Abstract
To explore the current status of nutrition knowledge, attitude, and practice (KAP) among maintenance hemodialysis (MHD) patients in Anhui province in China and identify the influencing factors, providing a scientific basis for nutritional management in MHD patients. From September to October 2022 and February to March 2025, a comprehensive survey was conducted among 772 MHD patients sourced from 20 hemodialysis hospitals situated within the Anhui province in China. This survey encompassed the KAP Questionnaire, in conjunction with a general information survey. Latent profile analysis (LPA) was employed to identify potential categories of nutritional KAP among patients. Chi-square tests and multivariate logistic regression were used to analyze the distribution differences and influencing factors among different KAP categories. A total of 740 valid questionnaires were collected with a response rate of 95.9% (740/772). LPA divided the patients’ nutritional KAP scores into three categories: low KAP group (40 patients, 5.41%), moderate KAP group (564 patients, 76.21%), and high KAP group (136 patients, 18.38%). Significant differences were observed in age, education level, dialysis cause, number of non-renal diseases, exercise, smoking, visiting the hospital alone, sleep duration, nursing status, albumin, hemoglobin, and sarcopenia among the different KAP categories. Multivariate logistic regression analysis indicated that independent factors affecting the nutritional KAP classification of MHD patients included education level, hemoglobin, physical exercise, and sleep duration. MHD patients exhibit distinct nutritional KAP profiles influenced by modifiable factors. Clinically, tailored interventions—such as simplified education and practice-focused support for Low and Moderate KAP Group—should address these subgroups’ unique needs. This paper’s limitations are its cross-sectional design, regional sampling bias in Anhui province.
Similar content being viewed by others
Introduction
The 2020 Annual Data Report from the United States Renal Data System indicates that the incidence of end-stage renal disease is 15%, with a notable 37% increase in all-cause mortality among hemodialysis patients compared to 20171. As a common renal replacement therapy, maintenance hemodialysis (MHD) is widely employed in the treatment of end-stage chronic kidney disease patients. While MHD effectively removes some metabolic waste and excess fluid, it cannot fully replicate normal kidney function and often precipitating various complications. One of the most prevalent complications in MHD patients is malnutrition, affecting between 15 and 75% of all individuals undergoing this treatment2,3. Prolonged malnutrition can result in cognitive impairment and significantly reduce quality of life. This issue has garnered attention from scholars worldwide, with current research primarily focusing on nutritional management and medical interventions for these patients. However, there is limited research exploring patients’ own knowledge, practices, and awareness regarding nutrition, as well as the interrelationship among these factors.
Our research team previously developed a comprehensive “nutrition KAP questionnaire” specifically for patients undergoing MHD4. This tool aims to accurately and comprehensively assess MHD patients’ nutritional KAP, thereby aiding in a more thorough understanding and evaluation of the patients. Latent profile analysis (LPA), a person-centered approach, is employed to classify individuals within a population into distinct subgroups based on internal heterogeneity when group classification is unclear5,6. By analyzing the scores across various items on the questionnaire, LPA identifies latent traits and determines the proportion of individuals within each subgroup. LPA has demonstrated its capability to identify latent traits in various health contexts, such as PTSD symptoms among UK veterans seeking treatment7 and depression and anxiety among adolescents8. LPA was also utilized to determine latent classes and traits of innovative behavior among clinical nurses, as well as to examine predictors relevant to different profiles9. This method has been widely applied in nursing education and management10,11,12. Nevertheless, the utilization of the LPA method for the stratification of nutritional KAP scores and the identification of influencing factors among patients undergoing MHD remains undocumented. This methodological approach facilitates a more nuanced comprehension of the heterogeneous nutritional profiles present within the MHD patient cohort, thereby enabling the identification of distinct subgroups that could potentially benefit from tailored interventions.
In this study, we apply LPA for the first time to assess the nutrition-related KAP of MHD patients across twenty hemodialysis hospitals in Anhui province in China, categorizing the patients into different groups. We aim to identify the influencing factors for each subgroup, providing a scientific basis for tailored nutritional education, attitude improvement, and practices modification interventions, ultimately offering precision care strategies for MHD patients with varying characteristics.
