Abstract
Creating and maintaining a stable osteogenic space is crucial for successful guided bone regeneration (GBR). This study aimed to develop a customizable composite material with a moderate degradation rate that provides sustained spatial support for GBR. An in situ embedding-reinforced strategy was proposed to develop a composite material consisting of alpha-tricalcium phosphate (α-TCP), polylactic acid (PLA), and nano-magnesium oxide (nMgO). The surface characteristics, thermal stability, strength, and hardness of the composites were tested. Biocompatibility, osteogenesis, and degradation rate were evaluated both in vitro and in vivo. Compared to PLA alone, the α-TCP/PLA/nMgO composite exhibited a fivefold increase in bending strength, surpassing 95.75 MPa, along with an improvement in surface hardness from 22.8 HV1 to 28.73 HV1. In vitro experiments demonstrated that α-TCP/PLA/nMgO exhibited minimal cell cytotoxicity, promoted excellent cell adhesion, and substantial induced osteogenesis in bone marrow mesenchymal stem cells (BMSCs). In vivo experiments in mice confirmed that α-TCP/PLA/nMgO displayed excellent biocompatibility comparable to antigen-extracted xenografts and had a moderate degradation rate that provided sustained spatial support. Importantly, the α-TCP/PLA/nMgO composite can be manufactured into personalized spatial supporting meshes in accordance with individual bone defects using CAD/CAM technology, making it a promising solution for precise guided bone regeneration in scenarios where addition supporting apparatus is needed.
Similar content being viewed by others
Introduction
Guided bone regeneration (GBR) employs barrier membranes to prevent soft-tissue invasion into the bone defect, thereby creating a stable space for bone regeneration. It has been widely adopted for alveolar bone regeneration and proven effective for reconstructing bone defects where the residual bone provides sufficient spatial support1. However, when the residual bone surrounding the defect lacks adequate spatial support, a space-sustaining apparatus should be incorporated into the GBR process to ensure success2. This necessity arises from the tendency of particulate bone grafts to shift and resorb under pressures from the oral environment during graft maturation3. Auxiliary devices, such as tenting screws and titanium meshes, may assist in creating and maintaining space during GBR4,5,6. However, their application is not ideal, as they require re-entry for removal7. More importantly, they can be time-consuming during the procedure and lack precision in reconstructing the desired bone contours, potentially leading to increased treatment time and costs8. Consequently, there is an urgent need for a material that is biocompatible, resorbable, and capable of retaining its structure long enough for bone graft maturation. Furthermore, this material should be customizable for individual cases and possess adequate mechanical strength to meet the demands for precise bone reconstruction.
As bioactive materials, tricalcium phosphate (TCP) is commonly used for repairing bone defects because it resembles natural bone minerals and possesses osteoconductive properties9. It provides a conductive pathway for bone cells to migrate and grow, facilitating the formation of new bone tissue along its surface10. α-TCP has a degradation period of more than 3 mouths within bone regeneration area and is ultimately substituted by new bone, while it takes about 12 months for β-TCP to degrade completely11. Researchers have found that the combination of TCP and polymers, such as PLA and PCL, endows the material with shaping adaptability12,13, which made it a potential implant material for precise GBR. Efforts have been made to fabricate TCP-based scaffolds using three-dimensional (3D) printing and electrostatic spinning techniques. However, most scaffolds produced by 3D printing exhibit inadequate mechanical strength14,15,16. Although a moderate increase in mechanical strength can be attained by augmenting the TCP components, such modifications may lead to severe outlet clogging and result in print failure14. Moreover, the solution mixing method is also susceptible to material aggregation in electrostatically spun fibers, which consequently compromises the mechanical properties of the materials17. Therefore, achieving high-strength biomaterials necessitates high-content microfillers with optimal dispersion. The incorporation of solid particles without obstructing the solution bonding action allows micro- or nanoparticles of various materials to move freely, facilitating ideal and homogeneous mixing of high filler contents.
In the current study, we initiated an “in situ embedding-reinforced” strategy based on solids mixing to prepare an α-TCP/PLA/nMgO composite with a high α-TCP content. The addition of PLA facilities bonding effect on various particles under pressure and heating. Under tested condition, the uniformly distributed PLA effectively encapsulated the α-TCP and nMgO particles in situ and eliminated existing micropores.This strategy dramatically increases proportion of α-TCP, hence mechanical properties of the composite. The incorporation of nMgO enhances osteogenic outcomes through dual mechanisms. Mg²⁺ ion release from nMgO directly stimulates osteoblast proliferation/differentiation while suppressing osteoclast-mediated bone resorption18,19, and the alkaline microenvironment generated by nMgO dissolution promotes hydroxyapatite crystallization and mitigates inflammatory responses20,21. Notably, this pH elevation counteracts the acidic byproducts released during PLA degradation, thereby modulating the composite’s degradation kinetics to better align with alveolar bone regeneration timelines. This dual functionality—combining bioactive ion delivery and pH buffering—optimizes the material’s mechanical stability and biocompatibility, making it particularly suitable for alveolar bone reconstruction applications. Importantly, through computer-aided design and computer-aided manufacturing (CAD/CAM) technology, this α-TCP/PLA/nMgO composite material can be fabricated into customized meshes according to individual needs, effectively meeting the demand for customizable and high-strength solutions. This study developed a high-performance material with potential applications for the reconstruction and regeneration of alveolar bone defects, and the use of solids mixing and in situ embedding-reinforced methods provides valuable insights for novel biomaterial manufacturing.
Results
Strength and hardness of the materials with different PLA ratio
The SEM scans indicated that the outer surfaces of α-TCP/PLA/nMgO became denser and smoother as the ratio of PLA increased (Fig. 1A). Additionally, SEM scans of the cross-section revealed that there was a large amount of PLA evenly embedding α-TCP in PLA-0.7 and higher. PLA-0.7 and PLA-0.8 exhibited the most optimal material distribution. A few microbubbles were observed in PLA-0.6 due to insufficient PLA content, while PLA-0.9 and PLA-1.0 contained excessive PLA. As anticipated, PLA-0.7 demonstrated the highest flexural strength, averaging 95.75 MPa, which was approximately five times that of pure PLA (Fig. 1B). Furthermore, the Vickers’ hardness of PLA-0.7 reached 28.73 HV1, comparable to the highest value of 31.06 HV1 observed in PLA-0.8 (Fig. 1C & D). Considering that flexural strength is the most critical property for a space creation and maintenance apparatus, the PLA-0.7 composite was selected for further studies.
Mechanical properties of the composites with different PLA ratios. (A) SEM scanning of the outer surfaces and sections of different materials. Magnification: ×2000. (B) Flexural resistance of the materials. Significant to PLA: **P < 0.01, ***P < 0.001. Significant to others: ##P < 0.01, ###P < 0.001. (C) & (D) Vickers hardness of the materials. Significant to PLA: *P < 0.05, ***P < 0.001. Significant to others: ##P < 0.01.
