Abstract
This study aimed to evaluate and compare the fracture load and fracture mode of three-unit implant-supported fixed dental prostheses (ISFDPs) fabricated from polyetheretherketone (PEEK), composite, and zirconia, using two prosthetic designs: a bilateral cantilever supported by a single central implant (T-bridge) and a conventional two-implant-supported configuration (C-bridge). In this preclinical in vitro study, Straumann tissue-level regular implant analogs were embedded in Paladur resin and fitted with SN Variobase® abutments. Five restorative materials, PMMA-based polymer, resin composite, PEEK, 5 mol% yttria-stabilized zirconia (5Y-TZP), and 3 mol% yttria-stabilized zirconia (3Y-TZP), were used to fabricate standardized ISFDPs. Specimens were luted and subjected to vertical loading until failure using a universal testing machine. Fracture load, fracture mode, and abutment deformation were recorded and analyzed. 3Y-TZP exhibited the highest median fracture load (T-bridge: 5108 N [IQR: 1415]; C-bridge: 6572 N [IQR: 2438]). C-bridges consistently showed significantly higher fracture resistance than T-bridges. PEEK demonstrated no visible fractures and minimal deformation, indicating a distinct mechanical behavior. Significant differences in fracture patterns were found across materials, with zirconia and PEEK performing most favorably. 3Y-TZP zirconia provides the highest fracture resistance. While C-bridges provided superior mechanical performance, T-bridges with appropriate materials such as PEEK or 3Y-TZP show clinically acceptable strength. Absence of fatigue and long-term aging limits direct clinical extrapolation. T-bridge configurations may offer a less invasive alternative when C-bridges are not feasible, provided that high-performance materials are selected. Further validation through long-term and clinical studies is recommended.
Similar content being viewed by others
Introduction
With the increased demand for dental implants, innovative implant-supported fixed dental prostheses (ISFDPs) concepts to replace missing teeth in partially edentulous patients are emerging, challenging traditional methods1,2. Recent advancements include smaller implant sizes and the strategic implementation of cantilevers to maximize support, which support structures at one end (mesial or distal)3,4,5. With the latter approach, a single implant can bear the pontic component, beneficial in scenarios with limited space or financial constraints6,7.
Despite short cantilevered implant-supported prostheses, particularly unilateral designs, have been reported to induce higher bending moments and stress concentrations on supporting implants, leading to increased risk of mechanical complications and crestal bone loss1,6,7,8,9, are an accepted treatment modality in Europe. The concept of using bilateral cantilevers on a single central implant to support a three-unit implant-supported fixed dental prosthesis (ISFDP) is novel, and only two recent studies have explored this configuration to understand these mechanical stresses1,9, yet systematic evaluation of fracture resistance across multiple restorative materials remains limited.
Traditionally, a 3-unit ISFDP requires at least two implants. In contrast, bilateral cantilevers on a single central implant could reduce surgical interventions and optimize prosthetic distribution, offering a practical solution in cases with limited bone volume or financial constraints. Indeed, each prosthetic method has distinct surgical and prosthetic implications, indications and limitations. Two-implant approaches might necessitate additional procedures such as sinus lifts or bone grafts, increasing costs and patient morbidity. Conversely, the T-bridge method might present challenges in maintaining biomechanical stability when subjected to occlusal forces, potentially impacting long-term outcomes. However, the T-bridge design may offer valuable clinical advantages in select cases. These include posterior regions with limited bone volume or proximity to anatomical structures (e.g., maxillary sinus, inferior alveolar nerve), patients with financial limitations precluding multiple implants, or situations requiring minimally invasive treatment. In such scenarios, avoiding extensive augmentation procedures and reducing surgical time may justify the use of a bilateral cantilever configuration. Nevertheless, the biomechanical demands of this design necessitate careful case selection and evaluation of material behavior under load. In this context, the choice of prosthetic material is key. Modern materials like milled composite, zirconia, and polyetheretherketone (PEEK) influence the mechanical behavior of different bridge designs. In the studied context, preliminary research has indicated substantial differences in fracture resistance between experimental (T-bridge) and control (two-implant-supported bridge) polymer samples, indicating that research should use other materials to provide more mechanical stability and clinical utility for the T-bridge design10. Another recent study assessed the mechanical durability of monolithic zirconia implant-supported T-bridge compared to traditional bridges using Roxolid Tissue level and TLX implants, finding that conventional designs are generally preferable regardless of implant type, while the T-bridge design also performed well, however, with significant differences in fracture loads based on reconstruction design11.
