Abstract
This study investigates the efficacy of Astaxanthin and Quercetin as potential therapeutic agents for mitigating chloramphenicol-induced liver toxicity. Despite chloramphenicol’s broad-spectrum antibiotic properties, its clinical utility is hampered by hepatotoxic side effects. This research assesses the impact of chloramphenicol-induced mitochondrial toxicity, reactive oxygen species (ROS) production, and gene expression alterations in HepG2 liver cells. To enhance mitochondrial sensitivity, cells were cultured in galactose-containing media and exposed to chloramphenicol (up to 3000 µmol/L) for 48 h, with or without Astaxanthin (5–15 µM) or Quercetin (10–30 µM). Untreated and DMSO vehicle controls were included. Mitochondrial toxicity was evaluated using ATP content, ROS levels (ROS-Glo™ assay), and gene expression profiling. Expression of five mitochondrial-related genes SOD2, UCP2, NRF1, SURF1, and TFAM were analyzed due to their roles in oxidative stress, membrane potential regulation, biogenesis, and respiratory complex assembly. Antioxidant treatments resulted in significant reductions in ROS levels (p < 0.005) and restoration of mitochondrial gene expression patterns (p < 0.05, n = 3), alongside improved ATP retention. IC50 values and statistical comparisons were derived using GraphPad Prism with one-way ANOVA and appropriate post hoc tests. These findings suggest that Astaxanthin and Quercetin confer mitochondrial protection through modulation of oxidative stress and gene expression.
Similar content being viewed by others
Introduction
As Liver’s role is in concentrating and metabolizing a significant portion of medications, the liver becomes particularly susceptible to damage caused by pharmaceuticals. Various pharmacological agents, such as anaesthetics, anticancer drugs, antibiotics, anti-tuberculosis agents, anti-retrovirals, and cardiac medications, can induce liver damage. Furthermore, it is interesting to note that even numerous traditional medical therapies and herbal remedies may also pose hepatotoxic risks1.
In the last decade, our understanding of drug-induced liver injury (DILI) has significantly advanced through a multitude of studies, encompassing both prospective and retrospective analyses. Notably, antibiotics have consistently surfaced as primary contributors to idiosyncratic liver injury2. Investigations into cases of acute liver failure (ALF) attributable to drugs have consistently pinpointed antibiotics as the leading cause of drug-induced liver failure or as one of the major contributors to ALF3. A recent study, focused on the categorization of drugs causing idiosyncratic liver injury, revealed antimicrobials as the predominant class of drugs in category A, with over 50 reported cases in the literature4. Though, the reason why antibiotics exhibit a higher propensity for inducing liver injury compared to other drug classes remains unclear5.
Due to the indiscriminate use of antibiotics and the associated risk of liver toxicity, our investigation focuses specifically on antibiotic drugs. Specifically, Chloramphenicol which has been selected for scrutiny. Chloramphenicol is recognized for their efficacy in specific indications, although notorious for side effects, with hepatotoxicity being a particular concern.
Chloramphenicol is a broad-spectrum antibiotic derived from Streptomyces venezuelae and is now also synthesized. Chloramphenicol is effective against various microorganisms, but due to some significant side effects its use is typically reserved for some life-threatening infections (e.g.,typhoid fever)6.
Chloramphenicol is known to cause liver toxicity in humans through several mechanisms. The primary reason is its impact on the bone marrow, leading to a condition known as aplastic anaemia, which can subsequently affect the liver7.
In addition to its hematological effects, chloramphenicol has been shown to induce hepatotoxicity through mitochondrial dysfunction. It disrupts mitochondrial protein synthesis by inhibiting mitochondrial ribosomes, leading to impaired oxidative phosphorylation (OXPHOS) and reduced ATP production in hepatic cells8. This energy depletion contributes to hepatocellular stress and injury. Furthermore, chloramphenicol-induced mitochondrial dysfunction has been associated with altered metabolic responses in HepG2 cells, particularly when cultured under conditions that force mitochondrial reliance, such as galactose media9. These findings highlight mitochondrial disruption as a key contributor to chloramphenicol’s hepatotoxic profile. Furthermore, its toxicity extends beyond hepatocytes, as mitochondrial dysfunction and associated systemic oxidative stress is a key factor in chloramphenicol’s broader adverse effects8,10.
Chloramphenicol reversibly binds to the 50 S subunit of the 70 S ribosome of prokaryotic organisms and 39 S subunit of 55 S ribosome of eukaryotic mitochondria, thereby inhibiting mitochondrial protein synthesis, and suppressing the activity of the enzyme peptidyl transferase. This action inhibits mitochondrial membrane protein synthesis, resulting in the suppression of mitochondrial respiration and, ultimately, halting cell proliferation. Mechanisms could be involved in the development of reversible bone marrow depression, which is the most significant toxic effect observed in individuals using chloramphenicol11,12.
