Abstract
The elimination of the latent viral reservoir remains the main barrier in the quest for a cure for people with HIV (PWH). The administration of latency reversal agents (LRA) at antiretroviral treatment (ART) initiation could improve the effectiveness of strategies aimed at HIV remission. This study assessed the impact of maraviroc (MVC), an antiretroviral drug with HIV latency reversal properties, on the viral reservoir size when it is administered at ART initiation. We conducted a longitudinal observational study in PWH initiating ART with a regimen including (MVC-initiation, n = 12) or not including MVC (non-MVC-initiation, n = 22), or switching to an MVC-containing regimen after achieving an undetectable viral load (VL) (MVC-switch, n = 9). The HIV reservoir size was determined via Alu-LTR and Intact Proviral DNA Assay (IPDA) methods, and cell-associated HIV-RNA (ca-HIV-RNA) by nested-qPCR. Comparative analyses employed mixed multivariate linear models. After a median of 90 weeks, the MVC-initiation group showed a greater reduction in integrated and IPDA-total (7.1- and 4.0-fold, respectively), but not IPDA-intact, HIV-DNA reservoir compared to the non-MVC-initiation group. The reductions in integrated, IPDA-total, and IPDA-intact HIV-DNA levels in the MVC-initiation group were also greater compared to the MVC-switch group (from 5.4 to 13.8-fold). Moreover, no significant differences in the HIV transcriptional activity, assessed by ca-HIV-RNA levels or HIV-RNA/HIV-DNA ratios, were observed between the MVC-initiation and non-MVC-initiation groups. In conclusion, starting ART with a drug with HIV latency reversing activity at detectable VL phase may contribute to a greater reduction in the HIV-DNA reservoir. These findings could inform the design of future trials targeting HIV remission via a “kick and kill” strategy.
Similar content being viewed by others
Introduction
Current antiretroviral treatment (ART) does not eradicate HIV infection, as latently infected cells remain persistently infected and unrecognized by the immune system, with minimal expression of HIV genes or proteins. HIV RNA typically rebounds in plasma within 2–3 weeks when ART is interrupted1,2, indicating that even long-term suppression of HIV-1 replication by ART fails to eliminate HIV-1. Some barriers to HIV eradication include: viral persistence in long-lived latent reservoirs, residual replication of HIV-1, homeostatic and/or antigen-driven clonal expansion of HIV-infected cells, and the presence of the virus in anatomical reservoirs 3,4,5. The inability of ART to eradicate HIV was first suggested by the demonstration of latent infection in resting CD4 + T cells6, and subsequently confirmed by the recovery of rare, integrated replication-competent HIV from the resting CD4 + memory T cells of people with HIV (PWH) receiving ART7. The evidence suggests that the resting T-cell reservoir is established early after infection and is extremely stable, contributing to viral persistence8. The persistence of quiescent HIV infection, primarily within central memory CD4 + T cells, is currently the major obstacle to the eradication of HIV infection9.
Strategies for an HIV functional cure include the “kick and kill” approach, which involves the activation of the HIV proviral reservoir and the elimination of infected cells10. The administration of latency reversal agents (LRA) increases productive infection, with CD8 + cytotoxic cells eliminating infected cells, whereas ART counteracts the formation of new virions and the subsequent infection of new host cells. Although some of these drugs have increased the HIV transcription in different clinical trials, they have generally failed to reduce the HIV reservoir size11,12,13,14. Most trials have administered LRAs under ART- suppressed viremia, where specific cytotoxic T lymphocyte activity against HIV-infected cells may be reduced. In addition, in the chronic phase, the reservoir harbors a high proportion of viral variants15 that escape humoral16 and cytotoxic activity17. Additionally, several of these drugs tested in clinical studies can cause side effects, leading to the discontinuation of the clinical trial18. Thus, additional approaches to improve the efficacy of this strategy are needed.
Some studies suggest that administering LRAs during active HIV replication may enhance their effectiveness. One study on SIV DNA turnover in resting CD4 + T cells proposed that anti-latency drugs work best during active viral replication19. Additionally, a mathematical model supports their use at ART initiation, when the viral load, CD4 + T cell activation, and latent cell turnover are high20. Additionally, the cytotoxic T-lymphocyte (CTL) response is stronger in viremic patients than in those on ART with a suppressed viral load (VL)21. In people on suppressive ART, the frequency of CTLs against HIV is at least 10 times lower than before ART22,23.
Maraviroc (MVC) is an antiretroviral drug that inhibits the binding of the virus to the CCR5 co-receptor. Our group has shown that MVC can also activate NF-κB and subsequently induce latent HIV-1 transcription in resting CD4 + T cells from HIV-1-infected individuals on suppressive ART24. MVC has been shown to have a potency similar to or greater than that of other LRAs in vitro, including bryostatin-1, a potent PKC agonist25. Thus, current evidence suggests that MVC is a potential HIV latency reversal drug that could counteract HIV-1 persistence, and further research is needed to support this potential dual effect.
