Abstract
Although acute exacerbation of idiopathic interstitial pneumonia (AE-IIP) is a critical event, the detailed features of connective tissue diseases (CTD) that affect the incidence of AE-IIP have not been fully elucidated. This study aimed to clarify the CTD-related features that affect the incidence of AE-IIP. This was a post hoc analysis of a prospective and multicenter cohort study conducted between 2015 and 2020. Newly diagnosed patients with IIP were consecutively enrolled, and 74 autoimmune features and autoantibodies were comprehensively checked during IIP diagnosis. In total, 222 patients with IIP were enrolled. The median observation period was 36 months, during which 34 patients developed AE-IIP. In multivariate models adjusted for age, gender, and %predicted FVC, AE-IIP frequently occurred in patients positive for anti-cyclic citrullinated peptide (CCP) antibody (hazard ratio [HR]: 4.407, p = 0.004, q = 0.027), while it was less common in patients positive for antinuclear antibodies (ANA) ≥ 320 or polymyositis/dermatomyositis (PM/DM)- or systemic sclerosis (SSc)-related antibodies (HR < 0.001, p < 0.001, q < 0.001). A composite model consisting of these items stratified the incidence of AE-IIP (p < 0.001), which was closely related to the mortality. These results indicate that the presence of anti-CCP antibodies, ANA, or PM/DM/SSc-related antibodies, in addition to decreased lung function, could help determine the risk of AE-IIP in patients with IIP.
Similar content being viewed by others
Introduction
Acute exacerbation (AE) of interstitial lung diseases (ILD) is increasingly recognized as a serious event with high mortality rates during its clinical course. In particular, AE of idiopathic pulmonary fibrosis (IPF) has a devastating effect on the survival1,2,3. However, clinical studies on AE of non-IPF ILD are limited4,5,6,7. The overall incidence of AE varies widely across studies, and the annual incidence of AE-IPF has been reported to be 5–19%. It is more common in the advanced stages than early stages of IPF2,3,5,8,9,10. Furthermore, antifibrotics can suppress the incidence of AE-IPF11. In contrast, the annual incidence of AE-ILD in patients with connective tissue disease (CTD) was reported to be lower than that of AE-IPF12,13. Therefore, an exact diagnosis of ILD is important for the management and prediction of AE-ILD.
In the diagnosis of idiopathic interstitial pneumonia (IIP), ruling out other causes such as CTD and hypersensitivity pneumonitis is important for appropriate management. However, patients with IIP may have clinical features of autoimmunity but may not meet the criteria for CTD. Although such patients are known to have interstitial pneumonia with autoimmune features (IPAF)14 and have received much attention worldwide, the relationship between IPAF and AE-IIP has not been fully elucidated in patients with IIP. Our previous prospective study showed that patients meeting the criteria for IPAF had a lower frequency of AE and a better prognosis than those without IPAF in patients with IIP14,15,16,17. However, the relationship between details of autoimmune features and AE has not been well-known in patients with IIP including both IPAF and non-IPAF.
In this prospective study, we comprehensively examined 74 autoimmune features during IIP diagnosis and evaluated their relationship with the incidence and prognosis of AE-IIP in patients with IIP. To the best of our knowledge, this is the first study to demonstrate a detailed association between autoimmune features and AE-IIP.
Results
Clinical features of IIP at diagnosis
Two hundreds and twenty-six patients with IIP, who had visited or been referred to respiratory departments, were prospectively and consecutively enrolled (Supplementary Figure S1). Four patients were excluded from the study, and 222 patients with IIP were included. The clinical characteristics and lung physiology of all the patients are shown in Table 1. The median age at diagnosis of IIP was 71 years, 159 (71.6%) were male, and the median percentage predicted forced vital capacity (%FVC) was maintained (84.1%). The median observation period was 36 months. Of the 222 patients with IIP, 83 (37.4%) patients had IPF, 14 (6.3%) had cryptogenic organizing pneumonia (COP), 9 (4.1%) had nonspecific interstitial pneumonia (NSIP), 17 (7.7%) had NSIP with organizing pneumonia (OP) overlap, and 71 (32.0%) had unclassifiable IIP16.
