Abstract
Bladder cancer is the most prevalent malignancies in the urinary system. This study was designed to investigate the trends of bladder cancer in China and differences compared with various Socio-demographic index (SDI) regions. Data from the Global Burden of Disease (GBD) 2021 database were utilized to evaluate metrics associated with bladder cancer, including age-standardized incidence rate (ASIR), age-standardized prevalence rate (ASPR), age-standardized mortality rate (ASMR), and age-standardized disability-adjusted life years rate (DALY) (ASDR). All analyses, including joinpoint regression, age-period-cohort, decomposition, spearman correlation, frontier and cross-country inequality, and Bayesian age-period-cohort, were utilized. In 2021, bladder cancer posed a significant health burden in China, with 570,636 total cases, including 463,364 males. The disease burden increased from low to high SDI regions, with China falling in the middle to high-middle SDI range. Apart from China, middle SDI and low-middle SDI regions, the ASIR of all other SDI regions showed a decreasing trend. The ASPR of bladder cancer increase globally, particularly in China and middle SDI region. Meanwhile, the ASMR and ASDR declined in China and all SDI regions. The age-period-cohort analysis showed that period and cohort effects influenced the ASIR and ASPR differently across China and each SDI region. Population growth was the primary driver of increases in these metrics. Projections suggest continued increases in ASIR, ASPR, and ASDR for both genders in China through 2036. The burden of bladder cancer is significant in China and varies across SDI regions, highlighting the link between socioeconomic development and disease burden.
Similar content being viewed by others
Introduction
Bladder cancer is one of the most common malignancies in the urinary system. According to the World Health Organization (WHO), bladder cancer is ranked as the 9th most commonly diagnosed malignancy on a global scale with an estimated 614,000 new cases and 220,000 deaths annually1. Based on the result of the survey from GLOBOCAN 2020, bladder cancer exhibits an age-standardized incidence rate of approximately 5.0 per 100,000 individuals globally. The highest incidence rates are notably observed in North America and Europe, with particularly elevated rates in countries such as the United States and Sweden. The incidence rate in these high-prevalence areas exceeds 20 per 100,000 individuals. Conversely, regions such as Africa and Asia, with the exception of specific countries like Japan, exhibit markedly lower rates2,3. Its incidence is significantly higher in men compared to women, with lifestyle and environmental factors playing pivotal roles in its etiology, including smoking, occupational exposures, and specific chemical agents4.
In China, bladder cancer has been increasingly recognized as a public health issue. According to the latest data from the China National Cancer Center, bladder cancer ranks as the 13th most common cancer, with an estimated incidence rate of 3.44 per 100,000 people and mortality rate of 1.34 per 100,000 in 20225,6. Bladder cancer in China predominantly affects older males, with a male-to-female ratio of approximately 3.8:1. The peak incidence is observed in individuals aged 60 and above, which underscores the impact of an aging population and heightened exposure to risk factors. The incidence has shown a rising trend in the last 2 decades, particularly among urban populations. Urban areas exhibit a 1.4-fold higher incidence rate compared to rural regions, and eastern China bears a significantly heavier burden relative to central and western areas7.
Socio-demographic index (SDI) serves as a valuable metric for elucidating the intricate relationship between socio-economic factors and cancer epidemiology. It combines data on income, education, and fertility rates to categorize countries into five groups, ranging from low to high SDI8. Countries with a high SDI, such as the United States and Germany, exhibit higher incidence and mortality rates of bladder cancer due to advanced diagnostic techniques, increased screening, and better treatment options. In contrast, low-SDI countries, such as those in sub-Saharan Africa, report lower incidence rates. This phenomenon may be attributed to underdiagnosis and the limited availability of healthcare resources9.
China, categorized as a middle-SDI country, exhibits unique epidemiological trends. The urban–rural divide in healthcare access and lifestyle factors significantly influences bladder cancer rates. Urban areas report higher incidence rates, likely due to increased exposure to risk factors such as smoking and industrial pollutants. The Chinese government has made strides in cancer prevention and control, yet disparities in healthcare access persist10,11.
In this study, utilizing the updated dataset from the Global Burden of Disease Study 2021 (GBD 2021), we aimed to investigate the trends of bladder cancer in China and differences compared with various SDI levels from 1990 to 2021. The findings have the potential to address the existing knowledge gap concerning the changes and correlates of bladder cancer burden in China. Furthermore, this research provides valuable insights that can inform the development of effective bladder cancer prevention and control strategies, as well as optimize the allocation of medical resources across various SDI regions.
Methods
Dataset collection
GBD 2021 was a comprehensive database providing the anonymized data about the 371 diseases, 88 risk factors, and various injuries across 204 countries and territories, 7 super regions and 5 SDI levels12. Data are available on the Global Health Data Exchange (GHDx) online platform (https://vizhub.healthdata.org/gbd-results/), which was developed and maintained by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington13. The incidence, prevalence, mortality and disability-adjusted life years (DALYs) of bladder cancer and their corresponding for the period 1990–2021 for both males and females including 20 age groups (< 5, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, 85–89, 90–94, 95 +), all ages, and age-standardized rates (ASRs) were extracted and analyzed within 204 countries and territories, and 5 SDI levels. The models in GBD 2021 including DisMod-MR 2.1 tool, Cause of Death Ensemble modelling (CODEm) framework, Spatio-Temporal Gaussian Process Regression (STGPR) to access metrics13. The data are presented as estimate and their corresponding 95% uncertainty intervals (UIs).
Studies related to GBD 2021 were reviewed and approved a waiver of informed consent by the Institutional Review Board of the University of Washington. This work has been reported in accordance with the STROCSS criteria14. The data was from public database and then the ethnical approval was not required. Furthermore, this study strictly adheres to the GATHER (Guidelines for Accurate and Transparent Health Estimates Reporting) guidelines in order to guarantee the precision and transparency of health estimates15.
