Abstract
To compare efficacy and safety of glucagon-like peptide-1 receptor agonists (GLP-1RAs) in subjects with type 2 diabetes (T2DM). Electronic databases were searched from inception to 2nd October 2024 for randomised controlled trials comparing GLP-1RAs treating T2DM. Bayesian network meta-analyses were conducted to analyze metabolic and safety outcomes. 64 trials comprising of 25,572 participants were identified. Compared to placebo, tirzepatide showed the greatest reduction in HbA1-c (MD: -2.3%) and FPG (MD: -3.1mmol/L); semaglutide was second (HbA1-c: MD: -1.5%; FPG: MD: -2mmol/L); liraglutide was third (HbA1-c: MD: -1.2% FPG: MD: -1.6mmol/L) (P<0.05). All treatments showed no statistically significant differences in BMI, SBP, DBP, TC, HDL-C and LDL-C compared to placebo. Tirzepatide (MD: -9.1 kg), semaglutide (MD: -2.8 kg) and liraglutide (MD: -1.2 kg) (P<0.05) had significant reduction in body weight compared to placebo. GLP-1 RAs had higher risk of gastrointestinal symptoms. Semaglutide increased the risk of hypoglycemia compared to placebo while liraglutide reduced the risk of hypoglycemia compared to traditional antidiabetic drugs. GLP-1RAs improve glycaemic control, with tirzepatide, semaglutide and liraglutide exhibiting the most significant improvements. Tirzepatide is more suitable for treating T2DM with obesity. For individuals with normal weight, both semaglutide and liraglutide are generally more effective for treating T2DM. However, considering the potential for semaglutide to cause hypoglycemia, liraglutide may be the optimal choice for T2DM treatment to minimize the risk of hypoglycemia.
Similar content being viewed by others
Introduction
Type II Diabetes Mellitus (T2DM) is a metabolic disease characterized by insulin resistance and damage to islet β cells, which has attracted extensive attention because of its high incidence and multiple complications1. The tenth edition of the Global Diabetes Overview released by the International Diabetes Federation predicts that the number of people with diabetes worldwide will reach 643 million by 2030, accounting for 11.3% of the global population, and will rise to 783 million, accounting for 12.2% of the global population by 20452. T2DM has become a serious threat to public health worldwide in recent years and the variety of T2DM drugs is also increasing.
Glucagon-like peptide (GLP-1) is an insulin-stimulating hormone secreted by L cells during the digestion of food in the small intestine, which shows trophic effects on β cells and can promote the secretion of insulin to maintain the glucose homeostasis3,4. By fine-tuning the molecular structure of GLP-1, its pharmacological characteristics can be modified to generate therapeutic biological effects suitable for clinical applications. Glucagon-like peptide-1 receptor agonists (GLP-1RAs) reduce glucose levels by mimicking the action of the gut hormone GLP-1 to bind to GLP-1 receptors, stimulating the release of insulin and inhibiting glucagon secretion5. The American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) endorse the use of GLP-1RAs as an alternative when metformin alone fails to achieve the desired glycemic control, and also as a supplementary therapy to lifestyle modification6,7.
As of now, the US Food and Drug Administration (FDA) has approved EBID, once-weekly exenatide, semaglutide, dulaglutide, liraglutide, albiglutide, lixisenatide, and tirzepatide for the management of T2DM. However, clinical trials and development of taspoglutide were ceased in 2010, rendering it inaccessible for clinical utilization8.
While numerous randomized controlled trials (RCTs) have been conducted to evaluate the efficacy of GLP-1 RAs in the treatment of diabetes, no such studies have directly compared GLP-1 drugs with traditional antidiabetic drugs, in addition to comparing different GLP-1 drugs. Therefore, our study aimed to comprehensively compare the clinical profiles of GLP-1RAs. We conducted the most extensive network meta-analysis to date, evaluating not only the efficacy and safety of different GLP-1RAs but also comparing them directly with traditional antidiabetic drugs.
Materials and methods
The network meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Network Meta-Analyses (PRISMA-NMA)9,10, and it was performed prospectively registered in the PROSPERO (CRD42024595773).
Literature search
We performed a systematic literature search using PubMed, Cochrane, Embase, Web of Science, Chinese database China National Knowledge Internet (CNKI) WangFang database and China Science and Technology Journal Database (VIP) up to October 2024. The primary screening direction was an RCT of GLP-1 RAs in the treatment of T2DM. The included GLP-1 RAs were once-weekly exenatide, twice-daily exenatide, semaglutide, dulaglutide, liraglutide, albiglutide, tirzepatide and lixisenatide. We searched the databases using the following terms: “Glucagon-Like Peptide-1 Receptor Agonists”, “Exenatide”, “Semaglutide”, “Dulaglutide”, “Liraglutide”, “Albiglutide”, “Tirzepatide”, “Lixisenatide”, “Diabetes mellitus, type 2” and “Randomized Controlled Trials”. The detail search strategy is presented in Additional file 1. In addition, the reference lists of all eligible studies were manually reviewed. Two investigators searched and evaluated the included studies independently. Any disagreement in literature search was resolved by consensus.
Criteria for inclusion
Studies were included if they met the following criteria: (1) The study design was randomized controlled trail (RCT); (2) Studies were conducted in adults with T2DM (≥ 18 years old); (3) Studies comparing GLP-1 RAs with traditional antidiabetic drugs or placebo; (4) At least one outcomes indicator required by this study was reported; (5) The intervention time being at least 2 months. (6) English or Chinese studies; (7) Sufficient data to calculate relative ratio (RR) or odds ratio (OR) or mean difference (MD). Two investigators searched and evaluated the included studies independently. Any disagreement in literature search was resolved by consensus.
Exclusion criteria
Studies were excluded if they were: (1) letters, replies, comments, opinions, conference abstracts, awarded grants, trail registry records and erratum. (2) reviews, meta-analysis, case reports, adolescent articles, pediatric articles, animal articles, economic articles and non-randomized controlled trail articles. (3) unpublished articles, non-English articles and non-Chinese articles. (4) the required data cannot be obtained, or the existing data cannot be converted into the desired format required for network meta-analysis.
Data extraction
Data extraction was performed by two investigators independently. Any disagreement was resolved by another investigator to make the final decision. We extracted the following data from included studies: first author, publication year, country of study, duration of study, study design, intervention strategies, diabetes duration, sample size, age, gender, HbA1-c, FPG and BMI in baseline. We collected data on arm-specific number of participants, mean difference and standard error (SE) or standard deviation (SD) for continuous data (HbA1-c, FPG, body weight, BMI, systolic and diastolic blood pressure, total cholesterol, low- and high-density lipoprotein cholesterol). We also collected dichotomous data on the total number of participants and participants with safety outcomes (nausea, diarrhoea, vomiting, dyspepsia, constipation, decreased appetite, nasopharyngitis, headache, lipase increased and hypoglycemia). When continuous variables in the study were reported as median with interquartile range, we calculated the mean ± standard deviation (M ± SD) through the validated mathematical method11,12. When data were missing or not reported in the study, we contacted the corresponding authors to obtain the completed data if available.
