Abstract
The aim of this retrospective study was to analyze the efficacy and safety of lateral abdominal wall suspension during surgery compared with traditional procedures in patients with pelvic organ prolapse without uterine preservation. Collect the data of patients with uterine and vaginal wall prolapse who underwent surgery from January 2022 to December 2023. All patients were divided into three groups according to different surgical procedures: Study Group (laparoscopic total hysterectomy + bilateral salpingectomy/oophorectomy + lateral abdominal wall suspension + posterior colporrhaphy), Control Group 1 (laparoscopic-assisted vaginal total hysterectomy + bilateral salpingectomy/bilateral oophorectomy + anterior and posterior colporrhaphy), and Control Group 2 (vaginal total hysterectomy + anterior and posterior colporrhaphy).Statistically analyze the clinical indicators and recurrence situations in different Groups. Patients in Study group exhibited significantly higher preoperative POP-Q staging for pelvic organ prolapse severity(P < 0.01), longer operative times(P = 0.01, P < 0.01), but significantly reduced intraoperative blood loss(P = 0.01, P < 0.01)and shorter postoperative urinary catheterization duration(P = 0.01, P < 0.01) compared to the other two groups. No differences were detected in postoperative infection, vaginal bleeding or duration of hospitalization(P > 0.05). However, stress incontinence in 1-year after operation has no difference between study group and control groups. Recurrence rates in Control Group 1 is higher than Study Group (P = 0.02), While, it has no difference between Study Group and Control Group 2. Lateral abdominal wall suspension, despite a longer operative duration, surpasses traditional surgeries in minimizing intraoperative blood loss, cutting down the time of postoperative urinary catheter retention, and lowering the postoperative recurrence rate. To firmly establish the long-term curative effects and safety of lateral abdominal wall suspension, future research with larger sample sizes and longer follow-up periods is essential.
Similar content being viewed by others
Introduction
Pelvic floor dysfunction (PFD) is a common disease among middle-aged and elderly women. The lifetime risk of undergoing surgery for pelvic floor diseases is 11% to 20%. With the aggravation of the aging population, pelvic floor dysfunctional diseases have increasingly attracted people’s attention1,2. The main manifestations of pelvic floor dysfunction are the prolapse of the uterus and vaginal wall and in severe cases it may lead to dysfunctions in urination and defecation, pelvic pain, and sexual dysfunction3,4,5. Its main pathogenesis is the relaxation of the pelvic floor muscles and the decrease in muscle tension, making it unable to support the pelvic organs. Based on the structural changes, it further causes functional disorders6.Currently, there are various treatment methods for pelvic floor dysfunction, including pelvic floor function training, physical therapy, surgical treatment, and so on. Among them, surgical treatment is the most effective approach for uterine and vaginal wall prolapse7,8,9. However, with the advancement of medical technology, there are an increasing number of surgical approaches. Nevertheless, postoperative recurrence remains a rather thorny problem10.
In the past, the typical surgical methods for pelvic floor disorders were transvaginal hysterectomy along with anterior and posterior colporrhaphy. Nevertheless, with the progress in medical technology, laparoscopic-assisted surgeries have notably simplified the operation process11,12.Presently, to decrease the likelihood of postoperative recurrence, various types of meshes have gradually found their way into clinical practice, opening up new avenues for surgical treatment13.The widely used polypropylene mesh has also brought about a number of adverse reactions14.At present, the use of new-generation polypropylene mesh in the surgical treatment of uterine prolapse is becoming more and more common. It is mainly used in lateral abdominal wall suspension surgeries, whether the uterus is preserved or not15. However, there is still a lack of sufficient clinical data to support whether it has advantages over traditional uterine prolapse surgeries that do not preserve the uterus in terms of surgical outcome, postoperative recovery, and postoperative recurrence. This research intends to compare the pros and cons of laparoscopic total hysterectomy + bilateral salpingectomy/oophorectomy + lateral abdominal wall suspension + posterior colporrhaphy with traditional surgeries (laparoscopic-assisted vaginal hysterectomy + bilateral salpingectomy/oophorectomy + posterior colporrhaphy or vaginal hysterectomy + anterior and posterior colporrhaphy) for patients with uterine and vaginal wall prolapse, so as to offer a reference for clinical treatment.
