Abstract
This study examined the influence of physical activity (PA) on the retention of rate of torque development (RTD) effects achieved following a 16-week high-speed resistance training (HSRT) over a 12-month follow-up period. Secondly, the fear of falling was also assessed. After the follow-up, 36 participants were categorized into two groups according to the PA: light activity group (LAG, N = 20, age 70.00 ± 3.66 years) and moderate-to-vigorous activity group (MVAG, N = 16, age 68.50 ± 2.09 years). At the four time points, RTDPEAK and its time intervals for knee extension and flexion were measured using an isokinetic dynamometer at 60º/s, and the fear of falling was assessed using the Falls Efficacy Scale–International questionnaire. Both groups showed significant RTDPEAK improvements from pre-intervention to the 12-month follow-up (moderate-to-large effect sizes). However, PA levels suggested to influence the retention effects: LAG showed declines in dominant RTDPEAK (2% in extension and flexion) and in non-dominant side (6% extension and 5% flexion). In contrast, the MVAG maintained or slightly improved RTDPEAK performance in dominant (1% extension and 2% flexion) and in non-dominant side (3% extension and 1% flexion). Fear of falling scores remained significantly reduced in both groups compared to pre-intervention, regardless of PA level. In summary, maintaining moderate-to-vigorous PA during follow-up appears to enhance the long-term retention of HSRT-induced neuromuscular adaptations, whereas HSRT effects on fear of falling were sustained regardless of PA level, highlighting its clinical potential for fall prevention.
Similar content being viewed by others
Introduction
The global demographic shift toward an increasingly aged population, specifically individuals aged 65 and older, is occurring at an exponential rate, placing substantial demands on healthcare systems worldwide. Briefly, aging is an inevitable and universal biological process characterized by progressive declines in physiological functions, which increase vulnerability and, ultimately, lead to mortality1. Among these age-related impairments, the neuromuscular system is particularly affected2, primarily due to muscle mass atrophy, especially in type II (fast-twitch) fibers3 and a concurrent reduction in neuromuscular activation4. These factors collectively compromise the ability to produce force/torque rapidly, a key parameter known as the rate of torque development (RTD)5. Such declines negatively impact the daily lives of older adults by reducing functional capacity6 and increasing both the risk7 and fear of falls8.
In this context, structured exercise programs have been shown to effectively mitigate the detrimental effects of aging9,10. Among these, high-speed resistance training (HSRT) is widely recognized as a non-pharmacological and cost-effective intervention for older adults10,12 due to its ability to counteract neuromuscular deterioration associated with aging. Recent guidelines by Izquierdo et al.10 highlight the importance of HSRT interventions for older adults, emphasizing their ability to recruit fast-twitch muscle fibers, improve neuromuscular coordination through high-velocity contractions, optimize motor unit firing rates, and enhance both muscle activation and intermuscular coordination, factors closely related to RTD13.
Despite significant increases in RTD following resistance training (RT) programs in older adults11,14,16, some evidence suggests that these improvements are not sustained once structured and supervised RT is discontinued15,17. Unfortunately, as Douda et al.18 noted, the cessation or interruption of community-based exercise programs is often unavoidable. However, findings from Mertz et al.19 and Snijders et al.20 indicate that older adults who maintained RT participation at least once per week retained neuromuscular benefits, including RTD, muscle power, and quadriceps muscle cross-sectional area, over six-month and 12-month follow-up periods, respectively. These results underscore the importance of maintaining an active lifestyle and avoiding prolonged sedentary behaviors, such as excessive television viewing or mobile phone use, which are associated with reduced engagement in moderate-to-vigorous physical activity (PA) levels21,23.
Indeed, Izquierdo et al.10 emphasize that reduced PA habits can negatively impact muscle mass, power, strength, and functional capacity24,25. Consequently, discouraging older adults from maintaining or increasing their PA, or restricting their access to new exercise programs, raise important ethical concerns9,10,26. Rather than focusing solely on the traditional detraining effects, this study encouraged participants to sustain an active lifestyle following a 16-week HSRT program throughout a 12-month follow-up period. Thus, this study aimed to examine the role of PA levels in retaining RTD improvements over 12 months in independent older adults. Additionally, it explored whether PA levels contributed to sustaining the effects in fear of falling achieved during the intervention.
Materials and methods
Study design
This exploratory longitudinal study is part of the “Idade Activa” research project, registered clinicaltrials.gov (ID: NCT05586087 | https://www.clinicaltrials.gov/study/NCT05586087) with clinical trial registration on 19/10/2022. The project adhered to the principles outlined in the Declaration of Helsinki and was approved by the university’s Ethics Committee (approval no. 22030). All participants received detailed information regarding the study’s purpose, potential benefits, and associated risks, providing written informed consent prior to enrolment.
