Abstract
This study aims to explore the association between hearing impairment, visual impairment, dual sensory impairment, and depressive symptoms in middle-aged and elderly populations in China, with an analysis of gender differences. This research is based on data from the nationally representative sample survey CHARLS, conducted from 2013 to 2020. A total of 9,780 participants were included in the study. These participants were divided into four groups based on their hearing and vision status: no impairment, hearing impairment only, visual impairment only, and dual sensory impairment. A longitudinal analysis was conducted using Cox regression models to assess the hazard ratios (HR) for the occurrence of depressive symptoms associated with hearing, visual, and dual sensory impairments. The Cox regression model indicated that, in the unadjusted model, hearing impairment, visual impairment, and dual sensory impairment were all risk factors for depression (P < 0.05). After adjusting for multiple confounding factors, compared to the no impairment group, the risk of depressive symptoms was 1.017 times higher (95% CI 0.886–1.167) in the hearing impairment group, with a gender-specific risk of 1.072 times (95% CI 0.880–1.305) for males and 0.962 times (95% CI 0.793–1.168) for females. The visual impairment group had a 1.118 times higher risk (95% CI 1.017–1.231), with a risk of 1.092 times (95% CI 0.946–1.262) for males and 1.155 times (95% CI 1.017–1.311) for females. The dual sensory impairment group had a 1.274 times higher risk (95% CI 1.165–1.393), with a gender-specific risk of 1.291 times (95% CI 1.131–1.473) for males and 1.267 times (95% CI 1.123–1.429) for females. Visual impairment and dual sensory impairment are independent risk factors for the occurrence of depressive symptoms, with notable gender differences. Understanding these associations and gender differences can help in developing more effective interventions to improve the mental health of middle-aged and elderly populations.
Similar content being viewed by others
Introduction
With the intensifying global aging society, sensory impairments such as hearing and vision impairments are becoming increasingly common among middle-aged and older adults. According to the 2019 Global Burden of Disease data, over 1.5 billion people suffer from hearing loss, with approximately 403 million individuals (26%) experiencing moderate or more severe hearing loss1.Data from 2020 indicate that 43.2 million people are blind, 295.3 million have moderate to severe visual impairment, and 257.3 million have mild visual impairment2.In China, the prevalence of visual impairment among middle-aged and older adults is as high as 21.03%, and about one-third of the elderly population suffers from moderate or greater hearing loss3.Against this backdrop of high sensory impairment prevalence, differences in sensory impairment types between genders exist. Research shows that men are more likely to suffer from hearing impairments, while women are more prone to visual impairments4.Regardless of gender, studies indicate that many middle-aged and older adults with sensory impairments experience a decline in quality of life and daily functioning, manifested as social isolation, increased dependency, reduced social activities, and depression4.
Depression is one of the most common mental health issues worldwide. Although its prevalence varies significantly between countries, it remains high overall5.The high prevalence of depression is not only one of the main causes of global disability and suicide but is also considered an important predictor of suicide risk and physical function decline in middle-aged and older adults6.Among this population, sensory impairments are often accompanied by depression. Numerous studies have shown that a single sensory impairment increases the risk of depression in middle-aged and older adults. For instance, hearing loss affects communication ability, mental health, and quality of life, potentially leading to social isolation and depression7.However, while the individual impacts of hearing and visual impairments on depression have been studied, research on the combined effects of dual sensory impairment on mental health is relatively scarce.
Despite increasing awareness of sensory impairments, few studies have investigated the comprehensive impact of dual sensory impairment on depression, especially considering potential gender differences. By analyzing the differences in the relationship between hearing and visual impairments and depression across genders, this study aims to understand the role of gender in mental health, promote gender-specific personalized interventions, and improve the overall health levels of middle-aged and older adults. Therefore, this study aims to explore the following three questions: (1) What is the relationship between hearing, vision, and dual sensory impairments and depression in middle-aged and older adults? (2) Are there significant gender differences in this relationship? (3) What factors mediate the relationship between sensory impairments and depression?
