Abstract
The development of effective and safe insulin analogs remains pivotal in advancing diabetes management. This study addresses the limitations of existing insulin therapies by introducing insulin lisargine, a novel long-acting insulin analog that resolves impurity formation associated with trypsin cleavage in glargine insulin. Insulin lisargine is characterized by glycine substitution at A21 and the addition of lysine and arginine at B31 and B32, respectively. High-performance liquid chromatography (HPLC) and mass spectrometry confirmed its high purity and precise molecular weight. X-ray crystallography at 2.0 Å resolution revealed structural features closely resembling human insulin, crucial for optimizing drug formulations and understanding receptor interactions.In vivo experiments demonstrated that insulin lisargine exhibits superior glucose-lowering effects compared to glargine insulin (Lantus). At a dosage of 1.5 IU/kg, lisargine achieved glucose-lowering effects equivalent to glargine in normal rats. However, at 5 IU/kg, it significantly outperformed glargine in type 1 diabetic rats. Long-term safety assessments revealed a comparable safety profile between lisargine and glargine, with no significant toxicity observed. These findings position insulin lisargine as a promising candidate for diabetes management, offering enhanced blood glucose control, improved production efficiency, and reliable safety. The study’s findings provide a foundation for the development of more effective insulin analogs, addressing critical needs in diabetes therapy.
Similar content being viewed by others
Introduction
Insulin lisargine, a novel insulin analogue utilized for the treatment of diabetes1incorporates specific structural modifications compared to human insulin. In the A chain, asparagine at position A21 is replaced with lysine, while in the B chain, lysine and arginine are introduced at positions B31 and B32, respectively. These structural alterations confer distinctive pharmacological properties and advantages to insulin lisargine. As a long-acting insulin analog, insulin lisargine is specifically designed to provide a prolonged therapeutic effect compared to traditional human insulin2. When injected subcutaneously, it forms “microcrystals,” enabling a slow and continuous release without pronounced peak concentrations, thereby extending its duration of action. This unique mechanism facilitates a gradual and consistent insulin delivery over an extended period, ensuring stable blood glucose regulation throughout the day. These features establish insulin lisargine as a promising long-acting insulin alternative, offering improved therapeutic options for patients with diabetes3.
Despite extensive research into the pharmacokinetics and pharmacodynamics of insulin lisargine, its crystal structure has yet to be fully elucidated. This study seeks to conduct a detailed analysis of insulin lisargine’s primary and higher-order structures through mass spectrometry, circular dichroism spectroscopy, and X-ray diffraction. Obtaining high-quality crystals of insulin lisargine and performing crystallographic analysis will enable precise characterization of its three-dimensional structure, providing insights into its molecular organization and atomic-level folding.
The findings from this research are integral to understanding insulin lisargine’s pharmacological properties, molecular interactions, and receptor-binding mechanisms. Furthermore, structural comparisons with other insulin analogs will support the optimization of drug design to improve stability, efficacy, and bioavailability. Experimental investigations have evaluated the effects of insulin lisargine on blood glucose levels using normal rat models. Additionally, single-dose and multiple-dose administration experiments conducted on a type 1 diabetes rat model have validated its clinical efficacy.
In conclusion, insulin lisargine, as an innovative insulin analog, demonstrates significant clinical potential. Comprehensive structural analyses and initial studies of its pharmacological effects provide a deeper understanding of its mechanisms of action, paving the way for the development of more effective and stable insulin analogs.
Materials and methods
Materials
Recombinant insulin lisargine injection (Lot No. M201605003) was supplied by Hefei Tianmai Biotechnology Development Co., Ltd. CSA standards were procured from Sigma Corporation, while protein crystallization reagent kits and additive screening kits were obtained from Hampton Corporation.
Purification and molecular weight determination of insulin lisargine
Liquid Chromatography-Mass Spectrometry (LC-MS): Liquid chromatography conditions: An ACQUITY UPLC Peptide BEH C18 column (100 mm × 2.1 mm, 1.7 μm) was utilized. Mobile phase A comprised 0.1% formic acid in water, and mobile phase B consisted of 0.1% formic acid in acetonitrile. Gradient elution was performed at a flow rate of 0.3 mL/min, with a column temperature of 50 °C and an injection volume of 1 µL. Mass spectrometry conditions: Positive ion detection mode was used with a capillary voltage of 1–2.5 kV, cone voltage of 35 V, cone gas flow of 50 L/h, collision voltage of 30–45 V, MCP detector voltage of 2300 V, source temperature of 80 °C, and a scan range of m/z 50–2000. Determination of Molecular Weight: A sample solution of 1 mg/mL was prepared by dissolving 10 mg of insulin lisargine in 10 mL of 10 mM hydrochloric acid. A 2 µL aliquot was injected into a high-resolution mass spectrometer, and the data were processed to calculate the molecular weight. Mass Spectrometry for Amino Acid Sequencing: To prepare a 2 mg/mL sample solution, 10 mg of insulin lisargine was dissolved in 5 mL of Tris-EDTA buffer (pH 8.0). An equal volume (100 µL) of 12 M urea solution was added, followed by 2 µL of 0.1 M DTT solution. The mixture was incubated at 37 °C for 30 min. Subsequently, 4 µL of 1 M iodoacetamide solution was added for alkylation in the dark for 30 min. The sample was diluted 30-fold with ultrapure water for testing. A blank control solution was prepared using 100 µL of Tris-EDTA buffer in place of the sample solution and subjected to the same procedure.