Analysis of the components in PLA-0.7
XRD clearly demonstrated that the main diffraction peaks of PLA/α-TCP and PLA-0.7 were predominantly attributed to α-TCP, with characteristic peaks of nMgO also observed, albeit weakly (Fig. 2A). These findings suggested that α-TCP and nMgO have been successfully incorporated into PLA-0.7 without altering their inherent crystal structures. FTIR further revealed that pure PLA, PLA/α-TCP and PLA-0.7 exhibited characteristic absorption peaks corresponding to CH-CH3 and C-O-C, at 1381 cm−1 and 1182 cm−1, respectively (Fig. 2B). Notably in PLA/α-TCP and PLA-0.7, C = O corresponding to 1751 cm⁻¹ exhibits a slight redshift in the infrared spectrum, and the P = O corresponding to 3439 cm⁻¹ disappears (Fig. 2B), indicating P = O may interact with the π electrons of C = O.
Interestingly, the composite materials exhibited shifted thermal stability compared to PLA, as demonstrated by differential scanning calorimetry (DSC) (Fig. 2C). The glass transition temperature (Tg) of PLA was 57.81℃, while α-TCP/PLA and PLA-0.7 were slightly higher at 58.97℃ and 59.55℃, respectively. The addition of α-TCP or α-TCP/nMgO to PLA led to recrystallization of PLA during heating, as showed by the occurrence of the crystallization temperature (Tc) in α-TCP/PLA and PLA-0.7. Furthermore, the initial melting temperature (Tim) of PLA/α-TCP and PLA-0.7 were about 156.78℃ and 156.72℃, respectively, higher than that of PLA, which was about 140.54℃ (Table 1)22,23,24.
In vitro degradation assay
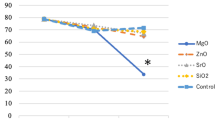
The degradation behaviors of the materials were first tested in a Tris-HCl buffer (pH = 7), with results recorded by measuring weight changes and pH dynamics (Fig. 3). As illustrated in Fig. 3A, both PLA and PLA/α-TCP demonstrated relative stability in weight over the 5-weeks tested period, accompanied with similarly decreased pH of their leachate solutions (Fig. 3B). In contrast, PLA-0.7 experienced a dramatic loss of its 6% of weight during the first week, followed by a relatively steady phase over the subsequent four weeks, during which it further lost an additional 2% of weight. In accordance with its weight change pattern, pH of the PLA-0.7 leachate solutions reached the highest of 7.53 at the first week and stayed at around 7.20 to 7.24 during the next four weeks. The increased pH introduced by nMgO maybe the main cause of the accelerated degradation of PLA in PLA-0.7 as the hydroxyl ions (OH⁻) in alkaline conditions directly catalyze the hydrolysis of PLA’s ester bonds, leading to rapid chain scission and depolymerization into low-molecular-weight oligomers or lactic acid monomers25,26. This hydrolysis is further enhanced by the neutralization of acidic byproducts (e.g., carboxylic acids) generated during degradation, which mitigates self-inhibition caused by excessive acidity and sustains the reaction kinetics.
Hydrophilicity, cytotoxicity and cell adhesion/migration behavior
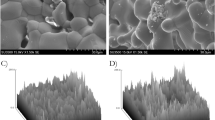
As illustrated in Fig. 4A, the average water contact angles of PLA and α-TCP/PLA are approximately 94.3° and 86.7°, respectively. The addition of nMgO, known for its high hydrophilicity, resulted in a significantly smaller water contact angle of 67.2° in PLA-0.7 (P < 0.001). The culture of MC3T3-E1 cells with leachate media from PLA-0.7 was employed to assess the material’s cytotoxicity. After 1, 3, and 7 days of culture, cell viability was evaluated using the CCK-8 assay. The mean optical density values for the PLA-0.7 group were significantly higher than those of the other three groups at all three time points (P<0.001), indicating an improved cell viability effect of PLA-0.7 (Fig. 4B). Furthermore, the live and dead assay of the cells indicated that none of the tested materials caused additional cell death compared to the control group (P > 0.05) (Fig. 4C & D). For cell affinity, A9 and MC3T3-E1 cells were inoculated onto PLA, PLA/α-TCP, and PLA-0.7 and co-cultured for 24 h, and the number of attached cells was subsequently observed. As depicted in the Fig. 4E & F, A9 and MC3T3-E1 cells exhibited the highest number of attachment to PLA-0.7, with a slight reduction observed for PLA/α-TCP, and the least attachment occurring with PLA alone. However, the migration ability of the cells was not affected by any of the tested materials (Fig. 4G & H).
Hydrophilicity and biocompatibility of the composites. (A) Water contact angle of the composites. Significant: ***P < 0.001. (B) CCK-8 assay of MC3T3-E1 cells cultured with different leachate media for 1, 3, and 7 d, respectively. Significant: *P < 0.05, **P < 0.01, ***P < 0.001. (C) Cell viability assay by immunofluorescence staining of the live and dead MC3T3-E1 cells cultured with different leachate media. (D) Statistical analysis of the immunofluorescent staining. NS: not significant. (E) & (F) SEM scanning showing cells attached on surfaces of different materials after co-culture for 24 h. (G) Scratch test was used to detect the migration ability of MC3T3-E1 cells cultured in respective leachate medium. (H) There was no significant difference in the percentage of cell migration area between groups: P > 0.05.
Cell osteogenesis induced by PLA-0.7
RUNX2 is a master transcription factor that regulates osteoblast differentiation, controls the expression of bone matrix protein genes and promotes osteoblast maturation27, all of which are essential for bone tissue formation. ALP activity and calcium nodule formation are also important markers of cell osteogenesis and were therefore evaluated in the current study28. BMSCs were cultured in a PLA-0.7 leachate medium-based osteogenesis induction medium, and the protein level of RUNX2 was measured using immunofluorescence. The results indicated that the expression of RUNX2 was approximately two times higher in the PLA-0.7 group compared to that treated with the control osteogenesis induction medium (P < 0.001), demonstrating the strong ability of PLA-0.7 in inducing osteogenesis (Fig. 5A & B).
Cell osteogenesis induced by PLA-0.7. (A) Immunofluorescence staining of RUNX2 protein in BMSCs cultured with PLA-0.7 leachate medium-based osteogenesis induction medium for 24 h. (B) Relative quantification of the RUNX2 expression by immunofluorescence. Significant to control: ***P < 0.001. (C) After co-cultured on PLA-0.7 for 1 and 2 w, BMSCs were stained with ALP and photographed by stereomicroscope. (D) After co-cultured on PLA-0.7 for 1 and 2 w, the ALP activity of BMSCs was quantitatively detected. Significant to control: *P < 0.05; NS: not significant. (E) BMSCs co-cultured with PLA-0.7 leachate medium-based osteogenesis induction medium for 3 w, followed by ARS staining and stereomicroscopy, and (F) semi-quantification of the calcium nodules. Significant to control: *P < 0.05.
