Abstract
After a clinically isolated syndrome (CIS), antinuclear antibodies (ANAs) are often measured in diagnostic workup of inflammatory diseases. Although ANAs are associated with systemic lupus erythematosus (SLE), increased prevalence has been observed in multiple sclerosis (MS) with controversial significance. We determined in a prospective cohort study the association of ANAs measured during diagnostic workup with shared MS and SLE risk factors, clinical characteristics and disease course in CIS patients aged 18–65 years. ANA positivity was found in 60/364 (16.5%) participants and associated with female sex (83.3% vs. 67.4%, p = 0.01) and higher anti-EBNA1 IgG titres (median 1450.0 vs. 588.0 U/ml, p < 0.01), compared to ANA-negative participants. ANA-positive participants were more often homozygous carriers of HLA-DRB1*15:01 (12.8% vs. 2.7%, p < 0.01), but did not show higher MS or SLE genetic risk. Clinical characteristics and early disease course, estimated with Cox regression, were similar between participants with or without ANAs, regardless of a subsequent MS diagnosis. This study helps clinicians better interpret ANA positivity in patients with CIS. Our data demonstrate that ANA positivity during diagnostic workup for MS does not indicate a different disease course, but may reflect shared genetic and environmental risk factors for MS and SLE. Further studies should explore shared disease mechanisms.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) is an immune-mediated disease of the central nervous system (CNS), predominantly affecting women1. Exposure to environmental factors such as infection with Epstein–Barr virus (EBV) and a genetic predisposition contribute to the onset of MS1,2. In recent years, genome-wide association studies (GWAS) have identified over 200 risk loci3,4, highlighting the major contribution of the adaptive immune system to the pathogenesis of MS5,6. B cells seem to be relevant in the disease process, as B cell-depleting therapies are effective in suppressing MS disease activity and B cells with an antibody-secreting phenotype are present in lesions and cerebrospinal fluid (CSF) of people with MS7,8. The majority of MS patients shows increased concentrations of immunoglobulin G (IgG) antibodies with a unique oligoclonal pattern in CSF. These intrathecally produced antibodies are directed against a plethora of antigens, with no MS-specific antigen identified to date9,10.
After presentation with a clinically isolated syndrome (CIS), antinuclear antibodies (ANAs) are often measured in diagnostic workup of inflammatory diseases. ANAs are a diverse group of circulating autoantibodies directed against intracellular antigens. ANAs are associated with connective tissue diseases such as systemic lupus erythematosus (SLE); autoimmune diseases with a shared genetic background to MS11,12. ANAs have also been detected in patients with MS in higher frequencies with prevalence between 22.5 and 75%13,14,15,16,17,18. ANA positivity in the workup of CIS can complicate the diagnostic interpretation. Additionally, the clinical relevance in relation to the disease course of MS remains unclear. Previous studies have reported ANA prevalence and explored associations with disease duration and disability in MS, but results have been inconsistent14,15,17,19,20. However, ANA testing in these studies has been performed in heterogeneous MS populations without a standardised time point. To date, no study has investigated the predictive value of ANA presence for disease course shortly after symptom onset, a critical window due to the fluctuating nature of ANAs and the common timing of ANA testing21. Additionally, ANA presence at time of CIS has not been linked to shared genetic and environmental risk factors for developing MS and SLE.
Despite their unclear significance, ANAs may serve as a prognostic serum biomarker. Their presence may indicate distinct immunological subgroups with peripheral antibody production, alongside intrathecal IgG synthesis. Identifying such subgroups could clarify early disease heterogeneity in CIS22 and shared immunological risk factors between MS and SLE. This study aims to investigate the association of ANAs with clinical characteristics and disease course in CIS and early MS and to explore shared risk factors for developing MS and SLE. Our study includes an unique approach with important standardisation of ANA measurement at time of CIS and the assessment of genetic and environmental risk factors, providing insight into a common diagnostic finding and its biological relevance.
Methods
Study design and participants
Patients with a first demyelinating event of the CNS were eligible for participation in a prospective observational cohort study (PROUD) at the MS Centre of the Erasmus MC, Rotterdam. Patients aged 18–65 years were included within 6 months after symptom onset. MRI-scan and routine laboratory tests were assessed at baseline to rule out other diagnoses. If an alternative diagnosis was made, the patient was excluded from analysis. For this study, participants with available ANA status and complete diagnosis information were selected. The inclusion period was from November 2006 until February 2024. The study protocol was approved by the Medical Ethical Committee of the Erasmus MC, Rotterdam. All research was performed in accordance with relevant guidelines/regulations and in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
Data collection
Clinical, laboratory and radiological data were obtained from routine practice. Clinical data included sex, age at onset, topography of CIS, relapses and usage of methylprednisolone or disease-modifying therapies (DMTs). Data on family history and comorbidities were collected at baseline. Lumbar punctures (LPs) were performed as part of the diagnostic workup. IgG index and presence of oligoclonal bands (OCBs) in CSF were collected. OCBs were determined using isoelectric focusing and considered positive with ≥ 2 unique bands in CSF compared to serum. Baseline MRI brain was performed using sequences according to diagnostic requirements. MRI spinal cord was performed on clinical indication. MRIs were scored for presence of ≥ 9 T2-weighted lesions, gadolinium-enhancing lesions (GELs) and topography of lesions (infratentorial or spinal cord). Patients were reassessed annually at the outpatient clinic and more frequently on clinical indication or suspected relapse.
