Abstract
The study aimed to evaluate the impact of various parameters on treatment plan quality and delivery time in helical tomotherapy (HT) for small cell lung cancer patients with extensive pleura metastasis (SCLC-EPM) and to identify the optimal parameter combination. Four SLCL-EPM patients were included. For each patient, the planning target volume (PTV) and organs at risk (OARs), including the left lung, right lung, total lung, heart, esophagus, spinal cord, were delineated. A total of 27 treatment plans per patient (108 total) were generated by varying three parameters: Field Width (FW), Pitch Factor (PF), Modulation Factor (MF). FW defined treatment field length at isocenter. Smaller FWs boosted precision but extend beam-on time. PF was couch movement per rotation relative to FW; tighter PFs reduced dose fluctuations; MF, the max-to-average leaf-opening ratio, improved modulation at the cost of longer delivery. The reference plan used default values (FW \(=\) 2.5 cm, PF \(=\) 0.287, MF \(=\) 3.6), assumed to yield the best dose distribution and treatment time. Plan quality was assessed using PTV metrics (Homogeneity index (HI), conformity index (CI), D95%, D90%, D2%), OAR metrics (Dmean, Dmax, V5Gy, V20Gy, V25Gy, V30Gy), and treatment time. FW significantly influenced dose distribution (particularly homogeneity, right lung, liver, and esophagus) and was the most critical parameter for reducing treatment time (average reduction \(>\) 50%). Tighter PF slightly decreased OARs dose (left lung, total lung, and live) without prolonging treatment time. Higher MF moderately increased treatment time and affected lung dose but showed no significant differences in CI or HI. Clinically, three patients achieved partial response, and one had stable disease at 6 months post-thoracic radiation, with no severe lung toxicities observed. Balancing plan quality and efficiency, the optimal HT parameters for SCLC-EPM were FW:2.5 cm, PF: 0.287, MF: 3. Radiotherapy for SCLC-EPM proved effective and safe after first-line chemotherapy with or without immunotherapy.
Similar content being viewed by others
Introduction
Small cell lung cancer (SCLC), accounting for 14–20% of all lung cancers, is the most aggressive malignancies with rapid tumor growth and early distant metastasis1. Approximately two-thirds of SCLC patients present with extensive-stage (ES-SCLC), of whom 20% exhibit extensive pleural metastasis (EPM) at diagnosis. For these patients with EPM, systematic chemotherapy with or without immunotherapy remains the standardized treatment. Prior to immunotherapy era, thoracic radiotherapy had showed to improve local regional control and overall survival in ES-SCLC. However, data on EPM-specific radiotherapy remain limited due to two key challenges: firstly, complex treatment planning. The highly irregular target volume (encompassing the entire hemithoracic pleura, from the lung apices to the diaphragmatic crura) and proximity to critical organs make planning and dose delivery time-consuming and technically demanding2. Secondly, dose distribution limitations. Conventional radiotherapy techniques struggle to achieve uniform target coverage while sparing OARs due to beam overlap or low dose cold spots2. Nevertheless, helical tomotherapy (HT) addresses these challenges by delivering well tolerated homogeneous dose distributions via overlapping intensity-modulated fan beams3,4,5.
Unlike conventional radiotherapy technique, HT is a specialized intensity-modulated radiation therapy (IMRT) system featuring a 6 MV photon beam with 64 binary multileaf collimators (MLC) and a continuously rotating gantry synchronized with couch movement, enabling precise dose sculpting6,7,8. During the process of HT radiotherapy, treatment planning is the key part. HT treatment planning relies on three critical parameters: Field width (FW), Pith factor (PF) and Modulation factor (MF). FW denotes the longitudinal axis extent of the treatment field at machine isocenter. Smaller FW (1,2.5, or 5 cm) increases beam-on time but may improve precision6. PF represents the ratio of couch movement per gantry rotation to FW. A tighter PF (e.g., 0.86/n, where n is an integer ) minimizes dose fluctuations (“thread effect”)9. MF shows the ratio of maximum to average leaf-opening time. Higher MF enhances beam modulation but prolongs treatment time10.
Selecting optimal parameters requires balancing plan quality (e.g., target coverage, OAR sparing) and treatment efficiency (beam-on time). While lower FW, PF and higher MF improve dose conformity for complex targets, they also increase treatment time11. An inaccurate selection of treatment planning parameters could significantly reduce the likelihood of achieving an adequate dose distribution12. It exists clinical trade-offs and unmet needs. Prior studies on parameter optimization in HT have primarily focused on cancers, like prostate11,13,14, total body irradiation15,16, total skin irradiation17, soft tissue sarcomas18, breast6,19, lung cancer4, but none have addressed SCLC-EPM, with uniquely challenging PTV and OARs geometry.