Incidence of AE-IIP and mortality
During the observation period, 34 patients (15.3%) experienced AE of IIP. The incidence rate of AE at 1, 2, 3, 4, and 5 years were 6.5%, 10.1%, 13.6%, 18.8%, and 18.8%, respectively (Fig. 1A). The median observation period before the onset of AE was 20.5 months. During the observation period, 66 patients (29.7%) died; the most common cause of death was AE-IIP (36.4%) (Fig. 1B). Patients with AE had significantly worse survival rates than those without AE (Fig. 1C, p < 0.001). Furthermore, AE was significantly associated with worse survival even after adjusting for age, sex, and %FVC (HR: 4.466, 95%CI: 2.651–7.524, p < 0.001). The proportion of each IIP subtype in patients who experienced AE was as follows IPF (32.3%), NSIP (5.9%), NSIP with OP overlap (11.8%), pleuroparenchymal fibroelastosis (PPFE) (2.9%), smoking-related interstitial lung disease (SR-ILD) (11.8%), and unclassifiable IIP (41.2%) (Fig. 1D). There was no significant difference in the proportion of IIP subtypes between patients who experienced AE and those who did not (Fig. 1D, p = 0.502). The %FVC and percentage predicted carbon monoxide diffusion lung capacity (%DLCO) at the time of IIP diagnosis were significantly lower in patients with AE than in those without AE (Table 1; median: 69.3% vs. 85.8%, p = 0.001 and 66.2% vs. 69.3%, p = 0.006, respectively).
Cumulative incidence of acute exacerbation (AE), survival curves, causes of death in patients with idiopathic interstitial pneumonia (IIP). The incidence rates of AE-IIP (A) at 1, 2, 3, 4, and 5 years after the initial diagnosis of IIP were 6.5%, 10.1%, 13.6%, 18.8%, and 18.8%, respectively. The most common cause of death was AE-IIP (36.4%) (B). Kaplan-Meier curves of survival in patients with and without AE-IIP show that the mortality rate was significantly lower in patients who experienced AE-IIP (p < 0.001) (C). There is no significant difference in the proportion of IIP subtypes between patients with and without AE-IIP (D). AE, acute exacerbation; IIP, idiopathic interstitial pneumonia; IPF, idiopathic pulmonary fibrosis; IPAF, interstitial pneumonia with autoimmune symptoms; NSIP, nonspecific interstitial pneumonia; COP, cryptogenic organizing pneumonia; SR-ILD, smoking-related interstitial lung disease; PPFE, pleuroparenchymal fibroelastosis; NSIP with OP, nonspecific interstitial pneumonia with organizing pneumonia; AIP, acute interstitial pneumonia.
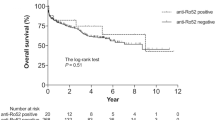
Risk factors for AE-IIP
The clinical characteristics at diagnosis, serum data, autoantibodies, and physiological characteristics were used to analyze the risk factors for the development of AE-IIP. In univariate analysis, %FVC (less than 84.1%; HR 2.324, p = 0.019, q = 0.050, divided by median value), Krebs von den Lungen-6 (KL-6, HR 1.000, p = 0.025, q = 0.060), and surfactant protein-D (SP-D, HR 1.001, p = 0.029, q = 0.063) were significantly associated with the development of AE before multiple testing correction, but these associations did not remain statistically significant after false discovery rate (FDR) adjustment (Supplementary Table E1). A trend toward association was still observed for these variables. Anti-cyclic citrullinated peptide (CCP) antibody positivity (positive, n = 9) was significantly associated with increased development of AE (HR 4.512, p = 0.005, q = 0.015). Presence of polymyositis/dermatomyositis (PM/DM)-(anti-aminoacyl tRNA synthetase (ARS) antibody [defined by enzyme-linked immunosorbent assay]: positive, n = 8; anti-Jo-1 antibody: positive, n = 1), systemic sclerosis (SSc)-related antibodies (anti-Scl70 antibody: positive, n = 3, anti-centromere antibody: positive, n = 5; anti-ribonucleoprotein (RNP) antibody: positive, n = 4; anti-RNA polymerase III antibody: positive, n = 2), or antinuclear antibodies (ANA) ≥ 320 (positive, n = 10) were significantly associated with the less development of AE (HR < 0.001, p < 0.001, q < 0.001), although estimates were unstable due to limited event numbers. A breakdown of the ANA staining patterns is shown Supplementary Figure S2. The Kaplan-Meier curves of the cumulative incidence of AE for each factor are shown in Fig. 