with 5% silver nitrate (Von Kossa) for 30 min, rinsed with distilled water, and developed with 5% sodium thiosulfate for 2 min. They were counterstained with Nuclear Fast Red for 5 min. HE staining was performed after 4 weeks of fixation and decalcification. The samples were stained with haematoxylin for 8 min, differentiated in 1% acid alcohol, and blued in Scott’s solution. Then, they were counterstained with eosin for 2 min. For histomorphometric measurements, BV/TV was calculated as the ratio of the bone area to the total tissue area using ImageJ.
Statistical methods
The experimental data were meticulously analysed using SPSS 22.0 software. Measurement data are expressed as means ± standard deviations, with three replicates per group (n ≥ 3). The normality of the data was verified by the Shapiro–Wilk test (P > 0.05), and the homogeneity of variance was assessed using Levene’s test. For comparisons between two groups, independent t-tests were employed. When comparing three or more groups, one-way ANOVA was conducted. If the ANOVA results indicated significant differences, multiple comparisons were performed using a Least Significant Difference (LSD) test; otherwise, Dunnett’s t test was utilized. A P value of less than 0.05 was considered to indicate statistical significance.
Results
Effects of water medium irrigation on the adhesion of MSCs/β-TCP
Following MSC enrichment by using the SECCS to generate MSC/β-TCP composites, we employed scanning electron microscopy (SEM) to evaluate the impacts of different durations (0–60 min) of aqueous medium irrigation on cellular adhesion. As shown in Fig. 1B, MSC-enriched β-TCP particles demonstrated significantly enhanced adhesion of bone marrow-derived cells compared with nonenriched β-TCP controls. Notably, prolonged aqueous exposure did not result in significant differences in the cell adhesion density across the irrigation durations (0–60 min).
Effects of water medium irrigation on the viability of MSCs/β-TCP
To assess the impact of aqueous irrigation on cell viability, the CCK-8 assay was performed on adherent MSCs/β-TCP after irrigation for different durations. As shown in Fig. 1C, cell viability remained relatively stable in the 0–15-min groups, with no significant differences observed (0 min: 100.23 ± 2.84%; 5 min: 96.17 ± 1.79%; 15 min: 96.07 ± 2.04%; P > 0.05). However, a marked decline in viability was detected in the 30- and 60-min groups (91.83 ± 2.08% and 78.90 ± 3.22%, respectively; P < 0.05 compared with the control). These results indicate that prolonged irrigation (> 30 min) significantly compromises MSC adhesion and survival.
The effect of water medium irrigation on the differentiation potential of MSCs/β-TCP
To further investigate the impact of different durations of water medium irrigation on the differentiation potential of cells in MSCs/β-TCP, we assessed the differentiation potential of bone marrow cells after rinsing with water. The ALP staining results revealed that compared with that in the control group (0 min; 42.46 ± 8.08%), the relative ALP staining areas did not significantly differ among the 5-min (42.99 ± 5.54%), 15-min (41.86 ± 8.25%) and 30-min (41.58 ± 9.51%) groups, but that in the 60-min group (25.89 ± 2.42%) significantly decreased (P < 0.05) (Fig. 2A,B). The Alizarin Red staining results indicated that as the irrigation time increased, the relative staining area decreased over time, without significant differences among the 0-min (35.12 ± 6.79%), 5-min (30.73 ± 8.02%), and 15-min (28.54 ± 3.17%) groups, but with a significant decrease relative to the 0-min group for the 30-min group (26.78 ± 6.57%) (P < 0.05 vs. 0-min group) and relative to the 0 and 30-min groups for the 60-min group (16.20 ± 5.34%) (*P < 0.05 vs. 0-min group and #P < 0.05 vs 30-min group) (Fig. 2C,D). The Oil Red O staining results also revealed that as the irrigation time increased, the relative staining areas decreased among the 0-min (27.69 ± 3.80%), 5-min (25.19 ± 3.80%), 15-min (26.51 ± 1.18%) and 30-min (23.64 ± 3.58%) groups, with a significant decrease in the 60-min group (14.24 ± 2.61%) (P < 0.05) (Fig. 2E,F), while the number of small oil droplets markedly increased.