This study includes other traditional antidiabetic drugs in addition to GLP-1 RAs. In addition to the network and forest plots for HbA1-c and FPG, we have combined these drugs into a single category termed “traditional drugs” for further analysis. The reasons are as follows: (1) To more comprehensively reflect the overall effects and characteristics of traditional antidiabetic drugs. (2) To increase the sample size and enhance the reliability of statistical analysis. (3) To simplify the analysis process and avoid the complexity caused by too many types of drugs. (4) To better compare with GLP-1 RAs.
Quality assessment
The Cochrane collaborative risk assessment tool was used to assess the risk of bias for included studies13. The following aspects were evaluated: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias) and other bias. Two investigators evaluated the quality of eligible studies independently, and discrepancies were resolved through discussion.
Statistical analysis
Statistical analyses of this NMA were performed with Review Manager 5.4 (Cochrane Collaboration, Oxford, UK), Stata 14.0 (StataCorp LP, College Station, Texas) package “net meta” and R. Mean difference (MD) was used to compare continuous variables and Risk ratio (RR) was used to compare dichotomous variables. The heterogeneity in studies was assessed through the Chi-squared (χ2) test (Cochran’s Q) and inconsistency index (I2)14. χ2 p value<0.05 or I2 >50% was considered as significant heterogeneity. χ2 p value<0.05 or I2 >50% was considered as significant heterogeneity and a random-effect model was used to estimate the combined MD or RR. Otherwise, the fixed-effect model was applied (p value>0.05 or I2 <50%). 95% confidence intervals (CIs) were used to determine the clinical effect of the included studies.
We performed a frequency NMA by using Stata software and R software to analyze indirect comparison between the difference interventions. For each outcome, we graphically summarised the evidence by using a network diagram15. We assessed consistency between direct and indirect evidence by using the “design by treatment” interaction model16. Deviance information criterion (DIC) statistics calculated from the random effects model was compared to the “design by treatment” model, with smaller DIC values indicating better fit. If the “design by treatment” model could not be fitted, the pairwise meta-analysis was used to compare the results from the NMA. Results were defined as consistent if NMA effect estimates fell within the 95% confidence intervals estimated from the pairwise meta-analysis.
The probability of one intervention being the most effective and safest was estimated by using the surface under the cumulative ranking curve (SUCRA). The node-splitting method and Bayes P value was used to confirm the inconsistencies of the results, and the league tables were used to express the effect values and 95CIs of pair-to-pair comparisons between the interventions. Meanwhile, as NMA included multiple closed loops, the inconsistency tests of direct and indirect evidence were carried out using the loop-specific approach. “Comparison-adjusted” funnel plots and Egger’s regression tests (only for outcomes with ten or more studies) were used to assess publication bias or other small study effects for all available comparisons15. p value<0.05 was considered as statistically significant publication bias.
Results
Literature search and study characteristics
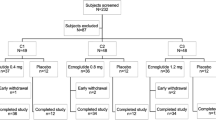
The flowchart of the systematic search and selection process was presented in Fig. 1. A total of 12,074 relevant articles in PubMed (n = 1,596), Embase (n = 3,496), Cochrane (n = 4,639), Web of Science (n = 2,265) and Chinese database (78) were yielded through systematic literature search. After removing duplicate articles, 8,523 titles and abstracts were reviewed. Finally, 64 full-text articles involving 25,572 patients were included for the NMA. Figure 2 showed the risk assessment using the Cochrane Collaboration risk assessment tool. The overall risk was moderate to low, which was mainly caused by performance bias and other bias.
Table 1 showed the characteristics of each included study. A total of 64 eligible articles involving 25,572 patients were included for the evidence synthesis17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80.
Primary outcomes
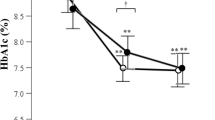
Outcome 1: HbA1-c
Analysis of primary outcome HbA1-c was conducted in 53 trails with 21,486 patients and the network plot was shown in Fig. 3A. NMA results of GLP-1 RAs compared to placebo were shown in Fig. 4A and all treatments reduced the level of HbA1-c from baseline compared to placebo. Tirzepatide showed the greatest reduction in HbA1-c (MD: −2.3%, 95% CI: −2.7, −1.9) in comparison to placebo. The reduction in HbA1-c of semaglutide was second (MD: −1.5%, 95%CI: −1.7, −1.3) and liraglutide (MD: −1.2%, 95% CI: −1.3, −1.0) was third while lixisenatide (MD: −0.56%, 95%CI: −0.75, −0.37) was last.
Compared to insulin, sulfonylureas, DDP-4 inhibitors and SGLT-2 inhibitors, tirzepatide, semaglutide oral, semaglutide injection, liraglutide, and dulaglutide showed statistically significant reduction in HbA1-c from baseline, while lixisenatide, EBID, EQW and albiglutide showed no statistically significant difference. Compared with metformin, only tirzepatide showed statistically significant reduction in HbA1-c from baseline (Fig. 4B-F). Since the analysis showed that semaglutide oral and semaglutide injection were almost identical, they would be combined into semaglutide to increase the sample size and enhance the reliability of the statistical analysis for further analysis.
Subsequently, insulin, metformin, sulfonylureas, DDP-4 inhibitors and SGLT-2 inhibitors were merged into a single category termed “traditional antidiabetic drugs” and semaglutide oral and semaglutide injection were combined into “semaglutide” for further analysis. NMA results of GLP-1 RAs compared to placebo were shown in Fig. 6A and all treatments reduced the level of HbA1-c from baseline compared to placebo. Compared to traditional antidiabetic drugs, tirzepatide (MD: −1.5%, 95%CI: −1.9, −1.1), semaglutide (MD: −0.73%, 95%CI: −0.91, −0.55), liraglutide (MD: −0.4%, 95%CI: −0.54, −0.26), EQW (MD: −0.36%, 95%CI: −0.6, −0.12) and dulaglutide (MD: −0.34%, 95%CI: −0.49, −0.2) showed statistically significant reduction in HbA1-c from baseline, while EBID and albiglutide showed no statistically significant difference. Lixisenatide (MD: 0.23%, 95%CI: 0.002, 0.45) had statistically significant increase in HbA1-c in comparison to other hypoglycemic agents (Fig. 6B).
Tirzepatide (100%) also showed the greatest probability of being the most effective treatment in the reduction of HbA1-c, followed by semaglutide in second (88.9%) and liraglutide (70.6%) in third while lixisenatide (11.9%) was last, as shown in S1 Figure A.