The aim of the study was to mitigate the liver toxicity induced by Chloramphenicol, by using combination therapy, Tests were conducted using two highly potent antioxidants, Astaxanthin (AXN) and Quercetin (QRN). Astaxanthin is one of the most abundant carotenoids in nature and is known as 3, 3ʹ-dihydroxy-β, β’-carotene-4, 4ʹ-dione, is a pro-carotenoid distinct from vitamin A. Its potency surpasses that of β-carotene by 10 times and exceeds vitamin E by 100 times13. Astaxanthin, a secondary carotenoid primarily derived from marine organisms, demonstrates both preventive and therapeutic effects on various liver-related conditions. Studies suggest its effectiveness in addressing liver fibrosis, tumours, ischemia-reperfusion injury, non-alcoholic fatty liver, and related ailments. Beyond its robust antioxidant properties, Astaxanthin also modulates multiple signalling pathways, and it inhibits apoptosis and autophagy, providing protection against liver ischemia-reperfusion injury14,15,16.
The flavonoid Quercetin is present in various plant parts, including apple skins, onions, berries, grains, herbs, and tea. It stands out as one of the most prevalent flavonoid compounds, known for its non-lethal, non-carcinogenic, non-teratogenic, and non-mutagenic effects in humans17. Its diverse biological effects encompass antioxidant, anticarcinogenic, anti-inflammatory, immunomodulatory, cardioprotective, and bacteriostatic properties18. Rat studies indicate that nano liposomal Quercetin demonstrates effective protection against acute liver injury, suggesting its potential as a novel hepatoprotective and therapeutic agent for individuals with liver diseases17,19,20.
In our investigation, we incorporated a comprehensive approach to evaluate mitochondrial toxicity and its implications in hepatotoxicity, utilizing methods such as reactive oxygen species (ROS) assessment, mitochondrial respiration, ATP production assays, and gene expression profiling.
The role of ROS, acknowledged for its involvement in various pathologies, particularly emphasizes mitochondria as the primary intracellular source. ROS have a dual role in cancer development; on one hand, it promotes growth, and progression, as well as acquisition of treatment resistance. On the other hand, permanent elevated ROS levels have cytotoxic effects, inducing activation of apoptotic pathways or inhibiting resistance to anticancer treatments. Among ROS, hydrogen peroxide (H2O2) stands out due to its longest half-life among ROS in cultured cells and its transformation from other ROS forms within cells. Our study aligns with previous research affirming that mitochondrial oxidative metabolism inherently produces ROS, with H2O2 emission being a well-established method for evaluating mitochondrial ROS production21. Galactose substitution for glucose in the growth media forces cells to depend on mitochondrial OXPHOS for ATP generation, making them a suitable model to study mitochondrial dysfunction. Consequently, the increased susceptibility of galactose-grown HepG2 cells to mitochondrial toxicants underscores their utility in assessing drug-induced mitochondrial dysfunction, as demonstrated by previous studies8,9,22,23.
Gene expression studies provide a powerful approach to investigating the impact of drug toxicity on mitochondrial function. By analyzing changes in the expression of genes related to mitochondrial biogenesis, energy metabolism, oxidative stress response, and apoptosis, we can gain insights into the mechanisms of drug-induced mitochondrial dysfunction and identify potential biomarkers for toxicity. Hence, these studies may help us understand the outcomes of this research, observed in respiratory and ROS studies.
To further explore the molecular basis of chloramphenicol-induced mitochondrial dysfunction, we included a targeted gene expression analysis in our study. We selected a panel of genes with well-established roles in mitochondrial structure and function: SURF1, involved in the assembly of cytochrome c oxidase (Complex IV)24; SOD2, a mitochondrial antioxidant enzyme that neutralizes superoxide radicals25; NRF1, a key transcription factor regulating nuclear genes essential for mitochondrial respiration and biogenesis26; TFAM, which controls mitochondrial DNA transcription and replication27; and UCP2, a mitochondrial inner membrane protein that modulates membrane potential and reduces ROS production28. These genes were chosen due to their relevance in mitochondrial integrity, energy metabolism, and oxidative stress processes known to be disrupted during chloramphenicol-induced hepatotoxicity.
Despite increasing awareness of antibiotic-induced liver toxicity and the general antioxidant properties of compounds like Astaxanthin and Quercetin, there remains limited evidence evaluating their role specifically in mitigating chloramphenicol-induced mitochondrial dysfunction in hepatic cells. To the best of our knowledge, this is one of the first studies to evaluate the comparative efficacy of astaxanthin and quercetin in a chloramphenicol-induced toxicity model using galactose-adapted HepG2 cells, which rely heavily on mitochondrial oxidative phosphorylation (OXPHOS). By integrating ATP-based viability assays, ROS quantification, and mitochondrial gene expression profiling, this study provides novel insights into the antioxidant-mediated protection mechanisms and proposes a targeted strategy for mitigating drug-induced hepatotoxicity.
Materials and methods
For Mitochondrial toxicity assay, Chloramphenicol, and antioxidants (Astaxanthin and Quercetin) were purchased from Sigma-Aldrich. Human liver carcinoma cells (HepG2) were procured from ATCC (USA). Cell culture media and supplements were procured from HiMedia, Galactose and CellTiter-Glo® Luminescent Cell Viability assay kit was procured from Sigma and Promega respectively. For ROS assay, Promega, ROS-Glo™ H2O2 Assay kit was used.
