Abstract
This study investigated the relationship between the dietary antioxidant index (DAI) with pathological markers (tumor size and Ki-67 marker) and the odds of breast cancer in Iranian women. In this matched case-control study, 155 women with breast cancer and 155 cancer-free women (18–70 years old) were recruited from Iran, using a convenience sampling method. Control participants were frequency-matched to cases by 5-year age-group. DAI score was calculated based on dietary data obtained from a 168-item FFQ. Linear regression with adjustment for confounding factors was used to determine the relationship between DAI and pathological markers. Logistic regression, adjusted for confounding factors, was employed to investigate the odds ratio (OR) of breast cancer according to the quantitative and qualitative (quartiles) scores of the DAI, with 95% CI. Logistic regression subgroup according to menopausal status was also performed. A non-significant inverse relationship was observed between DAI score and Ki-67 marker in the crude model and the adjusted models 2 and 3 (p ≥ 0.05). In the crude model, in the second quartile, the odds of breast cancer was significantly reduced compared to the first quartile (OR: 0.50, CI: 0.26–0.96). However, after adjusting for confounding factors in model 2, the odds of breast cancer decreased significantly in the second and third quartiles compared to the first quartile (p < 0.05). Also, by entering the DAI as a quantitative variable in model 3 of logistic regression, a significant decrease in the odds of breast cancer was observed (p = 0.03). In the postmenopausal stage, the odds of breast cancer in the second quartile decreased significantly compared to the first quartile in the crude model. Also, in model 3, after adjusting for confounding factors, the odds ratio of breast cancer in the second and third quartiles was significantly reduced compared to the first quartile (p < 0.05). This study suggests that a higher dietary antioxidant intake, as measured by the DAI, may be associated with a lower risk of breast cancer in Iranian women and this relationship is more significant in the postmenopausal stage. These findings highlight the potential benefits of dietary antioxidants and warrant further investigation into their role in breast cancer prevention strategies.
Similar content being viewed by others
Introduction
Cancer is the second most common cause of death in developed countries and the third most common cause of death in less developed countries1. Among women, breast cancer is the most common cancer globally, and it is also the leading cause of cancer death2. The risk of breast cancer has increased in recent decades, with estimates suggesting a rise from 1 in 10 women to 1 in 7 developing breast cancer in their lifetime3. According to the World Health Organization (WHO), in 2020, there were an estimated 2.3 million new cases of breast cancer diagnosed and 685,000 deaths globally4. Breast cancer is the most common cancer among Iranian women, and the mean age at diagnosis is significantly lower for Iranian women than for their Western counterparts5. Breast cancer comprises 42.53% of all malignancies in Iranian women, and more than 30% of these individuals are under 30 year’s old5,6. This cancer occurs due to uncontrolled growth and changes in the breast tissue and is usually accompanied by the appearance of a lump or mass in the patient7. To determine the effectiveness of primary treatments such as hormone therapy, adjuvant, and neoadjuvant chemotherapy, various prognostic and predictive pathological markers, including human epidermal growth factor receptor 2 (HER2), estrogen receptor (ER), progesterone receptor (PR), lymph node status, Ki-67, and tumor size are evaluated during invasive breast cancer8,9. Tumor size is usually expressed by the maximum diameter of the tumor and is an important index for assessing the status of breast cancer. There is an important relationship between tumor size and the prognosis of breast cancer and tumor metastasis. In fact, larger tumor size indicates a greater risk of metastasis and recurrence of the disease10. Also, Ki-67 is one of the markers currently used to determine the progress and degree of tumor proliferation in breast cancer. It has been shown that a higher Ki-67 index is associated with a more aggressive tumor and a higher risk of disease recurrence11.