Methods
Participants
We retrospectively reviewed the 112 patients who underwent surgeries without preserving the uterus due to uterine and vaginal wall prolapse in the Department of Gynecology of the second hospital of Tianjin Medical University from January 2022 to December 2023. According to different surgical methods, they were divided into the Study group: laparoscopic total hysterectomy + bilateral salpingectomy/bilateral oophorectomy + lateral abdominal wall suspension + posterior colporrhaphy; Control Group 1: laparoscopic-assisted vaginal total hysterectomy + bilateral salpingectomy/bilateral oophorectomy + anterior and posterior colporrhaphy; Control Group 2: vaginal total hysterectomy + anterior and posterior colporrhaphy. All patients had no history of pelvic surgery and other chronic diseases. A total of 33 patients were included in the Study group, 49 patients in Control Group 1, and 30 patients in Control Group 2. This study followed relevant ethical guidelines and regulations.
Surgical methods
Study group surgical procedure
The repair mesh used in the surgery is Titanized mesh implants, which is composed of a single-strand polypropylene and a titanium compound layer. A thin layer of fibrous tissue will grow into the mesh, and its cells will grow through the mesh pores, allowing the mesh to be enveloped by human tissues. Meanwhile, the mesh can maintain its softness and a certain degree of mobility. It has been confirmed that it has better histocompatibility16.
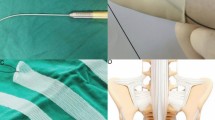
Patients were placed in the lithotomy position. After achieving satisfactory general anesthesia, laparoscopic total hysterectomy with bilateral salpingectomy/oophorectomy was performed using standard techniques. Excised tissues were extracted transvaginally, and vaginal vault closure was completed. The bladder apex was sutured to the anterior abdominal wall for suspension. A bowel retractor was used to elevate the vaginal vault, followed by meticulous dissection of the anterior and posterior vaginal walls. A pre-shaped T4 mesh was trimmed externally and inserted into the peritoneal cavity, then secured to the vaginal walls and vault using non-absorbable sutures. A 5 mm skin incision was made 4 cm superior and 3 cm lateral to each anterior superior iliac spine. A laparoscopic needle driver penetrated the subcutaneous tissue without breaching the peritoneum, passed obliquely beneath the round ligament, and exited the abdominal wall. The mesh was clamped and exteriorized (Fig. 1). After suspension, the anterior vaginal wall was elevated sufficiently without additional repair, and posterior colporrhaphy was thereafter performed.
Schematic diagram of lateral abdominal wall suspension (Photos taken during the operation). (a) The shape of the mesh after trimming. (b) After fully dissecting the bladder from the anterior vaginal wall, the mesh is laid flat on the anterior vaginal wall, folded back to the posterior vaginal wall after covering the vaginal stump. (c) The bilateral sides of the mesh are pulled through the extraperitoneal pathway of the lateral abdominal wall to the subcutaneous tissue 3 cm superior and 4 cm lateral to the anterior superior iliac spine, and sutured and embedded in the peritoneum with absorbable sutures.
Control group 1 procedure
Laparoscopic total hysterectomy with bilateral salpingectomy/oophorectomy and anterior/posterior colporrhaphy were performed. Patient positioning and anesthesia protocols mirrored those of the Study group. Following uterine and adnexal resection, anterior/posterior colporrhaphy was conducted according to preoperative evaluations.
Control group 2 procedure
Vaginal hysterectomy with optional bilateral salpingectomy/oophorectomy and anterior/posterior colporrhaphy were performed. Same surgical and anesthesia protocols as the Study group were used.
Statistical indicators
Patient age, pelvic organ prolapse (POP-Q) staging, stress incontinence, the duration of the operation, the amount of blood loss during the operation, the length of time the urinary catheter was kept after the operation (in hours), the incidence of urinary tract infections after the operation, the number of days spent in the hospital and complications ≥ Clavien-Dindo Grade 3 were statistically analyzed across all groups. Complications ≥ Clavien-Dindo Grade 3 incluse severe complications such as ureteral injury, bladder injury, and intestinal injury, which require further surgical intervention. In addition, the follow-up data of the patients 1 year after the operation were reviewed to evaluate the recurrence situation and the treatment results.In the evaluation of postoperative stress urinary incontinence (SUI), all patients were considered to have SUI regardless of their postoperative severity grade. During postoperative follow-up, the vaginal wall was assessed using the Pelvic Organ Prolapse Quantification (POP-Q) system, and vaginal wall prolapse with a degree of ≥ Stage 1 was defined as recurrence.
