Abstract
Brain gray matter volume (GMV) has been extensively examined in chronic pain and opioid therapy, but spinal GMV has not. As a first investigation of spinal cord GMV in chronic pain and opioid therapy, as our primary outcome, we compared averaged C5-C7 GMV of the spinal cord dorsal/ventral horns among 3 female cohorts: controls (CON, n = 30), and individuals with fibromyalgia taking opioids (FMO, n = 27) and not taking opioids (FMN, n = 31). After adjusting for age across the 3 groups (and adjusting for both age and pain duration across the FM patients), we observed differences in dorsal and ventral horn GMVs, with less GMV in FMOs vs. controls. Additionally, we evaluated within-group relationships between GMVs and clinical pain measures. Among FMNs, dorsal (D) and ventral (V) horn GMVs were positively associated with pain duration (D: p = 0.042, V: p = 0.015). Among FMOs, GMV was positively associated with pain severity (D: p = 0.028, V: p = 0.012), pain interference (D: p = 0.010, V: p = 0.004), and cold pain tolerance (D: p = 0.004, V: p < 0.001). Together with distinct within-group pain-related correlations between FMN and FMO cohorts, less spinal cord GMV in the opioid-taking FM patients suggests spinal cord GMV may be influenced by long-term opioid use in FM.
Similar content being viewed by others
Introduction
Numerous chronic pain conditions, including fibromyalgia (FM), involve structural brain alterations such as modifications in gray matter volume (GMV)1,2,3,4,5,6,7. The mechanistic underpinnings of these changes remain unclear8; however, it is clear that structural brain abnormalities yield valuable insight into chronic-pain related adaptations within the central nervous system (CNS). No prior chronic pain research has similarly evaluated spinal gray matter. Within the spinal cord, there are numerous opportunities for modulation of both ascending and descending nociceptive signaling; as such, spinal cord structural aberrations could further represent chronic pain-related CNS alterations. Analysis of gray matter in the spinal cord dorsal/ventral horns may provide lower-order diagnostic and prognostic biomarkers of chronic pain and thereby bolster our understanding of CNS states that underlie various chronic pain conditions, including FM.
Reduced GMV in the cervical spinal cord dorsal and ventral horns has been associated with disability and disease progression in multiple sclerosis (MS)9,10 and with clinical disability in amyotrophic lateral sclerosis (ALS)11. Moreover, clinical outcomes following spinal cord injury (SCI) have been associated with spinal gray matter atrophy. Specifically, sensory disturbances were associated with dorsal horn gray matter atrophy, and motor impairments were associated with ventral horn gray matter atrophy12,13. Together, these observations suggest that spinal gray matter may be broadly relevant to various forms of sensory processing disruptions, including chronic pain conditions—in particular, centralized pain conditions such as FM. Structural spinal cord features, including dorsal/ventral horn GMV, have not been examined in FM. However, functional distinctions in the dorsal and ventral horns have been demonstrated in FM14..
Indeed, in individuals with FM, functional magnetic resonance imaging (fMRI) has revealed unbalanced cervical spinal cord activity. Compared to pain-free controls, individuals with FM exhibit (1) greater ventral and lesser dorsal fMRI-measured resting-state activity14 and (2) lesser dorsal horn fMRI-measured activity during experimental heat pain15. These findings suggest functional imbalances between the ventral and dorsal horns of the cervical spinal cord, which may be implicated in the development and maintenance of FM. In particular, central sensitization—a persistent state of heightened CNS activity associated with FM16,17—may in part relate to imbalanced spinal cord activity. Meanwhile, prescription opioids have previously appeared to partially reduce these imbalances. For example, individuals with FM who take opioids may exhibit ventral and dorsal horn activity that is more similar to pain-free controls, while individuals with FM who do not take opioids exhibit more pronounced regional differences18. Alongside structural spinal cord evidence from other sensory processing disturbances discussed above, these functional spinal cord changes, as previously seen in FM and opioid-treatment of FM, may further point to the utility of evaluating spinal gray matter in FM.
