Abstract
In this study, orodispersible films (ODFs) were developed as fast-releasing formulations for pediatric patients suffering from Lennox-Gastaut or Dravet syndrome, with cannabidiol (CBD) selected as the active pharmaceutical ingredient (API). The properties of the ODFs were evaluated both before and after casting, with a focus on establishing a correlation between the properties of colloidal dispersion/suspension and ODFs to enhance understanding of the manufacturing process. Two blank colloidal dispersions were characterized for spreadability, viscosity, tangential stress, and pH, and their properties were correlated with those of blank ODFs, including mass uniformity, thickness, folding endurance, thickness-normalized crushing strength, disintegration time (evaluated through two different methods) and adhesivity. The strength and direction of the correlation were established via the Pearson coefficient. The same statistical approach was applied to assess correlation between CBD suspension (DCBD1, DCBD2) properties and CBD-ODF parameters. For the suspensions, particle size evaluation was also considered. Although few statistically significant positive or negative correlations were observed, a notable finding of this study was the dissolution behavior of CBD-ODF2, where nearly 100% of the API was released at 30 min, which is consistent with the disintegration behavior evaluated through the pharmacopeial method. Notably, CBD is classified as a Biopharmaceutical Classification System (BCS) Class II compound.
Similar content being viewed by others
Introduction
One of the main objectives in pharmaceutical research has been to develop effective pediatric drugs while minimizing side effects1. Despite recent advancements in pediatric medication, the availability of drugs specifically designed for children remains insufficient, with less than 50% being studied for pediatric patients2. It is well established that the market lacks appropriate pediatric formulations, leading to an increased risk of dosing errors and administration challenges. Factors such as age, ease of administration, swallowing ability, and accessibility of suitable formulations must be considered when selecting medicines for children3. A major limitation of the oral administration route is that the oral dosage forms are not always available in concentrations appropriate for pediatric use. Therefore, dosage forms, such as pills and tablets, are often manipulated in suboptimal ways, including dividing, crushing, or dissolving them in liquids, which may compromise dose accuracy, efficacy, and safety4. Significant pharmacotherapeutic differences between adults and children further complicate the development of pediatric formulations suitable across all pediatric age groups (neonates, toddlers, young children, and adolescents) concerning acceptable dose volumes, safety, specific needs, and palatability5.
A suspension is a heterogeneous system in which solid particles are dispersed within a liquid medium and can generally be categorized based on particle size into colloidal suspensions (< 1 μm) and coarse suspensions (> 1 μm)6. This pharmaceutical dosage form offers several advantages; for instance, it can accommodate water-insoluble drugs and protect active substances that are unstable or prone to degradation in solution. Suspension can also mask unpleasant odors or tastes associated with certain medications, improving patient compliance. Additionally, it can increase the bioavailability of certain substances compared to an equivalent dose in tablet or capsule form. This improvement in bioavailability, assessed after quality control evaluation, is particularly beneficial for drugs with poor solubility or dissolution rates7,8,9.
Orodispersible dosage forms (ODxs) have attracted increasing interest in the pharmaceutical market because of their distinctive properties, such as improved bioavailability of certain active pharmaceutical ingredients (APIs) and enhanced patient adherence/compliance. These advantages make ODxs particularly beneficial for populations with swallowing difficulties, such as pediatric and geriatric patients10. They can enhance patient compliance due to their ability to be absorbed without drinking or chewing, providing more accurate dosing compared to liquid dosage forms, reducing the risk of dose variability and administration errors11. Examples of such dosage forms (ODxs) include orodispersible films (ODFs), orodispersible tablets (ODTs), orodispersible granules (ODGs), and oral lyophilizates (OLs)10.
ODFs are thin, mechanically strong, flexible, single- or multilayered polymeric films designed to disintegrate rapidly in the oral cavity to produce either local or systemic effects. They possess several advantages, making them an ideal option for pediatric and geriatric patients, such as rapid and constant drug release, rapid permeation through the oral mucosa, and the ability to bypass first-pass effect, which may improve bioavailability of certain drugs12. Musazi et al. described a variety of manufacturing methods for ODF, ranging from the solvent casting method, one of the simplest procedures, to more complex methods, such as electrospinning, hot-melt extrusion, and printing, including 3D printing13. The physical properties of ODFs (appearance, texture, thickness, and structure) depend on the fabrication method, but regardless of the chosen fabrication technique, all the ODFs must dissolve rapidly in the oral cavity13,14. The solvent-casting method is the most widely used technique for manufacturing ODFs. The process begins with the dissolution/dispersion of the API and the excipients (film-forming polymers, plasticizer agents, saliva-stimulating agents, flavors, sweeteners, coloring agents, and surfactants) in a polymeric solution, followed by the removal of the air bubble to ensure uniformity. The resulting mixture is cast on a plain, smooth surface and dried at an appropriate temperature. After drying, the film is peeled off and cut to the desired size. This method is used both on an industrial scale and in laboratory settings15,16,17,18. The most commonly used excipients when formulating ODFs are film-forming polymers, such as hydroxypropyl methylcellulose (HPMC), hydroxypropyl cellulose (HPC), carboxymethyl cellulose (CMC), and polyvinyl alcohol (PVA), with molecular weights between 1000 and 9000 Da, and plasticizers, such as glycerol, polyethylene glycol (PEG), and propylene glycol19,20. HPMC (chemical structure shown in Fig. 1a- Supplementary) is an odorless, flavorless, transparent, nontoxic, white to slightly white fibrous or granular, free-flowing powder that is a synthetically modified derivative of natural cellulose21,22. Due to its ability to function as a pH-independent and viscous gelling agent, it is the most used hydrophilic, biodegradable polymer for film formation23,24. HPMC is available in different viscosity grades based on the level of methyl and hydroxypropyl substitution, and its viscosity varies when used at different concentrations and various temperatures. Moreover, the hydrophilic properties of hydroxypropyl methylcellulose can increase the solubility and dissolution of poorly water-soluble drugs in the manufacturing of solid dispersions25. By using hydroxypropyl methylcellulose as a film-forming polymer due to its chemical stability, biocompatibility, superior controlled-release properties, lower allergenic potential, and consistent quality, a variety of APIs can be incorporated, such as meloxicam, doxazosin, rosuvastatin, loratadine, phenytoin or levocetirizine20,26,27,28,29,30,31,32.
Polyvinyl alcohol (chemical structure shown in Fig. 1b-Supplementary) is a water-soluble polymer capable of forming flexible, transparent, nontoxic, and biodegradable films with good mechanical properties, enhance chemical resistance, and high biocompatibility33. The water solubility and physical properties of PVA, including its film forming stability, are significantly influenced by its degree of hydrolysis, molecular weight, and crystallinity34,35. The variety of applications, such as tissue regeneration, wound dressing, and drug delivery systems, have made PVA one of the most promising biodegradable polymers on the market36. Examples of APIs successfully formulated in PVA-ODFs include sildenafil, entecavir, amlodipine, tianeptine, and aripiprazole37,38,39,40,41.
Cannabidiol (CBD), a terpenophenol compound with the chemical structure 2-[(1R,6R)-3-methyl-6-prop-1-en-2-ylcyclohex-2-en-1-yl]-5-pentylbenzene-1,3-diol (chemical structure shown in Fig. 1 (c)-Supplementary), contains a cyclohexene ring, a phenolic ring and a pentyl side chain and can be found in Cannabis sativa species. The chemical activity of CBD is primarily influenced by the position of the hydroxyl groups in the phenolic ring, the methyl group of the cyclohexene ring, and the pentyl side chain42. This API has very low water solubility (12.6 mg/L), high lipophilicity (log P = 6.3), weak acidic properties (pKa = 9.1), a melting point of 67 °C and a molar mass of 314 g/mol. Due it its physicochemical properties and high permeability, CBD is placed in Class II of the Biopharmaceutics Classification System (BCS). Furthermore, CBD exhibits low oral bioavailability (6%) due to inconsistent absorption resulting from its instability in the acidic environment and extensive first-pass metabolism, which contribute to significant variations in plasma concentrations43,44.
The potential therapeutic effects of CBD are attributed to its anti-inflammatory, antiseizure, analgesic, and antiemetic properties. McGuire et al. studied the effect of CBD as an adjunctive therapy in adults with schizophrenia and found it to be associated with improvements in psychotic symptoms45. Another randomized, double-blind, controlled clinical trial revealed that CBD is effective in managing Lennox–Gastaut syndrome and is well-tolerated46. Owing to its effectiveness in seizure management, CBD has been used as adjacent therapy among patients with Dravet syndrome, including in early childhood47. The Food and Drug Administration (FDA) and European Medicines Agency (EMA) have approved the use of CBD for seizures associated with Lennox–Gastaut and Dravet syndromes48. Sativex®, a product containing both CBD and THC, has been approved by the EMA and FDA for the treatment of multiple sclerosis–associated spasticity. Although CBD has not yet been approved for this purpose, several clinical studies have been conducted to evaluate its effects in patients with Parkinson’s disease or multiple sclerosis, showing potential efficacy49,50. The pharmaceutical industry has begun developing CBD-based pharmaceutical dosage forms due to the growing interest and potential of this innovative compound. These dosage forms include liposomes, niosomes, creams, emulsions, suspensions, and oils51,52,53,54,55,56. Epidiolex® (GW Pharmaceuticals, Cambridge, UK) and Sativex® (GW Pharmaceuticals, Cambridge, UK) (Table 1) are two liquid-form products developed for the treatment of neurological disorders57,58,59,60,61.
Previous reviews have examined literature on the development of CBD buccal films, as well as manufacturers that have produced CBD-ODFs or related products. Chelminiak-Dudkiewicz et al. developed 1% chitosan-based films containing CBD oil at concentrations of 1%, 5%, and 10% (reported to have different chitosan contents) for use as wound healing dressings. The results revealed that an increased amount of CBD oil enhanced the antimicrobial effect (against Aliivibrio fischeri) and improved skin biocompatibility, making them promising candidates for wound healing. The films were prepared via the solvent casting method and dried at room temperature62. Abdella et al. developed 2% (w/w) CBD-nanostructured lipid carriers incorporated in buccal films, each containing 0.4 mg CBD, via a 3D printing technique. Several polymers have been examined for 3D printing, both individually or in combination, and the results revealed that hydroxyethyl cellulose was the most suitable for the intended purpose due to its excellent mucoadhesive properties and printability63. Klinsang et al. developed a CBD-fibroin film containing 100 µg/cm2 CBD using silkworm cocoons (Bombyx mori) as a source for fibroin. To enhance hydrophilicity, a CBD-hydroxypropyl β-cyclodextrin (HP-β-CD) complex was used at a molar ratio of 1:2 (CBD: HP-β-CD). The films were prepared using the solvent casting method and dried at 47 ± 2°C64. The manufacturer, Dr. Zimmermann GMBH Edimags, developed CBD ODFs intended for oral or sublingual administration, allowing them to bypass first-pass metabolism. The amount of CBD included in the ODF matches the CBD dose used in our study, while other parameters, such as thickness, dimension, and size were varied. Additionally, the purpose and target patient differ, as in this study, pediatric patients with epilepsy-derived pathologies were selected, whereas the manufacturer mentioned above aims to provide a smoke-free alternative to traditional CBD delivery through edible films65. Another product found online is CHYLL CBD-ODFs, which contain a mixture of CBD and cannabidiolic acid (CBDA) totaling 10 mg, along with 0.2 mg tetrahydrocannabinol (THC). These ODFs are manufactured through Versafilm® technology. The main advantages highlighted by the manufacturer include fast-acting relief, discretion, portability, and convenience, along with precise dose control, likely achieved by adjusting the film’s size or thickness66.