Definition
Base on the International Classification of Diseases (ICD), bladder cancer was coded as C67-C67.9 (Tenth Revision (ICD-10)) and 188–188.9, V10.51, V16.52, V76.3 (ICD-9)9.
Socio-demographic index
Socio-demographic index (SDI) is a metric to reflect the level of socioeconomic development in a region or country, providing a more comprehensive perspective to help understand the relationship between population health, economic development, and social welfare8. The SDI score ranges from 0 to 1, with a higher score indicating a greater level of social development in a country or region. The SDI categorizes into 5 groups base on SDI quintiles across 204 countries and territories, including low-SDI (0–0.466), low-middle-SDI (0.466–0.6119), middle-SDI (0.619–0.712), high-middle-SDI (0.712–0.810), and high-SDI (0.810–1). The SDI score of 204 countries and territories in 2021 were recorded in Table S1.
Joinpoint regression analysis
Joinpoint regression analysis is a powerful tool for detecting and modeling changes in trends over time. It splits the time series into stages by finding one or more “Joinpoints” in the data and fits a linear or log-linear model within each stage16. Based on Joinpoint regression analysis, the annual percent change (APC) and the average annual percent change (AAPC) in bladder cancer are calculated across China and 5 SDI groups. Joinpoint regression analysis was conducted to evaluate the long-term trends of age-standardized incidence rates (ASIR), age-standardized prevalence rates (ASPR), age-standardized mortality rates (ASMR), and age-standardized DALYs rates (ASDR) from 1990 to 2021. The operation of the joinpoint regression model by means of Joinpoint Regression Program version 5.3.0 (National Cancer Institute, Rockville, MD, USA), typically entails constructing a linear regression model via the grid search method, identifying “joinpoints” through Permutation tests (P < 0.05), and computing associated metrics. The formula of joinpoint regression analysis is as following (taking DALYs as an example):
where y represents the mortality rate, x denotes the year, \(\beta_{0}\) is the constant parameter, \(\beta_{1}\) is the regression coefficient, \(k\) signifies the number of joinpoints, and \(\delta_{k}\) represents the regression coefficient of the kth segment function.
The equation for APC and AAPC estimation of each segment can be formulated as follows:
where y refers to ASR, while x denotes the calendar year of ASR. \(\beta_{1}\) signifies the regression coefficient.
where \(\omega_{i}\) represents the width of each segment function interval (measured in years), while \(\beta_{i}\) denotes the regression coefficient associated with each respective interval.
Age-period-cohort analysis
Age-period-cohort analysis is a statistical model used to understand how different factors, such as age, time period, and birth cohort affect various outcomes17. The age-period-cohort analysis is conducted using a web-based tool supported by National Cancer Institute, Division of Cancer Epidemiology and Genetics, available at (https://analysistools.cancer.gov/apc/)18. The data extracted from GBD 2021 included 17 age cohorts (15–19 to 95+), and covered 5 periods from 1992–1996 to 2017–2021, and then formed 22 cohorts. The median period (2004) and birth cohort (1947–1951) were designated as the reference levels. Additionally, Wald Tests will be employed to determine the significance (P < 0.05), and both Net Drift and Local Drift will also be calculated.
Decomposition analysis
Decomposition analysis, proposed by Das Gupta et al. serves as a versatile method utilized across multiple disciplines, such as economics, statistics, and environmental studies, to dissect intricate phenomena into their fundamental components19. The decomposition analysis utilized in this study will quantify the respective contributions of aging, epidemiological transitions, and population expansion to the observed alterations in the burden of bladder cancer. The formula of decomposition analysis is as following (taking DALYs as an example):
where DALYay,py,ey denote the age structure, total population, and DALY rate respectively for a specific year y; aiy represents the proportion of the population in age group i among the 17 age groups in year y; py signifies the total population in year y; eiy indicates the DALY rate for age category i in year y. From 1990 to 2021, each factor’s contribution to the change in DALY was defined by the effect of one factor changing while the others remained constant. For example, the effect of age structure was calculated as:
Frontier analysis
Frontier analysis is an important quantitative tool in GBD database analysis. Data envelopment analysis (DEA) and local polynomial regression (LOESS) are used to evaluate and optimize the performance of health systems. With the help of frontier analysis, we identified the minimum DALYs under different SDI development by constructing the optimal “frontier”. We used the free disposal hull (FDH) model to perform the DEA and establish the nonlinear boundaries. Data from GBD 2021 were tackled through 100 bootstrap samples to calculate the average DALYs at each SDI value. Subsequently, the “frontier” would be smoothed by LOESS with a local polynomial number of 1 and a span of 0.2. Frontier analysis assesses the unmet health potential of countries relative to their level of development by quantifying the discrepancy between observed metrics and frontier benchmarks, which defined as effective difference20.
Cross-country inequality analysis
In order to reveal the disparities in the bladder cancer burden among different countries, two standard measures of absolute and relative inequality recommended by the WHO were adopted, including the Slope Index of Inequality (SII) and the Concentration Index21. The SII is an absolute measure of health inequality. It reflects the linear relationship between DALYs and the distribution of SDI. The value of SII is the slope in the regression model (X = SDI; Y = DALYs). An elevated SII value is typically indicative of a significant imbalance. The Concentration Index reflects the distribution of healthy metric amongst socio-economic entities. The value of Concentration Index is twice as large as the region between the Lorentz curve and the diagonal. The formula of Concentration is as following:
where CI represents Concentration Index, \(\mu\) denotes the average of health indicators, N represents the total population, hi refers to the health index values for i individuals.
The Concentration Index ranges from − 1 to 1, with a value closer to 0 indicating less inequality, while a positive value signifies better health outcomes for wealthier groups and a negative value denotes better health outcomes for poorer groups.
