Abstract
Chronic wasting disease (CWD) is a fatal neurodegenerative disease affecting cervids across North America, Northern Europe, and Asia. Disease transmission among cervids has historically been attributed to direct animal-to-animal contact with ‘secreta’ (saliva, blood, urine, and feces) containing the infectious agent, and indirect contact with the agent shed to the environment in these bodily components. Mounting evidence provides another mechanism of CWD transmission, that from mother-to-offspring, including during pregnancy (vertical transmission). Here we describe the detection of the infectious CWD agent and prion seeding in fetal and reproductive tissues collected from healthy-appearing free-ranging white-tailed deer (Odocoileus virginianus) from multiple U.S. states by mouse bioassay and in vitro prion amplification assays. This is the first report of the infectious agent in multiple in utero derived fetal and maternal-fetal reproductive tissues, providing evidence that CWD infections are propagated within gestational fetal tissues of white-tailed deer populations. This work confirms previous experimental and field findings in several cervid species supporting vertical transmission as an additional mechanism of CWD transmission and may help to further explain the facile dissemination of this disease among captive and free-ranging cervid populations.
Similar content being viewed by others
Introduction
Chronic wasting disease (CWD) is an efficiently transmitted prion disease of captive and free-ranging cervid species (deer, elk, moose, reindeer) that continues to be detected in parts of North America, Scandinavia, and Asia1,2,3,4. Transmissible spongiform encephalopathies (TSEs), including CWD, affect the central nervous system causing slow and progressive neurological damage resulting in behavioral changes, wasting, and eventual death5. It has been confirmed that infectious CWD prions are shed in ‘secreta’ (saliva, blood, urine and feces) during the characteristic long asymptomatic phase of disease, which can range from months to years6,7,8,9. Prions shed in secreta to the environment and those in the carcass after death have robust stability, withstanding degradation and remaining infectious for many years10,11,12,13. Thus, the facile dissemination of CWD among cervids has largely been attributed to contact with the infectious agent via direct animal-to-animal contact (e.g., grooming, breeding, birthing fluids) and indirect interactions with the infectious agent shed to the environment (e.g., foraging, tree rubs, mineral licks, soil consumption)14,15,16,17,18. What remains less understood is the role of maternal CWD infections and mother-to-offspring (vertical) transmission.
Previous studies have reported that offspring born to prion-infected deer, cattle, and sheep are at risk for developing CWD, bovine spongiform encephalopathy (BSE), and scrapie, respectively19,20,21,22. Maternal transmission of feline spongiform encephalopathy (FSE) has been implicated in a seven-year-old cheetah born to an FSE-infected mother that was raised in a TSE-free environment yet developed FSE23. To date there are no reports of human Creutzfeldt-Jakob disease (CJD) mother-to-offspring transmission, yet, prion deposition and infectivity have been demonstrated in human reproductive tissues and cord blood of variant CJD (vCJD) patients24,25. Several additional studies provide strong evidence for in utero or vertical prion transmission. in vitro prion deposition has been detected in reproductive tissues (ovary, uterus, placentomes, and amniotic fluid) of scrapie-infected sheep26,27,28.
We first described CWD exposure prior to parturition upon the demonstration of PrPCWD immunohistochemical (IHC) deposition within tonsillar lymphoid biopsies as early as 41 days post parturition in offspring born to experimental CWD-infected Reeves’ muntjac (Muntiacus reevesi) dams22. In these studies, amplifiable prions were demonstrated in multiple maternal reproductive tissues/fluids and fetal samples harvested throughout gestation demonstrating that in utero transmission could occur at any stage of gestation or CWD infection22,29. More importantly, we demonstrated the presence of the infectious prion agent within tissues of the maternal pregnancy microenvironment (placentomes, uterus, amniotic fluids) that had the capacity to initiate CWD infections and disease progression when inoculated into transgenic mice29. What remained unknown is if these findings would hold true for naturally infected, free-ranging cervid species that most assuredly receive smaller doses of CWD in their natural environment. Subsequently, we and others have detected amplifiable prions in dam reproductive and fetal tissues harvested from naturally exposed CWD-infected Rocky Mountain elk (Cervus canadensis nelsoni) and white-tailed deer (WTD; Odocoileus virginianus)30,31,32. What has not been shown is if the prion detection in these tissues is infectious. Thus, an overarching question has been, does prion deposition within gestational tissues of free-ranging cervids result in fetal prion infections?
Here, we assessed maternal reproductive tissues/fluids, and in utero derived fetal tissues from free-ranging WTD naturally exposed to CWD for the presence of prion seeding activity (prions) by amplification assays (protein misfolding amplification assay (PMCA) and real-time quaking induced conversion (RT-QuIC)). More importantly, to determine the biological relevance of in vitro prion detection, we assessed reproductive and fetal tissues for the presence of infectivity by bioassay in cervid prion protein (Prnp) transgenic mice. Bioassay is the only way to assess for the presence of the infectious agent that is known to lead to the initiation and progression of prion infections.
To account for the potential that Prnp genotype may impact vertical transmission, as has been demonstrated in sheep scrapie26,33 and is well known to affect cervid prion susceptibility34 disease progression and shedding34,35,36 we assessed the Prnp genotypes at codon 95 & 96 of both dams and fetuses, and correlated these findings to CWD disease status. Finally, as previous experimental studies in the native host demonstrate that CWD high dose saliva, blood and fomite exposures resulted in first CWD positive status between 12 and 19 months post-inoculation15 we retrospectively examined historical CWD surveillance data from three study sites in Arkansas (AR), Tennessee (TN), and West Virginia (WV) to look for evidence of natural infection in WTD fawns less than 12 months of age using tests of similar sensitivity (western blot and ELISA respectively)37.
We report the presence of the infectious CWD agent within the pregnancy microenvironment and fetal tissues of free-ranging, naturally exposed WTD (i.e. vertical transmission). This demonstrates that CWD can cross the maternal-fetal interface to initiate an active gestational infection. Our findings also reveal that no case of fetal positivity was identified when the codon 96 serine residue was expressed by either dam or fetus, yet, expanded studies will be required to fully address the impact of Prnp polymorphisms on vertical transmission. Furthermore, upon examination of historical CWD surveillance data using conventional tests (e.g., ELISA) CWD test positive WTD fawns < 6–10 months of age were identified. As described above, these findings suggest an earlier exposure to CWD than postpartum maternal saliva, blood, or environmental contact15. These findings lend biological relevance to earlier detection of in vitro prion seeding activity within maternal reproductive and fetal tissues of experimental and free-ranging cervids22,30,31,32 and demonstrates that in utero/vertical transmission is another factor in the transmission dynamics of CWD in the native cervid host.