Secondary structure analysis of insulin lisargine by circular dichroism (CD) spectroscopy
Near-ultraviolet (UV) and far-UV scanning were performed using a Jasco J-815 CD spectrophotometer equipped with a helium-neon laser light source and a temperature-controlled sample chamber. Insulin lisargine solutions were prepared in phosphate-buffered saline (PBS) at a concentration of 2 mg/mL and filtered through a 0.22 μm membrane. The solutions were transferred into quartz cuvettes with a path length of 1 cm for analysis. CD spectra were recorded within the wavelength range of 190–260 nm, near-UV scans between 200 and 400 nm, and far-UV scans between 250 and 400 nm. The scanning speed was set to 50 nm/min, with data intervals of 0.2 nm.
Data analysis was performed using CDPro software, including baseline correction, peak fitting, and spectral decomposition to determine the secondary structure composition, such as α-helix, β-sheet, and random coil. The CDNN program was used for spectral deconvolution, while Pro-Data Viewer software was utilized for baseline subtraction and smoothing. The CD value ratio between the peak and valley of the standard sample was calculated, with an acceptable range of 2.08 ± 0.06. These steps ensured accurate interpretation of the secondary structure composition of insulin lisargine.
X-ray crystallography of insulin lisargine
Crystallization and crystal harvesting
Insulin lisargine (10 mg) was dissolved in 1 mL of 10 mM hydrochloric acid solution and refrigerated at 4 °C overnight to prepare a 10 mg/mL sample solution. The solution was centrifuged at 13,200 rpm for 10 min, and the supernatant was collected as the crystallization sample. Crystallization was performed using the vapor diffusion hanging drop method, employing Crystal Screen™ and Crystal Screen 2™ kits (Hampton Research) under 98 different conditions at 12 °C for 2–3 days. Crystals suitable for X-ray diffraction were grown in a solution containing 24% (v/v) 2-propanol, 0.2 M sodium citrate tribasic dihydrate, and 0.1 M HEPES sodium (pH 7.5) with a protein concentration of 4 mg/mL. Crystals were gently picked with a φ = 0.2 mm loop under a microscope, immersed in a cryoprotectant solution containing the crystallization mother liquor and 22.5% ethylene glycol, and stored in liquid nitrogen for further use.
Data collection and reduction
Diffraction data were collected at the Shanghai Synchrotron Radiation Facility (beamline 19U1) equipped with a 100 K low-temperature device. The detector-crystal distance was set to 400 mm, with an exposure time of 0.0977 s, Δφ = 1.0°, and a wavelength of 0.97774 Å. A total of 360 frames were collected at 100 K. The single-crystal diffraction data were processed using HKL2000 and XDS software. The crystals belonged to space group H3 (R3) with cell parameters: a = b = 78.991 Å, c = 40.431 Å, α = β = 90°, and γ = 120°.
Structure determination and refinement
The processed data were used for structure determination via molecular replacement using Phaser in the Phenix software suite. The PDB ID 1EV3 was used as the search model for automated rotation and translation operations, leading to successful structure determination4. Refinement was performed iteratively using Coot for model adjustment and phenix.refine at a resolution of 1.95 Å. The crystallographic data and refinement statistics are presented in Table 2. The atomic coordinates and structure factors have been deposited in the PDB under entry 8WU0.
Blood glucose level assessment in rat models
Experimental animals
Healthy male Sprague-Dawley rats (8–10 weeks old) and male NOD rats (12–14 weeks old) were used. Type 1 diabetes was induced in NOD rats via spontaneous onset following a 21-day diet containing 1% streptozotocin. The rats were housed under a 12-hour light/dark cycle with free access to standard rodent chow and water.
Drug administration
Insulin lisargine was administered intraperitoneally at doses of 2.5 IU/kg, 5 IU/kg, or 10 IU/kg. Control groups received equivalent volumes of solvent (physiological saline) or commercial insulin glargine as a positive control. Dosages were measured in International Units (IU) per kilogram of body weight.
Experimental design
For the single-dose administration experiment, rats were fasted overnight before receiving the drug. Blood samples were collected at 1, 2, 4, and 6 h post-administration from the tail vein for glucose level measurement. In the multiple-dose administration experiment, type 1 diabetic rats received daily intraperitoneal injections of insulin lisargine or solvent. Blood glucose levels were measured at multiple time points after each dose, including 2, 4, and 6 h post-injection.
Blood glucose level analysis
Blood glucose concentrations were measured using a glucometer. Each time point and treatment group were tested in triplicate, and mean values were calculated.
Ethical considerations
All experimental procedures adhered to ethical guidelines for the care and use of laboratory animals and were approved by the Institutional Animal Care and Use Committee of the University of Science and Technology of China (USTC).
Isoelectric point determination of insulin by electrophoresis
The isoelectric point (pI) of insulin was determined via polyacrylamide gel electrophoresis using pI markers for calibration. After separation, the gel was stained and destained, and an image was captured with a gel documentation system. Analysis of the gel image enabled calculation of insulin’s relative migration distance, allowing for accurate determination of its isoelectric point.
Toxicokinetic study of insulin injection in beagle dogs
Experimental animals
Fifty-four healthy Beagle dogs (Canis lupus familiaris), comprising equal numbers of males and females, aged 8 to 9 months, were procured from the Shanghai Xingang Experimental Animal Facility. At the time of acquisition, male dogs weighed between 8.30 and 10.30 kg, while female dogs weighed between 7.55 and 10.10 kg. The Beagle dog study’s animal strain, ownership, animal ethics, drug administration, and blood sampling procedures were all approved by the Institutional Animal Care and Use Committee (IACUC) of Tianjin Institute of Pharmaceutical Research New Drug Evaluation Co., Ltd. The facility operates under an experimental animal production license (SCXK 2012-0009), and the quality certificate number for the experimental animals is 311,619,100,000,078. After a period of acclimatization, 50 animals were selected for the pharmacokinetic study.
