Abstract
Periodontitis is a chronic inflammatory disease that mainly occurs in the dental supporting tissues. Endoplasmic reticulum autophagy (ER-phagy) is a new type of selective autophagy. The main function of ER-phagy is to degrade excess ER membranes or toxic protein aggregates, control the volume of ER, and maintain cell homeostasis. This study utilized bioinformatics to identify and validate potential ER-phagy-related biomarkers for periodontitis. The relationship between immune cell infiltration and periodontitis as well as potential biomarkers was analyzed, to identify new targets for the diagnosis and treatment of periodontitis. Data from GeneCards and Gene Expression Omnibus (GEO) databases were utilized to identify differentially-expressed ER-phagy-related genes, and to conduct functional enrichment and pathway analyses. Random forest, least absolute shrinkage and selection operator (LASSO) and support vector machine-recursive feature removal (SVM-RFE) algorithms were used to identify hub genes. Receiver operating characteristic (ROC) curves and areas under the curve (AUCs) were calculated to assess diagnostic performance and identify potential biomarkers for periodontitis. The CIBERSORT deconvolution algorithm was used to study the link between potential biomarkers and distinct types of immune cells. In addition, clinical samples were examined using Real-time quantitative polymerase chain reaction (RT-qPCR) to verify the expression of genes related to ER-phagy in periodontitis and identify a signature which may better predict this disease. Bioinformatics analysis identified 88 differentially-expressed ER-phagy-related genes (DE-ERGs). 6 hub genes were found using LASSO, SVM-RFE and Random forest, namely ATP1A1, CD69, DNAJB11, GANAB, IL7, and PSME2. ATP1A1 and GANAB exhibited robust diagnostic efficacy in both the training set and validation set. The results of immune cell infiltration analysis revealed a significantly greater abundance of plasma cells in periodontitis tissue samples compared to healthy periodontal tissue samples (P < 0.05). Correlation analysis between potential biomarkers and immune cells demonstrated that the expression levels of ATP1A1 and GANAB were correlated with plasma cells and resting dendritic cells. Clinical samples examined by RT-qPCR verified that these ER-phagy-related signature genes in periodontitis may better predict the development of periodontitis.ER-phagy is closely related to the pathological process of periodontitis. The infiltration of immune cells differs between tissues affected by periodontitis and healthy periodontal tissues, and a variety of immune cell subsets are significantly correlated with ATP1A1 and GANAB, thus ATP1A1 and GANAB have good diagnostic efficiency for periodontitis and can be used as potential biomarkers for early diagnosis.
Similar content being viewed by others
Introduction
Periodontitis is a chronic inflammatory disease that can result in irreversible damage to the periodontal supporting tissues1. Typical clinical manifestations of periodontitis include gingival inflammation and bleeding, formation of periodontal pockets, loss of alveolar bone, and eventual tooth mobility leading to potential tooth loss if left untreated. Research has indicated that periodontitis is one of the most prevalent oral diseases worldwide, with approximately 11% of the global population suffering from severe forms2. Findings from the Fourth National Oral Health Survey revealed a prevalence rate of 52.8%, 69.3%, and 64.6% among individuals aged 35–44, 55–64, and 65–74 years old, respectively3.
Dental plaque biofilm serves as the initiating factor for periodontitis. The interaction between multiple pathogens and the dysbiosis of periodontal microecology in susceptible individuals contributes to the development of periodontitis. Stimulated by subgingival plaque, immune cells infiltrate extensively into the gingival connective tissue and secrete a plethora of cytokines. On the one hand, these cytokines play a crucial role in recruiting specific immune cells, controlling pathogenic microorganisms, and modulating osteoclast activity4. For instance, proinflammatory cytokines like IL-1β and chemokine CXCL-6 exert significant regulatory effects on the inflammatory process and immune cell response associated with periodontal bone destruction5. On the other hand, they can also contribute to periodontal tissue damage. Prostaglandin E2 is another cytokine that has been implicated in periodontal hard tissue destruction and resorption6. Furthermore, there exists an association between chronic periodontitis and several systemic diseases. Literature reports have demonstrated a clear bidirectional relationship between periodontitis and type II diabetes; thus managing both conditions may help prevent their mutual occurrence7. Therefore, investigating the inflammatory regulatory mechanisms involved in the progression of periodontitis and identifying related biomarkers can not only aid in its prevention and treatment but also contribute to mitigating the development of other diseases.
In recent years, the pathological changes of organelles in periodontal tissues have received widespread attention from the academic community. The endoplasmic reticulum (ER) is a crucial organelle involved in the synthesis, folding, and modification of membrane and secretory proteins. It also plays a role in forming connecting regions with other organelles. The dynamic remodeling of the ER is essential for maintaining intracellular homeostasis and preventing disease occurrence. When the protein folding load exceeds the capacity of the ER, ER stress (ERS) occurs, which is associated with the pathogenesis of various chronic inflammatory conditions8. Studies have shown that in the state of chronic periodontal inflammation, the expression of various inflammatory factors in periodontal tissues is upregulated, which can induce ERS. This in turn triggers selective autophagy of the ER, degrading dysfunctional ER membranes and restoring ER homeostasis9. Research indicates that ER-phagy, by regulating immune cells and controlling the release of inflammatory substances, plays a role in numerous processes such as multicellular organism development, differentiation, inflammation, and immune defense10. Additionally, it is closely related to the occurrence of cancer and neurodegenerative diseases11. However, research on the relationship between periodontitis and ER-phagy is currently limited, and the mechanisms of their interaction remain unclear.
With the continuous advancement of bioinformatics, the use of large amounts of raw data from databases and various algorithms has enabled the exploration of relationships between genes as well as between genes and diseases. Therefore, exploring the relationship between ER-phagy and the microenvironment of periodontitis at the molecular level could be of significant importance in improving inflammation and even alveolar bone remodeling in periodontitis patients. This study utilizes bioinformatics methods to screen ER-phagy-related biomarkers of periodontitis from a vast number of genes, providing valuable insights for disease diagnosis, progression, prognosis, and personalized treatment.