Research methodology
This study aimed to assess the protective effects of Astaxanthin and Quercetin against mitochondrial toxicity caused by the chloramphenicol in human liver cells (HepG2). The research was conducted in the following two stages:
In vitro assessment
-
Assessment of Mitochondrial Toxicity by cell viability assay, and.
-
Assessment Impact of antioxidants on ROS levels in the presence of a mitochondrial toxicant.
Gene expression study
-
Assessment of Mitochondrial etiology status through Gene expression study.
In vitro assessment
In vitro assessment of mitochondrial toxicity by respiratory study in HepG2 cell line
To explore the impact of drug-induced mitochondrial toxicity in a liver cell model, we opted for HepG2 cells. HepG2 cells, known for their resistance to mitochondrial toxicants owing to their high glycolytic capacity, were cultivated in galactose media. This approach aimed to elevate respiration rates, ensuring the maintenance of ATP levels29. By culturing HepG2 cells in galactose media, we aimed to enhance their reliance on mitochondrial oxidative phosphorylation (OXPHOS) rather than glycolysis, making them more susceptible to mitochondrial toxicants and drugs with mitochondrial liabilities. This shift in metabolic reliance was validated by the doubling of oxygen consumption in galactose-grown HepG2 cells compared to glucose-grown cells9.
Although HepG2 cells are widely used in liver toxicity studies due to their human origin, stable phenotype, and ease of culture, they do have limitations. As a hepatocellular carcinoma-derived line, they exhibit reduced expression of cytochrome P450 enzymes and lower metabolic capacity compared to primary hepatocytes30,31. However, they retain functional mitochondria and, when cultured in galactose-containing media, rely more heavily on mitochondrial oxidative phosphorylation (OXPHOS), making them particularly suited for studying mitochondrial toxicants such as chloramphenicol9. As the objective of our study was to explore mitochondrial dysfunction, rather than metabolic drug transformation, the HepG2 model offered a practical and mechanistically appropriate system. Nonetheless, we acknowledge the need for further validation in primary hepatocytes or in vivo systems to extend the translational relevance of our findings.
HepG2 cells maintenance
Prior to the experiments, HepG2 cells were cultured in a 75-cm2 flat bottomed cell culture flask and subjected to passage every 3 to 4 days. The medium for passage and seeding was composed of Dulbecco’s modified Eagle medium (DMEM) with glucose or galactose (1 mol/L), 10% fetal bovine serum (FBS), antibiotic-antimycotic, pyruvate, and L-glutamine. The cells were incubated in a CO2 incubator (37 °C, 5%CO2).
Preparation of solution
Drug Chloramphenicol was weighed, dissolved in DMSO to prepare stock concentration of 0.6, 2, 6, 20, 60, 200, and 600 mM. For exposure medium, stock concentration was diluted to 200-fold with each medium (DMEM-Glucose and DMEM- Galactose) in DMSO (0.5% vol/vol) to get final concentration of 3, 10, 30, 100, 300, 1000, and 3000 µM. All experimental groups included a vehicle control treated with 0.5% DMSO alone, which matched the highest DMSO concentration used in the exposure media. This control was used to assess and rule out any solvent-related effects in cell viability, ROS, and gene expression assays.
Respiration study
To evaluate the toxicological impact of Chloramphenicol on Mitochondria, exposure of Chloramphenicol was done for 6 days on HepG2 cells. HepG2 cells were seeded at a density of about 105 cells/mL (DMEM-glucose medium) in Collagen I coated 96-well plates and incubated in a CO2 incubator (37 °C, 5%CO2) for more than 4 h. Later the respective medium was replaced with DMEM-glucose medium or DMEM-galactose medium, and cells were incubated overnight. After incubation, each well medium was replaced with the exposure medium. After this treatment cells were further incubated for 6 days in a CO2 incubator (37 °C, 5%CO2). The exposure medium was renewed every 2 days. After 6 days all the medium from the plates was removed and CellTiter-Glo reagent (50 µL/well) was added and allowed to stand for 10 min. The luminescence was measured using a micro plate reader (Hidex Sense).
Assessment of impact of antioxidants on mitochondrial toxicant by ROS
For comparison of ROS production in the presence of chloramphenicol alone and chloramphenicol with antioxidants, HepG2 cells were maintained as described for respiration studies. The assay procedure was conducted according to the Promega ROS-Glo™ H₂O₂ assay protocol. The exposure medium contained chloramphenicol at the maximum concentration (3000 µmol/L), either alone or in combination with Astaxanthin (5–15 µM) or Quercetin (10–30 µM).
To account for basal ROS levels, untreated cells were included as a negative control. In addition, Rotenone (a mitochondrial complex I inhibitor) was used as a positive control to confirm the assay’s responsiveness to oxidative stress, consistent with Table 6 results. ROS production was quantified based on the Relative Luminescence Units (RLU) detected after reagent addition. These luminescence values were used to compare oxidative stress levels across treatment groups. To ensure comparability, consistent seeding densities and identical incubation conditions were maintained across all treatment groups. This consistency reduced variability and allowed for meaningful relative comparisons of ROS levels.