2. The incidence of AE was significantly higher in patients with a lower %FVC or in those positive for anti-CCP antibodies (Fig. 2A, p = 0.019 and Fig. 2D, p = 0.006, respectively). The incidence of AE was lower in patients positive for PM/DM-, SSc-related antibodies, or ANA ≥ 320 (Fig. 2E, p = 0.019). Patients with a higher %DLCO or those meeting the IPAF criteria tended to have a lower incidence of AE-IIP (Fig. 2B, p = 0.116 and Fig. 2C, p = 0.218, respectively). Multivariate fine and gray competing risk regression models for the incidence of AE adjusted for age, sex, and %FVC are shown in Table 2. In these models, anti-CCP antibody positivity was a significant positive risk factor (hazard ratio [HR] 4.407, p = 0.004, q = 0.027), and PM/DM-, SSc-related antibody positivity, or ANA ≥ 320 (HR < 0.001, p < 0.001, q < 0.001) were significant negative risk factors for the development of AE-IIP. In addition, the change in %FVC at one year (HR 0.965, p = 0.003, q = 0.027) was a significant factor in the development of AE-IIP. Other autoantibodies or symptoms/findings suggestive of CTD were not significant factors for the incidence of AE (Table 2 and Supplementary Table E1).
Kaplan-Meier curves of incidence of acute exacerbation of idiopathic interstitial pneumonia (AE-IIP). The incidence of AE was significantly higher in patients with lower %FVC (A, p = 0.019; divided by the median value) and in those positive for anti-CCP antibody (D), (p = 0.006). The incidence of AE was lower in patients positive for PM/DM- or SSc-related antibodies, or ANA ≥ 320 (E, (p = 0.019). Patients with higher %DLCO (B), (p = 0.116) or those meeting IPAF criteria (C), p = 0.218) tended to have lower incidence of AE-IIP. The p-values were determined using Gray’s test. PM/DM- and SSc-related antibodies included anti-ARS antibody, anti-Jo-1 antibody, anti-Scl70 antibody, anti-RNP antibody, anti-RNA polymerase III antibody, and anti-centromere antibody. FVC, forced vital capacity; AE, acute exacerbation; IIP, idiopathic interstitial pneumonia; ANA, antinuclear antibody; CCP, cyclic citrullinated peptide; ARS, aminoacyl tRNA synthetase; PM/DM, polymyositis/dermatomyositis; SSc, systemic sclerosis; DLCO, carbon monoxide diffusion lung capacity.
Predictive model for the incidence of AE-IIP and survival
Finally, we analyzed these factors related to the incidence of AE-IIP based on the decision tree to develop a novel predicting model for the incidence of AE-IIP (Fig. 3A). The risk grades were divided into four groups, namely low, moderate, high, and very high. This model clearly distinguished patients with IIP with different developmental risks for AE-IIP at the initial diagnosis of IIP (Fig. 3B; Gray test, p < 0.001). Time-dependent receiver operating characteristic (ROC) analysis was performed by treating the risk groups as an ordinal variable (1 = low, 2 = moderate, 3 = high, 4 = very high). The time-dependent positive predictive values (PPVs) in 5 years showed good stratification: 0.0% for the low-risk group, 20.7% for moderate, 35.8% for high, and 62.2% for very high, respectively. These results were consistent with the trends in the cumulative incidence shown in Fig. 3B. The time-dependent area under the curve (AUC) was 78.1% at 1 year, 72.0% at 3 years, and 73.9% at 5 years, indicating good discriminative performance of the model at all time points (Supplementary Figure S3). Furthermore, these severity groups were associated with survival from the diagnoses of IIP (Fig. 3C; log-rank test, p < 0.001). The 5-year survival rates in each grade were 88.4% for low-risk, 70.1% for moderate-risk, 47.9% for high-risk, and 29.2% for very high-risk groups. Although patients with low risk of AE-IIP received more immunosuppressive treatment compared to those in other risk groups (Supplenentary Table E2), neither immunosuppressive nor antifibrotic treatment before AE-IIP was significantly associated with the development of AE-IIP in the multivariate competing risk regression models adjusted for age, sex, and %FVC (Table 2). The severity grading system for AE-IIP was a significant prognostic factor in the Cox proportional hazards model (HR 2.289, p < 0.001, C-index = 0.666).