This study evaluated the impact of FW, PF and MF on plan quality and treatment time in HT for SCLC-EPM, aiming to identify the optimal parameter combination for clinical use.
Materials and methods
Patient selection, immobilization, delineation
Four ES-SCLC patients with pleural metastasis (ES-SCLC-EPM), previously treated with HT between 2021 and 2022, were retrospectively enrolled. This retrospective data collection was approved by our institutional review board (Shanghai Jiao Tong University Medical School Affiliated Ruijin Hospital) with waivers for the patient’s informed consent. The study was performed in accordance with the Declaration of Helsinki. Patients were position in the head-first supine position (HFS) using a vacuum cushion with a headrest. CT scans (both contrast/non-contrast) were acquired using a Philips Brilliance CT Big Bore system with a 3 cm slice thickness. The scan coverage extended ≥ 10 cm beyond the target boundary. Images were transferred to the Eclipse treatment planning system (V15.6, Varian). Target volumes and organs were contoured based on fusion contrast and non-contrast CT images. Following established oncology group guidelines, the clinical target volume (CTV) was delineated, the planning target volume (PTV) was generated by expanding the CTV by 5 mm. OARs included the left lung, right lung, combined lungs, heart, spinal cord, liver, and esophagus.
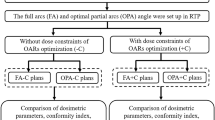
Treatment planning
After contouring in the Eclipse system, each patient’s planning CT and contoured structures were transferred to the HT treatment planning system (Radixact, Accuray, Sunnyvale, CA, USA). All plans employed a helical IMRT technique for HFS position, with a prescribed dose of 40 Gy delivered in 20 fractions (5 fractions per week). To achieve dose objectives, four auxiliary structures (NT1, NT2, NT, NT_E) were created (Fig. 1). NT1 and NT2 were generated by retracting PTV by 2-7 mm and 7-17 mm, respectively. NT and NT_E were designed to reduce right-side central lung dose and block left-side lung dose.
Schematic representation of four auxiliary structures (NT1, NT2, NT, NT_E) for helical tomotherapy (HT) treatment planning extensive-stage small cell lung cancer patient with pleural metastasis (ES-SCLC-EPM), (1) NT1: 2-7 mm uniform retraction from PTV; (2) NT2: 7-17 mm uniform retraction from PTV; (3) NT: right-side central lung dose-reduction structure; (4) NT_E: left-side blocking structure.
The study evaluated three parameter values: Field width (FW): 1, 2.5, and 5 cm. Modulation factor (MF): 2.4, 3, and 3.6 (representing low to high modification ability). Pith factor (PF): 0.215, 0.287, and 0.43 (derived from 0.86/n [9], representing high to low dose sculpting ability). For each patient, 27 treatment plans were created using all combinations of these parameters. The reference plan was optimized with FW \(=\) 2.5 cm, PF \(=\) 0.287, and MF \(=\) 3.6, balancing dose distribution and treatment time. Dose constraints from the reference plan were applied to all other plans.
The least-square optimization method was employed to optimize the objective function20,21, and the final dose calculation was carried out at a high resolution using a grid of 3.91 × 5x3.91 mm. This calculation utilized a convolution superposition algorithm. The final dose calculation underwent 600 iterations for each plan. Consistent machine parameters were maintained across all plans, including delivery mode, plan mode, and jaw mode. The treatment couch was modeled according to vendor recommendations15.
Plan evaluation parameters
The study required ≥ 90% of target volumes to receive the prescribed dose. Target evaluation metrics included D95%, D50%, D2% (near-maximum dose), heterogeneity index (HI), and conformity index (CI). The HI for PTV was calculated using the formula22 HI \(=\) Dmax/Dp, where Dmax was the max dose, Dp was the prescription dose. An HI value closer to 1 indicated a heterogeneous dose distribution within the target volume. The CI was determined using the Paddick Eq. 22,23: CI \(=\) VTref/VT x VTref /Vref, where VTref indicated the target volume enclosed by the prescription isodose (cm3), Vref denoted the volume surrounded by the prescription isodose (cm3), and VT represented the overall target volume (cm3). A CI value closer to 1 signified better dose conformity for the target volume. Both HI and CI values were automatically calculated by TPS.