Participants underwent assessments at four distinct time points: baseline (M0), immediately after the intervention (M1), six months post-intervention (M2), and 12 months post-intervention (M3). The follow-up period consisted of two evaluations spaced six months apart.
For this analysis, only participants from the intervention group (IG) were included. Participants in the control group (CG) were placed on a waiting list at baseline (M0) to be enrolled in future research projects after the intervention, which excluded them from the current investigation.
The research committee overseeing the project recommended against the use of the term detraining, traditionally associated with a deliberate or imposed reduction PA over a defined timeframe. Instead, IG participants were encouraged to sustain their PA or engage in new exercise programs throughout the 12-month follow-up period.
Participants
The present study focused exclusively on the participants who completed the 12-month follow-up assessment. As a result, the sample consisted of 36 older adults (mean age, 69.33 ± 3.12 years). After the follow-up, participants were categorized into two groups based on their PA, assessed by the International Physical Activity Questionnaire–Short Form (IPAQ-SF): the light activity group (LAG, N = 20, mean age, 70.00 ± 3.66 years) and the moderate-to-vigorous activity group (MVAG, N = 16, mean age, 68.50 ± 2.09 years). The general characteristics of the sample at baseline are presented in Table 1.
To qualify for inclusion in the study, participants needed to meet the following criteria: (a) be at least 65 years old; (b) walk independently without assistance; and (c) perform daily living activities autonomously. Exclusion criteria included having a diagnosis of diabetes or uncontrolled cardiac disease, undergoing surgery within the past six months, or living with an active oncological condition.
To enhance methodology transparency, we have included a supplementary Excel spreadsheet developed by Cheng27, which provides anonymized participant responses across the four assessment time points (M0, M1, M2, and M3). This file also contains the full set of standardized IPAQ-SF scoring criteria used to categorize participants into light, moderate, and vigorous PA levels, allowing readers to review and replicate the classification process in detail.
Procedures
All assessments were conducted in the morning over two consecutive days. On the first day, anthropometric measurements were taken, while the second day was dedicated to assessing RTD and completing the Falls Efficacy Scale–International (FES-I) questionnaire. To ensure consistency, a single researcher carried out all measurements following the same sequence for each participant.
Measurements
Rate of torque development
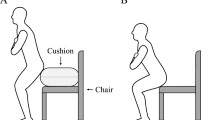
The RTD was measured by an isokinetic dynamometer (Biodex® System 3, Biodex Corp., Shirley, New York, USA), which was configured and calibrated according to the manufacturer’s guidelines and a previous study28. Participants were seated with the lateral femoral epicondyle aligned with the lever arm’s rotation axis, maintaining both the knee and hip angles at 90º. Straps were used to secure participants around their hips and shoulders to maintain this position during muscle contractions, while the evaluated leg was firmly fixed to the lever arm. Initially, the participants were asked to relax to register the passive effect of gravity acting on the limb. Standardized verbal encouragement was provided during the assessment to motivate participants to exert maximal effort.
Before the measurement, the participants walked for 10 min at their fastest pace to warm. They then performed 10 repetitions at 210º/s to familiarize themselves with the equipment and minimize errors in subsequent repetitions. After the familiarization phase, three maximal isokinetic strength repetitions of the knee extensors (KE) and flexors (KF) were performed during concentric actions at 60º/s within a knee joint range of motion from 90º to 10º flexion (0º representing full KE) on both the dominant (DS) and non-dominant side (NDS). For RTD calculation, the torque–time curves from the three repetitions at 60º/s were analyzed.
The raw torque signal was measured in Nm, sampled at a rate of 100 Hz, and then subjected to a low-pass filter (Butterworth, 6 Hz, 2nd order). RTD is defined as the slope of the torque‒time curve13, during the following intervals after torque onset: 0–30 ms, 0–60 ms, 0–80 ms, 30–60 ms, 30–80 ms and 60–80 ms (RTD0–30, RTD0–60, RTD0−80, RTD30–60, RTD30–80, and RTD60–80). Torque onset was determined as the moment when the torque value reached 5 Nm. For statistical analysis, the trial yielding the highest RTD value within the 0 to 80 ms timeline was selected. Considering that repetition, all remaining RTD values for the time intervals were subsequently considered for analysis. RTD and its time intervals were analyzed via a custom routine developed with MathWorks software (Natick, Massachusetts, USA).