Particularly for FM as condition of widespread chronic pain and unclear etiology19, the identification of spinal cord mechanisms may aid in understanding and lead toward new effective treatments. Reviewer 3 the cervical spinal cord, we targeted a region of the central nervous system both receiving and processing sensory/pain inputs from the upper extremities which were required to be reported as painful in all our FM patients, as well as a region receiving/sending inputs to the brain/brainstem. While structural spinal cord changes have been observed in conditions that involve sensory processing disruptions (e.g., ALS, MS, SCI), prior to this investigation spinal cord structure has not yet been evaluated in FM. However, functional spinal imbalances have been observed in FM within the cervical spinal cord14. In light of these considerations, we compared spinal cord GMV across CON, FMN, and FMO groups as our primary outcome. We posited that, vs. controls, FM may involve spinal cord GMV alterations at the cervical level. Further, given that opioid medications reduce GMV in brain regions involved in pain processing20,21,22and that cervical spinal cord fMRI-measured activity imbalances may be reduced with prescription opioid use18, we hypothesized that opioids may likewise impact spinal cord dorsal/ventral horn GMV. Due to the dearth of research examining spinal cord GMV differences in FM (or in any other chronic pain condition), we did not posit a directional hypothesis; instead, for our primary outcome, we hypothesized that we would observe significant group differences between FM individuals taking opioids, FM individuals not taking opioids, and pain-free controls. Additionally, we tested for relationships between spinal cord GMV and clinical/pain measures to aid our interpretation.
Results
General cohort characteristics
All study participants were recruited through electronic and paper media advertising in the Durham, North Carolina and surrounding regions. Per our eligibility criteria using the American College of Rheumatology research criteria for fibromyalgia23, all participants with FM reported upper extremity/quadrant of the body pain, relevant to sensory/pain input to the cervical spinal cord region imaged. A majority of participants were Caucasian and not Hispanic, had completed a Bachelor’s degree or less, and earned an annual income of $60,000 or greater (Supplementary Table 1). Clinical characteristics of each participant cohort are also shown in Supplementary Table 1. Group differences between our three groups were evaluated using one-way analysis of variance (ANOVA, for normally distributed variables), kruskal-wallis rank sum tests (for non-normally distributed variables), or fisher exact tests (categorical variables). Post-hoc pairwise comparisons were made for select variables (Supplementary Table 2). We observed significant group differences in age (p < 0.001). Post-hoc comparisons showed age was significantly lower among participants with FM who did not use opioids (FMN) relative to participants with FM who did use opioids (FMO; p < 0.001) and controls (CON; p = 0.016). As a measure of cold pain tolerance, significant group differences were also observed in cold pressor test (CPT) submersion times (p = 0.027). Post-hoc comparisons showed that CON participants exhibited significantly greater CPT submersion time compared to FMN participants (p = 0.024). (See Fig. 3c for group comparison of CPT times.) Finally, across FM groups only, we observed a significant difference in pain duration with FMO participants having a longer duration of pain than FMN participants (p = 0.001). Because our control cohort had no history of chronic pain, a significant difference in pain duration between our FM cohorts and our controls is unsurprising.
Cervical spinal cord (C5-C7) GMV differences
When comparing among FMO, FMN, and controls, we observed overall age-adjusted group differences in average C5-C7 ventral horn GMV (F(2,78) = 4.29, p = 0.017, η2 = 0.09) and dorsal horn GMV (F(2,78) = 3.44, p = 0.037, η2 = 0.07). Post-hoc pairwise comparisons showed that, compared to controls, FMO participants had significantly lower ventral (p = 0.019) and dorsal (p = 0.042) horn GMVs after adjusting for age. No pairwise comparisons were significant between FMN and CON. Additionally, no pairwise comparisons were significant between FMN and FMO after adjusting for age and pain duration (i.e., via subgroup analysis in FM groups only). Mean dorsal/ventral horn GMVs are represented in Fig. 1.
Gray matter volume (GMV) across groups. Group-stratified distributions are shown for mean C5-C7 (A) ventral and (B) dorsal horn grey matter volume. Tukey pairwise comparisons indicate statistically significant differences (p < 0.05) between groups at a univariate level for the CON vs. FMO group comparison. FMO individuals with fibromyalgia taking opioids; FMN individuals with fibromyalgia not taking opioids, CON controls.
Group-stratified associations between GMVs and clinical pain measures
To gain insight into the extent to which spinal GMV may be related to pain, we examined bivariate associations—stratified by group—between average dorsal and ventral horn GMVs, cold pain tolerance (measured as cold pressor test submersion time in seconds), and clinical measures of pain, which included the Brief Pain Inventory subscales for pain severity and pain interference24. All correlation coefficients are reported in Table 1.