The results of pair-to-pair comparisons between the treatments in reduction of HbA1-c were shown in Table 2. Compared to all the other treatments, tirzepatide had statistically significant reduction in HbA1-c. Semaglutide also had statistically significant reduction in HbA1-c compared to other treatments while liraglutide had statistically significant reduction compared to EBID, lixisenatide and traditional antidiabetic drugs. Heterogeneity test was shown in S1 Table; funnel plot of publication bias was shown in S2 Fig A and the egger’s test values for comparisons of each drug with the placebo and with the traditional antidiabetic drugs were both 0.22, indicating no publication bias.
Outcome 2: FPG
Analysis of primary outcome FPG was conducted in 41 trails with 17,621 patients and the network plot was shown in Fig. 3B. NMA results of treatment compared to placebo were shown in Fig. 5A and except for lixisenatide, all treatments reduced the level of FPG from baseline compared to placebo. Tirzepatide showed the greatest reduction in FPG (MD: −3.1mmol/L, 95% CI: −3.8, −2.4) in comparison to placebo and other treatments in the network. The reduction in FPG of semaglutide was second (MD: −2mmol/L, 95%CI: −2.5, −1.5) and liraglutide (MD: −1.6mmol/L, 95% CI: −2.1, −1.0) was third.
Compared to insulin, metformin sulfonylureas, DDP-4 inhibitors and SGLT-2 inhibitors, only tirzepatide showed statistically significant reduction in FPG from baseline. Semaglutide injection showed statistically significant reduction in FPG from baseline compared to sulfonylureas and DDP-4 inhibitors. Liraglutide and dulaglutide showed statistically significant reduction in FPG from baseline compared with DDP-4 inhibitors, while EBID, EQW and lixisenatide showed no statistically significant difference compared to traditional antidiabetic drugs (Fig. 5B-F).
Subsequently, insulin, metformin, sulfonylureas, DDP-4 inhibitors and SGLT-2 inhibitors were merged into a single category termed “traditional antidiabetic drugs” and semaglutide oral and semaglutide injection were combined into “semaglutide” for further analysis. NMA results of treatment compared to placebo were shown in Fig. 6C and except for lixisenatide, all treatments reduced the level of FPG from baseline compared to placebo. Compared to traditional antidiabetic drugs, tirzepatide (MD: −1.8mmol/L, 95%CI: −2.6, −1.0), semaglutide (MD: −0.69mmol/L, 95%CI: −1.2, −0.19) showed statistically significant reduction in FPG from baseline, while lixisenatide (MD: 0.96mmol/L, 95%CI: 0.31, 1.6) had statistically significant increase in FPG from baseline. EQW, EBID, dulaglutide and liraglutide had no statistically significant difference in FPG in comparison to other hypoglycemic agents (Fig. 6D).
Tirzepatide (100%) showed the greatest probability of being the most effective treatment in the reduction of FPG, followed by semaglutide in second (85.4%) and liraglutide (66%) in third while lixisenatide (11.7%) was last (S1 FigB).
The results of pair-to-pair comparisons between the treatments in reduction of FPG were shown in Table 2. Compared to all the other treatments, tirzepatide had statistically significant reduction in FPG. Semaglutide and liraglutide had statistically significant reduction in FPG compared to EBID and lixisenatide and semaglutide also had statistically significant reduction in FPG compared to traditional antidiabetic drugs. Heterogeneity test was shown in S2 Table and funnel plot of publication bias was shown in S2 FigB. The egger’s test values for comparisons of each drug with the placebo was 0.83 and with the traditional antidiabetic drugs was 0.28, indicating no publication bias.
According to the primary outcomes HbA1-c and FPG, tirzepatide was the most effective treatment for T2DM, followed by semaglutide in second, liraglutide in third.
Secondary outcomes
Changes from baseline in body weight, BMI, SBP, DBP, TC, HDL-C and LDL-C were analyzed and network plots for these secondary outcomes were presented in S3 and S4 Figs. Treatment ranking had been reported in S5 and S6 Figs and the top three treatments ranking was as follows: Body weight: tirzepatide > semaglutide > EBID; BMI: EBID > semaglutide > liraglutide; SBP: EBID > lixisenatide > liraglutide; TC: semaglutide > EBID > liraglutide; HDL-C: dulaglutide > semaglutide > lixisenatide; LDL-C: semaglutide > liraglutide > EBID.
NMA results of treatments compared to placebo were reported in S7 Fig. Compared to placebo, all treatments showed no statistically significant differences in BMI, SBP, DBP, TC, HDL-C and LDL-C. Tirzepatide (MD: −9.1 kg, 95% CI: −11, −7.4) > semaglutide (MD: −2.8 kg, 95% CI: −3.9, −1.8) > EBID (MD: −1.8 kg, 95% CI: −3, −0.64) > liraglutide (MD: −1.2 kg, 95% CI: −2.2, −0.12) had significant reduction in body weight in comparison to placebo.
Compared to traditional antidiabetic drugs, GLP-1 RAs showed no statistically significant differences in BMI, SBP, DBP, TC, HDL-C and LDL-C. Tirzepatide (MD: −10 kg, 95%CI: −12, −8.2), semaglutide (MD: −3.8 kg, 95%CI: −4.9, −2.7), EBID (MD: −2.8 kg, 95%CI: −4.2, −1.4), liraglutide (MD: −2.1 kg, 95%CI: −3.2, −1.1), lixisenatide (MD: −2.0 kg, 95%CI: −3.3, −0.75) and dulaglutide (MD: −1.2 kg, 95%CI: −2.1, −0.25) showed statistically significant reduction in weight from baseline in comparison to traditional antidiabetic drugs (S8 Fig).
The results of pair-to-pair comparisons between the treatments were shown in S3-S6 Tables. Compared to all treatments, tirzepatide had statistically significant reduction in body weight. Semaglutide also had statistically significant reduction in body weight compared to other GLP-1RAs and traditional antidiabetic drugs. No differences were found comparing treatments with each other in BMI, SBP, DBP, TC, HDL-C and LDL-C. Heterogeneity test was shown in S7-S9 Tables and funnel plots of publication bias were shown in S2 Fig C-F.
Adverse events
Nausea, diarrhoea, vomiting, constipation, dyspepsia, decreased appetite, nasopharyngitis, headache, lipase increased and hypoglycemia were analyzed and network plots of adverse events outcomes were presented in S9 and S10 Figs. Treatment ranking had been reported in S11 and S12 Figs.
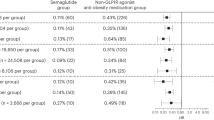
Compared to placebo, all treatments showed no statistically significant differences in nasopharyngitis, headache and lipase increased. Semaglutide, dulaglutide, liraglutide, lixisenatide and tirzepatide had higher risk of nausea, diarrhoea, vomiting, constipation, dyspepsia and decreased appetite in the comparison to placebo. EBID (RR: 3.3, 95%CI: 1.6, 6.9) and semaglutide (RR: 4.6, 95%CI: 1.6, 10.0) significantly increased the risk of hypoglycemia while the other GLP-1 RAs showed no statistically significant difference in hypoglycemia compared to placebo (S13 and S14 Figs).