Falls efficacy scale-international
The FES-I questionnaire29 was used to evaluate participants’ concerns about falling during both basic and more demanding physical and social activities. This study employed the Portuguese version, translated from the Prevention of Falls Network Europe version30 and validated by Figueiredo and Santos31.
The questionnaire is divided into three sections based on activity type and includes 16 items. Each of them rated on a scale from one (not concerned at all) to four (very concerned). Scores from all items are summed up to produce a total score ranging from 16 to 64, with higher scores reflecting a greater fear of falling.
Physical activity
Participants’ PA levels were evaluated using the IPAQ-SF32,33, which collects information on multiple aspects of activity, including the frequency (days/week) and duration (minutes/week) of walking, moderate, and vigorous activities, as well as total PA expressed in MET-minutes/week. Additionally, sitting time during weekdays and weekends was recorded.
Based on their answers, which can be consulted in the supplementary Excel spreadsheet developed by Cheng27, participants were then categorized into light, moderate, or vigorous activity levels (as detailed in supplementary file as Table S1). In this file it is possible to note what are the criteria to divide the sample in these groups (the participants with moderate were merged with participants with high levels). In addition, participants were asked to report the main activities they had carried out in the last six months (i.e., from six- to the 12-month follow-up) [Table S2 in the supplementary file].
Anthropometric
Anthropometric assessments included measuring weight and height by an electronic scale (TANITA®, MC 780MA, Amsterdam, Netherlands) and a stadiometer (SECA® 220, Hamburg, Germany), respectively. Body mass index (BMI) was subsequently calculated via the standard formula: BMI = body mass (kg)/height2 (m2).
High-speed resistance training protocol
The HSRT program was performed three times weekly for 16 weeks under supervision. The prescription was adjusted every two weeks. Each session consisted of an initial warm-up (10 to 15-minute), the main HSRT exercises (45 to 55-minute), and a concluding cool-down phase (5 to 10-minute). The main phase included the following upper- and lower-body exercises: squats on smith machine or with dumbbells (depending on each participant’s ability); leg press, leg extension; calf raise; seated row; peck fly; lat pull down; and incline bench press (Technogym, SPA, Cesena, Italy).
This present training protocol employs progressively increasing loads, tailored to the participants’ mean concentric phase velocity for each set across all exercises34,35: 1st to 4th weeks, an average speed over 1.3 m/s was required (starting strength); from the 5th to 10th weeks, speeds were adjusted to between 1.3 and 1.0 m/s (speed/strength); and in the 11th to 16th weeks, speeds ranged from 1.0 to 0.75 m/s (strength/speed). The mean concentric phase velocity for each set and exercise was monitored using a BEAST™ sensor (Beast Technologies, Brescia, Italy)36. This device provided real-time feedback on instantaneous velocity to both participants and supervisors and displayed the mean velocity at the end of each set. Each session used six accelerometers connected via Bluetooth to six separate cell phones. Participants were also actively encouraged to execute each repetition swiftly and explosively, while maintaining a controlled pace of 2–3 s during the eccentric phase.
Statistical analysis
Prior to the study, a sample size calculation was performed via G-power software (University of Dusseldorf, Germany)37 for F tests through ANOVA, repeated measured, within factors: f = 0.25, α error probability = 0.05, power (1-β err prob) = 0.80, number of groups = 1, and number of measurements = 4. The resulting power analysis indicated that this clinical trial should include at least 24 participants to achieve an 82% chance of successfully rejecting the null hypothesis. All statistical analyses were conducted using SPSS for Windows, version 26 (IBM Corp., Armonk, NY, USA), with the significance level set at p ≤ 0.050 (two-tailed). To complement traditional null hypothesis significance testing, an estimation-based analytical approach was employed38,39.
To evaluate the time effect across the four measurement points for each measure, repeated measures ANOVA were applied. Pairwise comparisons between time points and groups were conducted using the Bonferroni post-hoc test. The effect sizes (ESs) were then calculated according to Cohen40, using Cohen’s dunbiased (dunb) through a specific spreadsheet38. While the ESs for ANOVA were expressed as partial eta-squared values (ηp2) and interpreted using the following thresholds: 0.010–0.059 (small), 0.060–0.140 (medium), and greater than 0.140 (large), the pairwise comparisons’ ESs, expressed as dunb, were categorized as: less than 0.20 (trivial), 0.20–0.49 (small), 0.50–0.80 (medium), and greater than 0.80 (large). Graphical data representations were generated created using RStudio software.