Within the FMO cohort, we observed positive associations for ventral horn GMV with pain severity (p = 0.012, Fig. 2a), pain interference (p = 0.004, Fig. 2b), and cold pain tolerance (p = 0.001, Fig. 3a); and we observed moderate positive associations for dorsal horn GMV with pain severity (p = 0.028, Fig. 2c), pain interference (p = 0.010, Fig. 2d), and cold pain tolerance (p = 0.004, Fig. 3b).
Associations between gray matter volume and pain severity/interference. Group-stratified results are shown for bivariate associations between mean C5 – C7 ventral and dorsal horn gray matter volume, average pain severity, and average pain interference. Correlations between ventral horn gray matter volume (GMV) and pain severity and interference are represented in Panels A and B, respectively. Correlations between dorsal horn GMV and pain severity and interference are represented in Panels C and D, respectively. FMO individuals with fibromyalgia taking opioids; FMN individuals with fibromyalgia not taking opioids, Rs Spearman’s correlation coefficient. Statistical significance threshold set at p < 0.05. Lines representing the correlation trends that met this threshold are solid and bold.
Associations between gray matter volume and cold pain tolerance. Group-stratified results are shown for bivariate associations between mean C5 – C7 ventral (A) and dorsal (B) horn gray matter volumes (GMVs) vs. cold pressor test (CPT) submersion time in seconds. (C) Combined boxplot and violin plots are shown for group-stratified distributions of CPT submersion time in seconds. FMO individuals with fibromyalgia taking opioids; FMN individuals with fibromyalgia not taking opioids, CON controls, Rs Spearman’s correlation coefficient. Statistical significance threshold set at p < 0.05. Lines representing the correlation trends that met this threshold are solid and bold.
Within the FMN cohort, we observed associations distinct from those observed in the FMO cohort. Among FMNs, we observed positive associations of pain duration with both ventral horn GMV (p = 0.015, Fig. 4a) and with dorsal horn GMV (p = 0.041, Fig. 4b). No other correlations met our threshold for reporting (significance threshold, p < 0.05) among the FMN cohort, and no correlations met our threshold for reporting (significance threshold, p < 0.05) in the Control cohort.
Associations between gray matter volume and pain duration. Group-stratified results are shown for bivariate associations between mean C5 – C7 ventral (A) and dorsal (B) horn gray matter volumes (GMVs) and average pain duration in years. FMO = individuals with fibromyalgia taking opioids; FMN individuals with fibromyalgia not taking opioids, Rs Spearman’s correlation coefficient. Statistical significance threshold set at p < 0.05. Lines representing the correlation trends that met this threshold are solid and bold.
Sensitivity analysis results
Due to the identification of GMV outliers in our FMO cohort, we conducted a sensitivity analysis to determine changes in the group and correlation results with the exclusion of the 4 patients. We failed to identify a significant group effect on average C5-C7 ventral horn GMV (F(2,74) = 2.62, p = 0.079, η2 = 0.06) and dorsal horn GMV (F(2,74) = 1.54, p = 0.222, η2 = 0.04) while adjusting for age. Within the FMO group, our correlations remained fairly similar. We continued to observe positive associations for ventral horn GMV with pain interference (p = 0.007), and cold pain tolerance (p = 0.023); and we observed positive associations for dorsal horn GMV with pain interference (p = 0.020), and cold pain tolerance (p = 0.049). However, we saw a decrease in the strength of the correlation between GMV and pain severity in the FMO group which subsequently resulted in a failure to meet our significance threshold (V: p = 0.218; D: p = 0.397) (see Supplementary Fig. 1). The complete correlation results for the sensitivity analysis are reported in Supplementary Table 3.
Discussion
The present study contributes novel evidence of distinct, cohort-based relationships between spinal cord dorsal/ventral horn GMV and measures of pain, particularly regarding spinal cord GMV in patients who take opioids long-term (i.e., greater than 90 days opioid use). With regard to our primary outcome of spinal cord GMV, both FM cohorts demonstrated lower mean dorsal/ventral GMVs relative to controls. However, this finding was statistically significant only in the FMO cohort and when individuals with extreme GMV values were included. This observation somewhat aligns with previous reports of lower brain gray matter associated with FM6,7,25,26,27. Statistically significant differences (vs. CONs) in dorsal/ventral GMVs were observed only in the FMO cohort (but not after excluding outliers per our sensitivity analysis), suggesting some possible consistency with prior brain research demonstrating opioid therapy in chronic pain is associated with decreased regional brain GMV20,21,22. While, as compared to the FMN cohort, pain duration and age were significantly higher in the FMO cohort, we observed no statistically significant differences in GMV between FM cohorts after adjusting for age and pain duration. Thus, our data may suggest opioid use to be a distinguishing feature between otherwise matched comparisons for CONs vs. each FM cohort.
