Abstract
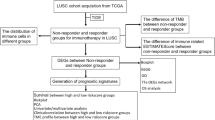
Lung squamous cell carcinoma (LUSC) is a common type of non-small-cell lung cancer with high mortality, lacks effective diagnostic indicators and therapeutic targets. This study aims to reveal that low expression of Alpha-Sarcoglycan (SGCA) promotes LUSC progression and to provide a biomarker for its diagnosis, prognosis evaluation, and targeted therapy. TCGA data and 70 clinical LUSC patients were analyzed. In vitro, H520 and H1703 cells with overexpressed SGCA were transfected with pc-SGCA plasmids, and their proliferation, apoptosis, and invasion were examined. In vivo, a subcutaneous tumorigenic mouse model was constructed. SGCA was significant in diagnosing LUSC and negatively correlated with T stage. Low SGCA expression enhanced proliferation, invasion, and migration, and inhibited apoptosis. Overexpression of SGCA inhibited tumor growth in mice. Low expression of SGCA is closely associated with LUSC progression, making it a potential prognostic factor and therapeutic target for LUSC.
Similar content being viewed by others
Introduction
Lung cancer shows the highest mortality rate and the second highest incidence globally among all tumor types1. According to its histopathological type, lung cancer can be divided into small-cell lung cancer and non-small-cell lung cancer (NSCLC). NSCLC accounts for approximately 85% of all lung cancer cases and is the main pathological type causing morbidity and mortality. To be specific, NSCLC can be further divided into lung adenocarcinoma (LUAD), lung squamous cell carcinoma (LUSC), large-cell lung cancer, and other subtypes2. Of them, LUSC takes up around 25–30% of NSCLC cases and is the second most common subtype after LUAD3. The epidermal growth factor receptor (EGFR) is the most common clinical target in NSCLC, which shows the mutation rates of 30% in NSCLC and 50% in LUAD; however, in LUSC, the EGFR mutation rate is only 10%4. Other common genetic mutations, such as those of vascular endothelial growth factor and anaplastic lymphoma kinase, are also rare in squamous cell carcinoma. So far, no specific biomarker has been identified for the diagnosis and prognosis evaluation of LUSC, compared with other pathological types, and most LUSC patients are diagnosed at an advanced stage, accompanied by multiple complications5. Further, these patients have limited treatment options, and most of them have unfavorable prognosis. Therefore, it is particularly important to identify potential biomarkers for LUSC diagnosis and molecular subtyping, as well as therapeutic targets for LUSC treatment.
In clinical practice, numerous LUSC patients exhibit sarcopenia in the course of their disease, and there is no available satisfactory explanation currently. Alpha-Sarcoglycan (SGCA), a member of the non-integrin family, not only forms part of the dystrophin-glycoprotein complex (DGC) that connects tissue cells with the extracellular matrix, but also has dual roles in signal transduction and structural integration6. The α-myoglycan protein, encoded by the SGCA gene, is usually engaged in protein-protein interactions through its independent transmembrane domain and cadherin-like domain7. Generally, SGCA, SGCB, SGCC, and SGCD co-encode the sarcoglycan complex, which forms a heterotetramer across the muscle membrane that connects the cytoskeleton and extracellular structure, thereby participating in the stabilization of the muscle membrane. Limb-girdle muscular dystrophy (LGMD) is the fourth most common inherited muscle disease, which has an incidence rate of about 1 in 20,000 individuals8. LGMD can be classified into LGMD type I and LGMD type II according to their genetic mode, with chromosome-recessive LGMD type II accounting for 90% of all cases9. The LGMD2D subtype of LGMD type II arises due to issues associated with the SGCA gene, which encodes the α-myoglycan protein. As one of the components of DGC, SGCA may be involved in the occurrence of sarcopenia. However, research on its role in oncology is still limited. And it remains to be further explored about whether SGCA expression is high or low in LUSC tissue, is the change of SGCA expression involved in the progression of LUSC, whether sarcopenia complicated with LUSC is related to SGCA, and is SGCA helpful for the diagnosis and prognosis of LUSC.
Based on the above scientific hypotheses, in this study, we investigated SGCA expression, its related biological functions and clinical significance with tumor tissue samples and clinical data of patients through performing bioinformatics analysis as well as experiments using cells cultured in vitro and xenograft models in vivo. The findings demonstrate that low expression of SGCA promotes LUSC progression, and SGCA may be a promising biomarker for the diagnosis and prognosis evaluation of LUSC.
Materials and methods
Bioinformation analysis based on the cancer genome atlas (TCGA) data
The RNA sequencing data and clinical characteristics of LUSC were sourced from TCGA database. Thereafter, the RNA matrix data were analyzed using R software 4.0.310. After excluding patients with incomplete clinical data, the data of 551 patients were included in this study.
The gene expression data, comprising 551 patients downloaded from TCGA website, were categorized into two groups, including normal tissue (n = 49) and tumor tissue (n = 504) groups, following standard data preprocessing and analysis protocols. Based on the thresholds of statistical significance, |log2 fold change|>2 and p < 0.05, the differentially expressed genes (DEGs) were screened from TCGA database.
Both the Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) databases were used as references. The KEGG images followed the reference guidelines: www.kegg.jp/kegg/kegg1.html11. The “cluster profiler” package in R was employed for enrichment analysis on DEGs selected from TCGA and GEO databases12. In addition, the Benjamini-Hochberg approach was utilized to correct for multiple factor differences, with a false discovery rate < 0.05 indicating statistical significance.