Several risk factors such as genetic mutations, gender, hormonal factors, age, family history, environmental factors, lifestyle, and diet can affect breast cancer12. Among the mentioned risk factors, the role of diet as a potential environmental factor in the incidence of breast cancer is significant13. It has been reported that dietary patterns including the Mediterranean (Med) diet, Dietary Approaches to Stop Hypertension (DASH) diet, and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet can have a beneficial and effective role against cancer14. These diets emphasize the consumption of fruits and vegetables, especially green leafy vegetables, fish, and seafood and limit the consumption of animal foods rich in saturated fatty acids such as cream, butter, red meat, margarine, and fast/fried food15. A meta-analysis study has emphasized the effects of these diets on cancers risk with the mediating role of metabolites16. In this sudy, 10 important metabolites have been introduced that can play an important mediating role in the risk of cancers (total cholines, citrate, total lipids in large HDL, omega-3 fatty acids, tyrosine, creatinine, glucose, total lipids in VLDL, albumin, and free cholesterol in IDL)16. Among these metabolites, omega-3 plays the most important role as a mediator16. Omega-3 inhibits the production of cytokines induced by nuclear factor-κB, reduces the production of pro-inflammatory lipid derivatives, and slows down growth factor receptor signaling by changing lipid raft of cell membrane and through these mechanisms, it plays a protective role against cancers17. The Med, DASH, and MIND diets play a more effective role against cancer due to having omega-3 fatty acids food sources15. In another study, a direct relationship has been reported between the consumption of sweet drinks, red meat, animal fat, and processed meats and the increased odds of developing breast cancer18. Conversely, other studies have shown the protective role of consuming foods high in phytochemicals and antioxidants and low in saturated and trans fatty acids (such as whole grains, legumes, fruits, and vegetables) against cancers19,20. The dietary antioxidant index (DAI) and the dietary total antioxidant capacity (TAC) were designed to assess the antioxidant content of the diet21. In this study, the DAI was considered to evaluate the antioxidant status of the diet. This index is calculated based on the global mean and standard deviation of six antioxidant nutrients, and this scoring method is considered a suitable way to assess the antioxidant properties of a diet21. Studies examining the relationship between the antioxidant index and the odds of breast cancer have been conducted in Iran and around the world with contradictory results. Some studies have indicated that increasing the DAI can reduce the odds of breast cancer22,23while the lack of relationship between the DAI and the odds of breast cancer has also been seen24. Also, in a study that was conducted with the purpose of investigating the relationship between tumor size and the DAI, no significant relationship was found23. To our knowledge, there was no study regarding the association between the DAI and the Ki-67 marker.
As mentioned above, in recent years, breast cancer is the main cause of death in Iranian women, and the incidence rate is on the rise. Therefore, given the limitations of the studies conducted in this field in Iran, which present varying results, and considering the diverse dietary patterns of the Iranian population, it appears necessary to conduct more studies with a case-control design to obtain better and more precise results. Moreover, in most of the conducted studies, the relationship between the DAI and pathological markers (such as tumor size and Ki-67 marker) has not been explored. Consequently, this study was undertaken to determine the relationship between the DAI and pathological markers (tumor size and Ki-67 marker) and the odds of breast cancer in Iranian women.
Methods
Ethical consideration
At the beginning of the study, an informed consent form was obtained from all participants. Proficient patients provided written consent by reading and signing informed consent forms, while illiterate patients gave verbal consent. The study received ethical approval from the Sirjan School of Medical Sciences’ ethical committee (approval number: IR.SIRUMS.REC.1402.011).
Study design and participants
Our study adheres to the rigorous standards set forth by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement. This includes a structured approach to the design and a thorough adherence to the established guidelines for the reporting of observational studies25.
In this case-control study, which was based on hospital records, 155 female patients with breast cancer (newly diagnosed without receiving specific treatment and without changes in diet) were selected with histopathological confirmation by a physician26 using convenience sampling. The patient group was recruited from the Javad Al-Aemeh clinic in Kerman, Iran, from September 2021 to March 2023, according to the bellow inclusion criteria. The control group consisted of 155 apparently healthy women who were selected from the same clinic but from different departments of the same hospital. Women in the control group were considered cancer-free if they verbally confirmed they had no current cancer or history of cancer (no confirmatory exam or test was required). The control group’s health status was assessed based on self-reported medical histories and screening for non-neoplastic diseases, including orthopedic disorders, disc disorders, and eye, nose, ear, or skin disorders. Control participants were frequency-matched to cases by 5-year age-group.
The inclusion criteria for the case group included women aged 18–70 years, breast cancer diagnosis confirmed by histopathology, willingness to participate in the study, and newly diagnosed patients who had not received any special treatment at the time of recruitment. The inclusion criteria for the control group were similar: women aged 18–70 years with no history of breast cancer or any other cancer, and a willingness to participate in the study. Additionally, the exclusion criteria for both groups included individuals with heart, kidney, liver diseases, autoimmune diseases, diabetes, those following special diets such as vegetarianism, pregnant and breastfeeding individuals, those with any kind of mental and social disorder or shock, energy intake of less than 800 kcal or more than 5000 kcal, and those who had consumed anti-inflammatory drugs and antioxidant supplements in the past six months.
A general information questionnaire was also completed by the researcher, which included details such as age, drug history, education, employment status, marital status, smoking habits, alcohol consumption, physical activity, anthropometric indices, age at the onset of menstruation, age at menopause, pregnancy history, number of pregnancies, number of children, number of abortions, breastfeeding history, duration of breastfeeding, history of contraceptive pill usage, and family cancer history. The amount of physical activity was calculated by the International Physical Activity Questionnaire (IPAQ). The IPAQ consists of 7 questions and includes three parts: heavy activity with a coefficient of 8, moderate activity with a coefficient of 4, and walking with a coefficient of 3.3. The score for each part is calculated separately and, finally, the numbers are added together. A range between 0 and 600 min per week is considered light activity, 600 to 3000 min per week as moderate activity, and more than 3000 min per week as heavy activity. To obtain a score, the patient must be active for at least 10 min. The validity and reliability of this questionnaire have been confirmed (r = 0.7)27. The values of anthropometric indices were recorded by a nutrition expert. For anthropometric evaluations, height was measured using a wall-mounted height meter accurate to 0.5 cm (without shoes, heels against the wall, knees straight, looking forward, and shoulders in a normal position). The patients’ weight was measured with minimal clothing and without shoes using a Seca digital scale accurate to 0.5 kg. Waist circumference was measured at the top of the iliac crest and below the navel using a tape measure accurate to 0.5 cm. Additionally, the body mass index (BMI) was calculated by dividing the weight (in kilograms) by the square of the height (in meters).
