Abstract
Myotonia and paramyotonia congenita (PC) are rare neuromuscular disorders characterized by muscle stiffness that intensifies in cold environments. These disorders are associated with variants in the SCN4A gene, that encodes the alpha subunit of the voltage-gated sodium channel Nav1.4. We report here the case of a 36-year-old female who experiences diverse neurological symptoms, including myotonia, cold induced myotonia, resulting in muscle stiffness, and tightness. A whole exome sequencing revealed a missense variant in the SCN4A gene at position c.1354G > A, named p.E452K. We characterized the biophysical properties of this SCN4A variant by overexpressing the wild-type (WT) and mutant channels with the β1 regulatory subunit in HEK293 cells by transfection. Sodium currents were recorded at different temperatures and different extracellular potassium concentrations using the patch-clamp technique. Functional studies of the E452K variant revealed both loss and gain of function phenotypes at different temperatures, which were characterized by a decrease in current density and an increase in the window current. This was related to the shift of inactivation toward more depolarized voltages at both 22 °C and 10 °C and a slower slope factor of activation at 22 °C. A further gain-of-function effect was also observed, which was characterized by a faster onset and recovery from slow inactivation. MD simulation of the alpha subunit in a lipid bilayer suggested that the charge reversal destabilized a native salt bridge (E452-K249). We concluded that the observed enhanced functionality facilitates the activation process, leading to enhanced muscle excitability.
Similar content being viewed by others
Introduction
Myotonia symptoms were first described in 1876 by Julius Thomsen1, who himself suffered from this muscle manifestation. It was later accurately described as a muscle issue by Adolph Seeligmüller2. Myotonia is now recognized as the hallmark symptom in a group of neuromuscular disorders characterized by impaired muscle relaxation following voluntary contraction, leading to transient stiffness and difficulties in releasing grips or executing movements3,4. The condition arises from irregularities in ion channels, notably sodium and chloride channels, which are crucial for the proper excitability of muscle cells5. Myotonia typically indicates a genetic disorder, which may either be confined to skeletal muscle, as seen in non-dystrophic myotonias, or manifest as part of a multi-systemic condition, such as myotonic dystrophy. Different patterns of muscle involvement are observed across various myotonic disorders, with symptom severity ranging widely. While some individuals may experience mild stiffness, others face more significant challenges with movement and muscle function. One example of a rare genetic non-dystrophic myotonia is paramyotonia congenita (PC). PC is characterized by episodes of muscle stiffness triggered by exposure to cold temperatures or repetitive physical activities. These episodes are typically transient and resolve either by eliminating the triggering factor or as the affected muscles warm up. The primary causative factor for PC is variants in the SCN4A gene, which encodes NaV1.4, the adult skeletal muscle sodium channel6,7. This sodium channel plays a crucial role in regulating the electrical excitability of muscle cells, facilitating the proper balance between muscle contraction and relaxation. Variants in the SCN4A gene disrupt the normal functioning of sodium channels, leading to increased muscle excitability and the characteristic symptoms of PC, including myotonia. Dysfunction in the function of Nav1.4 channels, result in a spectrum of autosomal dominant sodium channelopathies. These disorders include hypokalaemic periodic paralysis (HypoPP), hyperkalaemic periodic paralysis (HyperPP), paramyotonia congenita (PMC), potassium-aggravated myotonia (PAM, also known as sodium channel myotonia), and congenital myasthenic syndrome (CMS)6,8. Although there is no cure for PC, management strategies include medications to alleviate symptoms and enhance muscle function. Physical therapy and lifestyle modifications are often recommended to mitigate the impact of the condition on daily life. Avoiding triggering factors, such as maintaining warmth in cold environments, is crucial. Understanding the role of specific SCN4A variants and their effects on NaV1.4 function are essential for developing targeted therapies for these muscle disorders. In the present study, our aim was to investigate the biophysical properties of a recently reported SCN4A variant (E452K), where the glutamate at position 452 is substituted by a lysine. It was identified in our patient and has been reported in other patients with similar symptoms of myotonia9,10. However, E452K has not been functionally characterized to date. Our patient exhibited a spectrum of muscle-related complications, notably myotonia and PC. This variant is situated proximal to the beginning of the linker region connecting domains I and II in NaV1.4. We overexpressed both the wild-type (hNaV1.4/WT) and mutant (hNaV1.4/E452K) channels, along with the β1 regulatory subunits, in the HEK 293 cell. We recorded sodium currents using the patch-clamp technique. Crucially, our experimental approach also involved scrutinizing sodium currents over a range of temperatures and changes in potassium concentrations, which enabled us to capture potential alterations in channel behavior under varying thermal and hyperkalemia conditions. Additionally, we used molecular dynamics (MD) simulations to investigate the impact of the E452K mutation on the structure of the NaV1.4 channel. By simulating these environmental changes, our aim was to understand how mutation might influence channel function and stability in physiopathologically relevant conditions.