Clinical study
Tumor tissues of 70 inpatient surgical LUSC patients were collected from Taizhou People’s Hospital from March 2018 to March 2023. In the meantime, related clinical data of these patients including tumor staging, metastasis or not, blood biochemical index, tumor markers, and chest computed tomography (CT), were also extracted. Inclusion criteria: (1) patients with LUSC confirmed by pathological biopsy; (2) those aged between 18 and 75 years; (3) newly diagnosed patients not receiving any anticancer treatment; (4) those with Eastern Cooperative Oncology Group (ECOG) score of 0–2; and (5) patients or their legal representative, after fully understanding the study purpose, method, process, potential risks and benefits, voluntarily signed the informed consent to participate in the clinical study. Exclusion criteria: (1) patients with combined cardiovascular and cerebrovascular diseases, severe liver and kidney insufficiency, other malignant tumors or other serious diseases; (2) those with mental or cognitive impairment; (3) those with poor compliance; and (4) those receiving specific treatment or trial within the past 3 months. The SGCA expression in tissues was examined by immunohistochemistry, thereafter, the 70 LUSC cases were divided into high or low SGCA expression group according to the median SGCA expression, and the correlation of SGCA expression with patients’ clinical data was assessed. The study received approval from the Ethics Committee of Jiangsu Taizhou People’s Hospital, and was conducted in strict compliance with ethical standards and relevant principles outlined in the Declaration of Helsinki.
The cultured cell experiments in vitro
Cell culture and transfection
The LUSC cell line H520 and H1703 and the immortalized human bronchial epithelial mesothelial cell line BEAS-2B were sourced from the American Type Culture Collection (ATCC; Manassas, VA, USA), and cultivated in Dulbecco’s modified eagle medium (DMEM; Gibco, Thermo Fisher Scientific Inc., Waltham, MA, USA) and bronchial epithelial cell growth medium (Lonza, Walkersville, MD, USA), respectively, at 37 °C in the humidified atmosphere with 5% CO2, with 10% fetal bovine serum (FBS; Gibco) being used in both culture mediums.
The SGCA overexpression lentiviral plasmids were chemically synthesized by Shanghai GenePharma Co. Ltd. (Shanghai, China). After 293T cells were transfected with the appropriate lentiviral vector along with psPAX2 and pMD2.G (GenePharma Shanghai, China) and cultured at 37 °C for 48 h, the lentiviral particles were harvested. When cell density reached approximately 60–70% confluence, LUSC H520 and H1703 cells were transfected with the lentiviral particles by polybrene (MedchemExpress, New Jersey, USA). The next day, cells were intervened with puromycin for 48 h, so as to construct human LUSC cells with SGCA overexpression. Typically, these human LUSC transfected with pc-SGCA lentiviral plasmids were temporarily named the transfected H520 and H1703 cells.
Cell counting Kit-8 (CCK-8) and colony formation assays
The transfected cells were collected and resuspended in the complete culture medium at a concentration of 3 × 104 cells/ml and then inoculated to 96-well plates (100 µl/well ). At 24, 48 and 72 h later, the cells were probed with 10 µl CCK-8 solution (Beyotime) at 37 °C for 2 h. The optical density (OD) value was read at the 450-nm wavelength using a microplate reader (Bio-Rad, Hercules, CA, USA). In addition, the proliferation inhibition rate was calculated by OD value as follows: proliferation inhibition rate (%) = (1-OD value of experimental group / OD value of wild group)×100%.
To further investigate the proliferation inhibition, the transfected cells were spread evenly into the six-well plates at a density of 1,000 cells/well and then cultured to form colonies at 37 °C for 21 days. The colonies were later washed with phosphate-buffered saline (PBS), fixed with 100% methanol, stained with 0.05% crystal violet, and finally counted under a microscope (Nikon, Tokyo, Japan).
Transwell assays
To detect the cell migration capacity, 1 × 105 transfected cells were added to the upper compartments of the Transwell chambers (8-µm pores; Corning Costar, Cambridge, MA, USA) that contained 100 µl FBS-free medium. Then, the 20% FBS-supplemented culture medium was added into the lower chambers, and cells were incubated at 37 °C. After 36 and 72 h, the non-migrated cells were manually wiped away using cotton bud. Whereas the migrated cells were fixed with 100% methanol and stained with 0.05% crystal violet. Subsequently, an inverted light microscope was utilized to capture images and enumerate the migrated cells. To evaluate the cell invasion capacity, the upper surface of the membrane was pre-coated with Matrigel (BD Bioscience, San Jose, CA, USA), and the subsequent experimental procedures were identical to those outlined previously.
Flow cytometry analysis
The transfected cells were harvested using 0.25% EDTA-free trypsin, then washed with phosphate buffer saline (PBS) and centrifuged to discard the supernatant. To assess cell apoptosis, the Annexin V-FITC/PI Apoptosis Kit (KeyGEN, Nanjing, China) was employed. In brief, cells were resuspended in 500 µl binding buffer and then incubated with 5 µl annexin V-FITC and 5 µl propidium iodide for 30 min. After incubation at room temperature in dark, the percentage of apoptotic cells was quantified through flow cytometry (BD Bioscience), which involved the staining of cells with Annexin V-FITC and PI to differentiate among early apoptotic cells (Annexin V-FITC+/PI-), late apoptotic cells (Annexin V-FITC+/PI+), and necrotic cells (Annexin V-FITC-/PI+).
TUNEL assay
Terminal-deoxynucleotidyl transferase-mediated nick end labeling (TUNEL) assay was applied to further measure cell apoptosis. To be specific, the transfected cells were subcultured into 12-well plates for 24 h, subsequently fixed with 4% PFA for 15 min, and stained with TUNEL reagent (Beyotime) for 1 h at room temperature. Additionally, the nuclei were stained with 4’,6-diamidino-2-phenylindole (DAPI, Beyotime). At last, fluorescence signal was collected with a XSPY-3201LED fluorescent microscope (Shanghai CSOIF Co., LTD, Shanghai, China).