Experimental design
The 50 Beagle dogs were randomly assigned to five groups, each consisting of 10 animals (5 males and 5 females). The groups were designated to receive subcutaneous injections of recombinant human insulin injection solution at doses of 0.5, 1.0, and 1.5 IU/kg body weight; Lantus (insulin glargine) at a dose of 1.5 IU/kg body weight; and the solvent for recombinant human insulin injection solution (control group). The injections were administered once daily for 30 consecutive days.
Pharmacokinetic study
Dynamic blood samples were collected at baseline (day 1), mid-term (day 15), and endpoint (day 30) post-dose for pharmacokinetic analysis. Plasma insulin and C-peptide concentrations were quantified using radioimmunoassay (RIA). Pharmacokinetic parameters were calculated using a non-compartmental model fitted to plasma concentration-time data, with corrections for endogenous insulin levels based on C-peptide concentrations. The corrected exogenous insulin concentrations were determined by subtracting C-peptide concentrations at each time point from the total insulin concentrations measured via RIA.
Insulin receptor phosphorylation assay
Chinese Hamster Ovary (CHO) cells expressing both isoforms A and B of the insulin receptor were cultured in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin. Following serum starvation, the cells were treated with insulin at various concentrations (0.1 nM, 1 nM, 10 nM) for specific durations (5, 15, and 30 min). Phosphorylated insulin receptors were detected using a phospho-specific enzyme-linked immunosorbent assay (ELISA) kit. Cell lysates were incubated in microplate wells coated with anti-phosphotyrosine antibodies, followed by incubation with a horseradish peroxidase (HRP)-conjugated secondary antibody. Absorbance values were measured, and phosphorylation levels were quantified.
Insulin receptor binding assay
CHO cells expressing insulin receptor isoforms A and B were cultured and treated as described above. Cell lysates were prepared and incubated with [125I]-labeled insulin in the presence or absence of excess unlabeled insulin as a competitor. The reaction mixtures were subjected to gel filtration chromatography to separate bound and free [125I]-labeled insulin. Radioactivity in each fraction was measured, and competitive binding curves were constructed to determine the half-maximal inhibitory concentration (IC50) values of the unlabeled insulin.
IGF-1R binding assay
The H19-7/IGF-1R cell line was cultured and treated with [125I]-labeled insulin-like growth factor (IGF) as described. Cell lysates were immunoprecipitated using an anti-IGF-1R antibody, followed by incubation with [125I]-labeled IGF in the presence or absence of excess unlabeled IGF. Gel filtration chromatography was performed to separate bound and free [125I]-labeled IGF, and radioactivity in each fraction was measured. Competitive binding curves were analyzed to calculate the IC50 values for the unlabeled IGF.
Insulin glucose uptake assay
The glucose uptake assay was performed using differentiated 3T3-L1 adipocytes. Briefly, 3T3-L1 preadipocytes were cultured in DMEM supplemented with 10% newborn calf serum and 1% penicillin-streptomycin at 37 °C under 10% CO₂. Adipocyte differentiation was induced by treating confluent cells with induction medium (DMEM containing 10% FBS, 1 µM dexamethasone, 1 µg/mL insulin, and 5 mM IBMX) for 10 days, followed by maintenance medium (DMEM with 10% FBS and 1 µg/mL insulin) for an additional 2 days.
For the assay, differentiated adipocytes were trypsinized and seeded into 96-well plates (2 × 10⁴ cells/well). After overnight attachment, cells were serum-starved for 2 h in DMEM, then washed with KRPH buffer. Test compounds (e.g., insulin analogs) were serially diluted (3-fold, starting at 500 nM) in KRPH buffer and added to cells for 30 min. Subsequently, 0.25 µCi [³H]−2-deoxyglucose (50 µM) was added per well, and glucose uptake was measured after 20 min. The reaction was stopped by washing with ice-cold PBS containing 10 mM glucose. Cells were lysed with NaOH, and radioactivity was quantified using a scintillation counter. Data were normalized to the insulin (500 nM) positive control and KRPH buffer negative control.
Statistical analysis
Data are presented as mean ± standard error of the mean (SEM). Statistical significance among groups was evaluated using analysis of variance (ANOVA), followed by post hoc tests, with p < 0.05 considered statistically significant.
Results
Characterization of purity and molecular weight of insulin lisargine
This study presents the successful synthesis of a novel insulin variant, insulin lisargine. This variant is characterized by the substitution of Gly for Asn at position 21 in the A chain and the incorporation of Lys and Arg at positions 31 and 32 in the B chain, respectively. Comprehensive characterization confirmed the purity, molecular weight, and mass spectrometric properties of the synthesized insulin lisargine. High-Performance Liquid Chromatography (HPLC) was employed to assess its purity. Figure 1A illustrates a distinct, singular peak indicative of high purity, thereby validating the successful synthesis of the modified insulin.
Characterization of purity, molecular weight and secondary structure of insulin lysargine. (A). Liquid Chromatography-Mass Spectrometry (LC-MS) validated the molecular weight of insulin lisargine. (B). TOF-MS spectrum confirming the charge-to-mass ratio of insulin. CD spectrum spectrum of insulin lisargine insulin lisargine in the far-uv region (C) and near-uv region (D).