One possible mechanism underlying spinal gray matter differences is tissue water content. Multimodal imaging of the brain has previously been used to test whether regional brain GMV decreases observed in FM are related to compromised neuronal integrity, as measured by GABAA receptor concentration7. Importantly, regional brain GMV decreases did not appear to be explained by GABAA receptor concentration, but instead by decreased tissue water content—theoretically as a function of altered cerebral blood flow, which has been previously observed in FM7,28. It is plausible that, similar to prior brain research, decreased water content may likewise account for the lower cervical spinal cord ventral and dorsal horn GMVs observed among some of the opioid-using individuals with FM in the present study. Meanwhile, it is important to note that the prior multimodal brain research did not specifically examine relationships between opioid use and reduced regional brain GMVs in FM.
Our within-group correlation analyses provide an important complement to our between-group observations. The distinct correlations we report in each cohort present a framework for future research questions. To begin with, while average pain duration was nearly twice as long in the FMO cohort compared with the FMN cohort, the association between pain duration with ventral/dorsal horn GMVs was statistically significant only in the FMN cohort. Furthermore, this was a positive correlation in the FMN cohort, but an inverse relationship (non-significant) in the FMO cohort. In other words, pain duration was significantly positively correlated with GMV in the cohort with shorter pain duration, while a non-significant inverse relationship between pain duration and GMV was observed in the cohort with longer pain duration. These contrasts beg the question of whether spinal gray matter is modified by the ongoing presence of pain, and likewise whether opioid therapy in chronic pain could meaningfully impact such a process.
Another set of future questions emerge from our findings that the FMO cohort exhibited statistically significant positive associations between dorsal/ventral horn GMV and pain interference, while also exhibiting a positive association between dorsal/ventral horn GMV and cold pain tolerance. Moreover, it is also curious that the FMO cohort demonstrated greater cold pain tolerance than the FMN cohort. While both FM cohorts reported upper extremity/quadrant pain per our eligibility criteria, we expect that sensory processing changes within the investigated spinal cord segments would relate to the dermatomes stimulated during the cold pressor test. Together, these results suggest that lower GMV in the FMO cohort is simultaneously associated with greater pain interference and with greater pain tolerance. One possible explanation for these seemingly contradictory observations is that CPT submersion time is heavily influenced by psychological factors (e.g., anxiety, expectancy, positive affect)29,30,31,32. If opioids are indeed driving the cohort-based distinctions, it may be that opioids are acting on affective factors that improve tolerance to pain, while simultaneously acting on sensory processing mechanisms that paradoxically increase ongoing pain severity and interference. Alternatively, it may be that longer pain duration in the FMO cohort has facilitated desensitization and subsequently greater tolerance to acute experimental pain. Finally, as another possible explanation, longer CPT submersion times in the FMO cohort could have been due to the active pharmacological effects of opioids, because we allowed participants to continue their regular prescribed opioid use during the study. Overall, the results from our correlation analyses underscore the value of assessing within-group analyses alongside between-group comparisons. Future research should aim to continue identifying not only between-group differences in spinal cord GMVs, but also the extent to which those differences may relate to clinical measures in different cohorts.
A few limitations should be noted in consideration of these results. First, this study is cross-sectional and thus does not afford causal inferences regarding the impact of opioid use on spinal cord GMVs over time. Future longitudinal studies initiated at commencement of opioid therapy and with larger sample sizes will be essential to accurately and explicitly capture the discrete effects of opioids on spinal cord ventral and dorsal GMVs; these studies may shed critical light on whether it is meaningful to prescribe opioids to FM patients. Furthermore, as mentioned previously, longitudinal studies evaluating spinal gray matter change over time in a non-opioid cohort will also be essential for understanding the relationship between pain duration and spinal gray matter. Additionally, this study was conducted in an all-female sample. Pain and opioid responses vary across the menstrual cycle, and sex hormones may significantly modify responses to opioids33. As such, future studies that capture the effects of menstrual-cycle related variability are critical to validate and extend the results of the present study. Furthermore, replication studies in cohorts of both males and females are likewise necessary to assess sex-specific changes in chronic pain, which have been previously described in the brain34. In a similar vein, future studies of cervical spinal cord gray matter alterations in other chronic pain conditions will also be critical to assess the generalizability of the present results. Additionally, due to the technology currently available at our research site, our spinal cord GMV analysis was limited to the cervical spinal cord region. Further, all participants with FM (per our eligibility criteria) reported bilateral upper extremity/quadrant pain; therefore, we were unable to determine localized vs. more widespread nature of our observed GMV differences across the spinal cord.