Results
Patient clinical history and identification of the SCN4A variant
The patient, a 36-year-old female, reported that symptoms of her condition began in her mid-20 s. She mentioned experiencing issues with her left scapula as well as recurrent dislocations that were painful but that could be"popped back into place."She also mentioned signs of myotonia in her feet and hands during this time, describing it as a"tight constriction and slow release."Additionally, the patient reported various neurological problems, including a history of PC, seizures, and intractable migraine headaches. She indicated that the symptoms worsened with cold temperatures and stress. She took several medications, including 10 mg of propranolol for headaches, 500 mg of levetiracetam for seizures, 40 mg of citalopram for reactive depression, and 50 mg of dichlorphenamide twice daily for paramyotonia. Myotonia predominantly affects the upper limb muscles and hand grip closure. The patient was fully alert and oriented with normal speech and language. Her cranial nerves were intact, her reflexes are symmetric at 1 +, and her sensation was intact. There was no pronator drift, ataxia, or impairment of coordination. Gait and stride were normal. An EMG revealed discharges on nasal insertion as well as on multiple muscles distal to the right arm, which sometimes appear myotonic but, at other times, exhibit very high-frequency discharges suggestive of paramyotonia. Her baseline motor unit potential was normal.
Family history
The patient’s mother exhibits some evidence of cold intolerance, albeit less significant than the patient. A maternal male first cousin through her maternal uncle has a history of hemophilia, with no children or siblings affected. The patient has two sons, one of whom may have similar symptoms.
Laboratory evaluation
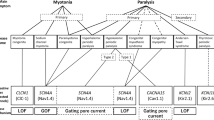
Laboratory evaluations for autoimmune disease were unremarkable. The patient underwent a myotonic dystrophy protein kinase (DMPK) repeat expansion analysis for myotonic dystrophy type 1, which was within normal limits (4 and 13 CTG repeats). In 2016, the patient was tested for PC with a full exome sequencing analysis performed by Greenwood Genetic Center (Greenville, USA), revealed a missense change in the SCN4A gene (NM_000334) (c.1354G > A) and which was classified as a variant of uncertain significance. The c.1354G > A alteration is in the coding exon 9 of the SCN4A gene (Fig. 1A) and the only mutation in the patient’s exome.
Localization of the E452K variant in hNaV1.4. (A) Sanger sequencing of a portion of exon 9 revealed the heterozygous mutation c.1354G > A that causes the E452K substitution. (B) The E452K mutation is in a region that is highly conserved in all voltage-gated sodium channels in humans and other species. (C) Schematic representation of the hNaV1.4 α-subunit highlighting the localization of the E452K mutation on the intracellular loop between domain I and domain II. (D) Side view of the α-subunit illustrating its four domains (I to IV) along with its β1 regulatory subunit. (E) Intracellular view of the channel protein illustrating the open pore cavity in the center, the four domains (I to IV), and the inactivation gate (III-IV linker). (F) A higher resolution view of the I-II linker, pinpointing the position of the glutamate (E) residue.
Location of the substitution and its impact on the overall structure of the Na V 1.4 channel
The glutamic acid residue at position 452 is highly conserved across sodium channels in a variety of vertebrate species, as illustrated in Fig. 1B, suggesting that this residue plays a critical functional role with respect to the structure and activity of sodium channels due to his localization on the DI-DII intracellular loop (Fig. 1C, D, E and F).
Biophysical characteristics of hNa V 1.4/E452K compared to hNa V 1.4/WT
Transfected HEK293 cells were maintained at a holding potential of –140 mV and were subjected to 50-ms pulses ranging from –140 mV to + 65 mV in 5-mV increments. A significant reduction in current density was observed as a result of the E452K substitution (Fig. 2A and B). The time constants of inactivation over voltage of the mutant channel were similar to those of the WT channel (Fig. 2C). The relative conductance (G) was also determined (Fig. 3A). Similar V0.5 values for hNaV1.4/E452K and hNaV1.4/WT were observed, but the slope factor k was higher in hNaV1.4/E452K (Fig. 3A and Table 1). No differences were observed between the different steady state inactivation parameters of hNaV1.4/E452K and hNaV1.4/WT (Fig. 3A and Table 1). The overlap between the activation and inactivation curves of sodium channels, known as the"window current,"delineates a range of membrane potentials where sodium channels are simultaneously activated and not fully inactivated, thus facilitating the entry of sodium ions into the cell. Interestingly, our observations revealed a significant shift of the window current toward more negative potentials accompanied by an increased probability of the window current occurring (Fig. 3B). No significant differences were observed between the time constants of recovery from inactivation of hNaV1.4/WT and hNaV1.4/E452K (Fig. 3C and Table 1).