Results
Participants
The participants’ general characteristics at all time points of the study are presented in Table 2. Several significant differences were observed in age, weight, and BMI over the study period.
Rate of torque development
Table 3 shows the changes in RTD values over the study period for KE. Several RTD values and their time intervals demonstrated medium to large time effect throughout the study period.
Table 3 also presents the interaction effects both within and between groups. Although no significant between-group differences were observed, several significant within-group changes were identified over time.
First, for RTDPEAK during KE-DS, both groups demonstrated significantly lower values at baseline compared to post-intervention (LAG: p = 0.002, dunb=0.95 [0.45 to 1.52]; MVAG: p = 0.003, dunb=0.66 [0.22 to 1.15]), six-month (LAG: p = 0.001, dunb=0.89 [0.48 to 1.37]; MVAG: p = 0.001, dunb=0.68 [0.24 to 1.18]), and 12-month follow-up (LAG: p = 0.018, dunb=0.76 [0.28 to 1.29]; MVAG: p = 0.007, dunb=0.69 [0.19 to 1.24]). Moreover, during KE-NDS, both groups exhibited significantly lower values at baseline compared to post-intervention (LAG: p < 0.001, dunb=1.19 [0.70 to 1.76]; MVAG: p = 0.001, dunb=0.53 [0.26 to 0.84]), six-month (LAG: p < 0.001, dunb=0.87 [0.46 to 1.33]; MVAG: p = 0.030, dunb=0.35 [0.12 to 0.62]), and 12-month follow-ups (LAG: p < 0.001, dunb=0.92 [0.45 to 1.45]; MVAG: p = 0.001, dunb=0.60 [0.27 to 0.98]).
Table 4 shows the changes in RTD values over the study period for KF. Several RTD values and their time intervals demonstrated medium to large time effect throughout the study period.
For RTDPEAK during KF-DS, both groups revealed significantly lower values at baseline compared to post-intervention (LAG: p = 0.006, dunb=0.49 [0.22 to 0.81]; MVAG: p = 0.013, dunb=0.76 [0.17 to 1.41]), six-month (LAG: p = 0.002, dunb=0.63 [0.31 to 0.98]; MVAG: p = 0.003, dunb=0.86 [0.26 to 1.54]), and 12-month follow-ups (LAG: p = 0.031, dunb=0.49 [0.13 to 0.89]; MVAG: p = 0.021, dunb=0.73 [0.22 to 1.29]). Lastly, during KF-NDS, both groups revealed significantly lower values at baseline than post-intervention (LAG: p = 0.001, dunb=1.28 [0.55 to 2.08]; MVAG: p = 0.031, dunb=0.68 [0.21 to 1.20]), six-month (LAG: p = 0.017, dunb=1.32 [0.65 to 2.08]; MVAG: p = 0.014, dunb=0.61 [0.09 to 1.18]), and 12-month follow-ups (LAG: p = 0.004, dunb=1.37 [0.74 to 2.09]; MVAG: p = 0.017, dunb=0.66 [0.09 to 1.28]). For clarity, we report here only the results for KE and KF for RTDPEAK. The results for the RTD time intervals, as indicated in Tables 3 and 4, are provided in the supplementary file. Figure 1 illustrates the changes in KE and KF for both sides of RTDPEAK.
Falls efficacy scale-international
Table 5 presents the changes in fear of falling across the four measurement points.
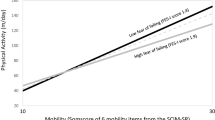
Although a significant time effect was observed during the study period, no significant differences were identified either between or within the groups. Figure 2 illustrates the fear of falling pattern over the study period for both groups.
Discussion
This exploratory study examined whether different PA levels influenced the long-term retention of improvements in RTD achieved through a 16-week HSRT program in independent older adults, assessed over a 12-month follow-up period. Additionally, changes in fear of falling over time were analyzed. The key findings were as follows: (i) regardless of PA levels, the RTDPEAK values for KE and KF remained significantly higher at the 12-month follow-up than baseline [small to large ESs] (Fig. 1); (ii) except for RTDPEAK values for KF-DS, the MVAG participants showed higher values at the 12-month follow-up compared to the LAG [small ESs]; (iii) the MVAG also exhibited a greater ability to generate force in the early phases of contraction (i.e., RTD0–30, RTD0–60) at the 12-month follow-up compared to the LAG [trivial to medium ESs]; and (iv) both groups demonstrated an improvement in their fear of falling values at the 12-month follow-up compared to baseline [LAG: medium ES; MVAG: large ES]. These findings are clinically meaningful, as older adults with reduced muscle power often struggle to rapidly generate sufficient torque or force to restore postural control in response to perturbations41. This underscores the importance of prioritizing muscle power, particularly RTD, in interventions within this population.