Statistical analysis
Data analysis was performed using SPSS 27 software. For continuous variables that conformed to a normal distribution, such as age and the number of hospital stay days, an independent samples t-test was employed to compare the differences between the two groups. For ordinal variables, including the staging of uterine prolapse, anterior vaginal wall prolapse, and posterior vaginal wall prolapse, the Mann–Whitney U test was utilized. In cases of comparisons involving small sample sizes and low expected frequencies, Fisher’s exact test was applied. A P value less than 0.05 was considered to indicate a statistically significant difference.
Results
Comparison of basic characteristics of patients
There was no significant difference in age between the patients in the Study group and those in Control Group 1 (P > 0.05). However, there were significant differences in the severity of pelvic organ prolapse. The conditions of uterine prolapse, anterior vaginal wall prolapse, and posterior vaginal wall prolapse in the Study group were all more severe than those in Control Group 1 (P < 0.01). The specific data are shown in Table 1. There was no significant difference in the occurrence of SUI between the two groups(P > 0.05).
There was no significant difference in age between the patients in the Study group and those in Control Group 2 (P > 0.05). However, significant differences existed in the severity of pelvic organ prolapse. The degrees of uterine prolapse, anterior vaginal wall prolapse, and posterior vaginal wall prolapse in the Study group were all more severe than those in Control Group 2 (P < 0.01). The specific data are presented in Table 2. There was no significant difference in the occurrence of SUI between the two groups (P > 0.05).
Comparison of surgical related indicators among patients
The patients in the Study group had a shorter hospital stay (P = < 0.01), a shorter duration of postoperative urinary catheterization (P = 0.01), and less intraoperative blood loss (P = 0.01) compared with those in Control Group 1. However, the operation time of the Study group was longer (P = 0.01). There were no significant differences in the incidence of postoperative urinary tract infections and vaginal bleeding between the two groups (P > 0.05). No complications of Clavien-Dindo Grade ≥ 3 happen in two groups. The data was shown in Table.3.
There was no significant difference in the number of hospital stay days between the patients in the Study group and those in Control Group 2 (P > 0.05). The intraoperative blood loss and the number of days with the urinary catheter in place for the patients in the Study group were superior to those in Control Group 2 (P < 0.01), while the operation time of the Study group was significantly longer than that of Control Group 2 (P < 0.01). There were no significant differences in the incidence of postoperative urinary tract infections, postoperative vaginal bleeding between the two groups (P > 0.05). Meanwhile, no surgical complications of Clavien-Dindo Grade 3 or higher occurred in two groups. The specific data are shown in Table 4.
Recurrence in different groups 1 year after operation
There was no marked difference in the occurrence of stress incontinence among patients in each group 1 year after the operation. Nevertheless, in the first control group, 5 patients developed anterior vaginal wall prolapse 1 year after the operation, with a higher incidence than that in the study group(P < 0.05). Moreover, there was no significant difference in the occurrence of vaginal wall prolapse between the control group 2 and the study group. The specific data are shown in Table 5.
Discussion
In the surgical treatment of patients with uterine and vaginal wall prolapse, the primary objectives are to alleviate symptoms, restore anatomical structure, and preserve organ function. The selection of surgical approach plays a critical role in patient outcomes and long-term prognosis17,18.Pelvic floor dysfunction surgeries are associated with high recurrence rates, but mesh repair has been shown to significantly delay recurrence compared to traditional procedures19,20.With advancements in biomaterial technology, novel composite materials such as titanium-reinforced polypropylene mesh have been introduced into clinical practice. These materials demonstrate improved histocompatibility, stable physical properties, and reduced inflammatory responses, thereby minimizing surgical complications21,22.