The concentration ranges of Astaxanthin (5–15 µM) and Quercetin (10–30 µM) were selected based on published studies that demonstrated significant antioxidant activity without inducing cytotoxic effects in HepG2 cells32,33. Prior to co-treatment studies with chloramphenicol, the selected concentrations of Astaxanthin and Quercetin were first evaluated independently using the ATP-based viability assay described in the respiration study section to confirm that they did not induce cytotoxicity. Final concentration ranges were then selected based on their ability to attenuate chloramphenicol-induced mitochondrial toxicity in respiration studies, making them suitable for subsequent ROS and gene expression experiments.
Statistical analysis
All experiments were conducted in triplicate on three independent days (n = 3 biological replicates), with three technical replicates per treatment group in each experiment. Data are presented as mean ± standard error of the mean (SEM). Statistical analyses were performed using GraphPad Prism version 8.0. Group comparisons were analyzed using one-way ANOVA, followed by Dunnett’s multiple comparisons test for ROS and ATP assays, and Bonferroni’s post hoc test for gene expression studies. A p-value < 0.05 was considered statistically significant.
Gene expression study
In gene expression study, we aim to investigate the impact of drug toxicity on mitochondrial function by analyzing mRNA levels of key genes like SURF1, SOD2, NRF1, TFAM and UCP2 (Table-2). The genes selected for scrutiny play crucial roles in various aspects of mitochondrial biology and are anticipated to shed light on the potential molecular mechanisms underlying observed outcomes in both respiratory and ROS studies conducted on HepG2 cells.
In gene expression study, primers for each selected gene are listed in Table 1. For internal control Ribosomal Protein Lateral Stalk Subunit P1 (RPLP1) gene was used. Data was acquired from SDS software ver.15.1 and analyzed; each CT value was calculated in fold change by 2 -ΔΔCT method. To assess gene expression in HepG2 cells, cells were treated with Chloramphenicol alone or in combination with Astaxanthin or Quercetin. HepG2 cells were maintained as described in Toxicity study. The cells were collected after 6 day of drug exposure, and total RNA was extracted using Trizol reagent (Invitrogen). Reverse transcription was performed with using cDNA reverse transcriptase kit from Thermos Fisher scientific.
To quantify the mRNA expression of selected genes, qPCR was carried out in a 7500 Fast Real Time PCR (Applied Biosystems) system, using SYBR Green dye (Invitrogen). Each reaction, comprised of SYBR Green master mix (KAPA), forward and reverse primers in a total volume of 10 µl, 2 µl of cDNA, equivalent to a 1/5 dilution of the cDNA, were utilized. The cycling condition was: 5 min at 95 °C, 40 repetitions of 10 s at 95 °C and 32 s at 60 °C and melt curve at 1 min at 60 °C, with a final stage of 15 s at 95 °C.
RPLP1 was selected as the reference gene for normalization based on prior studies demonstrating its stable expression in hepatic tissue under metabolic and stress conditions34. Although no dedicated geNorm or BestKeeper analysis was performed in this study. The raw Ct values for RPLP1 showed minimal variability across all treatment groups, supporting its reliability as an internal control in our experimental setup.
Results
Mitochondrial toxicity by cell viability assay
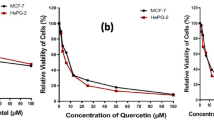
After exposure to chloramphenicol at the maximum concentration (3-3000 µmol/L), the measured ATP ratios (%) were 13.78% and 5.23% in media containing glucose and galactose, respectively. Similarly, the IC50 values were 797.39 and 130.61 µmol/L in media containing glucose and galactose, respectively. The fold change was 6.11, exceeding the critical threshold of 1.5, indicating evident mitochondrial toxicity after long-term exposure to chloramphenicol at concentrations > 100 µmol/L (Table 3 and Graph A-Fig. 1).
However, when cells were exposed for the long term in the presence of Astaxanthin, the measured ATP ratios (%) were 32.32% and 30.55% in media containing glucose and galactose, respectively, and the ATP amount fold change was 0.787, which is < 1.5 and indicates no significant toxicity (Table 4, Graph B–Figure 1). A similar observation was made with Quercetin, where the ATP fold change was 1.38 (Table 5, Graph C–Figure 1). These results indicate that the toxicological impact of chloramphenicol was significantly reduced when co-treated with Astaxanthin or Quercetin. To support these findings, IC50 values were calculated using non-linear regression in GraphPad Prism, and group comparisons of ATP levels were analyzed using one-way ANOVA followed by Dunnett’s multiple comparisons test (p < 0.05 was considered as statistically significant).
Assessment of cellular Adenosine Triphosphate (ATP)
Fold change of Adenosine Triphosphate (ATP) amount ratio of test was calculated by dividing observed IC50 Glucose Vs IC50 Galactose. IC50 was calculated using Graph Pad Prism software (significance at p < 0.05). If Fold change of IC50 is > 1.5 drug shall be considered toxic.