OARs were assessed using metrics, such as V5Gy, V20Gy, V30Gy, Dmean for the left lung, right lung, and lungs, V5Gy, V25Gy, Dmean for the heart, Dmean for the esophagus, V20Gy, Dmean for the liver, and Dmax for the spinal cord. V5Gy, V20Gy, V25Gy, and V30Gy represented the volume percent covered by the 5 Gy, 20 Gy, 25 Gy, 30 Gy dose, respectively, Dmeans was the mean dose, and Dmax was the max dose. Additionally, treatment time and gantry period were recorded as efficiency metrics.
Statistical analysis
In this study, continuous data was described using the mean values \(\pm\) standard deviation (\(\overline{x } \pm\) SD). Normality was assessed using the Shapiro–Wilk test: if p \(>\) 0.05, the data was considered normal, and if p \(\le\) 0.05, the data was considered non-normal. For normally distributed data: A one-way repeated-measures ANOVA (RANOVA) was applied to compare groups (e.g., F1, F2, F3). Post-hoc pairwise comparisons (e.g., F1 vs. F2, F1 vs. F3, F2 vs. F3) were conducted using Fisher’s LSD test. Some results were reported as: mean \(\pm\) SD, p-value, and 95% CI. For three dependent variables (FW, PF, MF), a three-way ANOVA was performed to assess: main effects (reported as F-statistic, p-value, partial eta-squared (η2)), interaction effects (e.g., FW × PF, FW × MF, PF × MF, FW × PF × MF). For Non-Normal Data: The Kruskal–Wallis test (non-parametric alternative to ANOVA) was used for multiple-group comparisons. All statistical analyses were performed using SPSS 26.0 software (IBM, USA), and a significance level of p \(<\) 0.05 was considered as indicating a statistically significant difference.
Results
The influence of FWs on plan quality
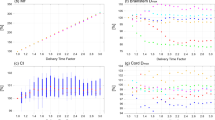
Figure 2 showed the dose comparison results for PTV and OARs across varied FWs at three PF conditions. As shown in Fig. 2.a, the D90% and D95% remained consistent across different FW settings. However, the D2% increased gradually with increasing FW, reaching its highest value at F3. This observation suggested that narrower FW (e.g., F1) may be preferable for maintaining plan quality. OAR evaluation (Fig. 2.b, d) showed that Dmean also increased with FW rise, reaching the largest value at F3. Clear trends were observed for the right lung, liver, and esophagus, while the Dmax to spinal cord remained stable across all plans with varying FWs and PFs. Figure 2. c, d further demonstrated that similar trends were observed for volume doses (V20Gy, V25Gy, V30Gy, V5Gy) of OARs. Compared with F2, F3 plans, F1 plans showed a significant reduction in volume doses (most p \(<\) 0.05). Notable reductions were particularly evident for the lung and liver volumes (V20Gy, V5Gy). For the Lung_S_V5Gy, F1 plans achieved the lowest mean dose (56.71 \(\pm\) 3.98), with statistically significant reductions compared with F2 (60.81 \(\pm\) 3.50, mean difference -4.10, p \(<\) 0.05) and F3 (66.84 \(\pm\) 2.79, mean difference -10.13, p \(<\) 0.05). All pairwise comparisons remained significant after LSD post-hoc, with the largest effect observed between F1 and F3 plans (95% CI: -11.75 to -8.51). Little difference was observed for Dmean, V5Gy of the heart, and V30Gy of the right lung. Overall, FW significantly impacted the dose distribution for both the target volume and OAR, particularly for homogeneity, right lung, liver, and esophagus.
Dosimetric comparison of helical tomotherapy (HT) plans with different combinations of Field Widths (FWs) and Pitch Factors (PFs) for PTV and OARs. FWs: F1(1 cm), F2(2.5 cm), F3(5 cm); PFs: P1(0.215), P2(0.287), P3(0.43). (a) PTV coverage analysis: D90%, D95%, and D2%; (b) Organ-at-risk (OAR) protection: Dmean and Dmax for Heart, Lungs (left/right/combined), Liver, esophagus, and spinal cord; (c) Volume-dose metrics: V20Gy, V25Gy, and V30Gy for Heart, right lung, combined lungs, and Liver; (d) Low-dose evaluation: V5Gy for Heart, lung structures. Abbreviations: D*: dose in Gray (Gy); V*Gy: volume receiving * Gy (%); Lung_R: right lung; Lung_L: left lung; Lung_S: combined lungs; SC: spinal cord; Eso: esophagus.
