Abstract
The COVID-19 pandemic caused immense mortality and morbidity reporting 704,753,890 cases worldwide. The repercussions of this pandemic are still being felt in the form of newly evolving variants and infections. The pandemic has pointed towards the need for the development of new and effective agents against SARS-CoV-2 infection. Sulfonohydrazides are a class of compounds with a wide range of therapeutic potential. The present study aims to identify the anti-SARS-CoV-2 potential of Sulfonohydrazide compounds. Twenty-five Sulfonohydrazides derivatives were evaluated for anti-viral potential via plaque reduction assay (PRA) and cytopathic effect (CPE) analysis in-vitro. Treatment point assay was employed for the strategic evaluation of antiviral compound at the particular stages of the SARS-CoV-2 life cycle. Gene expression analysis was also carried out, which was supported by immunofluorescence assays targeting the N and S proteins of SARS-CoV-2, alongside fold-change analysis, to identify a robust and multifaceted approach for the understanding of viral dynamics. Moreover, ligand-inhibitor interactions were assessed by in- silico studies. Compound 24 (4(E)-4-methyl-N’-(2,3,4-trihydroxybenzylidene)benzenesulfonohydrazide) was identified as the most potent molecule that inhibited SARS-CoV-2 infection (92.85 ± 3.57%) via PRA. The time point assay revealed that the effect of the compound might be at the entry point, which might be due to the down-regulation of the Spike (S) and Angiotensin-converting enzyme 2 (ACE-2) genes by the compound. The gene expression analysis of ORF1a/b by qRT-PCR indicated reduction in viral load after compound treatment, as indicated by a higher cycle threshold (Ct) value. Moreover, the compound 24 also downregulated the expression of S, RdRp, and ACE-2. Furthermore, the interaction of compound 24 with S, RdRp, and ACE-2 was predicted via molecular docking, which validated the interaction and possible anti-SARS-CoV-2 effect. Additionally, immunofluorescence staining analysis of spike and nucleocapsid proteins also showed downregulation in SARS-CoV-2 infected cells. Overall, the acquired data suggested that Sulfonohydrazide derivative 24 inhibits SARS-CoV-2 entry and replication.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) is a Coronavirus (CoVs) and belongs to the family Coronaviridae, which primarily cause infections of the respiratory and gastrointestinal tracts1. In the late 2019, SARS-CoV-2 emerged as a highly transmissible and pathogenic virus causing a deadly pandemic of COVID-19 by early 2020 worldwide2. Like other RNA viruses, SARS-CoV-2 is prone to genetic alterations and rapidly adapt to new human host3. These viral genome mutations have resulted in the emergence of new variants with increased replicative fitness, altered pathogenicity, or differences in their ability to evade adaptive immune responses and resist antiviral drugs4.
Clinical manifestations of COVID-19 can be asymptomatic or symptomatic and, in severe cases, fatal5. The immunopathology of each patient varies according to their common health status6,7,8. Currently, many different anti-viral therapeutic options are available against COVID-19 such as paxlovid (Nirmatrelvir + Ritonavir)9, repurposed antiviral drugs (e.g., molnupiravir and remdesivir)10, and monoclonal antibodies (e.g., adintrevimab)11. However, new SARS-CoV-2 variants have been emerging frequently, and there is no curative regimen yet available to tackle the infection and symptoms effectively. Therefore, identifying new and effective inhibitors of SARS-CoV-2, covering a wide range of variants, is crucial.
Hydrazides are organic compounds with diverse pharmacological and biological properties, such as antimicrobial, antiviral, antiparasitic, antifungal, anti-inflammatory, analgesic, and anticancer activities. Different functional groups in each compound give it unique characteristics12. A study has indicated that a series of synthetic α-aminophosphonate-hydrazone derivatives have antiviral activity with 65.1% curative, 74.3% protective, and 94.3% inactivation activities13. In a study, two compounds derived from benzylidene hydrazides were found to be active against Vesicular stomatitis virus (VSV) in HeLa cell cultures14. A study has reported anti-hepatitis C activity of diflunisal hydrazide-hydrazones. These have also been observed to show hepatocellular carcinoma inhibition15. A tecovirimat analogue, p-Trifluoromethylbenzohydrazide (spirovirimat) has shown potent antiviral activity against Monkeypox virus by abolishing extracellular virus production. In silico evaluation suggested that the derivative targets the same protein as the tecovirimat16. In a research evaluating a series of novel aryl benzoyl hydrazide analogs, some of the derivatives demonstrated potent inhibitory activity against the avian H5N1 flu strain. One of these analogs, even exhibited nanomolar antiviral effects against both the H5N1 and Flu B virus. Primary mechanistic studies proposed that these derivatives act by mainly interacting with the PB1 subunit of RNA-dependent RNA polymerase (RdRp)17. In a study, a synthesized hydrazide-containing oseltamivir analog demonstrated strong inhibition of neuraminidases from H5N1, H1N1, H5N1–H274Y, and H1N1–H274Y mutants18. In a molecular docking study, the binding affinity of a newly synthesized hydrazide derivative (E)-N’-(1-(4-bromophenyl)ethylidene)-2-(6-methoxynaphthalen-2-yl)propanehydrazide for the SARS-CoV-2 main protease enzyme was observed and intermolecular binding interactions were studied. The compound showed a stable binding mode at the enzyme active pocket with a binding energy value of -8.1 kcal/mol. Moreover, the enzyme-compound complex showed stable dynamics with highly favorable binding energies. Overall, the compound might be a good lead for further structural optimization against the main protease enzyme19. Another in silico study has explored a complex compound containing hydrazone-derived ligand-protein, which has shown potential to be antiviral drug in cervical cancer caused by HPV-18 (human papillomavirus)20. Therefore, these compounds could possibly have anti-SARS-CoV-2 potential can be investigated to be developed into antivirals agents. This present study is aimed at investigating the anti-SARS-CoV-2 activity of a Sulfonohydrazide derivative in vitro. The non-cytotoxic compounds were evaluated for their effects on viral and host gene, and protein expressions by qRT-PCR and immunofluorescence microscopy, respectively, to evaluate their antiviral potential. Out of 25 derivatives assessed, 11 non-cytotoxic compounds indicated moderate to high anti-SARS-CoV-2 activity (50–100% viral plaque reduction). The compound 24 was further assessed for its potential viral targets by time-point assay.