Based on published literature on pharmaceutical formulations with CBD (authorized or under development), this study aims to develop ODFs containing CBD using various concentrations of HPMC and PVA as film-forming polymers. Additionally, it seeks to investigate the relationship between the properties of the initial suspension and those of the resulting orodispersible films cast into predetermined shapes. The selection of the dosage form is intended to increase absorption, avoiding first-pass metabolism.
Results and discussion
Preformulation studies
In this subchapter, two analytical methods were employed to assess potential interactions between the API and the selected excipients (Differential scanning calorimetry (DSC) and Fourier-Transform Infrared (FTIR) spectroscopy).
DSC evaluation
The CBD thermogram revealed an endothermic peak, indicating a melting point of 69 °C (Fig. 2 – Supplementary), confirming the results of Andriotis et al. and Abdella et al.63,67. Similarly, the Tonset was 66.45 °C, and the Tendset was 71.43 °C68,72. The decomposition of CBD occurs at temperatures higher than 300 °C, as shown in a previously published study with a wider temperature range for thermal evaluation (25–500 °C)68 Because the active ingredient decomposes > 300 °C, it will remain stable during the pharmaceutical processing techniques, such as spray drying, hot-melt extrusion, and lyophilization. As a result, different methodologies can be applied to obtain ODFs with CBD. Citric acid, a versatile excipient, exhibited two endothermic peaks with the following characteristics: Tonset=147.45 °C, Tpeak = 155.92 °C, and Tendset=163.34 °C (endothermic peak 1) and Tonset = 163.42 °C, Tpeak = 203.55 °C, and Tendset = 219.43 °C (endothermic peak 2) (Table 2). The second peak was broader than the first peak, as previously reported in an article that used different conditions (the previous study in nitrogen atmosphere while the present study in air atmosphere). For the first selected polymer (HPMC E3), a peak indicating water loss was observed in the thermal analysis (Table 2)68. Small shifts in the analyzed parameters Tonset(°C), Tpeak(°C), and Tendset(°C) were observed in the binary mixtures between CBD and citric acid, with the most significant shift recorded in the case of the second endothermic peak of citric acid (8 °C in the case of Tonset and Tpeak and 3 °C in the case of Tendset). In both binary mixtures (CBD: CA and CBD: HPMCE3), the cannabinoid displayed parameter values similar to those of pure CBD (Table 2). The thermal shifts in the CBD thermogram suggest potential hydrogen bonding, molecular dispersion, or eutectic formation with citric acid and HPMCE3. The endothermic peak of CBD was reduced in the binary mixture because of the halved amount used compared with when the ingredients were analyzed individually. Sucralose (SUCR) displayed an endothermic peak that starts at 113.89 °C and ends at 141.25 °C, with Tpeak = 122.12 °C (Table 3). In the CBD: SUCR mixture, no notable shift in the CBD peak was observed, whereas the endothermic peak of the SUCR shifted to an exothermic peak, indicating that the formation of bonds between CBD and SUCR releases more energy than is consumed. In the case of the other polymers selected in this study, no significant shifts were observed in the physical mixture (CBD: PVA), and only PVA-Tonset, was altered due to the presence of the API, causing a notable shift of this value (Table 2) The fact that the Tonset increased is an advantage since the API is enhancing the thermal stability of PVA, through stronger molecular interactions. This change in thermal behavior allows the film to be dried at high temperatures.
FTIR spectroscopy analysis
The spectra of CBD and the solid excipients, along with their characteristic bands, are presented in Fig. 1a–d and Table 1 (Supplementary).
The spectra revealed characteristic bands at ~ 2930 cm− 1, corresponding to an asymmetric aliphatic C–H stretch vibration (-CH2), which were observed in the spectra of CBD, CA, SUCR, CBD: CA, CBD: PVA, CBD: HPMCE3, and CBD: SUCR (Fig. 1a–d). Another band at 2900 cm− 1 was attributed to the polymers (HPMCE3 and PVA, Fig. 1b, c) and the selected sweetener but was not observed in the binary mixture, probably due to the differences in amplitude or interaction between closely spaced bands. Four characteristic peaks can be observed within the 2800–3000 cm− 1 range (2965, 2928, 2856, and 2825 cm− 1), which can be associated with CH3 asymmetric, CH2 asymmetric, CH3 symmetric, and CH2 symmetric stretching, respectively. CH2 stretching is more intense due to the higher number of CH₂ groups present in the molecules of all analyzed ingredients. These peaks appear in all binary mixtures without shifts, while the characteristic peaks of additional components in this region appear exclusively in the CBD: SUCR mixture. The band at 1730–1740 cm− 1 is attributed to the C = O stretching vibration, which is typically associated with excipients with a carboxylic functional group. An asymmetric aliphatic C-H deformation of the methylene or methoxy group can be observed at 1458 cm− 1 in the case of the selected polymers (HPMCE3 and PVA) but is absent in the binary mixtures with the cannabinoid. The absence of this band in the binary mixture could result from its overlap with the band at 1440 cm− 1 attributed to aromatic C = C stretching vibrations; another explanation could be that the signal intensity may be too low compared to the surrounding peaks of CBD, reducing its visibility. The absorption band at 1373 cm− 1 is attributed to symmetric aliphatic C‒H bending of the methyl groups found in all evaluated materials, with minor shifts observed within the 1360–1379 cm− 1 range. Absorption bands below 1000 cm− 1 were not analyzed as they fall within the fingerprint region.
The presence of CBD is confirmed by the characteristic absorption bands corresponding to C=C and =C–H aliphatic groups (1582 and 1625 cm− 1). These bands were reported in previous studies67,68,69. These bands were identified as CBD-specific and used in the evaluation of the binary mixture. The presence of CBD in the binary mixture was confirmed by its trace amounts, while it suggests possible API interaction or amorphization. The API was observed in all the binary mixtures, with minor shifts (< 4 cm− 1) recorded.
In the study by Chelminiak-Dudkiewicz et al., four bands were identified as CBD-specific: 3006, 2923, 2856, and 1741 cm− 1, two of which were also observed in this study (2928 and 2856 cm− 1), while the other two were recorded at slightly shifted wavenumbers (3032 and 1772 cm− 1). Some bands identified in this study were not considered characteristic as they were also present in certain excipients62.
CBD suspension and blank colloidal dispersion (DB1, DB2, DCBD1, DCBD2)
Two blank colloidal dispersions and two CBD suspensions were analyzed for their pH, conductivity, particle size distribution, viscosity, tangential stress, spreadability, and CBD content as a starting point for assessing the correlation between the blank colloidal dispersion and CBD suspension properties and the physicochemical characteristics of the ODFs.
pH characterization
pH is a critical parameter for orally administered formulations. The resulting intermediate formulations (colloidal dispersions and suspensions) may serve as final formulations or can be further cast into ODFs.
The pH ranged between 3.25 (DB2) and 3.52 (DCBD1), indicating a narrow variation (Fig. 2a). Dunn’s multiple comparisons test showed no significant differences between the colloidal dispersions and the suspensions.
(a) Dunn’s multiple comparisons test results for the pH of the prepared colloidal dispersions. (b) Dunn’s T3 multiple comparisons test results for the conductivity of the prepared colloidal dispersions. ns (p > 0.05), ns—not significant, * (p < 0.05); ** (p < 0.01); *** (p < 0.001); **** (p < 0.0001).
However, the Kruskal‒Wallis test revealed significant differences among the median pH values (p = 0.0055).
Colloidal dispersion conductivity
The Kruskal‒Wallis test revealed a significant difference among medians (p = 0.002). The conductivity decreased in the following order: DB1 > DB2 > DCBD1 > DCBD2, with values ranging from 77.55 µS (DCBD2) to 125.51 µS (DB1) (Fig. 2b). Dunn’s multiple comparison test revealed a significant difference between DB1 and DCBD2 (p = 0.0014), indicating that the addition of the API and polymer modification contributed to the observed differences.
Particle size distributions (DCBD1 and DCBD2)
The particle size distribution was assessed for DCBD1 and DCBD2, where CBD was incorporated as the internal phase of a suspension. Two bell-shaped graphs were obtained highlighting the average size (dominant value) of the suspended ingredients, which were 2.2 μm (DCBD1) and 2.7 μm (DCBD2) (Fig. 3). In both cases, the frequency curve is relatively symmetric, however, the first curve has a broader base, while the second curve appears narrower.
Stukelj et al. developed CBD suspensions using different solvents, varying the ethanol - water ratio and surfactant concentration, indicating the formation of nanosized particles with a concentration of 0.5% surfactant, yielding the smallest particle size (< 100 nm), in contrast to other methods that resulted in microsized particles. The particle sizes are comparable to our results, particularly those obtained 24 h after the initial particle size determination55. The polydispersity index (PdI) was calculated for both CBD suspensions, and a PdI of less than 0.1 was observed in both cases. This indicates a uniform particle size distribution, reducing the risk of CBD inhomogeneity in both the intermediate and final products (CBD-ODF).