Predictive model for the incidence of acute exacerbation of idiopathic interstitial pneumonia (AE-IIP). A decision tree for predicting AE incidence after the initial diagnosis of IIP was constructed by recursive partitioning (A). The partitioning process was completed when the study cohort was divided into four groups, namely low, moderate, high, and very high risk. PM/DM- and SSc-related antibodies included anti-ARS antibody, anti-Jo-1 antibody, anti-Scl70 antibody, anti-RNP antibody, anti-RNA polymerase III antibody, and anti-centromere antibody. Cumulative incidence of AE-IIP classified by the decision tree (B): blue line for low-risk group, green line for moderate-risk group, orange line for high-risk group, and red line for very high-risk group (p < 0.001). Kaplan-Meier curve of survival in each group by a predictive model for AE-IIP (C). FVC, forced vital capacity; AE, acute exacerbation; IIP, idiopathic interstitial pneumonia; ANA, antinuclear antibody; CCP, cyclic citrullinated peptide; ARS, aminoacyl tRNA synthetase; PM/DM, polymyositis/dermatomyositis; SSc, systemic sclerosis.
Discussion
This post-hoc analysis of a multicenter prospective cohort study on IIP16which comprehensively checked 74 autoimmune features including autoantibodies at the diagnosis of IIP, showed detailed relationships between autoimmune features and incidence and prognosis of patients with AE-IIP. Patients with IIP were older and predominantly male compared to typical patients with CTD. The incidence of AE-IIP was significantly higher in patients positive for anti-CCP antibodies or in those with lower %FVC. In addition, the incidence of AE-IIP was significantly lower in patients positive for PM/DM- or SSc-related antibodies or those with ANA ≥ 320. Furthermore, a novel predictive model for the incidence of AE-IIP, consisting of an anti-CCP antibody, PM/DM- or SSc-related antibodies, ANA, and %FVC at the diagnosis of IIP, could predict the future risks of AE-IIP. To the best of our knowledge, this is the first study to show a detailed association of autoimmune features with AE-IIP that is closely related to a worse prognosis in patients with IIP.
AE-ILD leads to a devastating condition, which is associated with a poor survival, and AE-IPF accounts for 40% of deaths in patients with IPF18. AE-ILD frequently occurs in patients with IPF, especially in the late stage with low %FVC10,19,20. AE-CTD-ILD also occurs, and its prognosis is poor similar to that of AE-IPF13,21. However, the incidence of AE-ILD is higher in patients with IPF than in those with CTD-ILD21. In addition, the occurrence of AE-ILD is frequent in the advanced stages of IPF, but sometimes occurs even in the early stages of CTD-ILD13. This information will be useful for managing patients with IIP or CTD-ILD in clinical practice.
In patients with ILD associated with systemic autoimmune diseases, the proportion of AE-ILD was higher in those with rheumatoid arthritis (RA) than in those with other CTD-ILDs21. The number of patients with AE-RA-ILD was highest, accounting for 68% of those with AE-CTD-ILD21. Furthermore, in patients with RA-ILD, AE-RA-ILD accounts for 34.4% of the cause of death22. Therefore, information regarding the presence of anti-CCP antibodies may be important for predicting AE-ILD in clinical practice. On the other hand, patients with PM/DM-ILD frequently show acute/subacute onset, although cases of AE-PM/DM-ILD are rare in clinical practice21,23,24. Therefore, the presence of PM/DM-associated antibodies may be related to a lower incidence of AE-IIP. Frequencies and predictive factors of AE-SSc-ILD have not yet been fully elucidated. In terms of anti-SS-A antibody, which is a marker of Sjögren’s Syndrome, anti-SS-A antibody is also associated with dermatomyositis and has a high affinity for ILD. Furthermore, anti-SS-A antibody is frequently found both in patients with IIP15,16 and in the general Japanese population25. Patients with adolescent myositis with anti-SS-A antibody are more likely to develop ILD, have more severe disease, and have a worse prognosis26. However, in the present study, presence of anti-SS-A antibody was not a significant predictive factor of AE-IIP. This information should be helpful for the management of patients with IIP in clinical practice.