New implant bridge materials are typically compared in scenarios with two implant-retainers and one central pontic or one lateral cantilever. However, the novel concept of a T-bridge design requires further investigations and comparisons with conventional implant-bridges. Therefore, this study aimed to investigate and compare the fracture load and fracture mode of 3-unit ISFDPs made of PEEK, composite, as well as 3 mol% yttria- (3Y-TZP) and 5 mol% yttria-stabilized tetragonal zirconia polycrystal (5Y-TZP) materials, supported by one implant with a T-bridge design, a configuration scarcely reported in current literature10,11, versus those supported by two implants in conventional implant-bridge configurations. The null hypothesis tested posits that the fracture load and fracture mode of these 3-unit ISFDPs will not differ significantly between these designs.
Materials and methods
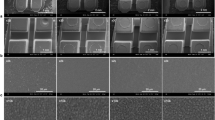
Tissue level implant analogues with a 4.1 mm diameter (Straumann) were embedded in resin (Paladur, Pala). The corresponding SN Variobase® (Straumann) abutments for Crown AS (Ø 5.1 mm, AH 4 mm, TAN, including screw) were individually mounted with a torque of 35 Ncm. Five different materials for the ISFDPs were tested: PMMA polymer (CAD-Temp, VITA Zahnfabrik, LotNo: 94600), resin composite (Telio CAD, Ivoclar, LotNo: YB5W2M), PEEK (breCAM BioHPP, Bredent, LotNo: 504894), 5Y-TZP ceramic (Ceramill Zolid FX, AmannGirrbach, LotNo: LotNo: 1909002), and 3Y-TZP ceramic (Ceramill ZI, AmannGirrbach, 1702000 and 200200) (Table 1). The sample size for each group (n = 10) was chosen based on prior in vitro studies evaluating fracture resistance in ISFDPs11. For construction of the standardized final bridges, digital impressions were obtained with a scanning device (Primescan AC, Dentsply Sirona) and machined with a milling machine (CEREC MC X5, Dentsply Sirona). All specimens were produced under identical parameters to minimize variability.
All zirconia FDPs were polished to a high gloss/luster for clinical use to a high with special polishing paste (Dental Direkt) and the composite ISFDPs with brushes and polishing pastes (Acrypol and Abraso Starglanz, Bredent). Before placement, abutments were air-abraded using alumina powder with the mean particle size of 50 μm ( ALOX-2, Benzer Dental AG) in a sandblaster (KaVo EWL 5423, Kaltbach & Voigt) and then luted with a self-curing cement (Multilink Hybrid Abutment HO 0, Ivoclar Vivadent). All specimens were then subjected to 24 h of incubation at 37 °C. PEEK restorations were finished with fine-grit diamond burs under water-cooling and polished using a dedicated PEEK paste to achieve a smooth, lustrous surface. PMMA restorations were sequentially finished with 400–1200 grit silicon carbide papers under wet conditions and polished with an acrylic-specific paste to produce a clinically smooth, homogeneous surface.