Methods
Participants
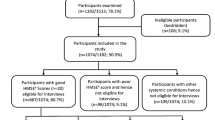
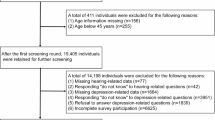
The subjects of this study were derived from the China Health and Retirement Longitudinal Study (CHARLS) participants. CHARLS is a national longitudinal survey targeting Chinese individuals aged 45 and above and their spouses, covering 150 counties and 450 communities (villages) across 29 provinces (autonomous regions, municipalities) in China. The baseline study was conducted in 2011, with assessments and follow-ups every two years, including physical measurements during follow-ups. The CHARLS database comprises seven modules: basic information, family information, health status and function, healthcare and insurance, work retirement and pensions, income expenditure and assets, housing conditions, as well as detailed physical examination and blood test information. This study selected eligible participants from the longitudinal data spanning 2013–2020 for analysis. The data comply with the Declaration of Helsinki and have been approved by the Institutional Review Board (IRB00001052-11,015) of Peking University8.This study defines individuals aged 45 and above as middle-aged and older adults. Inclusion criteria: (1) Middle-aged and older adults (age ≥ 45). (2) At least three follow-ups. Exclusion criteria: (1) Excluding individuals with missing health status and basic information. (2) Excluding individuals with missing baseline vision, hearing, and depression information. (3) Excluding individuals with baseline depression. (4) Excluding individuals with missing follow-up depression data and those lost to follow-up. A total of 9,781 individuals were included in this study (Fig. 1).
Variables and measurement methods
Depression measurement
In the CHARLS survey, the simplified CES-D10 scale was integrated into the questionnaire (DC009-018) to assess the respondents’ level of depression. The Chinese version of this scale has been widely used among the elderly population in China, demonstrating good reliability and validity, with a total Cronbach’s alpha coefficient of 0.8159.Each question in the questionnaire is scored on a four-point scale: "Rarely or none of the time" (0 points), "Some or a little of the time" (1 point), "Occasionally or a moderate amount of the time" (2 points), and "Most or all of the time" (3 points). The total score is 30 points, with higher scores indicating a higher risk of depression. Among the 10 questions, questions 5 and 8 are reverse scored, while for the remaining 8 questions, "Rarely or none of the time" scores 0 points, with scores increasing incrementally. A CES-D10 score of 10 or higher is considered indicative of depression, while a score below 10 is considered within the normal range.
Vision and hearing measurement
Self-reported hearing was assessed using the following questionnaire item DA039: "Would you say your hearing is excellent, very good, good, fair, or poor (if you use a hearing aid)?" Self-reported vision was assessed using two questions (DA033 and DA034): "How good is your vision for seeing things at a distance/close up (with glasses or corrective lenses, if needed)? Would you say your vision for seeing things at a distance/close up is excellent, very good, good, fair, or poor?" Vision and hearing reported as “fair” or “poor” were classified as visual or hearing impairments, respectively. In this study, participants with only visual impairment were defined as having a visual impairment, those with only hearing impairment as having a hearing impairment, and those with both visual and hearing impairments as having dual sensory impairment.
Covariate measurement
Based on previous research, the following influencing factors were included in the model for confounder adjustment: ①Demographic Factors: Including age and gender. ②Sociological Factors: Including education level, marital status, and residence (urban or rural). ③Health-related Factors: Including sleep, social participation, cognitive ability, activities of daily living, hospitalization status, number of chronic diseases, and pain status (whether there is pain or not).Cognitive ability was assessed using the MMSE scale, which includes fixed and variable abilities, specifically evaluating episodic memory (memory test, delayed memory test), mental status (orientation to time and place, calculation, drawing ability test). The score ranges from 0 to 30, with higher scores indicating better cognitive function10.Activities of daily living (ADL) were assessed using the ADL scale, which includes 6 activities: dressing, bathing, eating, getting in or out of bed, toileting, and controlling urination and defecation. The responses are categorized as "no difficulty," "some difficulty but can complete," "difficulty and needs help to complete," and "completely unable to complete." Difficulty in completing any task indicates ADL impairment11.Social participation was measured through question DA056, asking respondents if they had engaged in any of the following 12 social activities in the past month: (1) Interacted with friends; (2) Played mahjong, chess, cards, or went to a community club; (3) Helped family, friends, or neighbors who do not live with them; (4) Participated in a sports club, social club, or other club; (5) Participated in community organizations; (6) Engaged in volunteer or charity work; (7) Cared for sick or disabled adults who do not live with them; (8) Attended an educational or training course; (9) Invested in stocks; (10) Used the internet; (11) Other social activities; (12) None of the above. If any of the first 11 options were selected, the middle-aged individual was considered to have participated in social activities; otherwise, they were considered not to have participated in social activities.