Serology
Serum samples were collected at baseline. ANAs were detected in clinical diagnostic workup using indirect immunofluorescence assay on the substrate of Human epithelial type-2 cells. ANAs titres of ≥ 1:80 were defined as ANA positivity23. Epstein–Barr virus nuclear antigen-1 (EBNA-1), early antigen (EA), viral capsid antigens (VCA) and Cytomegalovirus (CMV) IgG antibodies were measured using LIAISON® IgG chemiluminescent immunoassays (CLIA) on LIAISON® XL analyser (DiaSorin, Italy). Detection of Human Herpesvirus subtype-6 (HHV6) IgG antibodies was performed using ELISA-VIDITEST anti-HHV6 IgG kit (VIDIA, Prague, Czech Republic). Serological tests and analyses were conducted according to the manufacturer’s instructions. Serum samples were diluted (1:20) to prevent results from exceeding the detection limit.
Genotyping
Genomic DNA was isolated using baseline blood samples24. Samples were genotyped using Illumina Infinium High-Throughput Screening (HTS) iSelect custom-730K single nucleotide polymorphism (SNP) BeadChip array. Genotypes were imputed to the Haplotype Reference Consortium. Samples and variants with extremely low quality with genotyping call rate < 90% were excluded. Afterwards, another filtering was applied excluding samples with low quality with call rate < 97.5%. Hardy–Weinberg Equilibrium filter of 1 × 10−5 was applied and checked of excess of heterozygosity or homozygosity. Alleles with minor allele frequency < 0.05 and samples with familial relations were excluded.
Genetic variations and weighted genetic risk scores
Weighted genetic risk scores (wGRS) were calculated using the R script PRSice-225,26. We used the MS susceptibility GWAS of the International Multiple Sclerosis Genetics Consortium (IMSGC) as base file with the allelic odds ratio to calculate the wGRS of SNPs that reached genome-wide significance (PT < 5 × 10−8)3,27. Similarly, we calculated the SLE wGRS using a wide scale SLE GWAS, including the SNPs that reach PT < 2.5 × 10−5 for new loci discovered and PT < 1 × 10−4 for loci previously described28. We combined the MS and SLE susceptibility GWAS datasets and calculated a composite MS-SLE wGRS considering the p-value indicated in each study. Lastly, presence of the HLA-DRB1*15:01 allele was determined using rs3135388 as a tagging SNP29.
Definitions
MS was diagnosed according to the McDonald 2017 criteria30. Clinically definite MS (CDMS) was defined according to Poser as two attacks of at least 24 h with clinical evidence of dissemination in space31. A relapse was specified as the appearance of new neurological symptoms or exacerbation of known symptoms for at least 24 h, after at least 30 days of improvement or stable disease and in absence of fever or alternative diagnosis32.
Statistical analysis
ANA-positive and ANA-negative participants were compared in clinical characteristics and disease course after CIS. Descriptive statistics were used to present the data. Demographic and clinical data were compared using the Mann–Whitney U-test, T-test or ANOVA for continuous data, and Chi-squared test or Fisher’s exact test for categorical data. In anti-EBNA1 IgG analyses, we did not adjust for potential confounders age and sex, as these covariates did not improve the models’ fit. Survival analyses were used to assess time from CIS to McDonald 2017 MS and CDMS diagnosis. Multivariate Cox proportional hazards model analyses were performed to address potential confounders, as age at onset, sex, OCBs and ≥ 9 T2 lesions on baseline MRI. Patients who did not reach the endpoint by the end of follow-up were considered censored. The results were expressed as hazard ratios (HR) with their 95% confidence intervals (95% CI). Only complete cases were used in the Cox proportional hazard models. Sensitivity analyses were conducted in subgroup of patients with a confirmed McDonald 2017 MS diagnosis (MS subgroup) during follow-up and by stratification based on ANA titres (negative, 1:80 and ≥ 1:160). Statistical analyses were performed using the R software package version 4.4.1.