Western blotting analysis
Total protein of the transfected cells was extracted using radio-immunoprecipitation assay (RIPA) lysis buffer containing phenylmethanesulfonyl fluoride (Beyotime). After quantification with a Bicinchoninic Acid (BCA) Protein Assay Kit (Beyotime), protein aliquots were loaded and subjected to separation in 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), followed by transfer onto the polyvinylidene difluoride (PVDF) membranes. Subsequently, the membranes were immersed in 5% nonfat dry milk at room temperature for 2 h and incubated overnight at 4 °C with primary antibodies against SGCA (Cat. No. #54828; SAB, Maryland, USA), GAPDH (Cat. No. ab8245; Abcam, Cambridge, UK), MMP2 (Cat. No.40994; Cell Signaling, USA), MMP9 (Cat. No.13667; Cell Signaling, USA), Bax (Cat. No.5032; Cell Signaling, USA) and Bcl-2 (Cat. No.4423; Cell Signaling, USA). Next, the membranes were further incubated with the corresponding horseradish peroxidase (HRP)-conjugated secondary antibody (Cat. No. ab205719; Abcam) for 2 h at room temperature. Eventually, the Pierce™ ECL Western Blotting Substrate (Thermo Fisher Scientific Inc.) was adopted for target signal visualization.
Tumor xenograft experiments in vivo
The animal experimental protocols in this study were approved by the Huachuang Sino Animal Experiment Ethics Committee (SK23035-P001-01). All animal experiments complied with the ARRIVE guidelines and were carried out in accordance with the Guide for the Care and Use of Laboratory Animals released by the National Research Council.
Briefly, male BALB/c nude mice, aged 4–6 weeks, were acquired from Vital River Laboratory (Beijing, China) and maintained under specific pathogen-free conditions (25 °C, 50% humidity, 10-h/14-h light/dark cycle), with ad libitum access to food and water. Afterwards, a total of 1 × 106 stable transfected cells were resuspended in 100 µl PBS and subcutaneously injected into the flank of mice. One week later, the tumor sizes were recorded every 4 days and the tumor volumes were calculated by the following equation: volume = 0.5×length×width2. Tumor growth was monitored for 28 days, and then the growth curves were plotted. At 28 days post-cell injection, the mice were euthanized through CO2 inhalation in strict accordance with the animal ethics guidelines of our institute and animal welfare regulations. Subsequently, the tumors were excised. The tumor volume suppression rate was computed using the formula: tumor suppression rate = (mean volume of wild group - mean volume of experimental group) / mean volume of wild group×100%.
Also, the tumor samples were cut into 2-µm sections from at least 3 different planes and stained with hematoxylin and eosin (H&E). The histopathological features were observed under an optical microscope (Nikon, Tokyo, Japan).
Immunohistochemistry
For immunohistochemistry detection, paraffin-embedded sections were first dehydrated and stained with immunoperoxidase. Meanwhile, antigenic epitopes were exposed using 10 mM citrate buffer under microwaving. The sections were subsequently incubated with rabbit antibodies against SGCA (Cat. No. #54828; SAB, Maryland, USA, 1:100), Bcl-2 (Cat. No. #48496; SAB, Maryland, USA, 1:100), Bax (Cat. No. #48690; SAB, Maryland, USA, 1:100), MMP2 (Cat. No. #33144; SAB, Maryland, USA, 1:100), and MMP9 (Cat. No. #29042; SAB, Maryland, USA, 1:100). Thereafter, primary Ab staining was detected using the peroxidase-conjugated anti-rabbit IgG. The images were acquired under a Leica DM4000B fluorescence microscope equipped with a digital camera. For quantitative analysis, histoscore (H-score) was calculated based on the staining intensity and the percentage of stained cells, the grading of staining intensity (0–3) was later multiplied by the corresponding percentage of positive cells, and all the results were finally added to obtain the final H-score. Generally, the H-score ranges from 0 to 300, where 0 represents negative (-), 1-100 (+) stands for weakly positive, 101–200 (++) indicates moderately positive, and 201–300 (+++) is indicative of strongly positive. Tissue sections were examined and scored separately by two independent investigators blinded to the clinicopathological data of patients.
Statistical analysis
All data were obtained from three independent experiments and expressed as mean ± standard deviation. The significance of differences between two groups was analyzed using either paired or unpaired Student’s t-tests, as exemplified by the comparison of male and female heights. One-way analysis of variance (ANOVA) followed by Tukey’s test was employed to assess differences among multiple groups. Gene expression correlation was tested by Pearson’s correlation coefficient. A value of p < 0.05 was considered to indicate a statistically significant difference.
Results
Screening for SGCA genes associated with LUSC by bioinformatics analysis
The mRNA expression data of LUSC patients were obtained from the standardized mRNA analysis pipeline of the TCGA LUSC project. Utilizing the screening criteria of p < 0.05 and |log2 fold change| >2, our analysis of tumor and adjacent tissues in LUSC identified 3348 DEGs, with 2085 genes being up-regulated and 1263 being down-regulated in the tumor samples (Fig. 1A). This approach aligned with the methodologies used in similar studies, such as those detailed in the references, which also employed TCGA data and robust statistical methods to identify genes with prognostic significance and those involved in the molecular mechanisms of LUSC. Further analysis indicated that SGCA expression significantly decreased in tumor tissues compared with adjacent counterparts (p < 0.001; Fig. 1B). Receiver operating characteristic curve was plotted to verify the diagnostic significance of SGCA. According to our results, SGCA down-regulation had high diagnostic value for LUSC (area under the curve (AUC): 0.985; 95% confidence interval (CI) 0.975–0.994; Fig. 1C). Additionally, a survival curves were plotted to assess the prognostic significance of SGCA. The survival of the high SGCA expression group was significantly longer than low SGCA expression group, and SGCA was able to prolong LUSC survival (p = 0.003; Fig. 1D).