The Influence of PFs on plan quality
Figure 3 displayed dose distribution of a plan with F:0.25 cm, P:0.215,0.287,0.43, M:3 and DVH of the plan with F:0.25 cm, P:0.215, M:3. Table 1,2 showed the statistical results of dose parameters for target volume and OARS across varied PFs at three FW conditions. As shown in the Table 1, D95%, D90% and D2% increased gradually with the rise in PFs, reaching the largest values at P3. The dose difference (D95%, D90%, D2%) with varied PFs was statistically significant (D95%: F(2,105) = 4.354, p \(=\) 0.015, \({\eta }^{2}=0.077(small effect)\); D90%: F(2,105) = 6.062, p \(=\) 0.003, \({\eta }^{2}=0.104(medium effect)\); D2%: F(2,105) = 25.355, p \(=\) 0.001, \({\eta }^{2}=0.326(large effect)\)). The observation indicated that looser PFs resulted in higher dose distribution. Balancing D90% and D2%suggested that a medium-tightened PF (P2) would be the optimal parameter. Although D2% increased slightly, no significant change was observed in HI. Additionally, not all CI values were statistically significant under varied PFs conditions: P2 \(vs\) P3: non-significant (p \(=\) 0.708, 95% CI: -0.049 to 0.072); P1 \(vs\) P2: significant (p \(=\) 0.012, 95% CI: 0.018 to 0.138); P1 \(vs\) P3: significant (p \(=\) 0.004, 95% CI: 0.029 to 0.149), but the largest CI values consistently came from P1, suggesting that tighter PFs did not significantly improve either CI or HI.
Dose distribution and dose-volume histogram (DVH) analysis for a helical tomtherapy (HT) plan. A-C: axial isodose distributions demonstrating the effect of varying Pith Factors (PFs) while maintaining Field Width (F \(=\) 0.25 cm) and Modulation Factor (M \(=\) 3), (A) P:0.43, (B) 0.215, (C) 0.287; (D) DVH analysis of the optimal plan (F \(=\) 0.25 cm, P \(=\) 0.215, M \(=\) 3), showing coverage of PTV and critical organs at risks (OARs).
Table 2 revealed that most dose distribution parameters (Dmean and volume dose) for OARs increased slightly with the rise in PFs. While Dmean and volume dose for the right lung didn’t show statistically significant differences, the significant differences were observed for the Left lung and total lung (Lung_S_Dmean: F(2,105) \(=\) 3.309, \(p < 0.05\), \({\eta }^{2}=0.106(medium effect))\). This indicated that the dose values for the left lung could notably impact the total lung. Similarly, Dmean for the liver showed statistically significant differences (F(2,105) \(=\) 4.052, p \(<\) 0.05, \({\eta }^{2}=0.11(medium effect)\)). Overall, the results suggested that a tighter PF could slightly reduce OARs dose, especially for the left lung, total lung, and liver.
The influence of MFs on treatment plan quality
Table 3,4 summarized the statistical results of dose parameters for target volume and OARs across varied MFs at three FW conditions. As shown in the Table 3, D95% slightly increased with the rise in MFs, but D90% and D2% reduced gradually with the rise in MFs. Just dose difference (D90%) with varied MFs was statistically significant (F(2,105) \(=\) 6.055, p \(=\) 0.003, \({\eta }^{2}=0.103(medium effect)\)). The balance between D90% and D2% suggested that M2 should be the better parameter. No significant differences were observed for CI or HI under varied MFs conditions.
As showed in the Table 4, most dose distribution parameters (Dmean and volume dose) for OARs decreased gradually with the rise in MFs. Particularly notable reductions were observed for V5Gy and V20Gy for the right lung and total lung, with an average decrease of 1-2 Gy. Only V5Gy for the left lung and total lung showed statistically significant (Lung_L_V5Gy: F(2,105) \(=\) 9.514, p \(=\) 0.001, \({\eta }^{2}=0.153\left(large effect\right);\) Lung_S_V5Gy: F(2,105)\(=\) 10.68, p \(=\) 0.001, \({\eta }^{2}=0.169 (large effect))\) differences under three MF conditions. These findings indicated that MF could impact the dose distribution, especially for the lung.
The interaction effects of FWs, PFs, and MFs on treatment plan quality
Table 5, 6 summarized the interaction effects of FWs, PFs and MFs on treatment plan quality. Table 5 revealed that FW and PF significantly influenced D95%, D90%, and D2% (all p \(<\) 0.05). MF only affected D90% (p \(<\) 0.05). PF significantly impacted CI (p \(<\) 0.05). No significant interactions were observed for any combination of factors (FW x PF, FW x MF, PW x MF and FW x PF x MF, all p \(>\) 0.05). Table 6 further showed that interaction effects of FWs, PFs and MFs on OARs protection. It revealed that FW significantly affected Heart (Dmean, V5Gy), Lungs (L/R/Sum) (Dmean, V5Gy, V20Gy), and Liver (Dmean). PF influenced Lung-L and Lung-S (Dmean, V5Gy) and Liver (Dmean). MF impacted Lung-R (V5Gy), Lung-L (Dmean), and Lung-S (Dmean, V5Gy, V20Gy). No significant interactions were found for OARs (all p \(>\) 0.05).