The accurate determination of molecular weight is essential for precise protein sequencing and constitutes a critical step in the structural analysis of insulin lisargine. High-resolution Time-of-Flight Mass Spectrometry (TOF-MS) was utilized to determine the charge-to-mass ratio of insulin lisargine. The results presented in Fig. 1B indicate that the observed average molecular weight [M + H] + is 6036.2 m/z, which closely corresponds to the theoretical molecular weight of 6034.97. This alignment provides strong evidence for the accuracy and reliability of the synthesized insulin lisargine.
Insulin lisargine contains three disulfide bonds, which can influence peptide fragmentation in tandem mass spectrometry, potentially resulting in insufficient ion fragments for sequence analysis. To enhance fragmentation efficiency, the disulfide bonds were reduced using dithiothreitol (DTT) prior to sequence determination. The reduction cleaved the inter-chain disulfide bonds, thereby separating insulin into its A and B chains. The reduced cysteine residues were subsequently alkylated before individual sequence analysis.
The A chain of insulin lisargine consists of 21 amino acids and 20 amide bonds. High-resolution mass spectrometry identified numerous b and y ions, enabling complete sequence coverage. The determined sequence, GIVEQCCTSICSLYQLENYCG, matches the theoretical sequence. The B chain comprises 32 amino acids and 31 amide bonds. Abundant fragment ions were observed, and all 31 amide bonds were cleaved, resulting in complete sequence coverage. The determined sequence, FVNQHLCGSHLVEALTLVCGERGFFYTPKTKR, aligns precisely with the theoretical sequence.
Determination of insulin secondary structure via circular dichroism spectroscopy
Circular dichroism (CD) spectroscopy in the far-ultraviolet region was utilized to investigate the configuration of protein peptide bonds. Analysis using CDNN software facilitated the prediction and quantification of the relative content of protein secondary structures, including α-helix, β-fold (antiparallel and parallel), β-turn, and random coil. The CD spectra in the near-ultraviolet region provided insights into the orientation of chromophores in protein side chains, such as tryptophan and phenylalanine residues. Notably, disulfide bonds exhibited characteristic circular dichroism signals in the near-ultraviolet region (250–340 nm), serving as spectral probes to assess asymmetric microenvironment disturbances without interfering with peptide bond signals in the far-ultraviolet region.
Figure 1 illustrates the circular dichroism spectra of insulin lisargine in both the far-ultraviolet (Fig. 1C) and near-ultraviolet (Fig. 1D) regions. The secondary structure content, predicted using CDNN software, was calculated based on fitted data across various wavelengths, as detailed in Table 1. The results indicated that the α-helix predominates, constituting approximately 40% of the total structure across all wavelengths. Random coil structures represented about 27%, while β-fold and β-turn structures were comparable, each accounting for approximately 15% Table 2.
This investigation also analyzed the isoelectric point (pI) of insulin through electrophoresis, aiming to experimentally determine the pH at which insulin molecules exhibit no net electrical charge, a critical factor influencing their biochemical behavior. Electrophoretic analysis was conducted using Gel Doc™ XR + software for data interpretation, yielding a calculated pI value of 6.8, which closely aligns with the theoretical expectation (Fig. 2A).
Crystallization and X-ray diffraction. (A). Determination of the Isoelectric Point (pI) of Insulin by Electrophoresis Analysis.M: Marker. Lanes 1–4: Insulin samples at a concentration of 1 mg/ml, including human insulin, insulin lisargine, insulin glargine, and insulin aspart, respectively.Lanes 5–8: Insulin samples at a concentration of 0.3 mg/ml, including human insulin, insulin lisargine, insulin glargine, and insulin aspart, respectively. (B). Protein Crystal of Insulin Lisargine.A crystal with dimensions of 0.10 × 0.10 × 0.15 mm3. (C). X-ray Diffraction Pattern of Insulin Lisargine. (D). Crystal Structure of Insulin Lisargine. The dimer of lisargine, labeled with chain IDs within an asymmetric unit, is displayed in cyan. Two chloride ions (large green spheres) and two zinc ions (small silver-black spheres) are also represented. (E). Disulfide Bonds within Insulin Lisargine. (F). Structural Alignment Between Insulin Lisargine and Human Insulin. The structural alignment of insulin lisargine (TV-blue) and human insulin (TV-yellow) is illustrated. (G). Structural Comparison Between the AB Monomer (teal) and the CD Monomer (lime green).
X-ray crystallography
Crystallization and X-ray diffraction
Preliminary screening of crystallization conditions identified a 2-propanol-based solution as conducive to insulin crystallization. Additive screening kits were employed within this system to optimize crystal morphology and enhance diffraction quality. The addition of thiocyanate was found to produce larger crystals, as demonstrated in Fig. 2B. As seen in Fig. 2C, the X-ray Diffraction Pattern of Insulin Lisargine is presented.
Overall structure and disulfide bond formation
The overall crystal structure of insulin lisargine is depicted in Fig. 2D. Each asymmetric unit within the crystallographic data comprises an insulin dimer containing two A chains and two B chains, along with 30 water molecules (refer to Table 1; water molecules not shown in the figure). The A chains are designated as A and C, and the B chains as B and D. The A chain features two α-helices connected by a loop, while the B chain includes an extended α-helix region (residues B2–B19) followed by a loop-sheet-loop configuration, representative of a typical insulin hormone fold.