Screening for SGCA in the TCGA database and LUSC patient tissues. (A) 3348 DEGs in LUSC and normal group, and 2085 DEGs were upregulated and 1263 genes were downregulated in LUSC group; (B) Expression of SGCA in LUSC and normal group in TCGA; (C) ROC curve to assess the diagnostic significance of SGCA; (D) Survival curves were used to assess the prognostic significance of SGCA; (E) GO and KEGG enrichment analysis and select the top 12 pathways with high correlation with SGCA; (F) Enrichment plots from GSEA; (G) Expression of SGCA in LUSC and normal group in LUSC patient tissues; (H) Cross-sections of adjacent tissues were SGCA stained; (I) Cross-sections of low SGCA expression groups tumor tissues were SGCA stained; (J) Cross-sections of high SGCA expression groups tumor tissues were SGCA stained; (K) Cross-sections of low SGCA expression groups tumor tissues were H&E stained; (L) Cross-sections of high SGCA expression groups tumor tissues were H&E stained. GSEA, gene set enrichment analysis; TCGA, The Cancer Genome Atlas; DEGs, differentially expressed genes.
To further investigate the biological role of SGCA, GO and KEGG enrichment analyses were performed using the “clusterProfiler” package in R. Altogether 1272 pathways associated with DEGs identified from TCGA data were obtained, and the top 12 pathways that were most significantly correlated with SGCA expression were selected (Fig. 1E). These pathways were mainly related to cell migration, keratinization, and cell division. Subsequently, gene set enrichment analysis (GSEA) was conducted on the two groups, and it was found that the biological processes of cell migration and keratinization were significantly less enriched in LUSC tissues (Fig. 1F). These results suggest that low expression of SGCA promotes cell migration and keratinization in LUSC.
To further explore the prognostic significance of the SGCA gene in LUSC, clinical data from the TCGA LUSC project were utilized to categorize patients into high or low pc-SGCA expression group. The results indicated significant differences between the two groups in terms of gender (p = 0.006) and clinical stage (p = 0.025), as shown in Table 1.
Univariate Cox regression analysis demonstrated that the SGCA expression level (hazard ratio (HR) = 0.655, 95% CI 0.498–0.864, p = 0.003) was negatively correlated with T stage (p = 0.014) (T3 vs. T1, HR = 1.816, 95% CI 1.160–2.843, p = 0.009; T4 vs. T1; HR = 2.324, 95% CI 1.248–4.327, p = 0.008), M stage (p = 0.034) (M1 vs. M0, HR = 3.112, 95% CI 1.272–7.616, p = 0.013) and overall survival (p = 0.003).
Moreover, the significant factors obtained from univariate Cox regression analysis (p < 0.05) were incorporated in multivariate Cox regression analysis, revealing that SGCA was a protective factor for LUSC prognosis, with the HR of 0.655 (95% CI0.498–0.864, p = 0.003; see Table 2). Hence, the expression level of SGCA was correlated with clinical stage and played a significant role in predicting the prognosis of LUSC patients.
The association of low expression of SGCA with the poor prognosis of LUSC demonstrated by clinical data verification
To elucidate the impact of SGCA on the progression of LUSC, a comprehensive analysis was conducted using surgical samples and clinical data of 70 LUSC patients. By conducting immunohistochemistry, the expression levels of SGCA in tissues were examined, and it was discovered that SGCA expression significantly increased in tumor tissues compared with adjacent tissues (p < 0.001) (Fig. 1G).
To explore the clinical significance of SGCA, 70 patients were categorized into two groups based on their SGCA expression levels, as determined by the immunohistochemical H-Scores (Fig. 1H–J). Subsequently, the clinical test data between these two groups were compared. The results indicated a significant negative correlation between SGCA expression and both the T stage (p < 0.001) and the pathological stage (p = 0.020), as shown in Table 3, aligning with the clinical significance of TNM staging where T stage reflects the size and extent of the primary tumor. Such findings validated our bioinformatics analysis results mentioned above. CYFRA21-1, a soluble fragment of cytokeratin 19, has an implication for the clinical diagnosis of LUSC. SGCA expression was distinctly negatively correlated with CYFRA21-1 (p < 0.001), suggesting that SGCA could be a potential diagnostic biomarker for LUSC. The blood creatinine level is closely related to human body metabolism. SGCA expression was significantly negatively correlated with the creatinine level (p < 0.001). Based on such result, SGCA participated in organismal metabolism. SGCA was also positively correlated with the mean lesion CT value (p = 0.048), indicating that SGCA might be involved in the keratinization process. To further validate the relationship between SGCA and keratinization, H&E staining was conducted in both the high and low SGCA-expression groups to compare the differences in the keratinization degree (Fig. 1K–L). As suggested by our observations, the keratinization degree in the high SGCA-expression group was significantly higher than that in the low SGCA-expression group.
In clinical settings, many LUSC patients exhibit sarcopenia with disease progression. As a metabolite of skeletal muscle, creatinine has a suggestive effect on sarcopenia. To further explore the relationship between SGCA and clinical indicators like creatinine, Spearman correlation analysis was implemented (Table 4). The findings indicated a negative correlation between SGCA expression and clinical T stage (p < 0.001), CYFRA21-1 level (p < 0.001), and creatinine level (p < 0.001). These results confirm that low expression of SGCA promotes LUSC progression and may be associated with tumor cachexia hypermetabolism that causes muscle breakdown.