Regarding the impact of medications on the occurrence of AE-ILD, administration of the antifibrotic agent nintedanib was associated with a decreased incidence of AE-IPF11. Furthermore, nintedanib was tended to reduce the development rate of AE-ILD in patients with autoimmune disease-related progressive fibrosing ILD27. In contrast, immunosuppressive therapy, including corticosteroids and azathioprine, was associated with an increased rate of AE-IPF28. Therefore, attention to AE-IIP may be required when administering strong immunosuppressive therapy to patients with a low %FVC and anti-CCP antibodies. In the preent study, although patients with low risk of AE-IIP received more immunosuppressive treatment compared to those in other risk groups, neither immunosuppressive nor antifibrotic treatment before AE-IIP was significantly associated with the development of AE-IIP in the multivariate competing risk regression models.
The current study has several limitations. First, the number of patients with AE-IIP was relatively small and we did not have a validation cohort. Second, the treatments for IIPs were not uniform. Finally, the current study was a post hoc analysis of a prospective multicenter cohort study, and clinical data at the time of AE-IIP onset were not available. Therefore, larger studies with a uniform treatment regimen are required to validate these findings in the future.
In conclusion, this study analyzed the effects of CTD features on the incidence of AE-IIP. The incidence of AE-IIP was significantly higher in patients positive for anti-CCP antibodies or in those with lower %FVC. Furthermore, the incidence of AE-IIP was significantly lower in patients positive for PM/DM- or SSc-related antibodies or in those with ANA ≥ 320. In addition, we developed a novel predictive model for the incidence of AE-IIP that consists of an anti-CCP antibody, PM/DM- or SSc-related antibodies, ANA, and %FVC at the time of IIP diagnosis. This model could predict the future risk of AE-IIP. These results provide important information for the management of patients with IIP, and predicting the risk of AE-IIP, which is closely related to a poor prognosis, will be helpful in clinical practice.
Methods
Study design and participants
This was a post hoc analysis of a prospective and multicenter cohort study (PAIR-2 cohort study)16. In our previous study, we prospectively enrolled and followed consecutive patients with IIP aged 15 years or older who visited or were referred to respiratory departments from 2015 to 2022 16. All diagnoses of IPF and other IIPs were made in accordance with the 2011 international guidelines for IPF29the 2013 international statement for IIPs30. At diagnosis, we collected chest HRCT scans and serum samples and evaluated lung histopathological specimens from surgical lung biopsies, when performed. The IIP was diagnosed through multidisciplinary discussions (MDD) involving expert pulmonologists, radiologists, and pathologists. Additionally, detailed radiological and pathological findings were independently assessed by two pulmonary radiologists (HS and HS) and two pulmonary pathologists (MK and HT). Systemic autoimmune diseases were excluded based on the criteria outlined in the previous study16. The condition and survival status of the enrolled patients were monitored annually. The study protocol was approved by the Ethics Committee of Hamamatsu University School of Medicine (approval number: E14-123) and the study was registered in the University Hospital Medical Information Network (UMIN) System (http://www.umin.ac.jp/, ID: UMIN000015370). This study was conducted in accordance with the approved protocol and tenets of the the 1964 Declaration of Helsinki, as amended. Informed consent was obtained from all the patients.
Data collection and evaluation of CTD-related features
Clinical data were collected at the time of IIP diagnosis. Acute, subacute, and chronic IIPs were defined as follows by the duration from the onset of respiratory symptoms to diagnosis: less than 1 month for acute, 1–3 months for subacute, and 3 months or more for chronic. At the time of diagnosis, 74 autoimmune features related to CTD, including arthritis, skin rash, and autoantibodies, were systematically evaluated according to the “Checklists for detecting CTD-related features”16in collaboration with specialists from various fields.