Materials and methods
Data download and processing
The Gene Expression Omnibus (GEO) database (https://www.ncbi.nlm.nih.gov/geo/) is a public database used to store microarray gene expression data and other forms of high-throughput functional genomics data12. Gene expression profile datasets containing samples from healthy periodontal tissues and periodontitis tissues were retrieved from GEO. Two datasets, GSE16134 and GSE10334, were used as the training and validation sets, respectively.
The training set GSE16134 included 239 patient samples and 69 control samples, and the validation set GSE10334 included 183 patient samples and 64 control samples. The raw data of both microarray datasets were based on the GPL570 platform, and probe IDs were converted to gene symbols according to the annotation information of the platform. The R package “Linear Models for Microarray Data”(“limma”) was used for data correction. ER-phagy-related genes (ERGs) were retrieved from the GeneCards database (https://www.genecards.org). Genes with a relevance score ≥ 2 were extracted for this study.
Differential expression analysis
The GSE16134 dataset was used as the training set. The “limma” software package was employed for the analysis of differentially-expressed genes (DEGs). Genes were considered differentially expressed if they exhibited P < 0.05 and |log2 FC|> 0.5. Visualization of the results pertaining to the DEGs was carried out utilizing the “ggplots” and “pheatmap” packages.
Weight gene correlation network analysis (WGCNA)
WGCNA, used to describe the association pattern between genes in microarray samples, can be used to find modules of highly correlated genes13. Firstly, hierarchical clustering was employed to observe sample aggregation. Once the clustering effect was deemed appropriate, scale independence and average connectivity analysis were conducted to determine the suitable soft threshold. Subsequently, the selected soft threshold was utilized to construct a co-expression network, topological overlap matrix, and gene clustering tree. Genes exhibiting similar expression patterns were assigned to corresponding modules. The expression of ERGs in each sample from the training set GSE16134 was extracted, with the module most strongly associated with periodontitis being defined as the core module. This approach aimed to further investigate the biological relationship between genes and phenotypes within this specific module. Genes in this core module were considered key genes related to periodontitis and ER-phagy (WGCNA-ERGs) for further analysis. Venn diagrams were used to identify the intersecting genes between DEGs and WGCNA-ERGs, which were then used for subsequent analysis.
Gene set variation analysis (GSVA) was performed to estimate the active variation of a predetermined gene set in the samples. The ssGSEA algorithm of R package “GSVA” was used to calculate the scores of ER-phagy genes in all samples. The Wilcoxon test was used to analyze the GSVA-ERG scores between periodontitis samples and normal control samples.
Construction of a protein–protein interaction (PPI) network
The search tool to retrieve interacting genes/proteins (STRING) (https://string-db.org/) is an interactive network for studying gene and protein interactions. We used Cytoscape (https://cytoscape.org/) to build the PPI network for visual representation and additional experimental testing. Cytoscape is a visualization platform that combines biomolecular interaction networks, high-throughput expression data, and other molecular states into a conceptual framework14. Furthermore, the Molecular Complex Detection (MCODE) (http://apps.cytoscape.org/apps/mcode) plugin Cytoscape was used with a plugin with default parameters to discriminate the modules that best reflect key gene clusters. Genes from cluster 1 were selected for further analysis. Key genes (GSVA-ERGs) were combined with DEGs to identify ER-phagy genes that were highly relevant to periodontitis.
Enrichment analysis
To understand the functions of genes and identify pathways with important functions, we conducted enrichment analysis, encompassing the Kyoto encyclopedia of genes and genomes (KEGG) and gene ontology (GO) analyses15,16. GO enrichment analysis was used to analyze the enrichment of DEGs in different biological process (BP), cellular component (CC) and molecular function (MF) categories. KEGG enrichment analysis was used to achieve effective clustering of DE-ERGs in signaling pathways17. Enrichment results were filtered using thresholds of P-value < 0.05 and q-value < 0.25. The analysis was performed using the R software package “clusterProfiler”.
Screening of hub genes
The LASSO algorithm is a linear regression-based machine algorithm that helps improve the accuracy of prediction by screening gene expression data18. SVM-RFE can filter out the feature subset with the highest accuracy in the data19. Random forest (RF) is a machine learning method that creates a set of classification trees through a bootstrapping process of randomly selecting a set of variables from the variable space and a cyclic selection of a small part of the sample space to fit the model20. Several machine learning algorithms can be used to identify disease-related biomarkers.
The R packages “glmnet”, “e1071” and “random forest” were used to run the LASSO algorithm, SVM-RFE algorithm and RF algorithm, respectively, to further screen the DE-ERGs. A Venn diagram was used to obtain intersecting genes from the three algorithms, identifying key DE-ERGs for subsequent analysis.
Diagnostic value analysis of hub genes
ROC curves for key DE-ERGs were plotted using the R “pROC” package in both the training and validation sets. The area under the curve (AUC) was calculated to evaluate the diagnostic value of the gene21. Genes with an AUC value ≥ 0.75 in both the training set and the validation set were considered to have significant predictive value as potential biomarkers for periodontitis. The “ggpubr” package was used to show the difference in the expression of key DE-ERGs in the training set and validation set of periodontitis tissue and healthy periodontal tissue samples.
Gene set enrichment analysis (GSEA)
GSEA was performed using the R “GSEA” package to analyze potential biomarkers22. This analysis identified biological functions and processes associated with DEGs in periodontitis. Pathways with q < 0.25 and P < 0.05 were considered statistically significant.