The effect of SGCA overexpression on reducing the malignancy of LUSC verified by cell experiments in vitro.
To further verify the above findings, cytological validation in vitro was performed. The findings showed that the protein expression levels of SGCA in human LUSC H520 and H1703 cells were significantly lower than those in normal human bronchial epithelial cells (BEAS-2B) (Fig. 2A). Therefore, H520 and H1703 cells were chosen for the biofunctional experiments of SGCA in LUSC. As shown in Fig. 2B, after transfection with pc-SGCA plasmids, SGCA expression in H520 and H1703 cells significantly increased. While SGCA overexpression inhibited cell proliferation at 72 h (H520: p = 0.004; H1703: p = 0.003) (Fig. 2C), weakened the cell colony formation capacity (H520: p < 0.001; H1703: p < 0.001) (Fig. 2D), and concurrently reduced the cell migration and invasion capacities (H520: p < 0.001; H1703: p < 0.001) (Fig. 2E–F). Consistently, at the molecular level, the expression levels of MMP2 and MMP9 were down-regulated in H520 and H1703 cells transfected with pc-SGCA plasmids (Fig. 2G), indicating that low expression of SGCA might promote LUSC metastasis.
SGCA overexpressing attenuates the behaviors of H520 and H1703 cells. (A) The expression of SGCA in BEAS-2B, H520 and H1703 cell; (B) The transfection efficiency of SGCA overexpressing in NSCLC; (C, D) SGCA overexpressing H520 and H1703 cell proliferation and colony formation; (E, F) The migratory and invasive properties of SGCA overexpressing H520 and H1703 cells were determined via Transwell experiments; (G) MMPs expression was measured in SGCA overexpressing-transfected H520 and H1703 cells; (H) BAX, Bcl-2 expression was measured in SGCA overexpressing-transfected H520 and H1703 cells; (I) The level of apoptosis of Wild cells, NC cells and SGCA overexpressing H520 and H1703 cells. Apoptotic cells were labelled with Tunel in green fluorescently labelled phalloidin. The nucleus was stained with DAPI in blue fluorescently labelled phalloidin; (J) Apoptosis of H520 and H1703 cells transfected with the SGCA overexpressing was examined (*p < 0.05; **p < 0.01;***p < 0.001).
To test whether SGCA was associated with LUSC apoptosis, the expression levels of apoptosis-related proteins Bax and Bcl-2 were detected in H520 and H1703 cells after SGCA overexpression. According to our observations, Bax was up-regulated whereas Bcl-2 was down-regulated (Fig. 2.H). Concurrently, TUNEL assay and flow cytometry (apoptosis rates: H520: 1.4 ± 0.2% vs. 11.7 ± 1.5% for Control group vs. pc-SGCA group, p < 0.001; H1703: 3.7 ± 0.4% vs. 7.9 ± 2.9% for Control group vs. pc-SGCA group, p = 0.004) also exhibited the apoptosis promotion effect of SGCA on H520 and H1703 cells (Fig. 2.I, J).
Overall, the results of our in vitro cell experiments demonstrated that SGCA overexpression reduced the malignancy of LUSC.
The effect of low expression of SGCA on promoting LUSC progression confirmed by tumor xenograft experiments in vivo
Finally, tumor xenograft experiments were performed to evaluate the impact of SGCA on tumor growth in vivo. On day 28 post-injection, mice were euthanized, and tumor xenografts were excised (Fig. 3A–B). Throughout the neoplastic process, alterations in mouse body weight (Fig. 3C) and tumor volume (Fig. 3D) were monitored. As discovered, there were no significant weight differences among the three groups, and tumors in the pc-SGCA group exhibited a markedly slower growth rate than those in the control group (inhibition rates: H520: 3.7 ± 1% vs. 68.3 ± 8.9% for Control group vs. pc-SGCA group, p < 0.001; H1703: 4.5 ± 1.3% vs. 73.2 ± 11.8% for Control group vs. pc-SGCA group, p < 0.001). These findings aligned with the in vitro experimental results indicating that overexpression of SGCA suppressed the proliferation of LUSC cells.
SGCA overexpressing represses tumor growth in vivo. (A) Images of 3 groups mice. Each group had five nude mice; (B) Images of the representative tumor xenografts; (C) Mice weight ware recorded and applied to plot a growth curve; (D) Tumor volume ware recorded and applied to plot a growth curve; (E) Immunohistochemistry analysis of Ki-67, BAX, Bcl-2, MMP2 and MMP9 levels in tumor xenografts. (***p < 0.001).
Tumor tissues of both groups were stained with H&E for histopathological analysis (Fig. 3E). It was confirmed that the tumor tissue structure was preserved in both groups. SGCA was associated with the apoptosis of LUSC cells, with more distinct nuclear lysis in pc-SGCA group than Control group.
To further verify the inhibitory effect of SGCA on tumor growth in vivo, immunohistochemical staining was performed on tumor tissues from both groups. The results indicated that Ki-67, Bcl-2, MMP2, and MMP9 protein levels were down-regulated in the SGCA overexpression group, whereas the Bax protein level was up-regulated (Fig. 3E). In summary, these in vivo findings demonstrated that the increased SGCA expression resulted in the suppression of tumor growth, migration, and invasion. In other words, low expression of SGCA promoted LUSC progression.
Discussion
The widespread application of chest CT imaging has enabled the early diagnosis and early treatment of LUSC, greatly improving the prognosis of patients13,14. However, despite the advances in early diagnosis, surgery, chemotherapy, radiotherapy, and immunotherapy for LUSC, more than 60% of patients are diagnosed with locally advanced (stage III or IV) or metastatic disease15,16 and thus have poor prognosis, usually accompanied by severe complications such as bleeding, airway obstruction, and mediastinal invasion. Therefore, it is crucial to identify novel predictive, diagnostic, and therapeutic targets for improving the prognosis of LUSC patients.