This study aims to test the hypothesis that the impact of administering a drug with a potential HIV latency reversing effect, such as MVC, during the initiation of ART and the viral phase of HIV infection on the HIV reservoir size is greater than when MVC is administered to individuals with suppressed viremia under ART.
Material and methods
Patients and clinical statement
We conducted a longitudinal study of HIV-1 infected adults selected from the CORIS Biobank (Madrid, Spain). The CoRIS is an open, prospective, multicenter cohort of confirmed HIV-infected adults, recruited since 2004. All participants provided written informed consent prior to enrollment in the study. Data follow the HIV Cohorts Data Exchange Protocol (HICDEP) with annual quality controls. The study protocol was approved by the Research Ethics Committees of Instituto Ramón y Cajal de Investigación Sanitaria (20/070) and the CoRIS Review Board (RIS EPICLIN 07_2021), adhering to the Helsinki Declaration.
The participants were grouped as follows: (1) people with HIV (PWH) who started ART including MVC (MVC-Initiation), (2) PWH who started ART without MVC (non-MVC-Initiation), and (3) PWH under ART with undetectable VL who switched to an MVC-containing regimen (MVC-switch). The MVC-Initiation and non-MVC-Initiation groups were matched by age, sex, and the number and type of drugs in the ART regimen (excluding MVC).
Quantification of HIV integrated DNA levels
DNA was extracted from stored PBMCs using AllPrep DNA/RNA Mini Kit (Qiagen, Hilden, Germany), following manufacturer’s instructions. DNA extraction and PCR procedures were performed simultaneously in pre-ART and post-ART samples from each individual. The HIV reservoir was determined by measuring integrated proviral DNA in peripheral blood mononuclear cells (PBMC) by Alu-LTR method, as previously described26. Briefly, the first PCR was performed on 10 µL of DNA (500–1000 ng of DNA) on a conventional PCR machine (Primus 25 advanced®; Peqlab), with primers that anneal to Alu and HIV-LTR. The second PCR, using TaqMan detection (LightCycler480 qPCR, Roche) targeted the HIV-specific R and U5 regions within the HIV-LTR. A standard curve of integrated DNA from the 8E5 cell line was used as a control for absolute quantification of HIV DNA copies. Proviral HIV-1 DNA copy numbers were calculated relative to CCR5 gene copies and reported as copies per million CD4 + cells.
Intact proviral DNA assay (IPDA)
To determine the size of intact HIV DNA in the studied PWH, we performed IPDA via digital PCR technology, as described previously27. Each IPDA consisted of 2 multiplex digital droplet (dd) PCR (QX600 Droplet Digital PCR, System Bio-Rad) reactions: the HIV-1 discrimination reaction (distinguishing IPDA-intact from IPDA-defective proviruses) and the hRPP30 reaction (quantifying the DNA shearing and number of cells). For HIV-1 proviral discrimination reactions, a mean of 1 µg of genomic DNA was analyzed in each reaction well. For DNA shearing and copy number reference reactions, 25 ng of genomic DNA was analyzed in each reaction well. Both reactions were corrected by the DNA shearing index (under 0.5 every assay). The assay was performed for 6 replicates that were batch-processed and analyzed. The IPDA-total HIV-DNA was determined by the addition of intact and defective copies. CEM.NKRCCR5 cells were included as negative controls, whereas ACH-2 cells, which carry one single HIV provirus per cell, served as positive controls. The results were reported as the number of HIV-DNA copies per million CD4 + cells.
RNA extraction and reverse transcription
RNA was extracted from stored PBMCs using the AllPrep DNA/RNA Mini Kit (Qiagen, Hilden, Germany), following the manufacturer’s instructions. For cDNA preparation, 10 µL of RNA (100–1000 ng of total RNA) was reverse transcribed with the SuperScript IV Reverse Transcriptase kit (Invitrogen) in 20 μL of PCR mix, according to the manufacturer’s instructions. The combination of random hexamers and oligo-dT avoids bias toward specific RNA regions28. Control reactions included RNA from an HIV- negative donor (negative control) and a “no RT” control with patient RNA but no reverse transcriptase.