This study retrospectively analyzed clinical data of patients with non-uterus-sparing uterine and vaginal wall prolapse, comparing outcomes between different groups: those undergoing lateral abdominal wall suspension with mesh implantation versus traditional surgical approaches (laparoscopically assisted vaginal hysterectomy with bilateral salpingectomy/ oophorectomy + posterior colporrhaphy, or vaginal hysterectomy + anterior/posterior colporrhaphy). Demographic analysis revealed no significant differences in age among the Study group, Control group 1, and Control group 2, confirming balanced baseline characteristics. Notably, patients undergoing lateral abdominal wall suspension had more severe uterine and vaginal wall prolapse, as this procedure was preferentially selected for cases with higher prolapse grades. Despite this selection bias, subsequent analyses demonstrated superior outcomes in multiple domains for patients treated with lateral abdominal wall suspension compared to traditional surgical methods.
In the subsequent analysis, we further evaluated intergroup differences in surgical parameters. The lateral abdominal wall suspension group demonstrated significantly longer operative time compared to both laparoscopic-assisted vaginal hysterectomy and vaginal hysterectomy groups. This discrepancy can be attributed to the technically demanding nature of the procedure, which requires meticulous dissection of anterior/posterior vaginal walls, laparoscopic mesh suture fixation, and complete extraperitoneal mesh embedding to prevent exposure23,24. Despite the extended operative duration, no significant increase in intraoperative blood loss was observed in the lateral abdominal wall suspension group; conversely, a statistically significant reduction in blood loss was documented. Potential mechanisms include improved visualization afforded by pelvic floor muscle relaxation reducing operative complexity, and minimized anterior vaginal wall manipulation directly decreasing vascular trauma—though this hypothesis remains unreported in current literature. Notably, lateral abdominal wall suspension achieved significant vaginal apex elevation without requiring additional anterior colporrhaphy, thereby reducing urethral injury risk and shortening catheterization duration, which was corroborated by our data analysis. Postoperative care for prolonged catheterization cases included daily perineal cleansing and topical levofloxacin application to urethral orifices, effectively mitigating urinary tract infection risks. Although mesh fixation involving multiple suture points theoretically could reduce vaginal bleeding, no postoperative vaginal hemorrhage occurred in the Study group, whereas 6 cases of minor vaginal bleeding were observed in Control group 1 (without statistical significance due to limited sample size).In clinical practice, urethral suspension is commonly performed to improve symptoms in patients with pelvic floor dysfunction primarily characterized by stress urinary incontinence (SUI). In contrast, the patients included in this study who underwent lateral abdominal wall suspension predominantly presented with pelvic organ prolapse (POP), with a low preoperative incidence of concomitant SUI (only 5/33, 15.15%). Although lateral abdominal wall suspension may transiently increase the risk of SUI in the short term, no cases of SUI were observed at 10 days postoperatively. Additionally, over a 1-year follow-up period, no SUI developed as tissue repair and urination function recovered. These results may be partially attributed to the small sample size.
Procedural selection prioritized recurrence prevention. One-year follow-up demonstrated 0% recurrence in the lateral abdominal wall suspension group, compared to 5 cases of mild posterior vaginal wall prolapse in Control group 1, underscoring the recurrence prevention advantage of this technique25. While no statistically significant difference existed between the Study group and Control group 2, 2 recurrences observed in Control group 2 suggest potential differences may emerge with extended follow-up.
Conclusion
This study compared the outcomes of different surgical approaches for uterine prolapse and found that patients undergoing concurrent lateral abdominal wall suspension during laparoscopic surgery had significantly longer operative times but demonstrated significantly shorter catheterization duration and reduced intraoperative blood loss. No statistically significant differences were observed between groups in postoperative complications such as vaginal hemorrhage, urinary tract infections or other serious complications(Clavien-Dindo Grade ≥ 3). However, patients receiving lateral abdominal wall suspension showed a significant reduction in postoperative recurrence rates.Different surgical approaches have distinct characteristics. Clinicians should consider individual patient factors including the type of pelvic organ prolapse, primary symptoms, severity of prolapse, age, and general health status for comprehensive consideration to select the most appropriate procedure, aiming to optimize surgical outcomes and patient quality of life. Future studies with larger sample sizes and longer follow-up periods are warranted to further validate the long-term efficacy and safety profiles of these surgical techniques.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Enklaar, R. A. et al. Manchester procedure vs sacrospinous hysteropexy for treatment of uterine descent: A randomized clinical trial. JAMA 330(7), 626–635. https://doi.org/10.1001/jama.2023.13140 (2023).
