Abstract
Over the past decade, Taiwan has seen rising rates of overweight and obesity across all age groups. In a large cross-sectional analysis involving 27,473 adults from the MJ Health Research Foundation, we examined how sleep duration and dietary patterns, stratified by age, relate to obesity and excess adiposity. Participants completed the MJ Health Questionnaire, blood tests, and anthropometric assessments. Four dietary patterns emerged via factor analysis: vegetables and fruits, processed/ultra-processed foods, protein-based, and dairy–complex carbohydrates. Chi-square and t-tests evaluated baseline differences, and multivariable logistic regression modeled the relationships among sleep, diet, and obesity. Short sleep duration was linked to 21% greater odds of obesity than adequate sleep (OR 1.21; 95% CI, 1.15–1.29). The processed/ultra-processed (OR 1.24; 95% CI, 1.16–1.33) and protein-based patterns (OR 1.52; 95% CI, 1.42–1.64) were associated with higher odds of obesity and excess body fat, while the dairy–complex carbohydrate pattern was protective (OR 0.81; 95% CI, 0.76–0.87). Notably, younger adults with insufficient sleep exhibited increased odds of obesity than older adults. These findings underscore inadequate sleep amplifies odds of obesity across dietary patterns and age modifies these interrelationships, highlighting the need for age‑tailored, integrative lifestyle interventions.
Similar content being viewed by others
Introduction
Obesity has become an increasing global public health concern. Several countries worldwide have witnessed a double or triple prevalence rate of obesity in the last three decades, probably due to westernization, sedentary lifestyle, and increasing consumption of high-calorie, high-fat processed foods1,2,3. Health Promotion Administration statistics indicate that roughly 23% of Taiwanese adults are classified as obese, corresponding to nearly one in four individuals4. Obesity arises from a dynamic interplay among genetic predispositions, biological mechanisms, environmental influences, and behavioral choices5. While genes contribute to 40–70% of interindividual differences—impacting metabolism, appetite regulation, hormonal signaling (e.g., leptin, ghrelin), fat storage, and gut microbiota—genetic susceptibility alone does not account for the rapid global rise in obesity6. Instead, it is the convergence of this biological susceptibility with an obesogenic environment characterized by sedentary lifestyles, widespread access to calorie-dense ultra‑processed foods, chronic stress, insufficient sleep, and socioeconomic disparities that drives the epidemic5.
Habitual consumption of calorie- and fat-rich foods is a significant contributor to metabolic syndrome, type 2 diabetes, insulin resistance, and obesity7. Prior studies have demonstrated that inadequate sleep quality and duration contribute causally to adverse metabolic outcomes, primarily through circadian disruption and enhanced fat deposition8,9. The National Sleep Foundation advises that young and middle-aged adults obtain 7 to 9 h of sleep per night, while older adults are recommended to sleep between 7 and 8 h10. Notably, approximately half of Americans indicate sleeping 7 to 9 h per night, whereas 15% report obtaining less than 7 h of sleep on weekday nights11. In Taiwan, a nationwide, walk-in survey on sleep quality revealed a high prevalence of poor sleep, particularly among Taiwanese residents in the northern area12. Sleep duration was derived based on participants’ answers to the following self-administered question: “During the past month, how many hours of actual sleep did you get at night?”12. Participants with poor sleep quality reported an average of 5.5 h of sleep per night, which was notably shorter than the 6.8 h reported by those with good sleep quality12. Insufficient and poor-quality sleep have been correlated with decreased dietary fiber intake alongside elevated consumption of carbohydrates, sugars, cholesterol, and saturated fats. This imbalance can result in excess calorie intake and disrupt the body’s energy balance13. Long-term energy imbalance can lead to overweight and obesity.
Numerous well-designed investigations on the relationship between eating behaviors and obesity or overweight have been documented in the literature13,14,15. While the dietary patterns in individual studies were characterized using varying statistical approaches (i.e. principal component analysis, factor analysis), studies concluded a prudent dietary pattern (a diet rich in fruit, vegetables, lean meat, fish and unprocessed grains) may decrease overweight/obesity risk, while a western dietary pattern (a diet rich in processed foods and foods high in sugars and fats) may increase overweight/obesity risk14,15.
Age may modify the association between sleep duration and overweight/obesity. Prior research has indicated that the impact of sleep duration on obesity risk may differ by age group3,16. The association between sleep and age follows a nonlinear pattern, implying that its characteristics and consequences may differ notably across various life stages3. For instance, sleep needs are higher in children and adolescents than in both young and older adults16. Previous research also found a weakened relationship between sleep and weight with aging17. Insufficient sleep duration, especially in younger individuals, is strongly linked to increased dietary intake, hormone imbalances, and a higher risk of obesity, with these effects diminishing or becoming more complex with age and influenced by both dietary patterns and circadian factors13. This investigation seeks to address: (1) how sleep duration relates to obesity, (2) how dietary patterns contribute to obesity, and (3) whether such associations differ across age groups.