Each monomer incorporates a zinc ion and a chloride ion, with both ions occupying partial sites, similar to the 2-zinc insulin hexamer described by Jarosinski et al.4. The zinc ion coordinates with the side chain of residue B10H (or D10H), along with a chloride ion (not illustrated). Consistent with most insulin crystal structures, significant disorder was observed at the C-terminal region of the B chains, with models including only up to residue B30, excluding residues B31–B32. The dimer model revealed the same disulfide bond configuration as natural insulin, with each monomer comprising three disulfide bonds: A6–A11, A7–B7, A20–B19, C6–C11, C7–D7, and C20–D19. Figure 2E presents the electron density map for the disulfide bonds, all of which exhibit a bond length of 2.03 Å, consistent with standard values.
Structural comparison and alignment
Superposition of the AB and CD monomers revealed nearly identical conformations, except for the N- and C-terminal regions. The root-mean-square deviation (r.m.s.d.) was calculated to be 0.424 Å for 45 superimposable Cα atoms (Fig. 2G), indicating structural flexibility at both termini. To further analyze the structure of insulin lisargine, alignment was performed with the publicly available insulin model (PDB entry: 1EV3), which shares the same crystallographic space group. This alignment, shown in Fig. 2F, demonstrates a high degree of similarity between the two structures, with a superposed r.m.s.d. of 0.503 Å for all 98 superimposable Cα atoms.
The alignment indicates a conserved spatial arrangement between insulin lisargine and human insulin. Based on the conformation of the N-terminus of Chain B, the crystal structure of insulin lisargine, like 1EV3, can be classified as an R-state hexamer characterized by the extended α-helix spanning residues B2–B191. The observed structural divergences may be attributed to the unique modifications in insulin lisargine, potentially influencing its biological activity and metabolic properties. These findings provide valuable insights for further exploration of the functional and biological implications of insulin lisargine.
Enhanced glucose control by insulin lisargine compared to glargine insulin in a rat model
This study evaluated the glucose-lowering efficacy of insulin lisargine, formulated as an injectable solution, using a rodent model. Blood glucose levels were rigorously assessed over a 10-hour period. The results, depicted in Fig. 3, demonstrated that insulin lisargine exerted a more pronounced glucose-lowering effect than the control. The control group established baseline glucose stability, serving as a reference for evaluating the impact of the novel insulin variant.
At a dose of 1.5 IU/kg, insulin lisargine exhibited glucose-lowering effects comparable to those of commercially available Glargine insulin, with no statistically significant differences observed. However, at an increased dose of 4.5 IU/kg, insulin lisargine displayed significantly enhanced glucose-lowering efficacy, showing a statistically significant difference compared to the Glargine group. These findings underscore the superior glucose-lowering potential of insulin lisargine, particularly at higher doses, and provide robust evidence of its efficacy as a hypoglycemic agent. The results highlight the importance of this study and emphasize the necessity for further clinical investigations.
Insulin lisargine effectively reduces blood glucose levels in a rat model of type 1 diabetes
Validation experiments for Insulin Lisargine were conducted using a rat model of type 1 diabetes, incorporating both single-dose and multiple-dose administration protocols. In the single-dose study, Insulin Lisargine significantly reduced blood glucose levels at various doses. Compared to the solvent control group, Insulin Lisargine-treated groups demonstrated statistically significant reductions in blood glucose levels at 1, 2, 4, and 6 h post-administration, with the most pronounced effect observed at the 4-hour time point. Notably, even the lowest dose of Insulin Lisargine produced significant reductions in blood glucose levels at 1 and 2 h post-administration (Fig. 4A).
In the multiple-dose study, Insulin Lisargine consistently reduced blood glucose levels across successive administrations. Compared to the solvent control group, the Insulin Lisargine-treated groups exhibited significant reductions in blood glucose levels at 2, 4, and 6 h post-administration (Fig. 4B). This indicates that the glucose-lowering effects of Insulin Lisargine were sustained and amplified with repeated administration. At doses of 2.5 IU/kg and 5 IU/kg, Insulin Lisargine demonstrated substantial glucose-lowering effects at 2 and 4 h post-administration, with the most pronounced effect occurring at 4 h in the 5 IU/kg group. At a dose of 10 IU/kg, significant reductions were observed at 2, 4, 6, and 8 h, with the peak effect noted at 6 h.
Additionally, the formulated Insulin Lisargine exhibited glucose-lowering effects comparable to the clinical drug Aspart Insulin at an equivalent dose of 5 IU/kg, with no statistically significant differences observed in both single-dose and multiple-dose studies. These findings underscore the potent glucose-lowering effects of Insulin Lisargine in a rat model of type 1 diabetes, highlighting its potential for clinical application.
Evaluation of the long-term safety of insulin lisargine in large animal Beagles
To assess the potential long-term toxicity of Insulin Lisargine in large animals, a one-month toxicokinetic study was conducted using beagle dogs. Insulin Lisargine was administered at doses of 0.5, 1, and 1.5 IU/kg, with Lantus (insulin glargine) (1.5 IU/kg) serving as the control. Plasma concentrations of Insulin Lisargine and Lantus (insulin glargine) were monitored at multiple time points over the study period. Sampling was conducted within the first 24 h post-administration, at 0 and 3 h on day 15, and within the final 24 h on day 30.