Immune cell infiltration analysis
The CIBERSORT algorithm was used to evaluate the infiltration of 22 immune cell subsets in healthy periodontal tissue and periodontitis tissue samples23. The results were plotted as boxplots to visualize the relative content of the above immune cells in all samples. A beanplot was drawn using the package ggplot2 to show the difference in immune cell infiltration between periodontitis tissues and healthy periodontal tissues. Finally, Spearman correlation analysis was used to calculate the relationship between potential biomarkers and immune cell infiltration, and the results are presented as a lollipop chart.
Collection of clinical samples
To experimentally the key genes, healthy gingival samples (including marginal epithelial tissues and periodontal connective tissues) were collected during clinical tooth extraction, and periodontitis samples (including gingival epithelial tissues and periodontal pocket connective tissues) of patients with stage III–IV periodontitis were collected during clinical scaling and tooth extraction. Periodontitis was diagnosed according to the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions criteria24. A total of 6 patients (mean age: 40 ± 15 years, 3 males and 3 females) were included in this study. 6 healthy volunteers were frequently matched to patients by age (± 3 years) and gender. All patients met the following inclusion criteria: no use of antibiotics in the past month, no periodontal treatment, and overall good health. Exclusion criteria included any systemic diseases or immunodeficiencies that could affect periodontal disease. All of the participants were informed and provided their consent. Our study was approved by the Ethics Committee of the Affiliated Stomatological Hospital of Dalian Medical University (approval number 2024005) and was conducted in accordance with the Declaration of Helsinki.
Real-time quantitative polymerase chain reaction
First, RNA was extracted from gingival tissues of both the periodontitis and control groups using the Trizol method. The RNA concentration and purity of the samples were measured using a NanoDrop® ND-1000 analyzer, and RNA was stored at − 80°C for later use. To remove genomic DNA, a reaction mixture was prepared with reaction conditions set at 42 °C for 2 min. Then, another reaction mixture was prepared for the reverse transcription reaction, with conditions of 37 °C for 15 min, followed by 85 °C for 5 s, to convert mRNA into cDNA. The obtained cDNA was stored at − 80 °C for future analysis. For RT-qPCR, a reaction mixture was prepared according to the instructions of the SYBR® Green Pro Taq HS qPCR kit. GAPDH was used as the internal reference transcript in this experiment. The relative expression levels of target genes were calculated using the 2−ΔΔCt method. To ensure the reliability of the experiment, each test was repeated three times. The primer sequences for RT-qPCR are provided in Supplementary Table 1.
Statistical analysis
All data processing, statistical analyses, and plotting were conducted using R 4.3.0 software. The graphs, calculations, and statistical analyses of RT-qPCR results were performed using GraphPad Prism version 10.0 (GraphPad Software Inc., San Diego, CA, USA). Differences of the means between the groups were compared using the Student’s t test. Differences were considered significant at P < 0.05.
Results
Data acquisition and differential expression analysis
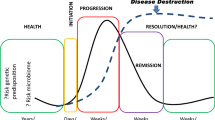
The overall study design is shown in Fig. 1. The periodontitis datasets GSE16134 and GSE10334 were obtained from the GEO database. Using GSE16134 as the training set, the R package “limma” was used to process the data, and the data were used to generate a box graph (Fig. 2A). The median was basically on the same line, which proved that the data quality was good and could be used for subsequent analysis. After data processing, “P value < 0.05, |log2 FC |> 0.5” were used as the screening criteria to analyze and screen differential genes. A total of 1,067 DEGs were identified in the training set. Among them, 673 genes were significantly up-regulated in the periodontitis tissues, represented in red, and 394 genes were significantly down-regulated in the periodontitis tissues, represented in blue (Fig. 2B). The relative expression levels of these genes across all samples are visualized as a heatmap, where deeper red represents higher expression and deeper blue represents lower expression (Fig. 2C). ER-phagy-related genes (ERGs) with a relevance score ≥ 2, were identified from the GeneCards database, totaling 53 genes.
WGCNA to obtain key genes
WGCNA was conducted on the GSE16134 dataset. First, a sample cluster tree was constructed based on the expression pattern of each sample, and the soft threshold P was determined through network topology analysis. A topological overlap matrix (TOM) was generated to assess gene expression similarity (Fig. 3A). Each vertical bar in the graph represents one gene, with genes exhibiting similar expression patterns being positioned closer to each other in the graph. Gene modules were then identified based on shared expression patterns after merging highly-correlated modules. The resulting hierarchical clustering dendrogram represented subordinate modules (Fig. 3B). The first principal component (eigengene) of each module was selected as a representative indicator of module information and correlated with clinical grouping data, which led to the creation of a correlation heat map. A higher correlation value indicated a stronger association between the module and periodontitis as well as ER-phagy (Fig. 3C). Genes in the gray module represent genes not included in any module, while the blue module showed significant positive correlations with both periodontitis status (R = 0.46, P = 8e−18) and ER-phagy (R = 0.46, P = 9e−39) (Fig. 3D). A total of 1,383 genes from the blue module intersected with DEGs, resulting in identification of key genes related to periodontitis and ER-phagy (WGCNA-ERGs). The intersection of DEGs and WGCNA-ERGs identified 657 shared DEGs (Fig. 3E).
Weight gene correlation network analysis (WGCNA) to obtain modules associated with periodontitis. (A) The soft threshold power in WGCNA was determined by analysis of network topology. (B) Clustering dendrogram of filtered genes (C) Heatmap showing the correlations between the gene modules and phenotypes. (D) Scatter plot of blue module correlation. (E) Venn diagram of the shared genes between the datasets of WGCNA-ERGs and DEGs.
Acquisition of key DEGs
A protein–protein interaction (PPI) network for the 657 key genes was constructed using the STRING database to explore their interactions. The MCODE plug-in of Cytoscape software was used to screen the key genes, with Cluster 1 receiving the highest MCODE score. Genes from Cluster 1, including CD69, IL18, and CD3D among 43 others, were selected for further analysis (Fig. 4A).