Methods
Data source
The present cross-sectional analysis draws on information gathered from 2001–2015 from the Mei Jau (MJ) International Health Management Institution in Taiwan. The MJ International Health Management Institution operates as an autonomous entity specializing in health screening and management within Taiwan, encompassing a network of 8 screening centers in Asia, including 4 located in key urban cities in Taiwan (Kaohsiung, Taichung, Taoyuan and Taipei). The MJ Health Screening Database consists of three integrated components: a comprehensive questionnaire database, a detailed biomedical data repository, and an extensive biobank. At each screening visit, participants complete a self-administered health questionnaire, undergo blood testing, and have key anthropometric measurements recorded. The MJ Health Questionnaire obtains information on demographics, medical history, dietary behaviors, lifestyle factors, and physical activity patterns. Subsequently, participants were asked to complete a written consent form allowing MJ International Health Management Institution to collect personal data solely for the use of research purpose. The study population consisted of 27,473 individuals aged 18 years or over—11,891 men and 15,582 women.
Ethical consideration
Ethical approval for this research was obtained from the Joint Institutional Review Board of Taipei Medical University (TMU-JIRB No.: N202010035). All procedures were performed in compliance with the principles of the Declaration of Helsinki and pertinent regulatory guidelines. Participation was voluntary, and all individuals gave written informed consent, permitting the use of their de-identified data for academic research.
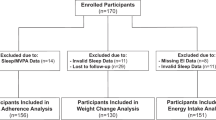
Participants
This study enrolled participants aged eighteen and above and excluded those with the following conditions: 1)Taking psychiatric medications; 2) pregnant women; 3)cancer patients; 4) missing data.
Sleep duration assessment
Participants’ sleep duration assessment was based on self-reported sleep hours. For example, “How long do you sleep every day?” with response options include: < 4, 4–6, 6–7, 7–8, ≥ 9 h. Sleep duration was classified into inadequate (< 7 h/day) and adequate (≥ 7 h/day) The classification of sleep duration was based on findings from previous literature18,19.
Definitions on overweight and obesity
Definitions of overweight and obesity follows the Ministry of Health and Welfare in Taiwan’s recommendation (BMI of 24 kg/m² ≤ BMI < 27 kg/m² for overweight and BMI ≥ 27 kg/m² for obesity), rather than the higher thresholds recommended by the WHO (25 ≤ BMI < 29.9 kg/m² for overweight and BMI ≥ 30 kg/m² for obesity)20,21,22,23.
Definition on excessive body fat
Body fat percentage can be measured by the following methods, including skinfold thickness, bioelectric impedance (BIA), underwater weighing (Densitometry or Hydrostatic Weighing), Dual Energy X-ray Absorptiometry (DEXA), and computerized tomography (CT) and Magnetic Resonance Imaging (MRI)24. For non-Asian populations, obesity is defined as body fat exceeding 30% in men and 40% in women25,26. Taiwan adopts stricter criteria, classifying men with body fat >25% and women with body fat > 30% as obese27,28.
Dietary patterns
Participants provided dietary information by reporting how often they consumed specified portion sizes of each item in the preceding month, expressed in daily or weekly servings. The serving size of the food item consumed was clearly defined for each question. For instance, participants reported vegetable intake (light- and dark-colored, oil/dressing-prepared, root crops) using five categories: < 0.5, 0.5–1, 1–1.5, 1.5–2 and 2 bowls/day (1 bowl = 11 cm in diameter). Fruit and rice/flour consumption was recorded as < 1, 1–2, 2–3, 3–4 and ≥ 4 servings/day (1 serving = 1 medium-sized apple, 1 bowl of rice, 2 bowls of noodles). For milk, the categories were: none or < 1, 1–3, 4–6, 1 and ≥ 2 glasses/day (1 glass = 240 mL). For all remaining food items, the responses consisted of: < 1, 1–3, 4–6 servings/week, 1 and ≥ 2 servings/day28.
Other baseline variables
Participants reporting daily, occasional, or intermittent smoking were classified as current smokers, while all others were considered as non-smokers. Alcohol consumption of ≥ 1–2 times per week was defined as current drinkers, while lower intake or abstinence was defined as non-drinkers. Physical activity was classified into two groups: active (≥ 150 minutes per week) or inactive (< 150 minutes per week). BMI was categorized as underweight (< 18.5 kg/m²), normal weight (18.5 to 23.9 kg/m²), and overweight (24 to 26.9 kg/m²). A sex-specific criterion was applied to define central obesity: waist circumference > 90 cm for males and > 80 cm for females. Educational level was divided into two groups: below college and college or above.