Results
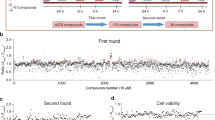
Cytotoxicity and anti-SARS-CoV-2 activity of sulfonohydrazide derivatives
After screening of various classes of organic compounds, 25 Sulfonohydrazide derivatives were identified as potential inhibitors of SARS-CoV-2. Subsequently, their cytotoxicity profile and the antiviral potential were assessed (Supplementary Table-1). Remdesivir (RDV) was used as a positive control. The inhibitory effects of the compounds on the growth of Vero cells (ATCC-CCL-81) were assessed using an MTT assay. The most potent anti-SARS-CoV-2 effect was observed at the concentration of 83 µM. The cytotoxicity of 25 derivatives indicated that only 11 derivatives had < 20% cytotoxicity. Compound 24 indicated the highest viability/proliferation (> 90%), of Vero cells therefore, it was selected for subsequent assessments. The CPE reduction assay indicated consistent antiviral potential of compound 24. IC50 of RDV and compound 24 were found to be 31.54 and 8.320 respectively while the CC50 values of RDV and compound 24 were 307.2 and 202.3, respectively (Fig. 1A,B).
The cytotoxicity profile and anti-SARS-CoV-2 potential of compound 24 and Remdesivir (RDV). (A) Represents the IC50 of compound 24 and RDV with the R2 0.998 and 0.996, respectively; while (B) represents the CC50 of compound 24 and RDV with the R2 0.895 and 0.906, respectively. The data is represented as mean ± SD.
The selectivity index (SI) of individual compound, is the ratio of 50% cytotoxicity concentration (CC50) of normal kidney cells over IC50, was also evaluated. SI represents the safety of testes compound relative to its anti-SARS-CoV-2 activity. The obtained results indicated that the compound 24 showed high selectivity index as compared to standard drug RDV (Table 1).
Compound 24 inhibits cytopathic effects of SARS-CoV-2
The reduction of cytopathic effect of the compound and drugs was observed under a light microscope at 72 h post-infection (hpi), which indicated that compound 24 reduced > 90% of SARS-CoV-2 infection (Fig. 2). The potential of compound 24 to reduce the viral-induced CPE was further validated through a plaque reduction assay (PRA), which indicated that at the concentration of 83 µM compound 24 reduced plaque formation by 92.85 ± 3.57%. In contrast, plaque reduction by RDV was observed as 85.71 ± 5.45% (Fig. 2).
Compound 24 efficiently reduced SARS-CoV-2-induced plaque formation. (A) A marked decrease in the PFU/mL was observed after treatment with compound 24 as compared to the Remdesivir at the concentration of 83 µM. (B) Representative images of Vero cells 5 dpi with SARS-CoV-2. Infected cells treated with compound 24 and RDV showed a lesser number of plaques than non-treated infected cells. The data is represented as mean ± SD.
Effect of compound 24 at different time-points
To elucidate the possible viral entry or life cycle points (multi-target therapeutics) at which compound 24 acts to inhibit SARS-CoV-2, a time-point assay was carried out. The results indicated that compound 24 possesses strongest inhibitory effect at the “entry” time-point (2.17-fold inhibition), suggesting that it might inhibits SARS-CoV-2 entry into the cells. The assay also indicated towards prophylactic potential of the compound indicated by inhibition at this time point (0.8-fold inhibition). Additionally, the assay revealed that the compound also inhibits the post-entry stage, indicating its therapeutic potential (0.822-fold inhibition) (Fig. 3). A p-value < 0.001 with a R2-score of 0.936 indicated the significance of the results and goodness-of-fit.
Effect of compound 24 at different viral time points in compound-treated SARS-CoV-2 infected Vero cells. Log fold-change was calculated compared to virus-treated cells before (prophylactic), during (entry), and after (therapeutic) compound treatments at 83 µM concentration, and the mean fold-change was plotted. The asterisk indicates the significance between different groups. One-way ANOVA, followed by Bonferroni’s Multiple Comparison Test was performed as a statistical analysis (∗p < 0.05, ∗∗p < 0.01, ***p < 0.001).
Potential gene targets of the compound 24
To further confirm the anti-SARS-CoV-2 activity of compound 24, the effects of the compound 24 on expression of viral genes open reading frames 1a and 1b (ORF1a/b), nucleocapsid (N), spike (S), and RNA-dependent RNA polymerase (RdRp), and host cellular gene angiotensin-converting enzyme 2 (ACE-2) were assessed. The results indicated a significant decrease in the expression of N gene (fold-change = 0.29) by compound 24, as compared to the RDV (p-value < 0.05) (Fig. 4). The compound treatment also significantly reduced the expression of the S gene (fold-change = 1.1), as compared to the RDV (p-value < 0.01). Furthermore, compound 24 caused highly significant (p-value < 0.001) down-regulation of the gene expressions of ORF1a/b, ACE-2, and RdRp with fold-changes of 2.05, 0.58, and 1.4, respectively (Fig. 4A–E) as compared to the drug control RDV.