Measurement of pathobiological markers
In the present study, the Ki-67 marker was measured based on mastectomy specimens using immunohistochemistry (IHC) by a pathologist. The ultrasound was used to measure tumor size. The grade of tumor was determined by a pathology test.
Dietary intake assessment and calculation of DAI score
In this study, information related to the participants’ food intake over the past year was collected through a 168-item Food Frequency Questionnaire (FFQ) by a trained nutritionist28. Subsequently, the reported values for each food item were converted to grams per day using the Iranian Home Scale Guide and analyzed with Nutritionist IV (NUT4) software. Consequently, the amounts of energy, macronutrients, and micronutrients consumed by each individual were determined by this software.
To calculate the DAI score, six nutrients with antioxidant properties including magnesium, selenium, zinc, vitamin A, vitamin C, and vitamin E were used. The method recommended by Benzie was employed to measure the DAI score According to the formula provided below, to calculate an individual’s DAI score, the mean intake of each of the six nutrients consumed by the individual was subtracted from the global mean intake and then divided by the global standard deviation. The resulting scores were then summed to determine the overall DAI score for each individual21.
Sample size
In this research, using the study of Pinar et al.29 and considering DAI score as the main variable, the sample size was calculated with a 15% loss of 155 individuals for each group.
In this formula, r is the ratio of controls to cases in the study. SD is the standard deviation of the outcome measure. Z_beta is the Z-score corresponding to the desired power of the study. Also, Z a/2 is the Z-score corresponding to the desired level of significance. And finally, d is the desired precision or effect size.
Data analysis
All data are reported as mean ± standard deviation (SD) for quantitative data and frequency (percentage) for qualitative data. The normality of the data was checked using the Kolmogorov-Smirnov test. Dependent variables were divided into quartiles based on the DAI score, and the differences between the quartiles were evaluated using one-way analysis of variance (ANOVA) for quantitative variables (with LSD post hoc) and the chi-square test for categorical variables. The comparison of quantitative results between case and control groups was performed using the independent samples t-test. Similarly, the chi-square test was used to compare qualitative variables between the case and control groups. The one-sample t-test was used to compare the food intake of individuals with the mean global consumption in the two groups. Linear regression, along with modeling by adjusting for confounding factors (model 1; without adjustment, model 2; adjustment for energy, and model 3 (stepwise); with correction for age, PA, marital status, education, pregnancy status, history of breastfeeding, family history of cancer, alcoholic beverages status, estrogen receptor (ER) expression, and human epidermal growth factor receptor2 (HER2) expression was used to determine the relationship between the DAI (independent variable) and tumor size and Ki-67 marker (dependent variables) in case group. The correlation between two quantitative variables (tumor size and Ki-67 marker) was assessed using the Pearson correlation test. Additionally, the odds of breast cancer (95% CI) according to DAI quartiles compared to the reference (OR = 1) were measured using logistic regression, with adjustment of confounding factors (model 1; unadjusted, model 2; adjusted for energy, and model 3; adjustment for energy, age, BMI, PA, marital status, status of menopause, number of pregnancies, number of abortion, duration of breastfeeding, education, employment, history of taking contraceptive pills, family history of cancer, smoking status, and alcoholic beverages status). Also, in the pre and post menopause status, the odds of breast cancer (95% CI) according to DAI quartiles compared to the reference (OR = 1) were measured using logistic regression, with adjustment of confounding factors (model 1; unadjusted, model 2; adjusted for energy, and model 3 (backward); adjustment for age, education, pregnancy status, number of pregnancies, number of children, lactation years, alcoholic beverages, history of contraceptive use, family history of cancer, and age of first menstruation). In this study, a p-trend was calculated for each model to compare the ORs associated with quartiles in each model. SPSS software version 23 (IBM SPSS Statistics, Armonk, USA) was used for data analysis. A p-value of less than 0.05 was considered statistically significant.