Bayesian age-period-cohort analysis
Bayesian age-period-cohort (BAPC) model is a statistical model used to analyze and predict the impact of age, time period and birth cohort on an event such as mortality and disease incidence in population data. In order to perform fully Bayesian inference and avoid the Markov chain Monte Carlo (MCMC) sampling, the model adopted the Integrated Nested Laplace Approximation (INLA) algorithms22. Using the R packages BAPC (version 0.0.36) and INLA (version 24.06.27), the data spanning from 1990 to 2021, along with the GBD population forecasts for the period 2017–2100, were fitted into the model, and predictions for the year 2036 were subsequently generated.
Statistical analysis
The correlation between the SDI and ASR was evaluated by means of Spearman correlation analysis. All statistical analyses were conducted using R-studio software (version 4.4.2). P-values were considered statistically significant only when they were less than 0.05.
Results
Bladder cancer burden in China and 5 SDI regions
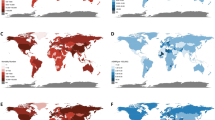
In 2021, bladder cancer presented a significant health burden in China, with a total prevalence of 570,636 cases, of which 463,364 were males. The incidence of bladder cancer in China was 105,791 cases, with 45,114 deaths and 930,100 DALYs lost in 2021 (Table S2). As illustrated in Fig. 1, the ASIR, ASPR, ASMR and ASDR in China fell within the range of high-middle to middle SDI. Additionally, the ASIR, ASPR, ASMR and ASDR of bladder cancer exhibited consistently higher levels among males compared to females, as illustrated by the joinpoint graphs, both in China and in the 5 SDI regions. Notably, as the SDI level increased, all epidemiological indicators in different SDI areas increased correspondingly. The high SDI region bore the greatest burden of bladder cancer, experiencing an ASPR of 66.81 (per 100,000) and an ASMR of 3.40 (per 100,000) (Table 1). Figure S1 depicted the distribution of bladder cancer prevalence cases stratified by age and gender across China and different SDI regions in 2021. Similarly, the number of bladder cancer is significantly higher in males than in females, indicating a notable gender disparity, especially in elderly.
Trends in bladder cancer metrics by gender across China and different SDI regions from 1990 to 2021. (A) Trends in age-standardized of incidence rate (per 100,000). (B) Trends in age-standardized of prevalence rate (per 100,000). (C) Trends in age-standardized of mortality rate (per 100,000). (D) Trends in age-standardized of DALYs rate (per 100,000). SDI socio-demographic index, DALYs disability-adjusted life-years.
As shown in Table 1, between 1990 and 2021, the ASIR of bladder cancer in China showed an increasing trend, with an AAPC of 0.27% (95% CI (confidence interval) 0.02–0.52%). However, apart from middle SDI (AAPC: 0.45%, 95% CI 0.31–0.60%) and Low-middle SDI (AAPC: 0.098%, 95% CI − 0.026–0.22%) regions, all other SDI regions, including the global context, presented a decreasing trend. The ASPR in China maintained a consistent growth trend from 1990 to 2021, with an AAPC of 1.66% (95% CI 1.50–1.83%). All SDI regions also exhibited an increase in ASPR. Among these, the most rapidly expanding SDI region within ASPR was the middle SDI region, with an associated AAPC of 1.50% (95% CI: 1.38–1.62%). Inspiringly, the change both in ASMR and ASDR were sustained declined across China and each SDI regions (AAPC < 0). Moreover, high SDI region experienced the most significant decline, while low SDI region showed the smallest decrease.
To further exploring the change of each metrics in China and various SDI regions between 1990 and 2021, corresponding APC was calculated. As presented in Fig. 2A, the period during which ASIR exhibited the most rapid growth in China was from 2016 to 2021, with an APC was 1.45% (P < 0.05). The ASIR increased significantly between 1990 and 1994 and between 2007 and 2010 in high-middle SDI (APC: 1.53%; P < 0.05) and middle SDI regions (APC: 1.49%; P < 0.05), respectively. By contrast, high SDI region showed a greatly declined in the period of 2016 to 2021 (APC: − 1.15%; P < 0.05). The ASPR in China maintained a steady growth trend, with the most significant increase occurring between 2007 and 2011 (APC: 2.67%; P < 0.05) (Fig. 2B). Although the ASPR of high SDI and high-middle SDI regions grew rapidly in the early stage, it showed a negative increase in the later stage. The change of ASPR in low-middle SDI region showed a fluctuated trend. In terms of ASMR and ASDR, China included each SDI regions exhibited an overall decline. The maximum declined was observed in China from 2004 to 2007 for ASMR (APC: − 3.98; P < 0.05) (Fig. 2C,D).
Joinpoint regression analysis of bladder cancer metrics for the overall population across China and different SDI regions from 1990 to 2021. (A) Joinpoint regression analysis of ASIR. (B) Joinpoint regression analysis of ASPR. (C) Joinpoint regression analysis of ASMR. (D) Joinpoint regression analysis of ASDR. ASIR age-standardized incidence rates, ASPR age-standardized prevalence rates, ASMR age-standardized mortality rates, ASDR age-standardized DALYs rates, DALYs disability-adjusted life-years rates, SDI socio-demographic index.