Furthermore, ALP levels were measured by ALP staining and enzyme activity assessment both on day 7 and day 14. As shown in Fig. 5C, there was an increased level of ALP both in quantity and enzyme activity on day 7, although these differences were not statistically significant. However, on day 14, the PLA-0.7 group exhibited a stronger ALP staining intensity and significantly higher enzyme activity (P < 0.05) (Fig. 5D). To estimate cellular osteogenic activity at late time, calcium nodule formation was quantified using ARS and semi-quantitative method after 21 days of co-culture. BMSCs in the PLA-0.7 group produced significantly more calcium nodules than the control group did (Fig. 5E). Similarly, semi-quantitative measurements of the dissolved calcium nodules further confirmed that PLA-0.7 induced greater calcium nodule formations (Fig. 5F, P < 0.05).
In vivo biocompatibilities
At 2 weeks post-implantation, samples were collected for HE staining and analyzed. As a result, PLA-0.7 demonstrated comparable, and even reduced, infiltration of inflammatory cells compared to the xenograft, which is widely used in alveolar bone regeneration. A small number of multinucleated cells, characterized as osteoclasts, were also observed at the edges of both the xenograft and PLA-0.7, accompanied by the typical morphology of bone resorption (Fig. 6A). At 12 weeks post-implantation, the infiltration of inflammatory cells and formation of fibrous tissue were similar in both the xenograft and PLA-0.7 groups (Fig. 6B). Additionally, inflammatory cells count in whole blood and HE staining of the kidneys, hearts, and livers of the mice were performed to assess the material’s biosafety (Supplemental Figs. 2 & 3). There were no significant differences between the two groups, and no abnormalities were observed.
The degradation of PLA-0.7 in mice was measured by weight changes of the materials. At 2, 6, 12 weeks post-implantation, PLA-0.7 lost approximately 4.6%, 9.3%, and 21.9% of its weight, respectively, while the cortical bone xenograft lost about 1.9%, 11.2%, and 15.8% of its weight, respectively (Fig. 7A). The degradation rate of PLA-0.7 in mice was quite similar to that of the xenograft at all three time points (P > 0.05). Figure 7B shown that body weights of the mice had no significant difference during experiment. These results indicated that PLA-0.7 possessed ideal biocompatibility and degradation properties comparable to those of the xenograft.
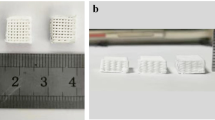
Manufacture of a customized mesh by CAD/CAM
A vertical alveolar bone defect on the first molar area was created in a plastic mandibular model and transferred to STL file obtained by digital scanning (Fig. 8A & B). Then a customized mesh aiming for precise bone augmentation was designed and manufactured by CNC (Fig. 8C, D & E). The resulting mesh made of PLA-0.7 composite shown precise supporting for the alveolar bone contour (Fig. 8F).
A customed supporting mesh aiming for precise regeneration of the alveolar bone defect. (A) & (B) A vertical bone defect created on a plastic model of human mandibular and transfered to digital format. (C) to (F) A customed supporting mesh made of PLA-0.7 designed and manufactured according to the bone defect.
Discussion
An ideal material for space creation and maintenance in GBR should possess sufficient strength and hardness for spatial supporting. In the meantime, the material should be manufacturable and customized for each individual, as well as be degradable while sustains long enough allowing new bone formation. To achieve such goals, bioactive ceramics and ceramics-based materials were proper candidates as they have been used and proved to be effective bone substitutes and possess high mechanical properties. However, the bioactive ceramic alone is lack of elasticity and difficult to be manufactured with 3D printing or CNC technologies that could fulfill personalized medicine needs. Additionally, the natures and components of inks in 3D printing would limit the strength of the printed ceramics-based materials. Hwang et al.. reported that a PCL/PLGA/β-TCP scaffold achieved a tensile strength of only 15 N29. Similarly, Wu et al. demonstrated that the compressive strength of 3D printed α-TCP/gel scaffolds was only approximately 10 MPa14. Thus, composites based on bioactive ceramics and manufactured by CNC should be a better choice for our purpose.
PLA has been widely used as implant material and the addition of PLA will confer plasticity to composite materials. It is well known that PLA undergoes hydrolysis in aqueous environments that long chains are fragmented into shorter oligomers and eventually lactic acid30. The retention rates of PLA in miniature pigs were 58.5% at 30 days and 34.7% at 90 days on average31. Compared to β-TCP, α-TCP shows closer degradation rate to PLA and should be better in the synergistic degradation of the composite32. It has been known that MgO undergoes hydrolysis in physiological fluids, dissociating into Mg²⁺ ions and hydroxyl ions (OH−) that increases local pH. Also, Mg²⁺ ions are essential for enzymatic reactions, ATP synthesis, and DNA repair33. Mg²⁺ ions can also stimulate osteoblast proliferation and collagen synthesis, accelerating bone healing34. Xu et al. had showed that when mass weight ratio of nMgO to PLA was set closer to 0.04, their synergistic degradation would conduct ideal biocompatibility. We also showed that the addition of nMgO in PLA (mass ratio 0.04) did not induce cell cytotoxicity12. Thus, the addition of MgO in PLA would neutralize the acidic environment produced by PLA degradation and promote osteogenesis. In the current study, an in situ embedding-reinforced strategy was proposed to develop the composites that consist of α-TCP/PLA/nMgO. Under high pressure, solid mixtures of α-TCP, PLA, and nMgO particles were physically remolded and bonded to minimize the unfavorable phenomena of uneven mixing and bubble generation that tend to occur in molten or solution mixtures. Following heat treatment at 156 °C, the PLA particles underwent a transition to a viscous fluid state, serving as a binder and achieved tight in situ encapsulation of α-TCP and nMgO. The in situ embedding-reinforced strategy overcomes the limitation of α-TCP proportion in 3D printing and thus strengthens mechanical properties of the composite.
Previous studies showed that the flexural strength of α-TCP cement is only about 5 to 8 MPa35. However, in current study, the flexural strength of the PLA embedded α-TCP composite improved dramatically and reached 95.75 MPa. The enhanced flexural strength and hardness of the PLA-0.7 composite material can be attributed to the physical binding of these components, which functions similarly to a combination of reinforcement bars and cement. In this context, the bonding effect of the organic PLA contributes to the increased flexural strength, while α-TCP provide higher hardness. However, these enhancements require an optimal ratio of PLA to α-TCP. When the ratio of PLA falls below 0.7, there is insufficient binder fully embedding the α-TCP particles and eliminate microgaps among them, resulting in weakened physical properties. Conversely, excessive PLA reduces the flexural strength of the α-TCP/PLA/nMgO composite.