Results
The comparison of participants’ characteristics between the two groups of case and control
Table 1 shows the comparison of participants’ characteristics between the two groups of case and control. According to the results, there was no significant difference in the mean age between the case and control groups (46.72 ± 10.78 vs. 46.66 ± 11.15, p = 0.96, respectively). In the case group, about 32% of cancer patients were under 40 years old. Also, the mean score of DAI did not show a significant difference between the two groups (9.51 ± 8.47 vs. 8.89 ± 11.15, p = 0.58, respectively). Among the food components of the DAI (magnesium, vitamin C, vitamin E, vitamin A, zinc, and selenium), only the mean intake of vitamin C was significantly higher in the case group compared to the control group (127.09 ± 77.80 vs. 107.83 ± 72.04, p = 0.02, respectively), and no significant difference was observed between the intake of other components in the two groups (p for all ≥ 0.05). The mean BMI was significantly higher in the case group compared to the control group (26.88 ± 4.08 vs. 25.92 ± 4.34, p = 0.04). In terms of education, marital status, history of pregnancy and breastfeeding, number of pregnancies, number of children, period of breastfeeding, use of contraceptive pills, family history of cancer, and menopause status, there was a significant difference between the case and control groups (p for all < 0.05) (Table 1).
The characteristics at baseline across quartiles of DAI score in the case group
As shown in Table 2, a significant difference was observed between the quartiles of DAI score in the case group (p < 0.001). Specifically, the mean score of DAI was significantly higher in the second, third, and fourth quartiles compared to the first quartile; the third quartile compared to the second quartile; and the fourth quartile compared to the second and third quartiles (Table 2). Additionally, regarding the dietary intake of patients according to the DAI quartiles, there was a significant difference in magnesium, vitamin C, vitamin A, vitamin E, zinc, selenium, and energy in the case group (p for all < 0.05). Thus, the mean intake of energy, vitamin E, and zinc was significantly higher in the second, third, and fourth quartiles compared to the first quartile; the third quartile compared to the second quartile; and the fourth quartile compared to the second and third quartiles. The mean intake of magnesium was significantly higher in the second, third, and fourth quartiles compared to the first quartile and the fourth quartile compared to the second and third quartiles. The mean intake of vitamin C was significantly higher in the second, third, and fourth quartiles compared to the first quartile and the fourth quartile compared to the third quartile. The mean intake of vitamin A was significantly higher in the third quartile compared to the first quartile and the fourth quartile compared to the first quartile. The mean intake of selenium was significantly higher in the third and fourth quartiles compared to the first quartile and the fourth quartile compared to the second and third quartiles (Table 2). Furthermore, with the increase in the DAI score, a significant difference was noted in the mean score of the Ki-67 marker (p = 0.01). The mean score in the third quartile was significantly higher compared to the first quartile, and the mean score in the fourth quartile was significantly lower compared to the third quartile (Table 2).
The characteristics at baseline across quartiles of DAI score in the control group
In the control group, along with a significant increase in the DAI quartiles, a significant increase was observed in the mean of energy intake and the components of DAI (magnesium, vitamin C, vitamin A, vitamin E, zinc, and selenium) from the first quartile to the fourth quartile (p for all < 0.01). The results of the LSD post-hoc analysis showed that the mean of energy intake, magnesium, vitamin E, and zinc intakes were significantly higher in the second, third, and fourth quartiles compared to the first quartile; the third quartile compared to the second quartile; and the fourth quartile compared to the second and third quartiles. The mean intake of vitamin C was significantly higher in the third and fourth quartiles compared to the first quartile and the fourth quartile compared to the second and third quartiles. The mean intake of vitamin A was significantly higher in the second, third, and fourth quartiles compared to the first quartile and the fourth quartile compared to the second and third quartiles. With an increase in the DAI score, the mean intake of selenium increased significantly in the second, third, and fourth quartiles compared to the first quartile and the third and fourth quartiles compared to the second quartile (Table 3). Additionally, a significant difference was observed in the mean age and physical activity according to the quartiles of the DAI score (p < 0.001 and p = 0.03, respectively). As such, the mean age was significantly higher in the first quartile compared to the second, third, and fourth quartiles, and the second quartile compared to the fourth quartile. In terms of physical activity, the mean score was significantly higher in the second quartile compared to the first and fourth quartiles (Table 3).
Comparison of daily intake of energy and components of DAI with the global average daily consumption in the two case and control groups
The findings presented in Table 4 indicate that the average intakes of energy, magnesium, vitamin E, zinc, and selenium were significantly higher than the global averages in both the case and control groups (p < 0.001 for all). Conversely, the average intake of vitamin A was significantly lower than the global average in both groups (p < 0.001 for both). No significant differences were observed in the intake of vitamin C compared to the global averages in either group (p = 0.15 and p = 0.07, respectively).