Viscosity and tangential stress assessment
The viscosity and tangential stress were assessed for the blank colloidal dispersions and CBD suspensions. Low viscosity values were obtained only between the shear rate range of 10–12–10 for DB1, DCBD1, and DCBD2, whereas for DB2, measurable results were obtained at shear rates of 11–12–11. DB1 presented the highest tangential stress and viscosity values during both the destructuring and restoration phases across all applied rotation speeds, while DB2 recorded the lowest value. Furthermore, the choice of polymer used significantly influenced both parameters (tangential stress and viscosity), with PVA leading to a reduction in these values (Table 4). The addition/inclusion of the API to the prepared colloidal dispersions resulted in similar results, with only minor differences observed at shear rates of 11–12–11. During the destructuring phase, the tangential stress increased, whereas viscosity exhibited the opposite behavior. Another important observation is that in the first colloidal dispersion, CBD addition was conducted to reduce both the tangential stress and viscosity. In contrast, in the second colloidal dispersion, CBD addition resulted in an increase in both parameters. Additionally, the values obtained for the two DCBDs were nearly identical. The viscosity and tangential stress were evaluated since the viscosity can influence the thickness of the cast films, their average weight, and the mechanical properties of the ODFs. The opposite rheological behaviors observed in the two colloidal dispersions where different polymers were used suggest that CBD interacts differently with the polymeric networks formed by HPMC and PVA. In CBD-ODF1, CBD may act as a plasticizer, disrupting polymer-polymer interactions and reducing both viscosity and tangential stress. In contrast, in CBD-ODF2, the API may enhance intermolecular interactions between the PVA chains, leading to increased viscosity. HPMC is hydrophilic while PVA has an amphiphilic structure and as a result, CBD interacts with the hydrophobic part of the PVA resulting in entanglement and increased viscosity.
Spreadability
Considering the amount of polymer used in the development of dispersions, an important parameter that needs to be evaluated is the extensometric property, particularly for formulations intended for local administration, such as wound dressings. The spreadability increased in the following order: DB1 < DB2 < DCBD1 < DCBD2 (based on the final surface spread). A distinction between the two DCBDs is necessary, as DCBD1 exhibited superior spreadability throughout the experiment, except for the final surface spread value, while maintaining consistent parameter values when a mass of 96.87 g was applied until reaching 576.87 g. Through this evaluation, the influence of the polymer and the API presence/absence can be highlighted. As illustrated in Fig. 3 (Supplementary), the presence of CBD enhances spreadability because the API is suspended in the polymeric network, which disrupts the polymeric chain formed in the selected solvent mixture. Additionally, a 2.5-fold increase in the final spread surface was noticed through the addition of CBD. The active ingredient reduces intermolecular forces within the polymeric matrix, decreasing viscosity, altering the spreadability, and increasing fluidity.
CBD assay
The CBD content (in the suspension, determined on the same day as preparation) was evaluated via a previously validated HPLC method. Acetonitrile (Fig. 4a—Supplementary) and the two colloidal dispersions were used as blanks (Fig. 4b, c-Supplementary). The CBD content in the two suspensions was quantified (Table 3). The retention time of the analyte was set at 2.57 min (Fig. 4d-Supplementary), and a representative chromatogram at 25 µg/mL is also shown in Fig. 4d-Supplementary. In addition to the specificity, which was verified using blank colloidal dispersions, the methods’ linearity was assessed over a concentration range of 1–50 µg/mL. The calibration curve demonstrated good linearity with a coefficient of determination (R2 = 0.9990). The CBD content evaluation for the two suspensions revealed values close to the theoretical concentration, with the absolute deviations from the declared amount being less than 5.5% for the first suspension and less than 1% for the second suspension (Table 3).
CBD-ODF
During the experiments, different types of HPMC with varying viscosities (HPMC E3, HPMC E5, and HPMC E15) were used. Although many exhibited good mechanical properties, none demonstrated satisfactory disintegration behavior. Consequently, different types of film-forming agents were investigated, and the proposed active ingredient PVA yielded better results, suggesting its superior suitability for achieving the desired formulation characteristics.
Organoleptic properties
The blank ODFs were transparent, whereas the CBD-ODFs were slightly opaque (Fig. 5 – Supplementary). During storage at room temperature, CBD ODF1 films gradually developed a pale yellow colour, a phenomenon that can be correlated with the film-forming agent. Similar behavior has been observed for another pharmaceutical ingredient (tetrabenazine)75. All four film formulations maintained fine surfaces on both sides.
Weight uniformity
The average weight of the films varied between 45.9 ± 12.95 mg (ODBF2) and 111.92 ± 27.43 mg (CBD-ODF2) (Fig. 4a). To assess statistical differences, the Kruskal‒Wallis test alongside Dunn’s multiple comparison test was performed. Statistically significant differences were observed between ODBF2 and CBD-ODF2, attributed to the addition of the API (p < 0.0001), and between CBD-ODF1 and CBD-ODF2 (p < 0.0001) due to the use of different film-forming agents. The results show a significant in film weight in CBD-ODF2, nearly double that of ODBF2 (Fig. 4a). The Kruskal‒Wallis test confirmed significant variations in the medians (p < 0.0001), that the inclusion of CBD in the polymeric matrix leads to an increase the average weight. This effect was evident in the case of the formulation where PVA was used as a film-forming agent. Also, when the polymer was changed while maintaining the amount of CBD constant, a statistically significant difference was noticed between CBD-ODF1 (HPMC was used as a film-forming agent) and CBD-ODF2 (PVA was used as a polymer).
(a) Dunnett’s T3 multiple comparisons test results for the uniformity of mass. ns (p > 0.05), ns—not significant, * (p < 0.05); ** (p < 0.01); *** (p < 0.001); **** (p < 0.0001). (b) Dunn’s multiple comparisons test results for the thickness measurement. ns (p > 0.05), ns—not significant, * (p < 0.05); ** (p < 0.01); *** (p < 0.001); **** (p < 0.0001). (c) Dunnett’s T3 multiple comparisons test results for the folding endurance. ns (p > 0.05), ns—not significant, * (p < 0.05); ** (p < 0.01); *** (p < 0.001); **** (p < 0.0001). (d) Dunnett’s T3 multiple comparisons test results for thickness-normalized tensile strength. ns (p > 0.05), ns—not significant, * (p < 0.05); ** (p < 0.01); *** (p < 0.001); **** (p < 0.0001). (e) Dunn’s multiple comparisons test results for adhesivity. ns (p > 0.05), ns—not significant, * (p < 0.05); ** (p < 0.01); *** (p < 0.001); **** (p < 0.0001). (f) Dunnett’s T3 multiple comparisons test results for pH. ns (p > 0.05), ns—not significant, * (p < 0.05); ** (p < 0.01); *** (p < 0.001); **** (p < 0.0001). (g) Dunn’s multiple comparisons test results for the disintegration time through the pharmacopeial method. ns (p > 0.05), ns—not significant, * (p < 0.05); ** (p < 0.01); *** (p < 0.001); **** (p < 0.0001). (h) Dunn’s multiple comparisons test results for the disintegration time through the slide frame method. ns (p > 0.05), ns—not significant, * (p < 0.05); ** (p < 0.01); *** (p < 0.001); **** (p < 0.0001). (i) UV‒Vis spectrophotometry method linearity (1) and the statistical evaluation between the two CBD-ODFs via the t-test with Welch’s correction (2). ns (p > 0.05), ns—not significant, * (p < 0.05); ** (p < 0.01); *** (p < 0.001); **** (p < 0.0001).
Thickness
The thickness of the films varied between 125.11 ± 37.85 μm (ODBF1) and 295.56 ± 114.08 μm (CBD-ODF2) (Fig. 4b). The same trend as in the case of weight uniformity was observed, with CBD-ODF2 formulation accounting for the statistically significant differences. The combination of CBD and PVA resulted in a substantial increase in thickness (nearly double that of the previous three formulations). Statistical analysis confirmed significant differences, with a p-value < 0. when comparing each of the first three formulations with CBD-ODF2, a significant difference was observed between the blank formulations, (ODBF1 and ODBF2, p < 0.01).
In the literature, different values of thickness have been reported for CBD-containing films. Chelminiak-Dudkiewicz et al. (2022) developed chitosan CBD oil films with thicknesses ranging from 49.9 to 51.7 μm, which can be correlated with the results obtained in this study for the first three formulations. In the study conducted by Abdella et al., higher values of this parameter (284 ± 9 μm) were recorded. Additionally, for the orally dissolvable edible films produced by Optimags GmbH, Dr. Zimmermann (10 mg CBD) mentioned a constant thickness of 150 μm, which is close to the thickness recorded for CBD-ODF262,65. In conclusion, our results align with the results published in the literature and fall within the reported range of 50–1000 μm, which is valid for ODFs71.
Folding endurance
An important mechanical parameter that is assessed for polymeric films is folding endurance, which helps to determine whether special packing is needed, particularly when the mechanical strength is low, which may need special precautions. This parameter increased in the following order: ODBF1 > CBD-ODF2 > ODBF2 > CBD-ODF1, with values ranging between 3 ± 1 (ODBF1) and 45 ± 1 (CBD-ODF1). The addition of CBD improved this parameter; in the case where PVA was the film-forming agent and CBD was added, comparable results were obtained, with average values ranging between 25–30-fold (Fig. 4c). Statistically significant differences were recorded between ODBF1 and CBD-ODF1 (p < 0.0001) and ODBF1 and CBD-ODF2 (p = 0.0187). Additionally, no outliers were detected, and a Gaussian distribution was observed; consequently, Brown-Forsythe and Welch’s ANOVA tests alongside Dunnett’s T3 multiple comparison tests were used for statistical analysis.
PVA has a more rigid structure compared to HPMC, which is more flexible, thereby limiting the plasticizing effect that could improve folding endurance. Due to the chemical structure, PVA is likely to form stronger hydrogen bonds with CBD, which may reduce film flexibility and make it more brittle compared to CBD-ODF1.
Since this experiment was not conducted in previous studies aiming to incorporate CBD into polymeric films, the results were compared to those of another study in which caffeine was included in an ODF formulation where the influence of Vivapharm® HPMCE5 (8 and 9%) and suitable hydrotropic substances (citric acid and sodium benzoate) was outlined, where folding endurance ranged from 9 to 36-fold, with the highest values being observed in the formulation where 8% Vivapharm® HPMC E5 was used without any hydrotropic ingredients71.
Thickness-normalized tensile strength
An important parameter influencing tensile strength is thickness; since this dimensional parameter was measured before assessing this property, it is referred to as thickness-normalized tensile strength.
This parameter is commonly used alongside folding endurance to evaluate the mechanical properties of films. Due to the different polymers used and the presence of CBD in the last two formulations, varying results were obtained for the proposed formulations, with thickness-normalized tensile strengths ranging between 0.241 ± 0.009 N/mm2 (CBD-ODF1) and 0.741 ± 0.008 N/mm2 (ODBF1). Statistically significant differences were recorded in all cases, with p values < 0.0001 for ODBF1 and ODBF2, ODBF1 and CBD-ODF1, and ODBF2 and CBD-ODF2 and between the two CBD-ODFs; for the remaining comparisons, p values were 0.0006 (ODBF1 and CBD-ODF2) and 0.0004 (ODBF2 and CBD-ODF1) (Fig. 4d).