Results
Patient characteristics
The inclusion criteria were met by 364/445 CIS participants (Fig. 1). The median follow-up was 6.2 years (IQR 2.3, 10.8). Baseline characteristics were compared between ANA-positive (ANA +) and ANA-negative (ANA−) participants with CIS (Table 1). ANA positivity was found in 60/364 (16.5%) participants. Females were more represented in ANA+ compared to ANA− (83.3% vs. 67.4%, p = 0.01). ANA+ participants presented less frequently with optic neuritis (35.0% vs. 52.3%, p < 0.01) and more often with spinal cord symptoms (41.7% vs. 26.3%, p = 0.04) compared to ANA− participants. We found no other differences in baseline characteristics regarding clinical presentation, comorbidities with other autoimmune disease, family history of MS, presence of OCBs or MRI characteristics (Table 1). Next, we compared the baseline characteristics of participants with a confirmed McDonald 2017 MS diagnosis during follow-up (Supplementary Table S1). In total, 37/242 (15.3%) participants with a subsequent MS diagnosis were ANA+. Again, more females were ANA+ compared to ANA− (89.2% vs. 68.8%, p = 0.01). Multiple OCBs were present in all ANA+ compared to 80.6% of ANA− participants (p < 0.05), with other baseline characteristics similarly distributed. A sensitivity analysis stratifying for ANA titres did not show any other differences (Supplementary Table S2).
ANAs and EBV seropositivity
Since ANA positivity was associated with female sex as shared risk factor for developing MS and SLE, we investigated EBV seropositivity as another shared environmental risk factor33,34. We compared anti-EBNA1 IgG titres between 49 ANA + and 257 ANA− CIS participants. Within the CIS population, anti-EBNA1 IgG titres were almost 2.5-times higher in ANA+ compared to ANA− (Fig. 2, median 1450.00 U/ml [IQR 482.00, 3140.00] vs. 588.00 U/ml [IQR 247.00, 1640.00], respectively, p < 0.01). Among these, anti-EBNA1 IgG levels were over 2-times higher in 32 ANA+ compared to 174 ANA− participants with a McDonald 2017 MS diagnosis (Fig. 2, median 1520.00 U/ml [IQR 527.00, 3247.50] vs. 703.00 U/ml [IQR 319.00, 1707.00], respectively, p = 0.03). Stratifying for ANA titres 1:80 (n = 18) or titres ≥ 1:60 (n = 28), showed a slight dose–response relationship between ANA status and median anti-EBNA1 IgG (ANA− 588.00 U/ml [IQR 247.00, 1640.00], 1:80 1400.00 U/ml [IQR 412.25, 3087.50] and ≥ 1:160 1405.00 U/ml [IQR 497.00, 2915.00], p = 0.03, Supplementary Table S3).
Boxplots of EBNA1, EBV EA, EBV VCA, CMV and HHV6 IgG antibody titres. Panel (A, F and K) show the boxplots of anti-EBNA1 IgG titres in the total population, MS subgroup and CIS subgroup, with significantly increased levels in the ANA+ group for all analyses. Panel (B, G and L) present the EBV anti-EA IgG levels, with higher levels in the total population, but no differences in MS or CIS subgroup. In panel (C, H and M) the EBV anti-VCA IgG titre are shown with even distribution regarding ANA status for the total population, MS and CIS subgroup. The distribution of anti-CMV IgG are presented in panel (D, I and N), higher titres associated with ANA positivity in the total population and CIS subgroup, but not in MS subgroup. Panel (E, J and O) shows the anti-HHV6 IgG levels, with higher titres in the ANA-positive group in the total population and CIS subgroup, but similar distribution in the MS subgroup.
To explore antigen-specificity of this association, we compared the distribution of IgG levels against other antigens (Fig. 2). In the total cohort, ANA positivity was associated with increased IgG levels of EBV anti-EA (median 9.92 U/ml, [IQR 5.00, 42.50] vs. 6.08 U/ml, [IQR 5.00, 24.60], p < 0.01), anti-CMV (46.80 AU/ml [IQR 5.00, 144.00] vs. 5.00 AU/ml [IQR 5.00, 92.70], p = 0.01) and anti-HHV6 (2.06 U/ml [IQR 1.74, 2.44] vs. 1.89 U/ml IQR [1.46, 2.30], p = 0.02), without differences in anti-EBV VCA (median 592.00 U/ml [IQR 277.00, 894.00] vs. 492.00 U/ml, [IQR 220.00, 774.00], p = 0.36) (Fig. 2). Contrastingly, in analyses of the McDonald 2017 MS subgroup, anti-EBNA1 IgG levels were exclusively higher in ANA+ participants, with anti-EA, anti-VCA, anti-CMV, and anti-HHV6 evenly distributed (Fig. 2, Supplementary Table S4). In line, analyses with solely CIS participants showed ANA positivity associated with increased IgG levels of anti-EBNA1 (median 1160.00 U/ml [IQR 413.00, 2520.00] vs. 510.00 U/ml [IQR 117.00, 1250.00], p = 0.03), anti-CMV (102.00 U/ml [IQR 82.60, 153.00] vs. 5.00 U/ml [IQR 5.00, 94.75], p < 0.01) and anti-HHV6 (2.21 U/ml [IQR 1.75, 2.50] vs. 1.86 U/ml [IQR 1.38, 2.33], p = 0.03). This was not found for EBV anti-EA and anti-VCA (Fig. 2, Supplementary Table S5).