Association between pathobiological markers of breast cancer including tumor size and Ki-67 and the relationship of these variables with DAI and age
As shown in Table 5, we found a positive and marginally significant relationship between tumor size and the Ki-67 marker (correlation coefficient = 0.14, p = 0.06). Multilinear regression analysis revealed no significant relationship between DAI and tumor size in the crude model and adjusted models 2 and 3 (P for all ≥ 0.05). Also, in both crude and adjusted models, a non-significant inverse relationship was observed between DAI and the Ki-67 marker (P for all ≥ 0.05) as shown in Table 5. In this study, the relationship between age and pathological markers of breast cancer was also investigated. The results showed a significant inverse relationship between age and Ki-67 marker (β = -0.39, p = 0.01). That is, with increasing age, the levels of this marker decreased (Table 5).
Odds ratios (95%CI) of breast cancer according to the DAI score
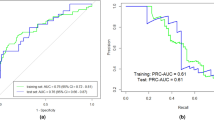
Table 6 presents the odds ratios for breast cancer based on the DAI score, as determined by logistic regression. In the crude model, which did not adjust for confounding factors, an increase in the DAI score was associated with a reduction in the odds of breast cancer. But this reduction was only significant in the second quartile compared to the reference (OR: 0.50, CI: 0.26–0.96). Furthermore, in model 2, which adjusted for the effects of energy, a significant reduction in the odds of breast cancer was observed in the second and third quartiles compared to the reference (OR = 1) (OR: 0.28, CI: 0.10–0.77 and OR: 0.35, CI: 0.15–0.84, respectively). In model 3, after including additional confounding factors, a reduction in the odds of breast cancer was reported in all three quartiles, but this reduction was not significant (p for all ≥ 0.05), as indicated in Table 6. Boxplot of OR in all 3 models is reported in Fig. 1. Also, by entering the DAI as a continuous variable in the logistic regression, in models 1 and 2, there was no significant decrease in the odds ratio of breast cancer (p ≥ 0.05). But by adding more confounding factors in model 3, a significant decrease in the odds ratio of breast cancer was seen (OR: 0.95, CI: 0.90–0.99, p = 0.03).
Odds rations (95%CI) of breast cancer according to the DAI score in the pre and post menopause status
As shown in Table 7, the association between the DAI and the odds of breast cancer was examined separately in premenopausal and postmenopausal women. In the pre-menopausal stage, the odds of breast cancer decreased with the increase of DAI score, but this relationship was not significant. Also, in the postmenopausal stage, the odds of breast cancer decreased with the increase of DAI score. Although, in the crude model, the odds of breast cancer in the second quartile decreased significantly compared to the first quartile (OR: 0.15, CI: 0.02–0.81). In model 3, after adjusting for confounding factors, the odds ratio of breast cancer in the second and third quartiles was significantly reduced compared to the first quartile (OR: 0.10, CI: 0.01–0.87, OR: 0.10, CI: 0.01–0.93, respectively) (Table 7).
Discussion
The current study’s findings demonstrated a non-significant inverse association between the DAI score and the Ki-67 marker. Furthermore, after adjusting for confounding factors, the results of this research indicated a notable reduction in the odds of developing breast cancer as the DAI score increased especially in the postmenopausal stage. This suggests that while dietary antioxidants may play a protective role in breast cancer risk, their influence on tumor characteristics may be more complex and context-dependent.
Our findings align with several previous studies that have reported an inverse association between dietary antioxidants and breast cancer risk. For example, a case-control study by Allahyari et al. (2022) found that higher DAI scores were associated with a reduced risk of breast cancer among Iranian women, consistent with our results22. Similarly, Vahid et al. (2023) reported a significant reduction in breast cancer odds with higher DAI scores, further supporting the protective role of antioxidant-rich diets23. Chung et al. documented that vitamin E has the potential to impede carcinogenesis and reduce the risk of developing cancer30. However, some studies have reported inconsistent findings. For instance, Fernandez-Lazaro et al. (2021) found no significant association between dietary antioxidants and breast cancer risk in a prospective cohort study25. These discrepancies may be due to differences in study design, population characteristics, or the methods used to assess dietary intake. Unlike our study, most previous research has not explored the relationship between the DAI and specific pathological markers such as tumor size and Ki-67, highlighting the novelty of our approach22,23,25. A noteworthy association between the DAI score and breast cancer was evident. After accounting for confounding factors, participants with higher DAI scores exhibited a 7% reduction in the odds of breast cancer compared to those with lower scores22. This aligns with our findings, reinforcing the potential protective role of dietary antioxidants. Additionally, a cross-sectional study by Sasanfar et al. (2021) found that higher dietary total antioxidant capacity (TAC) was associated with a reduced risk of breast cancer, further supporting the importance of antioxidant-rich diets in cancer prevention31. Despite these positive findings, some studies have not observed a significant relationship between dietary antioxidants and breast cancer risk. For example, Michels et al. (2007) conducted a review of prospective observational studies and found mixed results, with some studies reporting no association between antioxidant intake and breast cancer risk32. These inconsistencies may be attributed to variations in study populations, dietary assessment methods, and the specific antioxidants examined.