Impact of irrigation duration on the biological activities of the MSC/β-TCP composites. (A,B) ALP staining of MSCs/β-TCP at various irrigation times (0, 5, 15, 30, and 60 min) and quantitative analysis of ALP staining (n = 6). (C,D) Alizarin Red S staining of MSCs/β-TCP at various irrigation times (0, 5, 15, 30, and 60 min) and quantitative analysis of Alizarin Red S staining (n = 6). (E,F) Oil Red O staining of MSCs/β-TCP at various irrigation times (0, 5, 15, 30, and 60 min) and quantitative analysis of Oil Red O staining (n = 6). (G) Toluidine blue staining of MSC/β-TCP particles after irrigation for different durations (0, 5, 15 and 30 min) revealed reduced staining intensity (n = 6). *P < 0.05 versus the 0-min group, #P < 0.05 versus the 30-min group.
In vitro chondrogenic induction experiments revealed that compared with the orderly chondrogenic morphology in the control group, the chondrogenic formation became disordered after 15 min of irrigation, with reduced staining intensity, and this effect was more pronounced at 30 min (Fig. 2G).
The effect of water medium irrigation on the osteogenic potential of MSCs/β-TCP in vivo
To further evaluate the in vivo osteogenic capacity of MSCs/β-TCP under different irrigation durations, subcutaneous implantation models were analysed via micro-CT and histology. As shown in Fig. 3A, micro-CT reconstructions demonstrated progressive reductions in new bone formation with an extended irrigation time. Quantitative analysis (Fig. 3B) revealed a time-dependent decline in the bone volume/total volume (BV/TV) ratio as follows: the 0-min group exhibited a BV/TV ratio of 54.33 ± 6.03%, followed by 52.00 ± 3.00% at 5 min, a significant decrease to 33.33 ± 7.64% at 15 min (*P < 0.05 vs. the 0-min group and &P < 0.05 vs. the 5-min group), and a further reduction to 19.33 ± 5.13% at 30 min (*P < 0.05 vs. the 0-min group and #P < 0.05 vs. the 15-min group). These results indicate that irrigation beyond 15 min markedly inhibits osteogenesis in vivo.
Impact of the duration of water medium irrigation on the osteogenic capacity of MSCs/β-TCP in vivo. (A,B) Micro-CT images of MSC/β-TCP particles after irrigation for different durations (n = 6). (C,D) Von Kossa staining of MSC/β-TCP particles after irrigation for different durations, which revealed a decrease in mineralization (BV/TV) with an increasing irrigation time (n = 6). (E,F) HE staining of MSCs/β-TCP particles after different irrigation durations, indicating a reduction in BV/TV with longer irrigation (n = 6). *P < 0.05 versus the 0-min group, #P < 0.05 versus the 5-min group.
Similarly, Von Kossa and HE staining (Fig. 3C–F) corroborated these findings. The results of Von Kossa staining (Fig. 3C–D) indicated a gradual reduction in the deposition of mineralized matrix over time, specifically as follows: 55.33 ± 5.86% at 0 min, 56.67 ± 8.50% at 5 min (with no significant difference compared to 0 min), while there was a significant decrease to 34.33 ± 3.21% at 15 min (*P < 0.05 vs. the 0-min group and &P < 0.05 vs. the 5-min group), and a further reduction to 11.67 ± 3.51% at 30 min (*P < 0.05 vs. the 0-min group and #P < 0.05 vs. the 15-min group). Additionally, HE staining (Fig. 3E,F) also demonstrated a decrease in BV/TV in the group analysed at 15 and 30 min (32.00 ± 6.56% and 19.00 ± 3.00 compared to 49.67 ± 7.23% in the 0-min group) (*P < 0.05 vs. the 0-min group, &P < 0.05 vs. the 5-min group and #P < 0.05 vs. the 15-min group), findings that align with the results of the Von Kossa staining. Overall, the results indicate that prolonged irrigation beyond 15 min significantly undermines the osteogenic function of MSCs/β-TCP in vivo, presumably because of decreased cellular viability and hindered mineralization prospects.
Discussion
Failure of lumbar fusion can result in potential complications such as failure of internal fixation, adjacent segment disease, persistent low back pain, neurological symptoms, and pseudoarthrosis, all of which can adversely affect the long-term efficacy of the surgery23,24. Increasing the lumbar fusion rate has become a focal point of research in lumbar surgery, and the materials used for the fusion cage and the interbody bone graft are key factors that influence successful fusion25,26,27. Current research focuses on increasing the osteogenic efficacy of artificial bone substitutes by incorporating mesenchymal stem cells (MSCs) and β-TCP to optimize bone material modification12,14,28. In this study, we demonstrated that prolonged aqueous irrigation during simulated endoscopic spinal surgery significantly impacted the osteogenic capacity of MSC/β-TCP composites. Although cell adhesion remained robust up to 60 min of irrigation (SEM data), the osteogenic, adipogenic, and chondrogenic differentiation potentials declined progressively, with marked reductions at 60 min. In vivo, micro-CT and histological analyses confirmed diminished bone formation and mineralization under extended irrigation for more than 15 min. Our results contrast those of static or nonirrigated models in which MSCs/β-TCP exhibited robust osteogenicity12,14.