It is important to highlight that, unlike previous studies examining detraining effects on RTD in older adults11,15,17, which associated these effects with the absence of exercise stimuli, this study focused on sustaining lifestyle habits to address ethical concerns26, encouraging participants to maintain or increase their PA levels post-intervention. As detailed in Supplementary Table S2, ten participants started new exercise programs during the follow-up period.
This study presents clinically meaningful and sustained improvements in RTDPEAK for both groups, sustained from baseline to the 12-month follow-up. Specifically, KE-DS improved by 29% and 32% for the LAG and MVAG, respectively, while KF-DS improved by 31% and 38%. Similarly, substantial increases were noted for the NDS. While KE enhanced by 30% and 28% for the LAG and MVAG, respectively, the KF increased 39% and 30%, respectively. These improvements align with the thresholds established by Kirn et al.42, who defined clinically meaningful leg-extensor power effects as 9% to 10%, and substantial improvements as 15% to 18% in mobility-limited older adults. While this study focused on independent older adults, the findings suggest that HSRT could be an effective strategy to mitigate and prevent age-related neuromuscular decline.
Additionally, previous research suggests that RT programs lasting more than 12 weeks, particularly those incorporating explosive movements and controlled velocity, may minimize losses in neuromuscular function following intervention cessation11,14,16. In this study, the use of accelerometers to ensure adherence to specific velocity zones during HSRT may have contributed to reverse (or delay) the decline in the ability to rapidly develop force in these participants. Future studies should compare the long-term effects of traditional RT and HSRT to elucidate the potential role of contraction velocity in preserving neuromuscular function.
Nevertheless, PA levels played a critical role in preserving RTDPEAK effects. Over the study period (M0 vs. M3), participants who substantially reduced their PA after post-intervention experienced declines of 2% in both KE-DS and KF-DS, with greater reductions on the NDS, 6% and 5%, respectively. In contrast, the MVAG maintained their performance. These findings align with the results of Mertz et al.19, who reported that participants who continued RT at least once per week presented a better preservation in force development values [small ES] over six months. Moreover, the MVAG’s superior ability to generate torque within shorter time intervals (in the supplementary file as Fig. S1 to S4), suggests a more economical neuromuscular system43, which is critical for fall prevention44.
On the other hand, the previous studies which have focused on detraining effects have reported inconsistent results in RTD values following RT interventions. While Sakugawa et al.17 and Lovell et al.15 observed decreases over four-month and one-month follow-ups, respectively, Baxter et al.11 found greater retention of training-induced improvements over three months. In addition, the 12-month follow-up data for LAG suggest a more pronounced decline compared to Reid et al.45, who reported significant three-year reductions of 9% and 8% in muscle power, and 8% and 13% in contraction velocity, in healthy and mobility-limited older adults. These findings are practically significant, as potential losses in force production can lead to reductions in functional capacity6, and, ultimately, an increased risk of falls7. Participants who discontinued at least moderate PA and RT at least once weekly may experience neuromuscular impairments, including selective atrophy of the largest and fastest-contracting muscle fibers46, increased antagonist muscle co-contraction47, and accelerated demyelination impairing neural transmission of motor commands48.
In addition to these results, the fear of falling was assessed as a secondary aim using the FES-I, which is the most widely used questionnaire in this population49. The results demonstrated a significant main benefit time effect [large ES] across the study period for all participants, irrespective of PA levels (Table 5). Within-group analyses also revealed improvements in both groups from baseline to the 12-month follow-up [LAG: medium ES; MVAG: large ES]. These improvements may be related to the observed enhancements in neuromuscular function (M0 vs. M3). Indeed, recent systematic review findings49 suggest that a reduced concern about falling may be related to improvements in motor function. Moreover, the sustained benefits observed during the follow-up period provide valuable insights beyond a previous systematic review50, which highlighted uncertainty regarding the sustainability of intervention effects after cessation. The medium-to-large ESs observed in this study are clinically relevant, as fear of falling is significantly associated with the occurrence of falls in the previous month or year51. These findings underscore the importance of addressing fear of falling in future research.