The results showed no significant differences in plasma insulin concentrations between Insulin Lisargine and Lantus (insulin glargine) across all doses (Fig. 5). Peak plasma concentrations of Insulin Lisargine were observed at 2 h post-administration, while Lantus (insulin glargine) peaked at 3 h. Plasma insulin concentrations in all groups returned to baseline levels within 6–8 h. These findings demonstrate that Insulin Lisargine has a comparable safety profile to the clinically established long-acting insulin Lantus, with no evidence of long-term toxicity in beagle dogs. In this study, the key pharmacokinetic (PK) parameters for recombinant Insulin Lisargine were comprehensively characterized in our animal model. These parameters, including AUC (Area Under the Curve), Tmax (Time to Maximum Concentration), and Cmax (Maximum Concentration), are detailed in Table 3. The data presented provide a robust characterization of the in vivo pharmacokinetic profile of recombinant Insulin Lisargine, facilitating an in-depth understanding of its absorption and exposure characteristics.
Long-term Toxicity and Pharmacokinetic Study of Recombinant Insulin Lisargine in Beagle Dogs. The pharmacokinetic profiles of recombinant insulin lisargine injection (Test) and Lantus (insulin glargine) following single and multiple subcutaneous injections at different doses are illustrated. The study spans one month and includes long-term toxicity and pharmacokinetic analysis in Beagle dogs. Mean drug concentration-time curves are expressed as mean ± standard deviation (n = 10).
In vitro safety assessment of insulin lisargine
An in vitro study was conducted to evaluate the safety and efficacy of Insulin Lisargine. Doses of 0.5, 1, and 1.5 IU/kg of Insulin Lisargine were compared with Lantus (insulin glargine) (1.5 IU/kg) as a control. The phosphorylation of insulin receptor isoforms A (IR-A) and B (IR-B) upon Insulin Lisargine exposure was analyzed. Figure 6A and B illustrate the phosphorylation patterns of IR-A and IR-B, respectively, indicating receptor activation. Quantitative analysis revealed no significant differences in phosphorylation levels between Insulin Lisargine and Lantus, suggesting similar receptor activation profiles.
In Vitro Analysis of Insulin Lisargine Detection. (A) Curve illustrating the phosphorylation of insulin receptor isoform A (IR-A) upon treatment with insulin lisargine. (B) Curve depicting the phosphorylation of insulin receptor isoform B (IR-B) following exposure to insulin lisargine. (C) Experimental results demonstrating the binding affinity of insulin lisargine to IR-A. (D) Experimental outcomes illustrating the binding affinity of insulin lisargine to IR-B. (E) Results of the insulin-like growth factor 1 receptor (−1R) binding experiment. (F) Analysis of insulin-mediated glucose uptake in the in vitro experiment.
Figure 6C and D demonstrate the binding affinity of Insulin Lisargine to IR-A and IR-B. Quantitative analysis confirmed comparable binding affinities between Insulin Lisargine and Lantus, supporting equivalent receptor interactions. Additionally, Fig. 6E presents the results of the insulin-like growth factor 1 receptor (IGF-1R) binding study. Both qualitative and quantitative analyses revealed no significant differences in binding affinity or IC50 values between Insulin Lisargine and Lantus (insulin glargine), indicating similar interactions with IGF-1R.
Furthermore, glucose uptake experiments, as shown in Fig. 6F, demonstrated comparable glucose uptake rates between Insulin Lisargine and Lantus (insulin glargine) treatment groups. Quantitative analysis indicated no significant differences in glucose uptake kinetics, confirming equivalent effects on cellular glucose metabolism. Collectively, these findings provide strong evidence that Insulin Lisargine exhibits safety and efficacy comparable to Lantus, supporting its potential as a therapeutic agent.
Discussion
Lisargine, an innovative insulin analogue, is engineered for extended therapeutic action. This study reports the development of a recombinant Lisargine variant through genetic engineering. The molecular structure of Lisargine is defined by the substitution of Asn with Gly at position 21 of the A chain and the addition of Lys and Arg at positions 31 and 32 of the B chain. These modifications prevent Asn deamidation at the A chain’s C-terminus, thereby inhibiting covalent dimer formation under acidic conditions. Additionally, the introduced amino acids in the B chain alter its isoelectric point, promoting microcrystal formation upon subcutaneous injection and extending its therapeutic effect.
The primary objectives of this study were to compare Insulin Lisargine with commercial Glargine insulin and to evaluate the biological equivalence and potential enhanced efficacy of purified Insulin Lisargine. The results demonstrate that Insulin Lisargine possesses glucose-lowering effects comparable to, or exceeding, those of Glargine.
The development of insulin analogues is crucial for improving diabetes management by enabling efficient blood glucose regulation and therapeutic convenience, ultimately enhancing patient quality of life5. It also broadens the range of treatment options, offering insulin analogues tailored to individual needs, including rapid-acting, intermediate-acting, and long-acting formulations. These advancements facilitate personalized diabetes management. Moreover, the development of insulin analogues drives technological progress in the pharmaceutical industry. Techniques such as genetic engineering, protein engineering, and crystallography underpin insulin analogue development, yielding insights applicable to broader pharmaceutical research2.
Our study revealed that the dimeric model comprises six disulfide bond pairs: A6-A11, A7-B7, A20-B19, C6-C11, C7-D7, and C20-D19. Specifically, insulin lisargine, a variant of human insulin, contains three disulfide bonds. These bonds are essential for linking segments of the insulin molecule, stabilizing its structure, and preserving its biological activity. In insulin lisargine, the disulfide bonds connect Cys7 to Cys19 and Cys46 to Cys30 of the A chain, as well as Cys20 of the A chain to Cys6 of the B chain. The presence of these disulfide bonds is critical for maintaining the insulin molecule’s structural integrity and functional efficacy. Disulfide bonds significantly contribute to insulin structure by stabilizing its three-dimensional conformation, facilitating folding, and influencing both stability and half-life. The six pairs of disulfide bonds in insulin lisargine are particularly important for its extended half-life and the maintenance of its biological activity.