The XRD and FTIR analyses were conducted to further investigate the chemical status of composites after preparation. As a result, though there was no direct new chemical bond formation observed, the diminishment of the P = O along with the occurrence of carbonyl stretching vibration peak of C = O shifting towards lower wavenumbers suggested that P = O may interact with the π electrons of C = O, leading to an equalization of electron cloud density and the formation of a mesomeric effect. The lone pair electrons in P = O form p-π conjugation with the π bond in C = O, resulting in a more stable structure. This could also explain the increased Tim and Tg in α-TCP/PLA and PLA-0.7 in DSC. The α-TCP microparticles, which may function as “nuclei”, aiding the molten PLA in reattaching and crystallizing upon heating, might also contribute to the increased Tim and Tg. This process generated an exothermic effect and shifted the crystallization peaks, consistent with findings from Moldovan A and Pérez-Davila S36,37. The temperature employed for in situ embedding corresponded with the DSC results. At about 156℃, PLA began to melt and attach on α-TCP and nMgO particles, ultimately leading to a uniform material. The addition of nMgO did not significantly affect the thermodynamic properties of the materials, likely due to its minimal proportion in the composites.
The absorbable supporting material required for bone regeneration should also exhibit a degradation rate that matches the growth rate of bone tissue. This alignment allows for the timely substitution of the material with new bone while maintaining sufficient mechanical strength for protection. For alveolar bone reconstruction, degradation within 5–6 month was considered appropriate38. The quick degradation of PLA-0.7 in Tris-HCl buffer in the first week maybe due to introduction of nMgO. nMgO readily reacts with water to produce magnesium hydroxide (Mg (OH)2), which raises the pH of the buffers to an alkaline range (pH = 7.2 ~ 7.5) that subsequently shifts the chemical equilibrium and accelerates the degradation of PLA. Along the loss of nMgO on the exposed outer surface, degradation of the PLA-0.7 slowed down. As seen in mice, degradation of the PLA-0.7 was comparable to that of xenograft bone, indicating that PLA-0.7 may sustain long enough and allow new bone formation and maturation.
Studies have demonstrated that the hydrophilicity of implanted grafts significantly affects osteogenesis and wound healing39. Pure PLA is highly hydrophobic due to the absence of hydrophilic chemical groups40. The addition of MgO has been known to increase the hydrophilicity of composite materials12,41,42, and the hydrogen bonding interactions between the material and the cells are essential for effective cell anchoring. Consistent with hydrophilicity test of the materials, the smaller water contact angle of PLA-0.7 led to more cell attachments on it. What’s more, coculture of the cells and the materials suggested that PLA-0.7 is highly biocompatible and even may promote cell proliferation. The ideal biological characteristics of PLA-0.7 would well facilitate the attachment of regenerative tissues, which is a prerequisite for cell proliferation and differentiation in tissue regeneration and wound healing.
Although not essential for a supporting material, the induction of osteogenesis will accelerate new bone formation. PLA-0.7 was shown to significantly induce osteogenesis in BMSCs, which may promote bone regeneration upon implantation. The osteogenic effects induced by PLA-0.7 may arise from several aspects directly related to its degradation. First of all, the weak alkaline environment upon degradation can inhibit osteoclast activity and promote osteogenesis through the stimulation of osteogenic differentiation, bone mineral salt deposition, and vascularization43,44,45,46. Secondly, MgO can significantly enhance osteoblast activity while effectively inhibiting osteoclast proliferation, thereby providing a solid physiological basis for bone regeneration19. The released Mg2+ ions are involved in various enzymatic reactions and can indirectly promote mineralization by increasing the activity of alkaline phosphatase20,33,47,48,49,50. Lastly, the degradation and dissolution of α-TCP release a substantial amount of Ca2+ into the culture medium, which may also contribute to the promotion of osteogenesis51.
In vivo biocompatibilities of PLA-0.7 were also evaluated and compared to those of xenograft. As a result, a mild inflammatory cells infiltration in PLA-0.7 was observed to be comparable to that of xenograft bone. The absence of a rejection reaction further demonstrated the good biocompatibility of PLA-0.7. Additionally, multinucleated cells were noted to infiltrate the edges of both PLA-0.7 and the xenogeneic bone, with both materials exhibiting a nibbling appearance at their interfaces. This suggested that both xenogeneic bone and PLA-0.7 can be replaced and possess the capability for integration and absorption within the body. Furthermore, evaluations of inflammatory cells in whole blood and tissue sections from the livers, kidneys, and hearts indicated that PLA-0.7 does not provoke systemic inflammation or adversely affect vital organs, thereby ensuring its biological safety.
Conclusion
In this study, we introduced the synergistic strategy of in situ embedding-reinforced, which significantly increased the proportion of microfillers in the composite material and enhanced its mechanical properties. The solid-state physical mixing strategy resulted in a more uniform distribution of a high proportion of α-TCP and nMgO particles, effectively avoiding stress concentrations caused by agglomerates and nodules. The moderate heat treatment ensured the in situ encapsulation of α-TCP and nMgO by PLA, while the uninterrupted polymer flow prevented the formation of numerous bubbles, resulting in a denser material. Furthermore, by integrating this strategy with CAD/CAM technology, we achieved controlled on-demand designation of the materials. The in situ embedding-reinforced strategy can be easily applied to manufacture various implant composite material with different degradation rates. For example, PLLA and β-TCP and HA can be used instead of PLA and α-TCP to slow down degradation of the composite. In conclusion, given the widespread solid-state characteristics of polymeric materials and microfillers, we believe that our strategy can be generalized to a broader range of material systems to enhance the preparation of high-performance scaffolds for bone regeneration.Further studies should be conducted to evaluate performance of the PLA-0.7 composite in reconstruction of large alveolar bone defects with GBR.
Materials and methods
Raw materials
The sizes of α-TCP (EPirui, China), PLA (Tesulang, China), and MgO nanoparticles (nMgO) (McLean, China) particles were 1 μm, 10 μm, and 50 nm, respectively, with corresponding densities of 1.26 g/cm³, 3.14 g/cm³, and 3.58 g/cm³. To verify the reliability of each raw material, an X-ray diffractometer (XRD) (Ultima IV, Rigaku, Japan) was employed, and the results were compared with the ICDD standards (Supplemental Fig. 1).