Evaluation of cell associated HIV-RNA
Cell associated HIV RNA (ca-HIV-RNA) was measured via seminested PCR. The cDNA was subjected to two rounds of PCR amplification. In the first round, on a Primus 25 advanced® PCR machine (Peqlab), 20 μL of PCR mix, containing 4 μL cDNA, dNTPs (250 μM), 300 μM each of the GAG1 and SK431 primers, and Platinum Taq Polymerase (Roche) was used. Cycling was 94 °C for 3 min, then 15 cycles of 94 °C 30 seg, 55 °C 30 seg and 72 °C 1 min. The second qPCR, performed on the LightCycler480 qPCR machine (Roche), used TaqMan detection with 2 μL of the first PCR product in 20 μL of PCR mix containing LightCycler480 Probes Master (Roche), 200 μM of GAG3 probe and each GAG1 and GAG2 primers. Cycling was 50 °C 2 min, 95 °C 10 min, followed by 45 cycles of 95 °C 15 seg and 60 °C 1 min29. Serial dilutions of 8E5 cell line standard (1 to 10,000 HIV copies) were used for absolute quantification. HIV-1 RNA copy numbers were standardized using glyceraldehyde phosphate dehydrogenase (GAPDH) and actin beta (ACTB) genes. Results were reported as ca-HIV-1 RNA copies per million CD4 cells. Primers and probes are listed in Supplementary Table 1.
Statistics
To estimate the changes of the primary variables over time (pre-ART/post-ART) and between groups, we used mixed linear regression models with treatment group, time (pre-ART/post-ART) and their interaction as covariates, adjusting by potential cofounding variables as baseline plasma HIV RNA copies and CD4 + T cell counts, due to the differences of these parameters among the study groups. HIV-DNA or ca-HIV-RNA per million CD4 + cells, and plasma HIV RNA were log10 transformed to meet linear assumptions. Effect size was reported as the difference in log10 HIV-DNA or HIV-RNA between the time points and groups, with back transformation indicating a fold-change in one group relative to the other (fold-decline, if the estimate was negative). Comparisons of the clinical and sociodemographic characteristics of PWH were performed via ANOVA or Chi-square tests. Statistical analyses were conducted with Stata v18 and graphs with GraphPad Prism v.9.5.1.
Results
Characteristics of PWH in the study groups
A total of 43 PWH were included in the study and categorized into three groups: MVC-Initiation (ART initiation including MVC, n = 12), non-MVC-Initiation (ART initiation without MVC, n = 22), and MVC-switch (on ART switched to an ART regimen including MVC, n = 9). In the MVC-switch group, the median switch time post-ART was 126 weeks [interquartile range (IQR): 100–257]. The median follow-up time from ART initiation (MVC-Initiation and non-MVC-Initiation) or ART switch (MVC-switch) was 90 weeks [IQR: 70–116].
Baseline clinical and sociodemographic characteristics are summarized in Table 1. Ninety-one percent (n = 39) of PWH were male, with MSM as the most prevalent transmission route (69.8%) and 76.7% born in Spain. The median age was 35 years [IQR: 25–43], with the MVC-switch group showing a higher age (46 years, IQR: 33–59) (p < 0.05). Compared with the other groups, the MVC-Initiation group had a greater viral load (median 661,150 copies/mL) and a lower CD4 + T-cell count (median of 96 cells/mm3) (p < 0.01). No significant differences in terms of sex, mode of transmission, region of origin, initial ART regimens or viral undetectability post-ART among the study groups were observed. The baseline clinical characteristics of MVC-switch group before ART initiation are provided at Supplementary Table 2.
The administration of MVC at ART initiation significantly reduces the HIV-DNA reservoir levels
We assessed the variation in integrated HIV-DNA levels using the Alu-LTR method. The integrated HIV-DNA levels decreased from 31,047 [IQR 299–207,228] to 502 [IQR 36–3226] copies per 106 CD4 cells in the MVC-Initiation group (33.1-fold reduction, p < 0.001), and from 7439 [IQR 514–37,425] to 2531 [IQR 191–8080] copies per 106 CD4 cells in the non-MVC-Initiation group (4.7-fold reduction, p < 0.001). For the MVC-switch group, integrated HIV-DNA levels decreased from 1335 [IQR 288–27,477] to 268 [IQR 156–3988] copies per 106 CD4 cells (6.2-fold reduction, p < 0.01) (Fig. 1).
Variation in the integrated HIV-DNA reservoir in the study groups. The HIV-DNA reservoir was determined in PBMCs and values were normalized according to CD4 percentage data. Values below 1 copy of integrated HIV-DNA/million PBMCs were considered as 1. Statistical analysis: mixed linear regression analysis (** p < 0.01; *** p < 0.001). The median CD4 counts were: (a) 96 and 367 at pre-ART in MVC-Initiation and non-MVC-Initiation groups, respectively; and 279 pre-MVC in the MVC-switch group; (b) 468 and 668 at post-ART in MVC-Initiation and non-MVC-Initiation groups, respectively; and 515 post-MVC in the MVC-switch group.