The influence of parameters (FW, PF, and MF) on treatment time
Figure 4 highlighted the specific values and trends for treatment time across varied FWs, PFs, and MFs. Among these parameters, FW was identified as the most influential parameter affecting treatment time. The average treatment time exhibited a significant decrease, reaching more than half when comparing F1 to F2. For instance, the average treatment time for F1 was 1700s, whereas the value for F2 reduced to 655 s. In contrast, PFs had less influence on treatment time. The treatment time increased gradually with the rise in MFs, but the increase was modest. For instance, the average treatment time for M1 was 734 s, whereas the value for M2 increased to 897 s. Considering only treatment time alone, the parameters combination (F2-F3, P1-P3, M1-M2) was suggested as a better balance range.
Treatment outcomes
Three of ES-SCLC-EPM archived partial response and one patient archived stable disease after 6-months of radiotherapy. Figure 5 showed a typical case of SCLC patients with extensive pleura metastasis treated by Helical Tomotherapy. Disease of this patient progressed after 4 cycles of first-line platinum plus etoposide chemotherapy. Following one cycle of lurbinectedin, the patient received a total dose of 40 Gy in 20 fractions to the primary tumor and thoracic metastases using helical tomotherapy. After six months post-irradiation, a major partial response and grade 1 pneumonia were observed (Fig. 5. E and F). Second-line treatment with lurbinectedin was continued after irradiation. In a recent follow-up, the disease of this patient remained controlled after 1 year irradiation.
Discussion
The analyses of FW demonstrated that FW significantly influenced plan quality, particularly for treatment time, homogeneity, volume dose (right lung, liver, and esophagus). The variation trends of D90%, D95%, and D2% were inversely related. For instance, while D90% and D95% decreased slightly, D2% increased with the rise in FWs. Additionally, FW emerged as a crucial factor affecting treatment time. When FW was reduced from 1 cm to 2.5 cm, treatment time decreased by nearly 50%. This reduction was attributed to dose manipulation in the cranial caudal direction, represented by FW11. Although smaller FW enhanced computer accuracy and plan quality, they also led to longer irradiation time. Analogously, higher resolution improved image clarity but could result in an increase in “hot spot”. These findings regarding FW were consistent with previous studies on other cancers13,24,25. Furthermore, the study found that FW primarily impacted the right lung, liver, and esophagus, with minimal influence on the heart and spinal cord. This was explained by the proximity of these OARs to the target. Discrepancies with other studies (Muthuselvi6, Philippe Meyer16) regarding the impact on different OARs were mentioned, potentially due to incomplete organ selections in those studies. Ideally, smaller FW values yielded better results21. However, the prolonged treatment time associated with smaller FWs were deemed clinically impractical. Considering these factors, F2 was identified as the optimal parameter.
In contrast to FW, PF exhibited consistency between D95% and D2%. Both values increased with the rise in PFs, likely due to the loss of longitudinal resolution in the dose distribution26. The study revealed that tighter PFs didn’t significantly enhance the CI and HI of the target without affecting the treatment time. The results for CI and HI were inconsistent with previous studies on breast cancer6, prostate cancer27, but findings regarding treatment time aligned with previous research. For OARs doses (e.g., left lung and liver), tighter PFs provided a dose advantage. Similar results were reported by other researchers, such as Philippe et al. 18, and skorska et al11, who highlighted the dose advantage for OARs. Based on these observations, P2 was recommended as the optimal parameter.
In general, high MFs facilitated steeper dose gradients, which corelated with lower D2%, resulting in longer treatment time. The study supported this observation, finding that both D95% and D2% decreased with the rise in MFs. However, higher MFs could significantly affect OARs dose, particularly for the lungs. Similar to PF, the influence on treatment time aligned with previous studies11,27,28. Additionally, the results indicated that reduced MF constraints could impact dose distribution for PTV and OARs. Lower MF values decreased treatment time but compromised dose conformity and homogeneity. Takayuki et al29 reported similar findings for several cancers. Similarly, Santos30, Cavinato et al31 noted that higher MFs increased plan complexity, potentially leading to unacceptable dose delivery. Therefore, a good balance between treatment time and plan quality was essential. The study concluded that M2 was the optimal parameter.