Analysis of whole-cell sodium currents recorded from HEK 293 cells expressing hNaV1.4/WT or hNaV1.4/E452K. (A) INa from hNaV1.4/WT and hNaV1.4/E452K were obtained using depolarizing pulses ranging from –140 mV to + 65 mV, with 5-mV increments at each step. (B) Current density at –15 mV. The current density of hNaV1.4/E452K decreased by 51% compared to hNaV1.4/WT (**p < 0.01). The current–voltage relationships of hNav1.4/WT (n = 15) and hNaV1.4/E452K (n = 16) were analyzed, with the current amplitude normalized to the membrane capacitance. (C) Voltage-dependence of fast inactivation was assessed by fitting current decays to an exponential function and was plotted against voltage.
Gating properties of hNaV1.4/WT and hNaV1.4/E452K. (A) Voltage-dependence of steady-state activation and inactivation of hNaV1.4/WT (activation, n = 15; inactivation, n = 8) and hNaV1.4/E452K (activation, n = 16; inactivation, n = 9). The activation curves were obtained from I/V relationships, while the inactivation curves were derived using the protocol shown in the insets. The resulting data were fitted to a standard Boltzmann distribution. The slope factor k activation for hNav1.4/E452K was significantly greater than for hNav1.4/WT (**p < 0.01). (B) The predicted window current was obtained using the following equation: (1/(1 + exp ((V0.5activation—V)/k activation)) x ((1—C)/(1 + exp ((V -V0.5inactivation)/kinactivation)) + C) × 100. The open probability was 2.2 times higher in hNav1.4/E452K than in hNav1.4/WT. (C) Time courses of recovery from inactivation in hNaV1.4/WT (n = 7) and hNaV1.4/E452K (n = 8).
Closed-state inactivation refers specifically to the process by which a sodium channel transitions directly from the closed state to the inactivated state, without first opening. The closed-state inactivation of hNaV1.4/E452K at three voltages did not show any significant differences compared to hNaV1.4/WT (Fig. 4A and Table 1).
Gating properties of the slow inactivation. (A) Closed-state inactivation in hNaV1.4/WT (–100 mV, n = 12; –80 mV, n = 7; –60 mV, n = 8) and hNaV1.4/E452K (–100 mV, n = 5; –80 mV, n = 6; –60 mV, n = 6). (B) Recovery from slow inactivation of hNaV1.4/WT (n = 7) and hNaV1.4/E452K (n = 13). (C) Onset of slow inactivation in hNaV1.4/WT (n = 4) and hNaV1.4/E452K (n = 4). All the protocols used to generate the currents are shown in the insets. The slow time constant (τSlow) was faster in hNaV1.4/E452K than in hNaV1.4/WT (*p < 0.05).
Recovery from slow inactivation is described by a two-time constant. Although the slowest time constant was not affected, the faster time constant was faster in hNaV1.4/E452K than in hNaV1.4/WT, suggesting that the slow activation state was destabilized (Fig. 4B). The onset and exit from slow inactivation were also assessed using a double pulse protocol (Fig. 4C). A faster entry to slow inactivation of hNaV1.4/E452K was observed with a slow time constant that was shorter than that of hNaV1.4/WT.
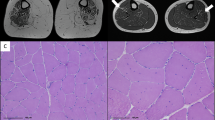
One notable clinical trait observed in patients harboring the E452K variant is the exacerbation of muscle stiffness when exposed to colder temperatures. To investigate this phenomenon, we conducted a comprehensive examination of how cooling impacts the biophysical properties of hNaV1.4/WT and hNaV1.4/E452K. Interestingly, both channels exhibited similar reductions in current density at colder temperatures (15 °C and 10 °C). No differences were observed between hNaV1.4/E452K and hNaV1.4/WT at colder temperatures (Fig. 5 and Table 2).
Temperature influences the biophysical properties of the hNaV1.4. (A) Examples of currents recorded from hNaV1.4/WT and hNaV1.4/E452K at –10 mV at different temperatures (22 °C, 15 °C, and 10 °C). (B, C) Current density at –10 mV. The current density of hNaV1.4E452K decreased by 46% (**p < 0.01) at 15 °C (B) and by 52% (**p < 0.01) at 10 °C (C) compared to hNaV1.4/WT. For comparison purposes, the I/V curves of hNaV1.4/WT and hNaV1.4/E452K at 22 °C are shown in gray. The current amplitude was normalized to membrane capacitance. (D, E) Relationships between the inactivation time constant and voltage. These relationships were obtained by fitting the time constant of current decay to an exponential function and then plotted against voltage.