Statistical analysis
Continuous variables with non-normal distributions were described using the median (interquartile range), and differences between two groups were compared using the Wilcoxon Mann–Whitney test, while differences among multiple groups were compared using the Kruskal–Wallis test. Continuous variables with normal distributions were described using the mean ± standard deviation, and differences between two groups were compared using the t-test, while differences among multiple groups were compared using one-way ANOVA. Categorical variables were described using frequency (percentage), and differences between groups were compared using the chi-square test. To explore the association between baseline visual and hearing impairments, dual sensory impairment, and the risk of depressive symptoms, Schoenfeld residuals were used to test the proportional hazards (PH) assumption for model variables. After confirming that all variables met the PH assumption (P > 0.05), Cox proportional hazards regression models were used to calculate hazard ratios (HR) and 95% confidence intervals (CI) to analyze the association between baseline sensory impairment levels and the risk of depressive symptoms. During the process of establishing the COX model, confounding factors were gradually controlled. Model 1 does not control for any factors; Model 2 adjusts for age and gender; Model 3 adjusts for socioeconomic variables based on Model 2; and Model 4 controls for health behavior factors based on Model 3.Subgroup analyses were conducted for males and females. To ensure the stability of the results, multiple imputation (Random Imputation) was performed for the covariate data12, and sensitivity analyses were conducted comparing imputed and non-imputed data. All statistical analyses were conducted using SPSS 26.0 and R (version 4.1.3).
Results
Basic characteristics of study subjects
A total of 9,780 subjects were included in this study. Among them, 1,798 (18.3%) middle-aged and older adults had no sensory impairments, 694 (7.1%) had only hearing impairment, 2654 (27.1%) had only visual impairment, and 4,634 (47.4%) had dual sensory impairments. The average age of the study population was 58 years, with 4947 (50.5%) males. Compared to those without sensory impairments, the age was higher in the visual impairment group (56 vs. 57.3), and even higher in the hearing impairment and dual sensory impairment groups (56 vs. 59 vs. 59). The proportion of males was higher in the hearing impairment group compared to those without sensory impairments (54% vs. 56%), while the proportion of females was higher in the visual impairment group (45% vs. 51%). The gender ratio in the dual sensory impairment group was relatively balanced (50% male and female).
Compared to those without sensory impairments, individuals with visual, hearing, and dual sensory impairments had lower levels of education, more severe disability, and shorter sleep duration. Additionally, compared to older adults without sensory impairments, those with visual, hearing, and dual sensory impairments showed significant differences in hospitalization status, social participation, cognitive ability, number of chronic diseases, and pain status (P < 0.05). See Table 1 for details.
Longitudinal association between hearing, visual, and dual sensory impairments and depression
In the longitudinal analysis of hearing, visual, and dual sensory impairments and depression (see Table 2), the unadjusted Model 1 shows that compared to the group without sensory impairments, the risk of depressive symptoms was 1.172 (95% CI 1.023–1.343) in the hearing impairment group, 1.271 (95% CI 1.157–1.396) in the visual impairment group, and 1.684 (95% CI 1.548–1.833) in the dual sensory impairment group. After adjusting for age and gender, the risk decreased to 1.162 (95% CI 1.014–1.332) in the hearing impairment group, 1.239 (95% CI 1.277–1.361) in the visual impairment group, and 1.634 (95% CI 1.500–1.778) in the dual sensory impairment group. Further adjustments for education level, marital status, and residence resulted in risks of 1.233 (95% CI 1.122–1.355) in the visual impairment group and 1.568 (95% CI 1.440–1.708) in the dual sensory impairment group. Finally, after adjusting for sleep, social participation, cognitive ability, hospitalization status, number of chronic diseases, activities of daily living, and pain status, the risk of depressive symptoms was reduced to 1.017 (95% CI 0.886–1.167) in the hearing impairment group, 1.118 (95% CI 1.017–1.231) in the visual impairment group, and 1.274 (95% CI 1.165–1.393) in the dual sensory impairment group.
