Abstract
Cerebral small vessel disease (CSVD) is a major neurovascular contributor to stroke and cognitive impairment, yet its interaction with chronic high-altitude adaptation remains poorly understood. This first neuroimaging investigation examined 499 Tibetan natives residing at 2000–4800 m using 3 T MRI to quantify CSVD burden and to assess its association with residential altitude. Multivariable logistic regression, treating altitude as both a continuous variable (per 500 m increment) and a categorical variable (mid-high [2000–3500 m] vs. ultra-high [> 3500 m]), revealed that 51.5% of participants had CSVD (CSVD score ≥ 1), with adjusted odds ratios of 0.94 (95% CI: 0.74–1.21) per 500 m altitude and 0.78 (95% CI: 0.42–1.44) for ultra-high versus mid-high altitude. Partial proportional odds model showed no significant association between altitude and CSVD score (OR = 1.18, 95% CI 0.99–1.40). These null findings, in contrast to the well-established paradoxical impact of altitude on stroke risk, suggest potential neuroprotective mechanisms in altitude-adapted populations. Our results challenge conventional cerebrovascular paradigms and highlight the need for further research into Tibetan-specific genetic adaptations that may modulate CSVD pathophysiology. This study provides essential insights for refining altitude-related cerebrovascular risk models.
Similar content being viewed by others
Introduction
Cerebral small vessel disease (CSVD) represents a prevalent neurological disorder strongly associated with various cerebrovascular abnormalities and neurodegenerative diseases. Epidemiological data consistently demonstrate that CSVD is particularly common in the elderly, with its prevalence significantly increasing with age1. The clinical manifestations of CSVD vary widely, with approximately 20% of elderly individuals remaining asymptomatic, while others may experience cognitive impairment, mood disturbances, gait abnormalities, or urinary dysfunction2. An increasing body of research links CSVD to both dementia and stroke3,4. Studies indicate that cognitive impairment (CI) resulting from CSVD accounts for 36–67%4 of all cases of vascular dementia (VaD) and 15–30% of all dementia cases, positioning it as the second most common cause after Alzheimer’s disease (AD)3,5. Given the substantial economic burden of dementia and stroke on both individuals and society6, further investigation into the pathophysiological mechanisms and risk factors of CSVD holds significant clinical and public health value.
CSVD may exhibit different characteristics depending on ethnicity and environmental factors. For instance, a nationwide epidemiological study in China revealed regional variations in stroke incidence, with the northern and central regions showing the highest stroke burden7. Additionally, a study conducted in Shunyi demonstrated that the progression of CSVD in participants from the same age group was more pronounced than in Western populations8. High-altitude regions present unique environmental challenges, such as hypoxia, low temperatures, and increased ultraviolet radiation. Chronic exposure to these conditions can lead to a variety of physiological and pathological changes, including erythrocytosis, pulmonary hypertension, and chronic mountain sickness9. Globally, over 500 million people (5.7% of the world’s population) reside at altitudes above 1500 m10. In China, vast high-altitude areas include four major plateaus, with the Tibetan Plateau being the highest on Earth, often referred to as the “Roof of the World”. Approximately 80 million people in China live above 2500 m, with nearly 3.7 million residing at altitudes around 4000 m in Tibet11. Prior research on stroke characteristics in high-altitude populations remains inconclusive, with some studies suggesting a dual impact of altitude on stroke risk12,13,14. Certain studies have indicated lower stroke incidence and mortality rates among highland residents compared to those at lower altitudes13,14, while other research, such as a study conducted in India, reports a positive association between higher altitudes and elevated stroke risk12. Despite China’s vast high-altitude terrain, research on CSVD in these regions is still limited, and few studies have explored the relationship between different altitudes and CSVD.
This study aims to explore, for the first time, the association between varying altitudes and the severity of CSVD, along with its imaging biomarkers, in the native Tibetan population. By comparing the severity and imaging features of CSVD in populations residing at different altitudes, this study will provide novel insights into the impact of altitude on CSVD and contribute valuable information for managing cerebrovascular health in high-altitude communities.
Methods
Study population
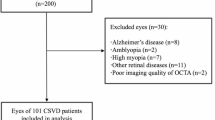
This retrospective hospital-based cohort study analyzed neurology inpatients admitted between November 2022 and February 2025 at the Department of Neurology, Chengdu Office Hospital of the People’s Government of Tibet Autonomous Region. Patients presented with a range of neurological conditions, including vestibular disturbances (vertigo), chronic primary headache disorders, cerebrovascular disease, Parkinsonian spectrum disorders, and affective comorbidities involving anxiety and depression. The study protocol was approved by the Institutional Review Board (IRB) of Chengdu Office Hospital (IRB number: 2022–65), with informed consent obtained from each participant at the time of enrollment. All research procedures were conducted in strict accordance with the relevant ethical guidelines, adhering to the principles outlined in the Declaration of Helsinki.