ERG-GSVA scores were calculated in the training set using the R package “GSVA”. Wilcoxon tests showed significant differences in ERG-GSVA scores between periodontitis and normal control samples, with 45 ERGs showing significant variation (Fig. 4B). The ERG-GSVA scores were higher in periodontitis samples, indicating that ER-phagy processes might be enhanced in periodontitis (Fig. 4C).
Combining Cluster 1 genes with key genes from the Wilcoxon test resulted in 88 genes strongly associated with periodontitis and ER-phagy.
Functional enrichment analysis
GO and KEGG enrichment analysis was performed using the “clusterProfiler” package in R software, and the results showed the biological functions and main pathways involved in 88 DE-ERGs. Among these 88 DE-ERGs, 763 GO enrichment pathways were identified. The top 10 significant terms at each level were listed. Biological processes (BP) were mainly enriched in macroautophagy, selective autophagy, organelle disassembly and related pathways. Cellular components (CC) were also closely associated with ER-phagy, including ER protein-containing complexes, phagophore assembly site and cytolytic granule; molecular functions (MF) were significantly correlated with ubiquitin protein ligase binding and primary active transmembrane transporter activity. There were 63 KEGG enriched pathways, and the top 20 significantly enriched entries were listed. KEGG analysis showed that they were mainly enriched in autophagy–animal, pathways of neurodegeneration—multiple diseases and other signaling pathways. The R package “ggplot” was used for visualization (Fig. 5A,B).
Results of GO and KEGG (www.kegg.jp/kegg/kegg1.html) pathway analyses of DE-ERGs. (A) GO enrichment results. (B) KEGG pathway enrichment results.
Machine learning to identify key DE-ERGs
LASSO logistic regression analysis was conducted on the 88 key genes using the R “glmnet” package. The LASSO model with the smallest error (Lambda.min) was selected (Fig. 6A,B). LASSO regression identified 28 genes: ATG16L1, ATP1A1, BECN1, CD38, CD3D, CD69, COX5B, DNAJB11, GABARAPL1, GANAB, HEATR3, HGF, HSPA4, HSPA5, IL2RB, IL7, LAG3, MAPK14, MDM2, NDUFS3, NPC1, PSMB7, PSME2, RETREG3, SEC22B, SEL1L, UFC1 and UFSP2.
Screening biomarkers. (A, B) Least absolute shrinkage and selection operator (LASSO) regression analysis results; (C, D) support vector machine-recursive feature removal (SVM-RFE) analysis results; (E) results of random forest (RF) analysis; (F) Venn diagram of gene intersection screened by machine.
The SVM-RFE algorithm in R package “e1071” was used to screen the biomarkers, and the results are presented in Fig. 6C,D, showing the accuracy and error rates of the model under different variables; the abscissa is the number of features, and the ordinate is the accuracy rate of ten-fold cross-validation and the corresponding error rate. Finally, 17 feature genes with the highest accuracy rate were screened. These were HGF, LAG3, MAPK14, DNAJB11, CD69, NDUFB4, MAP1LC3B, IL7, PSME2, HEATR3, PSMC4, ATP1A1, KLRB1, UBA5, KEAP1, HSPA5 and GANAB.
Using the RF algorithm from the R package “random forest” to solve classification and regression problems by building multiple decision trees, we identified 33 genes of interest: GANAB, ATP1A1, SEL1L, IL2RB, CD38, CD69, GZMB, IRF1, CD3D, MAP1LC3B, UFSP2, CD22, ATG3, PSMA4, CCPG1, KLRB1, CALR, CANX, ATL1, IL7, PSME2, DNAJB11, UFC1, RETREG1, IL18, NKG7, HSPA4, NPC1, ATG16L1, NT5E, SEC62, MTIF2, and DNAJC10 (Fig. 6E).
The results of three machine learning methods, LASSO, SVM-RFE and RF, were intermixed to obtain 6 genes, which were identified as the key DE-ERGs (Fig. 6F). These genes were ATP1A1, CD69, DNAJB11, GANAB, IL7, and PSME2.
Identification of potential biomarkers
ROC curves were plotted for the key DE-ERGs using data from the training set GSE16134 and the validation set GSE10334. Genes with higher AUC values indicated better diagnostic value. In the training set, AUC values for ATP1A1 (AUC:0.867), DNAJB11 (AUC:0.813), GANAB (AUC:0.905), and IL7 (AUC:0.768) were the highest. In the validation set, ATP1A1 (AUC:0.767) and GANAB (AUC:0.842) also demonstrated good diagnostic performance, with significantly higher expression in periodontitis tissues compared to healthy tissues (P < 0.05). Therefore, ATP1A1 and GANAB were identified as potential biomarkers related to ER-phagy in periodontitis (Fig. 7A,B).
Two ER-phagy-related transcriptional biomarkers classification model. (A) Receiver operating characteristic (ROC) analysis of classification models for the training set. (B) ROC analysis of classification models for the validation set. (C, D) Boxplots of expression differences of potential biomarkers in the training set and validation set.
Boxplots representing the differential expression of biomarkers in the training set and validation set are presented in Fig. 7C,D. The results showed that the biomarkers in the training set and validation set were highly expressed in the periodontitis group, and expression of all of them was significantly changed (P < 0.05).
Gene set enrichment analysis (GSEA)
Based on the above results, 2 genes highly related to ER-phagy, ATP1A1 and GANAB, were selected for subsequent analysis. Single-gene GSEA was performed using the R “GSEA” package to evaluate the biological functions of the biomarkers in periodontitis. The enrichment of ATP1A1 and GANAB in KEGG gene sets was analyzed, with the top five activating and inhibiting pathways displayed (Fig. 8A,B). The activated pathways were other glycan degradation, glycosaminoglycan biosynthesis-keratan sulfate, protein export, various types of N-glycan biosynthesis, primary immunodeficiency. Inhibitory pathways included: mismatch repair, nucleocytoplasmic transport, biosynthesis of unsaturated fatty acids, N-glycan biosynthesis, and steroid biosynthesis.