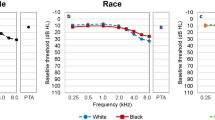
Gender differences in the association between hearing, visual, and dual sensory impairments and depression
In the longitudinal analysis of hearing and visual impairments and depression (see Table 3), compared to the group without sensory impairments, the unadjusted risk of depressive symptoms for men in the hearing impairment group was 1.276 (95% CI 1.051–1.548), while it was not statistically significant for women (p > 0.05). After adjusting for sociodemographic and health status factors, the HR for women was 0.962 (95% CI 0.793–1.168) and 1.162 (95% CI 1.014–1.332) for men. In the visual impairment group, the unadjusted risk of depressive symptoms for women was 1.266 (95% CI 1.117–1.453), and after adjustments, the risk remained at 1.155 (95% CI 1.017–1.311). For men, the unadjusted risk was 1.211 (95% CI 1.050–1.397), which changed to 1.092 (95% CI 0.946–1.262) after adjustments. In the dual sensory impairment group, after adjusting for sociodemographic and health status factors, the HR was 1.291 (95% CI 1.131–1.473) for men and 1.267 (95% CI 1.123–1.429) for women (Fig. 2).
Sensitivity analysis
After performing multiple imputations for covariate data and adjusting for sociodemographic variables and personal health behaviors, the results remained consistent, indicating that visual impairment and dual sensory impairment are independent risk factors for the occurrence of depression, with risks significantly higher than those of single sensory impairments (see Table 4).
Discussion
This study aimed to investigate the longitudinal relationship between self-reported sensory impairments and depression in China. Over an average follow-up period of 5.57 years, middle-aged and older adults with dual sensory impairments had the highest prevalence of depressive symptoms (54.6%), followed by those with visual impairments (45.5%) and hearing impairments (42.9%). This is consistent with previous studies indicating that visual impairment has a more significant impact on the mental health of Chinese older adults compared to hearing loss13.Furthermore, this study found that the impact of sensory impairments on depressive symptoms accumulates over time. Specifically, individuals with dual sensory impairments face a higher risk of depression compared to those with only a single sensory impairment14,15. This finding suggests that in long-term health monitoring and intervention processes, particular attention should be paid to older adults whose sensory impairments are progressively worsening or developing from single to dual impairments.
Association between visual impairment and depressive symptoms and gender differences
This study demonstrates that visual impairment, after adjusting for confounding factors, is an independent risk factor for the occurrence of depressive symptoms, with this result being more pronounced in women than in men. This may be closely related to physiological, psychological, and sociocultural factors. Research indicates that women are more significantly affected by hormonal level changes, particularly after menopause16. The neuroprotective effects of estrogen on the brain have been widely studied, and the decline in estrogen levels may make women more sensitive to stress and depression. This physiological change could make the impact of visual impairment on women’s mental health more significant16. Additionally, studies show that visual impairment significantly affects daily living activities and quality of life, and women may bear more household responsibilities in their daily lives17. Visual impairment may make these activities more challenging, increasing psychological stress and the risk of depression. Understanding these mechanisms can help in developing more effective interventions to assist women in better coping with visual impairment and depressive symptoms.