The protective effects of dietary antioxidants on breast cancer risk may be mediated through several mechanisms. Oxidative stress, caused by an imbalance between reactive oxygen species (ROS), and reactive nitrogen species (RNS) and antioxidant defenses, plays a critical role in carcinogenesis which dietary antioxidants, such as vitamins C and E, selenium, and zinc, neutralize ROS and reduce oxidative damage to DNA, proteins, and lipids33. This may inhibit the initiation and progression of cancer by preventing mutations and cellular damage33,34. Chronic inflammation is a key driver of cancer progression which antioxidants can modulate inflammatory pathways by reducing the production of pro-inflammatory cytokines and inhibiting the activation of transcription factors such as NF-κB35,36. Antioxidants have been shown to regulate cell cycle progression and induce apoptosis in cancer cells37. For example, vitamin C and carotenoids can influence the expression of genes involved in cell cycle control and programmed cell death, potentially reducing tumor aggressiveness37. This mechanism may explain the observed inverse relationship between the DAI score and Ki-67 marker, although it did not reach statistical significance in our study. Emerging evidence suggests that dietary antioxidants can influence epigenetic changes, such as DNA methylation and histone acetylation, which regulate gene expression involved in tumor growth and proliferation. For instance, selenium has been shown to modulate DNA methylation patterns, potentially suppressing oncogene expression and enhancing tumor suppressor activity38. The interrelated effects of dietary antioxidants can result in diverse overall outcomes. Hence, the design of the DAI aims to scrutinize the total antioxidant content in a diet39,40. Essentially, antioxidants act as cellular signaling regulators41. Antioxidants are known to alleviate oxidative stress in the body by influencing transcription factors and modulating the expression of genes associated with oxidative stress. Notably, certain dietary antioxidants have been shown to decrease levels of ROS and RNS by inducing an increase in the activity of the nuclear factor erythroid 2-related factor 2 transcription factor. This regulatory role highlights the potential of antioxidants in maintaining cellular balance and mitigating oxidative damage38 .In the context of cancer risk, both inflammation and oxidative stress emerge as distinct mechanisms, each independently contributing to the likelihood of cancer development35,37. Further support for the role of diet in cancer risk comes from another investigation affirming that a diet deficient in antioxidants correlates with an increased risk of colorectal cancer. This finding underscores the potential significance of antioxidant-rich dietary choices in mitigating colorectal cancer risk42. The overall importance of total carotenoids may be greater than the significance of studying any single carotenoid in isolation. This is due to the observation that various carotenoids can neutralize specific free radicals located at different sites within cellular membranes38,43. In the framework of a prospective cohort investigation, Pantavos et al. observed a link between a dietary profile with substantial antioxidant capacity and a lower risk of breast cancer44. Their findings suggest that the association between dietary antioxidants and breast cancer risk may depend on the diet’s overall antioxidant capacity and its ability to include a variety of antioxidant components44. Remarkably, the findings of the current study revealed a notable inverse association between the DAI score and the likelihood of developing breast cancer.
To accurately interpret the results of our study, it is important to consider both its strengths and weaknesses. The current study’s results are promising, and the study benefited from a relatively adequate sample size to assess the odds of breast cancer. However, increasing the sample size can help improve the accuracy of the results. Efforts were made to account for various variables that could impact cancer outcomes, such as energy intake, body composition, smoking, and alcohol consumption status, to control the impact of potential confounders. However, it is important to acknowledge certain limitations that warrant consideration. Firstly, due to the case-control design of this investigation, further research is needed to elucidate the potential mechanisms underlying these relationships. Secondly, the use of the FFQ to assess dietary intake may have introduced recall bias. Additionally, while this study investigated the relationship between the DAI score, tumor size, and the Ki-67 marker, a more accurate evaluation of this relationship may necessitate the design of single-group studies with a larger cohort of breast cancer patients who are in more advanced stages of the disease. Also, in this study, we used the DAI to examine the antioxidant status of individuals’ diets, whereas it would have been better to use the dietary total antioxidant capacity (TAC), which was more comprehensive and included more antioxidants. Another limitation of this study was the possibility of bias in the definitive diagnosis of cancer patients.
Conclusion
In summary, present research contributes to the existing body of evidence by reinforcing the observed non-significant inverse relationship between the DAI score and the Ki-67 marker in breast cancer patients. Notably, after adjusting for confounding factors, our analysis revealed an inverse association between the DAI score and the likelihood of developing breast cancer, especially in the postmenopausal stage. These findings suggest that a higher DAI score, indicative of a diet rich in antioxidants, may be associated with reduced breast cancer risk. However, the intricacies of this relationship, particularly among Iranian women, remain to be fully elucidated. Therefore, we suggest further studies to explore this interaction more deeply, using large-scale studies and preferably OMIC studies (i.e., metabolomics and nutrigenomics) where possible, which could potentially inform dietary recommendations for breast cancer prevention in this population.