Overall, the present study provides the first examination of gray matter in the cervical spinal cord among a female-only sample of individuals with FM, individuals with FM who take opioids, and pain-free controls. We present novel evidence of variable, cohort-based associations between dorsal/ventral horn GMV and measures of pain. Our results build upon and help bridge multiple lines of prior research that have demonstrated (1) associations between spinal gray matter atrophy and clinical symptoms in disease processes that involve disrupted sensory processing, (2) FM-related distinctions in spinal cord functional activity at rest and during experimental pain, and (3) apparent opioid-related reductions of ventral-dorsal functional imbalance in FM. Together with the present findings, these studies highlight the importance of evaluating chronic pain-related structural changes throughout the entire central nervous system. While our study represents a first exploratory investigation of spinal cord GMV in individuals with FM and opioid use, the results require future validation and should not be used to inform opioid prescribing decisions. Our findings hold valuable implications for future mechanistic studies of FM—and of chronic pain in general—particularly regarding the extent to which chronic pain and opioid therapy may alter spinal cord structural integrity.
Methods
Participants
Data were obtained from female controls and females with fibromyalgia (FM, N = 96) who were recruited via local advertising from Durham, North Carolina and surrounding regions near Duke University Medical Center. Seven subjects were excluded due to missing scan data and 2 subjects were excluded for poor data quality. Thus, 87 participants were included in the final analysis: 29 control participants (CON), 27 individuals with fibromyalgia who were taking opioids (FMO), and 31 individuals with fibromyalgia who were not taking opioids (FMN). As this is the first spinal cord GMV analysis in patients with chronic pain, particularly FM, we were limited in our ability to conduct a power analysis a priori. However, other spinal cord GMV analyses in other clinical populations have reported significant group differences in spinal cord gray matter with similar group sizes10,11,12,13.
Regarding eligibility criteria, CON participants had no history of chronic pain and no history of substance abuse, including no extended (> 30 days) or recent (within the past 90 days) opioid use. Participants with FM were eligible if they met modified American College of Rheumatology 2016 criteria for fibromyalgia23. These criteria consisted of (1) a widespread pain index (WPI) of ≥ 7 plus a symptom severity (SS) score ≥ 5, or WPI score 3–6 plus SS score ≥ 9, (2) comparable symptoms present for at least 3 months, and (3) no diagnosis that would otherwise explain the pain. Additionally, participants were required to have pain in all 4 body quadrants (i.e., bilateral upper extremities, bilateral lower extremities), an average 0–10 verbal pain scale rating ≥ 2, and no uncontrolled psychiatric disorders. FMN participants were free of any substance use (confirmed by urine drug screen immediately prior to scanning) and endorsed no lifetime history of extended (> 30 days) or recent (within the past 90 days) opioid use. FMO participants reported current, regular use of opioids for at least the past 90 days.
Study procedures
All participants provided written informed consent prior to study procedures, and all study procedures were performed in accordance with protocols approved by Duke University’s Institutional Review Board (IRB). All methods were carried out in accordance with relevant guidelines and regulations, and all experimental protocols were approved by the Duke University IRB.
MRI acquisition and preprocessing
All study procedures were conducted in the Brain Imaging and Analysis Center at Duke University. Participants completed demographic and clinical questionnaires, as well as screening for MRI contraindications, prior to scanning. Imaging data were collected with a GE Signa Premier 3 Tesla scanner equipped with a 19-channel head and neck neurovascular array coil. Two structural scans were acquired: a T2-weighted sequence extending from the top of the cerebellum to the bottom of the T1 vertebra (single slab 3D fast spin echo, repetition time [TR] = 2500 ms, echo time [TE] = 85 ms, echo train length 70, field of view [FOV] = 240 × 240 mm2, matrix size = 256 × 256, slice thickness = 1.4 mm, effective resolution = 1.4 × 0.94 × 0.94 mm3, interpolated resolution = 0.7 × 0.47 × 0.47 mm3, number of averages = 2), and a 2D T2*-weighted axial multi-echo gradient-echo (MERGE) sequence acquired perpendicular to the spinal cord centered at the C6 vertebra (flip angle 20°, TE = 5.4 ms, TR = 525 ms, number of echoes = 3, 32 oblique slices, FOV = 180 × 144 mm2, matrix size = 320 × 192, in-plane resolution = 0.35 × 0.35 mm2, slice thickness = 3 mm, 0.5 mm spacing, number of averages = 2)35.