Results
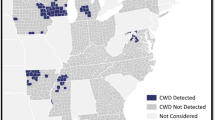
CWD detected in free-ranging white-tailed deer dams from Arkansas, Tennessee, and West Virginia
To survey the extent of CWD dissemination within free-ranging WTD, we evaluated peripheral lymphoid tissues (retropharyngeal lymph node (RPLN), tonsil, rectoanal mucosa-associated lymphoid tissue (RAMALT), and third eyelid) and central nervous system tissue (obex) from a total of n = 31 WTD dams by IHC and RT-QuIC (n = 28 from CWD endemic areas and n = 3 from a CWD nonendemic area). From our CWD endemic study cohort (n = 28), we detected CWD seeding activity and/or PrPCWD deposition in 16 of 28 (57.1%) RPLN, 14 of 28 (50.0%) tonsil, 12 of 28 (42.8%) RAMALT, 11 of 28 (39.2%) third eyelid, and 8 of 28 (28.6%) obex tissues (Table 1). The detection of CWD by RT-QuIC amyloid seeding preceded or coincided with IHC detection in all but three samples (Table 1). Additionally, in dams with sufficient secreta collected to assess prion shedding (n = 27 saliva; n = 21 urine), amyloid seeding was detected in 3 of 27 (11.1%) saliva samples and 0 of 21 (0%) urine samples (Table 1). Overall, 16 of the 28 dams were CWD-positive on one or more tests with results from each state as follows: 3 of 10 (30.0%) Arkansas, 8 of 10 (80.0%) Tennessee, and 5 of 8 (62.5%) West Virginia. All negative control deer harvested in Georgia (n = 3) had no detectable prions in all samples tested.
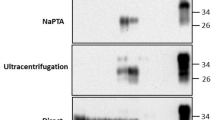
in vitro prion seeding present within the pregnancy microenvironment of free-ranging white-tailed deer
We assessed the pregnancy microenvironment of this study cohort, including negative control dams, for the presence of prions using RT-QuIC. We evaluated uterine tissue from 29 of 31 dams, a total of 50 amniotic fluid samples, and 202 placentomes. From the 16-CWD positive dams, prion seeding activity was found in 5 of 15 uterine tissues (33.3%), 5 of 26 amniotic fluid samples (19.2%) and 18 of 110 placentomes (16.4%) (Fig. 1a–c; Table 2). Of note, 17 of 18 (94.4%) positive placentomes correlated to dams with positive uterine tissue (Table 2). By state, we report positive seeding activity in the reproductive tissues and fluids of dams from Arkansas (2/10; 20%), Tennessee (3/10; 30%), and West Virginia (3/8; 37.5%). Reproductive tissues (uterus, placentome, amniotic fluid) collected from our study cohort dams that were lymphoid and obex RT-QuIC negative (n = 12), as well as dams harvested from a CWD non-endemic region (Georgia; n = 3) (Table 1), remained RT-QuIC negative. Overall, of the 16 confirmed CWD-positive free-ranging dams, in vitro amyloid seeding was demonstrated in the pregnancy microenvironment of 8 of 16 (50%).
CWD detection in female white−tailed deer pregnancy microenvironment determined by RT−QuIC. Grouped based on state of collection. Amyloid seeding in one or more of the following tissues: uterus, amniotic fluid, and placentomes (a–c; Table 2) from CWD−positive dams as determined by RT−QuIC & IHC (Table 1). Amyloid formation displayed as reaction rates (1/time (t) to Thioflavin T (ThT) fluorescent threshold). Horizontal lines represent the medians with n = 8 replicates (dam tissues). Negative controls from all Georgia deer (n = 3) remained negative in all samples tested and CWD−positive controls sourced from experimentally inoculated muntjac (last data point on the right). P values as follows: * <0.05, ** <0.01, *** <0.001, ****<0.0001. Grey shaded rectangles in panels A and C denote samples utilized for bioassay inoculations (Table 3).
In vitro prion seeding present in fetal tissues harvested from free-ranging white-tailed deer
After demonstrating positive seeding activity in tissues of the maternal reproductive tract (uterus) and at the maternal-fetal interface (placentomes and amniotic fluid), we evaluated 54 fetuses (CWD endemic (n = 51); nonendemic (n = 3)) with sufficient tissue available (thymus (n = 54), brain (n = 53), liver (n = 49), spleen (n = 47)) for the presence of CWD by PMCA38. Given the small size of each fetus and thus limited sample volume harvested, in conjunction with presumed low CWD burdens within each tissue type32we combined PMCA amplification with RT-QuIC readout37 to maximize detection sensitivity. Here we detected PMCA amplifiable amyloid seeds in thymus tissue harvested from four fetuses (4/51; 7.8%), brain tissue harvested from two fetuses (2/50; 4.0%), and liver tissues from two fetuses (2/46; 4.4%) (Fig. 2). Fetal spleen tissue did not reveal PMCA amplification (Table 2). In total, 6 of 51 (12%) fetuses from the endemic areas had PMCA positive results. All CWD negative dams carried fetuses that remained negative for PMCA amplification (Table 1). We report an individual case in which we found PMCA amplification in fetal brain tissue (Fig. 2) harvested from a free-ranging CWD-positive dam that did not have evidence of CWD dissemination within the reproductive tissues tested (Fig. 1a-c; Table 2). To summarize, 5 of the 16 (31.3%) free-ranging CWD-positive dams were carrying at least one fetus with tissues that harbored PMCA amplifiable prion seeds, with one each from Arkansas and Tennessee, and three from West Virginia.
CWD detection in white-tailed deer (WTD) fetal tissues determined by RT-QuIC. Amyloid seeding detected in fetal brain, thymus, and liver (Table 2) collected from CWD-positive dams as determined by RT-QuIC and IHC (Table 1). Amyloid formation displayed as reaction rates (1/time (t) to Thioflavin T (ThT) fluorescent threshold). Horizontal lines represent medians with n = 16 replicates (fetal tissues). Negative control fetal tissue samples from WTD collected in Georgia (n = 3) remained negative in all samples tested. P values as follows: * <0.05, ** <0.01, *** <0.001, ****<0.0001. Grey shaded rectangles denote samples utilized for bioassay inoculations (Table 4). Abbreviations represented as follows: (Th)ymus, (Br)ain, and (Liv)er.
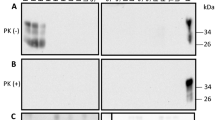
Infectious prions present within the pregnancy microenvironment and fetuses harvested from free-ranging white-tailed deer
To determine the biological relevance of the presence of in vitro conversion competent prions in maternal and fetal tissues, we assessed a subset of tissues harvested from the reproductive tract (uterus), the maternal-fetal interface (placentome), and fetuses (thymus and brain) for the presence of infectious CWD prions in TgCerPrP−E2265037+/− mouse bioassay.
Pregnancy microenvironment: All mice (35/35; 100%) inoculated with uterine or placentome tissue developed terminal clinical TSE disease (ataxia, limb paralysis, weight loss, etc.); uterine tissue (12/12; 264 ± 30 days post-inoculation (dpi) (mean ± SD)), placentome tissue (23/23; 256 ± 27 dpi). In vitro amyloid seeding activity was present in brain tissues harvested from all mice (35/35) as assessed by RT-QuIC (Table 3).
Fetal tissues: Six of eight (6/8; 75.0%) mice inoculated with fetal thymus (325 ± 44 dpi) and 6 of 11 (54.5%) inoculated with fetal brain (254± 80 dpi) developed terminal clinical disease which was confirmed in brain and/or spleen by RT-QuIC (Table 4). Of note, 5/5 mice (100%) inoculated with fetal brain tissue harvested from fetus 7 − 6 developed signs of terminal clinical TSE disease. Age-matched and mock-inoculated negative control mice remained free of clinical signs of disease throughout the 381-dpi study and were confirmed negative by RT-QuIC (Fig. 3).