Sulfonohydrazide derivative down-regulates the expression of SARS-CoV-2 spike and nucleocapsid proteins
In order to validate the gene expression studies, immunofluorescence assay of N and S proteins of SARS-CoV-2 in the infected Vero cells treated with the compound was carried out via fluorescence microscopic analysis (Fig. 5A,B). The results revealed that compound 24 reduced protein expression of S and N proteins as depicted by decreased fluorescent intensity (FI) of 1.34 and 0.88%, respectively as compared to the higher FI of 3.42 and 2.02% for S and N proteins, respectively in untreated virus-infected Vero control cells (Fig. 5C,D).
The effect of compound 24 on the expression of SARS-CoV-2 S- and N-proteins. Representative immunofluorescence microscopic images of (A) Spike, and (B) Nucleocapsid proteins. Histograms of fluorescence intensity of (C) Spike, and (D) Nucleocapsid protein expressions using ImageJ software. RDV = Remdesivir, Blue fluorescence indicates the nucleus, and green fluorescence illustrates S or N protein.
Protein-ligand docking indicated strong binding scores of the compound 24 with viral proteins
To assess how strongly compound 24 interacted with the Nucleocapsid-C terminal (NCT), Nucleocapsid-N terminal (NNT), S, ACE-2, and RdRp proteins, in silico molecular docking analysis was performed. Compound 24 interacted with ACE-2, S, NNT, NCT, and RdRp with the bond score of -5.242, -4.796, -5.778, -5.084, and − 5.375, respectively. Reported docking scores in general demonstrated that below − 6.0 kcal/mol are considered to indicate moderate binding, while scores below − 8.0 kcal/mol generally suggest strong binding and thus presented results indicate the moderate binding. Moreover, the hydrogen bond energies were − 2.09, -0.58, -3.77, -2.94, and − 0.49 (Fig. 6).
Discussion
In 2020, SARS-CoV-2 emergence brought a global pandemic with an unprecedented healthcare crisis21, accounting for 775,335,916 confirmed cases and 7,045,569 deaths globally. In Pakistan, approximately 1,580,631 confirmed cases and 30,656 deaths were reported22. The loss in terms of morbidity, mortality, and economy worldwide that the pandemic has brought about has indicated the need of new and efficient antivirals. The persistence of SARS-CoV-2 in the population long after the pandemic and emergence of new variants, points towards the necessity of developing better anti-SARS-CoV-2 agents. There is a need for potent anti-SARS-CoV-2 molecules that could inhibit the emerging variants. This study investigates the anti-SARS-CoV-2 potential of a series of Sulfonohydrazide derivatives on Vero cells. Out of the evaluated 14 Sulfonohydrazide derivatives, compound 24 was observed to have the standard drug-comparable cytotoxicity and the highest antiviral effects. In vitro SARS-CoV-2 infection in Vero cells was confirmed by assessing cytopathic effects (CPE). Virus binding with cellular receptors consequently leads to viral tropism and pathogenicity by viral genomic RNA replication23,24, which causes structural, metabolic, or functional alterations in the infected cell, this phenomenon is known as cytopathic effects (CPE)24,25,26. In our study, CPE analysis revealed that the monolayer of Vero cells was completely disrupted in non-treated virus-infected control cells; however, it was intact in the compound 24 and RDV treated cells. Furthermore, the number of morphologically healthy cells was higher in compound-treated infected cells as compared to that in the standard drug control. Consistent with the CPE assay, plaque reduction assay (PRA) also indicated that the infection was alleviated in compound-treated cells with a 92.85% infectivity reduction, as compared to RDV-treated infected cells (85.71%). The study demonstrated that the number of plaques in the compound-treated infected cells (5 × 102 PFU/mL) was reduced as compared to the RDV-treated infected cells (1 × 103 PFU/mL), indicating the potent effects of compound 24 in reducing viral load, replication, and infection as compared to the standard drug.
To assess the possible molecular targets of the compound 24 conducive to its antiviral potential, viral load after compound treatment was assessed at three-time points: (1) before the SARS-CoV-2 infection, to determine if a compound can be used as a prophylactic agent treatment, (2) during the infection, that is at the viral entry point, and (3) after the infection, to identify if the compound target viral replication cycle and could be used as a therapeutic agent against the infection. The efficacies of compound 24 and RDV were evaluated by quantifying viral copy numbers via qRT-PCR. The time-point assay revealed that compound 24 inhibited viral infection at all the three points; however, it demonstrated marked inhibition of viral entry, suggesting that it might suppress SARS-CoV-2 infection via ACE-2 receptor on the cell. Moreover, the data suggested that RDV had therapeutic potential, consistent with the previously reported studies, suggesting that RDV operates at the post-viral entry stage by targeting the replication cycle27,28, validating our data.
To evaluate the gene targets through which compound 24 might act as a potential anti-SARS-CoV-2 gene expression analysis of viral genes including Orf1a/b, N, S, RdRP, and host receptor ACE-2 was performed by qRT-PCR. Orf1a/b encodes ~ 70% of the SARS-CoV-2 genome29,30. It was observed that the compound significantly down-regulated the Orf1a/b gene with the fold change (FC) of 2.05 in comparison with the positive control (FC = 0.4) (p-value < 0.001), suggesting anti-SARS-CoV-2 activity of the compound.