Blood Collection and Laboratory Assessments
Serum analyses were conducted at the central laboratory of the MJ Health Management Institution.Prior to testing, participants were required to undergo an overnight fast of 12–14 h. Levels of total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), triglycerides (TG), fasting plasma glucose (FPG), C-reactive protein (CRP), alanine aminotransferase (ALT), and aspartate aminotransferase (AST) were determined using validated commercial assays. LDL-C concentration was estimated by the Friedewald formula28.
Statistical analysis
Factor analysis was employed to derive dietary patterns, retaining factors based on the Kaiser criterion with orthogonal rotation. Food items with factor loadings < 0.20 were excluded. In cases where an item had absolute loadings > 0.20 across multiple patterns, it was assigned to the pattern with the higher value. Four factors were extracted and labeled based on the interpretation of the observed data. Factor scores for each dietary pattern were obtained from the weighted sum of food intakes based on factor loadings. Participants were then categorized into tertiles within each pattern, reflecting low, moderate, and high consumption. Categorical data are reported as number or percentage, and continuous data as mean ± SD. Chi-square tests were used to evaluate categorical differences, while t-tests were applied for continuous variables across dietary pattern tertiles. The relationships of sleep duration and dietary patterns with obesity and excess body fat were investigated through multivariable logistic regression. Stratified analyses by age group were performed to evaluate effect modification. Baseline covariates for adjustment included sport, smoking, drinking, gender, age, education, TG, TC, HDL, and LDL. All statistical analyses were performed with STATA version 16MP. All p-values were two-tailed, with statistical significance set at p < 0.05.
Results
Baseline Characteristics of Study Population
The characteristics of study population are summarized in Tables 1 and 2. Among the 27,473 participants, there were 15,455 participants (56%) without obesity (BMI < 27) and 12,018 participants (44%) with obesity (BMI ≥ 27). Among the participants with obesity, the majority were females (52.98%), between age 31–40 (32.33%), non-smokers (82.69%), doing exercise (54.17%), drinking less than once/week (87.17%), having sleep time ≥ 7 h (73.08%), having excessive body fat (94.77%), and education below college (63.47%). In terms of blood lipids, people with obesity (BMI ≥ 27) had a significantly higher HDL and LDL levels compared to those without obesity (BMI < 27). The individuals with excessive body fat had significantly higher TC, HDL, and LDL levels compared to those with normal body fat.
Additionally, among participants with excessive body fat, the majority were females (87.76%), aged between 41 and 60 (52.29%), non-smokers (87.76%), doing exercise (55.40%), drinking less than once/week (89.31%), having sleep duration ≥ 7 h (72.81%), BMI ≥ 27 (52.26%), and education below college (72.07%).
When cross-comparing BMI with excess body fat, 94.77% of individuals from the BMI ≥ 27 group carry excessive body fat. Conversely, among the group with excessive body fat, 52.26% of participants have a BMI ≥ 27.
Dietary patterns
Factor analysis (FA) yielded four dietary patterns, as shown in Table 3. Dietary Pattern I, the “Vegetable & fruit diet”, accounted for 30.76% of the variance and comprised four food items: vegetables cooked with oil, light-colored vegetables, dark-colored vegetables, and fruit. Dietary Pattern II, labeled the “Processed and Ultra-processed Food Diet,” accounted for 28.85% of the variance and included nine food groups: organ meats, oil-cooked rice/flour, rice/flour products, jam/honey, sugar-sweetened beverages, processed foods, deep-fried foods, instant noodles, and assorted sauces. Dietary Pattern III, referred to as the “Protein-based diet”, accounted for 24.71% of the variance and included four food items: pork or beef steak, eggs (e.g., quail eggs, duck eggs, chicken eggs, etc.), seafood, and bean products. Dietary Pattern IV, the “Dairy-Complex Carbohydrate diet”, explained 15.68% of the variance and comprised five food items: whole grains, milk, root crops, dairy products (e.g., yogurt, cheese) and bread.