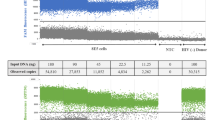
The HIV-DNA levels measured by IPDA followed a similar pattern. IPDA-total HIV-DNA levels decreased from 27,205 [IQR 7540–48,254] to 876 [IQR 195–10,071] copies per 106 CD4 cells in the MVC-Initiation group (17.0-fold reduction, p < 0.001), and from 3293 [IQR 1817–11,780] to 857 [IQR 446–1363] copies (4.3-fold reduction, p < 0.001) in the non-MVC-Initiation group (Fig. 2A). IPDA-defective HIV-DNA levels decreased from 17,783 [IQR 1355–30,053] to 762 [IQR 182–4498] copies per 106 CD4 cells in the MVC-Initiation group (6.0-fold reduction, p < 0.05), and from 2070 [IQR 1089–7318] to 649 [IQR 390–1227] copies per 106 CD4 in the non-MVC-Initiation group (3.2-fold reduction, p < 0.05) (Fig. 2B). IPDA-intact HIV-DNA levels decreased from 9422 [IQR 1313–26,654] to 89 [IQR 35–503] copies per 106 CD4 in the MVC-Initiation (52.5-fold reduction, p < 0.001), and from 780 [IQR 250–1223] to 39 [IQR 5–140] copies per 106 CD4 in the non-MVC-Initiation group (15.5-fold reduction, p < 0.001) (Fig. 2C). In the MVC-switch group, the levels of IPDA-intact showed a 3.8-fold reduction (p < 0.05).
Variation in the IPDA-total, IPDA-defective and IPDA-intact HIV-DNA reservoir in the study groups. The HIV proviral DNA levels: (A) IPDA-total, (B) IPDA-defective and (C) IPDA-intact, were determined in PBMCs and values were normalized according to CD4 percentage data. Values below 1 copy of HIV-DNA/million PBMCs were considered as 1. Statistics: mixed linear regression analysis (* p < 0.05; *** p < 0.001, n.s.: not significant). The median CD4 counts were: a) 92 and 369 at pre-ART in MVC-Initiation and non-MVC-Initiation groups, respectively; and 279 pre-MVC in the MVC-switch group; b) 486 and 677 at post-ART in MVC-Initiation and non-MVC-Initiation groups, respectively; and 515 post-MVC in the MVC-switch group.
We compared the variation in the HIV-DNA reservoir between the groups. We noted that the MVC-Initiation group displayed greater reductions in all the forms of HIV-DNA evaluated (Supplementary Table 3). Specifically, the MVC-Initiation group had a 7.1- and 4.0-fold greater decline in the integrated and IPDA-total HIV reservoir, respectively, compared to the non-MVC-Initiation group (p < 0.05). Additionally, the MVC-Initiation group showed a greater decline in integrated (5.4-fold), total (9.1-fold) and intact (13.8-fold) HIV-DNA levels compared to the MVC-switch group (p < 0.05), and lower differences were detected when the non-MVC-Initiation group was compared with the MVC-switch group (Table 2). Taken altogether, these results suggest that the administration of MVC has a greater impact on the HIV reservoir when it is administered at the initiation of ART during the active viral replication phase.
Evaluation of the HIV transcriptional activity during initial ART and ART-switching containing or not MVC
To assess MVC’s effect on HIV transcriptional activity, we measured the cell-associated HIV RNA (ca-HIV-RNA) levels in each study group. Before ART initiation, the ca-HIV-RNA levels were 190,598 [IQR 34,433–3,540,000] copies per 106 CD4 cells in the MVC-Initiation group and 25,110 [IQR 586–129,459] copies in the non-MVC-Initiation group. After ART initiation, similar reductions were observed in both groups: MVC-Initiation had 291 [IQR 24–2477] copies per 106 CD4 cells (912-fold reduction) and non-MVC-Initiation had 55 [IQR 0–426] copies (891-fold reduction) (p < 0.001), which indicates no differences between these groups (Fig. 3A, Supplementary Table 4). These results suggest that ART initiation significantly reduces ca-HIV-RNA levels, regardless of LRA administration, masking any potential impact of the LRA on transcriptional activity in this context. However, no significant changes were observed in ca-HIV-RNA before or after MVC inclusion in the MVC-switch group (Fig. 3A).
Variation in the HIV transcriptional activity among the study groups. (A) Values were normalized according to CD4 percentage data. (B) Ratio HIV-RNA/HIV-DNA (ca-HIV-RNA/ HIV-DNA). Ratio of 5 × 10–4 was considered the minimum value in MVC-Initiation and non-MVC-Initiation groups, and 1 × 10–4 was considered the minimum value in the MVC-switch group. Statistics: mixed linear regression analysis (**** p < 0.0001, n.s.: not significant).
We further analyzed the HIV-RNA/HIV-DNA ratio. The non-MVC-Initiation presented a 162-fold reduction, which was higher than the 60-fold reduction in the MVC-Initiation group (Fig. 3B). In addition, despite a trend toward an increase, there were no consistent effects on the HIV transcriptional activity levels in the MVC-switch group. The non-MVC-Initiation group showed a greater decline of the HIV-RNA/HIV-DNA ratio than MVC-Initiation when compared with the MVC-switch group (562-fold vs 209-fold, respectively) (Supplementary Table 5), suggesting a higher transcriptional activity in the initial MVC-containing regimen.