Despite the insights provided, the present study presents some limitations that warrant consideration. First, although a priori power analysis indicated that a sample of 24 participants would be sufficient to detect meaningful effects with 82% power, the final sample sizes in subgroup analyses may limit the generalizability of the findings. Second, PA levels were assessed using the IPAQ-SF, a validated tool32,52, but it relies on self-reported and may be subject to recall bias and overestimation, namely among older adults. While objective tools such as accelerometers could improve measurement accuracy, their higher cost may limit feasibility. Third, the assessor was aware of the study’s objectives, which may have introduced bias through expectancy effects. Lastly, caloric intake was not controlled during the follow-up period, which could have influenced the outcomes.
Conclusions
The findings of this study emphasize that the improvements in RTD and fear of falling scores achieved through the 16-week HSRT program were sustained over a 12-month follow-up period. Importantly, the results also suggest that maintaining moderate-to-vigorous PA levels post-intervention further enhanced the retention of neuromuscular benefits and contributed to a more efficient neuromuscular system, which is critical for fall prevention. In addition, the reduction in fear of falling observed across all participants, regardless of PA levels, suggests a link to the improvements in neuromuscular function.
Implications for practice
Given the importance of maintaining RTD in older adults to effectively respond to perturbations and reduce the risk of falls, and considering that the RTD improvements observed in this study exceeded established thresholds for clinically meaningful changes42, it is essential to implement health policies that promote active aging and neuromuscular health. These policies should also encourage collaboration between healthcare and exercise professionals to conduct longitudinal assessments of key health parameters, such as RTD, in clinical and community health settings. Additionally, practitioners should be aware of the potential influence of PA levels on long-term retention of training effects.
For future research, we recommend comparing traditional RT and HSRT programs to better understand the role of contraction velocity in preserving neuromuscular function in older adults, with consideration of PA levels during the follow-up period. Importantly, future studies should also examine the relationship between RTD and functional outcomes, such as balance and gait performance, to enhance clinical applicability. Finally, evaluating the magnitude and sustainability of RTD adaptations after exercise cessation, followed by the reintroduction of HSRT, could offer valuable insights into optimal program design for older adults.
Data availability
Data available on request from the corresponding author.
References
Harman, D. The aging process. Proc. Natl. Acad. Sci. 78, 7124–7128 (1981).
Ballak, S. B., Degens, H., de Haan, A. & Jaspers, R. T. Aging related changes in determinants of muscle force generating capacity: A comparison of muscle aging in men and male rodents. Ageing Res. Rev. 14, 43–55 (2014).
Lexell, J., Taylor, C. C. & Sjöström, M. What is the cause of the ageing atrophy? Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15- to 83-year-old men. J. Neurol. Sci. 84, 275–294 (1988).
Kostka, T. Quadriceps maximal power and optimal shortening velocity in 335 men aged 23–88 years. Eur. J. Appl. Physiol. 95, 140–145 (2005).
Korff, T., Newstead, A. H., Van Zandwijk, R. & Jensen, J. L. Age- and activity-related differences in the mechanisms underlying maximal power production in young and older adults. J. Appl. Biomech. 30, 12–20 (2014).
Thompson, B. J. et al. Age-related changes in the rate of muscle activation and rapid force characteristics. Age 36, 839–849 (2014).
Hu, B. et al. Lower quadriceps rate of force development is associated with worsening physical function in adults with or at risk for knee osteoarthritis: 36-month follow-up data from the osteoarthritis initiative. Arch. Phys. Med. Rehabil. 99, 1352–1359 (2018).
Kamo, T. et al. Rate of torque development and the risk of falls among community dwelling older adults in Japan. Gait Post. 72, 28–33 (2019).
Izquierdo, M. et al. International exercise recommendations in older adults (iCFSR): Expert consensus guidelines. J. Nutr. Health Aging 25, 824–853 (2021).
Izquierdo, M. et al. Global consensus on optimal exercise recommendations for enhancing healthy longevity in older adults (ICFSR). J. Nutr. Health Aging 29, (2025).
Baxter, B. A., Baross, A. W., Ryan, D. J. & Kay, A. D. Effects of detraining on neuromuscular function and structural adaptations following once- or twice-weekly eccentric resistance training in older adults. Aging Clin. Exp. Res. 36, 177 (2024).
Fragala, M. S. et al. Resistance training for older adults: position statement from the national strength and conditioning association. J. Strength Cond. Res. 33, 2019–2052 (2019).
Maffiuletti, N. A. et al. Rate of force development: physiological and methodological considerations. Eur. J. Appl. Physiol. 116, 1091–1116 (2016).
Andersen, L. L., Andersen, J. L., Zebis, M. K. & Aagaard, P. Early and late rate of force development: Differential adaptive responses to resistance training?. Scand. J. Med. Sci. Sports 20, e162–e169 (2010).