Assessment of impact of antioxidants on mitochondrial toxicant by ROS
For comparison of ROS production in presence of Chloramphenicol alone and Chloramphenicol with antioxidants, cells were maintained similarly as done for respiration studies and the assay procedure was followed as suggested in Promega ROS-Glo™ H2O2 assay kit protocol. Exposure medium contains chloramphenicol at the maximum concentration of 3000µmol/L along and with Astaxanthin (5 to 15 µM) or Quercetin (10–30 µM) which was used to check the ROS production. It was observed that at minimum of 10 µM of Astaxanthin and 25µM of Quercetin there was significant reduction in the ROS generation (Table-6 and Graph D-Fig. 1).
Graphs A–C show ATP-based cytotoxicity in HepG2 cells exposed to chloramphenicol alone (A) or co-treated with Astaxanthin (B) or Quercetin (C). IC₅₀ values were calculated using non-linear regression. Graph D compares ROS levels across treatment groups, including untreated (negative control) and Rotenone-treated (positive control) cells. Co-treatment with Astaxanthin (AXN) or Quercetin (QRN) significantly reduced ROS production compared to chloramphenicol (CMP) alone. Data are presented as mean ± SEM (n = 3). Statistical comparisons were performed using one-way ANOVA with Dunnett’s post-test (p < 0.005 vs. CMP).
Assessment of mitochondrial etiology status through gene expression study gene expression
Quantitative PCR (qPCR) analysis was performed on a panel of genes significantly implicated in liver toxicity. This panel included SURF1, SOD2, NRF1, TFAM and UCP2. We used housekeeping genes RPLP as a reference. Real-time PCR was employed to evaluate changes in the gene expression profiles after 6 days of drug exposure to HepG2 cells. Concentration of Chloramphenicol and antioxidant astaxanthin and Quercetin were chosen based on the cytotoxicity and ROS experiments outcome. Each mRNA/sample assigned a CT value calculated from the 7500 Fast Real Time PCR instrument software. The difference in threshold cycle between the targeted gene and the reference/housekeeping gene was used to represent ΔCT. The difference in ΔCT between treatment group and vehicle control group was expressed as ΔΔCT and fold changes were calculated with 2 -ΔΔCT compared to control vs. CMP and CMP vs. AXN or QRN. Calculated 2 -ΔΔCT value indicates that after long term exposure of chloramphenicol, gene expression of SURF1 and TFAM is showing downregulation, however, for NRF1, SOD2 and UCP2 upregulation is observed. Interestingly, in the presence of antioxidants (Astaxanthin and Quercetin), the expression levels were significantly reversed compared to observed in the presence of Chloramphenicol alone. Statistical analysis of gene expression data was conducted using one-way ANOVA followed by Bonferroni’s multiple comparisons test to evaluate differences among treatment groups. Statistical significance was considered at p < 0.05. (Fig. 2).
Graphs demonstrating the fold change representing relative gene expression for selected genes using RT-qPCR in HepG2 cells. The gene expression was checked for controls, in response to chloramphenicol alone, or in combination with astaxanthin or quercetin. Results are presented as means ± SEM, where n = 3. Significance levels are indicated as ***P value < 0.001 vs. control and ***P value < 0.003 Chloramphenicol Vs Antioxidants (one-way ANOVA followed by Bonferroni’s post-test).
Discussion
Members of important drug classes, such as thiazolidinediones, statins, fibrates, antivirals, antibiotics, and anticancer agents, have been shown to induce mitochondrial toxicity8,9. In this investigation we have focused on antibiotics specifically Chloramphenicol.
In our experiment, to enhance the detection of Chloramphenicol-induced mitochondrial effects in assays, HepG2 cells were cultured in galactose-containing media to promote reliance on mitochondrial oxidative phosphorylation rather than glycolysis. This metabolic shift resulted in increased oxygen consumption, making galactose-grown HepG2 cells more susceptible for Chloramphenicol8.
This experiment indicates that Chloramphenicol in > 100 µmol/L concentration is toxic for HepG2 cells, and the toxicity found alleviated in presence of Astaxanthin (15 µM) or Quercetin (30 µM) as demonstrated by ATP assay results (Fig. 1, p < 0.05, ANOVA with Dunnett’s test). These findings were also supported in Reactive oxygen species (ROS) experiments, where we found significant decrease in ROS levels in presence of antioxidants compared to in presence of Chloramphenicol alone (Table 6, p < 0.005, one-way ANOVA with Dunnett’s post-test).
The initial metabolic process which could be affected due to Mitochondrial dysfunction is oxidative phosphorylation (OXPHOS). During OXPHOS, energy is converted into ATP by five mitochondrial complexes (I to V), among these complexes, 84 subunits are encoded by nuclear DNA, while 13 are encoded by mitochondrial DNA35. In our gene expression studies, we have tried to understand the direct effect of Chloramphenicol on expression of the selected genes which are directly or indirectly responsible for mitochondrial function. The observed gene-specific responses were as follows:
-
SOD2: In response to chloramphenicol-induced mitochondrial dysfunction, cells have up regulated expression of SOD2 as a potential mechanism to mitigate the heightened oxidative stress.