Compared to traditional antidiabetic drugs, GLP-1 RAs showed no statistically significant differences in nasopharyngitis, headache, lipase increased and dyspepsia while showed higher risk of nausea and vomiting. Semaglutide, dulaglutide, liraglutide and tirzepatide had risk of diarrhoea, constipation, and decreased appetite in the comparison to traditional antidiabetic drugs. For hypoglycemia, liraglutide and lixisenatide significantly reduced the risk of hypoglycemia compared to traditional antidiabetic drugs (S15 and S16 Figs).
The results of pair-to-pair comparisons between the treatments were shown in S10-S13 Tables and almost no differences were found comparing GLP-1 RAs with each other for adverse events. Heterogeneity test was shown in S14-S22 Tables and funnel plots of publication bias were shown in S17 Fig.
Inconsistency test
Assessment of inconsistency between direct and indirect comparisons using a node-splitting model showed that there were no inconsistencies among most studies (P > 0.05) (S23-S34 Tables). The results of loop inconsistency test were shown in S35-S40 Tables. The results showed no significant inconsistencies between GLP-1 RAs.
Discussion
GLP-1RAs represent a category of medications used for treating hyperglycaemia in individuals with T2DM. GLP-1 RAs are now classified by duration of action into long-acting (EQW, albiglutide, semaglutide, dulaglutide, liraglutide and tirzepatide) and short-acting (EBID and lixisenatide)8. In RCTs, it has been demonstrated that GLP-1RAs enhance glycaemic management and promote weight reduction more effectively than conventional hypoglycemic agents. However, no studies have comprehensively evaluated both the efficacy and safety of different GLP-1RAs and compared them with traditional antidiabetic drugs. Therefore, by integrating both direct and indirect evidence, we conducted a systematic review and NMA to compare the efficacy and tolerability of different GLP-1RAs and to contrast them with traditional antidiabetic drugs, thereby offering valuable guidance for clinical treatment.
Semaglutide is available in two formulations: injection and oral tablet. Semaglutide injection involves the addition of a fatty acid side chain at the 26th position of the natural GLP-1 peptide chain, which can inhibit the degradation by DPP-4, thereby extending the half-life of semaglutide injection to one week81. Semaglutide oral tablet is based on the original peptide chain, with the addition of an absorption enhancer that can increase the local pH in the stomach, thereby inhibiting the degradation of semaglutide by pepsin and improving the oral bioavailability of semaglutide tablets82. However, there is no significant difference in efficacy between the two formulations. The oral semaglutide, due to its simplicity and convenience, is more likely to improve patient adherence. Therefore, in this study, the two formulations are collectively referred to as semaglutide for analysis.
In this systematic review and NMA involving 64 studies with a total of 25,572 participants, long-acting GLP-1RAs demonstrated more significant reductions in HbA1-c and FPG compared to short-acting GLP-1 RAs. In particular, tirzepatide, semaglutide and liraglutide treatments showed greater reductions in HbA1-c and FPG levels in comparison to other GLP-1 RAs, traditional antidiabetic drugs as well as placebo. The results are consistent with previous researches which have also indicated long-acting GLP-1RAs had a better hypoglycemic effect than short-acting GLP-1 RAs8,83.
Previous studies have shown that GLP-1RAs are effective in reducing body weight and blood pressure in comparison to placebo84,85. However, our results showed that GLP-1 RAs had no statistically significant differences in BMI, SBP, DBP, TC, HDL-C and LDL-C compared to placebo and traditional antidiabetic drugs. The study by Yao et al. demonstrated that all GLP-1 RAs can significantly improve weight conditions86, but their research was limited to comparisons only with placebo. Our study indicates that tirzepatide, semaglutide, EBID and liraglutide showed a significant reduction in body weight in comparison to placebo and traditional antidiabetic drugs. However, only tirzepatide and semaglutide had statistically significant reduction in body weight compared to other GLP-1RAs while no difference was found when compared liraglutide to other treatments. Our study not only compared GLP-1 receptor agonists with placebo groups but also with traditional antidiabetic drugs. Therefore, our conclusions differ from those of Yao et al. Tirzepatide is a new molecule capable of controlling blood glucose levels by combining the dual agonism of glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptors87 and it was approved by FDA in May 2022. Recent studies have shown that compared with selective GLP-1 RAs, GIP and GLP-1 receptor combined agonists have more significant effects in controlling blood glucose and body weight88. This NMA results indicate when there is no particular need to lose weight, liraglutide can be chosen for treatment. And we speculated that liraglutide’s weight-neutral profile might be particularly advantageous for older adults with low body weight or sarcopenia. If the treatment is for T2DM accompanied by obesity, tirzepatide and semaglutide might be the best chosen.
T2DM patients with poor blood glucose control or long duration of T2DM often have impaired gastric motility and delayed gastric emptying will lead to gastrointestinal symptoms89,90,91,92,93,94. Our NMA results showed that semaglutide, dulaglutide, liraglutide, and tirzepatide had higher risk of gastrointestinal symptoms in comparison to placebo and traditional antidiabetic drugs. As regards hypoglycemia, EBID and semaglutide significantly increased the risk of hypoglycemia while the other GLP-1 RAs showed no statistically significant difference in hypoglycemia compared to placebo. Compared to traditional antidiabetic drugs, liraglutide and lixisenatide significantly reduced the risk of hypoglycemia. However, almost no differences were found comparing GLP-1 RAs with each other for adverse events. These findings indicate that when selecting the best personalized strategy for reducing blood glucose, individuals with good gastrointestinal health may be prioritized for the use of liraglutide in T2DM treatment. Additionally, those who have experienced hypoglycemic reactions while using traditional antidiabetic drugs may be encouraged to consider switching to liraglutide in their subsequent treatment.
Therefore, hypoglycemic effect (HbA1-c and FPG), body weight, hypoglycemia and gastrointestinal symptoms are important factors when choosing GLP-1 RAs. The NMA suggests tirzepatide, semglutide and liraglutide are the three most effective GLP-1 RAs for T2DM. Given that semaglutide may increase the risk of hypoglycemia, tirzepatide appears to be a more suitable option for the treatment of T2DM in patients with obesity. For individuals with normal weight, both semaglutide and liraglutide are generally more effective for treating T2DM compared to other GLP-1 RAs. However, considering the potential for semaglutide to cause hypoglycemia, liraglutide may be the optimal choice for T2DM treatment to minimize the risk of hypoglycemia.