Methods
Study subjects
From September to October 2022 and February to March 2025, a convenience sampling approach was employed to recruit a total of 772 patients with maintenance hemodialysis (MHD) from twenty hemodialysis hospitals (Table S1) located in the region of Anhui province in China. Inclusion criteria for the study were as follows: (1) Patients who had undergone regular hemodialysis treatment for more than three months; (2) Patients without cognitive impairment and able to communicate normally. The cognitive assessment task requires participants to immediately recall five unrelated words (banana, white, car, sun, coffee) verbally presented by the examiner, with correct recall of three or more items constituting the threshold for normative cognitive performance13; (3) Patients who voluntarily agreed to participate in the questionnaire survey; (4) Patients undergo hemodialysis sessions at least twice each week. Exclusion criteria included: (1) Patients with recent significant changes in health conditions such as gastrointestinal bleeding or infections; (2) Post-surgery cancer patients or those living with cancer. Sample size calculation: For LPA, it is recommended that each latent category contains at least 50 samples, with an assumption that this study may have up to six latent categories (most studies have fewer than six categories)5,6,9,10,11,12, resulting in a minimum sample size of 300. The sample size for multinomial logistic regression should be more than 10 to 15 times the number of independent variables. Hence, with 32 variables, the sample size should be greater than 320. Given a 20% exclusion rate for invalid questionnaires, the sample size was estimated to be more than 400. This study were performed in accordance with the Declaration of Helsinki and the ethical approval was granted by the Ethics Committee of Lu’an People’s Hospital (Number: 2019LL045) and the informed consent was obtained from all subjects.
Research methods
General information
Based on the design of this study and a review of relevant literature, a general information questionnaire was developed to capture the participants’ basic sociodemographic and clinical indicators. These include gender, age, smoking/alcohol history, marital status, sleep duration, education level, place of residence, household income, living arrangements, whether the patient visits the hospital alone, number of comorbidities, cause/duration/frequency of dialysis, number of non-renal diseases, physical exercise habits, red blood cell count, hemoglobin levels, blood calcium, transferrin, BMI, blood potassium, blood phosphorus, prealbumin, albumin, total cholesterol, C-reactive protein, and pre- and post-dialysis urea levels.
Nutrition KAP questionnaire for MHD patients
Using the nutrition KAP questionnaire for MHD Patients, which was developed by our research team in earlier studies4 based on the KAP theory. The overall Cronbach’s α coefficient for the questionnaire is 0.853, test–retest reliability is 0.880, and content validity is 0.981. The questionnaire includes three dimensions with a total of 29 items: (1). The knowledge dimension comprises 11 items, with each item assigned a value of 5 points for correct responses and 0 points for incorrect responses. Consequently, the total score for the knowledge dimension ranges from 0 to 55 points. (2). Attitude dimension includes 8 items. Using a Likert-5 scale, responses range from “strongly willing” (5 points) to “strongly unwilling” (1 point), with a score range of 8–40 points. (3). The practices dimension is comprised of 10 items, with responses measured on a 5-point Likert scale ranging from “never” (1 point) to “always” (5 points). Consequently, the scores for the practices dimension span from 10 to 50 points. The total KAP score ranges from 18 to 145 points, with higher scores indicating better nutrition-related KAP. Table S2 provides a detailed list of items of the nutrition KAP questionnaire.
Nutritional risk screening
The Nutritional Risk Screening 2002 (NRS 2002) scale is a nutritional risk assessment tool developed based on 128 randomized controlled studies, with its reliability and validity well established14. The assessment includes three components: nutritional status score (1–3 points), severity of disease score (1–3 points), and an age score (an additional point for individuals over 70 years). The total score ranges from 2 to 7 points. A score of ≥ 3 indicates a risk of malnutrition, while a score of less than 3 suggests no risk of malnutrition.
Sarcopenia risk assessment scale
The Sarcopenia Risk Assessment (SARC-F) scale15, developed by Malmstrom et al., was used in this study with the Chinese version translated and validated by Huang Lijie et al.16. The Cronbach’s α coefficient of the SARC-F scale is 0.849. The SARC-F scale assesses five key factors: strength, assistance in walking, rising from a chair, climbing stairs, and falls. Each question is scored from 0 to 2, with a maximum total score of 10. A total score of ≥ 4 indicates a positive screening result, diagnosing the patient with sarcopenia.
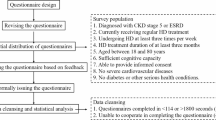
Data collection and quality control
Before the survey, a dedicated investigation team was established at each dialysis hospital, and all investigators received standardized training from the researchers. Questionnaires were distributed through the mobile survey platform Wenjuanxing, with each IP address restricted to one response and a minimum response time set at 5 min. For patients unable to use mobile devices, paper questionnaires were provided. Investigators closely monitored the entire survey process in real time, offering timely assistance to patients if needed, ensuring the authenticity of the data and the reliability of the questionnaires. A total of 772 questionnaires were distributed, with 740 valid responses collected, yielding an effective response rate of 95.9%.
Statistical analysis
Data entry was performed using EpiData 3.1 software by two individuals working in parallel, followed by consistency testing. Statistical analysis and descriptive statistics were conducted using SPSS 25.0. Normally distributed quantitative data were expressed as mean ± standard deviation. Categorical data were described using frequencies and proportions, and the chi-square test was applied to examine distribution differences. A P-value of less than 0.05 was considered statistically significant.