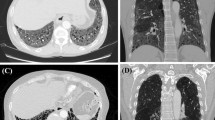
Diagnosis of AE-IIP
The definition of AE-IIP included: (1) previous or concurrent diagnosis of IIP, (2) acute worsening or development of dyspnoea typically < 1 month in duration; (3) computed tomography (CT) with new bilateral ground-glass opacity and/or consolidation superimposed on background findings of IIP, and (4) deterioration not fully explained by cardiac failure or fluid overload. AE-IIP was diagnosed by attending doctors on site.
Statistical analysis
Statistical analyses were performed using JMP 13.1.0 (SAS Institute Inc., Cary, NC, USA), R version 4.4.2 and EZR 1.51 31. The following R packages were used: cmprsk (version 2.2–12; Gray B, 2024)32qvalue (version 2.38.0; Storey JD et al., 2024)33and survival (version 3.8-3; Therneau TM, 2024). Categorical data were compared using Fisher’s exact probability test for independence and continuous data were analyzed using the Mann–Whitney U test. The time to the first AE-IIP and overall survival were measured from the time of IIP diagnosis. The overall survival of patients was estimated using the Kaplan–Meier method, and the curves were compared using the log-rank test. Gray’s test was used to analyze the time to the first AE-IIP. Unadjusted and adjusted analyses were performed using the Fine-Gray proportional hazards models to identify the risk factors for AE-IIP. Death before AE was treated as a competing risk event. Thereafter, hazard ratios (HRs), 95% confidence intervals (CIs) and p-values were calculated. Clinically relevant and important variables were selected for the multivariate analysis from among the statistically significant covariates in the univariate analysis. For multiple testing correction, q-values were calculated using Storey’s q-value method33 applied to all candidate variables. Statistical significance was defined as q-value < 0.05. All other statistical tests were two-sided, and statistical significance was set at p < 0.05. The AE incidence prediction model was based on recursive partitioning to create decision trees. The identified factors of AE incidence, such as percentage predicted forced vital capacity (%FVC), presence of anti-cyclic citrullinated peptide (CCP) antibodies, and presence of polymyositis/dermatomyositis (PM/DM)- or systemic sclerosis (SSc)-related antibodies, and high titers (≥ 320) of antinuclear antibodies (ANA), were determined as candidate variables for partitioning. PM/DM- or SSc-related antibodies include anti-aminoacyl tRNA synthetase (ARS) antibody, anti-Jo-1 antibody, anti-Scl70 antibody, anti-ribonucleoprotein (RNP) antibody, anti-RNA polymerase III antibody, and anti-centromere antibody. The splitting process was terminated when the study cohort was split into four groups, low-, moderate-, high-, and very high-risk. To assess the predictive performance of the decision tree model, we performed time-dependent receiver operating characteristic (ROC) analysis using the timeROC package in R (version 0.4; Paul Blanche et al., 2019)34. This method accounts for right censoring and competing risks. Risk groups derived from the decision tree were treated as an ordinal variable (1 = low, 2 = moderate, 3 = high, 4 = very high), and were used as the marker variable to calculate the time-dependent AUC and PPV at 1, 3, and 5 years. Discriminative performance of the model was assessed using the concordance statistics (C-indices).
Data availability
The raw data collected in this study are not publicly available because of informed consent restrictions but are available from the corresponding author on reasonable request.
References
Kim, D. S. Acute exacerbations in patients with idiopathic pulmonary fibrosis. Respir Res. 14, 86. https://doi.org/10.1186/1465-9921-14-86 (2013).
Kondoh, Y. et al. Risk factors of acute exacerbation of idiopathic pulmonary fibrosis. Sarcoidosis Vasc Diffuse Lung Dis. 27, 103–110 (2010).
Song, J. W., Hong, S. B., Lim, C. M., Koh, Y. & Kim, D. S. Acute exacerbation of idiopathic pulmonary fibrosis: incidence, risk factors and outcome. Eur. Respir J. 37, 356–363. https://doi.org/10.1183/09031936.00159709 (2011).
Suda, T. et al. Acute exacerbation of interstitial pneumonia associated with collagen vascular diseases. Respir Med. 103, 846–853. https://doi.org/10.1016/j.rmed.2008.12.019 (2009).