Peinado-Molina, R. A., Hernández-Martínez, A., Martínez-Vázquez, S., Rodríguez-Almagro, J. & Martínez-Galiano, J. M. Pelvic floor dysfunction: Prevalence and associated factors. BMC Public Health 23(1), 2005. https://doi.org/10.1186/s12889-023-16901-3 (2023).
Ghaderi, F., Bastani, P., Hajebrahimi, S., Jafarabadi, M. A. & Berghmans, B. Pelvic floor rehabilitation in the treatment of women with dyspareunia: A randomized controlled clinical trial. Int Urogynecol J 30(11), 1849–1855. https://doi.org/10.1007/s00192-019-04019-3 (2019).
Mezes, C. M. et al. Effect of vaginal prolapse repair and midurethral sling on urgency incontinence symptoms. Urogynecology (Phila) 31(3), 250–257. https://doi.org/10.1097/SPV.0000000000001620 (2025).
Borello-France, D. et al. Adherence to perioperative behavioral therapy with pelvic floor muscle training in women receiving vaginal reconstructive surgery for pelvic organ prolapse. Phys. Ther. 103(9), pzad059. https://doi.org/10.1093/ptj/pzad059 (2023).
Chmielewska, D. et al. Electromyographic characteristics of pelvic floor muscles in women with stress urinary incontinence following sEMG-assisted biofeedback training and Pilates exercises. PLoS ONE 14(12), e0225647. https://doi.org/10.1371/journal.pone.0225647 (2019).
Zhu, H. et al. Effect of pelvic floor workout on pelvic floor muscle function recovery of postpartum women: Protocol for a randomized controlled trial. Int. J. Environ. Res. Public Health 19(17), 11073. https://doi.org/10.3390/ijerph191711073 (2022).
Artymuk, N. V. & Khapacheva, S. Y. Device-assisted pelvic floor muscle postpartum exercise programme for the management of pelvic floor dysfunction after delivery. J. Matern. Fetal Neonatal. Med. 35(3), 481–485. https://doi.org/10.1080/14767058.2020.1723541 (2022).
Liu, J. et al. Systematic review and meta-analysis of therapeutic effects of pelvic restoration combined with anti-stress urinary incontinence surgery on pelvic floor dysfunction. Ann. Palliat. Med. 10(11), 11678–11687. https://doi.org/10.21037/apm-21-2737 (2021).
Zhang, P., Du, W., Guo, G., Yuan, M. & Wei, J. Influencing factors of recurrence after pelvic organ prolapse surgery and construction of a nomogram risk prediction model. Rev. Assoc. Med. Bras. 70(12), e20240849. https://doi.org/10.1590/1806-9282.20240849 (2024).
Baekelandt, J. F. et al. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery versus laparoscopy as a day-care procedure: A randomised controlled trial. BJOG Int. J. Obstet. Gynaecol. 126(1), 105–113. https://doi.org/10.1111/1471-0528.15504 (2019).
Wattiez, A., Mashiach, R. & Donoso, M. Laparoscopic repair of vaginal vault prolapse. Curr. Opin. Obstet. Gynecol. 15(4), 315–319. https://doi.org/10.1097/01.gco.0000084246.09900.06 (2003).
de Tayrac, R.; Cosson, M.; Panel, L.; Compan, C.; Zemmache, M. Z.et al. Urinary and sexual impact of pelvic reconstructive surgery for genital prolapse by surgical route. A randomized controlled trial. Int. Urogynecol. J. 33(7), 2021–2030. https://doi.org/10.1007/s00192-021-05071-8 (2022).
Seifalian, A., Basma, Z., Digesu, A. & Khullar, V. Polypropylene pelvic mesh: What went wrong and what will be of the future?. Biomedicines 11(3), 741. https://doi.org/10.3390/biomedicines11030741 (2023).
Dubuisson, J. B. et al. Laparoscopic repair of pelvic organ prolapse by lateral suspension with mesh: A continuous series of 218 patients. Gynecol. Obstet. Fertil. 39(3), 127–131. https://doi.org/10.1016/j.gyobfe.2010.12.007 (2011).