Myotonia can also be triggered or exacerbated by an increase in potassium concentrations in patients with mutations associated with potassium-aggravated myotonia (PAM), as previously documented11,12,13. We examined the impact of increased extracellular potassium concentration on hNaV1.4/E452K to determine whether the biophysical abnormalities caused by this mutation were also sensitive to extracellular potassium concentrations. Increasing extracellular potassium concentrations from 2 to 9 mM did not alter the gating properties of either hNaV1.4/WT or hNaV1.4/E452K (Supplementary Fig. 1 and Supplementary Table 1) and none of the biophysical parameters (activation, inactivation, and recovery from inactivation) were affected.
Impact of the E452K mutation on the Na V 1.4 channel structure and salt bridge formation
During the past decade, Cryo-EM characterization and the availability of models generated by AlphaFold have afforded new opportunities for understanding the mechanisms that govern or modify ion channel function. Although transmembrane regions have been well described, structural descriptions of cytosolic components are often missing or require improvement. This is particularly true for human NaV1.414. To address this, we constructed all-atom models of human NaV1.4 in a lipid bilayer with explicit salt ions and explicit water. This approach uses individual atoms for all components of the system. We leveraged several notable advancements in the molecular dynamic force field (ff19sb) and paired this with an updated water model (OPC) as recommended for optimal predictive capabilities15. Improvements to computer graphical processors enabled us to perform four independent 1-μs MD simulations of hNaV1.4/WT and hNaV1.4/E452K in feasible timeframes. The NaV1.4 MD simulation predicted that the human channel would contain a salt bridge between K249 and E452 at the bottom of the lipid bilayer (Fig. 6A and B). In all four independent simulations, replacing the negative glutamic acid with a positive lysine increased the distance between the charged atoms of these side chains by an average of 3.0 Å (Fig. 6C). Additionally, the E452K channel model displayed a translocation in segment 6 of domain I. In the WT model, this alpha helical region contained a bend that oriented part of the helix away from the pore. In the E452K model, the bend was absent, and the helix was repositioned closer to the center of the pore (Fig. 6D).
Structural investigation by MD simulation. (A) Alpha subunit of hNaV1.4/WT in a lipid bilayer channel (dark gray), OL (transparent gray), PA (transparent yellow), PC (transparent purple) E452 (blue), and K249 (cyan). (B) Zoomed in region highlighting the E452 and K249 interaction for hNaV1.4/WT. (C) Distances between the charged atoms of the side chains at positions 249 and 452 plotted for each frame of the MD calculation (1-μs simulation with coordinates sampled every 100 ps). Data color-coded hNaV1.4/WT (dark blue) and hNaV1.4/E452K (orange). (D) Overlay of hNaV1.4/WT (grey) and hNaV1.4/E452K (purple) with K249 (cyan for both), WT E452 (blue), and K452 mutation (red).
Discussion
Two studies have implicated the NaV1.4/E452K mutation in the pathogenesis of myotonia9,10. This alteration was documented in two previous reports but was never functionally characterized. The first report described a family presenting with myotonia, episodic weakness, muscle stiffness, and variable muscle hypertrophy9. The second report detailed an individual diagnosed with sodium channel myotonia/PC4. This highlights the clinical relevance of the E452K mutation and its association with neuromuscular disorders and underscores the importance of understanding its structural and functional consequences. However, its biophysical properties and functional consequences remain unexplored. Conservation across different species underscores the evolutionary pressure to maintain this specific residue and highlights its significance in the physiological roles played by sodium channels in excitable tissues such as skeletal muscles. Consequently, the impacts of the E452K mutation on channel kinetics, voltage dependence, and overall muscle excitability have yet to be elucidated. Myotonia can be explained by the hyperexcitability of skeletal muscle induced by altered sodium channel gating properties. These changes in channel dynamics result in prolonged action potential firing.