Association between hearing impairment and depressive symptoms and gender differences
This study shows that hearing impairment increases the risk of depressive symptoms in unadjusted models, with this result being more pronounced in men than in women. This may be related to significant differences between men and women in the structure and function of the auditory system, neurotransmitter systems, and brain plasticity18. These physiological and biological differences may lead to a more pronounced negative impact on men when facing hearing impairment, making them more susceptible to depressive symptoms19. Research indicates that the cochlear basilar membrane in men is relatively thicker, which may make men more prone to high-frequency hearing loss. High-frequency hearing loss typically leads to difficulties in speech comprehension, subsequently affecting social interactions and emotional health20. Other studies suggest that the brain’s regulatory mechanisms for dopamine, serotonin (5-HT), and gamma-aminobutyric acid (GABA) differ between men and women. Hearing loss may disrupt the balance of these neurotransmitter systems, making men more prone to emotional fluctuations and depressive symptoms under such circumstances21,22.Hearing impairment was significantly associated with depressive symptoms before adjusting for demographic variables, but after adjusting for factors such as sleep, social participation, activities of daily living, and cognitive function, the association lost its statistical significance. This suggests that these health factors may play a key moderating and mediating role in this relationship. Multiple studies have confirmed this point23. For example, people with higher social participation generally enjoy better mental health, as social activities can provide emotional support and alleviate feelings of loneliness and depression. Hearing impairment may limit an individual’s social activities, leading to increased feelings of isolation24,25. By adjusting for the variable of social participation, the significant impact of social activities on depressive symptoms becomes evident, thereby weakening the role of hearing impairment as an independent variable. Furthermore, studies have shown that a decline in cognitive ability is often accompanied by an increase in depressive symptoms26. Hearing impairment may indirectly lead to depression by affecting cognitive functions such as information processing speed and memory27. However, when adjusting for cognitive ability, its direct impact on depressive symptoms is isolated, weakening the association between hearing impairment and depressive symptoms.
In conclusion, the relationship between hearing impairment and depression is likely not a single pathway but influenced by multiple pathways and factors. The specific mechanisms by which hearing loss increases the risk of depressive symptoms remain unclear. Therefore, future research should combine imaging, neuropsychology, and audiology to conduct more high-quality studies to improve the overall health status of patients with hearing impairment, effectively preventing and alleviating depressive symptoms.
Association between dual sensory impairment and depressive symptoms and gender differences
Although visual impairment is an independent risk factor for depressive symptoms, the presence of hearing impairment in addition to visual impairment significantly increases the risk of depressive symptoms. This dual sensory impairment is not only an independent risk factor for depressive symptoms but also has a much greater impact than either visual or hearing impairment alone. Notably, this effect is more pronounced in men than in women. Research has shown that the auditory cortex and visual cortex of the brain work closely together when processing sensory information, and dual sensory impairment disrupts the normal function and interaction between these cortices, leading to decreased information processing efficiency and cognitive impairment26. Studies also indicate that individuals often rely on both vision and hearing to complete daily tasks, and dual sensory impairment forces the brain to multitask with limited information, which may result in cognitive decline and difficulty in emotional regulation28. These combined effects explain why dual sensory impairment has a much greater impact on depressive symptoms than either visual or hearing impairment alone.
However, there is currently limited research specifically examining why this association is more significant in men than in women. From a social psychology perspective, studies have suggested that men in traditional Chinese society are often expected to be stronger and more independent. Dual sensory impairment may hinder them from fulfilling these expectations, leading to greater psychological stress and damage to their self-esteem28,29. This role conflict may make men more susceptible to depressive symptoms. Additionally, men typically engage in social activities more frequently than women and therefore rely more on their hearing and vision30. Consequently, dual sensory impairment may cause them to feel greater barriers and isolation in social settings, adversely affecting their mental health.
Strengths and limitations
This study utilized data from the most recently released nationally representative sample survey, CHARLS, in 2020, providing updated evidence on the association between hearing and visual impairments and depressive symptoms, as well as gender differences. The study employed a longitudinal design, excluding individuals with baseline depression, and adjusted for comprehensive confounding factors. Sensitivity analyses were also conducted with imputed data, making the conclusions more reliable.
However, there are certain limitations in this study. Firstly, the measurement of hearing and vision relied on subjective self-assessments, which may differ from objective measurements. However, it is important to note that subjective self-reports of sensory impairments remain highly relevant, particularly when exploring their relationship with quality of life. These self-assessments are widely accepted and utilized in research, especially in populations such as those with Mild Cognitive Impairment (MCI)31. Secondly, the study only assessed hearing and visual status at baseline, thus it was unable to capture the dynamic relationship between hearing and visual status and depression over time. Future studies could benefit from incorporating longitudinal data to explore these dynamic changes and their impact on depression.