Lovell, D. I., Cuneo, R. & Gass, G. C. The effect of strength training and short-term detraining on maximum force and the rate of force development of older men. Eur. J. Appl. Physiol. 109, 429–435 (2010).
Walker, S., Peltonen, H. & Häkkinen, K. Medium-intensity, high-volume “hypertrophic” resistance training did not induce improvements in rapid force production in healthy older men. Age 37, 41 (2015).
Sakugawa, R. L. et al. Effects of resistance training, detraining, and retraining on strength and functional capacity in elderly. Aging Clin. Exp. Res. 31, 31–39 (2019).
Douda, H. T., Kosmidou, K. V., Smilios, I., Volaklis, K. A. & Tokmakidis, S. P. Community-based training–detraining intervention in older women: a five-year follow-up study. J. Aging Phys. Act. 23, 496–512 (2015).
Mertz, K. H. et al. Changes in muscle mass and strength during follow-up after one-year resistance training interventions in older adults. J. Strength Cond. Res. 37, 2064–2070 (2023).
Snijders, T., Leenders, M., de Groot, L. C. P. G. M., van Loon, L. J. C. & Verdijk, L. B. Muscle mass and strength gains following 6 months of resistance type exercise training are only partly preserved within one year with autonomous exercise continuation in older adults. Exp. Gerontol. 121, 71–78 (2019).
Bernstein, M. S., Morabia, A. & Sloutskis, D. Definition and prevalence of sedentarism in an urban population. Am. J. Public Health 89, 862–867 (1999).
Ramsey, K. A. et al. The association of objectively measured physical activity and sedentary behavior with skeletal muscle strength and muscle power in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 67, (2021).
Varo, J. J. et al. Distribution and determinants of sedentary lifestyles in the European Union. Int. J. Epidemiol. 32, 138–146 (2003).
Bosquet, L. et al. Effect of training cessation on muscular performance: A meta-analysis. Scand. J. Med. Sci. Sports 23, 85 (2013).
Buendía-Romero, Á., Vetrovsky, T., Estévez-López, F. & Courel-Ibáñez, J. Effect of physical exercise cessation on strength, functional, metabolic and structural outcomes in older adults: a protocol for systematic review and meta-analysis. BMJ Open 11, e2023 (2021).
Esmonde, K. Exercising caution: A case for ethics analysis in physical activity promotion. Public Health Ethics 16, 77–85 (2023).
Cheng, H. L. A simple, easy-to-use spreadsheet for automatic scoring of the International Physical Activity Questionnaire (IPAQ) Short Form (updated November 2016). (2016).
Parraca, J. A., Adsuar, J. C., Domínguez-Muñoz, F. J., Barrios-Fernandez, S. & Tomas-Carus, P. Test-retest reliability of isokinetic strength measurements in lower limbs in elderly. Biology 11, 802 (2022).
Yardley, L. et al. Development and initial validation of the falls efficacy scale-international (FES-I). Age Ageing 34, 614–619 (2005).
ProFaNE, S. Prevention of falls network europe. Ten step FES-I translation protocol. (2014).
Figueiredo, D. & Santos, S. Cross-cultural validation of the falls efficacy scale-international (FES-I) in Portuguese community-dwelling older adults. Arch. Gerontol. Geriatr. 68, 168–173 (2017).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395 (2003).
Hagströmer, M., Oja, P. & Sjöström, M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 9, 755–762 (2006).
Mann, B. Developing explosive athletes: Use of velocity based training in athletes (Ultimate Athlete Concepts, 2016).
Mann, B., Ivey, P. A. & Sayers, S. P. Velocity-based training in football. Strength Cond. J. 37, 52–57 (2015).
Vallejo, F. T., Chien, L. T., Hébert-Losier, K. & Beaven, M. Validity and reliability of the BeastTM sensor to measure movement velocity during the back squat exercise. J. Sport Exerc. Sci. 4, 100–105 (2020).
Faul, F., Erdfelder, E., Buchner, A. & Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 41, 1149–1160 (2009).
Cumming, G. & Calin-Jageman, R. Introduction to the new statistics: Estimation, open science, and beyond (Routledge, 2017).
Ho, J., Tumkaya, T., Aryal, S., Choi, H. & Claridge-Chang, A. Moving beyond P values: Data analysis with estimation graphics. Nat. Methods 16, 565–566 (2019).
Cohen, J. Statistical power analysis for the behavioral sciences (Lawrence Erlbaum Associates, 1988).