Discussion
The primary aim of HIV cure strategies is to eliminate or reduce the viral reservoir. Among the approaches evaluated, use of drugs with HIV latency reversal activity to activate HIV transcription10, has generally failed to significantly reduce the HIV reservoir in most clinical trials. A proposed improvement is the administration of these drugs during the viral phase of infection, at ART initiation. Untreated HIV is characterized by a pro-inflammatory environment due to high antigen load and microbial translocation30, activating T cells through T-cell receptors and toll like receptors (TLRs), as well as through proinflammatory cytokines31. Factors such as bacterial products32, TLR ligands14,20,33, and proinflammatory cytokines34 may facilitate HIV latency reversion. Additionally, the CD8 cytotoxic response is stronger in acute than in chronic HIV infection35. Therefore, the inflammatory state at ART initiation could enhance LRA effectiveness, potentially boosting both latent virus reactivation and the cytotoxic response to eliminate infected cells.
We conducted a longitudinal study involving PWH who initiated ART with MVC (MVC-Initiation) or without MVC (non-MVC-Initiation), and those who switched to an MVC-containing regimen during the undetectable VL phase (MVC-switch). To quantify the HIV-DNA, we employed both the Alu-LTR and IPDA methods—classical qPCR-based and novel dPCR-based approaches, respectively—which may offer complementary insights into the HIV reservoir size. In initial therapy, the MVC-Initiation group showed a greater reduction in HIV-DNA, particularly in integrated and total HIV-DNA, possibly related to effective reactivation of the latent provirus by MVC. This observation showing a similar decline pattern in both determinations is interesting, despite the fact that differences on the levels of the HIV-DNA levels may be detected among the methods for viral reservoir quantification36. However, despite a trend on the higher reduction of the intact HIV-DNA that was observed in the MVC-Initiation group, no significant differences were observed in comparison with non-MVC-Initiation group, because it may be more challenging to detect an impact on the size intact reservoir, which is correlated with levels of the replication-competent viruses37.
The key findings from this study stem from the comparison of the two groups that received MVC. The impact of MVC as an LRA on the viral reservoir size in PWH with undetectable viral loads was limited. Concurrent LRA administration with initial ART during active HIV replication may result in a greater HIV-DNA reservoir reduction. We observed that differences in HIV reservoir reduction are more pronounced when comparing the MVC-switch group to the MVC-Initiation group than to the non-MVC-Initiation group, noting a higher impact on the intact viral reservoir (Figs. 1 and 2, Table 2). Therefore, the results suggest that MVC at ART initiation may be more effective, possibly due to enhanced HIV reactivation and/or cytotoxic activity during this phase19,20, suggesting a limited efficacy for strategies targeting the HIV reservoir during the undetectable VL phase. Understanding these timing differences and confirming findings with other LRAs of varying potency are essential.
To explore MVC’s latency-reversing effects, we measured the levels of cell-associated HIV RNA (ca-HIV RNA) as an indicator of viral transcription. In vitro studies have shown that MVC significantly induces HIV transcription in CD4 T cells at non-toxic concentrations25 without altering activation or metabolic parameters38. In the MVC-Initiation and non-MVC-Initiation groups, we observed a decrease in ca-HIV-RNA (approximately 900-fold reduction) as could be expected, due the antiviral activity of ART on high baseline ca-HIV-RNA (> 25,000 copies) (Fig. 3A). No significant variation in ca-HIV-RNA levels or the HIV RNA/DNA ratio among these groups was observed, suggesting the ART’s initial potency could mask differences in viral transcription between the LRA and non-LRA regimens.
Study limitations include its observational nature and group differences, particularly in CD4 counts and plasma HIV-RNA levels, which we mitigated by multivariate analysis adjustments. Likewise, the limited availability of samples hinders the evaluation of viral reservoir dynamics over a longer post-ART follow-up period and limits deeper investigation into the mechanisms involved. Also, prior trials have shown limited benefits of intensified regimens on viral reservoir reduction, including MVC39,40,41 or not including it in the ART regimen42,43. However, most of these studies have evaluated only one form of HIV-DNA, limiting comparisons with our study and precluding definitive conclusions. Our results showing that the MVC-Initiation group displayed higher decreases in several forms of HIV-DNA is according with a prior study showing that addition of MVC in early integrase inhibitor-based treatment results in faster reduction of 2-LTR newly infected cells and a modest reduction in total reservoir size44. Thus, although the MVC-Initiation group received additionally MVC in the ART regimen, we attribute the outcomes to its latency-reversal effects rather than the number of drugs in the regimen. Previous in vitro studies have shown that MVC’s latency-reversal effect is stronger at higher doses than those used therapeutically25,45, so it is plausible that a greater effect on the HIV-DNA reservoir decline could be observed if MVC were administered at higher doses. Finally, although the inclusion of MVC shows potential benefits in reducing the HIV reservoir, further research is needed to improve the effect of drugs with latency reversing effect on the intact HIV-DNA size.