Data availability
All data and materials are fully presented in the manuscript.
References
DeSantis, C. E. et al. Breast cancer statistics, 2019. CA Cancer J. Clin. 69, 438–451 (2019).
Torre, L. A. et al. Global cancer statistics, 2012. CA Cancer J. Clin. 65, 87–108 (2015).
Akram, M., Iqbal, M., Daniyal, M. & Khan, A. U. Awareness and current knowledge of breast cancer. Biol. Res. 50, 1–23 (2017).
WH O. https://www.who.int/news-room/fact-sheets/detail/breast-cancer. Breast cancer (2021).
Zahedi, A., Rafiemanesh, H., Enayatrad, M., Ghoncheh, M. & Salehiniya, H. Incidence, trends and epidemiology of cancers in North West of Iran. Asian Pac. J. Cancer Prev. 16, 7189–7193 (2015).
EnayatRad, M. & Salehinia, H. An investigation of changing patterns in breast cancer incidence trends among Iranian women. J. Sabzevar Univ. Med. Sci. 22, 27–35 (2015).
Wondmu, K. S., Tessema, M. T., Degu, G., Mihiret, G. T. & Sinshaw, M. T. Effect of breast cancer education based on the health belief model on knowledge, health belief, and breast self-examination among female students of Debre Markos University, Northwest Ethiopia, in 2021. Front. Oncol. 12, 1034183 (2022).
Urruticoechea, A., Smith, I. E. & Dowsett, M. Proliferation marker Ki-67 in early breast cancer. J. Clin. Oncol. 23, 7212–7220 (2005).
Jafari, S. H. et al. Breast cancer diagnosis: imaging techniques and biochemical markers. J. Cell. Physiol. 233, 5200–5213 (2018).
Wu, L., Zhou, X. & Yang, F. Assessing the relationship between tumor size, lymph node status, and ER/PR/HER2 expression in patients with breast cancer. Crit. Rev.™ Immunol. 45, 1– 9 (2025).
Choi, S. B. et al. Ki-67 and breast cancer prognosis: does it matter if Ki-67 level is examined using preoperative biopsy or postoperative specimen? Breast Cancer Res. Treat. 192, 343–352 (2022).
Jørgensen, K. J. et al. Overview of guidelines on breast screening: why recommendations differ and what to do about it. Breast 31, 261–269 (2017).
Hirko, K. A. et al. Healthy dietary patterns and risk of breast cancer by molecular subtype. Breast Cancer Res. Treat. 155, 579–588 (2016).
Sofi, F., Cesari, F., Abbate, R., Gensini, G. F. & Casini, A. Adherence to mediterranean diet and health status: meta-analysis. Bmj 337, a1344 (2008).
Ratjen, I. et al. Postdiagnostic mediterranean and healthy nordic dietary patterns are inversely associated with all-cause mortality in long-term colorectal cancer survivors12. J. Nutr. 147, 636–644 (2017).
Fan, Y. et al. Effects of diets on risks of cancer and the mediating role of metabolites. Nat. Commun. 15, 5903 (2024).
Fabian, C. J., Kimler, B. F. & Hursting, S. D. Omega-3 fatty acids for breast cancer prevention and survivorship. Breast Cancer Res. 17, 1–11 (2015).
Farvid, M. S. et al. Consumption of red and processed meat and breast cancer incidence: A systematic review and meta-analysis of prospective studies. Int. J. Cancer. 143, 2787–2799 (2018).
Kord-Varkaneh, H. et al. Association between healthy eating index-2015 and breast cancer risk: a case-control study. Asian Pac. J. Cancer Prevention: APJCP. 21, 1363 (2020).
Xiao, Y. et al. Association between whole grain intake and breast cancer risk: a systematic review and meta-analysis of observational studies. Nutr. J. 17, 1–12 (2018).
Wright, M. E. et al. Development of a comprehensive dietary antioxidant index and application to lung cancer risk in a cohort of male smokers. Am. J. Epidemiol. 160, 68–76 (2004).
Allahyari, P. et al. The association of dietary antioxidant index (DAI) with breast cancer among Iranian women. Int. J. Vitam. Nutr. Res. 93 (2022).
Vahid, F., Rahmani, W., Khodabakhshi, A. & Davoodi, S. H. Associated between dietary antioxidant index (DAI) and odds of breast cancer and correlation between DAI with Pathobiological markers: Hospital-Based incidence Case-Control study. J. Am. Nutr. Association. 42, 386–392 (2023).
Fernandez-Lazaro, C. I. et al. Dietary antioxidant vitamins and minerals and breast cancer risk: prospective results from the SUN cohort. Antioxidants 10, 340 (2021).
Von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370, 1453–1457 (2007).