By performing systematic review and NMA of RCTs, it was possible to obtain comparisons among GLP-1 RAs by combining results from a large number of RCTs to synthesise direct and indirect evidence. However, there are still some limitations. First, because of the sparsity of several networks, the inconsistency could not be all assessed using the design-by-treatment models for all efficacy and safety outcomes. Inconsistency is one of the most important assumptions which need to be considered when conducting a NMA95. However, most effect estimates from the NMA were within the confidence intervals of pairwise meta-analysis, indicating that the results were mostly consistent. Second, some baseline characteristics, such as included population, duration of study, background therapies and quality of studies are different across included RCTs which are particularly relevant as cardiometabolic effects of GLP-1RAs may differ when these agents are added to insulin, metformin, sulfonylureas, DDP-4 inhibitors and SGLT-2 inhibitors. Third, this review only included published RCTs. Although the risk of publication bias of RCTs should be lower than other study types, it is possible that some conducted RCTs have not been registered or reported. Fourth, this NMA shares the same drawbacks common to other NMAs96.
Conclusions
In conclusions, GLP-1RAs improve glycaemic control and long-acting GLP-1RAs demonstrated more significant reductions in HbA1-c and FPG compared to short-acting GLP-1 RAs, with tirzepatide, semaglutide and liraglutide exhibiting the most significant improvements. Tirzepatide is more suitable for the treatment of T2DM with obesity. For individuals with normal weight, both semaglutide and liraglutide are generally more effective for treating T2DM compared to other GLP-1 RAs. However, considering the potential for semaglutide to cause hypoglycemia, liraglutide may be the optimal choice for T2DM treatment to minimize the risk of hypoglycemia. The evidence suggested the choice of GLP-1 RAs should be tailored taking into account their differences in efficacy and safety along with the targets and needs of patients.
Data availability
The data supporting the conclusions of this article will be made available by the authors, without undue reservation. And the original contributions presented in the study are included in the articles and supplementary material. If someone wants to request the data from this study, please contact the first author or corresponding author.
Abbreviations
- ADA:
-
American Diabetes Association
- BMI:
-
Body Mass Index
- Cis:
-
Confidence Intervals
- CNKI:
-
Chinese database China National Knowledge Internet
- DBP:
-
Diastolic Blood Pressure
- DDP-4:
-
Dipeptidylpeptidase-4
- DIC:
-
Deviance Information Criterion
- EASD:
-
European Association for the Study of Diabetes
- EBID:
-
Twice-daily Exenatide
- EQW:
-
Once-weekly Exenatide
- FDA:
-
Food and Drug Administration
- FPG:
-
Fasting Plasma Glucose
- GIP:
-
Glucose-dependent Insulinotropic Polypeptide
- GLP-1:
-
Glucagon-like Peptide
- GLP-1 RAs:
-
Glucagon-like Peptide Receptor Agonists
- HbA1-c:
-
Glycosylated Hemoglobin, Type A1C
- HDL-C:
-
High-Density Lipoprotein Cholesterol
- LDL-C:
-
Low-Density Lipoprotein Cholesterol
- MD:
-
Mean Difference
- NMA:
-
Network Meta-analysis
- OR:
-
Odds ratio
- RCT:
-
Randomized Controlled Trail
- RR:
-
Relative Ratio
- SBP:
-
Systolic Blood Pressure
- SD:
-
Standard Deviation
- SE:
-
Standard Error
- SGLT-2:
-
Sodium-dependent Glucose Transporter 2
- SUCRA:
-
Surface Under the Cumulative Ranking Curve
- T2DM:
-
Type II Diabetes Mellitus
- TC:
-
Total Cholesterol
References
Tao, Y. W., Gu, Y. L., Mao, X. Q., Zhang, L. & Pei, Y. F. Effects of probiotics on type II diabetes mellitus: a meta-analysis. 18(1):30. (2020).
Magliano, D. J., Boyko, E. J. & committee IDFDAtes. IDF Diabetes Atlas. Idf diabetes atlas. Brussels: International Diabetes Federation © International Diabetes Federation, ; 2021. (2021).
Li, Y., Gao, S., Zhang, R. & Li, B. Y. Research progress on clinical application and mechanism of action of liraglutide. Mod. Med. Clin. 37 (01), 197–202 (2022).
Lovshin, J. A. Glucagon-like Peptide-1 receptor agonists: A class update for treating type 2 diabetes. Can. J. Diabetes. 41 (5), 524–535 (2017).
Boarder, M. et al. Pharmacology for Pharmacy and the Health Sciences: a patient-centred Approach (Oxford University Press, 2017).
8. Pharmacologic approaches to glycemic treatment: standards of medical care in Diabetes-2018. Diabetes Care. 41 (Suppl 1), S73–s85 (2018).
Davies, M. J., D’Alessio, D. A., Fradkin, J., Kernan, W. N. & Mathieu, C. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD). 41(12):2669–2701. (2018).
Htike, Z. Z. et al. Efficacy and safety of glucagon-like peptide-1 receptor agonists in type 2 diabetes: A systematic review and mixed-treatment comparison analysis. Diabetes Obes. Metab. 19 (4), 524–536 (2017).
Hutton, B. et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann. Intern. Med. 162 (11), 777–784 (2015).
Shamseer, L. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj 350, g7647 (2015).
Wan, X., Wang, W., Liu, J. & Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 14, 135 (2014).
Luo, D., Wan, X., Liu, J. & Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med. Res. 27 (6), 1785–1805 (2018).
Sterne, J. A. C. et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj 366, l4898 (2019).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21 (11), 1539–1558 (2002).
Chaimani, A., Higgins, J. P., Mavridis, D., Spyridonos, P. & Salanti, G. Graphical tools for network meta-analysis in STATA. PLoS One. 8 (10), e76654 (2013).
Jackson, D., Barrett, J. K., Rice, S., White, I. R. & Higgins, J. P. A design-by-treatment interaction model for network meta-analysis with random inconsistency effects. Stat. Med. 33 (21), 3639–3654 (2014).
Ahmann, A. J. et al. Efficacy and safety of Once-Weekly semaglutide versus exenatide ER in subjects with type 2 diabetes (SUSTAIN 3): a 56-Week, Open-Label, randomized clinical trial. Diabetes Care. 41 (2), 258–266 (2018).
Araki, E. et al. Efficacy and safety of once-weekly dulaglutide in combination with sulphonylurea and/or Biguanide compared with once-daily insulin glargine in Japanese patients with type 2 diabetes: a randomized, open-label, phase III, non-inferiority study. Diabetes Obes. Metab. 17 (10), 994–1002 (2015).
Aroda, V. R. et al. PIONEER 1: randomized clinical trial of the efficacy and safety of oral semaglutide monotherapy in comparison with placebo in patients with type 2 diabetes. Diabetes Care. 42 (9), 1724–1732 (2019).
Bergenstal, R. M. et al. Efficacy and safety of exenatide once weekly versus sitagliptin or Pioglitazone as an adjunct to Metformin for treatment of type 2 diabetes (DURATION-2): a randomised trial. Lancet 376 (9739), 431–439 (2010).