Latent Profile Analysis (LPA), a statistical approach for grouping individuals with similar characteristics, was utilized with Mplus 8.0 to classify the KAP scores of MHD patients into different potential categories. The process of LPA involves initiating with a one-class model and successively adding more classes, with parameters calculated for each model. The optimal model was selected based on fit indices, including Akaike information criterion (AIC), Bayesian information criterion (BIC), and adjusted Bayesian information criterion (ABIC)-with smaller values indicating better model fit. Entropy values, ranging from 0 to 1, were used to assess precision, with values closer to 1 indicating higher accuracy. The Lo-Mendell-Rubin (LMR) and Bootstrapped Likelihood Ratio Test (BLRT) were used for model comparisons, with significance (P < 0.05) indicating that the K-class model had a better fit than the K-1 class model. Chi-square tests were applied to compare the distribution differences in KAP scores across different latent profiles of MHD patients. Multivariate logistic regression was used to analyze the influencing factors of different latent profiles in the KAP scores.
Results
Demographic characteristics
Among the 740 MHD patients, 452 were male (61.1%) and 288 were female (38.9%). The primary causes of dialysis were chronic nephritis or kidney cysts for 332 patients (44.9%), and diabetes or hypertension for 329 patients (44.5%). Among the patients, 155 (20.9%) tested positive for sarcopenia, and 130 patients (17.6%) were at risk of malnutrition. Details are shown in Table 1.
Nutrition KAP scores
The total score range for the nutrition KAP questionnaire for MHD patients was 43 to 145, with an average score of 103.06 ± 19.30. The average item score was 3.55 ± 0.67. The scores for the three dimensions—knowledge, attitude, and practice—are detailed in Table 2. Among these three dimensions, the three items with the highest error rates and the lowest scoring rates are listed in Table 3. In clinical practice, standard body weight calculations are essential for evaluating malnutrition and obesity, while abnormal serum calcium levels can lead to complications like renal osteodystrophy and parathyroid dysfunction. High salt intake negatively impacts blood pressure and increases cardiovascular risks. Patients often avoid consulting registered dietitians and rely on unverified diets, worsening chronic disease management, particularly with protein intake and electrolyte imbalances. Resistance to dietary changes, such as high-sodium diets in hypertensive patients and excessive phosphorus in nephropathy, further hinders clinical outcomes. For practice dimension, neglecting key nutritional information on food labels, like sodium and phosphorus content, frequently leads to excessive intake, increasing the risk of complications such as volume overload and secondary hyperparathyroidism. Additionally, low physical activity is strongly linked to obesity, sarcopenia, and muscle loss, which may lead to chronic issues like osteoporosis and metabolic syndrome, worsening overall disease progression.
LPA of nutrition KAP
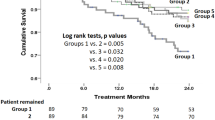
The scores for the three dimensions—knowledge, attitudes, and practices—of the nutrition KAP questionnaire for MHD patients were analyzed using LPA in Mplus 8.0 software. Latent profiles were fitted from one to six groups, labeled as Model 1 through Model 6 (Table 4). As the number of latent profiles increased from Model 1 to Model 6, the AIC, BIC, and ABIC values gradually decreased. However, Model 3 has the highest entropy of 0.911, indicating superior accuracy, and both LMR and BLRT values are below 0.05, signifying it is significantly better than Model 1 and Model 2. Models with 4–6 latent profiles show reduced entropy and a LMR greater than 0.05, demonstrating that Model 3 is more effective. Therefore, the 3-profile model (Model 3) demonstrated the best fit, with probabilities for each profile at 0.762, 0.184, and 0.054, respectively.
The distribution of latent profile characteristics is shown in Fig. 1. Class 1 comprised 136 patients (18.38%), characterized by high scores across all dimensions of knowledge, attitude, and practice, and was labeled the “High KAP Group”. Class 3 included 40 patients (5.41%), with low scores across all dimensions, and was labeled the “Low KAP Group”. Class 2 consisted of 564 patients (76.21%), with scores falling between Class 1 and Class 3, and was labeled the “Moderate KAP Group”. The scores for each profile across the knowledge, attitude, and practice dimensions are presented in Table 5.
Distribution of characteristics among the three latent profiles of nutrition KAP. The analysis of the nutrition KAP questionnaire scores for MHD patients revealed that a three-profile model (Classes 1 to 3) best fit the dimensions of knowledge, attitudes, and practices. Class 1 had 136 patients (18.38%) with high knowledge, attitude, and practice scores, termed the “High KAP Group”. Class 3 included 40 patients (5.41%) with low knowledge, attitude, and practice scores, known as the “Low KAP Group”. Class 2 comprised 564 patients (76.21%) with intermediate scores, referred to as the “Moderate KAP Group”. KAP, Knowledge-Attitude-Practice.