Participants in this cohort were required to meet the following inclusion criteria: age ≥ 35 years, birth and prolonged residence in the Tibetan Plateau region, and completion of head MRI scans (including T1-weighted, T2-weighted, and T2-weighted fluid-attenuated inversion recovery (FLAIR) sequences) that met the study’s specifications. Exclusion criteria included participants with large cortical infarctions or intracerebral hemorrhages, those diagnosed with intracranial infections, central nervous system demyelinating disorders, or other conditions associated with white matter demyelination. Considering that severe chronic hepatic or renal dysfunction and malignancies may induce systemic metabolic abnormalities that influence CSVD progression15,16, or interfere with the interpretation of CSVD biomarkers17,18, participants with a history of severe hepatic disease (Child–Pugh score ≥ 7 with clinical ascites), severe renal disease (chronic kidney disease stage 4–5, eGFR < 30 mL/min/1.73m2), or malignancies were excluded.
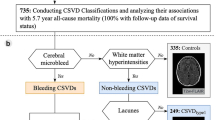
As illustrated in the flowchart (Fig. 1), a total of 499 participants, each of whom had complete MRI data, altitude measurements, and other relevant clinical variables, were included in the final analysis.
Data collection
Assessment of altitude
Altitude data for each participant were obtained based on their residential location. To ensure the scientific validity and practicality of the high-altitude exposure classification, we followed the recommendations of the International Society for Mountain Medicine, which we deemed most suitable for this study19. Among our study population, no participants lived at altitudes below 2000 m, and only nine participants resided between 2000 and 2500 m. Therefore, we used 3500 m as the cutoff point to categorize participants into the mid-high altitude group and the ultra-high altitude group.
Assessment of CSVD
The MRI scans were conducted on a 3.0 T Philips system (Best, Netherlands), following a standardized protocol that included T1-weighted, T2-weighted, and T2-FLAIR sequences. The assessment of MRI markers for CSVD was based on the Standards for Reporting Vascular Changes in Neuroimaging (STRIVE) criteria20. These criteria, developed through expert consensus, guide the reporting of vascular changes such as recent small subcortical infarcts (RSSI), lacunar infarctions (LI), cerebral microbleeds (CMB), white matter hyperintensities (WMH), enlarged perivascular spaces (EPVS), and brain atrophy. The use of the STRIVE criteria ensures consistent and accurate reporting, improving diagnostic precision and facilitating research into the clinical implications of these changes.
WMH were graded using the Fazekas scale based on T2-weighted or FLAIR sequences21. Periventricular WMH were classified as 0 points (no visible lesion), 1 point (caps or pencil lining), 2 points (smooth halo), and 3 points (irregular periventricular hyperintensity extending into deep white matter). Deep WMH were graded as 0 points (no visible lesion), 1 point (punctate lesions), 2 points (beginning confluence of lesions), and 3 points (large confluent lesions). Lacunar infarctions (LI) were identified as round or oval-shaped lesions, 3–15 mm in diameter, with central cerebrospinal fluid-like low signal on T2-weighted and FLAIR sequences, surrounded by high signal but not high signal on diffusion-weighted imaging (DWI)20. Recent small subcortical infarcts (RSSI) were identified as lesions with high signal on DWI, T2-weighted, and FLAIR sequences, but low signal on T1-weighted imaging, with a size ≤ 20 mm20. EPVS were defined as fluid-filled spaces surrounding vessels penetrating gray or white matter. These spaces appeared as point-like or linear shadows with cerebrospinal fluid on T1-weighted, T2-weighted, and FLAIR sequences, usually measuring < 3 mm in diameter. EPVS severity was graded based on the highest count in unilateral basal ganglia, with the following classification: grade 1 (1–10 spaces), grade 2 (11–20 spaces), grade 3 (21–40 spaces), and grade 4 (> 40 spaces or uncountable)22.
The CSVD burden score, which integrates multiple imaging markers (Due to the absence of SWI sequences in our MRI protocol, the composite CSVD burden score was calculated based on the presence of LI, RSSI, WMH, and EPVS) was used to quantify CSVD severity23,24. The total score ranged from 0 to 4 points, categorized as non-mild (0–1 point) or moderate (2–4 points)24,25. The score was determined by the presence of ≥ 1 lacunar infarct (1 point), ≥ 1 recent small subcortical infarct (1 point), moderate to severe EPVS (grades 2–4) (1 point), and Fazekas grade 3 periventricular white matter hyperintensity or grade ≥ 2 deep-brain white matter hyperintensity (1 point)23,25. This detailed scoring approach facilitates a more precise understanding of CSVD and its clinical relevance.
Assessment of covariates
Upon admission, anthropometric data were recorded. Weight and height were measured in accordance with World Health Organization guidelines, with participants wearing lightweight clothing and no footwear. The body mass index (BMI) was computed by dividing weight (kg) by height squared (m2). Blood pressure was measured twice using a digital sphygmomanometer, following standardized protocols. Participants were seated for at least 5 min of rest before measurements, and the average of the two readings was taken as the final value.