Buse, J. B. et al. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in sulfonylurea-treated patients with type 2 diabetes. Diabetes Care. 27 (11), 2628–2635 (2004).
Buse, J. B. et al. Exenatide once weekly versus liraglutide once daily in patients with type 2 diabetes (DURATION-6): a randomised, open-label study. Lancet 381 (9861), 117–124 (2013).
Chen, Y. H. et al. Efficacy and safety of dulaglutide monotherapy compared with glimepiride in East-Asian patients with type 2 diabetes in a multicentre, double-blind, randomized, parallel-arm, active comparator, phase III trial. Diabetes Obes. Metab. 20 (9), 2121–2130 (2018).
Dungan, K. M. et al. Once-weekly dulaglutide versus once-daily liraglutide in metformin-treated patients with type 2 diabetes (AWARD-6): a randomised, open-label, phase 3, non-inferiority trial. Lancet 384 (9951), 1349–1357 (2014).
Dungan, K. M. et al. A 24-week study to evaluate the efficacy and safety of once-weekly dulaglutide added on to glimepiride in type 2 diabetes (AWARD-8). Diabetes Obes. Metab. 18 (5), 475–482 (2016).
Frías, J. P. et al. Exenatide once weekly plus Dapagliflozin once daily versus exenatide or Dapagliflozin alone in patients with type 2 diabetes inadequately controlled with Metformin monotherapy (DURATION-8): a 28 week, multicentre, double-blind, phase 3, randomised controlled trial. Lancet Diabetes Endocrinol. 4 (12), 1004–1016 (2016).
Furusawa, S. et al. Glycaemic control efficacy of switching from dipeptidyl peptidase-4 inhibitors to oral semaglutide in subjects with type 2 diabetes: A multicentre, prospective, randomized, open-label, parallel-group comparison study (SWITCH-SEMA 2 study). Diabetes Obes. Metabolism. 26 (3), 961–970 (2024).
Garber, A. et al. Liraglutide versus glimepiride monotherapy for type 2 diabetes (LEAD-3 Mono): a randomised, 52-week, phase III, double-blind, parallel-treatment trial. Lancet 373 (9662), 473–481 (2009).
Giorgino, F., Benroubi, M., Sun, J. H., Zimmermann, A. G. & Pechtner, V. Efficacy and safety of Once-Weekly dulaglutide versus insulin glargine in patients with type 2 diabetes on Metformin and glimepiride (AWARD-2). Diabetes Care. 38 (12), 2241–2249 (2015).
Heise, T. et al. Effects of subcutaneous Tirzepatide versus placebo or semaglutide on pancreatic islet function and insulin sensitivity in adults with type 2 diabetes: a multicentre, randomised, double-blind, parallel-arm, phase 1 clinical trial. Lancet Diabetes Endocrinol. 10 (6), 418–429 (2022).
Inagaki, N., Takeuchi, M., Oura, T., Imaoka, T. & Seino, Y. Efficacy and safety of Tirzepatide monotherapy compared with dulaglutide in Japanese patients with type 2 diabetes (SURPASS J-mono): a double-blind, multicentre, randomised, phase 3 trial. Lancet Diabetes Endocrinol. 10 (9), 623–633 (2022).
Joubert, M. et al. Efficacy and safety of exenatide as add-on therapy for patients with type 2 diabetes with an intensive insulin regimen: A randomized double-blind trial. Diabetes Obes. Metabolism. 23 (2), 374–381 (2021).
Kadowaki, T. et al. Improved glycemic control and reduced bodyweight with exenatide: a double-blind, randomized, phase 3 study in Japanese patients with suboptimally controlled type 2 diabetes over 24 weeks. J. Diabetes Invest. 2 (3), 210–217 (2011).
Kaku, K., Rasmussen, M. F., Nishida, T. & Seino, Y. Fifty-two-week, randomized, multicenter trial to compare the safety and efficacy of the novel glucagon-like peptide-1 analog liraglutide vs Glibenclamide in patients with type2 diabetes. J. Diabetes Invest. 2 (6), 441–447 (2011).
Kimura, T. et al. Comparison of Clinical Efficacy and Safety of Weekly glucagon-like peptide-1 Receptor Agonists Dulaglutide and Semaglutide in Japanese Patients with Type 2 Diabetes: Randomized, parallel-group, Multicentre, open-label Trial (COMING study) (Diabetes Obesity & Metabolism, 2023).
Kondo, Y., Satoh, S. & Terauchi, Y. Effects of dulaglutide and trelagliptin on beta-cell function in patients with type 2 diabetes: a randomized controlled study: dUET-beta study. Diabetol. Int. 15(3):474–482, (2024).
Li, C. J. et al. Efficacy and safety comparison of add-on therapy with liraglutide, saxagliptin and vildagliptin, all in combination with current conventional oral hypoglycemic agents therapy in poorly controlled Chinese type 2 diabetes. Exp. Clin. Endocrinol. Diabetes. 122 (8), 469–476 (2014).
Li, Y. et al. Efficacy and safety of dulaglutide versus insulin glargine in Chinese T2DM patients: a subgroup analysis of a randomized trial (AWARD-CHN2). Diabetes Therapy. 10 (4), 1435–1452 (2019).
Lingvay, I. et al. Efficacy and safety of once-weekly semaglutide versus daily Canagliflozin as add-on to Metformin in patients with type 2 diabetes (SUSTAIN 8): a double-blind, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol. 7 (11), 834–844 (2019).
Ludvik, B. et al. Dulaglutide as add-on therapy to SGLT2 inhibitors in patients with inadequately controlled type 2 diabetes (AWARD-10): a 24-week, randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 6 (5), 370–381 (2018).
Moretto, T. J. et al. Efficacy and tolerability of exenatide monotherapy over 24 weeks in antidiabetic drug-naive patients with type 2 diabetes: a randomized, double-blind, placebo-controlled, parallel-group study. Clin. Ther. 30 (8), 1448–1460 (2008).
Nakaguchi, H. et al. Effects of liraglutide and empagliflozin added to insulin therapy in patients with type 2 diabetes: a randomized controlled study. J. Diabetes Invest. 11 (6), 1542–1550 (2020).
Nauck, M. et al. Once-Daily liraglutide versus lixisenatide as Add-on to Metformin in type 2 diabetes: a 26-Week randomized controlled clinical trial. Diabetes Care. 39 (9), 1501–1509 (2016).
Nauck, M. A. et al. Efficacy and safety of once-weekly GLP-1 receptor agonist albiglutide (HARMONY 2): 52 week primary endpoint results from a randomised, placebo-controlled trial in patients with type 2 diabetes mellitus inadequately controlled with diet and exercise. Diabetologia 59 (2), 266–274 (2016).
Onishi, Y. et al. Efficacy and safety of lixisenatide in Japanese patients with type 2 diabetes mellitus inadequately controlled by sulfonylurea with or without metformin: subanalysis of GetGoal-S. J. Diabetes Invest. 6 (2), 201–209 (2015).