Enomoto, N. et al. Acute exacerbation of unclassifiable idiopathic interstitial pneumonia: comparison with idiopathic pulmonary fibrosis. Ther. Adv. Respir Dis. 14, 1753466620935774. https://doi.org/10.1177/1753466620935774 (2020).
Tachikawa, R. et al. Clinical features and outcome of acute exacerbation of interstitial pneumonia: collagen vascular diseases-related versus idiopathic. Respiration 83, 20–27. https://doi.org/10.1159/000329893 (2012).
Park, I. N. et al. Acute exacerbation of interstitial pneumonia other than idiopathic pulmonary fibrosis. Chest 132, 214–220. https://doi.org/10.1378/chest.07-0323 (2007).
Collard, H. R. et al. Acute exacerbation of idiopathic pulmonary fibrosis. An international working group report. Am. J. Respir Crit. Care Med. 194, 265–275. https://doi.org/10.1164/rccm.201604-0801CI (2016).
Leuschner, G. & Behr, J. Acute exacerbation in interstitial lung disease. Front. Med. (Lausanne). 4, 176. https://doi.org/10.3389/fmed.2017.00176 (2017).
Kim, D. S. et al. Acute exacerbation of idiopathic pulmonary fibrosis: frequency and clinical features. Eur. Respir J. 27, 143–150. https://doi.org/10.1183/09031936.06.00114004 (2006).
Collard, H. R. et al. Acute exacerbations in the INPULSIS trials of nintedanib in idiopathic pulmonary fibrosis. Eur. Respir J. 49 https://doi.org/10.1183/13993003.01339-2016 (2017).
Enomoto, N. Relationship between idiopathic interstitial pneumonias (IIPs) and connective tissue disease-related interstitial lung disease (CTD-ILD): A narrative review. Respir Investig. 62, 465–480. https://doi.org/10.1016/j.resinv.2024.03.006 (2024).
Enomoto, N. et al. Differences in clinical features of acute exacerbation between connective tissue disease-associated interstitial pneumonia and idiopathic pulmonary fibrosis. Chronic Resp. Dis. 16 https://doi.org/10.1177/1479972318809476 (2018).
Fischer, A. et al. An official European respiratory society/american thoracic society research statement: interstitial pneumonia with autoimmune features. Eur. Respir J. 46, 976–987. https://doi.org/10.1183/13993003.00150-2015 (2015).
Enomoto, N. et al. Prospective nationwide multicentre cohort study of the clinical significance of autoimmune features in idiopathic interstitial pneumonias. Thorax 77, 143–153. https://doi.org/10.1136/thoraxjnl-2020-216263 (2022).
Enomoto, N. et al. Radiological and histopathological features and treatment response by subtypes of interstitial pneumonia with autoimmune features: A prospective, multicentre cohort study. Respir Med. 224, 107577. https://doi.org/10.1016/j.rmed.2024.107577 (2024).
Oldham, J. M. et al. Characterisation of patients with interstitial pneumonia with autoimmune features. Eur. Respir J. 47, 1767–1775. https://doi.org/10.1183/13993003.01565-2015 (2016).
Natsuizaka, M. et al. Epidemiologic survey of Japanese patients with idiopathic pulmonary fibrosis and investigation of ethnic differences. Am. J. Respir Crit. Care Med. 190, 773–779. https://doi.org/10.1164/rccm.201403-0566OC (2014).
Collard, H. R. et al. Acute exacerbations of idiopathic pulmonary fibrosis. Am. J. Respir Crit. Care Med. 176, 636–643. https://doi.org/10.1164/rccm.200703-463PP (2007).
Homma, S., Sugino, K. & Sakamoto, S. Usefulness of a disease severity staging classification system for IPF in japan: 20 years of experience from empirical evidence to randomized control trial enrollment. Respir Investig. 53, 7–12. https://doi.org/10.1016/j.resinv.2014.08.003 (2015).
Enomoto, N. et al. Frequency, proportion of PF-ILD, and prognostic factors in patients with acute exacerbation of ILD related to systemic autoimmune diseases. BMC Pulm Med. 22, 387. https://doi.org/10.1186/s12890-022-02197-3 (2022).