Immune cell infiltration analysis
Using the CIBERSORT algorithm on the GSE16134 gene expression profiles, the relative proportions of 22 immune cell subtypes were analyzed. There were significantly more plasma cells in periodontitis tissue samples compared with healthy periodontal tissue (Fig. 9A). Correlation analysis between immune cells and DE-ERGs was performed to explore their associations and potential interactions. Results indicated that ATP1A1 levels were positively correlated with plasma cells (r = 0.43, P < 0.01) and M0 macrophages (r = 0.36, P < 0.01), and negatively correlated with resting dendritic cells (r = − 0.47, P < 0.01). GANAB expression was positively correlated with plasma cells (r = 0.75, P < 0.01) and negatively correlated with resting dendritic cells (r = − 0.68, P < 0.01). (Fig. 9B–D).
The results showed that ATP1A1 and GANAB were correlated with the infiltration of plasma cells and resting dendritic cells. In periodontitis, there is a close link between hub DE-ERGs and host immune processes.
Clinical experiment validation
To further confirm the findings, we used RT-qPCR to identify the relative mRNA expression of the two ERGs in six pairs of samples from normal and periodontitis tissues. The results revealed that the expression of ATP1A1and GANAB varied between normal and periodontitis samples, (Fig. 10A,B) and were largely consistent with the microarray data analysis. ATP1A1 and GANAB were upregulated in the periodontitis group, with expression levels significantly higher than those in the control group.
Discussion
Periodontitis is a chronic inflammatory disease primarily caused by plaque microorganisms, leading to irreversible damage to periodontal tissues. The ER is a crucial membranous organelle in eukaryotic cells that plays a significant role in calcium homeostasis regulation and innate immunity. It is also the site for the synthesis and modification of proteins and lipids25. Periodontal inflammation can disrupt tissue homeostasis and initiate the osteogenic differentiation of periodontal ligament cells. These cells synthesize and secrete osteogenesis-related proteins, and the ER is the main site for the synthesis of these proteins. Persistent dysfunction of the ER may result in irreversible damage to periodontal tissues. Autophagy is a protective cellular mechanism involved in various essential physiological processes, including immune response, inflammation, and cell proliferation26. ER-phagy is a selective form of autophagy that occurs alongside the unfolded protein response (UPR), helping to alleviate ERS and maintain ER stability. The pathogenesis of common diseases like allergies and autoimmune disorders is also related to ER-phagy27,28. Although there have been no direct studies linking periodontitis to ER-phagy, some reports indicate that chronic inflammation can reduce the expression of Moz-related factor (MORF), leading to the upregulation of UPR sensors. This impairs ER function in periodontitis, resulting in defects in the osteogenic differentiation of periodontal ligament stem cells (PDLSCs)29. However, the role of ER-phagy in the pathogenesis of periodontitis remains unclear. Therefore, this study focused on a comprehensive bioinformatics analysis of ER-phagy-related genes in periodontal tissue from periodontitis patients.
This study used the GSE10334 and GSE16134 datasets from the GEO database as raw data to identify ER-phagy-related biomarkers of periodontitis. The datasets provided clinical indicators, and all patients included in the study met the diagnostic criteria for periodontitis. Through GO and KEGG analysis, the potential functions of DEGs in periodontitis were inferred. Enrichment analysis indicated that selective autophagy, organelle degradation, and mitophagy were the main biological processes involving these differential genes. The primary molecular functions involved ubiquitin-like protease activity and binding to unfolded proteins. Ubiquitination regulates various stages of autophagy, including initiation, elongation, and termination30. The ubiquitination of the ER-phagy receptor FAM134B promotes ER-phagy by receptor aggregation and controls ER remodeling in response to cellular demands31. Thus, it can be further speculated that ER-phagy participates in the pathogenesis of periodontitis through regulation of ubiquitination. The UPR is a protective reaction mediated by three protein sensors in the ER, and ER-phagy occurs alongside the UPR32. This aligns with our findings and provides additional evidence that ER-phagy may play a role in the progression of periodontitis. Different algorithms may yield varying computational results from the same raw data. Therefore, to ensure the predictive reliability of key genes, this study employed strict selection criteria, identifying the intersection of genes resulting from LASSO regression, SVM-RFE, and RF machine learning algorithms. Using the GSE10334 validation dataset, ROC curve analysis demonstrated that the genes ATP1A1 and GANAB play significant roles in the pathogenesis of periodontitis.The ROC curve demonstrates good predictive performance, though further research with expanded sample sizes and enhanced algorithms is needed to fully establish the superiority of machine learning models33. RT-qPCR was conducted to verify the expression of these two genes in periodontitis patients and control samples. The results showed that ATP1A1 and GANAB were highly expressed in periodontitis samples.
The CIBERSORT algorithm confirmed that ATP1A1 and GANAB are positively correlated with plasma cell infiltration. Periodontitis is an inflammatory response caused by the interaction between dental plaque biofilm and host immune defense. In fact, the progression of periodontitis involves the involvement of a variety of immune cells34. Plasma cells are the main infiltrating cells in gingival tissues during periodontitis35,36,37, and plasma cell inflammatory infiltration is a hallmark of periodontitis, with plasma cells in periodontal lesions primarily secreting pathogen-specific IgG and expressing NF-κB ligand receptor activators38. Some IgG+ plasma cells might inhibit alveolar bone loss by directly blocking osteoclast formation, thereby modulating the pathogenesis of periodontitis39. As antigen-presenting cells, dendritic cells regulate T cell differentiation and induce destructive immunity, and are also involved in the progression of periodontitis40. The correlation between ATP1A1 and GANAB, and immune cell infiltration suggests that these genes may be involved in immune cell regulation in the pathological process of periodontitis, providing new insights and directions for the study of the immune microenvironment in periodontitis.