Otowa-Suematsu, N. et al. Comprehensive evaluation of combination therapy with basal insulin and either lixisenatide or vildagliptin in Japanese patients with type 2 diabetes: a randomized, Open-Label, Parallel-Group, multicenter study. Diabetes Therapy. 9 (5), 2067–2079 (2018).
Patorno, E. et al. Efficacy and safety of lixisenatide in Japanese patients with type 2 diabetes insufficiently controlled with basal insulin ± sulfonylurea: A subanalysis of the GetGoal-L-Asia study. Pharmacoepidemiol Drug Saf. 47 (12), 895–900 (2015).
Pinget, M. et al. Efficacy and safety of lixisenatide once daily versus placebo in type 2 diabetes insufficiently controlled on Pioglitazone (GetGoal-P). Diabetes Obes. Metab. 15 (11), 1000–1007 (2013).
Pratley, R. et al. Oral semaglutide versus subcutaneous liraglutide and placebo in type 2 diabetes (PIONEER 4): a randomised, double-blind, phase 3a trial. Lancet 394 (10192), 39–50 (2019).
Pratley, R. E. et al. Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial. Lancet Diabetes Endocrinol. 6 (4), 275–286 (2018).
Pratley, R. E. et al. Liraglutide versus sitagliptin for patients with type 2 diabetes who did not have adequate glycaemic control with metformin: a 26-week, randomised, parallel-group, open-label trial. Lancet 375 (9724), 1447 (2010).
Pratley, R. E. et al. Once-weekly albiglutide versus once-daily liraglutide in patients with type 2 diabetes inadequately controlled on oral drugs (HARMONY 7): A randomised, open-label, multicentre, non-inferiority phase 3 study. Lancet Diabetes Endocrinol. 2 (4), 289–297 (2014).
Reusch, J. et al. Efficacy and safety of once-weekly glucagon-like peptide 1 receptor agonist albiglutide (HARMONY 1 trial): 52-week primary endpoint results from a randomized, double-blind, placebo-controlled trial in patients with type 2 diabetes mellitus not controlled on pioglitazone, with or without Metformin. Diabetes Obes. Metab. 16 (12), 1257–1264 (2014).
Riddle, M. C. et al. Adding once-daily lixisenatide for type 2 diabetes inadequately controlled by established basal insulin: a 24-week, randomized, placebo-controlled comparison (GetGoal-L). Diabetes Care. 36 (9), 2489–2496 (2013).
Rodbard, H. W. et al. Semaglutide added to basal insulin in type 2 diabetes (SUSTAIN 5): A randomized, controlled trial. J. Clin. Endocrinol. Metabolism. 103 (6), 2291–2301 (2018).
Rodbard, H. W. et al. Oral semaglutide versus empagliflozin in patients with type 2 diabetes uncontrolled on metformin: the PIONEER 2 trial. Diabetes Care. 42 (12), 2272–2281 (2019).
Rosenstock, J. et al. Beneficial effects of once-daily lixisenatide on overall and postprandial glycemic levels without significant excess of hypoglycemia in type 2 diabetes inadequately controlled on a sulfonylurea with or without Metformin (GetGoal-S). J. Diabetes Complicat. 28 (3), 386–392 (2014).
Rosenstock, J. et al. Efficacy and safety of lixisenatide once daily versus exenatide twice daily in type 2 diabetes inadequately controlled on metformin: a 24-week, randomized, open-label, active-controlled study (GetGoal-X). Diabetes Care. 36 (10), 2945–2951 (2013).
Rosenstock, J. et al. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist Tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet 398 (10295), 143–155 (2021).
Seino, Y. et al. Combination therapy with liraglutide and insulin in Japanese patients with type 2 diabetes: a 36-week, randomized, double-blind, parallel-group trial. J. Diabetes Invest. 7 (4), 565–573 (2016).
Seino, Y., Min, K. W., Niemoeller, E. & Takami, A. Randomized, double-blind, placebo-controlled trial of the once-daily GLP-1 receptor agonist lixisenatide in Asian patients with type 2 diabetes insufficiently controlled on basal insulin with or without a sulfonylurea (GetGoal-L-Asia). Diabetes Obes. Metab. 14 (10), 910–917 (2012).
Seino, Y., Rasmussen, M. F., Nishida, T. & Kaku, K. Efficacy and safety of the once-daily human GLP-1 analogue, liraglutide, vs Glibenclamide monotherapy in Japanese patients with type 2 diabetes. Curr. Med. Res. Opin. 26 (5), 1013–1022 (2010).
Sorli, C. et al. Efficacy and safety of once-weekly semaglutide monotherapy versus placebo in patients with type 2 diabetes (SUSTAIN 1): a double-blind, randomised, placebo-controlled, parallel-group, multinational, multicentre phase 3a trial. Lancet Diabetes Endocrinol. 5 (4), 251–260 (2017).
Su, X. & Zhao, T. Q. Effects of exenatide on glycemic control over 52 weeks in patients with type 2 diabetes. Chin. Pharm. J. 49 (11), 941–943 (2014).
Tamura, M. et al. Once-weekly glucagon-like peptide-1 receptor agonist dulaglutide is non-inferior to once-daily liraglutide and superior to placebo in Japanese patients with type 2 diabetes: a 26-week randomized phase III study. Diabetes Obes. Metab. 17 (10), 974–983 (2015).
Tan, M. H. et al. Comparison of insulin glargine and liraglutide added to oral agents in patients with poorly controlled type 2 diabetes. Diabetes Care. 17 (2), 170–178 (2015).
Terauchi, Y., Satoi, Y., Takeuchi, M. & Imaoka, T. Monotherapy with the once weekly GLP-1 receptor agonist dulaglutide for 12 weeks in Japanese patients with type 2 diabetes: dose-dependent effects on glycaemic control in a randomised, double-blind, placebo-controlled study. Endocr. J. 61 (10), 949–959 (2014).
Umpierrez, G., Tofé Povedano, S., Pérez Manghi, F., Shurzinske, L. & Pechtner, V. Efficacy and safety of dulaglutide monotherapy versus Metformin in type 2 diabetes in a randomized controlled trial (AWARD-3). Diabetes Care. 37 (8), 2168–2176 (2014).
van Eyk, H. J. et al. A double-blind, placebo-controlled, randomised trial to assess the effect of liraglutide on ectopic fat accumulation in South Asian type 2 diabetes patients. Cardiovasc. Diabetol. 18 (1), 87 (2019).
Vanderheiden, A. et al. Effect of adding liraglutide vs placebo to a High-Dose Lnsulin regimen in patients with type 2 diabetes: a randomized clinical trial. JAMA Intern. Med. 176 (7), 939–947 (2016).
Weissman, P. N. et al. HARMONY 4: randomised clinical trial comparing once-weekly albiglutide and insulin glargine in patients with type 2 diabetes inadequately controlled with Metformin with or without sulfonylurea. Diabetologia 57 (12), 2475–2484 (2014).