Sociodemographic information collected included sex, age, smoking status (categorized as non-smoker, former smoker, or current smoker), alcohol consumption (classified as non-drinker, former drinker, or current drinker), and residential altitude. Medical histories regarding cardiovascular disease (CVD) risk factors such as hypertension, type 2 diabetes, coronary artery disease (CAD), stroke, and hyperlipidemia were retrieved from participants’ medical records. The use of medications, including antihypertensives, glucose-lowering agents, antiplatelet drugs, and lipid-lowering medications, was also documented.
On the first day after admission, routine laboratory tests were performed following an overnight fast. These tests included measurements of fasting plasma glucose (FPG), triglycerides, total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), aspartate aminotransferase, alanine aminotransferase, estimated glomerular filtration rate (eGFR), and a complete blood count, which assessed parameters such as red blood cells (RBC), white blood cells (WBC), hemoglobin (HB) levels, hematocrit (Hct), and platelet count (PLT).
To explore the potential effect modification by manifest arterial disease (MAD) on the altitude–CSVD severity association, we conducted stratified analyses using MAD as the primary stratification variable. MAD was defined according to established clinical criteria26 and included: (1) coronary artery disease (CAD), confirmed by a documented history of myocardial infarction, coronary revascularization, or angiographically verified stenosis > 70%; (2) cerebrovascular disease, including either neuroimaging-confirmed ischemic stroke (acute or chronic) or clinically diagnosed transient ischemic attacks meeting WHO criteria; and (3) peripheral arterial disease (PAD), defined by either prior surgical or endovascular treatment for lower limb arterial stenosis or objective evidence of resting ischemia or claudication.
Statistical analyses
Descriptive statistics were utilized to summarize the characteristics of the study cohort. The Shapiro–Wilk test was applied to evaluate the normality of the data distribution. Continuous descriptive variables were stratified based on the classification of high-altitude exposure and the severity of CSVD, presenting normally distributed data as mean ± standard deviation, and non-normally distributed data as median (interquartile range). Categorical variables were reported as frequencies and percentages. Group comparisons for continuous variables were conducted using either the two-sample t-test or the Mann–Whitney U test, depending on the distribution of the data. For categorical variables, either the chi-square test or Fisher’s exact test was used as appropriate.
To evaluate the associations between residential altitude, CSVD severity, and its MRI markers, multivariable logistic regression analyses were performed. The primary outcome, defined as CSVD severity, was derived from the cumulative score of four neuroimaging markers (LI, RSSI, WMH, EPVS), and modelled as a binary variable (moderate-to-severe vs non-mild; with results reported as adjusted odds ratios [ORs] and 95% confidence intervals [CIs]). The presence of each MRI marker was considered a binary secondary outcome, analysed in separate logistic regression models. Variables demonstrating statistical significance (P < 0.05) in univariate analyses, along with clinically pertinent covariates, were included in the multivariable models. Model 1 was unadjusted, whereas Model 2 adjusted for age, sex, smoking status, alcohol consumption, HB, hypertension, diabetes mellitus, CAD, hyperlipidemia, and history of stroke.
To assess the robustness of the findings, a series of sensitivity analyses was conducted. First, altitude was incorporated into logistic regression models both as a continuous and a categorical variable to evaluate its associations with CSVD and associated neuroimaging markers. To enhance clinical interpretability, altitude was incorporated as a continuous variable ("altitude per 500 m" –calculated as altitude divided by 500). This transformation facilitated a more intuitive assessment of exposure-outcome relationships. Second, given the non-normal distribution of the CSVD burden score (range: 0–4; Shapiro–Wilk test: W = 0.79, p < 0.001; see FigureS1 for distribution histogram), sensitivity analyses treated this score as an ordinal outcome using partial proportional odds (PPO) models. The Brant test revealed violation of the proportional odds assumption for sex (χ2 = 9.39, p = 0.02) but not for altitude (χ2 = 2.6, p = 0.46). Consequently, a PPO model was implemented via the VGAM package in R, permitting non-proportional odds for sex while maintaining proportional odds constraints for altitude effects.
Previous studies have suggested a dual effect of altitude on stroke risk. To further explore whether different altitude levels also exhibit varying associations with CSVD, we conducted repeated analyses in both the mid-high altitude and ultra-high altitude groups, entering altitude as a continuous variable in logistic regression models.
CSVD primarily reflects Type 1 small vessel pathology, closely linked to vascular risk factors. To reduce confounding, we performed logistic subgroup analyses stratified by age (< 60 vs ≥ 60 years), residential altitude (mid-high vs ultra-high), and MAD status (yes vs no). Interactions between altitude and these factors were assessed using likelihood ratio tests.