This study, utilizing bioinformatics and machine learning techniques, identified SGCA as a significant diagnostic and prognostic biomarker for LUSC based on the TCGA LUSC project. By using data of 70 clinical patients and performing functional experiments with cultured human LUSC H520 and H1703 cells overexpressing SGCA, as well as nude mouse tumor xenograft experiments, it was verified that low expression of SGCA increased tumor malignancy and promoted LUSC progression. Furthermore, SGCA might serve as a potential biomarker for the diagnosis and prognosis prediction of LUSC and as a therapeutic target for targeted therapy.
Tumor proliferation and migration constitute the primary cause of cancer-related mortality. During the process of tumor proliferation and migration, cells lose epithelial properties and acquire mesenchymal properties, thus activating anti-apoptotic pathways and endowing cancer cells with metastatic properties5,6. Our cell experiments revealed that low expression of SGCA enhanced the proliferative and migratory abilities of LUSC. In our analysis of TCGA database and clinical data, SGCA expression was associated with specific clinical outcomes, and negatively correlated with the clinical stage, T stage and M stage of LUSC patients. Therefore, low expression of SGCA may be involved in LUSC proliferation and migration, thus leading to the poor prognosis of patients. SGCA may inhibit the malignant progression of LUSC through multiple pathways. On one hand, SGCA enhances the binding affinity of tissue metalloproteinase inhibitors (TIMPs), directly suppressing the enzymatic activity of MMP2 and MMP9. This action hinders the degradation of the tumor extracellular matrix (ECM), such as type IV collagen and laminin, thereby inhibiting tumor cell invasion and metastasis. On the other hand, SGCA maintains the integrity of cell-ECM adhesion, forming a physical barrier that indirectly restricts MMP-mediated tumor cell migration. These mechanisms collectively establish SGCA as a potential therapeutic target for blocking LUSC progression, offering new insights into anti-metastatic strategies for lung squamous cell carcinoma.
CYFRA21-1 has been proven to be suitable for the diagnosis of LUSC and is currently a commonly used detection indicator in clinical practice. However, its specificity in diagnosing LUSC is low. DGC, which is attached onto the muscle fiber membrane and connects the intracellular skeleton and the extracellular matrix in muscle, plays an important role in maintaining the stability of the cell membrane and preventing muscle cell injury and necrosis. It consists of dystrophin and three subunit complexes, namely, the dystrophin proteoglycan complex, the sarcoglycan complex (SGC), and the syntrophin complex17. The α-sarcoglycan protein, encoded by SGCA gene in healthy people, is a key component of human SGC. The invasion and metastasis of many tumors may be related to the changes in SGC18. So far, SGCA is mostly investigated in the diagnosis and other related study of LGMD in our knowledge, but its role in LUSC is still poorly known, especially in the LUSC prognosis.
As a common concomitant symptom of cancer, sarcopenia is caused by the abnormal metabolic effects of tumors, abnormal systemic inflammation, and treatment-related gastrointestinal toxicity resulting in abnormal nutritional intake and multiple human abnormal regulatory functions19. It is independently associated with the mortality risk of cancer patients20,21. About 25-60% of individuals are complicated with sarcopenia when diagnosed with cancer, with a higher prevalence in lung cancer and head and neck cancer22,23. This study revealed an association between SGCA, as a critical component of DGC on the muscle fiber membrane, and the incidence of sarcopenia in LUSC patients. Our analysis of clinical patient data showed a strong correlation between SGCA expression level and creatinine level (p < 0.001); specifically, a decrease in SGCA expression was accompanied by an increase in blood creatinine level (Table 3). In humans, creatine is present in skeletal muscle, and the creatine amount per unit of skeletal muscle and the creatine catabolism rate of skeletal muscle are consistent24,25. Derived from the catabolism of creatine, creatinine, which is excreted by kidney, is a reliable marker for predicting muscle mass26. Several studies have reported that serum creatinine level is associated with the mortality of critical ill patients27,28; that is, in the case of normal renal function, the higher blood creatinine level predicts the greater muscle decomposition and the lower muscle mass. Through inference, it is concluded that low SGCA expression in LUSC patients may result in sarcopenia.
In the combined analysis of SGCA and DEGs based on TCGA database, we found that keratinization-related pathways were gradually activated as SGCA expression increased. Keratinization is a major histological feature of LUSC. When epithelial cells keratinize the keratin layer, a unique terminal differentiation and apoptotic cell death program will be initiated29. Keratinization is thus a process by which epithelial cells adapt to their environment to protect cell integrity from environmental influences, such as physical damage, infection, and exogenous substance30. In addition to their functions as epithelial cytoprotective factors, keratins have other important functions as regulators of cell functions including apical-basal polarization, cell size determination, protein translation, and organelle location regulatory31. In the field of medical imageology, CT value, as a quantitative index reflecting the absorption characteristics of tissues, is closely related to a variety of tissue biological characteristics, among which the degree of keratinization is a critical correlation factor. The increased keratinization is usually accompanied by the massive accumulation of proteins such as keratins and the compaction of cell structures. Keratin is rich in sulfur-containing amino acids, and has a relatively high attenuation ability for X-rays. Therefore, elevated CT values can be observed when tissue keratinization occurs. For example, in some skin lesions like keratotic skin disease or skin tumors with keratinized hyperplasia, CT scan shows significant changes in the CT value compared with that in the surrounding normal skin tissue. This provides an important imaging basis for the diagnosis and differential diagnosis of the disease. We further analyzed the mean lesion CT value of LUSC patients, which is expected to change after tissue keratinization, and found that it was correlated with the expression of SGCA (p = 0.048). Meanwhile, H&E staining of LUSC tissues indicated that tissues with high SGCA expression exhibited the elevated keratinization. Previous studies have demonstrated that the expression of migration-related protein MMP2 is up-regulated after suppressing the keratinization pathway-related genes in head and neck cancer32. As revealed by our cell experiments, the migratory and invasive capacities of LUSC cells were reduced upon up-regulation of SGCA expression, accompanied by a decrease in the protein levels of MMP2 and MMP9. Therefor, we speculate that in LUSC, SGCA acts as a protective factor for inhibiting tumor invasion and metastasis.