Age-period-cohort effects for bladder cancer in China and different SDI regions
The results and the responding data of age-period-cohort analysis for bladder cancer in China and different SDI regions was presented in Fig. 3 and Table S3. Generally, the age growing was positive associated with the age-specific rates of incidence, prevalence, mortality and DALYs of bladder cancer increased (Fig. 3A–D). However, excessive advanced age weakened the influence of age. The period effects for China and 5 SDI regions in the ASIR of bladder cancer was different (Fig. 3A). Taking 2004 year as reference set, China and some lower SDI regions such as middle SDI, low-middle SDI and low SDI regions, demonstrated the fall-then-rise trend. By contrast, in some regions with higher SDI levels, the period effect was attenuated with increasing years (Fig. 3A). Notably, the period effects posing on ASPR showed a similar pattern (Fig. 3B). Regarding ASMR and ASDR, both China and all SDI regions exhibited negative period effects, with China being the most significantly impacted (Fig. 3C,D). There has been a notable disparity in the cohort effect on bladder cancer incidence in China over the past 3 decades. From 1897–1901 to 1907–1911, the cohort effects rapidly diminished on incidence. Subsequently, the cohort effect showed persistent fluctuations until 1972–1976. Next, from 1972–1972 to 1997–2001, with the increase of birth cohort, the incidence of bladder cancer expanding rapidly. Finally, the incidence risk decreased again (Fig. 3A). Across 5 SDI regions, the cohort effect typically increased and then decreased. The cohort effects observed in most of SDI regions peaked during the periods of 1922–1926 and 1927–1931, with the exception of the middle SDI region. Its period time of greatest cohort effect was in 1987–1991 (Fig. 3A). In general, the birth cohort effect on bladder cancer prevalence in China increased and then decreased over time, peaking between 1997 and 2001. There was a consistent trend across all SDI regions, characterized by an initial increase followed by a subsequent decrease (Fig. 3B). As for ASMR and ASDR, the cohort effect gradually decreased (Fig. 3C,D).
Age-period-cohort analysis on bladder cancer metrics across China and different SDI regions. (A) Age-Period-Cohort analysis of incidence. (B) Age-Period-Cohort analysis of prevalence. (C) Age-Period-Cohort analysis of mortality. (D) Age-Period-Cohort analysis of DALYs. SDI socio-demographic index, DALYs disability-adjusted life-years.
Net and local drifts emphasized the change trend of each metrics in bladder cancer across China and each SDI region (Fig. S2). As exhibited in Fig. S2A, three local shifts observed in China ASIR with the age of 45–49, 60–64 and 90–94 respectively. The net drift of all SDI regions was negative, with the exception of the middle SDI region. Furthermore, the local drift in the middle SDI region was basically positive, indicating a higher risk of bladder cancer in all ages. The local drift of ASPR revealed bladder cancer posed a huge burden on China across all age groups except for those aged 95 and above. Similarly, middle SDI and low SDI regions confronted significant challenges with an overall net drift > 0 as well as local drifts > 0 in all age group (Fig. S2B). Regarding ASMR and ASDR, both China and 5 SDI regions exhibited predominantly negative local drifts (Fig. S2C,D).
Decomposition analysis
The incidence, prevalence, deaths and DALYs of decomposition analysis on bladder cancer across China and different SDI regions from 1990 to 2021 were depicted in Fig. 4 and Table S4. Between 1990 and 2021, population growth was the principal driver of the rise in global bladder cancer incidence (84.57%), prevalence (47.84%), deaths (64.35%), and DALYs (81.92%). In China, ageing effect played the most significant role in each metrics, with the value of 81.83%, 49.67%, 128.45% and 155.3% respectively (Fig. 4A–D). Epidemiological change posed a negative influence on the incidence of bladder cancer, except in the middle SDI region (Fig. 4A). Besides, across China and 5 SDI regions, the impact of epidemiological changes on deaths and DALYs growth was negative (Fig. 4C,D).
Decomposition analysis on bladder cancer metrics across China and different SDI regions. (A) Decomposition analysis of incidence. (B) Decomposition analysis of prevalence. (C) Decomposition analysis of mortality. (D) Decomposition analysis of DALYs. SDI socio-demographic index, DALYs disability-adjusted life-years.
Correlation between SDI and bladder cancer burden across 204 countries and territories in 2021
The correlation between SDI and bladder cancer burden across 204 countries and territories in 2021 was illustrated in Fig. S3. Based on the results of Spearman correlation analysis, all metrics were positive with the development of SDI (p < 0.05). Among them the highest correlation was observed in ASPR (rho = 0.775), indicating that countries with higher SDI tend to bear a greater burden of bladder cancer. Additionally, according to the curve of Spearman correlation, there were a M-shaped curve found in ASMR and ASDR, reflecting countries with middle SDI level bearing less mortality and DALYs of bladder cancer.
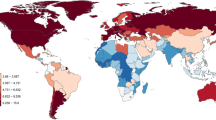
Frontier analysis
To investigate the potential extent to which DALYs can be improved relative to a country’s developmental status, a frontier analysis was conducted utilizing data on SDI and ASDR from 1990 to 2021. The unattained health improvements of countries or territories at varying stages of development during the period from 1990 to 2021 are illustrated in Fig. 5A. The DALYs burden and effective difference of bladder cancer across countries or regions with different SDI levels in 2021 were shown in Fig. 5B and Table S5. Countries (Malawi, Zimbabwe, Mali, Lebanon, Poland, Libya, Hungary, Greece, Georgia, Armenia, Bulgaria, Iraq, Croatia, Romania, Monaco) labeled in black were identified as having the top 15 most significant effective differences from the frontier, ranging from 99.70 to 169.25. Countries or territories with high SDI levels (> 0.89), including Belgium, the United Kingdom, Lithuania, Denmark, and Monaco, were designated in red to indicate high effective differences. Conversely, low SDI levels (< 0.49) countries or territories with high effective differences were labeled with blue (Somalia, Niger, Timor-Leste, Bhutan and Bangladesh). China was labeled with purple with effective difference of 39.65 and frontier value of 5.67.
Frontier analysis of bladder cancer based on SDI and ASDR across 204 countries and territories. Border is delimited in solid black; Countries and territories are represented by dots. (A) Frontier analysis of SDI and ASDR in bladder cancer from 1990 to 2021. The trend of SDI and age-standardized DALYs rates for each country or territories is shown in the form of a blue gradient. (B) Frontier analysis of SDI and age-standardized DALY rates in bladder cancer in 2021. Cyan dots represent a decrease trend in ASDR between 1990 and 2021, while coral-colored dots signify an increase in ASDR during the same period. SDI: Socio-Demographic Index; ASDR: age-standardized DALYs rates; DALYs: disability-adjusted life-years rates.