ATP1A1 encodes a protein that is a major component of the Na+/K+ ATPase (NKA) subfamily41. The NKA, a transmembrane protein complex, plays a crucial role in maintaining cellular ion and osmotic balance by consuming energy. It is capable of inducing the expression of osteogenic genes in osteoblasts and has been identified as a pivotal ion transporter involved in regulating osteogenesis42. ATP1A1 is mainly involved in tyrosine kinase (Src)-mediated signal transduction, and thus plays an important role in apoptosis. Src plays a key role in the functional activation of macrophages43. ATP1A1 is primarily enriched in pathways such as nucleocytoplasmic transport and circadian rhythm. Research shows that circadian rhythm disruption (CRD) may exacerbate periodontitis by increasing macrophage infiltration and activation, thereby promoting inflammatory responses and alveolar bone resorption44. In the present study, ATP1A1 was found to be overexpressed in the periodontal tissue-infiltrating plasma cells during periodontitis. It can be speculated that ATP1A1 participates in immune regulation in a variety of ways and is involved in the occurrence and development of periodontitis. The above results can provide appropriate theory for the prediction and efficient treatment of periodontitis related drugs. ATP1A1 has also been implicated in the development and progression of various cancers45. However, research on ATP1A1 is still relatively limited, and its role in periodontitis remains unreported.
GANAB encodes the alpha subunit of glucosidase II (GIIα), which plays a role in protein folding and quality control46. Osteoclasts are considered to play a dominant role in periodontitis, especially in the key contribution of alveolar bone loss47. GANAB expression is upregulated upon treatment with fibroblast growth factor 2, indicating its potential role in bone formation48. Our analysis revealed that GANAB expression is elevated in plasma cells infiltrated into periodontal tissues in periodontitis. The main functional pathways involve the synthesis and degradation of glycosaminoglycans and other polysaccharides, as well as protein output. Studies have revealed that Porphyromonas gingivalis lipopolysaccharide affects the expression and processing of core proteoglycan in the matrix, and alters the activity of alveolar bone cells and development of the osteoblast phenotype49. Thus, it can be speculated that GANAB in plasma cells during periodontitis may influence the regulation of inflammation and alveolar bone resorption and destruction by affecting the synthesis and degradation of proteoglycans. In addition, GANAB is a novel key molecule, with abnormal expression also reported in multiple sclerosis (MS) and systemic lupus erythematosus50. The hereditary disease polycystic liver disease (PLD) and GANAB variants may be associated with reduced or complete loss of glucosidase II enzyme activity51. However, the role of GANAB in the pathogenesis of periodontitis has not been clearly reported. Therefore, further research is needed to explore the role of GANAB-mediated plasma cell ER-phagy in periodontitis. It can provide a theoretical basis for predicting the development of periodontitis in clinical practice, and can play a key role in early clinical case management.
Multiple studies have identified promising biomarker candidates associated with periodontitis prediction and progression52,53. Research has shown that IL-1β and MMP-8, when used in combination, may serve as reliable biomarkers for distinguishing gingivitis from periodontal health54. Current evidence regarding the potential of ATP1A1 and GANAB as biomarkers for periodontitis remains limited. Our findings indicate that these chemokines may possess significant predictive value, and their combination with established biomarkers could potentially improve the accuracy of periodontitis prediction. However, several limitations should be acknowledged. Firstly, this study is based on the existing public datasets consisting of retrospective data, which still needs to be validated by large-scale prospective clinical cohort studies. Secondly, the accuracy of our bioinformatics analyses may be constrained by inherent data limitations, including potential inconsistencies, biases, or insufficient sample sizes. Lastly, while our computational approach identified potential key genes, molecular experiments are required to validate their specific roles in periodontitis pathogenesis. Therefore, prospective clinical samples with a large sample should be assessed in the future. In addition, animal models, biopsy and further molecular mechanism studies are necessary to evaluate the biomarker role of ATP1A1 and GANAB in the diagnosis and treatment of periodontitis.
Conclusions
In this study, we explored the role of ER-phagy in periodontology, screened and validated two novel biomarkers of periodontitis from ER-phagy-related genes, and analyzed the main enrichment pathways of these markers, which provided potential targets for early diagnosis of periodontitis. In addition, the analysis of the immune microenvironment associated with biomarkers in this study can help to assess the health status of periodontal tissues, and is expected to promote the development of precision medicine and efficacy monitoring technology for periodontitis. RT-qPCR further confirmed the important role of biomarkers in periodontitis. Our present pilot study suggests that ATP1A1 and GANAB have the potential to be used as a diagnostic biomarker of periodontitis.
Data availability
The datasets analysed during the current study are available from the GSE10334 and GSE161314 of GEO database. The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request. Correspondence and requests for materials should be addressed to X.Y. at yangx03@dmu.edu.cn.
References
Dannewitz, B., Holtfreter, B. & Eickholz, P. Parodontitis: Therapie einer Volkskrankheit [Periodontitis-therapy of a widespread disease]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 64(8), 931–940. https://doi.org/10.1007/s00103-021-03373-2 (2021).
Sanz, M. et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 47(3), 268–288. https://doi.org/10.1111/jcpe.13189 (2020).
Jiao, J. et al. The prevalence and severity of periodontal disease in Mainland China: Data from the Fourth National Oral Health Survey (2015–2016). J. Clin. Periodontol. 48(2), 168–179. https://doi.org/10.1111/jcpe.13396 (2021).
Pan, W., Wang, Q. & Chen, Q. The cytokine network involved in the host immune response to periodontitis. Int. J. Oral Sci. 11(3), 30. https://doi.org/10.1038/s41368-019-0064-z (2019).