Infectious CWD prions present in white-tailed deer maternal reproductive and fetal tissues determined by mouse bioassay. Cervidized (TgCerPrP−E2265037+/−) mice were inoculated with 10− 4 dilutions of uterus or placentome intracranially (uterus: n = 12 mice; placentome: n = 35 mice) or fetal thymus or fetal brain intraperitoneally (thymus: n = 8 mice; brain: n = 11 mice). Terminal mouse brains were tested by conventional RT-QuIC for amyloid seeding activity. Amyloid formation displayed as reaction rates (1/time (t) to Thioflavin T (ThT) fluorescent threshold). Horizontal lines represent the median (8 replicates per mouse). Mice inoculated with tissues from free-ranging negative control deer (uterus: n = 8 mice; placentome: n = 8 mice; thymus: n = 8 mice; brain: n = 6 mice; 8 replicates each) from Georgia served as negative controls. A Mann-Whitney unpaired t-test was used against negative controls to determine statistical significance. **** indicates a P value of < 0.0001.
In summary, we demonstrate that free-ranging WTD naturally exposed to CWD harbor infectious CWD prions in maternal and gestational fetal tissues.
Gestational age
Gestational age, as determined by the Hamilton39 equation of rump to head measurements, showed fetal age ranging between 79 and 158 days from conception, with an average age of 112.5 days (total gestational time for WTD is 201 days40. There were no fetuses harvested in the first trimester of development (0–67 days), n = 44 fetuses harvested in the second trimester (68–134 days), and n = 10 fetuses harvested in the third trimester (135–201 days). The age-matched negative control Georgia fetuses (n = 3) were an average age of 103.5 days. We found tissue positivity in fetuses at gestational age 90 to 158 days, correlating to 2nd and 3rd trimester pregnancies.
Prnp genotypes from free-ranging white-tailed deer dams and fetuses
As Prnp genotypes have been shown to be important in host susceptibility to prion infection and in utero transmission of scrapie in sheep, we evaluated maternal (n = 31) and fetal (n = 54) tissues to determine their genotypes at codon 95 and 96. The Prnp open reading frame was sequenced for all the WTD to determine the impact genotype (codon 95/96) may have on vertical transmission. Pregnant dams in this study (n = 28 CWD endemic; n = 3 nonendemic) represented all three polymorphisms at codon 96: GG = 21, GS = 9, and SS = 1. When Prnp polymorphisms were correlated with dam CWD positivity, we identified CWD-positive dam status in 12 of 21 (57.1%) codon 96GG, 4 of 9 (44.4%) codon 96GS, and 0 of 1 (0%) codon 96SS (Table 1). All dams were wildtype QQ at codon 95 (31/31).
To determine if polymorphisms at Prnp codons 95 and 96 may play a role in CWD transmission and deposition in the fetus, we determined the Prnp genotype of each fetus in this study. Of the 54 fetuses collected, all three genotypes were present at codon 96; GG = 36, GS = 16, and SS = 2. When compared to their CWD status, all 6 CWD positive fetuses were Prnp codon 96GG (6/36;16.7%), with no CWD detection in fetuses expressing 96GS or 96SS polymorphisms (Table 2). Interestingly, there were two instance of a mutation in the Prnp 95 codon where glutamine was substituted for histidine (QH). This was the case in one CWD positive fetus from a CWD positive dam (Table 2) and in one CWD negative fetal/dam dyad. The remaining fetuses were wildtype homozygous QQ at the same position (n = 52). Here we report that the presence of codon 96 serine residue in either dam or fetus correlated with a lack of vertical transmission, although expanded studies to address the impact of polymorphisms in CWD vertical transmission are needed.
Historical CWD surveillance data
All three states in the study area have historically conducted limited CWD ELISA and/or IHC testing on fawns as part of state wildlife agency CWD surveillance and monitoring programs (Table 5). CWD was detected in lymphoid (retropharyngeal lymph node; AR, TN, WV) or brain (obex; WV) tissues harvested from fawns (total 74/1476; 5%) that varied in age from < 6 to 10 months.
In summary, we demonstrate in vitro amyloid seeding in the pregnancy microenvironment of half (8/16; 50%) of the confirmed CWD-positive free-ranging dams tested, with a third (5/16; 31.3%) of these dams carrying at least one fetus with PMCA amplifiable prion seeds. Of most importance, a subset of fetal tissues inoculated into bioassay confirms the presence of infectious CWD prions in maternal and gestational fetal tissues providing the first evidence of the initiation of CWD infections in the fetus prior to parturition. To add additional biological relevance to these findings, state wildlife agency CWD surveillance and monitoring programs have detected CWD in fawns ≤ 10 months of age.
Discussion
The continued detection of CWD in free-ranging cervid populations and increasing prevalence in some locations demonstrate the need for a greater understanding of the impact maternal infections have on the transmission of this fatal neurodegenerative disease. With CWD prevalence as high as 50% in some localized areas of the U.S.41 understanding how mother-to-offspring transmission impacts the overall transmission dynamics of this disease will be imperative to those who enjoy, hunt, oversee, and manage captive and wild cervid populations. To this end, this multi-state and -agency study came together to determine if healthy-appearing female white-tailed deer from CWD endemic regions, that are naturally exposed to CWD, can transmit the disease to their fetus during pregnancy.
Here we report the presence of the infectious CWD agent within fetal and reproductive tissues of free-ranging WTD, revealing that dams can transmit the disease in utero to their offspring. In agreement with previous studies30,31 we also confirm CWD deposition within reproductive maternal tissues (Fig. 1) and in utero-derived fetal tissues (Fig. 2) harvested from free-ranging cervids using highly sensitive in vitro amyloid detection assays. Although this and previous studies have shown PrPCWD deposition in tissue, what was left unknown, was whether these detections represented infectious prions capable of initiating and progressing CWD infections. We employed mouse bioassays, regarded as the only tool to determine the presence of prion infectivity, and found that female reproductive (i.e., uterus, placentome) and fetal tissues (i.e., thymus, brain) harbor infectious CWD prions (Fig. 3; Tables 3 and 4). Thus, this study provides strong support that offspring can be exposed to and initiate CWD infections long before parturition.