ANAs, HLA-DRB1*15:01 and MS and SLE susceptibility wGRS
Not only female sex and EBV exposure are shared risk factors between MS and SLE, but there is also substantial overlap in genetic risk factors11. We first analysed distribution of HLA-DRB1*15:01 as risk factor for developing MS and SLE35,36. ANA+ participants were more frequently homozygous carriers of HLA-DRB1*15:01 compared to ANA− participants (12.8% vs. 2.7%, p < 0.01, Fig. 3), with a similar trend in the subgroup of subsequent McDonald 2017 MS diagnosis (14.3% vs. 3.5%, p = 0.05). Heterozygosity for HLA-DRB1*15:01 was not associated with ANA status (Supplementary Table S6). Stratification for ANA titres showed a dose–response relationship (negative 2.7% vs. 1:80 11.1% vs. ≥ 1:160 15.4%, p < 0.01, Supplementary Table S7).
HLA-DRB1*15:01 and weighted Genetic Risk Scores (wGRS) for MS and SLE. Panel A and B show the distribution of the major risk allele HLA-DRB1*15:01, in total population and MS subgroup. In the total population (A), ANA-positive participants are more frequently homozygous carrier of HLA-DRB1*15:01 with a similar trend in the MS subgroup (B). Panel (C) and (F), the wGRS of MS susceptibility is shown with similar distribution between ANA+ and ANA− in total population and MS subgroup. For the wGRS of SLE, similar results are found in the total population (D) and MS subgroup (G). Panel (E) and (H) show the overlapping MS and SLE wGRS in total population and MS subgroup respectively, with no association with ANA status.
MS susceptibility wGRS did not differ between ANA+ and ANA− participants (Fig. 3, mean 7.47 (SD 1.49) vs. 7.18 (SD 1.17), p = 0.21). In the McDonald 2017 MS subgroup, MS wGRS was similar between ANA+ (28) and ANA− (171) participants (Fig. 3, mean 7.43 (SD 1.56) vs. 7.29 (SD 1.23), p = 0.66). The SLE wGRS neither associated with ANA status in the total cohort (ANA+ mean 5.87 (SD 0.78) vs. ANA− 6.01 (SD 0.96), p = 0.26) nor the McDonald 2017 MS subgroup (ANA+ 5.94 (SD 0.89) vs. ANA− 6.06 (SD 0.96), p = 0.51) (Fig. 3). To evaluate the effect of overlapping MS and SLE susceptibility wGRS, the composite wGRS revealed no association with ANA status in the total cohort and McDonald 2017 MS subgroup (Fig. 3, ANA+ mean 13.34 (SD 1.43) vs. ANA− 13.20 (SD 1.44), p = 0.53, and ANA+ 13.36 (SD 1.48) vs. ANA− 13.35 (SD 1.46), p = 0.97, respectively).
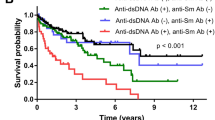
ANAs and early disease course
Next, the association between ANAs and time to McDonald 2017 MS diagnosis was analysed. During follow-up, 37/60 (61.7%) ANA+ and 205/304 ANA− (67.4%) participants were diagnosed with McDonald 2017 MS, with a similar median time from CIS to MS (Fig. 4A, 0.77 vs. 0.63 years, respectively, log-rank p = 0.65). Likewise, in patients with a confirmed McDonald 2017 MS diagnosis during follow-up, no difference in time to MS diagnosis was found (Fig. 4B, ANA+ 0.16 vs. ANA− 0.24 years, log-rank p = 0.33). In univariate Cox proportional hazard analysis of the total CIS population, ANA positivity was not associated with an earlier MS diagnosis (HR 0.92, 95% CI 0.65–1.30). After adjusting for potential confounders, we found no association between ANA positivity and an earlier MS diagnosis (HR 0.98, 95% CI 0.60–1.60). However, our model showed multiple OCBs and ≥ 9 T2 lesions on baseline MRI as significant predictors for earlier MS diagnosis (Fig. 5A). In both univariate (HR 1.20, 95% CI 0.84–1.70) and multivariate analyses (HR 1.20, 95% CI 0.71–1.90) of the subgroup reaching McDonald 2017 MS, ANA positivity was not associated with earlier MS diagnosis (Fig. 5B).
Kaplan Meier curves for time to McDonald 2017 MS and CDMS diagnosis. ANA-negative is shown in blue and ANA-positive in green. Panel (A) demonstrates time to McDonald 2017 MS in the total population and panel (B) for the MS subgroup. No differences in time to McDonald MS diagnosis were found with log-rank test p = 0.65 in total population and log-rank test p = 0.33 in the MS subgroup. In panel (C) time to CDMS is shown for the total population and in (D) the time to CDMS for the MS subgroup. In both analyses, no statistical difference was found (log-rank test p = 0.38 and 0.68, respectively).
Forest plots of the multivariate Cox proportional hazards models for time to McDonald 2017 MS and CDMS diagnosis. In panel (A) time to McDonald 2017 MS is shown for the total population and panel (B) for the MS subgroup. In both analyses, no association is found with ANA positivity and earlier McDonald MS diagnosis (HR 0.98, 95% CI 0.60–1.60 and HR 1.20, 95% CI 0.71–1.90). In panel (C) time to CDMS is shown for the total population and in (D) the time to CDMS for the MS subgroup. In total population and MS subgroup, no association between ANA status and earlier CDMS diagnosis was found (HR 0.71, 95% CI 0.37–1.36 and HR 0.84, 95% CI 0.43–1.60).