Plemmenos, G. et al. Central regulatory role of cytokines in periodontitis and targeting options. Curr. Med. Chem. 28(15), 3032–3058. https://doi.org/10.2174/0929867327666200824112732 (2021).
Ebersole, J. L. et al. Patterns of salivary analytes provide diagnostic capacity for distinguishing chronic adult periodontitis from health. J. Clin. Immunol. 33(1), 271–279. https://doi.org/10.1007/s10875-012-9771-3 (2013).
Michaud, D. S., Fu, Z., Shi, J. & Chung, M. Periodontal disease, tooth loss, and cancer risk. Epidemiol. Rev. 39(1), 49–58. https://doi.org/10.1093/epirev/mxx006 (2017).
Hu, Q. et al. The active nuclear form of SREBP1 amplifies ER stress and autophagy via regulation of PERK. FEBS J. 287(11), 2348–2366. https://doi.org/10.1111/febs.15144 (2020).
Bernales, S., Schuck, S. & Walter, P. ER-phagy: Selective autophagy of the endoplasmic reticulum. Autophagy 3(3), 285–287. https://doi.org/10.4161/auto.3930 (2007).
Das, G., Shravage, B. V. & Baehrecke, E. H. Regulation and function of autophagy during cell survival and cell death. Cold Spring Harb. Perspect. Biol. 4(6), a008813. https://doi.org/10.1101/cshperspect.a008813 (2012).
Liu, S. et al. Role of endoplasmic reticulum autophagy in acute lung injury. Front. Immunol. 14, 1152336. https://doi.org/10.3389/fimmu.2023.1152336 (2023).
Edgar, R., Domrachev, M. & Lash, A. E. Gene expression omnibus: NCBI gene expression and hybridization array data repository. Nucleic Acids Res. 30(1), 207–210. https://doi.org/10.1093/nar/30.1.207 (2002).
Langfelder, P. & Horvath, S. WGCNA: An R package for weighted correlation network analysis. BMC Bioinformat. 9, 559. https://doi.org/10.1186/1471-2105-9-559 (2008).
Otasek, D. et al. Cytoscape automation: Empowering workflow-based network analysis. Genome Biol. 20(1), 185. https://doi.org/10.1186/s13059-019-1758-4 (2008).
Kanehisa, M. et al. KEGG: Biological systems database as a model of the real world. Nucleic Acids Res. 53(D1), D672–D677. https://doi.org/10.1093/nar/gkae909 (2025).
Gene Ontology Consortium. The gene ontology resource: enriching a GOld mine. Nucleic Acids Res. 49(D1), D325–D334. https://doi.org/10.1093/nar/gkaa1113 (2021).
Kanehisa, M. Toward understanding the origin and evolution of cellular organisms. Protein Sci. 28(11), 1947–1951. https://doi.org/10.1002/pro.3715 (2019).
Alhamzawi, R. & Ali, H. T. M. The Bayesian adaptive lasso regression. Math. Biosci. 303, 75–82. https://doi.org/10.1016/j.mbs.2018.06.004 (2018).
Lin, X. et al. A support vector machine-recursive feature elimination feature selection method based on artificial contrast variables and mutual information. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 910, 149–155. https://doi.org/10.1016/j.jchromb.2012.05.020 (2012).
Hu, J. & Szymczak, S. A review on longitudinal data analysis with random forest. Brief Bioinform. 24(2), bbad002. https://doi.org/10.1093/bib/bbad002 (2023).
Robin, X. et al. pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformat. 12, 77. https://doi.org/10.1186/1471-2105-12-77 (2011).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl. Acad. Sci. U. S. A. 102(43), 15545–15550. https://doi.org/10.1073/pnas.0506580102 (2005).
Newman, A. M. et al. Robust enumeration of cell subsets from tissue expression profiles. Nat. Methods 12(5), 453–457. https://doi.org/10.1038/nmeth.3337 (2015).
Tonetti, M. S., Greenwell, H. & Kornman, K. S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Periodontol. 89(Suppl 1), S159–S172. https://doi.org/10.1002/JPER.18-0006 (2018).
Grumati, P. et al. Full length RTN3 regulates turnover of tubular endoplasmic reticulum via selective autophagy. Elife 6, e25555. https://doi.org/10.7554/eLife.25555 (2017).
Mizushima, N. & Levine, B. Autophagy in human diseases. N. Engl. J. Med. 383(16), 1564–1576. https://doi.org/10.1056/NEJMra2022774 (2020).
van Beek, N., Klionsky, D. J. & Reggiori, F. Genetic aberrations in macroautophagy genes leading to diseases. Biochimica et biophysica acta. Mol. Cell Res. 1865(5), 803–816. https://doi.org/10.1016/j.bbamcr.2018.03.002 (2018).
Levine, B. & Kroemer, G. Biological functions of autophagy genes: A disease perspective. Cell 176(1–2), 11–42. https://doi.org/10.1016/j.cell.2018.09.048 (2019).
Xue, P. et al. Decreased MORF leads to prolonged endoplasmic reticulum stress in periodontitis-associated chronic inflammation. Cell Death Differ. 23(11), 1862–1872. https://doi.org/10.1038/cdd.2016.74 (2016).
Cen, X., Li, Z. & Chen, X. Ubiquitination in the regulation of autophagy. Acta Biochim. Biophys. Sin. 55(9), 1348–1357. https://doi.org/10.3724/abbs.2023149 (2023).
González, A. et al. Ubiquitination regulates ER-phagy and remodelling of endoplasmic reticulum. Nature 618(7964), 394–401. https://doi.org/10.1038/s41586-023-06089-2 (2023).
Yang, M. et al. ER-Phagy: A New Regulator of ER Homeostasis. Front. Cell Dev. Biol. 9, 684526. https://doi.org/10.3389/fcell.2021.684526 (2021).