Logistic regression analysis of sleep duration and dietary patterns associated with obesity
Table 4 shows participants with inadequate sleep duration (< 7 h/day) had significantly greater odds of obesity (OR: 1.21, 95% CI: 1.15–1.29) and excessive body fat (OR: 1.36, 95%CI: 1.25–1.49) compared to those havin ≥ 7 h of sleep. No significant link was observed between the “Vegetables-Fruit” dietary pattern and obesity or body fat. In contrast, high adherence to the “Processed Food” dietary pattern increased the risk of obesity (OR:1.24, 95% CI: 1.16–1.33) and excessive body fat (OR: 1.18, 95% CI: 1.07–1.31). The “Protein-Based” dietary pattern showed similar associations with higher risks of obesity (OR = 1.52, 95% CI 1.42–1.64) and excess body fat (OR: 1.62, 95% CI: 1.45–1.81). Conversely, the “Dairy-Complex Carbohydrate” dietary pattern conferred protective effects, lowering the risk of obesity (OR: 0.81, 95% CI: 0.76–0.87) and excess body fat (OR: 0.87, 95% CI: 0.79–0.96).
Subgroup analyses
Association between sleep duration, obesity and excessive body fat stratified by dietary pattern
Table 5 summarizes the stratified associations of sleep duration with obesity and excessive body fat across different dietary patterns. Our results showed regardless of dietary pattern, participants with sleep duration < 7 h were at increased odds of obesity, and the odds further increased across the tertiles. Among participants sleeping fewer than 7 h, those in the highest tertile of the dairy–complex carbohydrate dietary pattern exhibited the greatest likelihood of obesity (OR: 1.31, 95% CI: 1.18–1.46), followed by the vegetable–fruit pattern (OR: 1.25, 95% CI: 1.13–1.39), the processed and ultra-processed food pattern (OR: 1.25, 95% CI: 1.13–1.38), and the protein-based pattern (OR: 1.23, 95% CI: 1.11–1.37). Likewise, participants with sleep duration less than 7 h were at increased odds for having excessive body fat regardless of dietary pattern, and the risk further increased across the tertiles. When sleep time was less than 7 h, participants from the highest tertile of vegetable–fruit pattern had the highest odds of obesity (OR:1.60, 95%CI: 1.35–1.90), followed by dairy-complex carbohydrate dietary pattern (OR:1.49, 95% CI: 1.27–1.77), processed and ultra-processed food pattern (OR:1.43, 95% CI: 1.24–1.64), and protein-based pattern (OR: 1.41, 95% CI: 1.23–1.61).
Association between sleep duration, obesity and excessive body fat stratified by age
The link of sleep duration with obesity and excess body fat seems to vary by age. Our study results (Table 6) indicated that prior to age 51, age moderated the relationship between sleep duration, obesity, and excessive body fat. Participants from the age group 18–30 had significantly higher odds (OR = 1.58; 95% CI = 1.27–1.97) of being obese and having excessive body fat (OR = 1.40; 95% CI = 1.13–1.75) compared to those from the age group of 31–40 (OR = 1.36; 95% CI = 1.28-1.66) and age group of 41–50 (OR = 1.23; 95% CI = 1.05–1.44). No significant relationship between sleep duration, obesity, and excess body fat was observed among participants aged over 50 years.
Discussion
The study analyzed the associations of sleep duration and dietary patterns with obesity, with particular attention to effect modification by dietary practices and age. Sleeping fewer than 7 h per day was significantly linked to increased odds of obesity. Additionally, younger participants with inadequate sleep duration were at significantly greater odds of obesity and having excessive body fat compared to older participants; however, such significant risk diminishes at age over 50. Moreover, our study showed there was no association between vegetable-fruit pattern with obesity. The processed and ultra-processed food pattern and protein-based patterns were obesogenic, being associated with greater risks of obesity and excess body fat, whereas the dairy–complex carbohydrate pattern exhibited a protective relationship. Participants with insufficient sleep duration had increased odds of obesity regardless of dietary pattern.
The interconnection among inadequate sleep duration, dietary intake, and obesity is multifaceted and complex because these factors influence each other through various physiological, behavioral, and environmental mechanisms29,30. Our study shows that insufficient sleep duration will amplify the odds of obesity and having excessive body fat. Sleep duration has been shown to influence metabolic hormones and body weight. Sleep affects the levels of two important hormones in our body – leptin and ghrelin. A reduction in leptin levels coupled with an elevation in ghrelin associated with insufficient sleep duration may stimulate orexin activity, ultimately promoting increased caloric intake21,31. Allied with our study findings, Watanabe et al. found in a Japanese population study that sleeping < 7 h/day was significantly associated with higher BMI, relative to 7–8 h/day32. Consistently, another investigation of 740 adults aged 21–64 years reported that individuals sleeping 7–8 h exhibited lower fat accumulation and a reduced prevalence of obesity relative to those with only 5–6 h of sleep33. Current evidence speculates that multiple pathways may underlie the association between obesity and sleep duration: (1) Disrupted signaling of appetite and satiety hormone; (2) Suppressed metabolic activity leading to decreased energy expenditure; and (3) abnormal glucose metabolism34. In the face of altered appetite/satiety regulation hormones, even participants from the healthy dietary pattern may not have reduced odds of obesity and excessive body fat. The evidence consistently demonstrates that obesity is not driven by one factor alone: genetic predisposition interacts with diet, physical activity, sleep, socioeconomic environment, and behavioral traits (like appetite), manifesting complex gene–environment–behavior interplays35,36. Experimental studies indicated short sleep duration may increase circulating ghrelin level and decrease leptin level, a hormonal pattern that is consistent with increased appetite and decreased energy expenditure prompting obesity35. From a behavioral perspective, prolonged awake time increases the likelihood of individual consuming additional food and beverages, and as a result leading to weight gain36.