Univariate analysis of different latent profiles of nutrition KAP
Univariate analysis results revealed that in the three latent profiles (High, Moderate, and Low KAP Group) of nutrition KAP scores for MHD patients, variables including age, education level, dialysis cause, number of non-renal diseases, physical exercise, smoking, visiting the hospital alone, sleep duration, nursing status, albumin, hemoglobin, and sarcopenia showed statistically significant differences in distribution across different KAP group (P < 0.05). The details are shown in Table 6.
Multivariate logistic regression analysis of factors influencing different latent profiles of nutrition KAP
Taking the 3 latent profiles (High, Moderate, and Low KAP Group) of nutrition KAP for MHD patients as the dependent variable, and using the factors with statistical significance from the univariate analysis as independent variables, a multivariate logistic regression analysis was conducted. The parallelism test result showed χ2 = 38.770 (P = 0.010), indicating that ordinal logistic regression analysis was not suitable, so multinomial logistic regression analysis was adopted. The results are shown in Table 7. Patients with a high school education or above (OR = 3.341, P = 0.003) and normal hemoglobin level (110–130 g/L) (OR = 4.146, P = 0.032) were more likely to belong to the high KAP group (taken low KAP group as the reference). Patients with higher education levels are more likely to possess comprehensive nutritional management knowledge and demonstrate better adherence to dietary recommendations. Conversely, those with no weekly physical exercise (OR = 0.059, P = 0.020) and less than 5 h of sleep duration (OR = 0.518, P = 0.007) were more likely to fall into the Low KAP Group. Physically inactive hemodialysis patients are more prone to muscle loss and fatigue, hindering their ability to follow nutritional plans. Sleep deprivation worsens this issue by further reducing their adherence to dietary guidelines.
When comparing the moderate KAP group with the Low KAP Group, patients with a high education level (OR = 2.001, P = 0.008) and normal hemoglobin level (110–130 g/L) (OR = 3.652, P = 0.041) were more likely to be in the Moderate KAP Group, anemic conditions coupled with nutritional deficiencies directly compromise patients’ energy reserves and impair health-promoting behavioral capacities. Additionally, when comparing the high KAP group with the Moderate KAP Group, patients with no weekly physical exercise (OR = 0.445, P = 0.003) were more likely to fall into the Moderate KAP Group. Collectively, elevated educational attainment provides foundational knowledge reserves, while regular physical activity reinforces behavioral implementation through enhanced physiological functions (e.g., appetite regulation, metabolic efficiency), synergistically driving KAP enhancement. Notably, normal hemoglobin levels consistently demonstrated associations with High KAP scores, underscoring anemia as a central limiting factor in nutritional management optimization.
Discussion
Nutrition knowledge, attitudes, and practices (KAP) analysis was widely utilized in public health research across diverse populations and contexts. In the study conducted by Chen et al.17, particular attention was directed towards a distinct cohort of medical patients, specifically those undergoing hemodialysis, highlighting the importance of tailored interventions. A Madagascar study18 revealed moderate KAP scores regarding plague among residents of the Central Highlands, with mobile phone ownership and prior exposure to confirmed cases associated with higher KAP levels. In contrast, a Spanish university student cohort19 demonstrated that COVID-19 diagnosis indirectly influenced KAP outcomes through fear-mediated pathways, while female gender correlated with greater adherence to preventive measures. These studies employed cross-sectional designs with KAP questionnaire-based data collection, yet analytical approaches varied substantially. The hemodialysis research utilized latent profile analysis to categorize KAP patterns, whereas the COVID-19 study applied structural equation modeling to validate mediation effects. The Madagascar study primarily relied on multivariate regression techniques.
Nutrition KAP assessment, followed by latent profile analysis (LPA), has been utilized across various populations. Research on hemodialysis patients17 identified substantial positive correlations between dietary knowledge and attitudes, as well as between attitudes and practices. Additionally, socioeconomic status and gender emerged as significant predictors of membership within each KAP profiles identified through LPA. Simultaneously, Hu et al.20 concentrated on the disparities in health literacy concerning prevalent chronic diseases among ethnic minority residents, underscoring the necessity for targeted health education. Both studies identified obstacles in translating knowledge into practice, although the specific influencing factors differed. Consequently, it was recommended that intervention strategies be designed according to the unique characteristics of different groups to improve the efficacy of health behaviors.
Recent studies have highlighted the significant role of socio-cultural and economic contexts in shaping health-related KAP among chronic disease populations21,22. For instance, disparities in healthcare access, educational attainment, and cultural dietary habits may influence nutritional practices in patients undergoing maintenance hemodialysis (MHD)23. While our study focuses on Anhui province in China, regional variations in healthcare infrastructure and patient education programs could lead to heterogeneity in nutritional KAP outcomes. The novelty of our study lies in its application of LPA to the nutritional KAP of MHD patients, a method that has not been extensively used in this context before. This approach allows for a more nuanced understanding of the diverse nutritional profiles within the MHD patient population, enabling the identification of specific subgroups that may benefit from targeted interventions. By incorporating these contextual factors into our analysis, our study not only advances the understanding of nutritional KAP in MHD patients but also provides a framework for future research to explore similar dynamics in other regions and populations.