Otsuka, J. et al. Clinical features of acute exacerbation in rheumatoid arthritis-associated interstitial lung disease: comparison with idiopathic pulmonary fibrosis. Respir Med. 200, 106898. https://doi.org/10.1016/j.rmed.2022.106898 (2022).
Suda, T. et al. Interstitial lung diseases associated with amyopathic dermatomyositis. Eur. Respir J. 28, 1005–1012. https://doi.org/10.1183/09031936.06.00038806 (2006).
Fujisawa, T. et al. Differences in clinical features and prognosis of interstitial lung diseases between polymyositis and dermatomyositis. J. Rhuematol. 32, 58–64 (2005).
Hayashi, N. et al. Prevalence of disease-specific antinuclear antibodies in general population: estimates from annual physical examinations of residents of a small town over a 5-year period. Mod. Rheumatol. 18, 153–160. https://doi.org/10.3109/s10165-008-0028-1 (2008).
Sabbagh, S. et al. Anti-Ro52 autoantibodies are associated with interstitial lung disease and more severe disease in patients with juvenile myositis. Ann. Rheum. Dis. 78, 988–995. https://doi.org/10.1136/annrheumdis-2018-215004 (2019).
Matteson, E. L. et al. Nintedanib in patients with autoimmune Disease-Related progressive fibrosing interstitial lung diseases: subgroup analysis of the INBUILD trial. Arthritis Rheumatol. 74, 1039–1047. https://doi.org/10.1002/art.42075 (2022).
Raghu, G., Anstrom, K. J., King, T. E. Jr., Lasky, J. A. & Martinez, F. J. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl. J. Med. 366, 1968–1977. https://doi.org/10.1056/NEJMoa1113354 (2012).
Raghu, G. et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am. J. Respir Crit. Care Med. 183, 788–824. https://doi.org/10.1164/rccm.2009-040GL (2011).
Travis, W. D. et al. An official American thoracic society/european respiratory society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am. J. Respir Crit. Care Med. 188, 733–748. https://doi.org/10.1164/rccm.201308-1483ST (2013).
Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 48, 452–458. https://doi.org/10.1038/bmt.2012.244 (2013).
Fine, J. P., Gray, R. J. & and A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94, 496–509. https://doi.org/10.1080/01621459.1999.10474144 (1999).
Storey, J. D. & Tibshirani, R. Statistical significance for genomewide studies. Proc. Natl. Acad. Sci. U S A. 100, 9440–9445. https://doi.org/10.1073/pnas.1530509100 (2003).
Blanche, P., Dartigues, J. F. & Jacqmin-Gadda, H. Estimating and comparing time-dependent areas under receiver operating characteristic curves for censored event times with competing risks. Stat. Med. 32, 5381–5397. https://doi.org/10.1002/sim.5958 (2013).
Acknowledgements
This study was assisted by the Japanese Respiratory Society, the Study Group on Diffuse Lung Disease, and the Scientific Research/Research on Intractable Diseases in the Ministry of Health, Labour and Welfare of Japan. We would like to thank Editage (www.editage.jp) for English language editing.
Author information
Authors and Affiliations
Contributions
SY, NE, and TS contributed to the study conceptualization, NE and TS project administration, and funding acquisition. SY, NE, SN, YM, AF, YT, HN, YA, YI, HY, MK, YS, HH, KF, MT, MK, SI, MF, TA, NK, KY, HM, YK, MS, KM, MM, TF, NI, and YN contributed to the data curation. SY, NE, KM, HS, HS, MK, KT, and NO analyzed and interpreted the data. SY, NE, YN, HS, HS, MK, KT, NO, and TS contributed to critical revision for important intellectual content. SY, NE, SN, YM, AF, YT, HN, YA, YI, HY, MK, YS, HH, KF, MT, MK, SI, MF, TA, NK, KY, HM, YK, MS, KM, MM, TF, NI, YN, HS, HS, MK, KT, NO, and TS approved the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Competing interests
Noriyuki Enomoto has received grants from Boehringer Ingelheim Co., Ltd. The other authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yazawa, S., Enomoto, N., Nakai, S. et al. Risk stratification of acute exacerbations by autoantibodies in patients with idiopathic interstitial pneumonia. Sci Rep 15, 35623 (2025). https://doi.org/10.1038/s41598-025-19487-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-19487-5