Poor eating behaviors and food choices have been linked to weight gain and obesity37. Evidence indicates that diets rich in whole, unprocessed foods and low in calorie-dense items help reduce energy intake and prevent obesity38. Longitudinal data from Chinese adults demonstrated protective effects of diets abundant in vegetables, fruits, whole grains, and fish against obesity, whereas patterns characterized by ultra-processed foods, sugar, and convenience items are obesogenic39. Consistent with earlier studies, we observed that the processed and ultra-processed food pattern and protein-based patterns were associated with greater risks of obesity and excessive body fat. Processed foods typically rich in salt, sugar, and unhealthy fats40, and excessive consumption of these nutrients is regarded as a major contributor to the increased risk of obesity41. However, no significant link was found between the vegetable–fruit dietary pattern and obesity. This finding may be attributable to the traditional Taiwanese practice of preparing vegetables with cooking oil (e.g., stir-frying or sautéing), which increases total caloric intake. For obesity prevention, the dairy–complex carbohydrate dietary pattern appeared protective, showing lower risks of obesity and excess body fat. This finding is consistent with prior research. Observational research have shown that both dairy consumption and Mediterranean diet (MD) may have a protective effect against obesity4344.
Interestingly, our study suggests that insufficient sleep duration will increase the odds of obesity and having excessive body fat regardless of dietary pattern. Sleep deprivation can cause behavioral changes in food cravings. In younger individuals, sleep loss can often cause junk food cravings, particularly nighttime snacking44.
Current evidence indicates that sleep deprivation markedly reduces activity in brain regions involved in appetite regulation, thereby promoting greater food consumption, particularly of calorie-dense foods46,47. Reduced sleep duration, resulting in more awake time for food intake, also contributes to weight gain and obesity48. On the other hand, alterations in energy expenditure may represent another mechanism linking short sleep duration with obesity. For instance, insufficient sleep duration can cause fatigue and thus reduce one’s ability to engage in physical activity49. One study concluded insufficient sleep duration was associated with increased sedentary activities such as screen time use among middle-aged adults50. In summary, short sleep disrupts hormonal regulation of appetite, promotes cravings for high-calorie foods, and impairs decision-making around eating behaviors, all of which can lead to increased energy intake42,43. Simultaneously, insufficient sleep reduces physical activity and metabolic efficiency, further tipping the energy balance toward weight gain. These interrelated pathways underscore the critical role of sleep in shaping dietary habits and long-term obesity risk34,35,36,50.
Sleep duration in this study was measured with a single self-reported item. This approach was also being used in the Behavioral Risk Factor Surveillance System (BRFSS), where a single-item sleep question “On average, how many hours of sleep do you get in a 24‑h period?”51. This approach had been validated in a subsample of 300 community-dwelling adults against objective measures such as actigraphy and in-home sleep studies51. Self-reported sleep duration, though overestimated by 0.72–1.13 h/day, is still commonly used in observational research because it is inexpensive and easy to administer52. By contrast, more standardized procedures to access sleep duration are accelerometry and sleep diary52. Accelerometry is considered the standard approach for measuring sleep in free-living environments 53. The downside of this approach is accelerometry tends to overestimate sleep duration53. A sleep diary demonstrates greater validity than a questionnaire, as it is completed daily and more accurately captures variations in respondents’ sleep54. Nevertheless, reliance on sleep diaries can create notable respondent burden and generated systematic bias, as recorded onset and wake times often diverged from actual sleep behavior52. Therefore, despite concerns regarding their validity, self-reported questionnaires continue to be a practical approach for assessing sleep duration.