-
UCP2: Given its role in reducing oxidative stress, the observed-up regulation of UCP2 expression could function as a protective mechanism. By lowering the mitochondrial membrane potential, UCP2 may reduce ROS production, thereby safeguarding cells from oxidative damage.
-
NRF1: Chloramphenicol-induced inhibition of mitochondrial protein synthesis may impair mitochondrial function and energy production. The observed-up regulation of NRF1 expression may represent an effort to compensate for this dysfunction by promoting mitochondrial biogenesis and enhancing the expression of respiratory chain components.
-
SURF1: The observed down regulation of SURF1 expression likely reflects a decrease in mitochondrial protein synthesis capacity, resulting in reduced demand for SURF1’s role in cytochrome c oxidase (COX) assembly.
-
TFAM: Chloramphenicol-induced reduction in ATP levels, potentially stemming from down regulation of the oxidative phosphorylation (OXPHOS) system, may lead to the observed down regulation of TFAM expression. This down regulation could impact mitochondrial DNA replication and transcription due to decreased availability of ATP.
These gene-specific changes were statistically significant compared to the CMP only group, as shown in Fig. 2 (p < 0.05, one-way ANOVA followed by Bonferroni’s test).
This study provides novel insights into the protective effects of Astaxanthin and Quercetin against Chloramphenicol-induced mitochondrial toxicity in human hepatic cells. Unlike earlier research that primarily focused on the general antioxidant properties of these compounds, our study specifically demonstrates their efficacy in a drug-induced toxicity model, which is a significant advancement in understanding their therapeutic potential. This research uniquely contributes to the field by:
-
Targeted Application: Demonstrating the specific application of Astaxanthin and Quercetin in mitigating mitochondrial damage caused by Chloramphenicol, highlighting their potential as targeted therapeutic agents for drug-induced liver toxicity.
-
Mechanistic Insights: Providing initial evidence on the molecular pathways through which these antioxidants exert their protective effects, setting the stage for future studies to elucidate the precise mechanisms involved.
-
Comparative Efficacy: Offering a comparative analysis of the effectiveness of Astaxanthin and Quercetin, thereby guiding future research and clinical applications in selecting appropriate antioxidants for mitigating specific types of drug-induced toxicity.
-
Broader Implications: Opening new avenues for research into other antioxidants that may have similar or enhanced protective effects, thus broadening the scope of potential therapeutic interventions for drug-induced liver damage.
Previous studies have also explored the hepatoprotective roles of various antioxidants. For example, N-acetylcysteine (NAC) significantly reduced liver enzyme levels and prevented hepatotoxicity in patients undergoing anti-tuberculosis therapy36. Likewise, resveratrol attenuated vancomycin-induced liver damage in rats by reducing oxidative stress and inflammatory markers37. Vitamin E has also been shown to mitigate doxorubicin-induced hepatotoxicity by enhancing antioxidant enzyme activity and reducing lipid peroxidation38. Compared to these antioxidants, Astaxanthin and Quercetin not only exhibit potent antioxidant properties but also uniquely modulate mitochondrial-specific genes such as SURF1, TFAM, and UCP2, offering a targeted mechanism to counteract chloramphenicol-induced mitochondrial dysfunction.
Conclusion
This study highlights valuable insights into the therapeutic efficacy of antioxidants, particularly Astaxanthin and Quercetin, in alleviating Chloramphenicol-induced liver toxicity. Chloramphenicol, while effective against a wide range of microbes, is associated with hepatotoxicity. By using human liver cells (HepG2) in this investigation, we present a relevant in-vitro model to elucidate the effects of these antioxidants in mitigating liver toxicity and their potential implications for human health. This is particularly noteworthy as it highlights the potential of these antioxidants in hepatoprotection and therapeutic intervention in liver diseases. The study also underscores the antioxidant-based strategies in managing drug-induced liver injury. However, it is important to note that while these results are promising, further research is needed to fully understand the mechanisms through which astaxanthin, and quercetin exert their protective effects. Additionally, in vivo studies and clinical trials are necessary to validate these findings and assess the safety and efficacy of these antioxidants in humans.
Data availability
“The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request”.
Change history
11 November 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41598-025-28069-4
References
David, S. & Hamilton, J. P. Drug-induced liver injury. US Gastroenterol. Hepatol. Rev. 6, 73–80 (2010). PMID: 21874146; PMCID: PMC3160634.
Bjornsson, E. S. et al. Incidence, presentation, and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 144, 1419–1425. https://doi.org/10.1053/j.gastro.2013.02.006 (2013).
Chalasani, N. et al. United States drug induced liver injury network. Features and outcomes of 899 patients with drug-induced liver injury: the DILIN prospective study. Gastroenterology 148 (7), 1340–1352e7. https://doi.org/10.1053/j.gastro.2015.03.006 (2015).