The tensile strength parameter can vary based on the assessment method, the apparatus used, and the type of polymer employed in film formulation. For example, Chelminiak-Dudkiewicz et al. in 2022 reported a tensile strength between 4.23 and 12.24 MPa, which could be attributed to the different polymers used compared to those in this study (1% low molecular weight chitosan) as well as the low amounts of CBD oil content utilized in their formulation62. Conversely, Abdella et al. 2024 reported results like those obtained in this study, with a tensile strength of 0.67 MPa when 8% hydroxyethyl cellulose (NF) was used as the film-forming agent63.
In a study conducted by Klinsang et al. in 2023, a fibroin film incorporating an HP-β-CD: CBD (2:1 molar ratio) complex was developed, and the results revealed a tensile strength of 48.7 ± 2.57 MPa64.
Adhesivity
The adhesivity of the formulations decreased in the following order: ODBF1 > ODBF2 > CBD-ODF2 > CBD-ODF1. Among them, CBD-ODF1, where HPMCE3 was used as a film-forming agent, exhibited very low adhesivity, however, this may not necessarily be considered a disadvantage. The incorporation of the API appears to negatively affect this parameter. A statistically significant difference was recorded between ODBF1 and CBD-ODF1, highlighting the impact of incorporating an API classified under the second class of the Biopharmaceutical Classification System (BCS II) into the first matrix (Fig. 4e). Given that the ODF formulation is intended for pediatric use, high adhesivity might be recommended to avoid premature elimination from the mouth (ODF spitting). Additionally, strategies such as improving palatability with sweeteners and flavors and enhancing the overall sensorial experience can help minimize such issues. Considering the age group for which the ODF is intended, all potential drawbacks need to be evaluated to ensure patient compliance. The inclusion of CBD in the polymeric matrix containing HPMC as the film-forming agent resulted in reduced film wettability, impeding water penetration. Consequently, during the adhesivity test, no measurable values were obtained for the CBD-ODF1 formulation, the adhesivity being dramatically decreased by the API incorporation, resulting in a film that was less sticky and easily detachable.
Although this test is characteristic of buccal films or mucoadhesive films, it can still be a valuable tool considering the target patient category; therefore, many studies focused on developing ODFs also evaluate adhesivity properties72,73,74.
In a study aiming to combine 3D-printed buccal films with nanostructured lipid carriers for personalized CBD delivery (where HEC was used as a film-forming agent), adhesion was assessed using porcine buccal mucosa. The inclusion of CBD led to a reduction in adhesion from 0.16 N (blank formulation) to 0.14 N (CBD formulation)62. A similar trend was observed in the present study, where both cases showed a decrease in adhesion upon adding CBD to the blank film (ODBF1 vs. CBD-ODF1 and ODBF2 and CBD-ODF2); this reduction was statistically significant in the comparison between ODBF1 and CBD-ODF1 (p = 0.0274).
pH
Another parameter that can influence patient compliance is the pH of the formulation; usually, a pH close to that of saliva is considered favorable, but the buffering capacity of saliva must be considered, as some ODFs with a low pH may not negatively impact the sensorial mouthfeel71.
The pH ranged between 3.11 ± 0.08 for ODBF2 and 3.53 ± 0.08 for CBD-ODF1. As shown in Fig. 4f, the use of CBD increased the film pH, with some cases showing statistically significant differences between CBD-ODF1 and CBD-ODF2 (p = 0.0005).
Ideally, the pH should be close to that of saliva; from this perspective, CBD-ODF1 is closer to the physiological pH (6.2–7.6)75. This parameter can be increased by reducing the concentration of citric acid, as citric acid is responsible for the low pH values. Considering that citric acid offers multiple advantages, including stimulation of salivary secretion, pleasant taste, and a plasticising effect, and the fact that the selected active ingredient is not pH-dependent, its use underscores more benefits than drawbacks. Upon contact with saliva, its buffering capacity gradually neutralizes the film’s acidity, resulting in a progressive increase in pH. Therefore, a slightly acidic pH cannot be considered necessarily an impediment.
Disintegration ability
Disintegration ability was evaluated using two methods: a pharmacopeial method typically used to evaluate the disintegration time of solid pharmaceutical formulations (capsules, tablets, coated tablets, ODF tablets, etc.) and a specific method mentioned in the literature, known as the slide frame method. Water was selected as a disintegration medium due to its pH being similar to that of saliva. However, this choice comes with certain limitations, as saliva exhibits interindividual variability in viscosity. Other parameters must be taken into consideration when evaluating the disintegration ability when using water, including the composition and ionic strength of saliva. Notably, no special mentions regarding disintegration media for ODFs are currently included in the pharmacopoeias. The lack of standardization is reflected in the diverse range of solvents used across studies, including phosphate buffer (pH = 6.8), artificial saliva, and different types of water (deionized or distilled water). In many studies focused on ODF development, the disintegration time requirements for orodispersible are often used as a reference (< 180 s in Ph. Eur. 11 and < 30 s in USP 45). As is evident, the USP sets stricter requirements, so while developing ODxs, manufacturers should take into account the regulatory framework of the intended market when developing orodispersible formulations71,76,77,78,79,80.
The first method was selected because the pharmacopeial method is frequently employed in the literature for assessing disintegration behavior. This method is considered useful due to its constant movement upward and downward (30 moves/min) and the inclusion of disks. The disk can mimic the action of the tongue, which is relevant for evaluating in vivo disintegration. Several studies have reported that in vivo disintegration behavior has been evaluated, and disintegration times are faster than those reported in vitro tests78.
The disintegration time was evaluated according to Ph. Eur. 11 requirements for the disintegration behavior of ODTs. Three formulations met the recommended criteria: the blank formulations (ODBF1 and ODBF2) and CBD-ODF2. In contrast, CBD-ODF1 did not disintegrate within the specified time frame. At the end of the experiment, CBD-ODF1 appeared hydrated and became opaque, forming white films with a softer texture, yet it did not fully disintegrate. This observation suggests the possible entrapment of the API within the film-forming agent matrix, potentially resulting in a slower or incomplete release of CBD79.
The ODFs containing PVA showed better disintegration times compared to those formulated with HPMCE3, with PVA being one of the polymers recognized for its superior disintegration ability when incorporated in a polymeric matrix81.
Due to the non-Gaussian distribution of data, the Kruskal‒Wallis test was used to evaluate whether the differences between the medians were statistically significant. The tests indicated a significant variation among the medians (p = 0.0019). A statistically significant difference was recorded between ODBF2 and CBD-ODF1 (p < 0.05), which can be attributed to the use of polymers and the incorporation of CBD in the CBD-ODF1 formulation (Fig. 4g).
The second disintegration test (slide frame method) was chosen because of the specific pharmaceutical formulation developed (ODF) and extensive literature research recommending this evaluation method for the ODFs. Unlike the first method, this approach lacks standardized requirements. The method is suitable due to the small amount of water used (2–3 drops), which mimics the presence of saliva in the oral cavity, and the water temperature, which closely matches that of saliva (37 °C). Some disadvantages associated with solvent selection for evaluating disintegration behavior were mentioned earlier in the first method. No significant differences were observed between the proposed formulations (Fig. 4h). Using this method, the disintegration times for the CBD-ODFs were greater than 180 s, whereas, in the pharmacopeial method, CBD-ODF2 showed better disintegration behavior. Considering that disintegration time is a preamble to the dissolution test, CBD-ODF2 might release more API than CBD-ODF1. This inference could be supported by the appearance of CBD-ODF1 at the end of the disintegration test, a white film that maintained its form, with slight consistency differences observed. The film tended to be somewhat softer and had a gel-like consistency on its surface, while the core remained unmodified, indicating a hydration phenomenon.
Because disintegration behavior is considered a preamble to the dissolution test, sometimes only the dissolution test is conducted, even though it is important to recognize that the disintegration test holds significance and can aid in identifying formulations that do not meet the preestablished pharmacopeial requirements.
In many cases, a variation in disintegration time between the blank and the API-ODFs is noticed, with the latter exhibiting higher disintegration times. CBD is a lipophilic ingredient which repels water and reduces the wettability of the film, hindering water penetration and, as a result, delaying the disintegration time. Another aspect that might be responsible for the variation in disintegration time in the case of blank versus CBD-ODF is the fact that the active ingredient produced thicker ODFs, and as a result, the disintegration time was negatively affected.
One method that has been discussed lately for improving disintegration behavior is the use of disintegrants. The results regarding the use of disintegrants are equivocal, even if in some cases the disintegration time is improved, in many cases the polymeric matrix tends to be altered and the disintegrant/superdisintegrant tends to be suspended in the mixture that will be poured. As a result, when the film is dried, heterogeneous ODFs are obtained, which are not very appealing from a macroscopic point of view, and the film also loses its smoothness, becoming rougher. In the literature, several methods are mentioned for assessing disintegration behaviour. In a previously published study, disintegration time was evaluated via the pharmacopeial and slide frame method, where all the formulations adhered to the proposed requirements for this parameter (< 180 s). The results indicated that variations in the polymer used as a film-forming agent and the substitution of citric acid with sodium benzoate led to statistically significant differences when the basket-rack assembly was used71.
CBD assay
The method’s specificity and linearity were assessed to evaluate the CBD concentration from the CBD-ODFs. For the specificity evaluation, the ODBFs were selected as blanks to eliminate the risk of interference from other ingredients that might absorb at a wavelength of 209 nm (Fig. 3 – Supplementary). Linearity was determined in the 1–25 µg/mL range, considering the ICH requirements and the maximum amount that might be released in the dissolution medium within 30 min82. One of the parameters that highlighted the linearity is R2, with a value of 0.9975 (Fig. 4i).
Statistical analysis revealed a significant difference between the medians of the CBD-ODFs (9.01 for CBD-ODF1 and 10.21 for CBD-ODF2), with a p-value of 0.0022 (Fig. 4j). The difference between the two can be explained by the fact that two different polymers served as film-forming agents. Even though the number of statistical differences between the blank ODFs was limited when the API was introduced in the matrix, several alterations occurred due to the polymers’ different physico-chemical properties, which were reflected in the evaluated properties of the ODFs.
Dissolution profiles
Drug release is typically evaluated according to the requirements for solid dosage forms via either the basket or paddle method. In this study, the basket method was selected to prevent film flotation.
Differences in dissolution behavior were observed between the two CBD-ODFs; for the first formulation, less than 25% of CBD was released at 30 min, whereas for CBD-ODF2, almost 100% was released in the same timeframe (Fig. 5). Although some pharmacopeias recommend evaluating the amount of API released for 60 min, the test was conducted for 1 h for CBD-ODF1, yet less than 30% of CBD was released. Differentiation in the dissolution test is evident from the beginning of the process, with the second formulation showing greater API release. This trend persisted throughout the experiment at all the time points used for the dissolution test. The lower amount of API release in the case of CBD-ODF1 can be correlated with the low disintegration behavior, as mentioned earlier; it is possible that the API was included in the film matrix and was not released due to its core consistency.