Based on the results, we emphasize an important time-sensitive threshold (< 15 min) for maintaining MSC/β-TCP functionality in surgical environments abundant in fluids. Although earlier in vitro research recognized MSC-seeded β-TCP as a promising bone substitute25,26,27, no prior investigation addressed the influence of dynamic irrigation, a vital factor for its wider clinical application. While no clinical studies have directly correlated the irrigation duration with fusion rates, our data suggest that prolonged exposure (> 30 min) reduces MSC viability, potentially contributing to reported fusion rates of 72.70–85.30% in certain studies utilizing endoscopic LIF18,29. Future studies should track intraoperative irrigation times and confirm MSC retention. From a clinical standpoint, this research highlights the necessity to refine surgical procedures during endoscopic fusion to achieve a balance between operational efficiency and graft effectiveness6,30.
To date, few studies have reported the mechanisms affecting MSC adhesion or osteogenic differentiation directly in the water medium environment. Continuous irrigation under endoscopy creates a locally closed, high-pressure water environment. This unique microenvironment and the various mechanical forces generated may be key factors affecting MSC/β-TCP activity, including cell adhesion and differentiation25,31. Continuous irrigation generates hydrodynamic forces that may disrupt MSC/β-TCP adhesion. Moreover, prior studies have suggested that shear stress activates mechanosensitive pathways (e.g., the YAP1/NFAT2 pathway) to promote stem cell differentiation32,33. Continuous water flushing creates a low-temperature, dynamically changing oxygen concentration environment, which substantially impacts MSC osteogenic differentiation. Transient cyclic pressure may promote osteogenesis, yet sustained high pressure in a closed endoscopic space might induce cellular stress or apoptosis. The fluid in the endoscopic aqueous environment is typically maintained at room temperature, and continuous in vivo washing can significantly reduce the local temperature, potentially altering MSC metabolism. However, some studies proposed that short-term low-temperature stimulation might increase MSC activity and the differentiation potential34. Moreover, further research is needed to determine the specific effects in vivo. Similarly, previous studies have shown that a transient hypoxic environment can optimize the regenerative and therapeutic potential of MSCs, but severe or prolonged hypoxia may lead to functional loss35. These potential mechanisms align with our results, demonstrating that adipogenic and chondrogenic lineages, which are more sensitive to mechanical and metabolic stressors, showed earlier declines than did the osteogenic lineage.
However, this study has several limitations. First, the flow rates, pressure, and temperatures in our in vitro system may not fully replicate intraoperative conditions, which limits direct clinical extrapolation. Second, while we observed functional declines in MSCs/β-TCP, the specific signalling cascades (e.g., apoptosis, oxidative stress, or immunogenicity) that mediate these effects remain unvalidated, and the detailed molecular mechanisms require further study. Transcriptomic/proteomic profiling of irrigated MSCs will help clarify molecular drivers of their dysfunction. Finally, the long-term clinical impacts of irrigation on bone remodelling and graft integration still need further investigation.
In summary, this study provides valuable insights into the effects of water medium irrigation on the adhesion, viability, and differentiation capacities of MSC/β-TCP bone particles. To mitigate irrigation-related MSC loss, surgeons may consider minimizing the irrigation time (< 15 min) after MSC/β-TCP implantation, using lower flow rates during critical implantation phases, or pre-treating β-TCP with adhesion-enhancing coatings (e.g., fibronectin) before MSC/β-TCP implantation. Future research will focus on a more comprehensive evaluation of the biological characteristics of cells after water medium irrigation and explore potential cell protection measures to promote the clinical application of MSC/β-TCP bone particles in endoscopic lumbar fusion surgery.
Data availability
All the data generated or analyzed during this study are included in this published article and are available from the corresponding author upon reasonable request.
References
Kim, Y. H. et al. Lumbar interbody fusion and osteobiologics for lumbar fusion. Asian Spine J. 16(6), 1022 (2022).
Eum, J. H. et al. Endoscopic extreme transforaminal lumbar interbody fusion with large spacers: A technical note and preliminary report. Orthopedics 45(3), 163–168 (2022).
Kim, H. S., Wu, P. H., Raorane, H. D. & Jang, I. T. Generation change of practice in spinal surgery: Can endoscopic spine surgery expand its indications to fill in the role of conventional open spine surgery in most of degenerative spinal diseases and disc herniations: A study of 616 spinal cases 3 years. Neurol. India 68(5), 1157–1165 (2020).