Conculusion
In summary, SGCA inhibits the proliferation, migration, and invasion of LUSC cells. SGCA, a gene with low expression in LUSC, may contribute to the progression of the disease. Its expression level can potentially serve as a novel biomarker for LUSC diagnosis and prognosis evaluation, and as a therapeutic target for personalized therapy.
Data availability
The data used to support the findings of this study are available from the corresponding authors upon request.
Abbreviations
- NSCLC:
-
Non-small-cell lung cancer
- LUSC:
-
Lung squamous cell carcinoma
- SGCA:
-
Alpha-sarcoglycan
- TCGA:
-
The cancer genome atlas
- LUAD:
-
Lung adenocarcinoma
- DGC:
-
Dystrophin-glycoprotein complex
- LGMD:
-
Limb-girdle muscular dystrophy
- GO:
-
Gene ontology
- KEGG:
-
Kyoto encyclopedia of genes and genomes
- CT:
-
Computed tomography
- DEGs:
-
Differentially expressed genes
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 70(1), 7–30. https://doi.org/10.3322/caac.21590 (2020).
Nicholson, A. G. et al. The 2021 WHO classification of lung tumors: impact of advances since 2015. J. Thorac. Oncol. 17(3), 362–387. https://doi.org/10.1016/j.jtho.2021.11.003 (2022).
Cheng, T. Y. et al. The international epidemiology of lung cancer: latest trends, disparities, and tumor characteristics. J. Thorac. Oncol. 11(10), 1653–1671. https://doi.org/10.1016/j.jtho.2016.05.021 (2016).
Wu, Y. L. et al. Intercalated combination of chemotherapy and erlotinib for patients with advanced stage non-small-cell lung cancer (FASTACT-2): A randomised, double-blind trial. Lancet Oncol. 14(8), 777–786. https://doi.org/10.1016/s1470-2045(13)70254-7 (2013).
Socinski, M. A. et al. Current and emergent therapy options for advanced squamous cell lung cancer. J. Thorac. Oncol. 13(2), 165–183. https://doi.org/10.1016/j.jtho.2017.11.111 (2018).
Vogel, H. & Zamecnik, J. Diagnostic immunohistology of muscle diseases. J. Neuropathol. Exp. Neurol. 64(3), 181–193. https://doi.org/10.1093/jnen/64.3.181 (2005).
Dickens, N. J., Beatson, S. & Ponting, C. P. Cadherin-like domains in alpha-dystroglycan, alpha/epsilon-sarcoglycan and yeast and bacterial proteins. Curr. Biol. 12(6), R197–199. https://doi.org/10.1016/s0960-9822(02)00748-0 (2002).
Wicklund, M. P. & Kissel, J. T. The limb-girdle muscular dystrophies. Neurol. Clin. 32(3), 729–749. https://doi.org/10.1016/j.ncl.2014.04.005 (2014).
Nigro, V. & Savarese, M. Genetic basis of limb-girdle muscular dystrophies: The 2014 update. Acta Myol. 33(1), 1–12 (2014).
Döhner, H. et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood 115(3), 453–474. https://doi.org/10.1182/blood-2009-07-235358 (2010).
Kanehisa, M., Sato, Y., Kawashima, M., Furumichi, M. & Tanabe, M. KEGG as a reference resource for gene and protein annotation. Nucleic Acids Res. 44(D1), D457–462. https://doi.org/10.1093/nar/gkv1070 (2016).
Rosin, M. P., Saad el Din Zaki, S., Ward, A. J. & Anwar, W. A. Involvement of inflammatory reactions and elevated cell proliferation in the development of bladder cancer in schistosomiasis patients. Mutat. Res. 305 (2), 283–292. https://doi.org/10.1016/0027-5107(94)90248-8 (1994).
Khodabakhshi, Z. et al. Non-small cell lung carcinoma histopathological subtype phenotyping using high-dimensional multinomial multiclass CT radiomics signature. Comput. Biol. Med. 136, 104752. https://doi.org/10.1016/j.compbiomed.2021.104752 (2021).
Fusco, R. et al. Quantitative imaging decision support (QIDS(TM)) tool consistency evaluation and radiomic analysis by means of 594 metrics in lung carcinoma on chest CT scan. Cancer Control 28 (1073274820985786.). https://doi.org/10.1177/1073274820985786 (2021).
Vansteenkiste, J. et al. 2nd ESMO Consensus Conference on Lung Cancer: early-stage non-small-cell lung cancer consensus on diagnosis, treatment and follow-up. Ann. Oncol. 25(8), 1462–1474. https://doi.org/10.1093/annonc/mdu089 (2014).
Osmani, L., Askin, F., Gabrielson, E. & Li, Q. K. Current WHO guidelines and the critical role of immunohistochemical markers in the subclassification of non-small cell lung carcinoma (NSCLC): moving from targeted therapy to immunotherapy. Semin Cancer Biol. 52(Pt 1), 103–109. https://doi.org/10.1016/j.semcancer.2017.11.019 (2018).