Fracture load was evaluated using a universal testing machine (Zwick 1445, ZwickRoell), applying vertical force at a rate of 10 mm/min until a force cut-off threshold of 50% was reached. Although this rate exceeds physiological masticatory speeds, it was selected in accordance with ISO 14801 standards to simulate worst-case, static loading conditions in the absence of fatigue cycling. To minimize stress singularities and provide uniform stress distribution, a custom-designed three-point antagonist made of Cobalt-Chromium-Molybdenum (CoCrMo) was employed. This antagonist featured symmetrical contact geometry to exert equal force on each unit of the 3-unit ISFDPs (Fig. 1). The prototype was initially milled from wax (DD camWAX, Dental Direkt) and subsequently cast using a Co-Cr-Mo alloy (PX C62, PX Dental SA) through a centrifugal casting process in a PX Dental Silvercast Induction casting machine (PX Dental SA). This approach enabled a controlled, standardized application of force and facilitated reliable fracture mode analysis across groups.
Experimental setups for in vitro study of implant-supported fixed dental prostheses (ISFDPs). (A) (left), two-implant supported 3-unit ISFDP (C-bridge). (B) (right), one-implant supported 3-unit ISFDP (T-bridge). These configurations were used to compare mechanical performance and fracture behavior across different materials.
For the transition to the abutment, fracture types are classified as ‘complete’ (full detachment), ‘incomplete’ (partial retention of prosthetic components on the abutment or separation of fragments), and ‘none’ (no visible fracture). Fracture scores were assigned as follows: a score of 0 indicates no visible fracture, while a score of 1 denotes an incomplete fracture, characterized by partial separation without full detachment of the prosthetic components (Fig. 2). A complete fracture is when the prosthesis fully detaches or debonds from the underlying structure.
Abutment deformation was assessed using a binary scoring system (0 = none, 1 = visible deformation). This simple method provides reproducible evaluation of structural changes under load. The scoring was based on in-house protocols and mechanical rationale; thus, no published reference exists.
Data coding and documentation were performed using Microsoft Excel (version 2202, Build 16.0.14931.20806). Statistical analyses were conducted using an online statistics calculator (DATAtab Team, 2024). The normality of continuous data distributions was assessed with the Kolmogorov–Smirnov and Shapiro–Wilk tests, both of which indicated significant deviation from normality. Consequently, non-parametric statistical tests were used. Descriptive statistics are presented as median values and interquartile ranges (IQR) to appropriately summarize central tendency and variability in non-normally distributed data. Within-group comparisons of fracture load were performed using the Friedman test, the non-parametric equivalent of repeated-measures ANOVA, suitable for comparing matched or dependent observations across multiple conditions. Between-group comparisons were analyzed using the Mann–Whitney U test, appropriate for independent samples with non-normal distributions. Fracture mode, a categorical ordinal variable, was analyzed using the Kruskal–Wallis test, which compares ranks across multiple independent groups. Abutment deformation modes, treated as categorical data, were assessed using Chi-square, McNemar, and Fisher’s exact tests, chosen according to sample size, paired or unpaired design, and expected frequencies, ensuring valid inference even for small or unbalanced datasets. To control for type I error arising from multiple pairwise comparisons, the Dunn–Bonferroni correction was applied. The threshold for statistical significance was set at α = 0.05.
Results
Results of the mechanical properties including fracture load, fracture mode and abutment deformation using different materials under investigation are presented in Tables 2 and 3 as well as in Figs. 2 and 3, and 4.
T-Bridge design
Significant variation in median fracture load was observed among the tested materials (Table 2; Fig. 2). 3Y-TZP ceramic exhibited the highest median fracture load (5108 N), followed by 5Y-TZP ceramic (2960 N; p < 0.001) and PEEK (2333 N; p = 0.001). Resin composite and PMMA-based polymer showed considerably lower median fracture loads of 1771 N and 1250 N, respectively (p < 0.001).
The fracture modes also varied among the materials. PEEK exhibited no fracture pattern, with a median fracture mode of 0.0, significantly different from the other materials, all of which had a median fracture mode of 2.0, except PMMA-based polymer, which had a median fracture mode of 1.5.
Regarding deformation, there were also clear differences noticeable: PEEK, 5Y-TZP ceramic, and 3Y-TZP ceramic showed no deformation, while resin composite deformed in all cases. PMMA-based polymer had mixed results, however, with no deformation occurring in 9 out of 10 cases. The statistical analysis indicated significant differences between the materials, particularly between PMMA-based polymer and the other materials, as well as between PEEK and resin composite (p < 0.001).