The CBD and PVA combination elevated the API solubility in the dissolution media. Furthermore, the polymeric matrix was not completely dispersed in the dissolution media in the case of CBD-ODF1, highlighting that a portion of the API remained in the undispersed ODF as a result, the amount of API detected in the case of the dissolution test was lower in the case of this formulation.
The European Medicines Agency (EMA) has established recommendations for solid dosage forms regarding dissolution tests. CBD-ODF2 meets the third requirement mentioned in the “Reflection paper on the dissolution specification for generic solid oral immediate release products with systemic action”, where > 85% of the API is released at 30 min. This aligns with the dissolution specification limit (Q average value at a preestablished time point), which should fall between 75% and 85%83.
A comparison of the results obtained in this study with those of other studies that incorporated CBD into a polymeric matrix revealed that no dissolution test results for CBD-ODFs are available at the moment.
In other studies that conducted similar tests, the amount of CBD released ranged between 7% and 19%62, the differences depending on the quantities of CBD oils used (10% CBD oil − 7% CBD was released, 5% CBD oil − 19% CBD was released, and 1% CBD oil − 8% CBD was released) at 5100 min (85 h). Comparing the amounts released at 20 min with the results obtained in this study, the CBD released in this study was higher, which is correlated (in both cases) with the aim of the study (fast release in this case) in contrast to extended release in the case of chitosan-CBD films used for wound dressings.
Another group of researchers reported an amount of CBD released in the case of some 3D buccal films of 84% at 6 h and less than 15% at 30 min, which is lower than the amount released in this study but consistent with their intended purpose63.
Correlation study – Pearson/Spearman coefficients
The first step of the statistical analysis consisted of eliminating the outliers, followed by the normality test. If the results for both the colloidal dispersions and suspensions, as well as the ODF properties, followed a bell-shaped distribution, the Pearson coefficient (r) was calculated, whereas in cases where a non-Gaussian distribution was observed, the Spearman coefficient (rs) was calculated. The results regarding the coefficients are presented in Table 6, where the Pearson coefficients are marked with black, and the Spearman coefficient is marked with blue.
A statistically significant linear relationship was observed between the DCBD2 viscosity at the 12th gear and the adhesivity of CBD-ODF2 (r=-0.99, p = 0.0351), indicating that an increased viscosity may be reducing the ability of the film to stick to surfaces. A strong positive correlation was observed between the conductivity and adhesivity of DB1 (r = 0.97), although this correlation was not statistically significant. Conversely, a strong negative correlation was noted between the same colloidal dispersion property and the methods applied to assess disintegration behavior (pharmacopeial method, r=-0.94, p = 0.2172), and (slide frame method, r=-0.94, p = 0.2172) implying that higher conductivity leads to increased disintegration times. For the conductivity measured in the DB2 formulation, a strong negative correlation was observed with the ODF’s uniformity of mass (r=-0.74, p = 0.0589) and pH (r = −0.95, p = 0.1957), and a strong positive correlation was found with the ODF’s adhesivity (r = 0.96, p = 0.1749). Other strong positive or negative correlations that were not statistically significant are presented in Table 6.
Materials and methods
To prepare the blank colloidal dispersions, CBD suspensions, and the ODFs, the following ingredients were used: cannabidiol (Trigal Pharma, Vienna, Austria, 99.5% purity), Vivapharm® HPMCE3 (29% methoxy groups and 10% hydroxypropyl groups, for which a 2% dispersion provides a viscosity of 3 cPs) (JRS Pharma, Rosenberg, Germany), PVA (JRS PHARMA, Rosenberg, Germany), 1,2-propylene glycol (Scharlau, Barcelona, Spain), sucralose (Myprotein, Bucharest, Romania), citric acid (ViVoCHem, Almelo, The Netherlands), ethanol 96 (%V/V) (Chimreactiv S.R.L., Bucharest, Romania), and distilled water obtained with a Direct Q3 System apparatus (Millipore, Bucharest, Romania).
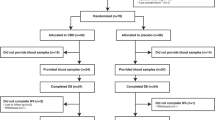
Four formulations of dispersions were prepared through magnetic stirring: two colloidal dispersions—blanks: DB1 and DB2 - and two CBD suspensions (DCBD1 and DCBD2) (Table 5).
The steps (coded from A-F) required to obtain the blank colloidal dispersions, CBD suspensions, blank ODFs, and CBD-ODFs are described in Fig. 6. The first steps, coded from A to C, must be followed to obtain the blank colloidal dispersions or CBD suspensions; subsequently, if all steps from A to F are followed, the ODF films will be obtained as mentioned previously:
-
A.
Sucralose, citric acid, HPMCE3 or PVA, and PG were dissolved/dispersed/mixed under continuous stirring (1000 rpm) in distilled water, resulting in the first colloidal dispersion (Dispersion A). HPMCE3 was used for DB1 and DCBD1, whereas PVA was used for DB2 and DCBD2.
-
B.
The second step consisted of a solution preparation (CBD dissolved in ethanol) for DCBD1 and DCBD2 (Solution A).
-
C.
Solution A was added under continuous stirring to the aqueous dispersion, resulting in two suspensions, DCBD1 and DCBD2.
-
D.
A total of 9.58 g of the colloidal dispersions/suspensions were poured into Petri dishes with a total surface area of 69.36 cm2, corresponding to 2.22% (w/w) CBD, yielding blank films labeled ODBF1 and ODBF2 and CBD-ODFs labeled CBD-ODF1 and CBD-ODF2.
-
E.
The cast films will be kept at room temperature (20 ± 2 °C) for 24 h so that the solvent evaporates, resulting in thin films.
-
F.
The ODFs were cut manually with a circular-sharpened mold (diameter = 2 cm) and a total surface area of 3.14 cm2 with 10 mg of CBD/surface.
Preformulation studies
DSC results
DSC analysis was employed to assess the absence of interactions between the CBD and each of the selected excipients. The DSC study was carried out with a DSC Shimadzu 60 (Shimadzu, Japan). A quantity of 5 mg from each sample (active ingredient, excipient, and a binary mixture 1:1 (w/w mass ratio) consisting of the API and an excipient) was introduced into aluminum pans (40 µL) under an ambient air atmosphere. The temperature ranged from 30 to 300 °C, with the heating rate set at 5 °C/min. The obtained results were plotted using OriginPro 2023 software (OriginLab Corporation, Northampton, USA).
FTIR spectroscopy evaluation
To obtain the FTIR spectra, CBD, excipients, and binary mixtures (1:1) were analyzed via an IR Thermo Nicolet 380 FTIR spectrophotometer (Thermo Fischer Scientific, MA, USA). The acquisition was performed by averaging 128 scans in the range of 4000–400 cm− 1, with a spectral resolution of 8 cm− 1, using Omnic 8.0 software and Spectragryph 1.2 for results evaluation. The background, which consisted of potassium bromide (ChiraSol GmbH, Germany) scanning, was updated every 30 min. A hydraulic press (Specac, United Kingdom) was used to obtain transparent tablets for the API, excipients (individually), and binary mixtures (1:1).
Investigations of CBD suspensions and colloidal dispersions
pH (DB1, DB2, DCBD1, DCBD2)
For the selected dispersions, pH was assessed by diluting 1 mL of dispersion with 9 mL of ultrapure water. The pH values of the samples were measured in triplicate using a Consort C831 multiparameter analyzer (Parklaan, Turnhout, Belgium).
Conductivity (DB1, DB2, DCBD1, DCBD2)
Electrical conductivity was measured on six samples of 10 g each, poured into a beaker using a Consort C831 multiparameter analyzer (Parklaan, Turnhout, Belgium). The results are expressed as the mean ± SD. Statistical analysis was conducted via the Kruskal‒Wallis test and Dunn’s multiple comparisons test with GraphPad Prism 10 software (Dotmatics, Boston, MA, USA).
Particle size distribution-CBD suspensions (DCBD1, DCBD2)
One drop of CBD suspension (previously mixed) was dispensed on a microscope slide and covered with a glass coverslip. The particle dimension was assessed with an Optika P190 electronic microscope (Optika microscope, Ponteranica, Italy) with a 40x lens. The particle size distribution was evaluated through a microscopic method, wherein 25 particles from the CBD suspension were measured. The mean size was calculated and expressed as the average ± SD. To facilitate comparison, the smallest and largest-sized particles were identified, and the difference between the maximum and minimum values was calculated, yielding the interval denoted as D. Dividing this large interval by five (representing the number of small intervals), the d value was obtained. The d value helps establish the limits of the five proposed intervals for each of the two suspensions. A granulometric distribution curve was then plotted, allowing for the determination of the average particle size corresponding to the highest frequency (N %) from the pictogram. Additionally, the PdI was calculated as the ratio between the squared standard deviation with the squared average size.
Viscosity and tangential stress evaluation (DB1, DB2, DCBD1, DCBD2)
A Rheotest RV (RHEOTEST Medingen GmbH, Ottendorf-Okrilla, Germany) equipped with two coaxial cylinders (S/S1) was used for the evaluation of the proposed samples. The sample was introduced into the external cylinder (30 mL), and the examination began by gradually increasing the first shear rate from the first to the twelfth rotation speed of the internal cylinder, inducing shear thinning of the dispersions. This step was followed by a gradual decrease in the rotation speed (from 12 to 1), a process known as restructuring (when it occurs). The force opposing rotation (α) was evaluated for each rotation speed applied, and the viscosity (cP) and tangential stress (dyne/cm2) were calculated accordingly.
Spreadability (DB1, DB2, DCBD1, DCBD2)
For the spreadability test, a 1 g sample was placed in a 1 cm diameter circle on a glass surface, beneath which millimetric paper was positioned. The sample was covered with a previously weighed glass plate, and the diameter occupied by the sample was measured after 30 s. Successive weights (10, 20, 50, 100, 200, 300, 400, and 500 g) were added, and after each addition, the diameter (cm) and surface area (S - cm2) occupied by the sample were recorded. Each sample was evaluated in triplicate, and spreadability curves were plotted for all four formulations.
CBD assay in CBD suspensions (DCBD1, DCBD2)
The CBD concentration in the CBD suspensions was assessed via a previously validated HPLC method84. DB1 and DB2 were used as blank samples to verify the specificity of the method. A stock solution of 1 mg/mL was prepared by dissolving CBD in acetonitrile, and further dilutions were made to verify the linearity of the method within the range of 1–50 µg/mL.