Current status of nutrition KAP in MHD patients
The body weight of MHD patients is closely associated with their mortality rate24. This study reveals that the three items with the highest error rates in the knowledge dimension were standard weight calculation, calcium control, and salt intake, with the lowest scores for patients’ ability to calculate their standard body weight. The observed knowledge gaps in standard weight calculation, calcium control, and sodium intake may stem from multiple factors. First, limited health literacy among patients with lower educational attainment (45.7% had primary education or were illiterate) likely hindered their ability to interpret complex medical guidelines25. Second, clinical education programs in Anhui province may prioritize acute symptom management over preventive nutritional counseling, leading to insufficient patient empowerment26. Third, cultural preferences for high-sodium diets in regional cuisine27 and inadequate follow-up by healthcare providers could perpetuate poor dietary practices. Patients undergoing hemodialysis for end-stage renal disease show poor awareness and control of their body weight, consistent with the findings of Harhay MN28. Addressing these gaps requires tailored educational interventions that account for patients’ literacy levels and cultural contexts.
Calcium abnormalities lead to a series of chronic complications that directly impact the survival rate of hemodialysis patients29; however, clinical signs of calcium abnormalities are less apparent compared to those of potassium or sodium imbalances, resulting in insufficient patient attention to calcium-related issues. Additionally, sodium and fluid imbalance is a critical factor contributing to protein-energy malnutrition30, and hypernatremia can lead to poor patient outcomes31. This investigation found that MHD patients, despite being on dialysis, lack sufficient awareness about the importance of sodium and calcium management, and their comprehension of the issue is insufficient. Therefore, clinical nursing care ought to prioritize increasing patients’ awareness about this matter.
Research32 suggests that establishing healthy nutritional practices requires patients to recognize their importance, as differences in patients’ attitudes and awareness directly affect habit formation. In this survey, the average item score in the nutritional attitude dimension for MHD patients was higher than in the knowledge and practice dimensions, indicating that patients generally have a positive attitude towards nutrition. However, lower scores were observed in their willingness to consult a nutritionist, belief in the need to change dietary habits, and proactive attitudes towards acquiring nutritional knowledge. Therefore, clinical efforts to assess and intervene in patients’ attitudes and awareness can positively influence practice formation. The low willingness to consult a nutritionist also reflects the weak influence of clinical nutrition work among dialysis patients, which aligns with Wang AY’s findings33, highlighting the need to enhance the role of nutrition professionals in improving the prognosis and rehabilitation of MHD patients.
Latent profiles of nutrition KAP in MHD patients
This study conducted a latent profile analysis on the KAP scores of MHD patients, classifying them into three groups: Low, Medium, and High KAP Groups. The model fitting indices were optimal under this classification method. The Low KAP Group, which comprised 5.41% of the sample, showed significantly lower scores in the knowledge dimension compared to the other two groups, indicating that this population is a key focus for clinical nursing interventions. For these patients, the dissemination and education of dialysis-related knowledge are critically important. The Moderate KAP Group, making up 76.21% of the sample, had the largest proportion of patients. While their knowledge scores were similar to those in the High KAP Group, their practice scores had room for improvement. Consistent with previous research34, this group faces challenges in translating dialysis-related knowledge into personal beliefs and practices, which is a common issue in clinical care. This suggests that healthcare workers and family members should focus on facilitating the transformation of patient knowledge into attitudes and practices as a priority in nursing care. The High KAP Group, accounting for 18.38%, showed superior performance in all dimensions of knowledge, attitude, and practice compared to the other groups. Further research on this group, such as their learning methods and practice patterns, could provide scientific evidence for targeted clinical nursing interventions.
Factors influencing the latent profiles of nutrition KAP in MHD patients
In clinical practice, the correlation between patients’ education levels and their self-care abilities and clinical outcomes is significant, with higher education levels generally being associated with advantages in knowledge acquisition, attitude formation, and behavioral development35.Similar to previous findings, this study shows that patients with a high school education or above are protective factors for entering the high KAP group compared to those with a lower education level. These results suggest that personalized and targeted clinical nursing approaches should be employed for patients with varying educational backgrounds. Sleep quality and physical exercise also have a notable impact on patients’ cognitive and behavioral states36,37. In this study, patients who slept less than five hours or engaged in limited physical exercise were more likely to be classified in the Low KAP Group. Insufficient sleep can negatively affect mental and cognitive functions, while a lack of physical activity is a significant risk factor contributing to metabolic disorders and slow recovery37. Therefore, focusing on improving patients’ sleep quality in clinical care could effectively enhance their nutritional status and promote the development of positive practices and cognition in MHD patients.