Mindikoglu, A. L. et al. Valproic acid-associated acute liver failure in children: case report and analysis of liver transplantation outcomes in the united States. J. Pediatr. 158 (5), 802–807. https://doi.org/10.1016/j.jpeds.2010.10.033 (2011).
Björnsson, E. S. & Hoofnagle, J. H. Categorization of drugs implicated in causing liver injury: critical assessment based on published case reports. Hepatology 63 (2), 590–603. https://doi.org/10.1002/hep.28323 (2016).
Björnsson, E. S. Drug-induced liver injury due to antibiotics. Scand. J. Gastroenterol. 52 (6–7), 617–623. https://doi.org/10.1080/00365521.2017.1291719 (2017).
Aronson, J. K. Meyler’s Side Effects of Drugs (Sixteenth Edition). Elsevier 229–236. https://doi.org/10.1016/B978-0-444-53717-1.00472-8 (2016).
Li, C. H., Cheng, Y. W., Liao, P. L., Yang, Y. T. & Kang, J. J. Chloramphenicol causes mitochondrial stress, decreases ATP biosynthesis, induces matrix metalloproteinase-13 expression, and solid-tumor cell invasion. Toxicol. Sci. 116 (1), 140–150. https://doi.org/10.1093/toxsci/kfq085 (2010).
Marroquin, L. D., Hynes, J., Dykens, J. A., Jamieson, J. D. & Will, Y. Circumventing the Crabtree effect: replacing media glucose with galactose increases susceptibility of HepG2 cells to mitochondrial toxicants. Toxicol. Sci. 97 (2), 539–547. https://doi.org/10.1093/toxsci/kfm052 (2007).
National Toxicology Program. RoC & Profile, C. 15th RoC (2021). Available from: https://ntp.niehs.nih.gov/sites/default/files/ntp/roc/content/profiles/chloramphenicol.pdf
West, B. C., DeVault, G. A. Jr., Clement, J. C. & Williams, D. M. Aplastic anemia associated with parenteral chloramphenicol: review of 10 cases, including the second case of possible increased risk with cimetidine. Rev. Infect. Dis. 10 (5), 1048–1051. https://doi.org/10.1093/clinids/10.5.1048 (1988).
Suárez-Rivero, J. M. et al. Mitochondria and antibiotics: for good or for evil? Biomolecules 11(7), 1050 (2021). https://doi.org/10.3390/biom11071050
Yamashita, E. Let Astaxanthin be Thy medicine. Pharma Nutr. 3 (4), 115–122. https://doi.org/10.1016/j.phanu.2015.09.001 (2015).
Li, J., Guo, C. & Wu, J. Astaxanthin in liver health and disease: a potential therapeutic agent. Drug Des. Devel Ther. 14, 2275–2285. https://doi.org/10.2147/DDDT.S230749 (2020).
Wu, L. et al. Astaxanthin attenuates hepatic damage and mitochondrial dysfunction in non-alcoholic fatty liver disease by up-regulating the FGF21/PGC-1α pathway. Br. J. Pharmacol. 177 (16), 3760–3777. https://doi.org/10.1111/bph.15099 (2020).
Sayuti, N. H., Nawawi, M. & Goon, K. N. Preventative and therapeutic effects of Astaxanthin on NAFLD. Antioxid. (Basel). 12 (8), 1552. https://doi.org/10.3390/antiox12081552 (2023).
Pizzorno, J. E. & Murray, M. T. Textbook of natural medicine-E-book. Elsevier Health Sci. (2020).
Liu, X. et al. Protective and therapeutic effects of nanoliposomal Quercetin on acute liver injury in rats. BMC Pharmacol. Toxicol. 21, 11. https://doi.org/10.1186/s40360-020-0388-5 (2020).
Zhao, X. et al. Quercetin as a protective agent for liver diseases: a comprehensive descriptive review of the molecular mechanism. Phytother Res. 35 (9), 4727–4747. https://doi.org/10.1002/ptr.7104 (2021).
Gwozdzinski, K., Pieniazek, A. & Gwozdzinski, L. Reactive oxygen species and their involvement in red blood cell damage in chronic kidney disease. Oxid. Med. Cell. Longev. 2021 (6639199). https://doi.org/10.1155/2021/6639199 (2021).
Juan, C. A., de la Pérez, J. M., Plou, F. J. & Pérez-Lebeña, E. The chemistry of reactive oxygen species (ROS) revisited: outlining their role in biological macromolecules (DNA, lipids and proteins) and induced pathologies. Int. J. Mol. Sci. 22 (9), 4642. https://doi.org/10.3390/ijms22094642 (2021).
Pernelle, K. et al. Automated detection of hepatotoxic compounds in human hepatocytes using HepaRG cells and image-based analysis of mitochondrial dysfunction with JC-1 dye. Toxicol. Appl. Pharmacol. 254 (3), 256–266. https://doi.org/10.1016/j.taap.2011.04.018 (2011).
Rossignol, R. et al. Energy substrate modulates mitochondrial structure and oxidative capacity in cancer cells. Cancer Res. 64 (3), 985–993. https://doi.org/10.1158/0008-5472.can-03-1101 (2004).