Carney, T. D., Hebalkar, R. Y., Edeleva, E., Çiçek, I. & Shcherbata, H. R. Signaling through the dystrophin glycoprotein complex affects the stress-dependent transcriptome in Drosophila. Dis. Model. Mech. 16(1). https://doi.org/10.1242/dmm.049862 (2023).
Arco, A. et al. Sarcoglycans in the normal and pathological breast tissue of humans: an immunohistochemical and molecular study. Cells Tissues Organs. 195(6), 550–562. https://doi.org/10.1159/000329508 (2012).
Baracos, V. E. Cancer-associated malnutrition. Eur. J. Clin. Nutr. 72(9), 1255–1259. https://doi.org/10.1038/s41430-018-0245-4 (2018).
Baracos, V. E., Reiman, T., Mourtzakis, M., Gioulbasanis, I. & Antoun, S. Body composition in patients with non-small cell lung cancer: A contemporary view of cancer cachexia with the use of computed tomography image analysis. Am. J. Clin. Nutr. 91(4), 1133s–. https://doi.org/10.3945/ajcn.2010.28608C (2010).
Prado, C. M. et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: A population-based study. Lancet Oncol. 9(7), 629–635. https://doi.org/10.1016/s1470-2045(08)70153-0 (2008).
Findlay, M., White, K., Brown, C. & Bauer, J. D. Nutritional status and skeletal muscle status in patients with head and neck cancer: impact on outcomes. J. Cachexia Sarcopenia Muscle 12(6), 2187–2198. https://doi.org/10.1002/jcsm.12829 (2021).
Kiss, N., Beraldo, J. & Everitt, S. Early skeletal muscle loss in Non-Small cell lung Cancer patients receiving chemoradiation and relationship to survival. Support Care Cancer. 27(7), 2657–2664. https://doi.org/10.1007/s00520-018-4563-9 (2019).
Heymsfield, S. B., Arteaga, C., McManus, C., Smith, J. & Moffitt, S. Measurement of muscle mass in humans: validity of the 24-hour urinary creatinine method. Am. J. Clin. Nutr. 37(3), 478–494. https://doi.org/10.1093/ajcn/37.3.478 (1983).
Kim, K. M. et al. Dissimilarity of femur aging in men and women from a nationwide survey in Korea (KNHANES IV). J. Bone Min. Metab. 31(2), 144–152. https://doi.org/10.1007/s00774-012-0386-9 (2013).
Stam, S. P. et al. Muscle mass determined from urinary creatinine excretion rate, and muscle performance in renal transplant recipients. J. Cachexia Sarcopenia Muscle 10(3), 621–629. https://doi.org/10.1002/jcsm.12399 (2019).
Thongprayoon, C., Cheungpasitporn, W. & Kashani, K. Serum creatinine level, a surrogate of muscle mass, predicts mortality in critically ill patients. J. Thorac. Dis. 8(5), E305–311. https://doi.org/10.21037/jtd.2016.03.62 (2016).
Udy, A. A., Scheinkestel, C., Pilcher, D. & Bailey, M. The association between low admission peak plasma creatinine concentration and in-hospital mortality in patients admitted to intensive care in Australia and New Zealand. Crit. Care Med. 44(1), 73–82. https://doi.org/10.1097/ccm.0000000000001348 (2016).
Eckhart, L., Lippens, S., Tschachler, E. & Declercq, W. Cell death by cornification. Biochim. Biophys. Acta 1833(12), 3471–3480. https://doi.org/10.1016/j.bbamcr.2013.06.010 (2013).
Deo, P. N. & Deshmukh, R. Pathophysiology of keratinization. J. Oral Maxillofac. Pathol. 22(1), 86–91. https://doi.org/10.4103/jomfp.JOMFP_195_16 (2018).
Karantza, V. Keratins in health and cancer: More than Mere epithelial cell markers. Oncogene 30(2), 127–138. https://doi.org/10.1038/onc.2010.456 (2011).
Liu, S. et al. 5-Hydroxymethylation highlights the heterogeneity in keratinization and cell junctions in head and neck cancers. Clin. Epigenetics 12(1), 175. https://doi.org/10.1186/s13148-020-00965-8 (2020).
Acknowledgements
We would like to thank Department of Pathology, Taizhou People’s Hospital for assistance in immunohistochemical staining.
Funding
This study was sponsored by The 333 Plan Foundation of Jiangsu, China (Su Talent Office [2022] 21 − 2)
Author information
Authors and Affiliations
Contributions
G.J.C.: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing—original draft, Writing—review & editing. G.Y.M.: Software, Validation, Formal analysis, Data curation, Writing—original draft, Writing—review & editing. X.Y.Z. & X.C.: Investigation, Data curation, Writing—review & editing. T.G.: Investigation, Writing—review & editing, Project administration. M.L.: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data curation, Writing—review & editing, Supervision, Project administration, Funding acquisition.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The clinical research section of this study was approved by Ethics Committee of Affiliated Taizhou People’s Hospital of Nanjing Medical University(KY 2023-162-01). All procedures performed in studies involving human participants were in accordance with 1964 Helsinki declaration and its later amendments or comparable ethical standards. The animal research section of this study was approved by the Huachuang Sino Animal Experiment Ethics Committee (SK23035-P001-01). All animal experiments complied with the ARRIVE guidelines and were carried out in accordance with the National Research Council’s Guide for the Care and Use of Laboratory Animals.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, G., Mao, G., Zong, X. et al. Low expression of SGCA promotes lung squamous cell carcinoma malignant progression. Sci Rep 15, 22578 (2025). https://doi.org/10.1038/s41598-025-05312-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-05312-6