Interestingly, our study reveals a nuanced picture of CWD transmission in the pregnancy microenvironment of cervid placentomes. We observed variable positivity within placentomes of fetal twin sets, as well as within each fetus’ own placentome structure, confirming findings from previous studies in Reeves’ muntjac and Rocky Mountain elk22,29,32. In addition, we demonstrate that prion deposition within the reproductive microenvironment (i.e., placentomes, uterus and amniotic fluid) does not always result in prion deposition within the fetus and confirm previous studies demonstrating that prion deposition is not required within the reproductive microenvironment for fetal positivity32 (Fetus 7 − 6 brain; Table 4). This suggests other factors, such as maternal and paternal genetic input, may contribute to the susceptibility of vertical transmission. In these cases it is possible that CWD progression within this environment has been slow to progress, or as noted in this study, may be associated with maternal-fetal dyads that express Prnp 96GS haploid, a polymorphism in the cervid prion protein known to delay disease onset33,34. The observation could hint at difficulties in overcoming the protective influence of 96GS genotypes in maternal transmission. Yet, other studies have shown evidence that 96GS fetuses contain CWD prions30indicating that, similar to adult WTD, protective effects of the polymorphism are not enough to prevent in utero transmission of the disease. We also demonstrate a CWD-positive fetus with the protective 95QH polymorphism, indicating that in utero transmission can also overcome this genetic variant (Table 2). These findings are in agreement with those conducted in the related sheep scrapie system27where it was demonstrated that sheep with Prnp polymorphisms that confer protection from disease resulted in reduced or absent in utero transmission to lambs. Also, gestational age did not have a correlative effect on fetal CWD status, showing that fetuses can be infected during the 2nd and 3rd trimesters of gestation (Table 2). We have previously reported this in experimental muntjac studies demonstrating CWD deposition in in utero-derived fetuses harvested from CWD-positive dams throughout all periods of gestation (1st, 2nd and 3rd trimester)22, while studies in the sheep scrapie system27 report progressively increasing placentome PrPSc deposition from early to term pregnancy. Expanded studies including larger cohorts of fetal/dam pairs are needed to address this question more fully.
Horizontal transmission has long been recognized as the primary driving force in the spread of CWD, yet vertical transmission continues to gain traction as a contributing mechanism. Vertical transmission has been shown to be an efficient route of transmission in several prion diseases including scrapie in sheep20,21,42,43,44,45,46, experimental CWD in Reeves’ muntjac29, and has been suggested for CWD in captive and free-ranging WTD30,31 and free-ranging Rocky Mountain elk32. The results reported here, evaluating free-ranging animals, are consistent with previous experimental cervid studies revealing the presence of prion seeding and infectious CWD agent within maternal uterus, placentomes, and amniotic fluid29. These findings will further our understanding of CWD prion transmission at a population level and enable investigation of the potential for influence on population dynamics. Experimental studies conducted in the Reeves’ muntjac demonstrate that muntjac at all stages of CWD infection were able to breed and maintain full term pregnancies22. However, these studies also revealed a 60% increase in nonviable offspring born to CWD-infected muntjac dams. If this is representative of white-tailed deer and other cervid species in a free-ranging setting, it may suggest a negative impact to recruitment. This will be an important, but difficult area of study. In mule deer and WTD, subtle negative effects on fawn survival and recruitment have been reported47,48. As CWD is known to result in population declines in mule deer and white-tailed deer48,49, there is need to understand if fetal infections contribute to such declines.
Questions remain about the impact of these findings on free-ranging cervid populations. Here, pregnant WTD were harvested from three southeastern U.S. states (Arkansas, Tennessee, and West Virginia) in areas with apparent CWD prevalence exceeding 20%50,51,52 to assess impacts of maternal infections. Our findings provide evidence that maternal CWD infections within these states are resulting in gestational infections demonstrating prion exposure and amplification within fetal tissues long before parturition. Our previous experimental studies in muntjac revealed that offspring born to CWD-infected dams became lymphoid tissue positive as early as 41 days after birth, and progressed to terminal clinical disease between 2 and 5 years of age22. Information regarding progression of in utero infection to a disease state after parturition is not known for free-ranging WTD populations; however, this is an important area of inquiry. Prion transmission from healthy-appearing CWD-infected dams to their offspring has the potential to influence future fawn recruitment and prevalence rates in conjunction with infections acquired via horizontal means. If the timing and progression of clinical CWD is such that offspring die from CWD earlier than they would from an indirect exposure and prior to replacing themselves in the population, recruitment can be impacted through decreased lifetime reproductive potential in females.
Our detection of CWD-positive fawns ≤ 10-month-old by ELISA testing provides indirect evidence of gestational infection, although direct or indirect CWD transmission after birth cannot be ruled out in these fawns (Table 5). The detection of CWD infection in ≤ 6-month-old fawns in the Arkansas and Tennessee study sites by ELISA test, which is not as sensitive as amplification assays37, was particularly suggestive of vertical transmission. Fawns less than 6 months of age are not routinely incorporated into statewide CWD surveillance programs because of the low likelihood of detectable infection using traditional assays (i.e., ELISA, IHC), yet have been previously identified17. Future studies should investigate the potential role of in utero transmission in local CWD transmission cycles. Considering the strong relationship between CWD infection probability and female white-tailed deer relatedness, in utero CWD transmission may serve as a small yet important route of transmission in addition to social interactions and indirect exposures53.
Overall, this study describes the dissemination of CWD prions throughout tissues and birthing fluids of the pregnancy microenvironment demonstrating that offspring are routinely exposed to the infectious prion in-utero prior to parturition. We report infectious prions in the reproductive and fetal tissue of naturally exposed free-ranging white-tailed deer suggesting that in utero maternal transmission is likely an underappreciated mode of CWD transmission. Our study shows that vertical transmission is indeed a viable route of infection within the southeastern U.S. and is another potential factor contributing to the relentless spread of chronic wasting disease.
Methods
Research reported in this publication was supported by the Wildlife and Sport Fish Restoration Programs of the U.S. Fish and Wildlife Service (Award number F20AP00172) and by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Numbers R01AI112956, P01-AI-077774, and R01AI156037. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additional support was provided by Southeastern Cooperative Wildlife Disease Study (SCWDS) member states (Alabama, Arkansas, Florida, Georgia, Kentucky, Kansas, Louisiana, Maryland, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, Tennessee, Virginia, and West Virginia), U.S. Fish and Wildlife Service National Wildlife Refuge System, and U.S. Geological Survey Ecosystems Mission Area. Field sampling was approved by the University of Georgia’s IACUC # A2018 02–010. Mouse bioassay was approved by Colorado State University’s IACUC #1524 and 5362. All methods and procedures were conducted in accordance with the relevant IACUC and ARRIVE guidelines and regulations. All authors adhered to the ARRIVE guidelines.
Study area, sample collection and preparation
Three CWD endemic areas of the southeastern United States were targeted for lethal collection of free-ranging, adult, female WTD, including: Newton County, Arkansas; Fayette County, Tennessee; and Hampshire County, West Virginia. Mature females were targeted January through April in these areas because the apparent CWD prevalence in WTD at each collection site was greater than 20%50,51,52, optimizing chances of collecting CWD-positive gravid WTD between 16 and 24 weeks gestation. Deer were similarly collected from a control site in Clarke County, Georgia, a location with no detection of CWD in WTD. CWD infections in WTD have recently been identified in Georgia1. At the time of collections for this study (2020) and at the time of this writing, CWD has not been detected in Clark County. All deer were lethally collected by state wildlife management agency or SCWDS (University of Georgia) personnel. Collection and sampling occurred across a calendar year, including January 2020 in Georgia (n = 3 dams; n = 3 fetuses), February 2020 in Arkansas (n = 10 dams; n = 17 fetuses), March 2020 in Tennessee (n = 10 dams; n = 20 fetuses), and April 2021 in West Virginia (n = 8 dams; n = 14 fetuses).