Patients in the low KAP group exhibit marked deficiencies in educational attainment, hemoglobin levels, frequency of exercise, and duration of sleep, highlighting the need for targeted interventions. Research suggests that the use of simplified educational materials and visual aids can significantly improve health literacy and behaviors. For example, an audio booklet tailored for individuals with low health literacy was shown to enhance their comprehension of the benefits and risks associated with statin use, leading to a notable increase in medication adherence and knowledge levels following the intervention38. Similar educational strategies applied to diabetic populations have demonstrated positive outcomes, with interactive educational methods significantly enhancing patients’ knowledge, attitudes, self-efficacy, and health behaviors, as well as improving their quality of life and hemoglobin levels39. In contrast, patients in the moderate KAP group, although exhibiting higher educational attainment and hemoglobin levels than those in the low KAP group, still show a significant deficiency in exercise frequency when compared to their high KAP counterparts. Intervention strategies should prioritize the translation of knowledge into sustained practices by employing behavioral nudges, such as goal-setting tools and peer support programs.
Health counseling effectively enhances health accountability, interpersonal relationships, and exercise-related knowledge, thereby facilitating lifestyle modifications40,41. Peer support is particularly influential; for instance, a study on breastfeeding demonstrated that peer education significantly improved maternal attitudes and knowledge, leading to extended breastfeeding duration42. This model holds promise for broader application in promoting adherence to exercise and dietary modifications. In hemodialysis populations, the integration of sleep hygiene counseling and structured exercise regimens into routine care significantly improves outcomes. Sleep quality is a critical factor influencing clinical status, with melatonin supplementation shown to enhance both sleep quality and cognitive function in this population43. Improved sleep is associated with higher treatment adherence rates. Additionally, theory-based exercise programs, such as a WeChat-delivered transtheoretical model intervention, have been shown to significantly enhance self-management capacity44. Integrated sleep and exercise interventions synergistically improve behavioral adherence and address multiple dimensions of health.
Overall, patients in the low KAP group may benefit from simplified educational materials and visual aids to address limited health literacy, while those in the moderate KAP group could require behavioral nudges (e.g., goal-setting tools or peer support programs) to translate knowledge into sustained practices. Additionally, integrating sleep hygiene counseling and structured exercise regimens into routine care may enhance cognitive function and behavioral adherence across all subgroups.
Limitations
The limitations of this paper include its cross-sectional design, which prevents causal conclusions, a regional sampling bias confined to Anhui province in China, and a sample size that needs to be increased. This study was a multicenter cross-sectional survey conducted in Anhui in China. First, its cross-sectional design precludes causal inferences between KAP levels and clinical outcomes; longitudinal studies are needed to evaluate whether improving nutritional KAP reduces morbidity or mortality in MHD patients. Second, the convenience sampling method and regional focus (Anhui) may limit generalizability to other socio-cultural contexts, particularly in regions with differing healthcare infrastructure or dietary norms. Future research should utilize random or stratified sampling techniques to improve population representativeness and consider increasing the sample size to include diverse countries and various socio-cultural or healthcare contexts. This approach will facilitate a more comprehensive understanding of the nutritional knowledge, attitudes, and practices (KAP) among patients with maintenance hemodialysis (MHD) and aid in identifying high-risk factors. Such findings will provide a scientific foundation for developing nutritional intervention strategies within clinical nursing for MHD patients.
Despite these limitations, this study contributes to the literature by applying latent profile analysis (LPA) to classify MHD patients’ nutritional KAP—a novel approach that moves beyond traditional variable-centered analyses. By identifying distinct patient subgroups, our findings underscore the need for precision interventions rather than one-size-fits-all strategies. Furthermore, this study highlights the critical role of multidisciplinary collaboration, particularly involving dietitians and mental health professionals, to address the multifaceted determinants of nutritional KAP in MHD populations.
Conclusion
This study utilized the nutrition KAP questionnaire for MHD patients to investigate and analyze the nutritional KAP status of patients in twenty hemodialysis hospitals in the Anhui province in China. The patients were categorized into three groups: low, medium, and high KAP levels, influenced by factors such as education level, physical exercise, sleep duration, and hemoglobin levels. Clinical nurses should adopt targeted nursing interventions based on the specific characteristics of different patients to effectively improve their nutritional KAP status. Simplified educational materials and visual aids can help patients with low KAP improve health literacy, while moderate KAP patients may benefit from behavioral nudges like goal-setting or peer support. Incorporating sleep hygiene counseling and structured exercise into routine care could boost cognitive function and adherence for all groups. In conclusion, our findings provide a foundation for developing tailored interventions to improve nutritional outcomes in MHD patients. Future work should expand to multi-center cohorts across diverse regions, incorporate qualitative insights into cultural and economic barriers, and evaluate the long-term impact of KAP-focused interventions on hard endpoints such as hospitalization rates and survival.