Ai, F. F., Mao, M., Zhang, Y., Kang, J. & Zhu, L. The in vivo biocompatibility of titanized polypropylene lightweight mesh is superior to that of conventional polypropylene mesh. Neurourol. Urodyn. 39(1), 96–107. https://doi.org/10.1002/nau.24159 (2020).
Hemming, C. et al. Surgical interventions for uterine prolapse and for vault prolapse: The two VUE RCTs. Health Technol. Assess 24(13), 1–220. https://doi.org/10.3310/hta24130 (2020).
Bulutlar, E. et al. Innovative minimally invasive technique for pelvic organ prolapse: V-Notes lateral suspension. J. Obstet. Gynaecol. Res. 51(2), e16232. https://doi.org/10.1111/jog.16232 (2025).
Deng, H. et al. A randomized single blind comparison of conventional bowel preparation and unplanned preoperative preparation for pelvic organ prolapse. Zhonghua Fu Chan Ke Za Zhi 54(2), 97–102. https://doi.org/10.3760/cma.j.issn.0529-567x.2019.02.005 (2019).
Glazener, C. et al. Mesh inlay, mesh kit or native tissue repair for women having repeat anterior or posterior prolapse surgery: Randomised controlled trial (PROSPECT). BJOG Int. J. Obstet. Gynaecol. 127(8), 1002–1013. https://doi.org/10.1111/1471-0528.16197 (2020).
Schopf, S., von Ahnen, T., von Ahnen, M. & Schardey, H. Chronic pain after laparoscopic transabdominal preperitoneal hernia repair: A randomized comparison of light and extralight titanized polypropylene mesh. World J. Surg. 35(2), 302–310. https://doi.org/10.1007/s00268-010-0850-4 (2011).
Campagna, G. et al. Titanized polypropylene mesh in laparoscopic sacral colpopexy. Int. Urogynecol. J. 31(4), 763–768. https://doi.org/10.1007/s00192-019-04146-x (2020).
Hiltunen, R. et al. Low-weight polypropylene mesh for anterior vaginal wall prolapse: A randomized controlled trial. Obstet. Gynecol. 110(2 Pt 2), 455–462. https://doi.org/10.1097/01.AOG.0000261899.87638.0a (2007).
Dubuisson, J. B., Yaron, M., Wenger, J. M. & Jacob, S. Treatment of genital prolapse by laparoscopic lateral suspension using mesh: A series of 73 patients. J. Minim. Invasive Gynecol. 15(1), 49–55. https://doi.org/10.1016/j.jmig.2007.11.003 (2008).
Loverro, G. et al. Surgical management of recurrence of multicompartment pelvic organ prolapse after failure of laparoscopic lateral POP suspension (LLPOPS): Initial report of six cases and outcomes at 2 years follow-up. Updates Surg. 72(1), 225–227. https://doi.org/10.1007/s13304-019-00698-1 (2020).
Acknowledgements
We would like to express our gratitude to all the doctors of Department of Gynecology in The Second Hospital of Tianjin Medical University;They provided great support and assistance to this study.
Funding
This study was funded by the Youth Fund of Tianjin Medical University Second Hospital (2023ydey03).
Author information
Authors and Affiliations
Contributions
Conception and design: Y.X. Collection and assembly of data: Y.W and X.G. Data analysis and interpretation: W.Yang. Manuscript writing: D.L and M.W.Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study adopts a retrospective research approach. During the research process, no special interventions were implemented on the included patients. All patient data used have been strictly stripped of personal privacy and sensitive information. This includes removing patients’ names, ID numbers, contact information, specific home addresses,ensuring that it is impossible to trace back to individuals through the data. Informed consent was obtained from all individual participants included in this retrospective study. The study protocol was approved by the Institutional Review Board of Tianjin medical university second hospital (approval number:KY2025K097). All procedures and methods in this study were carried out in strict accordance with ethical standards, relevant guidelines, and national regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, Y., Guo, X., Yang, W. et al. Retrospective comparative study on efficacy and safety of different surgical procedures for pelvic organ prolapse. Sci Rep 15, 21153 (2025). https://doi.org/10.1038/s41598-025-07878-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-07878-7