Inequality analysis of bladder cancer
The Slope Index of Inequality (SII) was 79.4599 (per 100,000) in 1990 (95% CI: 62.5420 to 96.3778) and increased to 115.7068 (per 100,000) in 2021 (95% CI 98.4899–132.9238). The increase of SII indicated the positive relationship between ASDR and SDI (Fig. 6A). This substantial increase suggested a widening disparity in the age-standardized bladder cancer burden between high-income and low-income countries during this period. Furthermore, the Concentration Index stood at 0.28 in 1990 and decreased to 0.26 by 2021 (Fig. 6B). The positive Concentration Index indicated that the affluent population exhibited superior health status. Notwithstanding regional reductions in disparities of the bladder cancer burden between low-income and high-income countries, substantial inequalities persisted, highlighting that global inequality in bladder cancer remained an enduring challenge. As illustrated in Fig. 6, the burden of bladder cancer in China has been gradually increasing over the years.
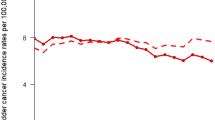
Projection analysis of bladder cancer burden in China up to 2036
The projection analysis of the gender-specific burden of bladder cancer in China up to 2036 using the BAPC model is illustrated in Fig. 7 and Table S6. Regarding the ASIR prediction, there is a significant projected increase for both males and females in China. The ASIR is expected to rise from 9.136 per 100,000 in 2021 to 11.233 per 100,000 in 2035 for males, and from 1.907 per 100,000 in 2021 to 2.369 per 100,000 in 2036 for females (Fig. 7A,B). Likewise, the predictive trend of ASPR of bladder cancer in China indicates an upward trajectory, with from 44.185 per 100,000 in 2021 to 60.323 per 100,000 in 2035 for males, and from 9.821 per 100,000 in 2021 to 12.284 per 100,000 in 2036 for females (Fig. 7C,D). Furthermore, the results indicate a slight increase in the ASDR for males, from 79.259 per 100,000 in 2021 to 86.503 per 100,000 in 2036, and for females, from 17.958 per 100,000 in 2021 to 18.195 per 100,000 in 2036 (Fig. 7E,F).
Projections on bladder cancer metrics in China up to 2036. (A) Projected ASIR for males. (B) Projected ASIR for females. (C) Projected ASPR for males. (D) Projected ASPR for females. (E) Projected ASDR for males. (F) Projected ASDR for females. ASIR age-standardized incidence rate, ASPR age-standardized prevalence rate, ASDR age-standardized DALYs rate, DALYs disability-adjusted life years.
Discussion
An in-depth analysis of the bladder cancer burden in China from 1990 to 2021 was conducted using the GBD 2021 database, with comparisons made across five SDI regions. This study aimed to enhance understanding of the trends and distribution of bladder cancer and to inform the development of health policies. Bladder cancer posed a significant threat to public health in China. Furthermore, as the SDI level increases, there was a corresponding rise in the incidence, prevalence, and mortality rate of bladder cancer. Remarkably, a significant gender disparity existed in the bladder cancer on a global scale, with males facing a significantly higher risk and more severe impact. Additionally, age disparity was also prominent in bladder cancer. Advanced age represented the most significant risk factor for bladder cancer, with the average age of diagnosis ranging from 70 to 84 years4. Globally, all epidemiological indicators of bladder cancer have generally exhibited a declining trend. However, the ASIR and ASPR of bladder cancer in China have been consistently rising, with a notable increase observed particularly in male populations. These phenomena were similarly observed in regions with middle and low-middle SDI. Furthermore, age-period-cohort analysis facilitated a deeper understanding of the contributions of age, time period, and birth cohort effects. Decomposition analysis aided in elucidating the respective contributions of population aging, demographic shifts, and epidemiological changes. Besides, based on the DALYs and SDI levels, frontier analysis and inequality analysis were employed to investigate the unmet health potential and imbalance in bladder cancer burden across countries or regions. Projections extending to 2036 indicated a continued upward trend in both the incidence and prevalence of bladder cancer in China, with a particularly significant increase observed among males. This underscored the urgent need for intervention.
The ASIR of bladder cancer in China has been on the rise over the past 32 years, which may be closely related to the ageing of the population. As we know, advanced age is regard as the greatest risk factor for bladder cancer4. The susceptibility of elderly individuals to bladder cancer can be attributed to the accumulation of chemical carcinogens and an age-related decline in DNA repair capacity23. China is currently experiencing rapid population aging, which brings a series of socioeconomic challenges to the existing healthcare system. It is projected that by 2050, there will be approximately 400 million Chinese citizens aged 65 and above, including 150 million who will be 80 years or older24. Consequently, the rising average age is associated with an increased incidence and prevalence of bladder cancer in China. Similarly, the findings from the age-period-cohort analysis and decomposition analysis corroborated the significant role of aging in the epidemiology of bladder cancer. Moreover, the imbalanced development between rural and urban areas is also a problem that should not be overlooked10,25. Therefore, it is crucial to enhance the awareness of cancer prevention and prioritize health management, particularly among elderly individuals and in rural areas.