Chromatograms were obtained with a Hitachi LaChrom Elite HPLC system (Hitachi LaChrom Elite HPLC System, San Jose, CA, USA) at a wavelength of 209 nm with a Gemini NX-C18 column with dimensions of 3.0 × 100 mm and a particle size of 3 μm. The elution was isocratic, and the mobile phase consisted of 70% (v/v) acetonitrile and 30% (v/v) ultrapure water with a flow rate of 1 mL/min. The suspensions were dispersed in a mixture of 50:50 (% V/V) water and acetonitrile (100 µL of sample diluted with the solvent mixture to 100 mL), followed by a further dilution of 1:10, resulting in a theoretical concentration of 23.2 µg/mL. A volume of 10 µL was injected for evaluation of the CBD concentration.
Evaluation of CBD-ODFs
Since the API had a very high purity, the reproducibility and effectiveness of the final ODF formulations were not altered. This high purity implies:
-
Minimal variability of the active ingredient;
-
Reduced risk of unwanted interactions with excipients;
-
High purity implies a reduced risk of API content variation;
Also, if impurities are outlined in the API, there is an increased risk of reducing the shelf life and more stable pharmacological activity.
Organoleptic properties
The films were evaluated in terms of their organoleptic properties, including color, opacity/transparency, and surface roughness/smoothness.
Weight uniformity
Taking into consideration the requirements outlined in Ph. Eur. 11, the average mass of the ODFs was determined by individually weighing 20 ODFs (A = 3.14 cm2) from each series. The average weight recommendation was compared with the specification specified in Ph. Eur. 11 (Chap. 2.9.5), which pertains to the uniformity of the mass of single-dose preparations79.
Thickness
To evaluate the thickness, 10 ODFs (A = 3.14 cm2) were randomly selected, and for each film, the thickness was measured at five locations using a digital micrometer (Yuzuki, India) with a precision of 0.001 mm. The results are expressed as the mean ± SD.
Folding endurance
This mechanical parameter was evaluated by subjecting the film (A = 3.14 cm2) to repeated folds at the same spot until it cracked or broke. Folding endurance was assessed on three ODFs from each series, and the results are expressed as the mean ± SD.
Thickness-normalized tensile strength
Through this test, the breaking ability was evaluated using an in-house manufactured instrument. Three circular films for which the thickness and mass had been previously determined to be S = 3.14 cm2 were placed between two clamps (upper-fixed and lower-mobile). On the lower clamp, weights were added in increments of 5 g successively until the film broke. To calculate the thickness-normalized tensile strength, Eq. (1) was applied:
where: TS - thickness-normalized tensile strength (N/mm2); M - the final mass at which the ODF broke (kg); g - gravitational acceleration (9.81 N*kg− 1); W - sample width (mm); T - ODF average thickness (mm)71,76,85.
Adhesivity
Adhesivity was evaluated by employing an in-house apparatus. The circular-shaped ODF, with S = 3.14 cm2, was placed between a metallic surface and the left plate of the scale. Two drops of distilled water were added to the ODF to moisten the sample, and a small weight of 2 grams was added to exert slight pressure. Weights were added to the opposite plate in ascending order until the detachment of the left plate from the ODF was observed71,76. The detachment force was expressed in N/cm2 and was calculated via Eq. (2):
where F - detachment force (N/cm2); M - the applied mass needed for detachment (kg); g - gravitational acceleration (9.81 m/s2); S - ODF area (3.14 cm2).
Measurement of pH
To achieve good compliance from patients, this parameter is extremely important. For the pH evaluation, one ODF (S = 3.14 cm2) from each batch was dissolved (blank ODFs) or dispersed (CBD-ODFs) in 20 mL of ultrapure water. Afterwards, the solution/dispersion mixture was filtered through a Millipore filter (Ø=0.45 μm), and the pH of the filtrate was measured using a pH meter (pH Check, TFA Dostmann, Wertheim am Main, Germany)77,85. The pH evaluation was conducted in triplicate, and the results are expressed as the mean ± SD.
Disintegration ability
The disintegration ability was evaluated via the following methods:
-
a.
The pharmacopeial method involved a disintegration tester consisting of a thermostated bath, a Berzelius beaker with a capacity of 1000 mL, and a basket-rack assembly (mobile part, containing six glass tubes), which could be coupled with the TFUT-3 (Tablet Four-usage Tester, China). The beaker was filled with 600 mL of distilled water thermostated at 37 ± 1 °C and placed into the apparatus. The basket-rack assembly continuously moved upward and downward (28–32 rpm) until either no palpable mass (fully disintegrated) or a soft mass with no palpable core was observed11,79,80.
-
b.
The slide frame method involved placing a film over a tube with a 1.5 cm diameter by adding 3 drops of distilled water heated to 37 ± 1 °C with an Eppendorf pipette/dropper. Disintegration evaluation commenced when the third drop was placed on the polymeric film, and the end of the experiment was determined when the film cracked, broke, or /disintegrated due to water action. The test was conducted on six samples, and the results are expressed as the average ± SD71.
CBD assay in ODFs
CBD content was assessed through a UV spectrophotometric method using a Shimadzu 1800 spectrophotometer (Mettler Toledo, Columbus, OH, USA). To evaluate the linearity of the method, 0.1000 g of CBD was weighed and dispersed in 100 mL of acetonitrile, resulting in a 1 mg/mL stock solution, and subsequent dilutions were made with the dissolution media used (phosphate buffer containing 0.052 M sodium lauryl sulfate) adjusted to pH = 6.8 to generate the linearity curve. The linearity was verified in the concentration range of 1–25 µg/mL, and for each sample, the absorbance was measured at 209 nm. To avoid interference from other excipients, ODBF1 and ODBF2 were used as blanks for CBD-ODF1 and CBD-ODF2, respectively.
To determine the CBD content, three films (A = 3.14 cm2) from each formulation were dispersed in 10 mL dissolution medium in a 10 mL volumetric flask. A dilution of 1:100 was applied using the same dissolution medium. The theoretical concentration was predetermined within the previously mentioned concentration range (10 µg/mL).
Given that only two samples were evaluated for the CBD assay, an unpaired t-test with Welch’s correction was applied.
Dissolution profiles
For this test, the amount of active pharmaceutical ingredient dissolved as a function of time was evaluated (n = 3, A = 3.14 cm2). The two main dissolution apparatus types are differentiated by the agitator: basket (type 1) and paddle (type 2). Considering that ODFs have an increased risk of floating, the basket type was selected for further evaluation. The following conditions were applied to perform this test:
-
The glass vessel was filled with 900 mL of buffer (pH = 6.8) and heated at 37 ± 0.5 °C to heat the media close to body temperature.
-
Three ODFs were placed in three different glass vessels containing 900 mL of buffer;
-
The number of rotations is set at 50 rpm;
-
Five-milliliter aliquots were removed at 2, 5, 10, 15, 20, and 30 min, and the withdrawn volume was substituted with fresh dissolution media previously heated in the pre-established temperature range.
-
The sample absorbances were read at 209 nm, and the dissolution media in which the ODBFs (ODBF1 or ODBF2) were introduced via a spectrophotometric method were used as blanks;
-
The results were presented graphically showing amount of API released as a function of time with the vertical standard deviation (SD) bars included at each sampling point.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 10 software (Dotmatics, Boston, MA, USA) through the ROUT test to eliminate one or more outliers with Q = 1%, followed by a normality test (Shapiro‒Wilk test), which revealed whether the data distribution was Gaussian or non-Gaussian. If the distribution was Gaussian, ANOVA-derived tests were used, assuming unequal e SDs (Brown‒Forsythe ANOVA, Welch one-way ANOVA, and Dunnett’s T3 multiple comparisons test), whereas if the residuals followed a non-Gaussian distribution, a nonparametric test was performed—Kruskal‒Wallis and Dunn’s multiple comparisons test. The results are presented as the mean ± SD. The significance level was set to 0.05 (p), with the p values presented as asterisks in the results and discussion sections:
-
ns (p > 0.05), ns - not significant;
-
* (p < 0.05);
-
** (p < 0.01);
-
*** (p < 0.001);
-
**** (p < 0.0001).
Pearson/Spearman correlation coefficient.
The first two steps mentioned in the previous subchapter were also applied while establishing a correlation between the colloidal dispersion/suspension properties and the properties belonging to the ODFs (the ROUT test was used to eliminate the outliers and the normality test). If the data followed a Gaussian distribution, the Pearson (r) coefficient was calculated, whereas if a non-Gaussian distribution was observed, the Spearman coefficient (rs) was calculated. The Pearson correlation coefficient was calculated to assess the linear correlation (significant relationship) between the blank colloidal dispersions/CBD suspensions and the blank-ODFs and CBD-ODFs. This test also allowed the identification of positive or negative correlations. For this evaluation, the conductivity, pH, and viscosity at the 12th shear rate were considered for the colloidal dispersions/suspensions and the dimensional, mechanical, and disintegration properties of the ODFs. The strengths and directions of the correlations were evaluated, and statistically significant differences were considered (p < 0.05) in the Results and Discussion sections. All the correlations are compiled in Table 7, with statistically significant correlations highlighted.
Conclusions
Four formulations (two blank ODFs and two CBD-ODFs) were developed to establish the influence of the API and the selected polymer on the characteristic properties of the ODFs. Disintegration behavior serves as a useful tool for screening in vitro dissolution performance, as inadequate disintegration behavior within a predefined timeframe may result in lower API release than needed. Since CBD belongs to Biopharmaceutics Classification System (BCS) Class II and has low solubility in water, one of the critical tests during film evaluation is the in vitro dissolution test, as ODFs are expected to dissolve rapidly. Consequently, the CBD-ODF2 formulation demonstrated faster dissolution than CBD-ODF1, making it potentially suitable for buccal administration if the adhesivity is improved. Balancing mechanical and disintegration/dissolution properties is crucial to obtain a pharmaceutical formulation that meets ODF quality attributes (such as easy handling and fast disintegration/dissolution). pH evaluation close to that of saliva is recommended for administration, although patient acceptance and saliva pH may vary.
The correlation between colloidal dispersions /suspensions and CBD-ODF properties highlights several shared evaluation parameters, such as content and pH. A significant negative correlation was observed.
While the results apply to this study, conducting a more extensive investigation involving additional film-forming agents and APIs from different BCS categories is recommended to support extrapolation. Additionally, considering that the physicochemical properties of the APIs vary greatly, these characteristics represent major influencing factors for colloidal dispersion behaviors. Formulations can be further optimized by applying Quality by Design (QbD) to obtain ODFs that meet both the initial development requirements and those outlined in the literature.
Data availability
All the relevant data generated and analyzed during this study, which include experimental, spectroscopic, and statistical data, are included in this article and its supplementary information.
References
Ward, R. M. Improving drug therapy for pediatric patients: unfinished history of pediatric drug development. J. Pediatr. Pharmacol. Ther. 28, 4–9. https://doi.org/10.5863/1551-6776-28.1.4 (2023).