Adult WTD necropsies and sample collection were performed by SCWDS personnel at each field site. Care was taken to use single-use instruments, single-use personal protective equipment, disposable supplies, intentional workflow, and proper technique to minimize risk of cross-contamination between animals, as well as between tissues within individual animals. Immediately upon death, whole blood was collected by cardiocentesis using a needle and syringe. The blood was transferred to vials containing citrate for processing and was archived for a future study. Saliva (1–2 mL) was collected using disposable transfer pipettes from the buccal cavity and transferred to cryovials for CWD testing by prion amplification assays. Each carcass was placed into a body bag and transported by vehicle to a field necropsy and sample collection site. Age of each animal was estimated based on tooth wear and replacement54. A small team of individuals with assigned roles sampled deer individually and collected brainstem, RPLN, palatine tonsils, RAMALT and third eyelids. Tissues were split between fresh-frozen and 10% neutral buffered formalin for later detection of PrPCWD by IHC or prion amplification assays (RT-QuIC, PMCA). Two plastic zipties were secured to the cervix and the intact, gravid uterus was excised and placed into large plastic bags. Urine (1–2 mL) was collected from the urinary bladder using needle and syringe and transferred to a cryovial. Blood (stored overnight at 4 °C), saliva, urine, intact uterus and all maternal tissue samples (stored at -20 °C overnight) were shipped to Colorado State University (CSU) where they were immediately processed (blood) or stored at -80 °C (saliva, urine, uterus, maternal tissue) until further processing.
At CSU, tissue samples were thawed and intact uteri and fetuses were individually necropsied by CSU personnel using single-use tissue and fetus instruments to mitigate cross-contamination between maternal and fetal tissues. Fetuses were placed at 4 °C overnight to thaw. Amniotic fluid was extracted by use of single-use needle and syringe from each amniotic sac. Each amniotic sac was opened using a single-use scalpel and fetuses were removed and measured for gestational age using the Hamilton Eq. [39]; (Age (days)= (body length (mm) x 0.32) + 36.82). Fetuses were carefully dissected using new PPE and sterile single-use instruments between each fetus and their respective tissues; all collected items were stored at -80 °C for future analysis. All tissues were assessed by the prion amplification assays PMCA and/or RT-QuIC for the presence of amyloid seeding activity. Dam and fetal tissue were made into 10% w/v tissue homogenates with 1x PBS (20 mM NaPO4, 150 mM NaCl, pH 7.4) in an Omni Bead Ruptor 24 and stored at -80 °C until tested. The following tissues and fluids were analyzed from each pregnant dam: obex, RAMALT, RPLN, tonsil, third eyelid, blood, uterus, placentomes, amniotic fluid, saliva, and urine. The following tissues were analyzed from each fetus: brain, thymus, liver, and spleen. Independent researchers assessed maternal and fetal tissues and remained blinded to outcomes until the study was completed.
Immunohistochemistry (IHC)
IHC was used to visualize prion deposition within fixed tissue. Paraffin embedded WTD dam tissue sections of RPLN, RAMALT, obex, third eyelid, or tonsil were deparaffinized with xylene (100%) and rehydrated in graded alcohols (100% − 70%) before treatment with 88% formic acid (30 min at room temperature) as previously described55. After washing with water, slides were placed in a 2100-Retriever (Prestige Medical) in sodium citrate buffer (0.01 M sodium citrate, 0.05% Tween 20, pH 6.0) for heat-induced epitope antigen retrieval. Endogenous peroxidase activity was quenched with 3% hydrogen peroxide and slides were blocked before overnight incubation in anti-prion antibody BAR224 (1 mg/mL; Caymen Chemical) diluted 1:750. Envision + anti-mouse HRP-labeled polymer secondary antibody (Dako) was followed by 3-amino-9-ethylcarbazole (AEC) (Dako) for visualization. Negative control tissues were run concurrently with test samples.
Iron oxide bead extraction (IOB)
As prion burdens are known to be relatively low in bodily fluids, we previously developed a pre-RT-QuIC concentration method, iron oxide bead (IOB) extraction, to enhance detection capability56. Amniotic fluid diluted 1:10 and 1:100 (1x PBS), saliva diluted 1:20 (1x PBS), or undiluted urine (1 mL total volume/each), were added to individual 1.7 ml conical tubes35,56. Two microliters (2 µL) of iron oxide beads (BM547 Bangs Laboratory) were added to each tube followed by end-over-end mixing at room temperature for 30–60 min. Tubes containing samples were placed on a magnetic particle separator (Pure Biotech, New Jersey) which permitted the bead bound prions to be immobilized against the tube wall. Supernatants were discarded and the tubes were removed from the magnet. The beads, containing extracted prions, were resuspended in 10 µL of 0.1% sodium dodecyl sulphate (SDS) and run in RT-QuIC at 42–55 °C. Positive and negative controls were run with all IOB-QuIC plates.
Real-time quaking induced conversion (RT-QuIC)
We used RT-QuIC to determine CWD status of fetal and maternal tissues, as previously described29,57. Briefly, 0.1 mg/mL of truncated Syrian hamster recombinant protein containing amino acids 90–231 was added to master mix (20 mM NaPO4, 1 mM ethylenediaminetetraacetic acid tetrasodium salt (EDTA) (Sigma), 320 mM NaCl, and 10 µM thioflavin T (ThT)). Master mix (98 µl) was added to each well of a black optical bottom 96-well plate. Two microliters (2 µl) of maternal tissue homogenates at a final dilution of 10− 3 (third eyelid, uterus, placentomes), 10− 4 (RAMALT, RPLN, tonsil), or 10− 5 (obex), while 2 µl fetal tissues prepared from round five PMCA product (final dilution of 10− 2 in 0.1% SDS in PBS) were loaded into each well in quadruplicate. Reproductive and fetal tissues were tested by two independent researchers blinded to the results of the dam tissues. Plates were inserted into a BMG Fluostar Omega plate reader and analyzed at 15-minute intervals for 250 rounds or 62.5 h at 42 °C or 55 °C as previously optimized for each tissue type and protocol56,58. A minimum of two independent quadruplicate plates were run per tissue sample for a total of 8 replicates per tissue. CWD positive and negative WTD tissue specific controls were assessed with all maternal tissues. Reeves’ muntjac and/or WTD specific fetal tissues served as positive and negative controls with all fetal tissues. Reactions were considered positive when fluorescent readouts reached five standard deviations above the average initial five fluorescent readings. Significance was determined by comparing age-matched negative control tissues to samples of interest using the unpaired, non-parametric, two-tailed Mann-Whitney Test in GraphPad Prism v9 to generate p-values. Significance was represented as follows: *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001.