Surprisingly, while investigating the biophysical properties of hNaV1.4/E452K, we observed a significant reduction in the density of sodium currents recorded from the mutant channel. This unexpected finding suggested that it had a loss-of-function phenotype. The reduced expression levels may be attributed to an alteration in the trafficking and/or the structure of the pore caused by the mutation. In contrast, no effect was observed on the kinetics of current inactivation, which is one of the characteristics of NaV1.4 variants associated with PC6. Additionally, there was no evidence of a persistent sodium current (data not shown), indicating that the mutation does not alter the rate at which inactivation occurs, nor does it result in a sustained sodium current, suggesting that these functional properties of the channel remain unchanged despite the mutation. Notwithstanding the reduced expression levels, further analyses revealed interesting changes in the activation properties of the channels. Specifically, the half-activation voltage (V0.5) values of both hNaV1.4/WT and hNaV1.4/E452K remained unchanged. However, the slope factor of the activation curve was significantly increased in mutant channels. This alteration indicated that there is a change in the voltage sensitivity of activation, while the inactivation parameters remain unaffected. Interestingly, this reduced slope factor of activation resulted in a significant increase in the window current of hNaV1.4/E452K. The window current, which is the overlap of the activation and inactivation curves, was larger in hNaV1.4/E452K. This enlarged window current indicates a gain-of-function phenotype as it implies a higher likelihood of sodium channels being open at subthreshold voltages, potentially leading to enhanced excitability. This is a common feature of myotonic mutations16. Interestingly, the persistence of an increased window current at 10 °C may enhance cellular excitability and potentially contribute to myotonia at lower temperatures. A similar enlargement of the window current has been associated with an epileptic phenotype in the NaV1.2 sodium channel or arrhythmogenic cardiac disease in the Na1.5 sodium channel17,18. This phenomenon underscores the potential for mutations in sodium channels to contribute to neurological and neuromuscular disorders. In summary, while the E452K variant exhibited a loss-of-function phenotype due to a reduced sodium current density, the increase in the slope factor of activation and the subsequent enlargement of the window current indicates a concurrent gain-of-function effect. This dualistic nature of the E452K variant’s biophysical properties highlights its complex impact on sodium channel behavior and suggests potential implications for cellular excitability and related pathophysiological conditions.
We also studied recovery from fast inactivation at −140 mV, consistent with all our protocols. A recovery from inactivation involves the return of sodium channels from an inactive state to a closed state, ready to be activated again, which clearly was not affected by the mutation. This process is highly dependent on the integrity of the channel’s gating mechanisms and the structural domains involved in inactivation and recovery. If the mutation, such as the E to K substitution at position 452, primarily affects other aspects of the function or structure of the channel, such as the formation of a salt bridge in a specific segment (e.g., DI-S6), it might not interfere with the regions and processes directly involved in recovery from inactivation.
The mechanism of closed-state inactivation of sodium channels is crucial for the proper functioning of excitable cells as it contributes to the regulation of excitability and the refractory period, ensuring that the cells do not become overexcited or fail to properly reset during action potential firing. Clearly, this phenomenon was not affected by the E452K substitution.
The onset of slow inactivation was rapid and the recovery from slow inactivation was notably quicker in hNaV1.4/E452K than in hNaV1.4/WT. This accelerated entry into and recovery from slow inactivation may further contribute to the gain-of-function phenotype, potentially enhancing the excitability and responsiveness of the myocytes. These changes in the kinetics of slow inactivation and recovery could play a critical role in the pathophysiology of related myotonia conditions.
As our patient also exhibited cold-induced myotonia as a sign of PC, we investigated the effect of cooling hNaV1.4/E452K even though the kinetics of inactivation were not affected by the mutation to determine whether cooler temperatures could exacerbate the observed phenotypes. To test this hypothesis, we conducted experiments to compare the biophysical properties of hNaV1.4/WT and hNaV1.4/E452K at cooler temperatures. Our analysis revealed that cooling does not exacerbate the phenotypic effects of the mutation. Specifically, the window current, which was observed to be larger in hNaV1.4/E452K at normal temperatures, did not exhibit further enlargement at cooler temperatures, similar window current was observed. This indicated that the gain-of-function effect, which is characterized by an increase in the window current, is not temperature-sensitive in this context. This suggests that the biophysical changes induced by the mutation are resistant to temperature variations, providing valuable insights into the behavior of hNaV1.4/E452K under different environmental conditions. Furthermore, additional experiments are needed to investigate the underlying mechanisms of the cold-induced myotonia observed in the patient.
Although a potassium loading test was not carried out during the diagnosis of the patient carrying the E452K variant, we investigated the effect of elevated extracellular potassium concentrations on channel activity. Our aim was to determine whether the biophysical defects associated with this mutation are also sensitive to changes in extracellular potassium levels. The present study showed that increasing the extracellular potassium concentration from 4 to 6 mM, (data not shown) or 9 mM (Supplementary Fig. 1) does not affect the gating properties of either hNaV1.4/WT or hNaV1.4/E452K. Specifically, none of the biophysical parameters, including activation, inactivation, and recovery from inactivation, were altered by this increase in extracellular potassium. Interestingly, hyperkalemia appears to counteract both the reduction in current density and the increase in window current associated with the variant. This finding suggests that the patient may benefit from a controlled hyperkalemic regimen, as elevated extracellular potassium levels could help restore a more physiological balance of channel activity. Such an approach may offer a potential therapeutic strategy to mitigate the functional impact of the mutation.