Pholprajug, P., Kotheeranurak, V., Liu, Y. & Kim, J. S. The endoscopic lumbar interbody fusion: A narrative review, and future perspective. Neurospine 20(4), 1224 (2023).
Ding, Y. et al. Comparison of efficacy and safety between unilateral biportal endoscopic transforaminal lumbar interbody fusion versus uniportal endoscopic transforaminal lumbar interbody fusion for the treatment of lumbar degenerative diseases: A systematic review and meta-analysis. BMC Musculoskeletal Disord. 25(1), 1037 (2024).
Nakajima, D. & Lim, Wu. Full-endoscopic posterior lumbar interbody fusion: A review and technical note. World Neurosurg. 189, 418–427 (2024).
Gan, Y. et al. The clinical use of enriched bone marrow stem cells combined with porous beta-tricalcium phosphate in posterior spinal fusion. Biomaterials 29(29), 3973–3982 (2008).
Re, F., Borsani, E., Rezzani, R., Sartore, L. & Russo, D. Bone regeneration using mesenchymal stromal cells and biocompatible scaffolds: A concise review of the current clinical trials. Gels 9(5), 389 (2023).
Pierini, M. et al. Efficient isolation and enrichment of mesenchymal stem cells from bone marrow. Cytotherapy 14(6), 686–693 (2012).
Gaul, B. & Hoenecke, D. A review of commercially available point-of-care devices to concentrate bone marrow for the treatment of osteoarthritis and focal cartilage lesions. Cartilage 10(4), 387–394 (2019).
Sanchez-Guijo, F. et al. Current challenges in cell and gene therapy: A joint view from the European committee of the international society for cell & gene therapy (ISCT) and the European society for blood and marrow transplantation (EBMT). Cytotherapy 26(7), 681–685 (2024).
Zhuang, Y. et al. A novel cytotherapy device for rapid screening, enriching and combining mesenchymal stem cells into a biomaterial for promoting bone regeneration. Sci. Rep. 7(1), 15463 (2017).
Ding, B., Wang, X., Zhao, C. & Zhao, J. Rapid preparation of bioactive composites for transforaminal lumbar interbody fusion. Sci. Rep. 15(1), 4715 (2025).
Chu, W. et al. Mesenchymal stem cells and porous β-tricalcium phosphate composites prepared through stem cell screen-enrich-combine (− biomaterials) circulating system for the repair of critical size bone defects in goat tibia. Stem Cell Res. Ther. 9, 1–12 (2018).
Chu, W. et al. Comparison and characterization of enriched mesenchymal stem cells obtained by the repeated filtration of autologous bone marrow through porous biomaterials. J. Transl. Med. 17, 1–16 (2019).
Chu, W. et al. Use of a novel screen–enrich–combine (-biomaterials) circulating system to fill a 3D-printed open Ti6Al4V frame with mesenchymal stem cells/β-tricalcium phosphate to repair complex anatomical bone defects in load-bearing areas. Ann. Transl. Med. 9(6), 454 (2021).
Nakajima, Y., Takaoki, K., Akahori, S., Motomura, A. & Ohara, Y. A review of fully endoscopic lumbar interbody fusion. J. Minim. Invas. Spine Surg. Techn. 8(2), 177–185 (2023).
Li, Y. et al. Full-endoscopic posterior lumbar interbody fusion via an interlaminar approach versus minimally invasive transforaminal lumbar interbody fusion: A preliminary retrospective Study. World Neurosurg. 144, e475–e482 (2020).
Yang, L. et al. Full-endoscopic posterior lumbar interbody fusion for the treatment of lumbar degenerative diseases: A technical note with 2-year follow-up. J. Orthop. Surg. Res. 20(1), 286 (2025).
Ishihama, Y. et al. Full-endoscopic trans-kambin triangle lumbar interbody fusion: Surgical technique and nomenclature. J. Neurol. Surg. Part A: Central Eur. Neurosurg. 83(04), 308–313 (2022).
Sharma, C. & Jain, S. Full endoscopic lumbar transforaminal interbody fusion in DDD lumbar degenerative disc disease: A latest technique. Int. J. Spine Surg. 14(s4), S71–S77 (2021).
Ferreira, M. M. et al. Doping β-TCP as a strategy for enhancing the regenerative potential of composite β-TCP: Alkali-free bioactive glass bone grafts. Experimental study in rats. Materials 12(1), 4 (2018).