Protein misfolding cyclic amplification (PMCA)
To further investigate prion burden in fetal tissues, we subjected each to PMCA as previously described for cervid maternal and fetal tissues32. Normal brain homogenate (NBH) was prepared from naive transgenic mice that over-expressed cervid PrP (TgCerPrP−E2265037+/−) to serve as PMCA conversion substrate. Briefly, mice were perfused with 5 mM EDTA prior to whole brain extraction. Brain tissue was flash frozen in liquid nitrogen, and subsequently made into a 10% w/v homogenate (5mM EDTA, 150 mM NaCl and 1% Triton X-100). Fetal tissue homogenates (10% w/v) and NBH were added in 0.2 mL microcentrifuge tubes containing 2.38 mm and 3.15 mm Teflon beads (McMaster-Carr)37,59. The first round of PMCA was initiated with the addition of fetal tissue homogenates at a ratio of 10 µL tissue sample to 90 µL NBH (exception: 10 µL spleen tissue diluted to 10− 2). PMCA rounds two through five were comprised of 20 µL previous rounds’ amplified product to 50 µL fresh NBH substrate37. Round one PMCA samples were placed in a Misonix sonicator for 72 h (144 cycles; each cycle consisting of 30 s sonication and 29.5 min incubation at 37 °C). PMCA rounds two through five were processed for 24 h (48 cycles; each cycle consisting of 30 s sonication and 29.5 min incubation at 37 °C). All samples were run with CWD positive and negative tissue specific controls in duplicate by two independent investigators.
sPMCA with RT-QuIC (PQ)
We have previously demonstrated enhanced prion detection sensitivity by combining PMCA with RT-QuIC60,61. Here, round five PMCA product was further prepared for amyloid seeding assessment by RT-QuIC with each sample being diluted 1:100 in 0.1% SDS. Each sample was prepared and assessed as per the RT-QuIC methods above.
Bioassay in cervid transgenic mice
Bioassay in natural host or rodent model species is the only way to determine if the presence of the infectious prion agent has the capacity to initiate and progress disease. Thus, we used mouse bioassay to determine the presence of the infectious CWD agent within tissues of the pregnancy microenvironment and fetus. Uterine and placentome tissues (pregnancy microenvironment) harvested from CWD naturally infected free-ranging dams were intracranially (IC)-inoculated into TgCerPrP−E2265037+/− mice62. Mice were inoculated at six to twelve weeks of age and maintained as previously described29 and approved by CSU’s IACUC. Each mouse was IC-inoculated in the right parietal lobe with 30 µl of 10% w/v homogenate of uterus or placentome (n = 12, n = 23 mice, respectively) or intraperitoneal (IP)-inoculated with fetal brain or fetal thymus (n = 11, n = 8 mice, respectively) using 80 µL of 1:2.5 round 5 PMCA material diluted in PBS that was treated overnight with 2% HyClone Pen-Strep. All mice were monitored daily for signs of prion infection (ataxia, weight loss, hypersensitivity) until termination due to clinical disease presentation. Dam pregnancy microenvironment tissues (uterine and placentome) and in utero-derived fetal tissues harvested from white-tailed deer in Clarke County, Georgia (n = 3) were treated identically and either IC or IP-inoculated into cohorts of mice (n = 16, n = 14 mice, respectively) serving as negative bioassay controls. Brain and spleen tissue harvested from each mouse at termination were assessed for amyloid seeding (prions) by RT-QuIC.
Genotyping
As polymorphisms within the Prnp coding sequence are known to affect disease characteristics34,63all dams and fetuses were genotyped with codon 95 and 96 reported for this study. DNA was extracted from dam (RPLN or spleen) and fetal (thymus or spleen) tissues using a DNeasy Blood and Tissue kit (QIAGEN). DNA concentration was determined for each sample (NanoDrop – 1000 UV/Vis Spectrophotometer) prior to polymerase chain reaction (PCR) to amplify the purified DNA. Deer specific PCR primer pair 213d AGGTCAACTTTGTCCTTGGAGGAG and 139u TAAGCGCCAAGGGTATTAGCAT, with sequencing primer 86d CAGTCATTCATTATGCTGCAGACT were used as previously described22. PCR amplified DNA was sent for Sanger sequencing by Quintara Biosciences and the returned results were analyzed using the sequencing software Chromas (Technelysium Pty Ltd v2.6.6).
Historical CWD surveillance data
Available CWD surveillance data from the three study areas was accessed via each state wildlife agency database. Data sources varied for each state. For Arkansas, county-level data for Newton County were examined, including all available sources for WTD ≤ 6 months (e.g., hunter-harvest, roadkill, sick/target deer). RPLN’s in Arkansas were tested by ELISA and/or IHC. In Tennessee, data from hunter-harvested fawns from Fayette and Hardeman counties were assembled. Tennessee fawns RPLN’s were tested by ELISA. In West Virginia, CWD data was assembled from routine agency special collections in a 39-mile square area of Hampshire County. All deer were < 6–10 months old at the time of collection and obex samples were tested by ELISA and/or IHC. All assays were performed routinely at accredited veterinary diagnostic laboratories.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
https://www.usgs.gov/media/images/distribution-chronic-wasting-disease-north-america-0. Distribution of Chronic Wasting Disease [USGS] (National Wildlife Health Center, 2024).
Sohn, H. J. et al. A case of chronic wasting disease in an elk imported to Korea from Canada. J. Vet. Med. Sci. 64, 855–858. https://doi.org/10.1292/jvms.64.855 (2002).
Tranulis, M. A. et al. Chronic wasting disease in europe: new strains on the horizon. Acta Vet. Scand. 63, 48. https://doi.org/10.1186/s13028-021-00606-x (2021).
Williams, E. S. & Young, S. Chronic wasting disease of captive mule deer: a spongiform encephalopathy. J. Wildl. Dis. 16, 89–98 (1980).
Williams, E. S. & Miller, M. W. Chronic wasting disease in deer and elk in North America. Rev. Sci. Tech. 21, 305–316. https://doi.org/10.20506/rst.21.2.1340 (2002).
Haley, N. J., Mathiason, C. K., Zabel, M. D., Telling, G. C. & Hoover, E. A. Detection of sub-clinical CWD infection in conventional test-negative deer long after oral exposure to urine and feces from CWD + deer. PLoS One. 4, e7990. https://doi.org/10.1371/journal.pone.0007990 (2009).
Mathiason, C. K. et al. Infectious prions in the saliva and blood of deer with chronic wasting disease. Science 314, 133–136. https://doi.org/10.1126/science.1132661 (2006).
Pulford, B. et al. Detection of PrPCWD in feces from naturally exposed Rocky mountain elk (Cervus Elaphus nelsoni) using protein misfolding Cyclic amplification. J. Wildl. Dis. 48, 425–434. https://doi.org/10.7589/0090-3558-48.2.425 (2012).
Safar, J. G. et al. Transmission and detection of prions in feces. J. Infect. Dis. 198, 81–89. https://doi.org/10.1086/588193 (2008).
Georgsson, G., Sigurdarson, S. & Brown, P. Infectious agent of sheep scrapie may persist in the environment for at least 16 years. J. Gen. Virol. 87, 3737–3740 (2006).
Haley, N. J. & Hoover, E. A. Chronic wasting disease of cervids: current knowledge and future perspectives. Annu. Rev. Anim. Biosci. 3, 305–325. https://doi.org/10.1146/annurev-animal-022114-111001 (2015).