The α-TCP, PLA, and nMgO powders were mixed in a planetary ball mill (YXQM-16 L, Changsha Miqi, China) by rotating forward for 30 min at 300 r/min, followed by a reverse rotation for an additional 30 min at the same speed. This rotation process was repeated three times to ensure thorough mixing of the samples. The homogeneously mixed α-TCP/PLA/nMgO composite powder was then compressed into either pieces (15 mm × 15 mm × 2 mm) or blocks (15 mm × 15 mm × 15 mm) using a manual tablet press (MC-15B, Changsha Miqi, China) at a pressure of 7 tons, held for 1 min. Subsequently, the samples were heated in a muffle furnace (B170, Nabertherm, Germany) at 156 °C for 5 min. The ratio of PLA to nMgO powder was 25:1, which has been shown to counteract the weak acidic environment produced by PLA degradation12. The different composite materials were made according to the various weight ratios presented in Table 2.
Characterization
The surface and cross-section of the materials were observed using a scanning electron microscope (SEM) (S-3400 N, Hitachi, Japan). The crystalline structures of the materials were examined using XRD. The chemical compositions of the composites were analyzed using Fourier Transform infrared spectroscopy (FTIR) (iN10, Thermo Scientific, USA). The thermal stability and crystallization behavior of the samples were determined by differential scanning calorimetry (DSC) (DSC25, TA, USA) within a temperature range of 40–200 °C under an argon atmosphere, with a temperature increase rate of 10 °C/min. The hydrophilicity of the samples was assessed by measuring the static water contact angle using a contact angle/surface tension meter (LSA100, Lauda Scientific, Germany). Each group consisted of three samples, and each test was replicated three times at various locations. A mechanical universal testing machine (HZ-1009 A, Lixian Instrument Co., Ltd., China) was used to perform three-point bending tests on square sheet samples (15 mm × 15 mm × 2 mm) to evaluate their flexural resistance. Each group of three samples was tested with a span of 10 mm and a loading rate of 0.1 mm/s until complete material failure occurred, at which point the maximum loads at the time of breakage were recorded. The Vickers hardness of the materials was measured using a microhardness tester (Falcon 507, Innovatest, the Netherlands).
Degradation assay in vitro
The volume ratio of each tested material to the Tris-HCl solution (PHC002, Phygene, China) was established at 1:40. The original materials were weighted to obtain the initial weight, denoted as W0. Then the materials were immersed in Tris-HCl solution (pH 7) and maintained at 37 °C. Measurements were taken at a 7-day interval, resulting in a total of 8 assessments. At each time point, the materials were lyophilized and weighed as W(n). The pH of the leachate solutions was measured using a pH meter (PE28, METTLER, Switzerland), and the solution was refreshed with Tris-HCl for subsequent degradation assay. The weight change of the sample was calculated as follows: \(\:Weight=\frac{Wn}{W0}\times\:100\%\).
Cell cultures
The pre-cranial parietal osteoblasts from mice (MC3T3-E1) (MeilunBio, China) were cultured in α-MEM (C12571500BT, Gibco, America) supplemented with 10% fetal bovine serum (FBS) (10099-141, Gibco, America) and 1% penicillin/streptomycin (P/S) (15140-122, Gibco, America). The subcutaneous connective tissue cells from mice (A9) (MeilunBio, China) and the bone marrow mesenchymal stem cells (BMSCs) (Cyagen, China) were cultured in DMEM (C11995500BT, Gibco, America) with 10% FBS and 1% P/S. The cell densities were set at 2000 cells per well in 96-well plates, 1 × 104 cells per well in 48-well plates, and 5 × 105 cells per well in 6-well plates. All cultures were maintained at 37 °C in a 5% CO2 atmosphere. The biocompatibility of PLA, PLA/α-TCP, and PLA-0.7 was assessed either through direct co-culture of the materials with cells or by culturing cells with the leachate media derived from the materials. Briefly, a material sample (15 mm × 15 mm × 2 mm) was immersed in 20 ml of α-MEM or DMEM in a conical tube and incubated at 37 °C for 7 d, yielding α-MEM-based or DMEM-based leachate medium. Subsequently, 10% FBS and 1% P/S were added to the leachate media for cell culture. For the induction of osteogenesis in BMSCs, the following components were added to either DMEM or DMEM-based leachate medium: 10% FBS, 1% P/S, 1% β-phosphoglycerol, 1% vitamin C, and 2%00 dexamethasone.
Cytotoxicity assay and cell viability assay
MC3T3-E1 cells were inoculated into 96-well plates with leachate medium or control medium. After 1, 3, and 7 d, the cells were washed twice with PBS prior to subsequent assays. For the cytotoxicity assay, α-MEM containing 10% CCK-8 (CK04, DOJINDO, China) was added and incubated for 2 h at 37 °C in a 5% CO2 atmosphere. The optical density (OD) values of the medium were measured at 450 nm using an enzyme marker. Cell viability was assessed using the Calcein-AM/PI cell viability/cytotoxicity assay kit (CA1630, Solarbio, China) according to the manufacturer’s instructions. Briefly, MC3T3-E1 cells were stained with calcein-AM/PI for 30 min at 37 °C in the dark. Fluorescence images were then obtained at 490 nm and 545 nm, respectively, using an inverted fluorescence microscope (DMI 300B/DFC450, Leica, Germany). The average fluorescence intensity was analyzed using ImageJ software (ImageJ2 Fiji 1.54f).
Cell migration test
The MC3T3-E1 cells were cultured in 6-well plates. Once the cells had fully expanded, a straight line perpendicular to the plane of the plate was drawn using a 200 µL pipette tip and subsequently photographed. The cells were then cultured in serum-free leachate medium for 24 h, washed twice with PBS, and photographed again to assess the area of cell migration.
Cell adhesion
Cell attachment is a critical property of implant materials for bone regeneration. The PLA-0.7 (5 mm × 1 mm) samples were first placed at the bottom of 48-well plates. Subsequently, the MC3T3-E1 and A9 cells were inoculated into the respective wells of the 48-well plates. Following a 24-hour incubation, the cells were fixed using 4% neutral paraformaldehyde (Golden Pan, China) for 30 min and rinsed twice with PBS. The cells then underwent a gradient dehydration process using 50%, 60%, 70%, 80%, 90%, and 100% ethanol in sequential order. After drying at 37 °C for 60 min, the surfaces of the PLA-0.7 and the attached cells were immediately imaged using a scanning electron microscope. A9 and MC3T3-E1 cells were inoculated onto PLA, PLA/TCP, and PLA-0.7 and co-cultured for 24 h, and the number of attached cells was subsequently observed. As depicted in the Fig. 5E, A9 and MC3T3-E1 cells exhibited the highest attachment to PLA-0.7, with a slight reduction in attachment observed for PLA/α-TCP, and the least attachment occurring with PLA alone.