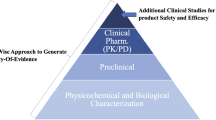
Insulin lisargine, a novel long-acting insulin analog, is evaluated for pharmacological efficacy and quality based on pertinent criteria. Protein-based drugs are produced via genetic engineering, which involves synthesizing active substances in organisms, followed by complex processes such as refolding, enzymatic cleavage, and purification. Composed predominantly of proteins, peptides, or peptide derivatives, these drugs exhibit a broad range of therapeutic functions6. Unlike traditional chemical drugs, protein-based drugs possess intricate two-dimensional and three-dimensional structures. The complexity of their production and structural intricacies poses significant challenges for quality research and control, necessitating advanced analytical methods to effectively characterize their physicochemical properties7.
Proteins exhibit higher-order structures that encompass secondary, tertiary, and quaternary levels, with secondary structures comprising α-helices, β-sheets, β-turns, and random coils. The higher-order structure of a protein profoundly affects its therapeutic efficacy, functionality, bioavailability, and safety8. Consequently, analyzing and controlling higher-order structures are essential for the development of protein-based biosimilars.
When evaluating the dissociation conclusions of the insulin analogue in solution, it is essential to acknowledge the limitations of relying solely on static crystallographic structures. The study emphasizes the structural aspects of the insulin analogue; however, despite efforts to deduce dissociation information, the inherent constraints of crystallographic methodologies are highlighted. Conclusions regarding solution dissociation must therefore be interpreted with caution. To address these limitations, future research could employ alternative methods, such as molecular dynamics simulations or fluorescamine assays, to gain deeper insights into the behavior of the insulin analogue in solution.
Our research aims to design an insulin, referred to as Lisargine insulin, which demonstrates significant advantages over traditional Glargine insulin. Firstly, experimental results indicate that Lisargine insulin, while maintaining comparable safety levels, exhibits a more pronounced long-lasting hypoglycemic effect. Secondly, structural optimizations have substantially enhanced the yield and safety of Lisargine insulin.
The structure of Glargine insulin differs slightly from that of human insulin, primarily due to modifications in its B and A chains. Glargine insulin incorporates two arginine residues at the C-terminus of its B chain and substitutes glycine for asparagine at position 21 of the A chain. These modifications render Glargine insulin nearly insoluble at physiological pH, leading to the formation of micro-precipitates upon injection, which gradually dissolve to provide consistent blood glucose control for up to 24 h. However, these structural alterations introduce certain challenges, particularly the susceptibility of the two arginine residues at the B-chain C-terminus to cleavage by pancreatic proteases. This cleavage generates numerous impurities, thereby reducing yield and compromising safety9.
To address these drawbacks, the design of Lisargine insulin involved replacing one arginine residue at the B-chain C-terminus with lysine. This modification aims to reduce the sensitivity of cleavage sites to pancreatic proteases, thereby decreasing impurity formation and enhancing yield and safety. This technique significantly enhances the stability and purity of Lisargine insulin, ensuring its safety and efficacy in practical applications10.
In our crystal structure determination of Insulin Lisargine, despite achieving high-resolution for the overall structure, it is notable that the B31 and B32 residues at the C-terminus of the B-chain exhibited relatively low electron density, precluding clear atomic resolution11. This suggests that these residues adopt a highly flexible or disordered conformation within this specific crystal environment. This flexibility likely stems from their terminal position on the B-chain and potentially weak interactions with neighboring molecules in the crystal packing, thereby preventing them from adopting a fixed conformation. Given the potential roles of B31 and B32 in proinsulin processing and insulin hexamer formation in native insulin, further studies are warranted to investigate the conformational dynamics of these residues in solution or upon interaction with receptors/binding proteins. Optimizing crystal growth conditions, or integrating other structural biology techniques such as solution Nuclear Magnetic Resonance (NMR) or Cryo-electron Microscopy (Cryo-EM), will facilitate a more comprehensive understanding of the structural flexibility of these critical residues and their potential implications for insulin function and pharmacological properties.
The aggregation behavior of insulin profoundly impacts its biological activity, pharmacokinetics, and potential immunogenicity risk. Insulin molecules tend to form oligomeric species such as dimers and hexamers, and under certain conditions, can further form irreversible aggregates. Such aggregation may not only reduce drug bioavailability but also potentially induce the formation of anti-drug antibodies, leading to immunogenic responses that compromise therapeutic efficacy12.
In the present study, we conducted a preliminary assessment of Insulin Lisargine’s anti-aggregation stability under routine conditions. Our Nuclear Magnetic Resonance (NMR) spectra (as shown in Figure S1) demonstrate a high degree of consistency in its predominant solution-state conformation compared to standard human insulin, indirectly supporting its structural integrity and a lower propensity for aggregation. Furthermore, our in vivo immunogenicity studies in animals have also demonstrated a favorable safety profile.
However, we recognize that in clinical applications, insulin may encounter various stress conditions (e.g., temperature fluctuations, shear forces, long-term storage) which could accelerate aggregation. While our current preliminary data are encouraging, future research is warranted to comprehensively evaluate the aggregation behavior of Insulin Lisargine under diverse stress conditions using techniques such as Dynamic Light Scattering (DLS), Analytical Ultracentrifugation (AUC), or Size Exclusion Chromatography (SEC) to fully assess its physical stability.