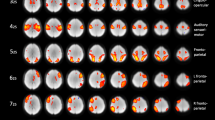
Image preprocessing was performed using Spinal Cord Toolbox (SCT) 5.0.1 36. The spinal cord segmentation was obtained using the sct_deepseg_sc command, then manually checked for quality control and updated as necessary. An invertebral disc levels mask was then created by manually identifying the posterior aspect of each intervertebral disc (C2/C3, C3/C4, C4/C5, C5/C6, C6/C7, C7/T1, T1/T2) on the T2-weighted images, which was subsequently used to register the T2-weighted images to the PAM50 T2-weighted template. The sct_deepseg_gm command was then used to segment the spinal cord gray matter, which was then registered to the PAM50 gray matter template using T2-to-template warps to initialize the T2* registration. The PAM50 atlas was then warped to the T2*-weighted images and the GMVs for ventral and dorsal horns (left and right combined) were extracted from the top of the C5 vertebra through the bottom of the C7 vertebra36 (Fig. 5). Total horn volumes were then calculated as left and right sums for each horn, and mean ventral and dorsal volumes per axial slice were computed by dividing horn size (voxels) by the number of slices.
Schematic of spinal cord gray matter volume analysis pipeline. Spinal cord preprocessing was performed using the Spinal Cord Toolbox. Images from a control participant were used to create the graphics for this figure. Panel A shows the PAM50 T2 -weighted template and the vertebral level masks. Panel B shows the template to T2-weighted structural image registration process. Panel C shows the process of segmenting the spinal cord gray matter. Gray matter volume (GMV) was extracted from the top of the C5 vertebra to the bottom of the C7 vertebra, and total horn GMVs were computed as left and right sums for each horn. D Dorsal, S Superior, V Ventral, R Right.
Quantitative sensory testing
Quantitative Sensory Testing (QST) was performed following the MRI scan. The Cold Pressor Test (CPT) is a test of cold pain tolerance and a validated measure of central sensitization37,38. Participants submerged their entire left hand up to the wrist into a container of cold water (approximately 5 °C) for up to 2 min. Total time (seconds) immersed in cold water served as the final metric representing cold pain tolerance. A proportion of the CPT data have been included in a previous publication39.
Clinical measures
Clinical questionnaires were administered to participants using a secure REDCap database and included the Brief Pain Inventory24. Additional information was collected regarding medications, including opioid dose (in morphine milligram equivalents, MME; FMO group only) and opioid use duration (years, FMO group only), and pain duration in years.
Statistical analysis
All statistical analyses were conducted using R 4.4.0 (IBM Corporation, Armonk, NY, USA). Due to our observed group differences in age across our 3 groups (described under Results “General Cohort Characteristics”), we assessed the association between our participant cohorts and average C5-C7 GMVs via one-way analysis of covariance (ANCOVA) models adjusting for age with a z-scale transformation across all 3 groups (N = 87) to improve model fit. Post-hoc pairwise assessments between our FM cohorts and controls also adjusted for age. Meanwhile, we further evaluated comparisons between FM cohorts through linear regression models adjusting for age with a z-scale transformation and pain duration (i.e., pain duration correction was conducted for the FM groups only). Spearman’s bivariate correlations—stratified by group—were conducted to examine relationships between dorsal horn and ventral horn GMVs and cold pain tolerance, pain questionnaires (pain severity and interference from the Brief Pain Inventory24), opioid use duration (years, FMO only), opioid dose (MME, FMO only), and pain duration (years). Since we evaluated only a few planned correlations and that this analysis is meant to be descriptive, we did not correct for multiple comparisons (i.e., for reporting purposes, significance was set at p < 0.05). Finally, given our final cohort size of 87 subjects and our smallest group size of 27 (FMO), we were ≥ 80% powered to detect a medium-large group effect (Cohen’s f = 0.36, η2 = 0.12) in our ANCOVA and moderate (rho = 0.51) correlations at a significance level of 0.05.