Alkaline phosphatase (ALP) staining and enzyme activity quantitative analysis
The PLA-0.7 (5 mm × 1 mm) and cell culture slides were initially placed at the bottom of 48-well plates. BMSCs were then inoculated into the 48-well plates and cultured until the cell density reached 80–90%. Osteogenesis was induced by replacing the culture medium with osteogenesis induction medium. On days 7 and 14, the medium was removed, and the cells on the PLA-0.7 and slides were rinsed twice with PBS, fixed with 4% paraformaldehyde for 15 min, and subsequently rinsed again with PBS. The cells were then stained using the BCIP/NBT Alkaline Phosphatase Chromogenic Kit (C3206, Shanghai Bain-Marie, China) and photographed with a stereomicroscope. To quantify ALP enzyme activity, the same culture method was employed, except that cells were cultured in 6-well plates with PLA-0.7 (15 mm × 15 mm × 1 mm) instead. On days 7 and 14, the PLA-0.7 and cell culture slides were removed, the proteins from the remaining cells in the 6-well plates were extracted, and the protein concentration was measured using the BCA Protein Quantification Kit (BB-3401, Shanghai BestBio, China). ALP activity was then measured using Alkaline phosphatase assay kit (P0321S, Biyuntian, China) according to the recommended manual.
RUNX2 Immunofluorescence
BMSC were inoculated onto cell culture slides in 48-well plates for 16 h. Following this, the medium was replaced with either leachate medium-based osteogenesis induction medium or control culture medium. After 24 h, the cells were fixed with 4% paraformaldehyde and subsequently rinsed with PBS in preparation for Runt-related transcription factor 2 (RUNX2) immunofluorescence. Briefly, the cells were treated with 0.5% Triton-X (T8200, Solepol, China) and blocked with 2% BSA (CAS9006-59-1, Ruyi, China) prior to treatment with anti-RUNX2 antibody (ab236639, Abcam, UK) and secondary antibody (A32754, Thermo Fisher, USA). The cells were further stained with phalloidin (40736ES75, Yeasen, China) for 30 min at room temperature, and the nuclei were labeled with DAPI (C0060, Solarbio, China) for 10 min. Finally, the cells were imaged using a confocal microscope (LEICATCSSP8, Solebo, China).
Alizarin red staining (ARS) and semi-quantification
BMSCs were inoculated into 48-well plates and cultured until the cell density reached 80–90%. Following this, the medium was changed to osteogenesis induction medium, which was renewed every 3 to 4 d. After 21 daysof induction, the cells were washed twice with PBS and fixed in 4% paraformaldehyde for 15 min. A 1% alizarin red staining solution (G1452, Solarbio, China) was then added to each well for 5 min. After washing twice with deionized water, the BMSCs were photographed using a stereomicroscope. Finally, an equal volume of 100 mmol/L cetylpyridinium chloride was added to each well and incubated for 1 h at room temperature to dissolve the mineralized nodules. The supernatant was collected and semi-quantified by measuring the optical density (OD) at 562 nm.
Animal study
The animal experiments were approved by the Laboratory Animal Ethics Committee of Guangdong Huawei Testing Co. Ltd. (Approval No. 202403002) and performed in compliance with ARRIVE guidelines and Chinese legal and ethical requirements. We confirm that all methods were performed in accordance with the relevant guidelines and regulations. A total of 25 male C57/BL6 mice (22 ± 1 g, 6 weeks old) were procured from the Animal Experiment Center of Guangdong Huawei Testing Co. Ltd. The mice were maintained under standard conditions. PLA-0.7 and cortical bone xenograft Bio-DBM (SDBM-GG-H, Lianjie, China) were bilaterally implanted subcutaneously in the dorsal region of the mice under anesthesia (Zoletil 50, 20 mg/kg, IP). At 2- and 12-w post-surgery, the mice were sacrificed, and the hearts, livers, kidneys, and dorsal tissues containing the implanted materials were excised and fixed in 4% paraformaldehyde. Tissue sections were then stained with hematoxylin-eosin (HE; G1120, soluble). Blood was collected from the ocular region for hematocrit analysis. To weight the implanted materials, proteinase K at a concentration of 30 units/mg (V900887, Sigma, USA) was diluted to 10 µg/mL using Tris buffer (PHC002, Phygene, China) at pH of 8.0. The implanted samples were immersed in this solution at 37 °C for 12 h to remove adhered soft tissues. The samples were subsequently washed, freeze-dried, and weighted to calculate the degradation rate.
Manufacture of a customized mesh by CAD/CAM
A vertical alveolar bone defect (11.0 mm × 9.7 mm × 4.5 mm) was created in a plastic mandibular model, followed by intra oral scanning (Model 3SPS1P-2, 3Shape, Denmark). The resulted STL file was import to Meshmixer software (version 3.5) for desigation of a customized mesh. UG software (NX2312) was used to reconstruct the mesh model into STP format. The resulted STP file was used for CNC (Computerized Numerical Control; Nanjing Jianke Machinery Co., Ltd; model MA25-5II) manufactured of the α-TCP/PLA/nMgO.
Statistics
GraphPad Prism 9.4 (GraphPad Software, San Diego, USA) was utilized for statistical analysis. Continuous data are presented as mean ± standard deviation. Two-tailed t-tests and ANOVA were conducted to identify significance between groups and among groups, respectively. A P < 0.05 was considered statistically significant.
Data availability
All datasets usded and/or analyzed are available upon requested to Hanfu Su.
References
Hämmerle, C. H. & Jung, R. E. Bone augmentation by means of barrier membranes, Periodontol. 33 (2003) 36–53. (2000). https://doi.org/10.1046/j.0906-6713.2003.03304.x
Wang, H. L. & Boyapati, L. PASS principles for predictable bone regeneration. Implant Dent. 15, 8–17. https://doi.org/10.1097/01.id.0000204762.39826.0f (2006).
Briguglio, F. et al. The use of titanium mesh in guided bone regeneration: A systematic review. Int. J. Dent. 2019, 9065423. https://doi.org/10.1155/2019/9065423 (2019).
Urban, I. A. & Monje, A. Guided bone regeneration in alveolar bone reconstruction, oral maxil. Surg. Clin. 31, 331–338. https://doi.org/10.1016/j.coms.2019.01.003 (2019).
Han, H. H. et al. Huge nasopharyngeal teratoma with a cleft palate and bifid tongue in a patient with Pierre robin syndrome. J. Craniofac. Surg. 25, e588–e590. https://doi.org/10.1097/SCS.0000000000001070 (2014).
Cucchi, A., Vignudelli, E., Napolitano, A., Marchetti, C. & Corinaldesi, G. Evaluation of complication rates and vertical bone gain after guided bone regeneration with non-resorbable membranes versus titanium meshes and resorbable membranes. A randomized clinical trial. Clin. Implant Dent. Relat. Res. 19, 821–832. https://doi.org/10.1111/cid.12520 (2017).