The gene expression analysis revealed that compound 24 highly significantly down-regulated S-gene (p-value < 0.01) and very highly significantly downregulated the ACE-2 gene (p-value < 0.001) expressions, validating that the compound controls the infection by targeting the SARS-CoV-2 entrance via S or ACE-2 proteins as observed in the time point assay. ACE-2 is a cellular membrane protein that has been shown to be implicated as a SARS-CoV-2 receptor in COVID-19 transmission and entry, thus is considered a competent target for viral inhibition. Several studies have revealed that reduced ACE-2 expression can alleviate SARS-CoV-2 infection31,32, whereas its upregulation enhances SARS-CoV-2 susceptibility33. Our data indicated that compound 24 could be used as a primary or secondary prophylaxis in COVID-19. Compound 24 also slightly reduced N-gene expression (p-value < 0.5). Moreover, RdRp expression analysis showed very highly significant inhibition by compound 24 as compared to the RDV-treated infected cells (p-value < 0.001), indicating that compound 24 might also target viral replication, which is consistent with the observations of the time point assay. These data suggest that compound 24 might inhibit in-vitro SARS-CoV-2 infection by targeting Orf1a/b, S, ACE-2, and RdRp genes.
The effect of compound 24 at the protein level was determined via immunofluorescence microscopy at 72 hpi. Since the above data suggested that compound 24 inhibits viral entrance and replication, S and N proteins were selected as the protein analysis targets. Immunofluorescence microscopy presented a clear picture of the SARS-CoV-2 infection of the Vero cells with or without treatment. The expression of both the S and N proteins in SARS-CoV-2-infected cells treated with compound 24 were observed to be reduced as compared to the untreated infected cells, indicating reduced protein expression. However, expression of both S and N proteins were higher for compound 24 treated infected group, as compared to the RDV-treated infected cells. Altogether, these observations indicate that compound 24 down-regulates S protein both at the genetic and protein levels, however, it is more potent at gene level when compared to the RDV-treated infected cells.
During the study, the Sulfonohydrazide derived compound 24, was further analyzed in silico molecular docking to elucidate the possible interaction sites of S, nucleocapsid-C terminal domain (N-CTD), N-terminal domain (N-NTD), RdRp, and ACE-2 proteins with the potential inhibitor33,34,35,36,37. In silico results revealed that NCT and NNT binding scores (BS) of the compound were − 5.084 and − 5.778, respectively (PDB ID: 7U0N and 7CE0, respectively). It was also demonstrated that OH at the C21 and C22 positions of the compound 24 interacted with N-CTD via hydrogen (H) bond at LYS45, ASP43, and GLU36 with H-bond energy (HE) = -2.94. Furthermore, the O at C9 and C10 of compound 24 formed an H-bond with ARG106, and OH at C21 interacted with ASP101 of N-NTD (HE = -3.77). When the compound was docked with RdRp protein (PDB ID: 7CDZ), it revealed that C20 and C9 of compound 24 formed H-bond with PHE321 and PHE396 of RdRp, respectively (BS = -5.375, HE= -0.49). Docking with ACE-2 protein (PDB ID: 7bW4) indicated that GLU375 of ACE-2 interacted with OH at C22 of compound 24, and a Pi-cation bond was also observed between ARG273 of ACE-2 protein and 24 (BS= -5.242, HE= -2.09). Moreover, in silico data also indicated that the NH group at C11 and OH at C21 of compound 24 interacted with GLU1092 and ARG1091 of S-protein via H-bond, respectively (BS = -4.796, HB = -2.09).
The findings of this study demonstrates the effects of Sulfonohydrazide derived compound 24 on SARS-CoV-2 entry, replication, and transcription as depicted by the downregulation of the Orf1a/b, N, S, RdRp, and ACE-2 genes. This was validated by protein expression analysis showing reduced expression of N and S proteins in SARS-CoV-2 infected cells after compound treatment. The compound also inhibited the viral infection depicted by reduced CPE and plaque formation. Time-point assay suggested that the probably target of compound 24 is the viral entry validated by the down-regulation of ACE-2 and S genes.
The current findings provide promising candidates for future drug development to fight against SARS-CoV-2, potentially targeting the COVID-19 pandemic and future viral threats. By identifying potent inhibitors, the research offers a foundation for subsequent investigations. However, there are some gaps particularly in terms of efficacy against emerging variant, and identification of potential effects in vivo studies. This work significantly contributes to the global health effort against COVID-19 and other viral pandemics. Future research should build on these results to bring this compound from the laboratory bench to the bedside, making them a potential tool in the global fight against infectious diseases.
Methodology
Compounds
The fully characterized and pure library of sylfonohdrazide derivatives were obtained from the Molecular Bank of PCMD, ICCBS, University of Karachi.
Cell lines
Vero cell line (ATCC CCL-81) was obtained from Bio-Bank, PCMD, ICCBS, University of Karachi and was grown as described previously38. Briefly, cells were cultured in Dulbecco’s minimal essential medium, supplemented with 10% fetal bovine serum (FBS), 100 unit/mL penicillin, 100 µg/mL streptomycin, 1 mM sodium pyruvate and 4 mM L-glutamine and termed as complete media (cDMEM). To propagate SARS-CoV-2 virus, infection media (iDMEM) was prepared with Dulbecco’s minimal essential medium, supplemented with 100 unit/mL penicillin, 100 µg/mL streptomycin, 1 mM sodium pyruvate and 4 mM L-glutamine.