C-Bridge design
The median fracture load also varied among the different materials tested (Table 3; Fig. 3). Again, 3Y-TZP ceramic exhibited the highest median fracture load (6572 N), followed by resin composite with an intermediate fracture load of 4025 N. PMMA-based polymer had the lowest median fracture load (2602 N), which was statistically significantly different from the ceramic materials (5Y-TZP ceramic: p = 0.029; 3Y-TZP ceramic: p < 0.001).
The median fracture modes also varied across the materials. Both PMMA-based polymer and 3Y-TZP ceramic had a median fracture mode of 1, while 5Y-TZP ceramic showed no fracture mode with a median fracture mode of 0. Statistically significant differences were observed between 5Y-TZP ceramic and the other materials (p = 0.007).
Regarding deformation, notable differences between the materials were observed as well. PMMA-based polymer exhibited deformation in all cases, while 5Y-TZP and 3Y-TZP ceramics showed mixed results. Specifically, 5Y-TZP ceramic no deformation in 4 out of 10 cases, and 3Y-TZP ceramic had no deformation in 3 out of 10 cases.
Comparison between the two Bridge designs
Figure 1 visualizes the comparison between the T- and C-Bridge designs. The C-Bridge significantly improved the fracture load capacity for all tested materials compared to the T-Bridge design, indicating superior mechanical performance (Fig. 4). Specifically, PMMA-based polymer’s fracture load increased from 1250 N to 2602 N (p < 0.001), resin composite’s from 1771 N to 4025 N (p = 0.023), and 3Y-TZP ceramic’s from 5108 N to 6572 N (p = 0.089). However, the latter statistical difference was only borderline and therefore can be interpreted only as a trend. In contrast, the robustness of 3Y-TZP ceramic was again corroborated.
Discussion
This study aimed to compare the fracture load and respective mode of 3-unit ISFDPs using two distinct configurations, i.e. the T-bridge (one implant with bilateral cantilevers) and the C-bridge (two implants with a pontic in the middle). The materials tested included two composites, a PEEK and two zirconia materials. The present findings rejected the null hypothesis and indicated significant differences in the mechanical performance between the two designs, with the C-bridge consistently demonstrating superior fracture load capacity.
3Y-TZP ceramic displayed the highest median fracture load across both bridge configurations, followed by 5Y-TZP ceramic and PEEK. This aligns with previous findings, which reported high flexural strength and fracture toughness for zirconia materials12,13. The current results further indicated that the C-bridge design significantly increased the fracture load capacity for all tested materials compared to the T-bridge design, corroborating the superior mechanical performance of the classical two-implant configuration10,11. Therefore, the prosthetic configuration significantly impacts the mechanical performance of the ISFDPs. The C-bridge design distributes load across two implants and may therefore result in higher fracture loads and more favorable fracture patterns. Regarding cantilevers, Chong et al.14 reported that cantilever designs on multiple implants demonstrate also better load-bearing capacity. Moreover, the study by Roccuzzo et al.15 supported the clinical viability of implant-supported cantilever extensions, further validating the present results. However, unilateral cantilever only was used15. The existing literature and the current results stress the fact that whenever possible, optimal distribution of implants should be strived for, however (especially on more than one implant), cantilevers could be a valuable option.
PEEK exhibited a distinct failure profile, characterized by an absence of visible fractures and minimal deformation. This behavior likely stems from its low elastic modulus and high ductility, which permit effective stress distribution and energy dissipation under load. Unlike brittle materials such as zirconia, PEEK’s ability to undergo elastic deformation without catastrophic failure may account for its favorable failure mode, despite recording lower absolute fracture loads. This property positions PEEK as a promising option in scenarios where resilience and fail-safe performance are prioritized over maximal strength. It is important to note that the present data are derived solely from an in vitro setting. Unlike the study by Molinero-Mourelle et al.11 which included a comprehensive chewing simulation with 1,200,000 cycles to mimic 5 years of clinical use, the current study did not incorporate an aging protocol. This limits the ability to predict long-term clinical performance. Future studies should integrate such protocols to provide more robust data on the durability and longevity of different prosthetic designs.