In conclusion, our findings suggest that initiating ART with an LRA may more effectively reduce HIV reservoir size than administration during the undetectable VL phase. These findings may guide clinical trials focused on “kick and kill” strategies aimed to the HIV eradication, with further studies needed to confirm these outcomes and clarify the mechanisms involved.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Fischer, M. et al. HIV RNA in plasma rebounds within days during structured treatment interruptions. AIDS 17(2), 195–199. https://doi.org/10.1097/00002030-200301240-00009 (2003).
Li, J. Z. et al. Time to viral rebound after interruption of modern antiretroviral therapies. Clin. Infect. Dis. 74(5), 865–870. https://doi.org/10.1093/cid/ciab541 (2022).
Kwon, K. J. & Siliciano, R. F. HIV persistence: Clonal expansion of cells in the latent reservoir. J. Clin. Invest. 127(7), 2536–2538. https://doi.org/10.1172/JCI95329 (2017).
Liu, R., Simonetti, F. R. & Ho, Y. C. The forces driving clonal expansion of the HIV-1 latent reservoir. Virol J. 17(1), 4. https://doi.org/10.1186/s12985-019-1276-8 (2020).
Chen, J. et al. The reservoir of latent HIV. Front. Cell Infect. Microbiol. 12, 945956. https://doi.org/10.3389/fcimb.2022.945956 (2022).
Chun, T. W. et al. In vivo fate of HIV-1-infected T cells: Quantitative analysis of the transition to stable latency. Nat. Med. 1(12), 1284–1290. https://doi.org/10.1038/nm1295-1284 (1995).
Wong, J. K. et al. Recovery of replication-competent HIV despite prolonged suppression of plasma viremia. Science 278(5341), 1291–1295. https://doi.org/10.1126/science.278.5341.1291 (1997).
Vanhamel, J., Bruggemans, A. & Debyser, Z. Establishment of latent HIV-1 reservoirs: What do we really know? J. Virus Erad. 5(1), 3–9. https://doi.org/10.1016/S2055-6640(20)30275-2 (2019).
Fromentin, R. & Chomont, N. HIV persistence in subsets of CD4+ T cells: 50 shades of reservoirs. Semin. Immunol. 51, 101438. https://doi.org/10.1016/j.smim.2020.101438 (2021).
Kim, Y., Anderson, J. L. & Lewin, S. R. Getting the “Kill” into “Shock and Kill”: Strategies to eliminate latent HIV. Cell Host Microbe. 23(1), 14–26. https://doi.org/10.1016/j.chom.2017.12.004 (2018).
Elliott, J. H. et al. Activation of HIV transcription with short-course vorinostat in HIV-infected patients on suppressive antiretroviral therapy. PLoS Pathog. 10(10), e1004473. https://doi.org/10.1371/journal.ppat.1004473 (2014).
Rasmussen, T. A. et al. Panobinostat, a histone deacetylase inhibitor, for latent-virus reactivation in HIV-infected patients on suppressive antiretroviral therapy: A phase 1/2, single group, clinical trial. Lancet HIV. 1(1), e13–e21. https://doi.org/10.1016/S2352-3018(14)70014-1 (2014).
Søgaard, O. S. et al. The depsipeptide romidepsin reverses HIV-1 latency in vivo. PLoS Pathog. 11(9), e1005142. https://doi.org/10.1371/journal.ppat.1005142 (2015).
Vibholm, L. et al. Short-course toll-like receptor 9 agonist treatment impacts innate immunity and plasma viremia in individuals with human immunodeficiency virus infection. Clin. Infect. Dis. 64(12), 1686–1695. https://doi.org/10.1093/cid/cix201 (2017).
Siliciano, J. D. & Siliciano, R. F. In vivo dynamics of the latent reservoir for HIV-1: New insights and implications for cure. Annu. Rev. Pathol. 17, 271–294. https://doi.org/10.1146/annurev-pathol-050520-112001 (2022).
Bertagnolli, L. N. et al. Autologous IgG antibodies block outgrowth of a substantial but variable fraction of viruses in the latent reservoir for HIV-1. Proc. Natl. Acad. Sci. U S A 117(50), 32066–32077. https://doi.org/10.1073/pnas.2020617117 (2020).
Deng, K. et al. Broad CTL response is required to clear latent HIV-1 due to dominance of escape mutations. Nature 517(7534), 381–385. https://doi.org/10.1038/nature14053 (2015).
Debrabander, Q. et al. The efficacy and tolerability of latency-reversing agents in reactivating the HIV-1 reservoir in clinical studies: A systematic review. J. Virus Erad. 9(3), 100342. https://doi.org/10.1016/j.jve.2023.100342 (2023).