Viral isolation and propagation
The SARS-CoV-2 wild-type strain was obtained from nasal swabs of COVID-19 patients and propagated in Vero cells as described by Case39. The virus was propagated by infecting Vero cells with 100 µL of viral transport medium (VTM) from the nasal swab in a tissue culture flask (25 cm2) in infection media (iDMEM). After 5 days post-infection (dpi), supernatants were harvested and centrifuged at 2,000 rpm for 5 min to remove cell debris40. Viral load was determined by PCR, and upon confirmation, the samples were stored in sterile falcons at -80 °C for further experimentation. All experiments involving virus were performed in an approved BSL-III facility of the National Institute of Virology, Dr. Panjwani Center for Molecular Medicine and Drug Research (PCMD), International Center for Chemical and Biological Sciences (ICCBS), University of Karachi, Pakistan.
Cell viability assay
The cytotoxic effect of the compounds and RDV on Vero cells was identified by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay41. Briefly, 2.5 × 104 cells/well were propagated in 96-well plates and incubated with the drugs and test compounds at 100, 75, 50, and 25 µM concentrations at 37 °C for 24 h. After incubation, MTT dye was added and was further incubated for 3–4 hours. Remdesivir was used as the positive control, untreated viral infected Vero cells were used as a negative control, and moreover DMSO control was also included in the study as a solvent control. All the experiments were performed in triplicates. After completion of the experiment, the absorbance was recorded by Multiskan Ascent Plate reader at 530 nm.
Cell viability (%)was measured as follows:
The standard antiviral drug, RDV, demonstrated the highest SARS-CoV-2 reduction at a concentration of 83 µM. Based on the optimization of the drug at this concentration, compounds that showed minimal or no toxicity were further evaluated at this selected concentration. For the purpose of this study, 83 µM is considered the reference concentration or endpoint measurement. Furthermore, for the evaluation of safety of tested compounds, the ratio of the 50% cytotoxic concentration (CC₅₀) in normal kidney cells to the 50% inhibitory concentration (IC₅₀) in term of selectivity index (SI) was also evaluated.
Confirmation of viral propagation in vero cells via q-PCR
For the confirmation and further quantification of viral copy number, whole cellular RNA was isolated using the QIAamp Viral RNA Mini Kit (Qiagen, Germany). qPCR was performed by using Bosphore® Novel Coronavirus (2019-nCoV) Detection Kit v7 (Turkey) by following the manufacturer’s protocol42.
Viral cytopathic effect (CPE) assay
The cytopathic effects (CPE) of virus was evaluated by following the Reed–Muench method40. Briefly, 2.5 × 104 cells/well were propagated in a 96-well plate. After 24 h, cells were infected with the virus for 1 h at a MOI of 0.01. After 1 h, viral inoculate was removed, and cDMEM was added to each well with compound (83µM) or RDV. CPE was observed at 3 dpi, and scoring was performed based on cell viability under a light microscope. Images were captured to record cellular morphology and inhibitory effects of the compound.
Scoring:
1 = 0–25% cell survival,
2 = 25-50% viable cells,
3 = 50-75% cells alive,
4 = 75-100% of cells survived infection.
Virus titration and infectivity assay
The virus titration and infectivity assay was performed as described previously43. The Vero cells (1 × 105/well) were propagated in 24-well plate for 24 h, then infected with SARS-CoV-2 at a MOI of 0.01. After 1 h, cells were treated with the compound and RDV at 100, 75, 50, and 25 µM concentrations for 1 h. After incubation, Carboxymethyle cellulose (CMC) was overlaid, and the plate was incubated for 5 days. After 5 days, CMC was aspirated, and cells were fixed with 4% paraformaldehyde (PFA) and stained with 1% crystal violet. The viral plaques were counted and PFU/mL was calculated.
Time-point assays
For the prophylactic analysis, a previously described assay was performed44. Briefly, the Vero cells (ATCC-CCL-81) were pre-treated with the drugs or compound and cultured in an infection medium (iDEME) for 1 h, and the virus was introduced for 2 h to allow infection. Subsequently, the cells were washed twice with 1x PBS and incubated for 48 h in drugs dissolved in a fresh infection medium. For the effect of compound or drugs on viral entry, the Vero cells were treated with the drugs during the infection period (2 h), followed by the removal of the drug-virus mixture and cell washing. Subsequently, the cells were incubated in an infection medium without any treatment for 48 h. For the assessment of therapeutic effect, the Vero cells were first infected with the virus for 2 h, washed with 1x PBS, and then treated with drugs in a fresh infection medium for 48 h. For the quantification of viral copy number, RNA was extracted via the QIAamp Viral RNA Mini Kit (Qiagen, Germany) followed by q-PCR and log 10-fold change was calculated.
Immunocytochemistry
The Vero cells were plated in a 96-well plate at a cell density of 2.5 × 104 cells/well for immunofluorescence microscopy and incubated at 37 °C in 5% CO2 for 5 days. At the end of 5 days, media was removed and the wells were washed with 1x PBS thrice. Following cell fixation with 4% PFA for 4 h, the cells were incubated with an optimized concentration of the spike (S) (MA5-35946, Invitrogen) and the nucleocapsid (N) (MAB10474, Invitrogen) monoclonal antibodies for 90 min, followed by 60 min of incubation with rabbit anti-mouse IgG FITC-linked secondary antibody. The cell nuclei were stained with DAPI for 15 min and the plate was observed under a fluorescence microscope (Nikon Eclipse). Representative images were captured at the magnification of 20x45.