In addition to the impact of population aging, several risk factors have also contributed to the rising burden of bladder cancer in China. Firstly, smoking as the most significant factor contribution to bladder cancer, is associated with an increased incidence of the disease. A meta-analysis comprising 90 studies demonstrated that the incidence risk of bladder cancer was significantly higher among current smokers (relative risk: 3.37, 95% CI 3.01–3.78) and former smokers (relative risk: 1.98, 95% CI 1.76–2.22) compared to nonsmokers26. Recently, despite a slight decline in smoking prevalence in China, the proportion of smokers remains at a high level, thereby contributing to an increased burden of bladder cancer27. Furthermore, high fasting plasma glucose has been reported to be not only associated with cardiovascular diseases but also identified as an independent risk factor for various cancers, including bladder cancer28. According to the GBD database, the DALYs of high fasting plasma glucose in China exhibited an increasing trend from 1990 to 2019. With the aging of the population, complications arising from high fasting plasma glucose levels will pose significant health risks to the elderly29. Strictly fasting plasma glucose supervision, early intervention, proper exercise, and diet control are necessary.
Inspiringly, the ASMR and ASDR in China have shown a steady decline from 1990 to 2021. One reason for this is the rapid urbanization30. It is widely known that there is a substantial urban–rural disparity in the socioeconomic context in China31. With the development of the social economy, both the environment and lifestyle have seen significant improvement. Moreover, the implementation of tobacco control policies has significantly contributed to the decline in smoking prevalence. In China, according to the four national tobacco surveys, the smoking prevalence gradually declined both in males and females32. Another reason is the spread of early screening and improved medical care. The advances in early detection techniques and therapeutic technologies enable the identification of patients in the early stages of disease, allowing them to receive timely treatment before their condition progresses29,33. Although the mortality of bladder cancer decreased in China, its prevalence remained keep rising. Therefore, it becomes evident that the country’s health system and cancer control strategies need to be tailored to address both urban and rural disparities.
There is a notable disparity in the epidemiology of bladder cancer between China and high or middle-high SDI regions, despite China’s rapid population aging, advancements in healthcare, and significant socioeconomic development in recent years. Compared with China, areas with high SDI (such as Western Europe and North America) generally have higher ASIR and ASPR for bladder cancer, and more significant decline in ASMR and DALYs, especially in male population. This phenomenon can be attributed to several factors. Firstly, high levels of socioeconomic development and rapid urbanization have resulted in an accelerating aging population, changes in environmental exposure and lifestyles, a shift in health awareness, and active interventions, all of which might contribute to an increasing incidence and prevalence of patients8,34,35. Secondly, the decline in ASMR and ASDR can likely be attributed to advancements in medical care and enhanced supervision of risk factors. For example, better screening systems (such as imaging, cystoscopy, and urine tests and biomarkers) and more advanced treatments (such as robot-assisted surgery, the use of PD-1/PD-L1 inhibitors) were applied universally4,36. Additionally, the implementation of stringent tobacco restriction policies represents the most effective strategy to mitigate the burden of bladder cancer in high or middle-high SDI regions. As far, the most substantial declines in consumption have been observed in the high SDI group, with a reduction of approximately 50%, as compared to a decline of 25%–30% in other SDI groups27. The high burden phenomenon of bladder cancer in high SDI region is the result of multiple factors acting together. Comprehensive prevention and control strategies should be implemented through cross-sectoral collaboration (public health, environmental protection, and industrial regulation).
Compared to China or higher SDI regions, lower SDI regions exhibited a relatively lower burden of bladder cancer, characterized by the lowest epidemiological metrics. There are four main explanations for this phenomenon. Firstly, limitations include those associated with the use of tumor registry data, potential unmeasured confounding factors, selection bias, and incomplete data reporting37. The health resources in low SDI regions such as sub-Saharan Africa were severely limited, resulting in a large number of cases going undiagnosed and unregistered. Secondly, according to GBD database, the healthy life expectancy in population decreases as the SDI value declines12. Moreover, infectious diseases, including malaria and HIV/AIDS, as well as maternal and infant mortality, predominate in cause-of-death statistics, especially in sub-Saharan Africa, whereas chronic conditions, such as bladder cancer, are relatively underrepresented38. Thirdly, due to the relatively lower level of socioeconomic development, regions with a lower SDI generally exhibit lower smoking prevalence, less industrialization, and diets with lower protein intake. Consequently, these factors contribute to reduced exposure to cancer-associated environmental risks4,39. Finally, in low SDI region, particularly in Egypt and parts of sub-Saharan Africa, Schistosoma haematobium infection is a significant risk factor for bladder squamous cell carcinoma40. However, these cases are frequently misclassified as complications of parasitic diseases and thus excluded from cancer statistics. The essence of the reduced burden of bladder cancer in low SDI regions is the result of data deficiency and survival competition, rather than actual risk differences. As these countries experience extended life expectancy, accelerated industrialization and improved diagnostic capabilities, the burden of bladder cancer may rise rapidly29.
The results revealed a significant disparity in gender differences for bladder cancer globally, with the burden being considerably higher in males than in females. Numerous explanations have been proposed to account for the gender discrepancy in incidence, including differential exposures to bladder cancer risk factors and the potential regulatory role of sex steroid hormones41. Gender differences in bladder cancer are attributable to a complex interplay of biological, environmental, and socio-cultural factors. Future research should prioritize the enhancement of sex-specific investigations to further elucidate these disparities.
This study elucidates the burden and comparison of bladder cancer among China and 5 SDI regions based on updated estimates from the GBD 2021; however, several limitations are acknowledged. Firstly, data originate from sources varying in quality, and differences in data collection and reporting standards across countries and regions may impact the accuracy and reliability of the data, especially in lower SDI regions. Secondly, the GBD database employs a range of sophisticated estimation techniques, which may involve certain assumptions and uncertainties that could influence the precision of the results. Thirdly, variations in the definition and classification of diseases across different studies and institutions may result in ambiguity and inconsistencies when comparing and analyzing data. Fourthly, our study is only based on the GBD 2021 dataset, which might not fully reflect the most recent trends in bladder cancer burden. This is particularly relevant considering the potential impacts of the COVID-19 pandemic on healthcare systems and cancer diagnoses. Lastly, the GBD database primarily focuses on disease burden at the population level. However, the absence of individual-level clinical or socioeconomic data (e.g., genetic information, income levels) restricts the development of precision medicine and targeted intervention strategies.