Yadalam, P. K. et al. Prediction of interactomic hub genes in PBMC cells in type 2 diabetes mellitus, dyslipidemia, and periodontitis. BMC Oral Health 24(1), 385. https://doi.org/10.1186/s12903-024-04041-y (2024).
Page, R. C. & Schroeder, H. E. Pathogenesis of inflammatory periodontal disease. A summary of current work. Lab. Invest. 34(3), 235–249 (1976).
Zouali, M. The emerging roles of B cells as partners and targets in periodontitis. Autoimmunity 50(1), 61–70. https://doi.org/10.1080/08916934.2016.1261841 (2017).
Marjanović, D. et al. Quantification of mast cells in different stages of periodontal disease. Vojnosanit Pregl. 73(5), 458–462. https://doi.org/10.2298/vsp141222030m (2016).
Rathod, S., Raj, A. & Wanikar, I. Quantitative analysis of mast cell count and density in chronic periodontal disease. J. Indian Soc. Periodontol. 22(2), 107–111. https://doi.org/10.4103/jisp.jisp_3_18 (2018).
Mahanonda, R. et al. Human memory B cells in healthy gingiva, gingivitis, and periodontitis. J. Immunol. (Baltimore, Md.: 1950) 197(3), 715–725. https://doi.org/10.4049/jimmunol.1600540 (2016).
Jing, L. et al. IL-37- and IL-35/IL-37-producing plasma cells in chronic periodontitis. J. Dent. Res. 98(7), 813–821. https://doi.org/10.1177/0022034519847443 (2019).
Wilensky, A. et al. Dendritic cells and their role in periodontal disease. Oral Dis. 20(2), 119–126. https://doi.org/10.1111/odi.12122 (2014).
Chang, J. T., Lowery, L. A. & Sive, H. L. Multiple roles for the Na, K-ATPase subunits, Atp1a1 and Fxyd1, during brain ventricle development. Dev. Biol. 368(2), 312–322. https://doi.org/10.1016/j.ydbio.2012.05.034 (2012).
Tang, Z. et al. Role of Na+, K+-ATPase ion pump in osteoinduction. Acta Biomater. 129, 293–308. https://doi.org/10.1016/j.actbio.2021.05.026 (2021).
Byeon, S. E. et al. The role of Src kinase in macrophage-mediated inflammatory responses. Mediat. Inflamm. 2012, 512926. https://doi.org/10.1155/2012/512926 (2012).
Ma, X. et al. Circadian rhythm disruption exacerbates the progression of macrophage dysfunction and alveolar bone loss in periodontitis. Int. Immunopharmacol. 116, 109796. https://doi.org/10.1016/j.intimp.2023.109796 (2023).
Xie, Z. & Cai, T. Na+-K+–ATPase-mediated signal transduction: From protein interaction to cellular function. Mol. Intervent. 3(3), 157–168 (2003).
Satoh, T., Toshimori, T., Noda, M., Uchiyama, S. & Kato, K. Interaction mode between catalytic and regulatory subunits in glucosidase II involved in ER glycoprotein quality control. Protein Sci. 25(11), 2095–2101. https://doi.org/10.1002/pro.3031 (2016).
Huang, X. et al. The roles of osteocytes in alveolar bone destruction in periodontitis. J. Transl. Med. 18, 479. https://doi.org/10.1186/s12967-020-02664-7 (2020).
Park, S. J. et al. Fibroblast growth factor 2-induced cytoplasmic asparaginyl-tRNA synthetase promotes survival of osteoblasts by regulating anti-apoptotic PI3K/Akt signaling. Bone 45(5), 994–1003. https://doi.org/10.1016/j.bone.2009.07.018 (2009).
Roberts, H. C. et al. Lipopolysaccharide alters decorin and biglycan synthesis in rat alveolar bone osteoblasts: Consequences for bone repair during periodontal disease. Eur. J. Oral Sci. 116(3), 207–216. https://doi.org/10.1111/j.1600-0722.2008.00535.x (2008).
De Masi, R. & Orlando, S. GANAB and N-glycans substrates are relevant in human physiology, polycystic pathology and multiple sclerosis: a review. Int. J. Mol. Sci. 23(13), 7373. https://doi.org/10.3390/ijms23137373 (2022).
van de Laarschot, L. F. M. et al. Novel GANAB variants associated with polycystic liver disease. Orphanet. J. Rare Dis. 15, 302. https://doi.org/10.1186/s13023-020-01585-4 (2020).
Hu, H. & Leung, W. K. Mass spectrometry-based proteomics for discovering salivary biomarkers in periodontitis: A systematic review. Int. J. Mol. Sci. 24(19), 14599. https://doi.org/10.3390/ijms241914599 (2023).
Zhang, Q. et al. Identification of endoplasmic reticulum stress-related biomarkers of periodontitis based on machine learning: A bioinformatics analysis. Dis. Mark. 2022, 8611755. https://doi.org/10.1155/2022/8611755 (2022).
Zhang, Y. et al. Evaluation of salivary biomarkers for the diagnosis of periodontitis. BMC Oral Health 21(1), 266. https://doi.org/10.1186/s12903-021-01600-5 (2021).
Funding
This work was supported by the National Natural Science Foundation of China (82100998, 82270971); Liaoning Provincial Natural Science Foundation Joint Fund (2023-MSLH-026); Provincial Basic Scientific Research Project of Liaoning Education Department (LJKZ0841).
Author information
Authors and Affiliations
Contributions
R.W. and J.H. write the manuscript; Q.S., S.G., G.Z. and A.L. performed the bioinformatic analysis, X.Y.,S.L. and L.W. designed the research and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, R., Hu, J., Sun, Q. et al. Identification and validation of endoplasmic reticulum autophagy-related potential biomarkers in periodontitis. Sci Rep 15, 24151 (2025). https://doi.org/10.1038/s41598-025-08180-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08180-2