Gene expression analysis
The gene expression analysis was performed as previously described46. Total RNA was extracted using the QIAamp Viral RNA Mini Kit (Qiagen, Germany) as per the manufacturer’s instructions. The expression of S, N, RdRp, and ACE-2 genes was evaluated by real-time PCR. GAPDH was used as endogenous control. For RdRp and ACE-2 gene analysis, each 10 µL reaction mixture comprised RT SYBR green PCR master mix, ddH2O, primer pairs, and cDNA template. For the gene expression analysis of RdRp and ACE-2, genes primers were obtained from Macrogen, Inc. The PCR conditions were: 95 °C for 3 min, 40 cycles of 95 °C for 10 s and (A) for 30 s, followed by 72 °C for 1 min and lastly, 72 °C for 5 min. Where A corresponds to an annealing temperature of 58 °C and 59.3 °C for RdRp and ACE-2, respectively. Melting curve analysis (65 °C for 5 s, and then 0.5 °C for 5 s until 95 °C) was performed after this reaction. For S and N gene expression analysis, the TaqPath COVID-19 Combo Kit (Applied Biosystems, Thermofisher Scientific) was utilized as per the kit’s guide. Relative RNA abundance was quantified by using the comparative CT (ΔΔCT) method and log10 fold-change was calculated. Briefly, the ΔCt was calculated for each sample and control, followed by difference in ΔCt of the sample and the control, which is known as ΔΔCT. In order to determine level of change in the expression of the target gene in the test sample differs from that in the control sample, fold-change was calculated by the following formula:
Fold Change = 2^(-ΔΔCT).
A log10 of the fold-change was calculated, which is interpreted as; positive log10 value indicates upregulation (fold change > 1), and a negative log10 value indicates downregulation (fold change < 1). If the fold change is 1 (no change), log10(1) = 0.
The primer sequences used were:
RdRp:
Forward: 5’-GTGARATGGTCATGTGTGGCGG-3’.
Reverse: 5’-CARATGTTAAASACACTATTAGCATA-3’.
ACE-2:
Forward: 5’-TCCAITGGTCTTCTGTCACCCG-3’.
Reverse: 5’-AGACCATCCACCTCCACTTCTC-3’.
Protein-ligand docking
The 3D crystallographic structure of S-protein, nucleocapsid-C terminal (NCT), nucleocapsid-N-terminal (NNT), RdRp, and ACE-2 were downloaded from the Protein Data Bank (PDB) database (PDB IDs: 7U0N, 7CE0, 7CDZ, and 7bW4). The Maestro software was employed to perform the protein-compound docking analysis47. The crystal structures were processed using the Protein Preparation Wizard. The compound’s (ligands) structure was obtained from the molecular bank of the International Institute of Chemical and Biological Sciences and drawn using Chem3Draw Ultra 13.0. The compound was prepared using the LigPrep tool21. The site map tool was used to generate the top 5 ligand binding sites; the highest affinity site was selected for the grid generation via the Receptor Grid Generation tool. The Ligand Docking tool was employed for docking. The interactions between the ligand and receptor, such as hydrogen bonds and hydrophobic and electrostatic interaction, were determined using the Maestro graphical interface.
Statistical analysis
The data entry, analysis, and processing were performed using GraphPad Prism (Version 8.02). All results are expressed as the mean ± standard deviation (SD). The data was analyzed using One-way ANOVA, followed by Bonferroni’s Multiple Comparison Test. The p-values less than 0.05 were designated as statistically significant for all results.
Conclusion
Our study provides evidence that studied Sulfonohydrazide derivative possess anti-SARS-CoV-2 properties. The study on compound 24 demonstrates that this molecule can efficiently alleviate the infection by targeting the cellular entrance of the SARS-CoV-2 viruses, and affecting overall replication or transcription by targeting ORF1a/b, S, RdRp, and ACE-2. The findings also suggest that compound 24 can serve as a potent drug molecule to treat COVID-19, and which can be developed as an anti-viral agent.
Data availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- RDV:
-
Remdisivir
- S:
-
Spike
- N:
-
Nucleocapsid
- RdRp:
-
RNA-dependent RNA polymerase
- ACE-2:
-
Angiotensin-converting enzyme 2
- hpi:
-
Hours post-infection
- dpi:
-
Days post-infection
- qRT-PCR:
-
Quantitative real-time–polymerase chain reaction
- PRA:
-
Plaque reduction assay
- CPE:
-
Cytopathic effect
References
Lamers, M. M. & Haagmans, B. L. SARS-CoV-2 pathogenesis. Nat. Rev. Microbiol. 20 (5), 270–284 (2022).
WHO. Coronavirus disease (COVID-19) pandemic. World Health Organization, Geneva. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (2020).
Sanjuán, R. & Domingo-Calap, P. Mechanisms of viral mutation. Cell. Mol. Life Sci. 73, 4433–4448 (2016).
Cascella, M. et al. Features, evaluation, and treatment of coronavirus (COVID-19) [Updated 2023 Aug 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; Jan (2024).
Flerlage, T., Boyd, D. F., Meliopoulos, V., Thomas, P. G. & Schultz-Cherry, S. Influenza virus and SARS-CoV-2: pathogenesis and host responses in the respiratory tract. Nat. Rev. Microbiol. 19 (7), 425–441 (2021).
Zhou, X., Li, Y., Li, T. & Zhang, W. Follow-up of asymptomatic patients with SARS-CoV-2 infection. Clin. Microbiol. Infect. 26 (7), 957–959 (2020).