All statistical analyses were performed using R version 4.3.1 (http://www.R-project.org, The R Foundation) and Free Statistics software version 2.027. A two-tailed test was used, and a p-value of less than 0.05 was considered statistically significant.
Results
Characteristics of the participants
Among the 499 participants, 51.5% (257/499) had CSVD (CSVD score ≥ 1). The mean age was 57.6 ± 11.7 years, with a slightly higher proportion of males than females (55.8% vs. 44.2%). Tables 1 and 2 detail the demographic and clinical characteristics stratified by altitude and CSVD severity. The mean residential altitude was 3746.2 ± 481.6 m. Compared to those at mid-to-high altitudes, participants at ultra-high altitudes had significantly higher hemoglobin levels and hematocrit but a lower prevalence of diabetes (all p < 0.05). Additionally, compared to the non-mild CSVD group, the moderate-to-severe CSVD group had a higher proportion of males and a greater prevalence of hypertension, coronary artery disease (CAD), and stroke. The distribution of smoking and alcohol consumption also differed significantly between the two groups (all p < 0.05).
Association between altitude and the severity of CSVD and MRI markers of CSVD among the 499 study participants
Multivariable logistic regression was used to assess the relationship between altitude and CSVD. Whether altitude was analyzed as a continuous variable (per 500 m increase) or a categorical variable (mid-to-high vs. ultra-high altitude), no significant association was found with CSVD (altitude per 500 m: OR = 0.94, 95% CI: 0.74–1.21; mid-to-high vs. ultra-high altitude: OR = 0.78, 95% CI: 0.42–1.44) or MRI markers of CSVD after adjusting for confounders (all p > 0.05, Table 3).
To ensure the robustness of these findings, additional PPO model analyses was conducted using CSVD score as an ordinal outcome. The results remained consistent, showing no significant association between altitude and CSVD score after adjustment (OR = 1.18, 95% CI 0.99–1.40, p = 0.061, sTable 1). This concordance underscores the robustness of our null findings.
Association between altitude per 500 and the severity of CSVD and MRI markers of CSVD among mid-high altitude and ultra-high altitude participants
Previous studies suggest altitude may have a dual effect on stroke risk. To explore whether altitude influences CSVD differently, we conducted subgroup analyses for mid-to-high and ultra-high altitude participants. Due to the limited number of RSSI and LI cases in the mid-to-high altitude group, these associations were not analyzed in this subgroup. After adjusting for confounders, altitude per 500 m showed no significant association with CSVD severity or MRI markers in either altitude group (all p > 0.05, Table 4).
Subgroup analysis
Logistic subgroup analyses stratified by age, altitude, and MAD status yielded results consistent with the main analysis. No statistically significant interactions were observed between altitude and any of these stratification factors (Figure S2).
Discussion
This study, conducted among the Tibetan population residing on the Tibetan Plateau, identified a substantial burden of CSVD, with 51.5% of participants (mean age: 57.6 ± 11.7 years) exhibiting at least one CSVD imaging marker. However, multivariable regression analyses revealed no significant association between residential altitude and the overall CSVD severity or individual imaging features. This finding suggests that the mechanisms by which altitude influences CSVD may differ from those affecting stroke pathogenesis.
Among our study population, nearly 50% of participants had at least one CSVD imaging marker (total CSVD score ≥ 1), with WMH being the most prevalent (27.9%), followed by LI (11.0%), basal ganglia EPVS, (10.0%), and RSSI (6.2%). Compared to low-altitude populations, we observed a notably higher prevalence of CSVD. A cross-sectional study conducted in community-dwelling residents of Lishui, China, reported that only 30.5% had at least one positive CSVD marker28. Furthermore, our study confirmed that WMH was the most frequent CSVD imaging feature, whereas basal ganglia EPVS and RSSI were the least common, aligning with previous findings28,29,30. A multi-center study conducted in three Asian regions (Singapore, Hong Kong, and South Korea) similarly reported that confluent WMH had the highest prevalence (36.6%) among all CSVD markers29. Additionally, a comparative study of hospitalized acute stroke patients in Lhasa, Tibet, and Beijing found that the proportion of small vessel occlusion was significantly lower in Tibet than in the lowland region (3.0% vs. 23.7%; p < 0.001)30. The presence of an early-onset CSVD burden in this relatively young population highlights a unique cerebrovascular vulnerability potentially driven by chronic high-altitude exposure. Although the exact mechanisms remain unclear, several factors may contribute: (1) Chronic hypoxia may induce endothelial dysfunction31; (2) Hemodynamic stress adaptation—evidence from a comparative study in high-altitude and sea-level populations in Peru suggests impaired cerebrovascular reactivity at high altitudes32; (3) The EPAS1 gene, which carries widespread variants in the Tibetan population, is associated with a reduction in VEGF expression, possibly impairing microvascular repair capacity33. This premature CSVD burden underscores the need for earlier neurovascular monitoring and more intensive management of modifiable risk factors (e.g., targeting blood pressure levels < 130/80 mmHg) in high-altitude populations.