Since no exercise test was performed on the patient, we are unable to determine whether a warm-up could alleviate muscle stiffness, a hallmark symptom of PC.
Structural investigation using an MD simulation predicted an increased distance between the side chains of K452 and K249, consistent with destabilization of the native salt bridge (E452-K249). Interestingly our structural studies predicted that the substitution of E with K at position 452 leads to the loss of a crucial salt bridge. This disruption is consistent with the observed elimination of the hockey stick-like structure of segment 6 of domain I, leading to the translocation of the lower half of the helix closer to the channel pore. It is important to note that our model represents a channel in a non-conducting configuration. Further research is needed to understand how the structural aspects of hNaV1.4/E452K might be altered in an open configuration, with voltage sensors and segment 4 of domains I-IV raised out of the lipid membrane. The extent to which these structural changes can be attributed to the observed biophysical alterations merits further investigation. For instance, substituting lysine at position 249 with either a negatively charged or a neutral amino acid could provide insights into the role of the salt bridge between lysine 249 and glutamate 452 in regulating the biophysical properties of the channel. This type of substitution experiment would help clarify the specific contributions of this interaction to the functioning of hNaV1.4/E452K. Such insights will not only deepen our understanding of the molecular basis of this neuromuscular disorder but will also pave the way for the development of targeted therapeutic interventions tailored to mitigate the adverse effects associated with this specific variant on channel dysfunction.
Material and methods
Patient consent
Written informed consent was obtained from the patient in accordance with the ethical guidelines and institutional protocols established by the Greenwood Genetic Center (106 Gregor Mendel Circle, Greenwood, SC, USA). All procedures were conducted in compliance with applicable regulations and ethical standards for human subject research.
Cell cultures
We employed Human Embryonic Kidney 293 (HEK 293) (ATCC, Manassas, Virginia, USA) cells were cultured in high-glucose Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 1% penicillin–streptomycin, and 1% GlutaMAX. The cells were maintained at a standard physiological temperature of 37 °C in a controlled humid environment with 5% CO2. For transfection purposes, HEK 293 cells were seeded onto 35-mm cell culture dishes to facilitate efficient transfection and subsequent experimental analyses. Transfection was carried out using lipofectamine 3000. Specifically, the cells were transfected with the pRc/CMV vector containing wild-type (WT) or mutant NaV1.4 cDNA (1 µg) and the pIRES2/EGFP vector containing the β1 subunit cDNA (1 µg).
Site directed mutagenesis
Mutant human NaV1.4/E452K was generated using Q5® Site-Directed Mutagenesis Kit according to the manufacturer’s instructions (NEB, Whitby, Ontario, CA). Oligonucleotide primers containing the corresponding E452K mutation were designed using NEBase changer (Interactive Tools by NEB) and synthesized by Life Technologies using following sequences:
5′-GGCATATGCCaagCAGAATGAGGCC-3′ (forward primer) and.
5′- ATGGCCACCACGGCCAGG-3′ (reverse primer). The mutated site is underlined.
Mutant and WT NaV1.4 channels were inserted in the pRc/CMV plasmid, amplified in E. coli DH5α, and purified using GenElute™ HP Plasmid Maxiprep Kit (Millipore Sigma, Oakville, Ontario, CAN).
Whole-cell patch-clamp recordings
Whole-cell patch-clamp recordings were performed to measure sodium currents. Low-resistance (1.5–2 MΩ), fire-polished pipettes were pulled from 8161 Corning borosilicate glass and coated with HIPEC (Dow Corning, Midland, MI, USA) to minimize electrode capacitance. Sodium currents were recorded using an Axopatch 200 amplifier in combination with the pCLAMP 11.2 Data Acquisition and Analysis Software Suite (Molecular Devices, Sunnyvale, CA, USA; https://www.moleculardevices.com/products). Series resistance was compensated to 80% to minimize voltage-clamp errors. Following the establishment of the whole-cell configuration, the cells were left to stabilize for 5 min. The membrane potential was held at –140 mV before applying different protocols to record sodium currents. All protocols are shown in respective figures. Cells were subjected to 50-ms pulses ranging from –140 mV to + 65 mV in 5-mV increments. The peak current amplitudes generated were normalized to cell capacitance and were plotted versus voltage to construct I/V curves. For the relative conductance (G), it was determined using the formula: G = INa/(V – ENa), where INa is the current, ENa is the Na+ ion reversal potential, and V is the applied voltage. The conductance then was normalized to the maximum conductance measured at + 20 mV (Gmax) and