Based on the high sequence homology of Insulin Lisargine with human insulin and the observed low aggregation propensity, we preliminarily assess its immunogenicity risk to be low. To fully validate its safety and efficacy in humans, we are currently conducting a Phase I clinical trial (Registration No.: CTR202311261; Clinical Application Acceptance No.: CXSL1700069; Study Protocol No.: HJG-CZLJYDS-HFTMSW). This study is designed to provide a more comprehensive assessment of safety, including immunogenicity, as well as pharmacokinetic and pharmacodynamic data, aiming to establish a solid foundation for the clinical application of Insulin Lisargine.
Conclusions
In summary, our study comprehensively demonstrates the significant characteristics of Insulin Lisargine in terms of structural optimization, preliminary safety profile, and pharmacokinetic advantages through multi-level analyses involving crystallography and insulin safety evaluations. These improvements not only lay the groundwork for the production efficiency of Insulin Lisargine but also provide valuable insights and references for the development of other insulin analogs. Through these optimized designs, Insulin Lisargine exhibits potentially superior characteristics compared to traditional Glargine insulin, with promising prospects for future widespread clinical applications, and its safety, tolerability, and preliminary pharmacokinetic and pharmacodynamic properties are currently undergoing further evaluation.
Data availability
Data availabilityThe data presented in this study are available on request from the corresponding author. The data are not publicly available due to a partner wanting to continue the research.DeclarationsThis study was conducted and reported in accordance with the ARRIVE guidelines (Animal Research: Reporting of In Vivo Experiments, Version 2.0). All experiments involving Beagle dogs (Canis lupus familiaris) were performed under standard laboratory conditions as outlined in the Methods section.
References
Ciszak, E. et al. ‘Role of C-Terminal B-Chain Residues in Insulin Assembly: The Structure of Hexameric LysB28ProB29-Human Insulin’. Structure (London, England: 1993) 3 (6): 615–22. (1995).
Lu, J. et al. Pharmacodynamics and pharmacokinetics of a new type of Recombinant insulin lisargine injection. BMC Complement. Med. Ther. 20 (1), 334 (2020).
Huang, B. et al. Protein Structure Prediction: Challenges, Advances, and the Shift of Research Paradigms (Genomics, Proteomics & Bioinformatics, 2023).
Jarosinski, M. A., Dhayalan, B., Chen, Y. S., Chatterjee, D. & Varas Nicolás and Michael A. Weiss. ‘Structural Principles of Insulin Formulation and Analog Design: A Century of Innovation’. Molecular Metabolism 52 (October): 101325. (2021).
Hua, Q. Insulin: A small protein with a long journey. Protein Cell. 1 (6), 537–551 (2010).
Terwilliger, T. C. et al. Iterative model building, structure refinement and density modification with the PHENIX autobuild Wizard. Acta Crystallogr. D. 64 (Pt 1), 61–69 (2008).
Retnakaran, R. & Bernard Zinman The ongoing evolution of basal insulin therapy over 100 years and its promise for the future. Diabetes Obes. Metabolism. 24 (S1), 17–26 (2022).
Varanko, A., Saha, S. & Chilkoti, A. ‘Recent Trends in Protein and Peptide-Based Biomaterials for Advanced Drug Delivery’. Advanced Drug Delivery Reviews, Advanced Drug Delivery 2020 - Part 1: Carriers for Advanced Drug Delivery, 156 (January): 133–87. (2020).
Caballero-Pérez, A. José María Viader-Salvadó, Ana Lucía Herrera-Estala, José Antonio Fuentes-Garibay, and Martha Guerrero-Olazarán. Buried Kex2 sites in glargine precursor aggregates prevent its intracellular processing in Pichia pastoris Muts strains and the effect of Methanol-Feeding strategy and induction temperature on glargine precursor production parameters. Applied Biochem. Biotechnology 193 (9), 2806–2829 (2021).
Hazra, P. et al. A novel peptide design aids in the expression and its simplified process of manufacturing of insulin glargine in Pichia pastoris. Appl. Microbiol. Biotechnol. 105 (8), 3061–3074 (2021).
Mikiewicz, D. et al. Soluble insulin analogs combining rapid- and long-acting hypoglycemic properties – from an efficient E. coli expression system to a pharmaceutical formulation. PLOS ONE. 12, e0172600 (2017).
Chrudinová, M. et al. A versatile insulin analog with high potency for both insulin and insulin-like growth factor 1 receptors: structural implications for receptor binding. J. Biol. Chem. 293, 16818–16829 (2018).
Acknowledgements
This work was supported by financial contributions from the YRD Collaborative Fundamental Research Project (2024CSJZN0800), National Natural Science Foundation of China (12375352), Anhui Provincial Natural Science Foundation (2308085MC76).
Author information
Authors and Affiliations
Contributions
P.W and Z.M.Z wrote the main manuscript text and Z.Z, H.W, L.W. and Z.W prepared Figs. 1, 2, 3, 4, 5 and 6. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Reporting statement
We confirm that this study was reported in accordance with the ARRIVE guidelines (https://arriveguidelines.org).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhu, Z., Zheng, Z., Wang, H. et al. X-ray crystallography reveals insulin lisargine structure and mechanisms of glucose regulation. Sci Rep 15, 32846 (2025). https://doi.org/10.1038/s41598-025-07243-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07243-8