The results of this study suggest that the C-bridge design remains the gold standard and offers superior mechanical performance compared to the T-bridge design indicating that clinicians should still consider the C-bridge design the best durability and stability in clinical applications whenever possible. The concept of using bilateral cantilevers on a single central implant (T-design) for three-unit ISFDPs represents a progressive and debatable concept but appears at the same time clinically feasible especially in cases where a less-invasive, cost-effective alternative to conventional treatments is desired. Noteworthy, the importance of implant diameter, length, position, occlusal scheme, and bone remodeling to ensure stability and prevent complications should be also highlighted in this context10. But in general, the T-bridge shows acceptable in vitro fracture resistance, suggesting at least a practical potential. In the context of the present study focusing on mechanical resistance, the key question remains, whether comparison of designs and comparing quantitative outcomes is enough to make clinical conclusions and recommendations. Of course, every material will break or bend under critical loads; the main question is if these loads are clinically relevant and of certain clinical indications can profit from lower-performing designs and would still work. Therefore, one should also consider clinical conditions and chewing forces. Cantilever prostheses have been associated with increased mechanical stresses on implants and surrounding bone, particularly in unilateral configurations. While this study focused on bilateral cantilever T-bridges, the clinical relevance of stress distribution on implants and peri-implant bone requires further investigation in vivo. Considering not just stresses but also judging the reliability or survival probability of designs and materials is extremely importance16. If applied forces (N) are correlated with the probability of failure, we get an S-type curve with probabilities of fracture failures (Pf) increasing as the load increases. At F = 285 N, the predicted fast fracture Pf accounts to 9e-6 and then increases to 0.998 at F = 950 N; at 500 N, the Pf value is still very low with a predicted value of 4.08e−3. When looking at the classical literature, the average maximum masticatory force for cantilever fixed dental prostheses in the posterior region is approximately 300 N17,18. Even if we add the so-called safety factor of 200 N, we are still well under 1000 N. Since all groups on the present study exhibited mean fracture loads exceeding 1000 N, we might assume that they could all resist to conventional and even more excessive chewing conditions. But again, higher resistance remains a desirable goal to predictably achieve. To facilitate clinical interpretation, a summary of the mechanical performance and clinical implications of each design/material combination is presented in Table 4.
This study compared two prosthetic designs across multiple restorative materials under controlled in vitro conditions, providing mechanical behavior data. Vertical loading with a multi-contact antagonist and controlled contact geometry minimized stress singularities, approximating clinical occlusal forces. Notwithstanding these strengths, several limitations warrant consideration. The experimental setup simulated vertical loading exclusively, without reproducing the lateral and oblique forces present in the oral environment. Testing was conducted immediately post-fabrication under static conditions, without thermomechanical aging, water storage, or cyclic fatigue, thereby representing a “best-case” mechanical scenario rather than long-term clinical performance. The in vitro nature of the study further limits direct extrapolation to patient outcomes.
Future investigations should incorporate multi-directional loading, thermomechanical cycling, and fatigue testing, coupled with quantitative metrics of abutment deformation (e.g., angular displacement, linear deviation) to enhance biomechanical characterization. Clinical studies are essential to validate the durability, safety, and functional relevance of these prosthetic configurations. While C-bridges remain the benchmark for mechanical stability, T-bridges may offer a clinically viable alternative in carefully selected cases, provided appropriate restorative materials are employed.