Tiranti, V. et al. Mutations of SURF1 in Leigh disease associated with cytochrome c oxidase deficiency. Am. J. Hum. Genet. 63 (6), 1609–1621. https://doi.org/10.1086/302139 (1998).
Zelko, I. N., Mariani, T. J. & Folz, R. J. Superoxide dismutase multigene family: a comparison of the CuZn-SOD (SOD1), Mn-SOD (SOD2), and EC-SOD (SOD3) gene structures, evolution, and expression. Free Radic Biol. Med. 33 (3), 337–349. https://doi.org/10.1016/S0891-5849(02)00905-X (2002).
Scarpulla, R. C. Transcriptional paradigms in mammalian mitochondrial biogenesis and function. Physiol. Rev. 88 (2), 611–638. https://doi.org/10.1152/physrev.00025.2007 (2008).
Ekstrand, M. I. et al. Mitochondrial transcription factor A regulates MtDNA copy number in mammals. Hum. Mol. Genet. 13 (9), 935–944. https://doi.org/10.1093/hmg/ddh109 (2004).
Brand, M. D. & Esteves, T. C. Physiological functions of the mitochondrial uncoupling proteins UCP2 and UCP3. Cell. Metab. 2 (2), 85–93. https://doi.org/10.1016/j.cmet.2005.06.002 (2005).
Maurya, A. K. & Vinayak, M. Anticarcinogenic action of Quercetin by downregulation of phosphatidylinositol 3-kinase (PI3K) and protein kinase C (PKC) via induction of p53 in hepatocellular carcinoma (HepG2) cell line. Mol. Biol. Rep. 42 (9), 1419–1429. https://doi.org/10.1007/s11033-015-3921-7 (2015).
Wilkening, S., Stahl, F. & Bader, A. Comparison of primary human hepatocytes and HepG2 cells with regard to their biotransformation properties. Drug Metab. Dispos. 31 (8), 1035–1042. https://doi.org/10.1124/dmd.31.8.1035 (2003).
Gerets, H. H. et al. Characterization of primary human hepatocytes, HepG2 cells, and HepaRG cells at the mRNA level and CYP activity in response to inducers. Cell. Biol. Toxicol. 28 (2), 69–87. https://doi.org/10.1007/s10565-011-9208-4 (2012).
Yang, Y. et al. Astaxanthin prevents alcohol-induced hepatotoxicity in HepG2 cells: involvement of the Nrf2 pathway in modulation of oxidative stress. J. Agric. Food Chem. 63 (4), 1800–1808. https://doi.org/10.1021/jf504638b (2015).
Li, Y., Ding, Y., Min, Q., Hu, W. & Hao, H. Quercetin protects human hepatoma HepG2 cells from oxidative stress-induced apoptosis via the Nrf2 signaling pathway. Biochem. Cell. Biol. 93 (5), 438–444. https://doi.org/10.1139/bcb-2015-0016 (2015).
Hernández, A. H., Curi, R. & Salazar, L. A. Selection of reference genes for expression analyses in liver of rats with impaired glucose metabolism. Int. J. Clin. Exp. Pathol. 8 (4), 3946–3954 (2015). PMID: 26097580; PMCID: PMC4466967.
Lunnon, K. et al. Mitochondrial genes are altered in blood early in alzheimer’s disease. Neurobiol. Aging. 53, 36–47. https://doi.org/10.1016/j.neurobiolaging.2016.12.029 (2017).
Baniasadi, S. et al. Protective effect of N-acetylcysteine on antituberculosis drug-induced hepatotoxicity. Eur. J. Gastroenterol. Hepatol. 22 (10), 1235–1238 (2010).
Alshehri, F. S. & Alorfi, N. M. Protective role of Resveratrol against VCM-induced hepatotoxicity in male Wistar rats. Front. Pharmacol. 14, 1130670 (2023).
Seif El-Din, S. H. et al. Resveratrol mitigates hepatic injury in rats by regulating oxidative stress, nuclear factor-kappa B, and apoptosis. J. Adv. Pharm. Technol. Res. 7 (3), 99–104 (2016).
Acknowledgements
We are highly grateful to Atmiya University for providing the resources and support to carry out the study.
Funding
This research received no funding from external sources, and no funding was received for the preparation or publication of the manuscript.
Author information
Authors and Affiliations
Contributions
DB: Conceptualization, Provided resources, Mentorship, Overall supervision and Review.BV: Planning and execution of the experiments, Manuscript writing and primary author of the manuscript.HP: Supports with the gene study component, contributing data review.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Consent for publication was obtained from all participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in the order of the author names which was incorrectly given as Brijesh Kumar Verma, Debashis Banerjee and Hiren M. Patel.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Verma, B.K., Patel, H.M. & Banerjee, D. Mitigating Chloramphenicol induced liver toxicity by exploring the therapeutic potential of Astaxanthin and Quercetin. Sci Rep 15, 33896 (2025). https://doi.org/10.1038/s41598-025-08809-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08809-2