Azkur, A. K. et al. Immune response to SARS-CoV‐2 and mechanisms of immunopathological changes in COVID‐19. Allergy 75 (7), 1564–1581 (2020).
Sourij, C. et al. Humoral immune response to COVID-19 vaccination in diabetes is age‐dependent but independent of type of diabetes and glycaemic control: the prospective COVAC‐DM cohort study. Diabetes Obesity Metab. 24 (5), 849 – 58 . (2022).
Wen, W., Chen, C., Tang, J., Wang, C., Zhou, M., Cheng, Y., & Mao, Q. Efficacy and safety of three new oral antiviral treatment (molnupiravir, fluvoxamine and Paxlovid) for COVID-19: a meta-analysis. Ann. Med. 54 (1), 516–523 (2022).
Mule, S. et al. Drug repurposing strategies and key challenges for COVID-19 management. J. Drug Target. 30 (4), 413–429 (2022).
Schmidt, P., Narayan, K., Li, Y., Kaku, C. I., Brown, M. E., Champney, E., … Walker,L. M. Antibody-mediated protection against symptomatic COVID-19 can be achieved at low serum neutralizing titers. Sci. Transl. Med. 15 (688), eadg2783. (2023).
Verma, G. et al. M. A review exploring biological activities of hydrazones. J. Pharm. Bioallied Sci. 6 (2), 69 (2014).
Tian, J., Ji, R., Wang, H., Li, S. & Zhang, G. Discovery of novel α-aminophosphonates with hydrazone as potential antiviral agents combined with active fragment and molecular Docking. Front. Chem. 10, 91145 (2022).
Kumar, D. et al. Benzylidene/2-chlorobenzylidene Hydrazides: synthesis, antimicrobial activity, QSAR studies and antiviral evaluation. Eur. J. Med. Chem. 45 (7), 2806–2816. https://doi.org/10.1016/j.ejmech.2010.03.002 (2010).
Şenkardes, S. et al. Synthesis of novel diflunisal hydrazide-hydrazones as anti-hepatitis C virus agents and hepatocellular carcinoma inhibitors. Eur. J. Med. Chem. 10, 301–308. https://doi.org/10.1016/j.ejmech.2015.10.041 (2016).
Rossi, S. et al. Discovery of p-Trifluoromethylbenzohydrazide derivatives as potent antiviral agents against Monkeypox virus. ACS Med. Chem. Lett. https://doi.org/10.1021/acsmedchemlett.5c00075 (2025).
Liu, X. et al. Discovery of Aryl benzoyl Hydrazide derivatives as novel potent Broad-Spectrum inhibitors of influenza A virus RNA-Dependent RNA polymerase (RdRp). J. Med. Chem. 65 (5), 3814–3832. https://doi.org/10.1021/acs.jmedchem.1c01257 (2022).
Zhao, H. et al. Discovery of hydrazide-containing oseltamivir analogues as potent inhibitors of influenza A neuraminidase. Eur. J. Med. Chem. 221 https://doi.org/10.1016/j.ejmech.2021.113567 (2021).
Mohamed, S. K. et al. Synthesis, crystal structure, and a molecular modeling approach to identify effective antiviral Hydrazide derivative against the main protease of SARS-CoV-2. J. Mol. Struct. 1265, 133391. https://doi.org/10.1016/j.molstruc.2022.133391 (2022).
Abidiy, S. I. et al. Antiviral activity of hydrazone derivatives based benzohydrazide/2-thiohydantoin analogs against HPV-18 (human papillomavirus): In silico study. AIP Conf. Proc. 3071 (1), 020015. https://doi.org/10.1063/5.0206875 (2024).
Ciotti, M. et al. The COVID-19 pandemic. Crit. Rev. Clin. Lab. Sci. 57 (6), 365–388 (2020).
WHO Coronavirus (COVID-19) Dashboard. World Health Organization. https://covid19.who.int/?adgroupsurvey={adgroupsurvey}&gclid=Cj0KCQjwhL6pBhDjARIsAGx8D58-_nkvD0e-LoIj0P-ZBF4C2ugQA_HXRtECt8OOCjCuToxfPkTAFf4aAtQhEALw_wcB. (2023).
V’kovski, P., Kratzel, A., Steiner, S., Stalder, H. & Thiel, V. Coronavirus biology and replication: implications for SARS-CoV-2. Nat. Rev. Microbiol. 19 (3), 155–170 (2021).
Oxford, A. E., Halla, F., Robertson, E. B. & Morrison, B. E. Endothelial cell contributions to COVID-19. Pathogens 9 (10), 785 (2020).
Lowenstein, C. J. & Solomon, S. D. Severe COVID-19 is a microvascular disease. Circulation 142 (17), 1609–1611 (2020).
Drożdżal, S. et al. J. FDA-approved drugs with pharmacotherapeutic potential for SARS-CoV-2 (COVID-19) therapy. Drug Resist. Updates. 53, 100719 (2020).
Wang, M. et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 30 (3), 269–271 (2020).
Nguyen, H. T., Falzarano, D., Gerdts, V. & Liu, Q. Construction of a noninfectious SARS-CoV-2 replicon for antiviral-drug testing and gene function studies. J. Virol. 95 (18), 10–128 (2021).
Helmy, Y. A. et al. The COVID-19 pandemic: a comprehensive review of taxonomy, genetics, epidemiology, diagnosis, treatment, and control. J. Clin. Med. 9, 1225 (2020).