Conclusion
In summary, this study explored the relationship between hearing, visual, and dual sensory impairments and depressive symptoms in middle-aged and older adults through longitudinal analysis, revealing the impact of gender differences. The results indicate that visual impairment and dual sensory impairment are independent risk factors for depressive symptoms, with visual impairment having a more significant impact on women and dual sensory impairment having a greater impact on men. Additionally, the association between hearing impairment and depressive symptoms weakened after adjusting for health factors, suggesting that these health factors play a moderating role in this relationship. Future research should consider using more objective measurement methods and dynamically monitoring changes in hearing and vision variables to more comprehensively assess and explore the association between sensory impairments and depressive symptoms and their dynamic trajectories. Furthermore, combining multidisciplinary approaches such as imaging, neuropsychology, and audiology is essential to further investigate the specific mechanisms by which hearing and visual impairments affect depressive symptoms. This will aid in developing more effective interventions to help middle-aged and older adults improve their mental health and quality of life. Finally, future research could explore how to develop targeted interventions for each group based on gender differences to improve quality of life. Given the significant impact of dual sensory impairments on depression symptoms in men, research could focus on providing more support for men, such as through mental health interventions, improving social activities, and offering targeted rehabilitation programs, to help them better cope with the challenges posed by dual sensory impairments. By gaining a deeper understanding of gender differences, we can provide more effective strategies for enhancing quality of life for different gender groups, thereby improving overall health and reducing the incidence of depression.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available because of the privacy implications but are available from the corresponding authors on reasonable request.
References
Haile, L. M. et al. Hearing loss prevalence and years lived with disability, 1990–2019: Findings from the Global Burden of Disease Study 2019. Lancet 397(10278), 996–1009 (2021).
Vos, T. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 386(9995), 743–800 (2015).
Xu, T. et al. Prevalence and causes of vision loss in China from 1990 to 2019: Findings from the Global Burden of Disease Study 2019. Lancet Public Health 5(12), E682–E691 (2020).
Pardhan, S. et al. Visual, hearing, and dual sensory impairment are associated with higher depression and anxiety in women. Int. J. Geriatr. Psychiatry 36(9), 1378–1385 (2021).
Ruiz, M. et al. Life course socioeconomic position and incidence of mid-late life depression in China and England: A comparative analysis of CHARLS and ELSA. J. Epidemiol. Commun. Health 73(9), 817–824 (2019).
Levi-Belz, Y. & Birnbaum, S. Depression and suicide ideation among suicide-loss survivors: A six-year longitudinal study. Int. J. Environ. Res. Public Health 19, 1656124 (2022).
Choi, Y., Go, J. & Chung, J. W. Association between hearing level and mental health and quality of life in adults aged > 40 years. J. Audiol. Otol. 28(1), 52–58 (2024).
Zhao, Y. et al. Cohort profile: The China health and retirement longitudinal study (CHARLS). Int. J. Epidemiol. 43(1), 61–68 (2014).
Malakouti, S. K. et al. Reliability, validity and factor structure of the CES-D in Iranian elderly. Asian J. Psychiatry 18, 86 (2015).
Jia, L. et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: A cross-sectional study. Lancet Public Health 5(12), e661–e671 (2020).
Mengqi, L. Influencing factors and policy suggestions of mental health of Chinese elderly-based on 2015 China health and retirement longitudinal study (Admin Zhejiang University, 2018).
Sterne, J. A. et al. Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. BMJ 338, b2393 (2009).
Harada, S. et al. Gender difference in the relationships between vision and hearing impairments and negative well-being. Prev. Med. 47(4), 433–437 (2008).
Marmamula, S. et al. Depression, combined visual and hearing impairment (dual sensory impairment): A hidden multi-morbidity among the elderly in Residential Care in India. Sci. Rep. 11(1), 16189 (2021).
Armstrong, N. M. et al. Associations of dual sensory impairment with long-term depressive and anxiety symptoms in the United States. J. Affect Disord. 317, 114–122 (2022).
Kundakovic, M. & Rocks, D. Sex hormone fluctuation and increased female risk for depression and anxiety disorders: From clinical evidence to molecular mechanisms. Front. Neuroendocrinol. 66, 101010 (2022).