Yu, Y., Robinson, D. L., Ackland, D. C., Yang, Y. & Lee, P. V. S. Influence of the geometric and material properties of lumbar endplate on lumbar interbody fusion failure: A systematic review. J. Orthop. Surg. Res. 17(1), 224 (2022).
Ye, Hu. & Zhang, Xu. Impact of lumbar interbody fusion surgery on postoperative outcomes in patients with recurrent lumbar disc herniation: Analysis of the US national inpatient sample. J. Clin. Neurosci. 70, 20–26 (2019).
Gao, Q. et al. Biomaterials regulates BMSCs differentiation via mechanical microenvironment. Biomater. Adv. 157, 213738 (2024).
Stamnitz, K. Mesenchymal stem cells, bioactive factors, and scaffolds in bone repair: From research perspectives to clinical practice. Cells 10(8), 1925 (2021).
Meng, B. & Burton, W. Lumbar interbody fusion: Recent advances in surgical techniques and bone healing strategies. Eur. Spine J. 30(1), 22–33 (2021).
Cho, S. et al. Preclinical study of human bone marrow-derived mesenchymal stem cells using a 3-dimensional manufacturing setting for enhancing spinal fusion. Stem Cells Transl. Med. 11(10), 1072–1088 (2022).
Ao, S. et al. Comparison of Preliminary clinical outcomes between percutaneous endoscopic and minimally invasive transforaminal lumbar interbody fusion for lumbar degenerative diseases in a tertiary hospital: Is percutaneous endoscopic procedure superior to MIS-TLIF? A prospective cohort study. Int. J. Surg. 76, 136–143 (2020).
Shen, X. et al. Early result of percutaneous full-endoscopic transforaminal lumbar interbody fusion in the treatment of single-level lumbar degenerative diseases: A retrospective study. Neurosurg. Rev. 47(1), 115 (2024).
Ghasemzadeh-Hasankolaei, M., Pinto, C. A., Jesus, D., Saraiva, J. A. & Mano, J. F. Effect of high cyclic hydrostatic pressure on osteogenesis of mesenchymal stem cells cultured in liquefied micro-compartments. Mater. Today Bio 23, 100861 (2023).
Zhou, Y. et al. Fluid shear force and hydrostatic pressure jointly promote osteogenic differentiation of BMSCs by activating YAP1 and NFAT2. Biotechnol. J. 19(4), 2300714 (2024).
Abbasloo, F., Vahidi, B., Khani, M. M., Sigaroodi, F. & Sarbandi, R. R. Osteogenic differentiation of mesenchymal stem cell on poly sorbitol sebacate scaffold under shear stress in a bioreactor. Tissue Cell 93, 102715 (2025).
Choudhery, M. S. Strategies to improve regenerative potential of mesenchymal stem cells. World J. Stem Cells 13(12), 1845 (2021).
Antebi, B. et al. Short-term physiological hypoxia potentiates the therapeutic function of mesenchymal stem cells. Stem Cell Res. Ther. 9, 1–15 (2018).
Acknowledgements
We would like to acknowledge the participants enrolled in this study. We gratefully acknowledge the help provided by the team of Dr. An Qin, Jie Zhao and Yaokai Gan from the Orthopedics Department of the Ninth Affiliated Hospital of Shanghai Jiao Tong University during this study.
Funding
This study was financially supported by several grants, the Fujian Provincial Natural Science Foundation (Nos. 2021J011452 and 2022J011513), the Qihang Foundation of Fujian Medical University (No. 2020QH1341) and the Ningde Natural Science Foundation (Nos. 2022J04 and 2022J010).
Author information
Authors and Affiliations
Contributions
Conceptualization: Wugui Chen, Guangfeng Ling, Chengzhao Liu; Data curation:Wugui Chen, Guangfeng Ling, Konging Chen, Shijie Chen, Yuchao Ye; Formal analysis: Chengzhao Liu, Chengshou Lin, Konging Chen, Hengmei Chen; Funding acquisition:Wugui Chen, Guangfeng Ling, Chengzhao Liu; Methodology:Wugui Chen, Guangfeng Ling, Konging Chen; Project administration: Wugui Chen, Chengzhao Liu; Writing-original draft: Wugui Chen, Guangfeng Ling, Kongning Chen; Writing-review & editing: Wugui Chen, Chengshou Lin, Chengzhao Liu.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication (from patients/participants)
Consent for publication was obtained from the patient and approved by all the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, W., Ling, G., Lin, C. et al. Prolonged irrigation time in endoscopic aqueous medium impairs MSC/β-TCP adhesion and osteogenic potential. Sci Rep 15, 19976 (2025). https://doi.org/10.1038/s41598-025-01340-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01340-4