Arya, R. et al. Structural insights into SARS-CoV-2 proteins. J. Mol. Biol. 433, 166725 (2021).
Brevini, T. et al. FXR Inhibition May protect from SARS-CoV-2 infection by reducing ACE-2. Nature 615, 134–142 (2023).
Oh, C. K. et al. Targeted protein S-nitrosylation of ACE-2 inhibits SARS-CoV-2 infection. Nat. Chem. Biol. 19, 275–283 (2023).
Garreta, E. et al. A diabetic milieu increases ACE-2 expression and cellular susceptibility to SARS-CoV-2 infections in human kidney organoids and patient cells. Cell Metabol. 34, 857–873 (2022).
Peng, Y. et al. Structures of the SARS-CoV‐2 nucleocapsid and their perspectives for drug design. EMBO J. 39, e105938 (2020a).
Peng, Q. et al. Structural and biochemical characterization of the nsp12-nsp7-nsp8 core polymerase complex from SARS-CoV-2. Cell Rep. 31 (2020).
Xu, Y. et al. Off-target in vitro profiling demonstrates that Remdesivir is a highly selective antiviral agent. Antimicrob. Agents Chemother. 65, 10–128 (2021).
Geng, Q. et al. Structural basis for human receptor recognition by SARS-CoV-2 Omicron variant BA.1. J. Virol. 96, e00249–e00222 (2022).
Ogando, N. S. et al. J. T. J. O. G. V. SARS-coronavirus-2 replication in vero E6 cells: replication kinetics, rapid adaptation and cytopathology. 101 (9), 925 (2020).
Case, J. B., Bailey, A. L., Kim, A. S., Chen, R. E. & Diamond, M. S. Growth, detection, quantification, and inactivation of SARS-CoV-2. Virology 548, 39–48. https://doi.org/10.1016/j.virol.2020.05.015 (2020).
Reed, L. J. & Muench, H. A simple method of estimating fifty-percent endpoints. Am. J. Hyg. 27, 493–497 (1938).
Rekha, S. & Anila, E. I. Vitro cytotoxicity studies of surface modified CaS nanoparticles on L929 cell lines using MTT assay. Mater. Lett. 236, 637–639 (2019).
Malik, H. et al. Identification of effective synthetic molecules against viral-induced cytokine release syndrome using in silico and in vitro approaches. Mol. Diversity 1–13. https://doi.org/10.1007/s11030-025-11136-3 (2025).
Farooq, S., Wahab, A. T., Rahman, A. U. & Choudhary, M. I. Preventive potential of dietary extracts against SARS-CoV-2 infections. Curr. Traditional Med. 10, 31–39. https://doi.org/10.2174/2215083809666230116141143 (2024).
Fatima, R., Farooq, S., Moin, S. T., Choudhary, M. I. & Yousuf, S. Creating cocrystal salts: synthesis, crystal structure, Hirshfeld surface analysis and quantum chemical calculations of pyrimethamine and their potential anti- SARS-Cov-2 activity. J. Mol. Struct. 1325 https://doi.org/10.1016/j.molstruc.2024.140982 (2025).
Yang, J. et al. Fluorogenic reporter enables identification of compounds that inhibit SARS-CoV-2. Nat. Microbiol. 8, 121–134. https://doi.org/10.1038/s41564-022-01288-5 (2023).
Khan, A. M., Wahab, A. T., Farooq, F., Ullah, A. & Choudhary Repurposing of US-FDA approved drugs against SARS-CoV-2 main protease (Mpro) by using STD-NMR spectroscopy, in Silico studies and antiviral assays. Int. J. Biol. Macromol. 234, 123540 (2023).
Schrodinger Maestro https://www.schrodinger.com/products/maestro (2023).
Acknowledgements
The authors would like to acknowledge Prof. Dr. Daniel Sauter from the Institute for Medical Virology and Epidemiology of Viral Diseases, University Hospital and Medical Faculty, Eberhard Karls University, Tuebingen-72076, Germany, for his guidance in manuscript review.
Funding
This research was conducted by the Institutional Recurring Research funds to Saba Farooq.
Author information
Authors and Affiliations
Contributions
Z.K.: performed the experiments and analysis, original draft writing, S.F.: supervision performed the formal analysis, designed the methodology, prepared, reviewed, and edited the manuscript. A-T.W.: Conceptualized and designed the study, managed the project, reviewed and edited the manuscript, and discussed the results critically; H.I.: reviewed and edited the manuscript and discussed the research and results. T.I.: Reviewed and edited the manuscript. K.M.K: Reviewed and edited the manuscript. FN: Compound Synthesis. M.Y.: Reviewed and edited the manuscript. M.I.C.: Provided the resources, conceptualization, managed the project, discussed the results critically, and reviewed and edited the manuscript. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The research study was ethically approved by the Independent Ethics Committee (IEC), Dr. Panjwani Center for Molecular Medicine and & Drug Research, International Center for Chemical and Biological Sciences, University of Karachi (Reference # ICCBS/IEC-066-HNS/PC2021/Protocol/2.0). This study was conducted in accordance with the principles of the Declaration of Helsinki. All experiments were performed in accordance with relevant guidelines and regulations.
Consent to participate
Informed consent for taking the nasal swab have been obtained from participant in accordance with relevant guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Khan, Z., Farooq, S., Atia-tul-Wahab et al. Sulfonohydrazide as a potential inhibitor of SARS-CoV-2 infection. Sci Rep 15, 18732 (2025). https://doi.org/10.1038/s41598-025-03685-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-03685-2