Additionally, the three-factor ANOVA (FW × PF × MF) results for both target and OARs revealed two key findings. The main effects of FW, PF and MF on target metrics (e.g., D95%, CI) and OARs (e.g., Heart: Dmean, Lung: Dmean, V5Gy) aligned with those observed in prior single-factor analyses. No significant interactions (FW × PF, FW × MF, PF × MF, or FW × PF × MF) were detected for any dependent variable (all p \(>\) 0.05). This indicated that these variables (FW, PF, MF) could be optimized independently in clinical practice without considering cross-factor adjustments.
Although SCLC-EPM presented inherently complexity, the parameter combination proposed in this study (FW: 2.5 cm, PF: 0.287, MF: 3) achieved a better balance between treatment efficiency and plan quality. This selection was guided by three key criteria: (1) dosimetric superiority in PTV coverage (e.g., The D95% of the PTV improved by 1% (from 39.32 Gy in P1 to 39.46 Gy in P2 ), while CI decreased by 3% (from 1.4886 in F1 to 1.4506 in F2), (2) OAR sparing (e.g., The V5Gy of the left lung and total lung dose reduced by 6% (from 85.81% in M1 to 80.74% in M2), and (3) treatment efficiency(e.g., The average treatment time decreased by 1005 s (from1700s in F1 to 655 s in F2)). These findings align with clinical priorities for SCLC-EPM, where rapid palliation and maximal organ protection are critical. While individual patient anatomy may require adjustments, this study provides evidence-based guidelines for HT planning in SCLC-EPM, potentially enhancing both efficiency and effectiveness. Such an approach could standardize care while maintaining flexibility for patient-specific adaptation. Furthermore, among the four ES-SCLC patients treated with EPM-radiotherapy, three achieved partial response and one had stable disease. Notable, no severe lung toxicities were observed in these patients.
To evaluate clinical performance, we conducted a comparative dose analysis between HT and conventional linear accelerator (LA)-based radiotherapy. The LA system was TrueBeam (Varian Medical Systems, Palo Alto, CA) with volumetric modulated arc therapy (VMAT). Treatment plans for LA were designed by Eclipse treatment planning system (TPS, v.15.6) using the Analytic Anisotropic Algorithm TPS (AAA) with 6 MV flattening filter-free (FFF) beams. For target Coverage and Homogeneity, D2% was comparable between HT and LA (HT: 41.9 Gy vs. LA: 45.3 Gy), and HT demonstrated superior CI and HI. For OAR sparing, HT provided obvious better OAR protection, particularly for the lungs: Dmean: HT (19.45 Gy) vs. LA (34.79 Gy), V5Gy: HT (83%) vs. LA (100%), V20Gy: HT (44%) vs. LA (99%), V30Gy: HT (30%) vs. LA (80%). Above all, HT offered superior OAR sparing—particularly in reducing low-to-intermediate lung doses. These results suggest HT may be preferable in cases where minimizing dose to critical structures is prioritized.
The limitations of this study included the examination of only a small number of patients. Although the study evaluated 27 different treatment plan parameter combinations, resulting in a total of 108 optimized plans, these plans were based on only four patients. Therefore, this limitation affects inter-patient comparisons but does not diminish the technical insights gained from intra-patient plan optimization. Further studies with large sample size are clearly needed. Another major limitation was the insufficient consideration of parameter combinations for FW, PF, and MF. Additionally, the study didn’t address motion management for SCLC-EPM. Future research should explore options such as motion tracking, compensating modality, or robust optimization.
Conclusions
The study assessed the influence of treatment plan parameters (FW, PF, MF) and identified the optimal combination of plan parameters for HT in treating lung cancer with extensive pleura metastasis. Considering the balance between plan quality and treatment time, the parameter combination of FW: 2.5 cm, PF: 0.287, MF: 3 was identified as optimal. EPM-radiotherapy proved to be both efficient and safe for highly-selected SCLC-EPM patients following first-line chemotherapy with or without immunotherapy.