Despite previous studies indicating a higher prevalence of acute stroke in high-altitude populations12,34,35, we did not observe an association between altitude and RSSI or lacunar infarcts. This may be attributed to the characteristic features of high-altitude stroke, which tend to involve larger infarct volumes and more severe clinical presentations36. Previous research has also demonstrated a lower prevalence of small vessel occlusion in high-altitude stroke patients compared to their lowland counterparts30, a trend that was also evident in our study population. Additionally, our study is the first to explore the relationship between altitude and EPVS, revealing no significant association. Further comparative studies between lowland and high-altitude populations are warranted to validate these findings.
We found no significant association between WMH and residential altitude, which contrasts with previous studies on participants exposed to low-pressure, hypoxic environments due to occupational factors, such as high-altitude pilots and military divers37,38. These studies reported an increased prevalence of WMH in these populations37,38. The discrepancy may be attributed to differences in ethnicity, age distribution, study populations, statistical models, and WMH assessment methods. The participants in previous studies were relatively young (mean age 34–37 years), physically healthy, and free from major cardiovascular risk factors37,38. In contrast, our study focused on the indigenous Tibetan population, with a higher mean age (57.6 ± 11.7 years) and a high prevalence of comorbid conditions such as hypertension, diabetes, dyslipidemia, and coronary artery disease. Acute exposure to hypoxia induces endothelial dysfunction, initially increasing cerebral blood flow and vascular permeability, potentially leading to brain injury39,40. However, chronic adaptation results in compensatory mechanisms that restore cerebral blood flow, including increased hemoglobin concentration, hematocrit, red blood cell count, and vascular density, ultimately enhancing cerebral oxygenation39. Additionally, a PET study revealed that, compared to lowlanders, Quechua natives—indigenous inhabitants of the high-altitude Andes—exhibited lower glucose metabolism, suggesting a protective mechanism against chronic hypoxia41. Moreover, genetic adaptations in Tibetans, such as EPAS1 and EGLN1 gene variants42,43, along with physiological adaptations, may mitigate hypoxia-induced damage to cerebral small vessels. Future studies integrating genomics, metabolomics, and neuroimaging are necessary to comprehensively elucidate the impact of altitude on CSVD and its underlying mechanisms.
In our study, residents living at ultra-high altitudes (> 3,500 m) demonstrated significantly lower prevalences of both hypertension and type 2 diabetes compared to those residing at mid-to-high altitudes (2,000–3,500 m). This observation is consistent with findings from several large-scale epidemiological studies. For instance, a nationally representative survey in Peru reported that participants living above 2,500 m had significantly lower hypertension rates than those at lower altitudes (adjusted prevalence ratio = 0.89; 95% CI: 0.86–0.93)44. A systematic review across Latin America and the Caribbean likewise demonstrated a lower risk of hypertension among high-altitude populations45. Notably, a cross-sectional study involving 1,631 Tibetan participants revealed a pronounced decline in hypertension prevalence with increasing elevation (20.4 vs. 40.6%)46, providing strong support for our findings in a similar ethnic and environmental context. Additionally, U.S. data showed that high-altitude residence (1500–3500 m) was associated with a lower adjusted prevalence of type 2 diabetes47.
Several mechanisms may underlie the reduced cardiometabolic burden in high-altitude populations. Chronic hypobaric hypoxia may promote vascular adaptations such as increased nitric oxide availability and improved endothelial function, thereby reducing systemic vascular resistance and blood pressure48. Hematologic adaptations, including elevated hemoglobin and hematocrit levels, enhance oxygen delivery and may contribute to vascular homeostasis49.
Regarding glucose metabolism, hypoxia has been shown to improve mitochondrial efficiency and activate AMPK-related pathways, which enhance insulin sensitivity and glucose utilization50. Furthermore, high-altitude residents tend to maintain lower body mass indices and reduced caloric intake51, both of which protect against insulin resistance and type 2 diabetes. Genetic variants prevalent among Tibetan highlanders—such as EPAS1 and EGLN1 polymorphisms—may further facilitate metabolic adaptation to chronic hypoxia42.
As far as we are aware, few studies have specifically examined the association between altitude and CSVD, making our research pioneering in this area. This is the first study to explore the relationship between residential altitude and both the severity of CSVD and its associated imaging biomarkers in a native Tibetan population residing on the Tibetan Plateau. Our work fills an important gap in the existing literature on CSVD in high-altitude environments. The results indicate that the Tibetan population, which has adapted to high-altitude living over extended periods, may possess unique physiological adaptations to chronic hypoxia. Notably, 84% of our study cohort resides at altitudes above 3500 m, providing valuable insights for cerebrovascular health management in ultra-high-altitude populations. Additionally, we employed a range of imaging biomarkers (including WMH, LI, RSSI, and EPVS) to assess the severity of CSVD and investigate the relationship between altitude and these imaging markers, offering a comprehensive phenotypic analysis of CSVD.