To account for changes in clinical practice over time, we associated ANA status with time to CDMS diagnosis. In ANA+ participants, 22/60 (36.7%) experienced a second relapse and received a CDMS diagnosis, compared to 138/304 (45.4%) ANA− participants. In the CIS cohort, median time from CIS to CDMS was similar between ANA+ and ANA− (Fig. 4C, 8.59 vs. 6.66 years respectively, log-rank p = 0.38). Within the McDonald 2017 MS subgroup, we found no differences in median time to CDMS (Fig. 4D, ANA+ 3.84 vs. ANA− 3.10 years, log-rank p = 0.68). No association between ANA positivity and time to CDMS was found in both univariate and multivariate analyses (HR 0.82 [95% CI 0.52–1.3] and HR 0.71 [95% CI 0.37–1.36] respectively, Fig. 5C). In the McDonald 2017 MS subgroup, ANA positivity was not associated with earlier CDMS diagnosis in univariate and multivariate analyses (HR 0.91 [95% CI 0.58–1.4] and HR 0.84 [95% CI 0.43–1.60] respectively, Fig. 5D).
Discussion
Our study demonstrates that ANA positivity is not associated with a distinct presenting clinical phenotype of CIS or subsequent diagnosis of MS. However, female sex, high anti-EBNA1 IgG titres and homozygous carriership of HLA-DRB1*15:01 associate with ANA presence in CIS patients. Shared environmental and genetic risk factors between SLE and MS may drive ANA presence in CIS and early MS. These findings indicate that ANAs are not useful as prognostic biomarker for disease course in early MS but rather reflect shared etiological mechanisms culminating in ANA positivity. This study provides clinicians a better understanding of ANA positivity in CIS and early MS.
In our study, ANA positivity was found in 16.5% of the CIS population and in 15.3% of the subgroup with subsequent McDonald MS diagnosis. This is lower than previous reported prevalence of 22.5–75% in MS populations13,14,15,16,17,18. However, ANA titres are heterogeneous and the differences could be attributed to the used cut-off, type of patients and the timing of ANA measurement, as ANA titres are known to fluctuate over time21. We were not able to perform additional immunoblotting to determine specific antibodies. Identifying specific ANA subtypes could provide deeper insight, particularly in light of recent findings showing associations between certain scleroderma-related autoantibodies and MS-like presentations37. In the total population, ANA+ and ANA− participants showed differences in CIS topography. CIS often marks the onset of MS, but other (inflammatory) CNS diseases can present similarly22,38. ANA− participants presented more often with optic neuritis, which has also non-inflammatory causes, such vascular and genetic disorders22. In contrast, myelitis—more frequently noted in ANA+ participants—has a broader inflammatory differential diagnosis, possible explaining the observed association39.
Several studies have reported conflicting associations between ANA positivity and disease course in MS, but in these studies ANAs were analysed in heterogeneous MS populations without a standardised time point. Our study adds clinical relevance by evaluating ANA presence at CIS—both a common diagnostic finding at this time point and potentially the most sensitive window to detect the influence of risk factors on disease onset. Yet, no associations with early disease course after CIS were observed and ANA positivity was not found to be a predictor of earlier McDonald 2017 MS or CDMS diagnosis. However, we found associations with known genetic and environmental risk factors for both MS and SLE susceptibility. Like MS, SLE shows strong associations with female sex and EBV infection33,34. The shared immunogenetic background of SLE and MS, among other AIDs, is increasingly supported40. Recently, genetic mapping found about 40% of shared loci for AIDs are driven by the same causal allele11,12. These overlapping genetic risk factors include variants in HLA-DRB111. Our observed association of ANA positivity with homozygous carriership of HLA-DRB1*15:01 fits within this context, as it may reflect shared genetic susceptibility. HLA-DRB1*15:01 is strongly associated with MS susceptibility, particularly in homozygous carriers, and it has also been linked to SLE, although stronger associations were found in different HLA-DRB1 alleles, reflecting the gene’s polymorphic features35,36,41. Recent work has shown that type I interferon signatures, elevated in SLE and Sjögren’s, differentiate between systemic autoimmune disease and MS, suggesting fundamental differences in their immunopathogenesis42. This supports the idea that, despite shared risk loci like HLA-DRB1 reflecting genetic susceptibility, distinct immune pathways drive disease specificity. Since OCBs have also been linked to HLA-DRB1*15:0143, a shared immunogenetic factor may explain the universal presence of OCBs in all ANA+ MS participants and support a link between of both circulating and intrathecal IgGs production. Several circulating antibodies, including pathogenic IgG fractions and autoantibodies against CNS antigens, have been detected in subgroups of patients with MS44,45.