was plotted versus voltage. The data were fitted to a Boltzmann function [G/Gmax = (1 + exp(V – V0.5)/k)] to determine the midpoint (V0.5) and slope factor (k). To study steady-state inactivation, 500-ms prepulses to voltages ranging from –140 mV to –30 mV, were applied before eliciting sodium currents using a standard test pulse (–10 mV/10 ms). The peak test currents (I) were normalized to the current (Io) measured from a negative holding potential (–140 mV/500 ms) and were plotted versus the pre-pulse voltage. The V0.5 and slope factors were determined by fitting the data to a Boltzmann function (1 – C)/{1 + exp [(V – V0.5)/k] + C}. A two-pulse protocol was used to assess the recovery time from inactivation. The channels were fully inactivated during the first pre-pulse by depolarizing them to –10 mV for 500 ms and then returning them to –140 mV for variable durations (1–5000 ms) before applying a second standard test pulse (–10 mV/20 ms) to assess the fractional current that recovers from inactivation. The fractional recoveries were then plotted versus the recovery interval, and the data were fitted with exponential functions to determine the recovery time constants. The window current was obtained using Eq. 1: {1/[1 + exp ((V0.5activation– V)/kactivation)] x [(1—C)/(1 + exp (V – V0.5inactivation)/kinactivation)] + C} × 100, which is the probability of having the channel in the open state. The open probability refers to the higth of the window current. For entry to slow inactivation pre-pulse potentials ranging from –140 mV to –10 mV were applied for variable times, and the resulting current was monitored using a 40-ms pulse and was plotted over time. No P/4 leak subtraction was used, we rather used the amplifier’s built-in leak subtraction. Experiments were conducted at either room temperature (22 °C) or at colder temperatures (15 °C and 10 °C) to assess any changes in sodium channel behavior at these temperatures. Temperature changes were performed using a bipolar temperature controller (Model TC-202, Medical Systems Corp., Greenvale, NY, USA) and were monitored near the cells using a bath sensor (Thermistor BSC-T3, Harvard Apparatus, Holliston, MA, USA).
Solutions
For the patch clamp recordings, the external solution consisted of 150 mM NaCl, 2 mM KCl, 1.5 mM CaCl2, 1 mM MgCl2, 10 mM glucose, and 10 mM HEPES. The pH was adjusted to 7.4 using 2 M HCl. For the high extracellular potassium solution, the concentration of NaCl decreased to 143 mM while the concentration of KCl increased to 9 mM. The patch pipette solution consisted of 35 mM NaCl, 105 mM CsF, 10 mM EGTA, and 10 mM HEPES. The pH was adjusted to 7.3 using 2 M CsOH.
Molecular dynamics simulation of the human Na V 1.4 channel in a lipid bilayer
A starting model of the human voltage-gated sodium channel type 4 alpha subunit (NaV1.4) was obtained from AlphaFold (P35499). The CHARMM-GUI Bilayer Builder was used to construct a lipid bilayer and the solvent ion box. The pH was set at 7.4 and potential disulfide bonds (identified in Chimera) were specified. The channel was oriented for a lipid bilayer (PPM 2.0). The bilayer was specified as heterogenous (POPC with a 1:1 ratio) with a rectangular water box (22.5 Å thick, X and Y lengths initially set at 200 Å). The system was built using the replacement method, and 0.145 M NaCl was applied with charge neutralization. An amber force field (ff19sb) with an explicit OPC water model was used. Equilibration was set to generate information for PME FFT automatically, NPT ensemble, temp = 300 K. The models were minimized and were equilibrated using Amber 23 and 100 ns of MD simulation (Amber 23). This was followed by H + + calculations to ascertain the status of amino acid protonation. A second round of CHARMM-GUI calculations was used to optimize the solvent box size. The resulting model was again minimized, and four independent equilibrations and 1000 ns of MD simulation were performed. Amber simulations were calculated with a step size of 0.004 ps employing SHAKE and hydrogen mass repartitioning. Coordinates were written every 100 ps. The resulting data files were analyzed using Amber tools 23 (cpptraj), ChimeraX, VMD, and gnuplot. Figures were constructed using ChimeraX, Excel, and Prism Graphpad. The experimental protocols have been approved by Laval University Ethic committee.
Statistical analysis
The results are expressed as means ± S.E.M. Statistical analyses were performed using the Mann–Whitney test in GraphPad Prism (GraphPad Software, Boston, MA, USA). Significance was determined at a threshold of p < 0.05.
Data availability
The sequence used in this study can be obtained at https://www.ncbi.nlm.nih.gov/nuccore/M81758.1. The raw data supporting the conclusions of this study will be made available by the corresponding author, without undue reservation.
References:
Thomsen, J. Tonische Krämfe in willkürlich beweglichen Musklen in Forge Von ererber psychischer Disposition. Arch. Psychiat. Nerukrankh. 6, 702 (1876).