In age-stratified subgroup analyses, insufficient sleep duration was linked to greater odds of obesity among participants aged 18–50, whereas this association was attenuated in those age > 50 years. Our results are consistent with a cross-sectional analysis of the NHANES 2015–2016 data, which found no association between sleep duration and obesity in older American adults50. A plausible explanation is that aging, a natural biological process, involves progressive declines in sensory and oral functions—such as vision, taste, smell, chewing, and swallowing—that shape habitual dietary intake of energy and macronutrients in later life55. Furthermore, for older adults, the likelihood of having chronic diseases and complications may promote chronic inflammation, resulting in decreased dietary consumption and body weight56,57. Evidence from a study of Chinese adults aged ≥ 60 indicated that increasing age correlated positively with healthier dietary patterns, characterized by higher vegetable and fruit intake and lower reliance on highly processed foods. This pattern was attributed to increasing health awareness with age and strategies to manage chronic diseases. In summary, our finding illustrates the importance of adequate sleep duration in obesity prevention among the younger adult population (aged 18–50 years).
There are several strengths of this study. First, the substantial sample size (n = 27,473) enabled comprehensive adjustment for potential confounding factors. Second, our study is distinctive in being among the limited number of investigations that link sleep duration to obesity, extending the analysis to include body fat percentage and dietary patterns. The findings hold significant scientific value and contribute to the relatively limited literature exploring the relationships among sleep duration, dietary patterns, and obesity. Nonetheless, this study has limitations. First, sleep duration was self-reported, making recall bias unavoidable. Individuals with short sleep durations tended to overestimate their sleep time compared to those who slept longer, potentially leading to misclassification of sleep duration. Second, the cross-sectional design prevents causal inference regarding the relationship between sleep duration and obesity-related indicators. Third, although several confounders were controlled for, unmeasured or residual confounding may remain. Sleep disorders—including insomnia, sleep apnea, narcolepsy, and restless legs syndrome—could influence both sleep duration and obesity58. Moreover, total energy intake should be considered as a covariate in the analysis of sleep duration and obesity/adiposity. However, because the dietary assessment used in this study was qualitative (capturing only food frequency rather than actual caloric intake), it was not possible to accurately estimate participants’ average energy consumption.
Conclusion
Short sleep was related to greater risks of obesity and excess body fat. Processed and ultra-processed food pattern and protein-based pattern increased these risks, whereas the dairy–complex carbohydrate dietary pattern reduced them. Participants with inadequate sleep duration were at increased odds of obesity and excessive body fat regardless of dietary pattern. Finally, inadequate sleep markedly increased the odds of obesity and excess body fat among younger participants, but this association attenuated in those over age 50.
Data availability
“The datasets analyzed during the current study are not publicly available due Mei Jau (MJ) Health Management Institute policy. Data are available from the author upon reasonable request and with permission of Mei Jau (MJ) Management Institute. Please contact the first author, Li-Yin Lin, to request access to the datasets used in this study.
References
Lin, X., & Li, H. Obesity: epidemiology, pathophysiology, and therapeutics. Front. Endocrinol. (Lausanne). 12:706978. (2021).
Yoo, S. Dynamic energy balance and obesity prevention. J. Of Obes & Metab Syndr. 27(4): 203-12. (2018).
Grandner, M., A., Jackson, N., Gerstner, J. R., & Knutson, K. L,. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite. 64:71-80. (2013).
Administration, H. P. Ministry of Health and Welfare. Nutrition and Health Survey in Taiwan (NAHSIT). 2017–2020. Accessed on July 1. (2025). https://www.hpa.gov.tw/Pages/List.aspx?nodeid=3998.
Llewellyn, C. & Wardle, J. Behavioral susceptibility to obesity: Gene-environment interplay in the development of weight. Physiol Behav. 152(Pt B), 494–501. (2015).
Loos, R. J. The genetics of adiposity. Curr Opin Genet Dev, 50. 86-95. (2018)
Bahadoran, Z., Mirmiran, P., & Azizi, F. Fast food pattern and cardiometabolic disorders: A review of current studies. Health Promot. Prospect. 5(4):231-40. (2015).
Taheri, S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch. Dis. Child. 91(11), 881 (2006).
Itani, O., Jike, M., Watanabe, N. & Kaneita, Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Medicine 32, 246–56 (2017).
Hirshkowitz, M. et al. National sleep foundation?s sleep time duration recommendations: methodology and results summary. Sleep Health 1(1), 40–3 (2015).
Knutson, K. L. et al. The National sleep foundation?s sleep health index. Sleep Health 3(4), 234–40 (2017).
Tai, S. Y., Wang, W. F. & Yang, Y. H. Current status of sleep quality in taiwan: a nationwide walk-in survey. Annals of General Psychiatry 14, 36 (2015).
Dashti, H. S., Scheer, F. A., Jacques, P. F., Lamon-Fava, S. & Ordovás, J. M. Short sleep duration and dietary intake: epidemiologic evidence, mechanisms, and health implications. Advances in Nutrition (Bethesda, Md) 6(6), 648–59 (2015).
Paradis, A. M., Godin, G., Pérusse, L. & Vohl, M. C. Associations between dietary patterns and obesity phenotypes. Int J Obes (Lond) 33(12), 1419–26 (2009).