Conclusions
In conclusion, the primary objective of this study is to elucidate the characteristics and disparities in bladder cancer burden between China and various SDI regions from 1990 to 2021. From low SDI region to high SDI region, the disease burden of bladder cancer exhibited a corresponding trend of increasing magnitude, with China positioned within the range of high-middle to middle SDI. The disease burden in China and middle SDI region has markedly increased compared to other SDI regions, as indicated by the rising range ASPR. The gender disparities in bladder cancer were significant globally with a higher burden in males than females. Other analyses, including age-period-cohort and decomposition analysis were applied to evaluated the correlative effects for bladder cancer across China and 5 SDI regions. Additionally, the burden and unattained health improvements of countries or territories were further evaluated based on their corresponding SDI values. Finally, the projection of bladder cancer in China by gender were exhibited. The study underscores the intricate interplay between socioeconomic development and disease burden, emphasizing the need for targeted strategies in public health planning and resource allocation to address the challenge of bladder cancer.
Data availability
The data supporting the findings of this study are accessible via the Global Health Data Exchange (GHDx) at http://ghdx.healthdata.org/gbd-results-tool.
References
Ferlay J et al. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer, https://gco.iarc.who.int/today (2024).
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. https://doi.org/10.3322/caac.21660 (2021).
Ferlay, J. et al. Cancer statistics for the year 2020: An overview. Int. J. Cancer 149, 778–789. https://doi.org/10.1002/ijc.33588 (2021).
Lenis, A. T., Lec, P. M., Chamie, K. & Mshs, M. D. Bladder cancer: A review. JAMA 324, 1980–1991. https://doi.org/10.1001/jama.2020.17598 (2020).
Xia, C. et al. Cancer statistics in China and United States, 2022: Profiles, trends, and determinants. Chin. Med. J. (Engl.) 135, 584–590. https://doi.org/10.1097/CM9.0000000000002108 (2022).
Han, B. et al. Cancer incidence and mortality in China, 2022. Journal of the National Cancer Center 4, 47–53. https://doi.org/10.1016/j.jncc.2024.01.006 (2024).
Li, H. Z. et al. Bladder cancer incidence, mortality and temporal trends in China. Zhonghua zhong liu za zhi [Chinese journal of oncology] 43, 293–298. https://doi.org/10.3760/cma.j.cn112152-20200421-00362 (2021).
Chen, X. et al. Comprehensive analysis of the global, regional, and national burden of benign prostatic hyperplasia from 1990 to 2021. Sci. Rep. https://doi.org/10.1038/s41598-025-90229-3 (2025).
Zi, H. et al. Global burden of benign prostatic hyperplasia, urinary tract infections, urolithiasis, bladder cancer, kidney cancer, and prostate cancer from 1990 to 2021. Mil. Med. Res. 11, 64. https://doi.org/10.1186/s40779-024-00569-w (2024).
Zhou, M. et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 394, 1145–1158. https://doi.org/10.1016/S0140-6736(19)30427-1 (2019).
Yuan, J. et al. Global burden of bladder cancer attributable to smoking in 204 countries and territories, 1990–2019. Heliyon 10, e34114. https://doi.org/10.1016/j.heliyon.2024.e34114 (2024).
Diseases, G. B. D. & Injuries, C. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2133–2161. https://doi.org/10.1016/S0140-6736(24)00757-8 (2024).
Catalá-López, F., Padron-Monedero, A., Sarmiento Suárez, R., 2021, GDB Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2100–2132. https://doi.org/10.1016/S0140-6736(24)00367-2 (2024).
Mathew, G. & Agha, R. STROCSS 2021: Strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int. J. Surg. Open https://doi.org/10.1016/j.ijso.2021.100430 (2021).
Stevens, G. A. et al. Guidelines for accurate and transparent health estimates reporting: The GATHER statement. Lancet 388, e19–e23. https://doi.org/10.1016/S0140-6736(16)30388-9 (2016).
Kim, H. J., Fay, M. P., Feuer, E. J. & Midthune, D. N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 19, 335–351. https://doi.org/10.1002/(sici)1097-0258(20000215)19:3%3c335::aid-sim336%3e3.0.co;2-z (2000).
Huang, D. et al. Global temporal trends and projections of acute hepatitis E incidence among women of childbearing age: Age-period-cohort analysis 2021. J. Infect. 89, 106250. https://doi.org/10.1016/j.jinf.2024.106250 (2024).
Rosenberg, P. S., Check, D. P. & Anderson, W. F. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol. Biomark. Prevent.: Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prevent. Oncol. 23, 2296–2302. https://doi.org/10.1158/1055-9965.EPI-14-0300 (2014).
Das Gupta, P. Standardization and decomposition of rates from cross-classified data. Genus 50, 171–196 (1994).
Yu, S. et al. Global burden and trends of testicular cancer in adolescents and young adults from 1990 to 2021, with predictions to 2035. Sci. Rep. 14, 31787. https://doi.org/10.1038/s41598-024-82897-4 (2024).
Hosseinpoor, A. R., Bergen, N. & Schlotheuber, A. Promoting health equity: WHO health inequality monitoring at global and national levels. Glob. Health Act. 8, 29034. https://doi.org/10.3402/gha.v8.29034 (2015).
Riebler, A. & Held, L. Projecting the future burden of cancer: Bayesian age-period-cohort analysis with integrated nested Laplace approximations. Biom J. 59, 531–549. https://doi.org/10.1002/bimj.201500263 (2017).
Lin, W., Pan, X., Zhang, C., Ye, B. & Song, J. Impact of age at diagnosis of bladder cancer on survival: A surveillance, epidemiology, and end results-based study 2004–2015. Cancer Control 30, 10732748231152322. https://doi.org/10.1177/10732748231152322 (2023).