Seeligmüller, A. Die Myotonie (Myotonia congenita). Dtsch. Z. Nervenheilkd. 9, 1–30 (1886).
Trivedi, J. R., Cannon, S. C. & Griggs, R. C. Nondystrophic myotonia: challenges and future directions. Exp. Neurol. 253, 28–30. https://doi.org/10.1016/j.expneurol.2013.12.005 (2014).
Stunnenberg, B. C. et al. Guidelines on clinical presentation and management of nondystrophic myotonias. Muscle Nerve. 62, 430–444. https://doi.org/10.1002/mus.26887 (2020).
Cannon, S. C. Channelopathies of skeletal muscle excitability. Compr. Physiol. 5, 761–790. https://doi.org/10.1002/cphy.c140062 (2015).
Chahine, M. et al. Sodium channel mutations in paramyotonia congenita uncouple inactivation from activation. Neuron 12, 281–294 (1994).
Chahine, M., Bennett, P. B., Horn, R. & George, A. L. Functional expression of the human skeletal muscle sodium channel. Biophys. J. 64, A4 (1993).
Jurkat-Rott, K., Holzherr, B., Fauler, M. & Lehmann-Horn, F. Sodium channelopathies of skeletal muscle result from gain or loss of function. Pflugers Arch. 460, 239–248. https://doi.org/10.1007/s00424-010-0814-4 (2010).
Dupré, N. et al. Clinical, electrophysiologic, and genetic study of non-dystrophic myotonia in French-Canadians. Neuromuscul Disord. 19, 330–334. https://doi.org/10.1016/j.nmd.2008.01.007 (2009).
Stunnenberg, B. C. et al. Prevalence and mutation spectrum of skeletal muscle channelopathies in the Netherlands. Neuromuscul. Disord. 28, 402–407. https://doi.org/10.1016/j.nmd.2018.03.006 (2018).
Heine, R., Pika, U. & Lehmann-Horn, F. A novel SCN4A mutation causing myotonia aggravated by cold and potassium. Hum. Mol. Genet. 2, 1349–1353 (1993).
Ricker, K., Moxley, R. T. III., Heine, R. & Lehmann-Horn, F. Myotonia fluctuans. A third type of muscle sodium channel disease. Arch. Neurol. 51, 1095–1102 (1994).
Kubota, T. et al. New mutation of the Na channel in the severe form of potassium-aggravated myotonia. Muscle Nerve. 39, 666–673. https://doi.org/10.1002/mus.21155 (2009).
Pan, X. et al. Structure of the human voltage-gated sodium channel Na(v)14 in complex with β1. Science https://doi.org/10.1126/science.aau2486 (2018).
Tian, C. et al. ff19SB: Amino-acid-specific protein backbone parameters trained against quantum mechanics energy surfaces in solution. J. Chem. Theory Comput. 16, 528–552. https://doi.org/10.1021/acs.jctc.9b00591 (2020).
Farinato, A. et al. Pharmacogenetics of myotonic hNav1.4 sodium channel variants situated near the fast inactivation gate. Pharmacol. Res. 141, 224–235. https://doi.org/10.1016/j.phrs.2019.01.004 (2019).
Huang, H., Priori, S. G., Napolitano, C., O’Leary, M. E. & Chahine, M. Y1767C, a novel SCN5A mutation, induces a persistent Na+ current and potentiates ranolazine inhibition of Nav1.5 channels. Am. J. Physiol. Heart Circ. Physiol. 300, H288-299. https://doi.org/10.1152/ajpheart.00539.2010 (2011).
Plumereau, Q. et al. Novel G1481V and Q1491H SCN5A mutations linked to long QT syndrome destabilize the Nav1.5 inactivation state. CJC Open 3, 256–266. https://doi.org/10.1016/j.cjco.2020.09.023 (2021).
Acknowledgements
The authors would like to express their gratitude to the Greenwood Genetic Center – Greenville Office, for their invaluable assistance in genotyping and for providing access to the clinical data
Funding
This work was supported by two Canadian Institutes of Health Research grants (MOP-111072 and MOP-130373) to M.C.
Author information
Authors and Affiliations
Contributions
Q.P.: Acquisition, analysis, and interpretation of data, and drafting the article. S.L.: Acquisition and analysis of data. C.H.N.: Acquisition and analysis of data. M.C.: Funding acquisition, conceptualization, methodology, validation, writing, reviewing, and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Plumereau, Q., Lile, S., Johnson, C.N. et al. Biophysical and structural insights into the SCN4A E452K variant linked to myotonia and paramyotonia congenita. Sci Rep 15, 33101 (2025). https://doi.org/10.1038/s41598-025-17816-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17816-2