ANA presence associated exclusively with high anti-EBNA1 IgG levels in the group with confirmed MS, while associations with several other antiviral antibodies were only found in CIS participants without subsequent MS. Specifically, anti-EBNA1 IgG responses are the strongest environmentally-determined risk factor for developing MS, while this is much less clear for antibodies against other EBV-antigens, such as EA and VCA2. In SLE cohorts, anti-VCA IgG antibodies have been associated with disease onset33. Additionally, anti-CMV IgG responses have been associated with a lower risk of MS46. The contrasting associations of ANA with antiviral antibody profiles between CIS and MS subgroups support the fundamental role for antiviral responses in MS susceptibility34. Like ANAs, the association of anti-EBNA1 IgG with course and severity of MS is controversial47. Additionally, genetic factors contributing to MS susceptibility have not been associated with severity or disability accumulation in MS3,48. These findings align with our observation that ANA presence reflects risk factors rather than disease course itself in MS.
There are some limitations of this study. First, around 20% of the patients, similarly distributed between ANA− and ANA+ participants, received methylprednisolone or DMTs before blood sampling. Corticosteroids could to lower the proportion of circulating antibodies, manifesting as potentially false-negative49. Yet, subgroup analyses of only untreated participants showed similar results. Second, the absence of a control group complicates the interpretation of the observed prevalence of 16.5% in the CIS population compared to background population levels. Although in the healthy population, ANA positivity is seen in 15–30% of people depending of cut-off titre and methods50,51, including local controls group would improve contextualise the findings. Furthermore, the small sample size of each group (including ANA titre subgroup) limited our statistical power and possibilities for within-group comparisons and may have prevented the detection of moderate effects on time-to-diagnosis analyses. However, we used Cox proportional hazard models with higher statistical power to be able to analyse associations. Additionally, we included participants in this study based on neurological symptoms consistent with CIS or suspected MS, with their clinical presentation not attributable to systemic AID at baseline or in follow-up. This resulted in exclusion of patients with an alternative diagnosis than CNS demyelination consistent with MS, including connective tissue disorders or other neuroinflammatory disorders. This could explain the similar distribution of known AID at baseline, but participants may have developed AIDs later in their course52. Selection bias could have occurred as not all eligible patients were included for analyses due to missing baseline information. Finally, since ANA status was only measured at baseline, we could not assess associations later in disease course. However, our study aimed to evaluate the prognostic value of ANA positivity in the context of CIS/MS at symptom onset, i.e. regardless of current or future comorbid autoimmune diagnoses. This approach reflects the real diagnostic settings in which ANA testing is often performed, highlighting its clinical relevance.
To conclude, the presence of ANAs in patients with CIS does not indicate a different disease course in MS, but reflects an effect of shared environmental and genetic risk factors for developing MS and SLE. This study supports clinicians in interpreting ANA positivity in patients with CIS and early MS. Further studies on shared disease mechanisms between SLE and MS could guide exploration of fundamental pathways underlying the onset of these diseases, resulting in potential novel avenues for prevention and treatment.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Abbreviations
- AID:
-
Autoimmune disease
- ANA:
-
Antinuclear antibody
- CIS:
-
Clinically isolated syndrome
- CMV:
-
Cytomegalovirus
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- DMTs:
-
Disease-modifying therapies
- EA:
-
Early antigen
- EBV:
-
Epstein–Barr virus
- EBNA1:
-
Epstein–Barr Nuclear Antigen-1
- GELs:
-
Gadolinium-enhancing lesions
- GWAS:
-
Genome-wide association studies
- HHV6:
-
Human Herpesvirus subtype 6
- HLA:
-
Human leukocyte antigen
- IgG:
-
Immunoglobulin G
- IMSGC:
-
International Multiple Sclerosis Genetics Consortium
- LP:
-
Lumbar puncture
- MS:
-
Multiple sclerosis
- OCBs:
-
Oligoclonal bands
- SLE:
-
Systemic lupus erythematosus
- SNP:
-
Single nucleotide polymorphism
- VCA:
-
Viral capsid antigens
- wGRS:
-
Weighted genetic risk score
References
Thompson, A. J., Baranzini, S. E., Geurts, J., Hemmer, B. & Ciccarelli, O. Multiple sclerosis. Lancet 391, 1622–1636 (2018).
Bjornevik, K. et al. Longitudinal analysis reveals high prevalence of Epstein–Barr virus associated with multiple sclerosis. Science 375(6578), 296 (2022).
International Multiple Sclerosis Genetics Consortium. Multiple sclerosis genomic map implicates peripheral immune cells and microglia in susceptibility. Science 365(6460), eaav7188 (2019).
Baranzini, S. E. & Oksenberg, J. R. The genetics of multiple sclerosis: From 0 to 200 in 50 years. Trends Genet. 33, 960–970 (2017).
International Multiple Sclerosis Genetics Consortium, Wellcome Trust Case Control Consortium et al. Genetic risk and a primary role for cell-mediated immune mechanisms in multiple sclerosis. Nature 476(7359), 214–219 (2011).