Sensitivity analysis
Due to the presence of outliers (i.e., GMV greater than 3 standard deviations from the group mean) in the FMO cohort dataset, we conducted a post-hoc sensitivity analysis to determine the effect of the outliers on (1) our group analyses of GMV and (2) on the correlations with pain/clinical data. The sensitivity analysis was conducted with the same statistical methods as for the main analysis described above, except for the exclusion of the 4 FMO patients. Results from the sensitivity analysis are presented in the Supplementary Table 3.
Data availability
Due to limitations of our IRB approved consent process during this study, the datasets cannot be shared publicly. The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Bagarinao, E. et al. Preliminary structural MRI based brain classification of chronic pelvic pain: A MAPP network study. Pain 155, 2502–2509 (2014).
Kairys, A. E. et al. Increased brain Gray matter in the primary somatosensory cortex is associated with increased pain and mood disturbance in patients with interstitial cystitis/painful bladder syndrome. J. Urol. 193, 131–137 (2015).
Apkarian, A. V. et al. Chronic back pain is associated with decreased prefrontal and thalamic Gray matter density. J. Neurosci. 24, 10410–10415 (2004).
Barad, M. J., Ueno, T., Younger, J., Chatterjee, N. & Mackey, S. Complex regional pain syndrome is associated with structural abnormalities in pain-related regions of the human brain. J. Pain. 15, 197–203 (2014).
Shi, H., Yuan, C., Dai, Z., Ma, H. & Sheng, L. Gray matter abnormalities associated with fibromyalgia: A meta-analysis of voxel-based morphometric studies. Semin Arthritis Rheum. 46, 330–337 (2016).
McCrae, C. S. et al. Fibromyalgia patients have reduced hippocampal volume compared with controls. J. Pain Res. 8, 47–52 (2015).
Pomares, F. B. et al. Histological underpinnings of grey matter changes in fibromyalgia investigated using multimodal brain imaging. J. Neurosci. 37, 1090–1101 (2017).
Martucci, K. T. & Mackey, S. C. Neuroimaging of pain: human evidence and clinical relevance of central nervous system processes and modulation. Anesthesiology 128, 1241–1254 (2018).
Schlaeger, R. et al. Spinal cord Gray matter atrophy correlates with multiple sclerosis disability. Ann. Neurol. 76, 568–580 (2014).
Agosta, F., Pagani, E., Caputo, D. & Filippi, M. Associations between cervical cord Gray matter damage and disability in patients with multiple sclerosis. Arch. Neurol. 64, 1302–1305 (2007).
Paquin, M. Ê. et al. Spinal cord Gray matter atrophy in amyotrophic lateral sclerosis. AJNR Am. J. Neuroradiol. 39, 184–192 (2018).
Huber, E. et al. Dorsal and ventral Horn atrophy is associated with clinical outcome after spinal cord injury. Neurology 90, e1510–e1522 (2018).
Smith, Z. A. et al. Magnetic resonance imaging Atlas-Based volumetric mapping of the cervical cord Gray matter in cervical Canal stenosis. World Neurosurg. 134, e497–e504 (2020).
Martucci KT, Weber KA, Mackey SC (2019) Altered Cervical Spinal Cord Resting-State Activity in Fibromyalgia. Arthritis & Rheumatology
Bosma, R. L. et al. FMRI of spinal and supra-spinal correlates of Temporal pain summation in fibromyalgia patients. Hum. Brain Mapp. 37, 1349–1360 (2016).
Woolf, C. J. Central sensitization: implications for the diagnosis and treatment of pain. Pain 152, S2–S15 (2011).
Latremoliere, A. & Woolf, C. J. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J. Pain. 10, 895–926 (2009).
Martucci KT, Weber KA, Mackey SC (2021) Spinal cord resting state activity in individuals with fibromyalgia who take opioids. Front. Neurol. 12:694271
Sluka, K. A. & Clauw, D. J. Neurobiology of fibromyalgia and chronic widespread pain. Neuroscience 338, 114–129 (2016).
Upadhyay, J. et al. Alterations in brain structure and functional connectivity in prescription opioid-dependent patients. Brain 133, 2098–2114 (2010).
Younger, J. W. et al. Prescription opioid analgesics rapidly change the human brain. Pain 152, 1803–1810 (2011).
Lin, J. C. et al. One month of oral morphine decreases Gray matter volume in the right amygdala of individuals with low back pain: confirmation of previously reported magnetic resonance imaging results. Pain Med. 17, 1497–1504 (2016).