Hartmann, A., Hildebrandt, H., Schmohl, J. U. & Kämmerer, P. W. Evaluation of risk parameters in bone regeneration using a customized titanium mesh: results of a clinical study. Implant Dent. 28, 543–550. https://doi.org/10.1097/ID.0000000000000933 (2019).
El Chaar, E. et al. Treatment of atrophic ridges with titanium mesh: A retrospective study using 100% mineralized allograft and comparing dental stone versus 3d-printed models. Int. J. Periodont Rest. 39, 491–500. https://doi.org/10.11607/prd.3733 (2019).
Farina, N. M., Guzón, F. M., Peña, M. L. & Cantalapiedra, A. G. In vivo behaviour of two different biphasic ceramic implanted in mandibular bone of dogs. J. Mater. Sci. Mater. Med. 19, 1565–1573. https://doi.org/10.1007/s10856-008-3400-y (2008).
Kobayashi, N., Hashimoto, Y., Otaka, A., Yamaoka, T. & Morita, S. Porous alpha-tricalcium phosphate with immobilized basic fibroblast growth factor enhances bone regeneration in a canine mandibular bone defect model. Materials 9, 853. https://doi.org/10.3390/ma9100853 (2016).
Kihara, H., Shiota, M., Yamashita, Y. & Kasugai, S. Biodegradation process of α-TCP particles and new bone formation in a rabbit cranial defect model. J. Biomed. Mater. Res. B Appl. Biomater. 79, 284–291. https://doi.org/10.1002/jbm.b.30540 (2006).
Xu, D. et al. Improvement of the mechanical properties and osteogenic activity of 3D-printed polylactic acid porous scaffolds by nano-hydroxyapatite and nano-magnesium oxide. Heliyon 8, e09748. https://doi.org/10.1016/j.heliyon.2022.e09748 (2022).
Vella, J. B. et al. Three dimensional printed calcium phosphate and Poly (caprolactone) composites with improved mechanical properties and preserved microstructure. J. Biomed. Mater. Res. Part. A. 106, 663–672. https://doi.org/10.1002/jbm.a.36270 (2018).
Wu, N. et al. Degradable calcium deficient hydroxyapatite/poly (lactic-glycolic acid copolymer) bilayer scaffold through integral molding 3D printing for bone defect repair. Biofabrication 13, 025005. https://doi.org/10.1088/1758-5090/abcb48 (2021).
Shim, J. H. et al. Comparative efficacies of a 3D-printed PCL/PLGA/α-TCP membrane and a titanium membrane for guided bone regeneration in beagle dogs. Polymers 7, 2061–2077. https://doi.org/10.3390/polym7101500 (2015).
Bilgili, H. K. et al. 3D-Printed functionally graded PCL-HA scaffolds with Multi-Scale porosity. ACS Omega. 10, 6502–6519. https://doi.org/10.1021/acsomega.4c06820 (2024).
Thomas, V. et al. Electrospun bioactive nanocomposite scaffolds of Polycaprolactone and nanohydroxyapatite for bone tissue engineering. J. Nanosci. Nanotechnol. 6, 487–493. https://doi.org/10.1166/jnn.2006.097 (2006).
Wang, G. et al. Magnesium ion implantation on a micro/nanostructured titanium surface promotes its bioactivity and osteogenic differentiation function. Int. J. Nanomed. 9, 2387–2398. https://doi.org/10.2147/ijn.s58357 (2014).
Aničić, N., Kurtjak, M., Jeverica, S., Suvorov, D. & Vukomanović, M. Antimicrobial polymeric composites with embedded nanotextured magnesium oxide. Polymers 13, 2183. https://doi.org/10.3390/polym13132183 (2021).
Serre, C., Papillard, M., Chavassieux, P., Voegel, J. & Boivin, G. Influence of magnesium substitution on a collagen–apatite biomaterial on the production of a calcifying matrix by human osteoblasts. J. Biomed. Mater. Res. 42, 626–633. https://doi.org/10.1002/(SICI)1097-4636(19981215)42:4<626::AID-JBM20>3.0.CO;2-S (1998).
Li, X. et al. Reduced inflammatory response by incorporating magnesium into porous TiO2 coating on titanium substrate. Colloids Surf. B Biointerfaces. 171, 276–284. https://doi.org/10.1016/j.colsurfb.2018.07.032 (2018).
Yan, Y. et al. Preparation and characterization of intumescent flame retardant biodegradable Poly (lactic acid) nanocomposites based on sulfamic acid intercalated layered double hydroxides. Fiber Polym. 18, 2060–2069. https://doi.org/10.1007/s12221-017-1153-2 (2017).
Zhou, X. et al. Additive manufacturing of CNTs/PLA composites and the correlation between microstructure and functional properties. J. Mater. Sci. Technol. 60, 27–34. https://doi.org/10.1016/j.jmst.2020.04.038 (2021).
Maiza, M., Benaniba, M. T., Quintard, G. & Massardier-Nageotte, V. Biobased additive plasticizing polylactic acid (PLA). Polimeros 25, 581–590. https://doi.org/10.1590/0104-1428.1986 (2015).
Vaid, R., Yildirim, E., Pasquinelli, M. A. & King, M. W. Hydrolytic degradation of polylactic acid fibers as a function of pH and exposure time. Molecules 26, 7554. https://doi.org/10.3390/molecules26247554 (2021).
Feng, P. et al. Degradation mechanisms and acceleration strategies of Poly (lactic acid) scaffold for bone regeneration. Mater. Des. 210, 110066. https://doi.org/10.1016/j.matdes.2021.110066 (2021).
Chan, W. C. W., Tan, Z., To, M. K. T. & Chan, D. Regulation and role of transcription factors in osteogenesis. Int. J. Mol. Sci. 22, 5445. https://doi.org/10.3390/ijms22115445 (2021).
Yin, N. et al. MiR-135-5p promotes osteoblast differentiation by targeting HIF1AN in MC3T3-E1 cells. Cell. Mol. Biol. Lett. 24, 1–11. https://doi.org/10.1186/s11658-019-0177-6 (2019).
Hwang, K. S. et al. Comparative efficacies of collagen-based 3D printed PCL/PLGA/β-TCP composite block bone grafts and biphasic calcium phosphate bone substitute for bone regeneration. Mater. (Basel). 10, 421. https://doi.org/10.3390/ma10040421 (2017).
Qi, X., Ren, Y. & Wang, X. New advances in the biodegradation of Poly (lactic) acid. Int. Biodeterior. Biodegrad. 117, 215–223. https://doi.org/10.1016/j.ibiod.2017.01.010 (2017).