Hemmer, B., Kerschensteiner, M. & Korn, T. Role of the innate and adaptive immune responses in the course of multiple sclerosis. Lancet Neurol. 14(4), 406–419 (2015).
Bogers, L. et al. Selective emergence of antibody-secreting cells in the multiple sclerosis brain. EBioMedicine 89, 104465 (2023).
Michel, L. et al. B cells in the multiple sclerosis central nervous system: Trafficking and contribution to CNS-compartmentalized inflammation. Front. Immunol. 6, 636 (2015).
den Dunnen, J., Mes, L., Hoepel, W. & Smolders, J. Multiple sclerosis: Why we should focus on both sides of the (auto)antibody. Neural Regen. Res. 16(12), 2422–2424 (2021).
Brandle, S. M. et al. Distinct oligoclonal band antibodies in multiple sclerosis recognize ubiquitous self-proteins. Proc. Natl. Acad. Sci. U. S. A. 113(28), 7864–7869 (2016).
Lincoln, M. R. et al. Genetic mapping across autoimmune diseases reveals shared associations and mechanisms. Nat. Genet. 56(5), 838–845 (2024).
Cotsapas, C. et al. Pervasive sharing of genetic effects in autoimmune disease. Plos Genet. 7(8), e1002254 (2011).
Barned, S., Goodman, A. D. & Mattson, D. H. Frequency of anti-nuclear antibodies in multiple sclerosis. Neurology 45(2), 384–385 (1995).
Collard, R. C., Koehler, R. P. & Mattson, D. H. Frequency and significance of antinuclear antibodies in multiple sclerosis. Neurology 49(3), 857–861 (1997).
Tourbah, A. et al. Systemic autoimmune features and multiple sclerosis: A 5-year follow-up study. Arch. Neurol. 55(4), 517–521 (1998).
Spadaro, M. et al. Autoimmunity in multiple sclerosis: Study of a wide spectrum of autoantibodies. Mult. Scler. J. 5(2), 121–125 (1999).
Szmyrka-Kaczmarek, M. et al. Antinuclear and antiphospholipid antibodies in patients with multiple sclerosis. Lupus 21(4), 412–420 (2012).
Alnajashi, H. & Alshamrani, F. Prevalence of antinuclear antibody in patients with multiple sclerosis: A case-control study. Egypt. J. Neurol. Psych. 57(1), 27 (2021).
Mejdoub, S. et al. Antinuclear antibodies positivity is not rare during multiple sclerosis and is associated with relapsing status and IgG oligoclonal bands positivity. Rev. Neurol. 178(8), 812–816 (2022).
Koshorek, J. et al. Relevance of antinuclear antibody in diagnosis and characteristics of multiple sclerosis. Mult. Scler. Relat. Disord. 87, 105639 (2024).
Pisetsky, D. S. & Lipsky, P. E. New insights into the role of antinuclear antibodies in systemic lupus erythematosus. Nat. Rev. Rheumatol. 16(10), 565–579 (2020).
Miller, D. H., Chard, D. T. & Ciccarelli, O. Clinically isolated syndromes. Lancet Neurol. 11(2), 157–169 (2012).
Aringer, M. et al. 2019 European league against Rheumatism/American college of rheumatology classification criteria for systemic lupus erythematosus. Ann. Rheum. Dis. 78(9), 1151–1159 (2019).
Miller, S. A., Dykes, D. D. & Polesky, H. F. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 16(3), 1215 (1988).
Euesden, J., Lewis, C. M. & O’Reilly, P. F. PRSice: Polygenic risk score software. Bioinformatics 31(9), 1466–1468 (2015).
Choi, S. W. & O’Reilly, P. F. PRSice-2: Polygenic risk score software for biobank-scale data. Gigascience 8(7), giz082 (2019).
De Jager, P. L. et al. Integration of genetic risk factors into a clinical algorithm for multiple sclerosis susceptibility: A weighted genetic risk score. Lancet Neurol. 8(12), 1111–1119 (2009).
Bentham, J. et al. Genetic association analyses implicate aberrant regulation of innate and adaptive immunity genes in the pathogenesis of systemic lupus erythematosus. Nat. Genet. 47(12), 1457 (2015).
Zivkovic, M. et al. The tag SNP for HLA-DRB1*1501, rs3135388, is significantly associated with multiple sclerosis susceptibility: Cost-effective high-throughput detection by real-time PCR. Clin. Chim. Acta 406(1–2), 27–30 (2009).
Thompson, A. et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 17, 162–173 (2018).
Poser, C. M. et al. New diagnostic criteria for multiple sclerosis: Guidelines for research protocols. Ann. Neurol. 13(3), 227–231 (1983).
Schumacher, G. et al. Problems of experimental trials of therapy in multiple sclerosis: Report by the panel on the evaluation of experimental trials of therapy in multiple sclerosis. Ann. N. Y. Acad. Sci. 122, 552–568 (1965).
Li, Z. X., Zeng, S., Wu, H. X. & Zhou, Y. The risk of systemic lupus erythematosus associated with Epstein–Barr virus infection: A systematic review and meta-analysis. Clin. Exp. Med. 19(1), 23–36 (2019).