Wolfe, F. et al. 2016 revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 46, 319–329 (2016).
Cleeland, C. S. & Ryan, K. M. Pain assessment: global use of the brief pain inventory. Ann. Acad. Med. Singap. 23, 129–138 (1994).
Ceko, M., Bushnell, M. C., Fitzcharles, M. A. & Schweinhardt, P. Fibromyalgia interacts with age to change the brain. Neuroimage Clin. 3, 249–260 (2013).
Kuchinad, A. et al. Accelerated brain Gray matter loss in fibromyalgia patients: premature aging of the brain? J. Neurosci. 27, 4004–4007 (2007).
Robinson, M. E., Craggs, J. G., Price, D. D., Perlstein, W. M. & Staud, R. Gray matter volumes of pain-related brain areas are decreased in fibromyalgia syndrome. J. Pain. 12, 436–443 (2011).
Williams, D. A. & Gracely, R. H. Biology and therapy of fibromyalgia. Functional magnetic resonance imaging findings in fibromyalgia. Arthritis Res. Ther. 8, 224 (2006).
Lee, J. E. & Watson, D. Frey law, L. A. Lower-order pain-related constructs are more predictive of cold pressor pain ratings than higher-order personality traits. J. Pain. 11, 681–691 (2010).
Feldner, M. T. & Hekmat, H. Perceived control over anxiety-related events as a predictor of pain behaviors in a cold pressor task. J. Behav. Ther. Exp. Psychiatry. 32, 191–202 (2001).
Hanssen, M. M., Vancleef, L. M. G., Vlaeyen, J. W. S. & Peters, M. L. More optimism, less pain! The influence of generalized and pain-specific expectations on experienced cold-pressor pain. J. Behav. Med. 37, 47–58 (2014).
Riquelme-Aguado V et al (2024) Correlation between different psychological variables in women with fibromyalgia with symptoms of neurogenic inflammation: A cross-sectional study. Biomedicines 12
Ribeiro-Dasilva, M. C. et al. Evaluation of menstrual cycle effects on morphine and Pentazocine analgesia. Pain 152, 614–622 (2011).
Baker, A. K. et al. Altered reward processing and sex differences in chronic pain. Front. Neurosci. 16, 889849 (2022).
Cohen-Adad, J. et al. Generic acquisition protocol for quantitative MRI of the spinal cord. Nat. Protoc. 16, 4611–4632 (2021).
De Leener, B. et al. Spinal cord toolbox, an open-source software for processing spinal cord MRI data. Neuroimage 145, 24–43 (2017).
Hazra, S. et al. A Cross-Sectional study on central sensitization and autonomic changes in fibromyalgia. Front. Neurosci. 14, 788 (2020).
Finan, P. H. et al. Discordance between pain and radiographic severity in knee osteoarthritis: findings from quantitative sensory testing of central sensitization. Arthritis Rheum. 65, 363–372 (2013).
Deng, E. Z., Weikel, D. P. & Martucci, K. T. Evaluation by survival analysis of cold pain tolerance in patients with fibromyalgia and opioid use. J. Pain Res. 15, 2783–2799 (2022).
Acknowledgements
We thank Lindsie Boerger for her assistance with participant recruitment and data collection. We especially thank all the participants for their generosity of time and effort spent in this study. This project was funded by the National Institutes of Health, National Institute of Drug Abuse (NIDA), K99/R00 DA040154, R01 DA055850 (awarded to K.T.M.), and L30DA059080 (awarded to A.K.B.) and National Institute of Neurological Disorders and Stroke (NINDS), K23 NS104211 and L30 NS108301 (awarded to K.A.W.).
Author information
Authors and Affiliations
Contributions
All authors contributed significantly to the manuscript and have read and approved the final manuscript. A.K.B., K.A.W. and K.T.M. developed and designed the study. A.K.B., S.H.P., and K.T.M. collected and organized the data. M.A.R. provided biostatistical expertise for data analyses. A.K.B., M.A.R., K.A.W., and K.T.M. analyzed and interpreted the data. A.K.B. wrote the first draft of the manuscript. A.K.B., M.A.R., S.H.P., K.A.W. and K.T.M. edited and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Baker, A.K., Rosser, M.A., Park, S.H. et al. Cross-sectional relationships between spinal cord gray matter volume and pain in individuals with fibromyalgia and opioid use. Sci Rep 15, 27810 (2025). https://doi.org/10.1038/s41598-025-13225-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-13225-7