D’Errico, S. et al. Medication errors in pediatrics: proposals to improve the quality and safety of care through clinical risk management. Front. Med. 8, 1–7. https://doi.org/10.3389/fmed.2021.814100 (2022).
Smith, L., Leggett, C. & Borg, C. Administration of medicines to children: a practical guide. Aust Prescr. 45, 188–192. https://doi.org/10.18773/austprescr.2022.067 (2022).
Galande, A. D., Khurana, N. A. & Mutalik, S. Pediatric dosage forms-challenges and recent developments: A critical review. J. Appl. Pharm. Sci. 10, 155–166. https://doi.org/10.7324/JAPS.2020.10718 (2020).
Wadher, K., Dhote, K., Mane, M., Khapne, A. & Umekar, A. G. M. Orodispersible dosage form: advancement and challenges (SJS). Int. J. Pharm. Res. Heal Sci. 7, 3013–3019. https://doi.org/10.21276/ijprhs.2019.04.01 (2019).
Edman, P. Pharmaceutical formulations— suspensions and solutions. J. Aerosol Med. Depos. Clear. Eff. Lung. 7, 3–6. https://doi.org/10.1089/jam.1994.7.suppl_1.s-3 (1994).
Doye, P., Mena, T. & Das, N. Formulation and bio-availability parameters of pharmaceutical suspension. Int. J. Curr. Pharm. Res. 9, 8–14. https://doi.org/10.22159/ijcpr.2017.v9i3.18892 (2017).
Kumar, S., Dongre, S. S., Demappa, R., Sannappa, J. & T. & Structural and mechanical characteristic study of HPMC polymer composite films. IOP Conf. Ser. Mater. Sci. Eng. 1221, 012011. https://doi.org/10.1088/1757-899X/1221/1/012011 (2022).
Praneta, D. Pharmaceutical suspensions: pharmacist has the very best possible formulation for the job at hand. Res. J. Pharm. Forms Tech. 5, 51–55 (2013).
Slavkova, M. & Breitkreutz, J. Orodispersible drug formulations for children and elderly. Eur. J. Pharm. Sci. 75, 2–9. https://doi.org/10.1016/j.ejps.2015.02.015 (2015).
Cilurzo, F., Musazzi, U. M., Franzé, S., Selmin, F. & Minghetti, P. Orodispersible dosage forms: biopharmaceutical improvements and regulatory requirements. Drug Discov Today. 23, 251–259. https://doi.org/10.1016/j.drudis.2017.10.003 (2018).
Jacob, S., Boddu, S. H. S., Bhandare, R., Ahmad, S. S. & Nair, A. B. Orodispersible films: current innovations and emerging trends. Pharmaceutics 15, 1–41. https://doi.org/10.3390/pharmaceutics15122753 (2023).
Musazzi, U. M. et al. Personalized orodispersible films by hot melt Ram extrusion 3D printing. Int. J. Pharm. 551, 52–59. https://doi.org/10.1016/j.ijpharm.2018.09.013 (2018).
Desai, N. et al. Modernising orodispersible film characterization to improve palatability and acceptability using a toolbox of techniques. Pharmaceutics 14, 1–15. https://doi.org/10.3390/pharmaceutics14040732 (2022).
Musazzi, U. M., Khalid, G. M., Selmin, F., Minghetti, P. & Cilurzo, F. Trends in the production methods of orodispersible films. Int. J. Pharm. 576, 118963. https://doi.org/10.1016/j.ijpharm.2019.118963 (2020).
Gupta, M. S., Gowda, D. V., Kumar, T. P. & Rosenholm, J. M. A comprehensive review of patented technologies to fabricate orodispersible films: proof of patent analysis (2000–2020). Pharmaceutics 14, 1–30. https://doi.org/10.3390/pharmaceutics14040820 (2022).
Janssen, E. M., Schliephacke, R., Breitenbach, A. & Breitkreutz, J. Drug-printing by flexographic printing technology – a new manufacturing process for orodispersible films. Int. J. Pharm. 441, 818–825. https://doi.org/10.1016/j.ijpharm.2012.12.023 (2013).
Pacheco, M. S., Barbieri, D., da Silva, C. F. & de Moraes, M. A. A review on orally disintegrating films (ODFs) made from natural polymers such as Pullulan, maltodextrin, starch, and others. Int. J. Biol. Macromol. 178, 504–513. https://doi.org/10.1016/j.ijbiomac.2021.02.180 (2021).
Cornilă, A., Iurian, S., Tomuță, I. & Porfire, A. Orally dispersible dosage forms for pediatric use: current knowledge and development of nanostructure-based formulations. Pharmaceutics 14, 1621. https://doi.org/10.3390/pharmaceutics14081621 (2022).
Centkowska, K., Ławrecka, E. & Sznitowska, M. Technology of orodispersible polymer films with micronized loratadine—influence of different drug loadings on film properties. Pharmaceutics 12, 250. https://doi.org/10.3390/pharmaceutics12030250 (2020).
Burdock, G. A. Safety assessment of hydroxypropyl Methylcellulose as a food ingredient. Food Chem. Toxicol. 45, 2341–2351. https://doi.org/10.1016/j.fct.2007.07.011 (2007).
Quinten, T., De Beer, T., Remon, J. P. & Vervaet, C. Overview of injection molding as a manufacturing technique for pharmaceutical applications (2010). https://www.researchgate.net/publication/287590984_Overview_of_injection_molding_as_a_manufacturing_technique_for_pharmaceutical_applications.
Kumar Verma, P., Arora, K. & Vats, V. Annals of clinical case reports a review on pharmaceutical suspension and its advancement. Ann. Clin. Case Rep. 7, 2321. https://doi.org/10.25107/2474-1655.2321 (2022).
Ghadermazi, R., Hamdipour, S., Sadeghi, K., Ghadermazi, R. & Khosrowshahi Asl, A. Effect of various additives on the properties of the films and coatings derived from hydroxypropyl methylcellulose—a review. Food Sci. Nutr. 7, 3363–3377. https://doi.org/10.1002/fsn3.1206 (2019).
Oh, C. M., Heng, P. W. S. & Chan, L. W. A study on the impact of hydroxypropyl Methylcellulose on the viscosity of PEG melt suspensions using surface plots and principal component analysis. AAPS PharmSciTech. 16, 466–477. https://doi.org/10.1208/s12249-014-0204-x (2015).
Jadach, B., Misek, M. & Ferlak, J. Comparison of hydroxypropyl Methylcellulose and alginate gel films with meloxicam as fast orodispersible drug delivery. Gels 9, 687. https://doi.org/10.3390/gels9090687 (2023).
da Silva, P. C. & Colucci, L. A. Mechanical, optical, and physicochemical properties of HPMC-based Doxazosin mesylate orodispersible films. Braz J. Pharm. Sci. 59, 1–18. https://doi.org/10.1590/s2175-97902023e21114 (2023).
Zaki, R. M. et al. Fabrication and characterization of orodispersible films loaded with solid dispersion to enhance Rosuvastatin calcium bioavailability. Saudi Pharm. J. 31, 135–146. https://doi.org/10.1016/j.jsps.2022.11.012 (2023).
Panraksa, P. et al. Hydroxypropyl Methylcellulose E15: a hydrophilic polymer for fabrication of orodispersible film using syringe extrusion 3D printer. Polymers 12, 2666. https://doi.org/10.3390/polym12112666 (2020).
Yan, T. T. et al. Semisolid extrusion 3D printing ODFs: an individual drug delivery system for small scale pharmacy. Drug Dev. Ind. Pharm. 46, 531–538. https://doi.org/10.1080/03639045.2020.1734018 (2020).
Antonoaea, P. et al. Comparative analysis of the release performance of indomethacin from transdermal therapeutic systems. Farmacia 68, 1029–1035. https://doi.org/10.31925/farmacia.2020.6 (2020).
Cao, Q. R., Choi, Y. W., Cui, J. H. & Lee, B. J. Effect of solvents on physical properties and release characteristics of monolithic hydroxypropylmethylcellulose matrix granules and tablets. Arch. Pharm. Res. 28, 493–501. https://doi.org/10.1007/BF02977682 (2005).
Liu, B., Zhang, J. & Guo, H. Research progress of Polyvinyl alcohol water-resistant film materials. Membranes 12, 1–13. https://doi.org/10.3390/membranes12030347 (2022).
Gaaz, T. S. et al. Properties and applications of Polyvinyl alcohol, Halloysite nanotubes and their nanocomposites. Molecules 20, 22833–22847. https://doi.org/10.3390/molecules201219884 (2015).
Aslam, M., Kalyar, M. A. & Raza, Z. A. Polyvinyl alcohol: a review of research status and use of Polyvinyl alcohol based nanocomposites. Polym. Eng. Sci. 58, 2119–2132. https://doi.org/10.1002/pen.24855 (2018).
Gherman, S. P. et al. Biomaterials based on Chitosan and Polyvinyl alcohol as a drug delivery system with wound-healing effects. Gels 9, 122. https://doi.org/10.3390/gels9020122 (2023).
Shi, L. L., Xu, W. J., Cao, Q. R., Yang, M. & Cui, J. H. Preparation, characterization and in vitro evaluation of a Polyvinyl alcohol/sodium alginate based orodispersible film containing sildenafil citrate. Pharmazie 69, 327–334 (2014). PMID: 24855822.
Wei, T. et al. Development of Polyvinyl alcohol/polyethylene glycol copolymer-based orodispersible films loaded with Entecavir: formulation and in vitro characterization. Curr. Drug Deliv. 21, 1362–1374. https://doi.org/10.2174/0115672018261294231024093926 (2024).
Liu, J. et al. The role of hydrophilic/hydrophobic group ratio of Polyvinyl alcohol on the miscibility of amlodipine in orodispersible films: from molecular mechanism study to product attributes. Int. J. Pharm. 630, 122383. https://doi.org/10.1016/j.ijpharm.2022.122383 (2023).
El-Setouhy, D. A. & Abd El-Malak, N. S. A. Formulation of a novel Tianeptine sodium orodispersible film. AAPS PharmSciTech. 11, 1018–1025. https://doi.org/10.1208/s12249-010-9464-2 (2010).
Jamróz, W. et al. 3D printed orodispersible films with Aripiprazole. Int. J. Pharm. 533, 413–420. https://doi.org/10.1016/j.ijpharm.2017.05.052 (2017).
Atalay, S., Jarocka-Karpowicz, I. & Skrzydlewska, E. Antioxidative and anti-inflammatory properties of Cannabidiol. Antioxidants 9, 1–20. https://doi.org/10.3390/antiox9010021 (2019).