Bogers, L., Kuiper, K. L., Smolders, J., Rip, J. & van Luijn, M. M. Epstein–Barr virus and genetic risk variants as determinants of T-bet+ B cell-driven autoimmune diseases. Immunol. Lett. 261, 66–74 (2023).
Patsopoulos, N. A. et al. Fine-mapping the genetic association of the major histocompatibility complex in multiple sclerosis: HLA and non-HLA effects. Plos Genet. 9(11), e1003926 (2013).
Morris, D. L. et al. Unraveling multiple MHC gene associations with systemic lupus erythematosus: Model choice indicates a role for HLA alleles and non-HLA genes in Europeans. Am. J. Hum. Genet. 91(5), 778–793 (2012).
Mavragani, C. P. et al. Scleroderma specific autoantibodies and MS-like manifestations: A novel association?. Autoimmun. Rev. 20(8), 102871 (2021).
Wildner, P., Stasiolek, M. & Matysiak, M. Differential diagnosis of multiple sclerosis and other inflammatory CNS diseases. Mult. Scler. Relat. Disord. 37, 101452 (2020).
Pardo, C. A. Clinical approach to myelopathy diagnosis. Continuum (Minneap Minn). 30(1), 14–52 (2024).
Nikolopoulos, D. et al. Demyelination with autoimmune features: A distinct clinical entity? Results from a longitudinal cohort. Rheumatology 60(9), 4166–4174 (2021).
Moutsianas, L. et al. Class II HLA interactions modulate genetic risk for multiple sclerosis. Nat. Genet. 47(10), 1107 (2015).
Karathanasis, D. K. et al. Differentiating central nervous system demyelinating disorders: The role of clinical, laboratory, imaging characteristics and peripheral blood type I interferon activity. Front. Pharmacol. 13, 898049 (2022).
Imrell, K., Landtblom, A. M., Hillert, J. & Masterman, T. Multiple sclerosis with and without CSF bands: Clinically indistinguishable but immunogenetically distinct. Neurology 67(6), 1062–1064 (2006).
Elliott, C. et al. Functional identification of pathogenic autoantibody responses in patients with multiple sclerosis. Brain 135(Pt 6), 1819–1833 (2012).
Kuerten, S. et al. Autoantibodies against central nervous system antigens in a subset of B cell-dominant multiple sclerosis patients. Proc. Natl. Acad. Sci. U. S. A. 117(35), 21512–21518 (2020).
Sundqvist, E. et al. Cytomegalovirus seropositivity is negatively associated with multiple sclerosis. Mult. Scler. J. 20(2), 165–173 (2014).
Munger, K. L. et al. No association of multiple sclerosis activity and progression with EBV or tobacco use in BENEFIT. Neurology 85(19), 1694–1701 (2015).
The International Multiple Sclerosis Genetics Consortium. Locus for severity implicates CNS resilience in progression of multiple sclerosis. Nature 619(7969), 323–331 (2023).
Weisbart, R. H. & Colburn, K. Effect of corticosteroids on serum antinuclear antibodies in man. Immunopharmacology 8(2), 97–101 (1984).
Li, Q. Z. et al. Risk factors for ANA positivity in healthy persons. Arthritis Res. Ther. 13(2), R38 (2011).
Marin, G. G., Cardiel, M. H., Cornejo, H. & Viveros, M. E. Prevalence of antinuclear antibodies in 3 groups of healthy individuals. Jcr-J. Clin. Rheumatol. 15(7), 325–329 (2009).
Wijeyesinghe, U. & Russell, A. S. Outcome of high titer antinuclear antibody positivity in individuals without connective tissue disease: A 10-year follow-up. Clin. Rheumatol. 27(11), 1399–1402 (2008).
Acknowledgements
The International MS Genetics Consortium (IMSGC) is acknowledged for providing the summary statistics for wGRS analysis. We thank J.P.A. Samijn, N. Jafari, B. van den Berg and J.W.K. de Beukelaar for their contributions to the PROUD study and the PROUD participants for their participation.
Funding
This work is funded by the Nationaal MS Fonds (Educational grant P2021-001) and Stichting MOVES ‘Klimmen tegen MS’ (Inspiratiebeurs).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Cato Corsten, Ana Marques and Despoina Masmanidou. The first draft of the manuscript was written by Cato Corsten and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
M. van Luijn received research support from EMD Serono, Merck, Novartis, GSK and Idorsia Pharmaceutical Ltd. J. Smolders reports grants for scientific research from Biogen, Roche and Siemens Healthineers and received speaker and/or consultancy fee of Biogen, Merck, Novartis, Roche and Sanofi. All the remaining authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Corsten, C.E.A., Marques, A.M., Masmanidou, D. et al. Antinuclear antibodies in early multiple sclerosis reflect systemic lupus erythematosus shared risk factors. Sci Rep 15, 32969 (2025). https://doi.org/10.1038/s41598-025-17254-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-17254-0