Data availability
The datasets related to patient information are not available. Other data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- FW:
-
Field width
- PF:
-
Pitch factor
- MF:
-
Modulation factor
- HT:
-
Tomotherapy
- SCLC:
-
Small cell lung cancer
- EPM:
-
Extensive pleura metastasis
- SCLC-EPM:
-
Small cell lung cencer patients with extensive pleura metastasis
- ES-SCLC:
-
Small cell lung cancer with extensive-stage
- ES-SCLC-EPM:
-
ES-SCLC with pleural metastasis
- OARs:
-
Organs at risk
- HI:
-
Homogeneity index
- CI:
-
Conformity index
- IMRT:
-
Intensity modulated radiotherapy
- MLC:
-
Multileaf collimator
- PTV:
-
Plan target volume
- CTV:
-
Clinical target volume
- HFS:
-
Head-first supine position
- CT:
-
Computed tomography
- VMAT:
-
Volumetric modulated arc therapy
- HT:
-
Helical tomotherapy
- LA:
-
Linear accelerator
- FFF:
-
Flattening filter-free
References
Bade, B. C., Dela Cruz, C. S. & Cancer, L. Epidemiology, etiology, and prevention. Clin. Chest Med. 41(1–24), 2020. https://doi.org/10.1016/j.ccm.2019.10.001 (2020).
Rimner, A. et al. Failure patterns after hemithoracic pleural intensity modulated radiation therapy for malignant pleural mesothelioma. Int. J. Radiat. Oncol. Biol. Phys. 90, 394–401. https://doi.org/10.1016/j.ijrobp.2014.05.032 (2014).
Cendales, R., Schiappacasse, L., Schnitman, F., Garcia, G. & Marsiglia, H. Helical tomotherapy in patients with breast cancer and complex treatment volumes. Clin. Transl. Oncol. 13, 268–274. https://doi.org/10.1007/s12094-011-0652-7 (2011).
Hong, C. S. et al. Normal lung sparing Tomotherapy technique in stage III lung cancer. Radiat. Oncol. 12, 167. https://doi.org/10.1186/s13014-017-0905-x (2017).
Ito, M. et al. Efficacy of virtual block objects in reducing the lung dose in helical tomotherapy planning for cervical oesophageal cancer: a planning study. Radiat. Oncol. 13, 62. https://doi.org/10.1186/s13014-018-1012-3 (2018).
Muthuselvi, C. A., Bijina, T. K. & Pichandi, A. Evaluation of optimal combination of planning parameters (Field Width, Pitch, and Modulation Factor) in helical tomotherapy for bilateral breast cancer. J. Med. Phys. 45, 234–239. https://doi.org/10.4103/jmp.JMP_31_20 (2020).
Langen, K. M. et al. QA for helical tomotherapy: report of the AAPM task group 148. Med. Phys. 37, 4817–4853. https://doi.org/10.1118/1.3462971 (2010).
Rong, Y. & Welsh, J. S. Dosimetric and clinical review of helical tomotherapy. Expert Rev. Anticancer Ther. 11, 309–320. https://doi.org/10.1586/era.10.175 (2011).
Kissick, M. W. et al. The helical tomotherapy thread effect. Med. Phys. 32, 1414–1423. https://doi.org/10.1118/1.1896453 (2005).
Sarkar, V., Lin, L., Shi, C. & Papanikolaou, N. Quality assurance of the multileaf collimator with helical tomotherapy: design and implementation. Med. Phys. 34, 2949–2956. https://doi.org/10.1118/1.2748105 (2007).
Skorska, M. & Piotrowski, T. Optimization of treatment planning parameters used in tomotherapy for prostate cancer patients. Phys. Med. 29, 273–285. https://doi.org/10.1016/j.ejmp.2012.03.007 (2013).
Piotrowski, T. et al. Tomotherapy: implications on daily workload and scheduling patients based on three years’ institutional experience. Technol. Cancer Res. Treat. 13, 233–242. https://doi.org/10.7785/tcrt.2012.500374 (2014).
Fiorino, C. et al. Physics aspects of prostate tomotherapy: planning optimization and image-guidance issues. Acta. Oncol. 47, 1309–1316. https://doi.org/10.1080/02841860802266755 (2008).
Grigorov, G. et al. Optimization of helical tomotherapy treatment plans for prostate cancer. Phys. Med. Biol. 48, 1933–1943. https://doi.org/10.1088/0031-9155/48/13/306 (2003).
Kaliyaperumal, V. et al. Optimal combination of pitch, modulation factor and dosimetric considerations in treatment planning for total body irradiation using helical tomotherapy. Asian Pac J Cancer Prev 24, 1239–1248. https://doi.org/10.31557/APJCP.2023.24.4.1239 (2023).
Wilhelm-Buchstab, T. et al. Total body irradiation: Significant dose sparing of lung tissue achievable by helical tomotherapy. Z Med. Phys. 30, 17–23. https://doi.org/10.1016/j.zemedi.2019.05.002 (2020).