Data availability
All data generated or analysed during this study are included in this published article and its Supplementary Information files.
References
Johansen, K. L. et al. US renal data system 2020 annual data report: Epidemiology of kidney disease in the United States. Am. J. Kidney Dis. 77(4), 7–8 (2021).
Bhandari, S. K. et al. Causes of death in end-stage kidney disease: Comparison between the United States renal data system and a large integrated health care system. Am. J. Nephrol. 53 (1), 32–40 (2022).
Canaud, B., Morena-Carrere, M., Leray-Moragues, H. & Cristol, J. P. Fluid overload and tissue sodium accumulation as main drivers of protein energy malnutrition in dialysis patients. Nutrients 14 (21), 4489 (2022).
Xu, Y. et al. Development and validation of a nutrition knowledge, attitude, and practice questionnaire for maintenance Hemodialysis patients. Chin. J. Mod. Nurs. 29 (10), 1286–1293 (2023).
Chen, S. S. et al. Latent class analysis of daytime sleepiness and its influencing factors among rotating nurses in ICU. J. Nurs. Sci. 38 (11), 63–66 (2023).
Xu, Y. H. et al. A study on the current status of nurses’ knowledge, attitude, and practice in preventing catheter-associated urinary tract infections based on cluster analysis. China Mod. Doctor. 57 (27), 153–157 (2019).
Murphy, D., Ross, J., Busuttil, W., Greenberg, N. & Armour, C. A latent profile analysis of PTSD symptoms among UK treatment seeking veterans. Eur. J. Psychotraumatol. 10 (1), 1558706 (2019).
Dai, Y. et al. Heterogeneity in the co-occurrence of depression and anxiety among adolescents: Results of latent profile analysis. J. Affect. Disord. 357, 77–84 (2024).
Shao, K. et al. Latent profile analysis of innovative behavior among oncology nurses. J. Nurs. Sci. 39 (6), 7–11 (2024).
Yi, L. et al. Development and validation of a machine learning-based predictive model for compassion fatigue in Chinese nursing interns: A cross-sectional study utilizing latent profile analysis. BMC Med. Educ. 24 (1), 1495 (2024).
Zhang, Y. et al. Psychosocial factors associated with career success among nurses: A latent profile analysis. J. Adv. Nurs. 79 (2), 652–663 (2023).
Tan, W. Y. et al. Latent profiles of academic resilience in undergraduate nursing students and their association with resilience and self-efficacy. Nurse Educ. Pract. 77, 103949 (2024).
Nasreddine, Z. S. et al. The Montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53 (4), 695–699 (2005).
Bolayir, B. et al. Validation of nutritional risk screening-2002 in a hospitalized adult population. Nutr. Clin. Pract. 34 (2), 297–303 (2019).
Malmstrom, T. K. & Morley, J. E. SARC-F: A simple questionnaire to rapidly diagnose sarcopenia. J. Am. Med. Dir. Assoc. 14 (8), 531–532 (2013).
Huang, L. J. et al. Validation of the Chinese version of the SARC-F scale in community-dwelling elderly populations. J. Nurs. Sci. 35 (19), 85–88 (2020).
Chen, Z. et al. Dietary knowledge-attitude-practice status in hemodialysis patients: A latent profile analysis. BMC Public. Health. 24 (1), 836 (2024).
Rakotosamimanana, S. et al. Spatial analysis of pulmonary tuberculosis in Antananarivo Madagascar: Tuberculosis-related knowledge, attitude and practice. PLoS One. 9 (11), e110471 (2014).
Cancela, A., González-Noriega, M. & Visiers, A. Fear of COVID-19: The mediation role between the COVID-19 diagnosis and KAP in Spanish university students. BMC Public. Health. 23 (1), 1909 (2023).
Hu, H. et al. A latent profile analysis of residents’ knowledge, attitude, and practice toward common chronic diseases among ethnic minority area in China. Front. Public. Health. 10, 940619 (2022).
Palmer, S. C. et al. Dietary and fluid restrictions in CKD: A thematic synthesis of patient views from qualitative studies. Am. J. Kidney Dis. 65 (4), 559–573 (2015).
Luyckx, V. A. et al. Sustainable development goals relevant to kidney health: An update on progress. Nat. Rev. Nephrol. 17 (1), 15–32 (2021).
Schiff, R. & Freill, H. Improving access to phosphorus- and sodium-restricted foods for people living with chronic kidney disease in remote first nations. Rural Remote Health. 20 (1), 5485 (2020).