Clark, D. J. & Fielding, R. A. Neuromuscular contributions to age-related weakness. J. Gerontol. Ser. A 67, 41–47 (2012).
Kirn, D. R., Reid, K. F., Hau, C., Phillips, E. M. & Fielding, R. A. What is a clinically meaningful improvement in leg-extensor power for mobility-limited older adults?. J. Gerontol. Ser. A 71, 632–636 (2016).
Cadore, E. L. et al. Neuromuscular economy, strength, and endurance in healthy elderly men. J. Strength Cond. Res. 25, 997–1003 (2011).
Pijnappels, M., Van Der Burg, P., Reeves, N. & Van Dieën, J. Identification of elderly fallers by muscle strength measures. Eur. J. Appl. Physiol. 102, 585–592 (2008).
Reid, K. F. et al. Longitudinal decline of lower extremity muscle power in healthy and mobility-limited older adults: Influence of muscle mass, strength, composition, neuromuscular activation and single fiber contractile properties. Eur. J. Appl. Physiol. 114, 29–39 (2014).
Mosole, S. et al. Long-term high-level exercise promotes muscle reinnervation with age. J. Neuropathol. Exp. Neurol. 73, 284–294 (2014).
Schmitz, A., Silder, A., Heiderscheit, B., Mahoney, J. & Thelen, D. G. Differences in lower-extremity muscular activation during walking between healthy older and young adults. J. Electromyogr. Kinesiol. 19, 1085–1091 (2009).
Hourigan, M. L. et al. Increased motor unit potential shape variability across consecutive motor unit discharges in the tibialis anterior and vastus medialis muscles of healthy older subjects. Clin. Neurophysiol. 126, 2381–2389 (2015).
Savvakis, I., Adamakidou, T. & Kleisiaris, C. Physical-activity interventions to reduce fear of falling in frail and pre-frail older adults: A systematic review of randomized controlled trials. Eur. Geriatr. Med. 15, 333–344 (2024).
Kendrick, D. et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD009848.pub2 (2014).
Chen, W.-C., Li, Y.-T., Tung, T.-H., Chen, C. & Tsai, C.-Y. The relationship between falling and fear of falling among community-dwelling elderly. Medicine 100, e26492 (2021).
Grimm, E. K., Swartz, A. M., Hart, T., Miller, N. E. & Strath, S. J. Comparison of the IPAQ-Short Form and accelerometry predictions of physical activity in older adults. J. Aging Phys. Act. 20, 64–79 (2012).
Acknowledgements
We would like to express our sincere gratitude to all the participants for their willingness to take part in this study. Lastly, the authors would like to pay a public tribute of deep honor to Mr. Ribeiro†, a dedicated employee of the University’s sports center, who tragically and unexpectedly passed away recently due to a car accident. His unwavering support was invaluable throughout the pre-intervention, data collection, and intervention phase. Among his many contributions, Mr. Ribeiro† ensured the facilities were always accessible, even outside regular hours. He meticulously cleaned the spaces, painted the gym room before the intervention began, and regularly inspected and replaced the cables on the weight machines as needed. His commitment and efforts were deeply appreciated, and he will be greatly missed.
Funding
This work is funded by national funds through the Foundation for Science and Technology (FCT), I.P., under the following projects: UID/04923 – Comprehensive Health Research Centre, and 2021.04598.BD (https://doi.org/10.54499/2021.04598.BD).
João Paulo Brito and Rafael Oliveira are research members of the Research Centre in Sports Sciences, Health and Human Development which was funded by National Funds by FCT under the following project UI/04045. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Author information
Authors and Affiliations
Contributions
Alexandre Duarte Martins: Contributed to the study concept, data collection, statistical analysis, and table development; created the graphs and wrote the original draft. He was the only author with full access to all study data and was responsible for its integrity. João Paulo Brito, Orlando Fernandes and Nuno Batalha: Contributed to the study concept, supervised all data collection procedures, and actively reviewed the original draft. Bruno Gonçalves and Rafael Oliveira: Contributed to the statistical analysis, table and graph design, and actively reviewed the original draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participants
The research was carried out in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the University of Evora (code no. 22030). All participants read and signed an informed consent form outlining the study’s objectives, potential benefits, and risks.
Consent for publication
All participants provided authorization for the publication of their data, although no individual participant’s data is presented in this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duarte Martins, A., Paulo Brito, J., Fernandes, O. et al. Long-term effects on rate of torque development and fear of falling following high-speed resistance training in older adults. Sci Rep 15, 29139 (2025). https://doi.org/10.1038/s41598-025-09095-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09095-8