Huang, C. H., Lee, S. Y., Horng, S., Guy, L. G. & Yu, T. B. In vitro and in vivo degradation of microfiber bioresorbable coronary scaffold. J. Biomed. Mater. Res. B Appl. Biomater. 106, 1842–1850. https://doi.org/10.1002/jbm.b.33987 (2018).
Sawada, K. et al. Comparison of three block bone substitutes for bone regeneration: long-term observation in the beagle dog. Odontology 106, 398–407. https://doi.org/10.1007/s10266-018-0352-7 (2018).
Park, J. W., Kim, Y. J., Jang, J. H. & Song, H. Osteoblast response to magnesium ion-incorporated nanoporous titanium oxide surfaces, clin. Oral Implants Res. 21, 1278–1287. https://doi.org/10.1111/j.1600-0501.2010.01944.x (2010).
Zhou, H., Nabiyouni, M., Lin, B. & Bhaduri, S. B. Fabrication of novel Poly (lactic acid)/amorphous magnesium phosphate Bionanocomposite fibers for tissue engineering applications via electrospinning. Mater. Sci. Eng. C. 33, 2302–2310. https://doi.org/10.1016/j.msec.2013.01.058 (2013).
An, J., Wolke, J. G., Jansen, J. A. & Leeuwenburgh, S. C. Influence of polymeric additives on the cohesion and mechanical properties of calcium phosphate cements. J. Mater. Sci. Mater. Med. 27, 1–9. https://doi.org/10.1007/s10856-016-5665-x (2016).
Moldovan, A. et al. Development and characterization of polylactic acid (PLA)-based nanocomposites used for food packaging. Polym. (Basel). 15, 2855. https://doi.org/10.3390/polym15132855 (2023).
Pérez-Davila, S. et al. González, 3D-printed PLA medical devices: physicochemical changes and biological response after sterilisation treatments. Polym. (Basel). 14, 4117. https://doi.org/10.3390/polym14194117 (2022).
Yeo, A., Rai, B., Sju, E., Cheong, J. J. & Teoh, S. H. The degradation profile of novel, bioresorbable PCL-TCP scaffolds: an in vitro and in vivo study. J Biomed Mater Res A. ;84(1):208 – 18. (2008). https://doi.org/10.1002/jbm.a.31454. PMID: 17607768.
Baheti, W. et al. Graphene/hydroxyapatite coating deposit on titanium alloys for implant application. J. Appl. Biomater. Funct. Mater. https://doi.org/10.1177/22808000221148104 (2023).
AngelopoulosP.M., Samouhos, M. & Taxiarchou, M. Functional fillers in composite filaments for fused filament fabrication; a review. Mater. Today Proc. 37, 4031–4043. https://doi.org/10.1016/j.matpr.2020.07.069 (2021).
Sanginario, V., Ginebra, M., Tanner, K., Planell, J. & Ambrosio, L. Biodegradable and semi-biodegradable composite hydrogels as bone substitutes: morphology and mechanical characterization. J. Mater. Sci. Mater. Med. 17, 447–454. https://doi.org/10.1007/s10856-006-8472-y (2006).
Shuai, C. et al. Surface modification enhances interfacial bonding in PLLA/MgO bone scaffold. Mater. Sci. Eng. C Mater. Biol. Appl. 108, 110486. https://doi.org/10.1016/j.msec.2019.110486 (2020).
Kaunitz, J. D., Yamaguchi, D. T. & TrAP, T. N. A. P. ecto-purinergic signaling, and bone remodeling. J. Cell. Biochem. 105, 655–662. https://doi.org/10.1002/jcb.21885 (2008).
Monfoulet, L. E. et al. The pH in the microenvironment of human mesenchymal stem cells is a critical factor for optimal osteogenesis in tissue-engineered constructs. Tissue Eng. Part. A. 20, 1827–1840. https://doi.org/10.1089/ten.tea.2013.0500 (2014).
Avnet, S., Di Pompo, G., Lemma, S. & Baldini, N. Cause and effect of microenvironmental acidosis on bone metastases. Cancer Metastasis Rev. 38, 133–147. https://doi.org/10.1007/s10555-019-09790-9 (2019).
Zhao, F. et al. 3D printing nanoscale bioactive glass scaffolds enhance osteoblast migration and extramembranous osteogenesis through stimulating Immunomodulation. Adv. Healthc. Mater. 7, 1800361. https://doi.org/10.1002/adhm.201800361 (2018).
Pei, A., Zhou, Q. & Berglund, L. A. Functionalized cellulose nanocrystals as biobased nucleation agents in Poly (l-lactide)(PLLA)--Crystallization and mechanical property effects. Compos. Sci. Technol. 70, 815–821. https://doi.org/10.1016/j.compscitech.2010.01.018 (2010).
Feng, C. et al. 3D printing of lotus root-like biomimetic materials for cell delivery and tissue regeneration. Adv. Sci. (Weinh). 4, 1700401. https://doi.org/10.1002/advs.201700401 (2017).
Lin, Z. et al. Precisely controlled delivery of magnesium ions thru sponge-like monodisperse PLGA/nano-MgO-alginate core-shell microsphere device to enable in-situ bone regeneration. Biomaterials 174, 1–16. https://doi.org/10.1016/j.biomaterials.2018.05.011 (2018).
Tarafder, S., Davies, N. M., Bandyopadhyay, A. & Bose, S. 3D printed tricalcium phosphate bone tissue engineering scaffolds: effect of SrO and MgO doping on in vivo osteogenesis in a rat distal femoral defect model. Biomater. Sci. 1, 1250–1259. https://doi.org/10.1039/C3BM60132C (2013).
Tronco, M. C. & Cassel, J. B. Dos Santos, α-TCP-based calcium phosphate cements: A critical review. Acta Biomater. 151, 70–87. https://doi.org/10.1016/j.actbio.2022.08.040 (2022).
Acknowledgements
This research was supported by Scientific Research Projects for Oral Implantology of China Oral Health Foundation(COHF ZZZX202403)to Hanfu Su. We also thank Lijing Wang and Janak L. Pathak for helpful discussions.
Author information
Authors and Affiliations
Contributions
W.D. prepared and evaluated the materials and performed in vivo experiments. X.G. evaluated cell biocompatibility. Q.Z. evaluated osteogenesis in vitro. W.D. and X.G. wrote the main manuscript text and W.D. prepared all the figures. L.W and H.S designed the experiments and revised the manuscript. H.S. received the funding. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Du, W., Guo, X., Zheng, Q. et al. Development of a biodegradable α-TCP/PLA/nMgO composite for enhanced guided bone regeneration. Sci Rep 15, 19675 (2025). https://doi.org/10.1038/s41598-025-03426-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-03426-5