Reece, J. C. et al. Measuring turnover of SIV DNA in resting CD4+ T cells using pyrosequencing: Implications for the timing of HIV eradication therapies. PLoS ONE 9(4), e93330. https://doi.org/10.1371/journal.pone.0093330 (2014).
Petravic, J., Martyushev, A., Reece, J. C., Kent, S. J. & Davenport, M. P. Modeling the timing of antilatency drug administration during HIV treatment. J Virol. 88(24), 14050–14056. https://doi.org/10.1128/JVI.01701-14 (2014).
Chomont, N., Okoye, A. A., Favre, D. & Trautmann, L. Wake me up before you go: A strategy to reduce the latent HIV reservoir. AIDS 32(3), 293–298. https://doi.org/10.1097/QAD.0000000000001695 (2018).
Casazza, J. P., Betts, M. R., Picker, L. J. & Koup, R. A. Decay kinetics of human immunodeficiency virus-specific CD8+ T cells in peripheral blood after initiation of highly active antiretroviral therapy. J. Virol. 75(14), 6508–6516. https://doi.org/10.1128/JVI.75.14.6508-6516.2001 (2001).
Janbazian, L. et al. Clonotype and repertoire changes drive the functional improvement of HIV-specific CD8 T cell populations under conditions of limited antigenic stimulation. J. Immunol. 188(3), 1156–1167. https://doi.org/10.4049/jimmunol.1102610 (2012).
Madrid-Elena, N. et al. Maraviroc is associated with latent HIV-1 reactivation through NF-κB activation in resting CD4+ T cells from HIV-infected individuals on suppressive antiretroviral therapy. J. Virol. 92(9), e01931-e2017. https://doi.org/10.1128/JVI.01931-17 (2018).
López-Huertas, M. R. et al. The CCR5-antagonist Maraviroc reverses HIV-1 latency in vitro alone or in combination with the PKC-agonist Bryostatin-1. Sci. Rep. 7(1), 2385. https://doi.org/10.1038/s41598-017-02634-y (2017).
Buzón, M. J. et al. HIV-1 replication and immune dynamics are affected by raltegravir intensification of HAART-suppressed subjects. Nat. Med. 16(4), 460–465. https://doi.org/10.1038/nm.2111 (2010).
Bruner, K. M. et al. A quantitative approach for measuring the reservoir of latent HIV-1 proviruses. Nature 566(7742), 120–125. https://doi.org/10.1038/s41586-019-0898-8 (2019).
Yukl, S. A. et al. HIV latency in isolated patient CD4+ T cells may be due to blocks in HIV transcriptional elongation, completion, and splicing. Sci. Transl. Med. 10(430), eaap9927. https://doi.org/10.1126/scitranslmed.aap9927 (2018).
Kiselinova, M. et al. Comparison of droplet digital PCR and seminested real-time PCR for quantification of cell-associated HIV-1 RNA. PLoS ONE 9(1), e85999. https://doi.org/10.1371/journal.pone.0085999 (2014).
Brenchley, J. M. et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat. Med. 12(12), 1365–1371. https://doi.org/10.1038/nm1511 (2006).
Klatt, N. R., Chomont, N., Douek, D. C. & Deeks, S. G. Immune activation and HIV persistence: Implications for curative approaches to HIV infection. Immunol. Rev. 254(1), 326–342. https://doi.org/10.1111/imr.12065 (2013).
Moriuchi, H., Moriuchi, M., Mizell, S. B., Ehler, L. A. & Fauci, A. S. In vitro reactivation of human immunodeficiency virus 1 from latently infected, resting CD4+ T cells after bacterial stimulation. J. Infect. Dis. 181(6), 2041–2044. https://doi.org/10.1086/315496 (2000).
Tsai, A. et al. Toll-like receptor 7 agonist GS-9620 induces HIV expression and HIV-specific immunity in cells from HIV-infected individuals on suppressive antiretroviral therapy. J. Virol. 91(8), e02166-e2216. https://doi.org/10.1128/JVI.02166-16 (2017).
Chun, T. W., Engel, D., Mizell, S. B., Ehler, L. A. & Fauci, A. S. Induction of HIV-1 replication in latently infected CD4+ T cells using a combination of cytokines. J. Exp. Med. 188(1), 83–91. https://doi.org/10.1084/jem.188.1.83 (1998).
Demers, K. R. et al. Temporal dynamics of CD8+ T cell effector responses during primary HIV infection. PLoS Pathog. 12(8), e1005805. https://doi.org/10.1371/journal.ppat.1005805 (2016).
Papasavvas, E. et al. Intact human immunodeficiency virus (HIV) reservoir estimated by the intact proviral DNA assay correlates with levels of total and integrated DNA in the blood during suppressive antiretroviral therapy. Clin. Infect. Dis. 72(3), 495–498. https://doi.org/10.1093/cid/ciaa809 (2021).