Miller, M. W., Williams, E. S., Hobbs, N. T. & Wolfe, L. L. Environmental sources of prion transmission in mule deer. Emerg. Infect. Dis. 10, 1003–1006. https://doi.org/10.3201/eid1006.040010 (2004).
Somerville, R. A. et al. BSE infectivity survives burial for five years with only limited spread. Arch. Virol. 164, 1135–1145. https://doi.org/10.1007/s00705-019-04154-8 (2019).
Gough, K. C. & Maddison, B. C. Prion transmission: prion excretion and occurrence in the environment. Prion 4, 275–282. https://doi.org/10.4161/pri.4.4.13678 (2010).
Mathiason, C. K. et al. Infectious prions in pre-clinical deer and transmission of chronic wasting disease solely by environmental exposure. PLoS One. 4, e5916. https://doi.org/10.1371/journal.pone.0005916 (2009).
Saunders, S. E., Bartz, J. C. & Bartelt-Hunt, S. L. Soil-mediated prion transmission: is local soil-type a key determinant of prion disease incidence? Chemosphere 87, 661–667. https://doi.org/10.1016/j.chemosphere.2011.12.076 (2012).
Huang, M. H. J. et al. Expanding CWD disease surveillance options using environmental contamination at deer signposts. Ecol. Solut. Evid. 5, e12298. https://doi.org/10.1002/2688-8319.12298 (2024).
Plummer, I. H., Johnson, C. J., Chesney, A. R., Pedersen, J. A. & Samuel, M. D. Mineral licks as environmental reservoirs of chronic wasting disease prions. PLoS One. 13, e0196745. https://doi.org/10.1371/journal.pone.0196745 (2018).
Castilla, J. et al. Vertical transmission of bovine spongiform encephalopathy prions evaluated in a transgenic mouse model. J. Virol. 79, 8665–8668. https://doi.org/10.1128/jvi.79.13.8665-8668.2005 (2005).
Dickinson, A. G., Stamp, J. T. & Renwick, C. C. Maternal and lateral transmission of scrapie in sheep. J. Comp. Pathol. 84, 19–25. https://doi.org/10.1016/0021-9975(74)90023-1 (1974).
Foster, J. D., Goldmann, W. & Hunter, N. Evidence in sheep for pre-natal transmission of scrapie to lambs from infected mothers. PLoS One. 8, e79433. https://doi.org/10.1371/journal.pone.0079433 (2013).
Nalls, A. V. et al. Mother to offspring transmission of chronic wasting disease in reeves’ Muntjac deer. PLoS One. 8, e71844. https://doi.org/10.1371/journal.pone.0071844 (2013).
Bencsik, A., Debeer, S., Petit, T. & Baron, T. Possible case of maternal transmission of feline spongiform encephalopathy in a captive cheetah. PLoS One. 4, e6929. https://doi.org/10.1371/journal.pone.0006929 (2009).
Luk, C. C. et al. Creutzfeldt-Jakob disease in pregnancy: the use of modified RT-QuIC to determine infectivity in placental tissues. Prion 15, 107–111. https://doi.org/10.1080/19336896.2021.1933872 (2021).
Tamai, Y. et al. Demonstration of the transmissible agent in tissue from a pregnant woman with Creutzfeldt-Jakob disease. N Engl. J. Med. 327, 649. https://doi.org/10.1056/nejm199208273270918 (1992).
Garza, M. C. et al. Detection of PrPres in genetically susceptible fetuses from sheep with natural scrapie. PLoS One. 6, e27525. https://doi.org/10.1371/journal.pone.0027525 (2011).
Tuo, W. et al. Pregnancy status and fetal prion genetics determine PrPSc accumulation in placentomes of scrapie-infected sheep. Proc. Natl. Acad. Sci. U S A. 99, 6310–6315. https://doi.org/10.1073/pnas.072071199 (2002).
Tuo, W. et al. Prp-c and Prp-Sc at the fetal-maternal interface. J. Biol. Chem. 276, 18229–18234. https://doi.org/10.1074/jbc.M008887200 (2001).
Nalls, A. V. et al. Infectious prions in the pregnancy microenvironment of chronic wasting disease-infected reeves’ Muntjac deer. J. Virol. 91 https://doi.org/10.1128/jvi.00501-17 (2017).
Bravo-Risi, F. et al. Detection of CWD prions in naturally infected white-tailed deer fetuses and gestational tissues by PMCA. Sci. Rep. 11, 18385. https://doi.org/10.1038/s41598-021-97737-y (2021).
Nalls, A. V. et al. Detection of chronic wasting disease prions in fetal tissues of free-ranging white-tailed deer. Viruses 13 https://doi.org/10.3390/v13122430 (2021).
Selariu, A. et al. In utero transmission and tissue distribution of chronic wasting disease-associated prions in free-ranging Rocky mountain elk. J. Gen. Virol. 96, 3444–3455. https://doi.org/10.1099/jgv.0.000281 (2015).
Baylis, M. & Goldmann, W. The genetics of scrapie in sheep and goats. Curr. Mol. Med. 4, 385–396. https://doi.org/10.2174/1566524043360672 (2004).
Robinson, S. J., Samuel, M. D., O’Rourke, K. I. & Johnson, C. J. The role of genetics in chronic wasting disease of North American cervids. Prion 6, 153–162. https://doi.org/10.4161/pri.19640 (2012).
Denkers, N. D. et al. Temporal characterization of prion shedding in secreta of White-Tailed deer in longitudinal study of chronic wasting disease, united States. Emerg. Infect. Dis. https://doi.org/10.3201/eid3010.240159 (2024).
Plummer, I. H., Wright, S. D., Johnson, C. J., Pedersen, J. A. & Samuel, M. D. Temporal patterns of chronic wasting disease prion excretion in three Cervid species. J. Gen. Virol. 98, 1932–1942. https://doi.org/10.1099/jgv.0.000845 (2017).
McNulty, E. et al. Comparison of conventional, amplification and bio-assay detection methods for a chronic wasting disease inoculum pool. PLoS One. 14, e0216621. https://doi.org/10.1371/journal.pone.0216621 (2019).
Saá, P., Castilla, J. & Soto, C. Cyclic amplification of protein misfolding and aggregation. Methods Mol. Biol. 299, 53–65. https://doi.org/10.1385/1-59259-874-9:053 (2005).
Hamilton, R., Tobin, M. L. & Moore, W. G. Aging fetal white-tailed deer. J. Southeast. Association Fish. Wildl. Agencies. 39, 389–395 (1985).
Verme, L. J. Reproduction studies on penned White-Tailed deer. J. Wildl. Manag. 29, 74–79. https://doi.org/10.2307/3798633 (1965).
Escobar, L. E. et al. The ecology of chronic wasting disease in wildlife. Biol. Rev. Camb. Philos. Soc. 95, 393–408. https://doi.org/10.1111/brv.12568 (2020).
Brotherston, J. G., Renwick, C. C., Stamp, J. T., Zlotnik, I. & Pattison, I. H. Spread and scrapie by contact to goats and sheep. J. Comp. Pathol. 78, 9–17. https://doi.org/10.1016/0021-9975(68)90107-2 (1968).