Jalali, S. et al. Dietary inflammatory index and odds of breast cancer in a case-control study from Iran. Nutr. Cancer. 70, 1034–1042 (2018).
Gholami Fesharaki, M. & AzadMarzabadi, E. Evaluation of the reliability and validity of Azad-Fesharaki’s physical activity questionnaire (AFPAQ). J. Arak Univ. Med. Sci. 14, 36–44 (2011).
Mirmiran, P., Esfahani, F. H., Mehrabi, Y., Hedayati, M. & Azizi, F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health. Nutr. 13, 654–662 (2010).
Acikgoz Pinar, A., Yildiz, E. & Altundag, K. Dietary phytochemical index and the risk of breast cancer: A case-control study. Nutr. Cancer. 75, 482–487 (2023).
Yang, C. S. et al. Vitamin E and cancer prevention: studies with different forms of tocopherols and tocotrienols. Mol. Carcinog. 59, 365–389 (2020).
Sasanfar, B., Toorang, F., Maleki, F., Esmaillzadeh, A. & Zendehdel, K. Association between dietary total antioxidant capacity and breast cancer: a case–control study in a middle Eastern country. Public Health. Nutr. 24, 965–972 (2021).
Michels, K. B., Mohllajee, A. P., Roset-Bahmanyar, E., Beehler, G. P. & Moysich, K. B. Diet and breast cancer: a review of the prospective observational studies. Cancer: Interdisciplinary Int. J. Am. Cancer Soc. 109, 2712–2749 (2007).
Kang, D-H. Oxidative stress, DNA damage, and breast cancer. AACN Adv. Crit. Care. 13, 540–549 (2002).
Salehi, B. et al. Antioxidants: positive or negative actors? Biomolecules 8, 124 (2018).
Schieber, M. & Chandel, N. S. ROS function in redox signaling and oxidative stress. Curr. Biol. 24, R453–R462 (2014).
Reitz, L. K. et al. Diet quality is associated with serum antioxidant capacity in women with breast cancer: a cross sectional study. Nutrients 13, 115 (2020).
Prakash, P., Krinsky, N. I. & Russell, R. M. Retinoids, carotenoids, and human breast cancer cell cultures: a review of differential effects. Nutr. Rev. 58, 170–176 (2000).
Rasaei, N. et al. Effect of green tea supplementation on antioxidant status in adults: A systematic review and meta-analysis of randomized clinical trials. Antioxidants 10, 1731 (2021).
Vahid, F., Rahmani, D. & Davoodi, S. H. Validation of dietary antioxidant index (DAI) and investigating the relationship between DAI and the odds of gastric cancer. Nutr. Metabolism. 17, 1–9 (2020).
Kolarzyk, E., Pietrzycka, A., Zając, J. & Morawiecka-Baranek, J. Relationship between dietary antioxidant index (DAI) and antioxidants level in plasma of Kraków inhabitants. Adv. Clin. Experimental Med. 26, 393–399 (2017).
Ma, R. et al. Association between composite dietary antioxidant index and coronary heart disease among US adults: a cross-sectional analysis. BMC Public. Health. 23, 2426 (2023).
Obón-Santacana, M. et al. Dietary inflammatory index, dietary non-enzymatic antioxidant capacity, and colorectal and breast cancer risk (MCC-Spain Study). Nutrients 11, 1406 (2019).
Nishino, H. et al. Cancer prevention by phytochemicals. Oncology 69, 38–40 (2005).
Pantavos, A. et al. Total dietary antioxidant capacity, individual antioxidant intake and breast cancer risk: the R Otterdam study. Int. J. Cancer. 136, 2178–2186 (2015).
Acknowledgements
The authors would like to express their gratitude to all the staff of Javad Al-Aemeh clinic in Kerman city and all the individuals who participated in the study.
Funding
This work has been financially supported by the Vice Chancellor of Education and Research of Sirjan School of Medical Sciences (No: 401000032).
Author information
Authors and Affiliations
Contributions
A-KB: all steps of research and writing the manuscript, MD, AA, and NR: drafting and revision of the manuscript, MR-M and SA-RN: clinical supervision and conception or design, MD, MV, and H-BB drafting of the manuscript, HB: corresponding author, supervision, and all steps of research and writing the manuscript. The final version of the manuscript was agreed by all authors.
Corresponding author
Ethics declarations
Ethics declarations
The research protocol was in accordance with the guidelines of the Declaration of Helsinki. The Ethics Committee in Research of Sirjan School of Medical Sciences approved the study protocol (Ethical code: IR.SIRUMS.REC.1402.011). The informed written consent form was acquired from all individuals at the beginning of the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Khodabakhshi, A., Rasaei, N., Masoudi, M.R. et al. The association between dietary antioxidant index with tumor size, proliferation marker, and the odds of breast cancer in Iranian women. Sci Rep 15, 29982 (2025). https://doi.org/10.1038/s41598-025-15041-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-15041-5