Ribeiro, M. V. et al. Association between visual impairment and depression in the elderly: A systematic review. Arq. Bras. Oftalmol. 78(3), 197–201 (2015).
Zhang, Z. Q. et al. Bidirectional associations between sensorineural hearing loss and depression and anxiety: A meta-analysis. Front Public Health 11, 1281689 (2023).
Reavis, K. M. et al. Sex-linked biology and gender-related research is essential to advancing hearing health. Ear Hear. 44(1), 10–27 (2023).
Sari, E. et al. The variations of osseous structure of the ınternal acoustic canal: An anatomical study. Brazil. J. Otorhinolaryngol. 90, 1014143 (2024).
Chakraborti, B. et al. Gender-specific effect of 5-HT and 5-HIAA on threshold level of behavioral symptoms and sex-bias in prevalence of autism spectrum disorder. Front. Neurosci. 13, 1375 (2020).
Rao, D. et al. Hearing loss alters serotonergic modulation of intrinsic excitability in auditory cortex. J. Neurophysiol. 104(5), 2693–2703 (2010).
Marques, T., Marques, F. D. & Miguéis, A. Age-related hearing loss, depression and auditory amplification: A randomized clinical trial. Eur. Arch. Otorhinolaryngol. 279(3), 1317–1321 (2022).
Wang, Z. et al. Hearing loss, depression and social participation of older adults: Evidence from the China health and retirement longitudinal study. Geriatr. Gerontol. Int. 22(7), 529–535 (2022).
Jiang, F. et al. Relationship between hearing loss and depression symptoms among older adults in China: The mediating role of social isolation and loneliness. Int. J. Geriatric Psychiatry 37, 6 (2022).
Petrovsky, D. V. et al. Social engagement, cognition, depression, and comorbidity in nursing home residents with sensory impairment. Res. Gerontol. Nurs. 12(5), 217 (2019).
Rong, H. et al. Association of sensory impairments with cognitive decline and depression among older adults in China. JAMA Netw. Open 3, 20141869 (2020).
Chou, K. Combined effect of vision and hearing impairment on depression in older adults: Evidence from the English Longitudinal Study of Ageing. J. Affect. Disord. 106(1–2), 191–196 (2008).
Zhang, Y. et al. Empirical research on male preference in China: A result of gender imbalance in the seventh population census. Int. J. Environ. Res. Public Health 19, 648211 (2022).
Hyde, J. S. Gender Similarities and Differences. In Annual Review of Psychology, S. T. Fiske, Editor. 373–398 (2014).
Utoomprurkporn, N. et al. Lack of association between audiogram and hearing disability measures in mild cognitive impairment and dementia: What audiogram does not tell you. Healthcare (Basel) 9, 6 (2021).
Acknowledgements
We would like to acknowledge the China Health and Retirement Longitudinal Study (CHARLS) team for providing data. We are grateful to all subjects who participated in the survey.
Funding
This study was funded by The Anhui Provincial University Science Research Project in 2022 (Grant No: 2022AH040212). The funding body had no roles in study design,data collection, and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Qiankun Liu was responsible for the design of the comprehensive study, data analysis, and manuscript composition; Jingwang, Zhongtao Zhou and Yang Xu collected the cohort data and responsibility for the integrity of the data; Jiaxue Pang, Li ma, Jiaoping Zhang and Pengyao Li revised the manuscript; Pengyao Li, Li Ma reviewed the manuscript;Hui Xie designed the study process. All authors read and approved the final manuscript and agreed to be responsible for all aspects of the work.
Corresponding author
Ethics declarations
Competing interest
The authors declare no competing interests.
Ethical approval
This study involves no data collected from human subjects. We only make use of the publicly available de-identified sample. This paper performed secondary data analysis on survey data which have obtained ethical approval before being fielded and are publicly available.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Q., Zhou, Z., Wang, J. et al. Gender differences in the relationship between hearing and visual impairments, dual sensory impairment, and depression in middle-aged and elderly populations. Sci Rep 15, 19442 (2025). https://doi.org/10.1038/s41598-025-04424-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04424-3