Grifoni, L., Vanti, G., Donato, R., Sacco, C. & Bilia, A. R. Promising nanocarriers to enhance solubility and bioavailability of Cannabidiol for a plethora of therapeutic opportunities. Molecules 27, 6070. https://doi.org/10.3390/molecules27186070 (2022).
Jennotte, O., Koch, N., Lechanteur, A. & Evrard, B. Formulation and quality consideration of Cannabidiol printed forms produced by fused-deposition modeling. J. Drug Deliv Sci. Technol. 87, 104837. https://doi.org/10.1016/j.jddst.2023.104837 (2023).
McGuire, P. et al. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial. Am. J. Psychiatry. 175, 225–231. https://doi.org/10.1176/appi.ajp.2017.17030325 (2018).
Thiele, E. A. et al. Cannabidiol in patients with seizures associated with Lennox-Gastaut syndrome (GWPCARE4): a randomized, double-blind, placebo-controlled phase 3 trial. Lancet 391, 1085–1096. https://doi.org/10.1016/S0140-6736(18)30136-3 (2018).
Devinsky, O. et al. Trial of Cannabidiol for drug-resistant seizures in the Dravet syndrome. N Engl. J. Med. 376, 2011–2020 (2017). DOI 10.1056/NEJMoa1611618.
Furgiuele, A., Cosentino, M., Ferrari, M. & Marino, F. Immunomodulatory potential of Cannabidiol in multiple sclerosis: a systematic review. J. Neuroimmune Pharmacol. 16, 251–269. https://doi.org/10.1007/s11481-021-09982-7 (2021).
Chagas, M. H. N. et al. Effects of Cannabidiol in the treatment of patients with Parkinson’s disease: an exploratory double-blind trial. J. Psychopharmacol. 28, 1088–1098. https://doi.org/10.1177/0269881114550355 (2014).
Meuth, S. G., Henze, T., Essner, U., Trompke, C. & Vila Silván, C. Tetrahydrocannabinol and Cannabidiol oromucosal spray in resistant multiple sclerosis spasticity: consistency of response across subgroups from the SAVANT randomized clinical trial. Int. J. Neurosci. 130, 1199–1205. https://doi.org/10.1080/00207454.2020.1730832 (2020).
Valh, J. V., Peršin, Z. & Von, B. Microencapsulation of Cannabidiol in liposomes as coating. Coatings 11, 1–18. https://doi.org/10.3390/coatings11010003 (2021).
Gugleva, V. et al. Development, characterization and Pharmacological evaluation of cannabidiol-loaded long Circulating niosomes. Pharmaceutics 15, 2414. https://doi.org/10.3390/pharmaceutics15102414 (2023).
Nakano, Y., Tajima, M., Sugiyama, E., Sato, V. H. & Sato, H. Development of a novel nanoemulsion formulation to improve intestinal absorption of Cannabidiol. Med. Cannabis Cannabinoids. 2, 35–42. https://doi.org/10.1159/000497361 (2019).
Giacoppo, S. et al. A new formulation of Cannabidiol in cream shows therapeutic effects in a mouse model of experimental autoimmune encephalomyelitis. DARU J. Pharm. Sci. 23, 1–17. https://doi.org/10.1186/s40199-015-0131-8 (2015).
Štukelj, R. et al. Synthesis of stable Cannabidiol (CBD) nanoparticles in suspension. Mater. Tehnol. 53, 543–549. https://doi.org/10.17222/mit.2018.253 (2019).
Brioschi, F. A. et al. Oral transmucosal Cannabidiol oil formulation as part of a multimodal analgesic regimen: effects on pain relief and quality of life improvement in dogs affected by spontaneous osteoarthritis. Animals 10, 1–14. https://doi.org/10.3390/ani10091505 (2020).
Peng, J. et al. A narrative review of molecular mechanism and therapeutic effect of Cannabidiol (CBD). Basic. Clin. Pharmacol. Toxicol. 130, 439–456. https://doi.org/10.1111/bcpt.13710 (2022).
Russo, M. et al. Sativex in the management of multiple sclerosis-related spasticity: role of the corticospinal modulation. Neural Plast. 656582; (2015). https://doi.org/10.1155/2015/656582 (2015).
O’Sullivan, S. E. et al. The therapeutic potential of purified Cannabidiol. J. Cannabis Res. 5, 21. https://doi.org/10.1186/s42238-023-00186-9 (2023).
Epidyolex Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/epidyolex-epar-product-information_en.pdf Accessed: 09 April 2024.
Sativex® oromucosal spray. Summary of product characteristics. April (2024). https://pp.jazzpharma.com/pi/sativex.au.PI.pdf Accessed 09.
Chelminiak-Dudkiewicz, D. et al. Chitosan-based films with cannabis oil as a base material for wound dressing application. Sci. Rep. 12, 18658. https://doi.org/10.1038/s41598-022-23506-0 (2022).
Abdella, S. et al. Combining the potential of 3D printed buccal films and nanostructured lipid carriers for personalized Cannabidiol delivery. Drug Deliv Transl Res. 14, 984–1004. https://doi.org/10.1007/s13346-023-01446-0 (2024).
Klinsang, T. et al. In vitro wound healing potential of a fibroin film incorporating a cannabidiol/2-hydroxypropyl-cyclodextrin complex. Pharmaceutics 15, 2682. https://doi.org/10.3390/pharmaceutics15122682 (2023).
Edible films with CBD. https://www.optimags.de/news-cbd-edible-films/ Accessed 26 March 2024.
CHYLL sublingual strips. https://waynepatrickcp.com/products/cannabidiol-edible-film/. Accessed 26 March 2024.
Andriotis, E. G. et al. Development of food grade 3D printable ink based on pectin containing Cannabidiol/cyclodextrin inclusion complexes. Drug Dev. Ind. Pharm. 46, 1569–1577. https://doi.org/10.1080/03639045.2020.1791168 (2020).
Vlad, R. A. et al. Structural and thermal analysis of Cannabidiol orodispersible formulations. Farmacia 69, 426–433. https://doi.org/10.31925/farmacia.2021.3.5 (2021).
Vlad, R. A. et al. Pharmacotechnical and analytical preformulation studies for Cannabidiol orodispersible tablets. SPJ 29, 1029–1042. https://doi.org/10.1016/j.jsps.2021.07.012 (2021).
Senta-Loys, Z. et al. Formulation of orodispersible films for pediatric therapy: investigation of feasibility and stability for tetrabenazine as drug model. J. Pharm. Pharmacol. 69, 582–592. https://doi.org/10.1111/jphp.12627 (2017).
Vlad, R. A. et al. Preparation and evaluation of caffeine orodispersible films: the influence of hydrotropic substances and film-forming agent concentration on film properties. Polymers 15, 2034. https://doi.org/10.3390/polym15092034 (2023).
Borges, A. F. S. Development of novel pharmaceutical forms for oral administration of bioactive agents. PQDT-Glob 335, 27981776 (2015).
Visser, J. C. et al. Quality by design approach for optimizing the formulation and physical properties of extemporaneously prepared orodispersible films. Int. J. Pharm. 485, 70–76. https://doi.org/10.1016/j.ijpharm.2015.03.005 (2015).
Borges, A. F., Silva, C., Coelho, J. F. J. & Simões, S. Outlining critical quality attributes (CQAs) as guidance for the development of orodispersible films. Pharm. Dev. Technol. 22, 237–245. https://doi.org/10.1080/10837450.2016.1199567 (2017).
Ferlak, J., Guzenda, W. & Osmałek, T. Orodispersible films-current state of the art, limitations, advances and future perspectives. Pharmaceutics 15, 361. https://doi.org/10.3390/pharmaceutics15020361 (2023).
Rédai, E. M. et al. Development and evaluation of Fluoxetine fast dissolving films: an alternative for noncompliance in pediatric patients. Processes 9, 778. https://doi.org/10.3390/pr9050778 (2021).
Tamer, M. A., Hammid, S. N. A. & Ahmed, B. Formulation and in vitro evaluation of Bromocriptine mesylate as fast dissolving oral film. Int. J. Appl. Pharm. 10, 7–20. https://doi.org/10.22159/ijap.2018v10i1.22615 (2018).
Gupta, M. S. & Kumar, T. P. Characterization of orodispersible films: an overview of methods and introduction to a new disintegration test apparatus using LDR - LED sensors. J. Pharm. Sci. 109, 2925–2942. https://doi.org/10.1016/j.xphs.2020.06.012 (2020).
European Pharmacopoeia. In disintegration of tablets and capsules/uniformity of dosage units and uniformity of mass of single-dose preparations 11th ed. 345–347, 421–423, (2020). 4523 (European Commission.
The United States Pharmacopeia. Disintegration in USP-NF 701:1–4. The United States Pharmacopeial Convention, (2022).
Olechno, K., Basa, A. & Winnicka, K. Success depends on your backbone—about the use of polymers as essential materials forming orodispersible films. Materials 14, 4872. https://doi.org/10.3390/ma14174872 (2021).
European Medicines Agency. Committee for Medicinal Products for Human Use. ICH Guideline Q2 (R2) on validation of analytical procedures April (2024). https://www.ema.europa.eu/en/documents/scientific-guideline/ich-guideline-q2r2-validation-analytical-procedures-step-2b_en.pdf Accessed 09.
European Medicines Agency. Reflection paper on the dissolution specification for generic solid oral immediate release products with systemic action. April (2024). https://www.ema.europa.eu/en/documents/scientific-guideline/reflection-paper-dissolution-specification-generic-solid-oral-immediate-release-products-systemic-action-first-version_en.pdf Accessed 09.
Vlad, R. A. et al. New UHPLC method for Cannabidiol determination in hard capsules. Acta Med. Marisiensis. 65, 45–48. https://doi.org/10.2478/amma-2019-0007 (2019).
Jadhav, J. K. & Sreenivas, S. A. Formulation and in vitro evaluation of indomethacin transdermal patches using polymers HPMCE5 and Ethyl cellulose. Int J. Pharm. Sci 4, 550–556 .
Funding
This research was funded by the University of Medicine, Pharmacy, Science and Technology “George Emil Palade” of Târgu Mures, Research Grant number 164/27/10.01.2023.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by V.R-A., P. A., A.P., R.E-M, H.G., F.L., I.S., C.A. Resources were provided by B.M., M.D-L., T. S., K.K., K.L., G.R. Jr., C.A. The methodology of the study and the formal analysis were performed by V.R.-A., A.P., and C.A. The first draft of the manuscript was written by V.R-A. and P.A. All the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
All the authors consent to this final form for publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Vlad, RA., Pintea, A., Antonoaea, P. et al. Exploring the interconnected properties of cannabidiol suspensions and orodispersible films. Sci Rep 15, 21564 (2025). https://doi.org/10.1038/s41598-025-02859-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02859-2