Yabe, D. et al. Safety and efficacy of oral semaglutide versus dulaglutide in Japanese patients with type 2 diabetes (PIONEER 10): an open-label, randomised, active-controlled, phase 3a trial. Lancet Diabetes Endocrinol. 8 (5), 392–406 (2020).
Yamada, Y. et al. Dose-response, efficacy, and safety of oral semaglutide monotherapy in Japanese patients with type 2 diabetes (PIONEER 9): a 52-week, phase 2/3a, randomised, controlled trial. Lancet Diabetes Endocrinol. 8 (5), 377–391 (2020).
Yang, W. et al. Efficacy and safety benefits of iGlarLixi versus insulin glargine 100 u/ml or lixisenatide in Asian Pacific people with suboptimally controlled type 2 diabetes on oral agents: the LixiLan-O-AP randomized controlled trial. Diabetes Obes. Metab. 24 (8), 1522–1533 (2022).
Yang, W. et al. Efficacy and safety of lixisenatide in a predominantly Asian population with type 2 diabetes insufficiently controlled with basal insulin: the GetGoal-L-C randomized trial. Diabetes Obes. Metabolism. 20 (2), 335–343 (2018).
Yin, T. T. et al. Comparison of glycemic variability in Chinese T2DM patients treated with exenatide or insulin glargine: a randomized controlled trial. Diabetes Therapy. 9 (3), 1253–1267 (2018).
Yu Pan, C. et al. Lixisenatide treatment improves glycaemic control in Asian patients with type 2 diabetes mellitus inadequately controlled on Metformin with or without sulfonylurea: a randomized, double-blind, placebo-controlled, 24-week trial (GetGoal-M-Asia). Diab./Metab. Res. Rev. 30 (8), 726–735 (2014).
Zang, L. et al. Efficacy and safety of liraglutide versus sitagliptin, both in combination with metformin, in Chinese patients with type 2 diabetes: a 26-week, open-label, randomized, active comparator clinical trial. Diabetes Obes. Metab. 18 (8), 803–811 (2016).
Zhang, J. et al. Comparison of the effects of twice-daily exenatide and insulin on carotid intima-media thickness in type 2 diabetes mellitus patients: a 52-week randomized, open-label, controlled trial. Cardiovasc. Diabetol. 19(1), 48. (2020).
Zinman, B. et al. Efficacy and safety of the human glucagon-like peptide-1 analog liraglutide in combination with Metformin and Thiazolidinedione in patients with type 2 diabetes (LEAD-4 Met + TZD). Diabetes Care. 32 (7), 1224–1230 (2009).
Lau, J. et al. Discovery of the Once-Weekly Glucagon-Like Peptide-1 (GLP-1) analogue semaglutide. J. Med. Chem. 58 (18), 7370–7380 (2015).
Buckley, S. T. et al. Transcellular stomach absorption of a derivatized glucagon-like peptide-1 receptor agonist. ;10(467). (2018).
Hussein, H., Zaccardi, F. & Khunti, K. Efficacy and tolerability of sodium-glucose co-transporter-2 inhibitors and glucagon-like peptide-1 receptor agonists: A systematic review and network meta-analysis. 22(7):1035–1046. (2020).
Potts, J. E. et al. The effect of Glucagon-Like peptide 1 receptor agonists on weight loss in type 2 diabetes: A systematic review and mixed treatment comparison Meta-Analysis. PLoS One. 10 (6), e0126769 (2015).
Sun, F. et al. Impact of GLP-1 receptor agonists on blood pressure, heart rate and hypertension among patients with type 2 diabetes: A systematic review and network meta-analysis. Diabetes Res. Clin. Pract. 110 (1), 26–37 (2015).
Yao, H. et al. Comparative effectiveness of GLP-1 receptor agonists on glycaemic control, body weight, and lipid profile for type 2 diabetes: systematic review and network meta-analysis. ;384:e076410. (2024).
Forzano, I., Varzideh, F., Avvisato, R. & Tirzepatide Syst. Update ;23(23). (2022).
Chen, M., Zhang, G. S., Han, F. & Zhu, H. A network meta-analysis of the efficacy and safety of different doses of Tezsporide in the treatment of type 2 diabetes. Practical Drugs Clin. 27 (04), 248–254 (2024).
Boland, B. S., Edelman, S. V. & Wolosin, J. D. Gastrointestinal complications of diabetes. Endocrinol. Metab. Clin. North. Am. 42 (4), 809–832 (2013).
Sogabe, M. et al. Ultrasonographic assessment of gastric motility in diabetic gastroparesis before and after attaining glycemic control. J. Gastroenterol. 40 (6), 583–590 (2005).
Mearin, F. & Malagelada, J. R. Gastroparesis and dyspepsia in patients with diabetes mellitus. Eur. J. Gastroenterol. Hepatol. 7 (8), 717–723 (1995).
Quan, C., Talley, N. J., Jones, M. P., Spies, J. & Horowitz, M. Gain and loss of Gastrointestinal symptoms in diabetes mellitus: associations with psychiatric disease, glycemic control, and autonomic neuropathy over 2 years of follow-up. Am. J. Gastroenterol. 103 (8), 2023–2030 (2008).
Rayner, C. K., Samsom, M., Jones, K. L. & Horowitz, M. Relationships of upper Gastrointestinal motor and sensory function with glycemic control. Diabetes Care. 24 (2), 371–381 (2001).
Fineman, M. S. et al. Effect on glycemic control of exenatide (synthetic exendin-4) additive to existing Metformin and/or sulfonylurea treatment in patients with type 2 diabetes. Diabetes Care. 26 (8), 2370–2377 (2003).
Tonin, F. S. & Rotta, I. Network meta-analysis: a technique to gather evidence from direct and indirect comparisons. 15(1):943. (2017).
Cipriani, A., Higgins, J. P., Geddes, J. R. & Salanti, G. Conceptual and technical challenges in network meta-analysis. Ann. Intern. Med. 159 (2), 130–137 (2013).
Acknowledgements
The authors greatly appreciate the Institution of Epidemiology and Statistics, School of Public Health, Lanzhou University and the financial support from the National Natural Science Foundation of China.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: Ning Cheng and Xiaoyu Ren; (II) Administrative support: Ning Cheng and Yana Bai; (III) Provision of study materials: Xiaoyu Ren; (IV) Collection and assembly of data: Xiaoyu Ren, Honghao Hua, Yuanqin Wu, Wei Zhang, Xianzhen Long; (V) Data analysis and interpretation: Xiaoyu Ren (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ren, X., Hua, H., Wu, Y. et al. Efficacy and safety of GLP-1 agonists in the treatment of T2DM: A systematic review and network meta-analysis. Sci Rep 15, 24103 (2025). https://doi.org/10.1038/s41598-025-09807-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09807-0