The study also has some limitations. This investigation is a cross-sectional study conducted in a single center, and as such, it may be influenced by selection bias. The proportion of participants residing in moderate-to-high-altitude regions is comparatively low (only 15%), which restricts the external validity of our findings to the broader Tibetan population residing on the Tibetan Plateau. Although our primary analysis did not reveal a significant association between residential altitude and the burden of CSVD, this result should be interpreted in the context of the limited altitude variation within our study population. Specifically, approximately 85% of participants resided at ultra-high altitudes (> 4500 m), potentially introducing a ceiling effect that may have obscured a possible dose–response relationship. This demographic concentration at extreme altitudes restricts our ability to detect subtle gradient effects across different altitude levels. Future research should pursue multi-center collaborations involving a broader cohort spanning from sea level to high-altitude regions to more comprehensively investigate the altitude–CSVD relationship and improve the generalizability of the findings. Furthermore, the cross-sectional nature of this study prevents the establishment of causal relationships. Longitudinal studies are warranted to evaluate the long-term effects of hypoxia on the progression of CSVD and to elucidate the causal pathways linking altitude to CSVD. Additionally, our study did not control for potential confounding variables such as lifestyle factors, dietary habits, and genetic predispositions, which could influence the relationship between altitude and CSVD.
Conclusion
This observational study conducted among the Tibetan population residing on the Tibetan Plateau identified a notable burden of CSVD. However, no significant association was observed between residential altitude and the severity of CSVD or its imaging biomarkers. These findings provide novel insights into the potential influence of high-altitude environments on CSVD, suggesting that the effects of altitude on CSVD may differ from its known associations with stroke. In clinical practice at high altitudes, greater emphasis should be placed on the management of conventional cardiovascular risk factors rather than on the elevation per se. For high-altitude residents, particularly older participants, routine brain imaging is recommended for early detection and timely intervention of CSVD. Interventions such as lifestyle modifications52, blood pressure control53, and cognitive training54 may be beneficial, though their effectiveness in high-altitude populations remains to be established. Future studies should further explore the unique adaptive mechanisms in the Tibetan population and expand the scope of investigation to elucidate the complex relationship between altitude and CSVD, as well as its broader clinical implications.
Data availability
The datasets generated or analyzed during the current study are not publicly available due to ethical restrictions but are available from the corresponding author upon reasonable request.
References
de Leeuw, F. E. et al. Prevalence of cerebral white matter lesions in elderly people: a population based magnetic resonance imaging study. The Rotterdam Scan Study. J. Neurol. Neurosurg. Psychiatry 70, 9–14 (2001).
Hussein, H. M. & Anderson, D. C. Small vessel disease: Perpetrator or predictor of stroke in patients with atrial fibrillation?. Stroke 52, 100–102 (2021).
Wardlaw, J. M., Smith, C. & Dichgans, M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. 18, 684–696 (2019).
Peng, D., Geriatric Neurology Group, Chinese Society of Geriatrics, & Clinical Practice Guideline for Cognitive Impairment of Cerebral Small Vessel Disease Writing Group. Clinical Practice Guideline for Cognitive Impairment of Cerebral Small Vessel Disease. Aging Med. Milton NSW 2, 64–73 (2019).
Boyle, P. A. et al. Person-specific contribution of neuropathologies to cognitive loss in old age. Ann. Neurol. 83, 74–83 (2018).
Prince, M., Wimo, A., Guerchet, M., Ali, G.-C., Wu, Y.-T., & Prina, M. World Alzheimer Report 2015. The Global Impact of Dementia: An Analysis of Prevalence, Incidence, Cost and Trends. Alzheimer's Disease International (ADI). https://www.alzint.org/resource/world-alzheimer-report-2015/ (2015).
Wang, W. et al. Prevalence, incidence, and mortality of stroke in China: Results from a nationwide population-based survey of 480 687 adults. Circulation 135, 759–771 (2017).
Pan, Z.-A. et al. Risk factor differences in five-year progression of Intracranial artery stenosis and cerebral small vessel disease in general population. BMC Neurol. 24, 328 (2024).
West, J. B. High-altitude medicine. Am. J. Respir. Crit. Care Med. 186, 1229–1237 (2012).
Tremblay, J. C. & Ainslie, P. N. Global and country-level estimates of human population at high altitude. Proc. Natl. Acad. Sci. U. S. A. 118, e2102463118 (2021).
Sherpa, L. Y. et al. Prevalence of metabolic syndrome and common metabolic components in high altitude farmers and herdsmen at 3700 m in Tibet. High Alt. Med. Biol. 14, 37–44 (2013).
Jha, S. K., Anand, A. C., Sharma, V., Kumar, N. & Adya, C. M. Stroke at high altitude: Indian experience. High Alt. Med. Biol. 3, 21–27 (2002).