Caplazi, P., O’Rourke, K., Wolf, C., Shaw, D. & Baszler, T. V. Biology of PrPsc accumulation in two natural scrapie-infected sheep flocks. J. Vet. Diagn. Invest. 16, 489–496. https://doi.org/10.1177/104063870401600601 (2004).
McIntyre, K. M., Gubbins, S., Goldmann, W., Stevenson, E. & Baylis, M. The time-course of a scrapie outbreak. BMC Vet. Res. 2, 20. https://doi.org/10.1186/1746-6148-2-20 (2006).
Pattison, I. H. Scrapie in the Welsh mountain breed of sheep and its experimental transmission to goats. Vet. Rec. 77, 1388–1390. https://doi.org/10.1136/vr.77.47.1388 (1965).
Touzeau, S. et al. Modelling the spread of scrapie in a sheep flock: evidence for increased transmission during lambing seasons. Arch. Virol. 151, 735–751. https://doi.org/10.1007/s00705-005-0666-y (2006).
Dulberger, J., Hobbs, N. T., Swanson, H. M., Bishop, C. J. & Miller, M. W. Estimating chronic wasting disease effects on mule deer recruitment and population growth. J. Wildl. Dis. 46, 1086–1095. https://doi.org/10.7589/0090-3558-46.4.1086 (2010).
Edmunds, D. R. et al. Chronic wasting disease drives population decline of White-Tailed deer. PLoS One. 11, e0161127. https://doi.org/10.1371/journal.pone.0161127 (2016).
DeVivo, M. T. et al. Endemic chronic wasting disease causes mule deer population decline in Wyoming. PLoS One. 12, e0186512. https://doi.org/10.1371/journal.pone.0186512 (2017).
Agency, T. W. R. TWRA Wildlife Technical Report 24 – 03. (2024).
Ballard, J. et al. Chronic Wasting Disease Management and Response Plan (2021–2025). (2021).
Dugovich, B. S. et al. Demographic risk factors vary in the invasion front of chronic wasting disease in West virginia, USA. J. Wildl. Dis. 60, 839–849. https://doi.org/10.7589/jwd-d-22-00160 (2024).
Grear, D. A., Samuel, M. D., Scribner, K. T., Weckworth, B. V. & Langenberg, J. A. Influence of genetic relatedness and Spatial proximity on chronic wasting disease infection among female white-tailed deer. J. Appl. Ecol. 47, 532–540. https://doi.org/10.1111/j.1365-2664.2010.01813.x (2010).
CW, S. Tooth development and war as criteria of age in white-tailed deer. J. Wildl. Mngmt. 13 (2), 195–216 (1949).
Denkers, N. D. et al. Aerosol transmission of chronic wasting disease in white-tailed deer. J. Virol. 87, 1890–1892. https://doi.org/10.1128/jvi.02852-12 (2013).
Denkers, N. D., Henderson, D. M., Mathiason, C. K. & Hoover, E. A. Enhanced prion detection in biological samples by magnetic particle extraction and real-time quaking-induced conversion. J. Gen. Virol. 97, 2023–2029. https://doi.org/10.1099/jgv.0.000515 (2016).
Wilham, J. M. et al. Rapid end-point quantitation of prion seeding activity with sensitivity comparable to bioassays. PLoS Pathog. 6, e1001217. https://doi.org/10.1371/journal.ppat.1001217 (2010).
Hoover, C. E. et al. Detection and quantification of CWD prions in fixed paraffin embedded tissues by Real-Time Quaking-Induced conversion. Sci. Rep. 6, 25098. https://doi.org/10.1038/srep25098 (2016).
Gonzalez-Montalban, N. et al. Highly efficient protein misfolding cyclic amplification. PLoS Pathog. 7, e1001277. https://doi.org/10.1371/journal.ppat.1001277 (2011).
McNulty, E. E. et al. In vitro detection of haematogenous prions in white-tailed deer orally dosed with low concentrations of chronic wasting disease. J. Gen. Virol. 101, 347–361. https://doi.org/10.1099/jgv.0.001367 (2020).
Davenport, K. A., Hoover, C. E., Denkers, N. D., Mathiason, C. K. & Hoover, E. A. Modified protein misfolding Cyclic amplification overcomes Real-Time Quaking-Induced conversion assay inhibitors in deer saliva to detect chronic wasting disease prions. J. Clin. Microbiol. 56 https://doi.org/10.1128/jcm.00947-18 (2018).
Angers, R. C. et al. Chronic wasting disease prions in elk antler Velvet. Emerg. Infect. Dis. 15, 696–703. https://doi.org/10.3201/eid1505.081458 (2009).
Arifin, M. I. et al. Cervid prion protein polymorphisms: role in chronic wasting disease pathogenesis. Int. J. Mol. Sci. 22 https://doi.org/10.3390/ijms22052271 (2021).
Acknowledgements
Funding for this research was provided by the Multistate Conservation Grant Program through the Wildlife and Sport Fish Restoration Programs of the U.S. Fish and Wildlife Service (grant # F20AP00172). Additional support was provided by the long-term financial support of SCWDS by member agencies in Alabama, Arkansas, Florida, Georgia, Kansas, Kentucky, Louisiana, Maryland, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, Tennessee, U.S. Virgin Islands, Virginia, and West Virginia coordinated under the Federal Aid in Wildlife Restoration Act (50 Stat. 917), and the U.S. Geological Survey Ecosystems Mission Area and U.S. Fish and Wildlife Service National Wildlife Refuge System. Further financial support was provided by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Numbers R01AI112956, P01-AI-077774, and R01AI156037. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The views and opinions expressed herein are those of the authors and do not necessarily reflect the views or policies of the Arkansas Game and Fish Commission. Product references do not constitute endorsements. We thank Michael Chamberlain for continued support of this work and the staff for their assistance in the field, especially John Wlodkowski (SCWDS); TWRA CWD field staff; Wes Wright and Stacey Clark (AGFC); Rich Rogers, Lee Strawn, and District 2 staff (WVDNR). We thank Joseph Westrich for critical review of this manuscript.
Author information
Authors and Affiliations
Contributions
AMS: data acquisition, analysis, interpretation, and manuscript drafting, AVN: data acquisition, analysis, interpretation and manuscript drafting, EEM: data acquisition, analysis, interpretation and manuscript review, NDD: data acquisition, analysis, interpretation and manuscript review, DJT: data acquisition, interpretation, and manuscript review, ZO: data acquisition, EB: animal collection, data acquisition and manuscript review JB: data acquisition and manuscript review DMG: design, facilitated field collections, manuscript review JSD: animal collection, data acquisition, manuscript review NS: design, data acquisition, manuscript review CAC: design, data acquisition, manuscript review JMC: state agency coordination, animal collection, financial grant collaborator, manuscript review MGR: study conception, financial support, data acquisition, analysis, interpretation, manuscript drafting, CKM: study conception, design, data analysis and interpretation, manuscript drafting, and financial support.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sandoval, A.M., Nalls, A.V., McNulty, E.E. et al. Vertical transmission of chronic wasting disease in free-ranging white-tailed deer populations. Sci Rep 15, 28553 (2025). https://doi.org/10.1038/s41598-025-12727-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-12727-8