Zhang, J. G. et al. Dietary patterns and their associations with general obesity and abdominal obesity among young Chinese women. Eur. J. Clin. Nutr 69(9), 1009–14 (2015).
Duffy, J. F., Willson, H. J., Wang, W. & Czeisler, C. A. Healthy older adults better tolerate sleep deprivation than young adults. J Am Geriatr Soc 57(7), 1245–51 (2009).
Patel, S. R. et al. The association between sleep duration and obesity in older adults. Int J Obes (Lond) 32(12), 1825–34 (2008).
Doo, M. & Kim, Y. The risk of being obese according to short sleep duration is modulated after menopause in Korean women. Nutrients. 9(3). (2017).
Weiss, A. et al. The association of sleep duration with adolescents? fat and carbohydrate consumption. Sleep 33(9), 1201–9 (2010).
Gallagher, D. et al. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups??. Am J Epidemiol 143(3), 228–39 (1996).
Tu, S. H. et al. Design and sample characteristics of the 2005?2008 nutrition and health survey in Taiwan. Asia Pac. J. Clin. Nutr 20(2), 225–37 (2011).
Clinical Guidelines on the. Identification, evaluation, and treatment of overweight and obesity in Adults?The evidence report. National institutes of health. Obesity Research 6(Suppl 2), 51s–209s (1998).
Health Promotion Administration, Ministry of Health and Welfare. Adult Healthy Body Mass Index. Accessed on Dec. 12. 2023. https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=542&pid=9737. (2020).
Silveira, E.A., et al. Body fat percentage assessment by skinfold equation, bioimpedance and densitometry in older adults. Arch Public Health. 78, 65 (2020)
Woolcott, O. O., & Bergman, R. N. Defining cutoffs to diagnose obesity using the relative fat mass (RFM): association with mortality in NHANES 1999-2014. Int J Obes (Lond). 44(6). 1301-10 (2020).
Romero-Corral, A. et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 32(6), 959–66 (2008).
Health Promotion Administration, Ministry of Health and Welfare. Methods for Measuring and Interpreting Adult Waist Circumference. Accessed on Dec. 12. 2023. https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=1125&pid=1697 (2020).
Syauqy, A., Hsu, C.Y., Rau, H. H., & Chao, J., C. Association of dietary patterns, anthropometric measurements, and metabolic parameters with C-reactive protein and neutrophil-to-lymphocyte ratio in middle-aged and older adults with metabolic syndrome in taiwan: a cross-sectional study. Nutr. J., 17(1):106. (2018).
Qi, L. & Cho, Y. A. Gene-environment interaction and obesity. Nutrition Reviews 66(12), 684–694 (2008).
Qi, Q. et al. Fried food consumption, genetic risk, and body mass index: gene-diet interaction analysis in three US cohort studies. BMJ 348, g1610 (2014).
Mosavat, M., Mirsanjari, M., Arabiat, D., Smyth, A. & Whitehead, L. The role of sleep curtailment on leptin levels in obesity and diabetes mellitus. Obesity Facts 14(2), 214–21 (2021).
Watanabe, M., Kikuchi, H., Tanaka, K. & Takahashi, M. Association of short sleep duration with weight gain and obesity at 1-year follow-up: a large-scale prospective study. Sleep 33(2), 161–7 (2010).
Chaput, J. P., Després, J. P., Bouchard, C. & Tremblay, A. Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec family study. Obesity (Silver Spring, Md) 15(1), 253–61 (2007).
Knutson, K. L., Spiegel, K., Penev, P. & Van Cauter, E. The metabolic consequences of sleep deprivation. Sleep Med. Rev. 11(3), 163–78 (2007).
Prinz, P. Sleep, appetite, and obesity-what is the link?. PLoS Medicine 1(3), e61 (2004).
Soltanieh, S., Solgi, S., Ansari, M., Santos, H. O. & Abbasi, B. Effect of sleep duration on dietary intake, desire to eat, measures of food intake and metabolic hormones: A systematic review of clinical trials. Clinical Nutrition ESPEN 45, 55–65 (2021).
Karl, J. P. & Roberts, S. B. Energy density, energy intake, and body weight regulation in adults. Advances in Nutrition (Bethesda, Md) 5(6), 835–50 (2014).
Bray, G. A. & Siri-Tarino, P. W. The role of macronutrient content in the diet for weight management. Endocrinol. Metab. Clin. North Am 45(3), 581–604 (2016).
Zhao, Z. et al. Association of dietary patterns with general and central obesity among Chinese adults: a longitudinal population-based study. BMC Public Health 23(1), 1588 (2023).