Winkelmayer, W. C., Hurley, M. P., Liu, J. & Brookhart, M. A. Altitude and the risk of cardiovascular events in incident US dialysis patients. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transplant. Assoc. Eur. Ren. Assoc. 27, 2411–2417 (2012).
Faeh, D., Gutzwiller, F., Bopp, M., Swiss National Cohort Study Group. Lower mortality from coronary heart disease and stroke at higher altitudes in Switzerland. Circulation 120, 4095–4501 (2009).
Tang, X. et al. Association of kidney function and brain health: A systematic review and meta-analysis of cohort studies. Ageing Res. Rev. 82, 101762 (2022).
Milewski, K., Orzeł-Gajowik, K. & Zielińska, M. Mitochondrial changes in rat brain endothelial cells associated with hepatic encephalopathy: Relation to the blood-brain barrier dysfunction. Neurochem. Res. 49, 1489–1504 (2024).
Sharma, A., Mannan, A., Singh, S. & Singh, T. G. A second act for spironolactone: cognitive benefits in renal dysfunction - a critical review. Metab. Brain Dis. 40, 194 (2025).
Gurevich, M., Waknin, R., Stone, E. & Achiron, A. Fingolimod-improved axonal and myelin integrity of white matter tracts associated with multiple sclerosis-related functional impairments. CNS Neurosci. Ther. 24, 412–419 (2018).
Imray, C., Booth, A., Wright, A. & Bradwell, A. Acute altitude illnesses. BMJ 343, d4943 (2011).
Wardlaw, J. M. et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 12, 822–838 (2013).
Fazekas, F. et al. Pathologic correlates of incidental MRI white matter signal hyperintensities. Neurology 43, 1683–1689 (1993).
Perivascular spaces in the brain: anatomy, physiology and pathology - PubMed. https://pubmed.ncbi.nlm.nih.gov/32094487/.
Staals, J., Makin, S. D. J., Doubal, F. N., Dennis, M. S. & Wardlaw, J. M. Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology 83, 1228–1234 (2014).
Kaffashian, S. et al. Long-term clinical impact of vascular brain lesions on magnetic resonance imaging in older adults in the population. Stroke 47, 2865–2869 (2016).
Zhang, L. et al. Analysis of risk factors for the development of cognitive dysfunction in patients with cerebral small vessel disease and the construction of a predictive model. Front. Neurol. 13, 944205 (2022).
Tiehuis, A. M. et al. Metabolic syndrome, prediabetes, and brain abnormalities on mri in patients with manifest arterial disease: the SMART-MR study. Diabetes Care 37, 2515–2521 (2014).
Yao, S. & Chen, X.-W. Association of pain with falls and fractures among middle-aged Korean community-dwelling adults. J. Gerontol. A Biol. Sci. Med. Sci. 80, glae241 (2025).
Yang, Y. et al. Prevalence and risk factors of cerebral small vessel disease from a population-based cohort in China. Neuroepidemiology 57, 413–422 (2023).
Hilal, S. et al. Prevalence, risk factors and consequences of cerebral small vessel diseases: data from three Asian countries. J. Neurol. Neurosurg. Psychiatry 88, 669–674 (2017).
Lu, Y. et al. Characteristics of acute ischemic stroke in hospitalized patients in Tibet: a retrospective comparative study. BMC Neurol. 20, 380 (2020).
Pichler Hefti, J. et al. Increased endothelial microparticles and oxidative stress at extreme altitude. Eur. J. Appl. Physiol. 116, 739–748 (2016).
Norcliffe, L. J. et al. Cerebrovascular responses to hypoxia and hypocapnia in high-altitude dwellers. J. Physiol. 566, 287–294 (2005).
Yang, J. et al. Genetic signatures of high-altitude adaptation in Tibetans. Proc. Natl. Acad. Sci. U. S. A. 114, 4189–4194 (2017).
Ortiz-Prado, E., Cordovez, S. P., Vasconez, E., Viscor, G. & Roderick, P. Chronic high-altitude exposure and the epidemiology of ischaemic stroke: a systematic review. BMJ Open 12, e051777 (2022).
Li, Z., Hu, Q., Ji, W. & Fan, Q. Prevalence of stroke and associated risk factors: a population-based cross-sectional study from the Qinghai-Tibet Plateau of China. BMJ Open 12, e065605 (2022).
Liu, M. et al. Acute ischemic stroke at high altitudes in China: Early onset and severe manifestations. Cells 10, 809 (2021).
Erdem, I. et al. Cerebral white-matter lesions in asymptomatic military divers. Aviat. Space Environ. Med. 80, 2–4 (2009).
McGuire, S. et al. White matter hyperintensities on MRI in high-altitude U-2 pilots. Neurology 81, 729–735 (2013).