Wang, H., Pi, Y., Guo, Y., Pei, X. & Xu, X. G. Influencing factors of total skin irradiation with helical tomotherapy. Front. Oncol. 12, 852345. https://doi.org/10.3389/fonc.2022.852345 (2022).
Meyer, P. et al. The optimal tomotherapy treatment planning parameters for extremity soft tissue sarcomas. Phys. Med. 31, 542–552. https://doi.org/10.1016/j.ejmp.2015.05.005 (2015).
Sugie, C. et al. Efficacy of the dynamic jaw mode in helical tomotherapy with static ports for breast cancer. Technol. Cancer Res. Treat. 14, 459–465. https://doi.org/10.1177/1533034614558746 (2015).
Mackie, T. R. From model-based dose computation to tomotherapy. Med. Phys. 50(Suppl 1), 70–73. https://doi.org/10.1002/mp.16292 (2023).
Mackie, T. R. et al. Tomotherapy: a new concept for the delivery of dynamic conformal radiotherapy. Med. Phys. 20, 1709–1719. https://doi.org/10.1118/1.596958 (1993).
Feuvret, L., Noel, G., Mazeron, J. J. & Bey, P. Conformity index: a review. Int. J. Radiat. Oncol. Biol. Phys. 64, 333–342. https://doi.org/10.1016/j.ijrobp.2005.09.028 (2006).
Singh, V. P., Kansai, S., Vaishya, S., Julka, P. K. & Mehta, V. S. Early complications following gamma knife radiosurgery for intracranial meningiomas. J. Neurosurg. 93(Suppl 3), 57–61. https://doi.org/10.3171/jns.2000.93.supplement (2000).
Moldovan, M. et al. Investigation of pitch and jaw width to decrease delivery time of helical tomotherapy treatments for head and neck cancer. Med. Dosim. 36, 397–403. https://doi.org/10.1016/j.meddos.2010.10.001 (2011).
Pardo-Montero, J. & Fenwick, J. D. Tomotherapy-like versus VMAT-like treatments: a multicriteria comparison for a prostate geometry. Med. Phys. 39, 7418–7429. https://doi.org/10.1118/1.4768159 (2012).
Binny, D., Lancaster, C. M., Harris, S. & Sylvander, S. R. Effects of changing modulation and pitch parameters on tomotherapy delivery quality assurance plans. J. Appl. Clin. Med. Phys. 16, 87–105. https://doi.org/10.1120/jacmp.v16i5.5282 (2015).
Cao, Y. J. et al. Patient performance-based plan parameter optimization for prostate cancer in tomotherapy. Med. Dosim. 40, 285–289. https://doi.org/10.1016/j.meddos.2015.03.005 (2015).
Ishibashi, A., Kurosaki, H., Miura, K., Utsumi, N. & Sakurai, H. Influence of modulation factor on treatment plan quality and irradiation time in hippocampus-sparing whole-brain radiotherapy using tomotherapy. Technol. Cancer Res. Treat 20, 15330338211045496. https://doi.org/10.1177/15330338211045497 (2021).
Yagihashi, T. et al. Impact of delivery time factor on treatment time and plan quality in tomotherapy. Sci. Rep. 13, 12207. https://doi.org/10.1038/s41598-023-39047-z (2023).
Santos, T., Ventura, T., Mateus, J., Capela, M. & Lopes, M. D. C. On the complexity of helical tomotherapy treatment plans. J. Appl. Clin. Med. Phys. 21, 107–118. https://doi.org/10.1002/acm2.12895 (2020).
Cavinato, S., Fusella, M., Paiusco, M. & Scaggion, A. Quantitative assessment of helical tomotherapy plans complexity. J. Appl. Clin. Med. Phys. 24, e13781. https://doi.org/10.1002/acm2.13781 (2023).
Funding
Science and Technology Innovation Plan Of Shanghai Science and Technology Commission,23Y11904700,Clinical Research Special Project of Shanghai Municipal Health Commission Health Industry,202340226,Shanghai Science and Technology Innovation Action Plan,23Y41900100,Shanghai Hospital Development Center Foundation,SHDC12023108
Author information
Authors and Affiliations
Contributions
L.D designed the study, performed some analyses, and wrote the main manuscript text. W.Q was responsible for statistical analysis and clinical data collection, C.L prepared some figures and tables, J.C and G.Z were responsible for project administration. All authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Duan, L., Qi, W., Li, C. et al. A case study on optimizing helical tomotherapy parameters for small cell lung cancer with extensive pleural metastasis. Sci Rep 15, 33390 (2025). https://doi.org/10.1038/s41598-025-18445-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-18445-5