Fang, E. F. et al. A research agenda for aging in China in the 21st century. Ageing Res. Rev. 24, 197–205. https://doi.org/10.1016/j.arr.2015.08.003 (2015).
Yuan, S. & Xie, S. H. Urban-rural disparity in cancer incidence in China, 2008–2012: A cross-sectional analysis of data from 36 cancer registers. BMJ Open 11, e042762. https://doi.org/10.1136/bmjopen-2020-042762 (2021).
Luo, L. S. et al. The disease burden of bladder cancer and its attributable risk factors in five Eastern Asian countries, 1990–2019: A population-based comparative study. BMC Public Health 24, 2404. https://doi.org/10.1186/s12889-024-19909-5 (2024).
Dai, X., Gakidou, E. & Lopez, A. D. Evolution of the global smoking epidemic over the past half century: Strengthening the evidence base for policy action. Tob. Control 31, 129–137. https://doi.org/10.1136/tobaccocontrol-2021-056535 (2022).
Collaborators, G. B. D. R. F. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1223–1249. https://doi.org/10.1016/S0140-6736(20)30752-2 (2020).
Xiang, Z., Ye, Z., Ma, J., Lin, Y. & Zhou, Y. Temporal trends and projections of Bladder cancer burden in China from 1990 to 2030: Findings from the global burden of disease study. Clin Epidemiol 14, 1305–1315. https://doi.org/10.2147/CLEP.S387289 (2022).
Pompa, I. R. et al. Longitudinal analysis of bladder cancer-specific mortality trends in the United States. Bladder Cancer 9, 345–353. https://doi.org/10.3233/blc-230062 (2023).
Huang, Q. et al. Secular trends of morbidity and mortality of prostate, bladder, and kidney cancers in China, 1990 to 2019 and their predictions to 2030. BMC Cancer 22, 1164. https://doi.org/10.1186/s12885-022-10244-9 (2022).
Liu, X. et al. Secular trends in incidence and mortality of bladder cancer in China, 1990–2017: A joinpoint and age-period-cohort analysis. Cancer Epidemiol. 61, 95–103. https://doi.org/10.1016/j.canep.2019.05.011 (2019).
Antoni, S. et al. Bladder cancer incidence and mortality: A global overview and recent trends. Eur. Urol. 71, 96–108. https://doi.org/10.1016/j.eururo.2016.06.010 (2017).
Su, X., Tao, Y., Chen, F., Han, X. & Xue, L. Trends in the global, regional, and national burden of bladder cancer from 1990 to 2021: An observational study from the global burden of disease study 2021. Sci. Rep. 15, 7655. https://doi.org/10.1038/s41598-025-92033-5 (2025).
Huang, Q. et al. Changes in disease burden and global inequalities in bladder, kidney and prostate cancers from 1990 to 2019: A comparative analysis based on the global burden of disease study 2019. BMC Public Health 24, 891. https://doi.org/10.1186/s12889-024-18353-9 (2024).
Zhang, L. Y., Wang, P., Wang, Y. B. & He, Z. Q. Global, regional, and national burden of bladder cancer, 1990–2019: An age-period-cohort analysis based on the Global Burden of Disease 2019 study. Public Health 236, 193–203. https://doi.org/10.1016/j.puhe.2024.07.027 (2024).
Fan, J. et al. Global trends in the incidence and mortality of esophageal cancer from 1990 to 2017. Cancer Med. 9, 6875–6887. https://doi.org/10.1002/cam4.3338 (2020).
Global Budeb of Disease Pediatrics, C. et al. Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: Findings from the global burden of disease 2013 study. JAMA Pediatr. 170, 267–287. https://doi.org/10.1001/jamapediatrics.2015.4276 (2016).
van Hoogstraten, L. M. C. et al. Global trends in the epidemiology of bladder cancer: Challenges for public health and clinical practice. Nat. Rev. Clin. Oncol. 20, 287–304. https://doi.org/10.1038/s41571-023-00744-3 (2023).
Yohana, C., Bakuza, J. S., Kinung’hi, S. M., Nyundo, B. A. & Rambau, P. F. The trend of schistosomiasis related bladder cancer in the lake zone, Tanzania: A retrospective review over 10 years period. Infect. Agent Cancer 18, 10. https://doi.org/10.1186/s13027-023-00491-1 (2023).
Shadab, R., Nerli, R. B., Bidi, S. R. & Ghagane, S. C. Risk factors for bladder cancer: Results of a survey of hospital patients. J. Cancer Allied Spec. 9, 485. https://doi.org/10.37029/jcas.v9i1.485 (2023).
Acknowledgements
Thanks to the GBD 2021 database for providing data.
Funding
This study was supported by Guangdong Medical Research Foundation (A2024395).
Author information
Authors and Affiliations
Contributions
Xiaosheng Chen: Data curation, Software, Methodology, Visualization, Validation, Writing-original draft. Hanbin Guo: Data curation, Software, Methodology, Visualization, Writing-original draft. Sizhe Cao: Data curation, Software, Methodology, Visualization, Writing-original draft. Jieming Lin: Validation, Writing-review and editing. Peidong Huang: Validation, Writing-review and editing. Wei Zhang: Validation, Writing-review and editing. Huirong Lin: Validation, Writing-review and editing. Yong Lu: Validation, Writing-review and editing. Xinji Li: Conceptualization, Supervision, Writing-review and editing. Hui Zhang: Conceptualization, Supervision, Funding acquisition, Writing-review & editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, X., Guo, H., Cao, S. et al. Disease burden of bladder cancer in China and the different SDI regions over the world from 1990 to 2021. Sci Rep 15, 20811 (2025). https://doi.org/10.1038/s41598-025-08634-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08634-7