Olopade, J. O., Mensah, E., Gupta, S., Noro, S.eki, S., & De Jesus, J. F. A method for measuring brain partial pressure of oxygen in unanesthetized unrestrained subjects: The effect of acute and chronic hypoxia on brain tissue PO2. J. Neurosci. Methods 193(2), 217–225 (2010).
Luks, A. M., Swenson, E. R. & Bärtsch, P. Acute high-altitude sickness. Eur. Respir. Rev. Off. J. Eur. Respir. Soc. 26, 160096 (2017).
Hochachka, P. W. et al. The brain at high altitude: hypometabolism as a defense against chronic hypoxia?. J. Cereb. Blood Flow Metab. 14, 671–679 (1994).
Yi, X. et al. Sequencing of 50 human exomes reveals adaptation to high altitude. Science 329, 75–78 (2010).
Petousi, N. & Robbins, P. A. Human adaptation to the hypoxia of high altitude: the Tibetan paradigm from the pregenomic to the postgenomic era. J. Appl. Physiol. 1985(116), 875–884 (2014).
Ortiz-Saavedra, B., Montes-Madariaga, E. S., Moreno-Loaiza, O. & Toro-Huamanchumo, C. J. Hypertension subtypes at high altitude in Peru: Analysis of the demographic and family health survey 2016–2019. PLoS ONE 19, e0300457 (2024).
Zila-Velasque, J. P. et al. Prevalence of hypertension in adults living at altitude in Latin America and the Caribbean: A systematic review and meta-analysis. PLoS ONE 18, e0292111 (2023).
Song, C. et al. Relationship between hypertension and geographic altitude: a cross-sectional survey among residents in Tibet. J. Int. Med. Res. 48, 300060520903645 (2020).
Woolcott, O. O. et al. Inverse association between diabetes and altitude: a cross-sectional study in the adult population of the United States. Obes. Silver Spring Md. 22, 2080–2090 (2014).
Beall, C. M., Laskowski, D. & Erzurum, S. C. Nitric oxide in adaptation to altitude. Free Radic. Biol. Med. 52, 1123–1134 (2012).
Simonson, T. S. Altitude adaptation: A glimpse through various lenses. High Alt. Med. Biol. 16, 125–137 (2015).
Chen, Y.-C., Lee, S.-D., Kuo, C.-H. & Ho, L.-T. The effects of altitude training on the AMPK-related glucose transport pathway in the red skeletal muscle of both lean and obese Zucker rats. High Alt. Med. Biol. 12, 371–378 (2011).
Woolcott, O. O., Seuring, T. & Castillo, O. A. Lower prevalence of body fat-defined obesity at higher altitudes in Peruvian adults. High Alt. Med. Biol. 24, 214–222 (2023).
Simpson, F. R. et al. Does the impact of intensive lifestyle intervention on cardiovascular disease risk vary according to frailty as measured via deficit accumulation?. J. Gerontol. A Biol. Sci. Med. Sci. 76, 339–345 (2021).
Goldstein, E.D., Wolcott, Z., Garg, G., Navarro, K., Delic, A., Yaghi, S., Sederholm, B., Prabhakaran, S., Wong, K.H., McLean, K., de Havenon, A.H. Effect of Antihypertensives by Class on Cerebral Small Vessel Disease: A Post Hoc Analysis of SPRINT-MIND. Stroke 53(8), 2435–2440 (2022).
Hill, N. T. M. et al. Computerized cognitive training in older adults with mild cognitive impairment or dementia: A systematic review and meta-analysis. Am. J. Psychiatry 174, 329–340 (2017).
Acknowledgments
We want to express our deep gratitude to the participants who gave their time and consent to participate in the research. We thank Free Statistics team for providing technical assistance and valuable tools for data analysis and visualization. We would like to extend our gratitude to Mr. Yong Cao (Department of Information, Hospital of Chengdu Office of People’s Government of Tibetan Autonomous Region) for extracting the laboratory data for this study. The funder had no role in the study design, data collection, analysis, interpretation, or writing of the manuscript.
Funding
This study was supported by the hospital-level research project of the Hospital of Chengdu Office of People’s Government of Tibetan Autonomous Region Chengdu, China (grant number: 2022-YJ-3).
Author information
Authors and Affiliations
Contributions
SY and XC conceived of the study. SY acquired funding and supervised the project. SY, SMB, YYX, HRF, QZ, and ZRQ wrote the original draft. SY, XC, SMB, YYX, HRF, QZ, ZRQ, YT, and WHG reviewed and edited the manuscript. All author qualifications meet the criteria of ICMJE or relevant institutions. No professional medical writers will be used for the preparation of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by the Institutional Review Board (IRB number: 2022-65) of the hospital, and written informed consent was obtained from all participants at enrollment.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yao, S., Qi, Zr., Bao, Sm. et al. The association between altitude and cerebral small vessel disease burden in the Tibetan population: a cross-sectional study. Sci Rep 15, 24035 (2025). https://doi.org/10.1038/s41598-025-09891-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09891-2