Falcinelli, S. D. et al. Longitudinal dynamics of intact HIV proviral DNA and outgrowth virus frequencies in a cohort of individuals receiving antiretroviral therapy. J. Infect. Dis. 224(1), 92–100. https://doi.org/10.1093/infdis/jiaa718 (2021).
De La Torre, T. E., Passaes, C., Moreno, S., Sáez-Cirión, A. & Alcamí, J. High concentrations of Maraviroc do not alter immunological and metabolic parameters of CD4 T cells. Sci. Rep. 14(1), 13980. https://doi.org/10.1038/s41598-024-64902-y (2024).
Chéret, A. et al. Intensive five-drug antiretroviral therapy regimen versus standard triple-drug therapy during primary HIV-1 infection (OPTIPRIM-ANRS 147): A randomised, open-label, phase 3 trial. Lancet Infect. Dis. 15(4), 387–396. https://doi.org/10.1016/S1473-3099(15)70021-6 (2015).
Ananworanich, J. et al. Markers of HIV reservoir size and immune activation after treatment in acute HIV infection with and without raltegravir and maraviroc intensification. J. Virus Erad. 1(2), 116–122. https://doi.org/10.1016/S2055-6640(20)30482-9 (2015).
Chaillon, A. et al. Composition, and evolution of HIV DNA populations during early antiretroviral therapy and intensification with Maraviroc. J. Virol. 92(3), e01589-e1617. https://doi.org/10.1128/JVI.01589-17 (2018).
Bruzzesi, E. et al. HIV-DNA decrease during treatment in primary HIV-1 infection with three different drug regimens: Italian Network of Acute HIV Infection (INACTION) clinical trial. J. Med. Virol. 95(9), e29114. https://doi.org/10.1002/jmv.29114 (2023).
Collier, A. C. et al. A pilot study of raltegravir plus combination antiretroviral therapy in early human immunodeficiency virus infection: Challenges and lessons learned. Biores. Open Access 5, 15–21. https://doi.org/10.1089/biores.2015.0038 (2016).
Puertas, M. C. et al. Intensification of a raltegravir-based regimen with maraviroc in early HIV-1 infection. AIDS 28, 325–334. https://doi.org/10.1097/QAD.0000000000000066 (2014).
Vicenti, I. et al. Maraviroc as a potential HIV-1 latency-reversing agent in cell line models and ex vivo CD4 T cells. J. Gen. Virol. 102(1), 001499. https://doi.org/10.1099/jgv.0.001499 (2021).
Acknowledgements
We want to particularly acknowledge the patients in this study for their participation and to the HIV BioBank. We also thank Leire Berrocal for support in the statistical analysis and Francesco Simonetti for his advice in the IPDA analysis. EDLTT was supported by the Sara Borrell program (CD21/00102, Ministry of Science and Innovation from the Spain). EM was supported by a grant from the HIV Unit, Hospital Clinic (Barcelona) and donation of Mr Javier Moreno (II040141). We thank the GILEAD Sciences Fellowship to JA (GLD 18/0090). We also thank CIBER -Consorcio Centro de Investigación Biomédica en Red- (CB21/13/00091), Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación and Unión Europea – NextGenerationEU. We also thank ViiV Healthcare Sciences for an unrestricted support (TOLERANT 20/070).
Funding
This study was funded by the Instituto de Salud Carlos III (ISCIII) through the projects PI20/00945, PI20/00676, PI23/01896 and CIBERINFEC INFECG30 S.N./ 2024, and co-funded by the European Union.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization, S.M.; methodology, E.D.L.T.T., E.M., R.V., S.S.P., L.L. and S.V.; validation, E.D.L.T.T., S.S.P., J.A. and S.M.; formal analysis, E.D.L.T.T. and E.L.; investigation, E.D.L.T.T., E.M., R.V., S.S.P., E.L, L.L., S.V., L.J.G.F.F., J.P., M.G.G., L.B., S.G.M., L.L.P., S.S.V.; I.J., J.A. and S.M.; resources, J.A. and S.M; data curation, E.D.L.T.T., E.M, S.S.P, J.A. and S.M.; writing—original draft preparation, E.D.L.T.T.; writing—review and editing, E.D.L.T.T., S.S.P., S.S.V., J.A. and S.M.; visualization, E.D.L.T.T., S.S.P., J.A. and S.M; supervision, J.A. and S.M.; funding acquisition, E.D.L.T.T. and S.M. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
De La Torre Tarazona, E., Moraga, E., Vaquer, R. et al. Impact of the initial administration of an antiretroviral drug with latency reversal properties on the HIV reservoir size. Sci Rep 15, 25306 (2025). https://doi.org/10.1038/s41598-025-09474-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09474-1