Albuquerque, T. G., Bragotto, A. P. A. & Costa, H. S. Processed food: nutrition, safety, and public health. Int J. Environ. Res ;19(24). (2022).
Mambrini, S. P. et al. Ultra-Processed food consumption and incidence of obesity and cardiometabolic risk factors in adults: A systematic review of prospective studies. Nutrients 15(11), 2583 (2023).
Estruch, R. & Ros, E. The role of the mediterranean diet on weight loss and obesity-related diseases. Rev Endocr Metab Disord. 21(3), 315–27 (2020).
Louie, J. C. Y., Flood, V. M., Hector, D. J., Rangan, A. M. & Gill, T. P. Dairy consumption and overweight and obesity: a systematic review of prospective cohort studies. Obesity Reviews 12(7), e582–e92 (2011).
Sanchez, C., Killgore, W., Gehrels, J., Alfonso-Miller, P. & Grandner, M. 0127 nighttime snacking: prevalence and associations with poor sleep, health, obesity, and diabetes. Sleep 41(suppl_1), A49–A50 (2018).
Greer, S. M., Goldstein, A. N. & Walker, M. P. The impact of sleep deprivation on food desire in the human brain. Nat Commun 4, 2259 (2013).
Brondel, L., Romer, M. A., Nougues, P. M., Touyarou, P. & Davenne, D. Acute partial sleep deprivation increases food intake in healthy men. Am. J. Clin. Nutr 91(6), 1550–9 (2010).
Chaput, J.-P. & Tremblay, A. Insufficient sleep as a contributor to weight gain: an update. Curr. Obes. Rep 1(4), 245–56 (2012).
Schmid, S. M. et al. Short-term sleep loss decreases physical activity under free-living conditions but does not increase food intake under time-deprived laboratory conditions in healthy men. Am. J. Clin. Nutr 90(6), 1476–82 (2009).
Creasy, S. A. et al. Higher amounts of sedentary time are associated with short sleep duration and poor sleep quality in postmenopausal women. Sleep 42, 7 (2019).
Li, Q. The association between sleep duration and excess body weight of the American adult population: a cross-sectional study of the National health and nutrition examination survey 2015?2016. BMC Public Health. 21(1), 335 (2021).
Jungquist, C. R. et al. Validation of the behavioral risk factor surveillance system sleep questions. J Clin Sleep Med 12(3), 301–310 (2016).
Lee, P. H. Validation of the National health and nutritional survey (NHANES) single-item self-reported sleep duration against wrist-worn accelerometer. Sleep and Breathing 26(4), 2069–2075 (2022).
Carazo-Vargas, P. et al. Lack of agreement between polysomnography and accelerometry devices for measuring sleep efficiency and movement in university Stu dents. Measure Phys Educ Exerc Sci 24(4), 291–302 (2020).
Jungquist, C. R., Pender, J. J., Klingman, K. J. & Mund, J. Validation of capturing sleep diary data via a wrist-worn device. Sleep Dis. 2015:758937. (2015).
Mathieu, M. E., Reid, R. E. R. & King, N. A. Sensory profile of adults with reduced food intake and the potential roles of nutrition and physical activity interventions. Adv. Nutr. (Bethesda Md). 10 (6), 1120–1125 (2019).
Sieske, L. et al. Inflammation, appetite and food intake in older hospitalized patients. Nutrients 11, 9 (2019).
de Boer, A., Ter Horst, G. J. & Lorist, M. M. Physiological and psychosocial age-related changes associated with reduced food intake in older persons. Ageing Res. Rev. 12 (1), 316–328 (2013).
Wang, X. et al. Factors associated with eating behaviors in older adults from a socioecological model perspective. BMC Public. Health. 23, 1726 (2023).
Hargens, T. A., Kaleth, A. S., Edwards, E. S., & Butner, K. L. Association between sleep disorders, obesity, and exercise: a review. Nature and science of sleep. 5, 27–35. (2013).
Acknowledgements
We appreciate the support from National Taipei University of Nursing and Health Sciences [Grant Number: 107EH12-506].
Funding
This work was supported by National Taipei University of Nursing and Health Sciences [Grant Number: 107EH12-506].
Author information
Authors and Affiliations
Contributions
L.Y.L designed the study, collect & analyzed the data, wrote the first draft of the paper, and critically revised the paper. Y.N.C. analyzed the data, and critically revised the paper. H.C.Y., J.C-J.C., and H.Y.C. interpreted the data and critically revised the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lin, LY., Hsu, CY., Chao, J.CJ. et al. Interactive effects of sleep duration and dietary patterns on obesity moderated by age. Sci Rep 15, 34548 (2025). https://doi.org/10.1038/s41598-025-17886-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17886-2