Cabezas-Rodriguez, I. et al. Influence of body mass index on the association of weight changes with mortality in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 8 (10), 1725–1733 (2013).
Devraj, R. & Gordon, E. J. Health literacy and kidney disease: Toward a new line of research. Am. J. Kidney Dis. 53 (5), 884–889 (2009).
Palmer, S. C. et al. Dietary interventions for adults with chronic kidney disease. Cochrane Database Syst. Rev. 4 (4), CD011998 (2017).
Campbell, K. L., Palmer, S. C. & Johnson, D. W. Improving nutrition research in nephrology: An appetite for change. Am. J. Kidney Dis. 69 (5), 558–560 (2017).
Harhay, M. N. et al. Patient and health care professional perspectives on addressing obesity in ESKD. Am. J. Kidney Dis. 82 (4), 419–428 (2023).
Xiao, P. et al. Association between corrected serum calcium levels after dialysis and post-dialysis fatigue risk: A hospital-based case-control study. Eur. J. Med. Res. 28 (1), 173 (2023).
Dekker, M. J. et al. Impact of fluid status and inflammation and their interaction on survival: A study in an international Hemodialysis patient cohort. Kidney Int. 91 (5), 1214–1223 (2017).
Mc Causland, F. R., Waikar, S. S. & Brunelli, S. M. Increased dietary sodium is independently associated with greater mortality among prevalent hemodialysis patients. Kidney Int. 82 (2), 204–211 (2012).
Czaja-Stolc, S. et al. Adherence to caloric and protein recommendations in older hemodialysis patients: A multicenter study. Nutrients 14 (19), 4160 (2022).
Wang, A. Y. et al. Assessing global kidney nutrition care. Clin. J. Am. Soc. Nephrol. 17 (1), 38–52 (2022).
Kelly, M. P. & Barker, M. Why is changing health-related behaviour so difficult? Public. Health. 136, 109–116 (2016).
Daniel, S. C., Azuero, A., Gutierrez, O. M. & Heaton, K. Examining the relationship between nutrition, quality of life, and depression in hemodialysis patients. Qual. Life Res. 30 (3), 759–768 (2021).
Ho, L. L., Chan, Y. M. & Daud, Z. M. Dietary factors and sleep quality among hemodialysis patients in Malaysia. J. Ren. Nutr. 32 (2), 251–260 (2022).
Pedersen, B. K. & Saltin, B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports. 25 (Suppl 3), 1–72 (2015).
Gossey, J. T. et al. Promoting knowledge of Statins in patients with low health literacy using an audio booklet. Patient Prefer Adherence. 5, 397–403 (2011).
Didarloo, A., Shojaeizadeh, D. & Alizadeh, M. Impact of educational intervention based on interactive approaches on beliefs, behavior, hemoglobin A1c, and quality of life in diabetic women. Int. J. Prev. Med. 7, 38 (2016).
Cingil, D. & Göger, S. Effect of education and counseling on anthropometric measures and healthy lifestyle behavior among overweight and obese women. Transl Behav. Med. 10 (6), 1450–1457 (2020).
Pandit-Agrawal, D., Khadilkar, A., Chiplonkar, S. & Khadilkar, V. Knowledge of nutrition and physical activity in apparently healthy Indian adults. Public. Health Nutr. 21 (9), 1743–1752 (2018).
Kempenaar, L. E. & Darwent, K. L. The impact of peer support training on mothers’ attitudes towards and knowledge of breastfeeding. Matern Child. Nutr. 9 (3), 359–368 (2013).
Marzieh, S. H. et al. The effect of melatonin on sleep quality and cognitive function of individuals undergoing hemodialysis. Sleep. Med. 111, 105–110 (2023).
Ren, Q. et al. Effects of a transtheoretical model-based WeChat health education programme on self-management among haemodialysis patients: A longitudinal experimental intervention study. J. Adv. Nurs. 75 (12), 3554–3565 (2019).
Acknowledgements
We thank all patients who participated in the questionnaire.
Funding
This work was supported by Natural Science Foundation of China (82301185) and Natural Science Foundation of Henan Province (232300421317).
Author information
Authors and Affiliations
Contributions
Study design: Yuan Xu and Sen Zou. Data collection: Yuan Xu and Zihan Chen. Data analysis: Yuan Xu, Xinlong Tang, Xiaojie Xia, and Nina Zhao. Study supervision: Yuan Xu. Manuscript writing: Yuan Xu and Sen Zou. Critical revisions for important intellectual content: Yuan Xu and Sen Zou.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, Y., Chen, Z., Tang, X. et al. Latent profile analysis of nutrition knowledge, attitudes, and practices and their influencing factors in maintenance hemodialysis patients. Sci Rep 15, 17246 (2025). https://doi.org/10.1038/s41598-025-02142-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02142-4