Conclusion
Under vertically applied forces, conventional C-bridges demonstrated superior mechanical performance compared to T-bridges. While T-bridges exhibited lower fracture resistance, all tested materials exceeded typical posterior masticatory forces, indicating potential clinical applicability in selected cases with careful planning. The findings show that three-unit ISFDPs supported by a single central implant can achieve sufficient mechanical stability in vitro. Material selection and cantilever design critically influence fracture behavior: rigid materials such as zirconia provide higher fracture resistance, whereas more resilient materials like PEEK offer favorable deformation capacity with reduced risk of catastrophic failure. Clinically, T-bridge configurations may serve as a viable alternative to conventional C-bridges in scenarios with anatomical or economic constraints, provided occlusal load, material properties, and abutment design are carefully considered. The absence of thermomechanical aging and fatigue simulation limits direct extrapolation to long-term clinical performance; thus, future studies should incorporate fatigue testing, aging protocols, and clinical evaluations to guide evidence-based prosthetic planning for minimally invasive implant-supported rehabilitations.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Lulic, M. et al. Ante’s (1926) law revisited: a systematic review on survival rates and complications of fixed dental prostheses (FDPs) on severely reduced periodontal tissue support. Clin. Oral. Implants Res. 18, 63–72 (2007).
Ghanem, H., Afrashtehfar, K. I., Abi-Nader, S. & Tamimi, F. Impact of a TED-style presentation on potential patients’ willingness to accept dental implant therapy: a one-group, pre-test post-test study. J. Adv. Prosthodont. 7, 437–445 (2015).
Dini, C. et al. Peri-implant and esthetic outcomes of cemented and screw-retained crowns using zirconia abutments in single implant-supported restorations - A systematic review and meta-analysis. Clin. Oral Implants Res. 32, 1143–1158 (2021).
Gamborena, I., Sasaki, Y. & Blatz, M. B. Predictable immediate implant placement and restoration in the esthetic zone. J. Esthet Restor. Dent. 33, 158–172 (2021).
Vargas-Moreno, V. F. et al. Clinical performance of short and extrashort dental implants with wide diameter: A systematic review with meta-analysis. J. Prosthet. Dent. 132, 1260e1–126013 (2024).
Ramanauskaite, A. & Sader, R. Esthetic complications in implant dentistry. Periodontol 2000. 88, 73–85 (2022).
Roccuzzo, A. et al. Implant-supported fixed dental prostheses with cantilever extensions: state of the Art and future perspectives. Int. J. Oral Implantol. 16, 13–28 (2023).
Crothers, A. J., Wassell, R. W., Jepson, N. & Thomason, J. M. The use of cantilever bridges. Dent. Update. 22, 190–198 (1995).
Freitas da Silva, E. V. et al. Does the presence of a cantilever influence the survival and success of partial Implant-Supported dental prostheses? Systematic review and meta-analysis. Int. J. Oral Maxillofac. Implants. 33, 815–823 (2018).
Afrashtehfar, K. I., Stawarczyk, B., Micovic Soldatovic, D. & Schmidlin, P. R. A proof of concept on implant-supported bilateral cantilever bridges: the T-Bridge approach. Swiss Dent. J. 134, 1–17 (2024).
Molinero-Mourelle, P. et al. Load bearing capacity of 3-unit screw-retained implant-supported fixed dental prostheses with a mesial and distal cantilever on a single implant: A comparative in vitro study. J. Mech. Behav. Biomed. Mater. 151, 106395 (2024).
Stawarczyk, B. et al. Three generations of zirconia: from veneered to monolithic. Quintessence Int. 48, 441–450 (2017).
Lümkemann, N., Pfefferle, R., Jerman, E., Sener, B. & Stawarczyk, B. Translucency, flexural strength, fracture toughness, fracture load of 3-unit FDPs, Martens hardness parameter and grain size of 3Y-TZP materials. Dent. Mater. 36, 838–845 (2020).
Chong, K. K., Palamara, J., Wong, R. H. & Judge, R. B. Fracture force of cantilevered zirconia frameworks: an in vitro study. J. Prosthet. Dent. 112, 849–856 (2014).
Roccuzzo, A. et al. Clinical and radiographic outcomes of implant-supported fixed dental prostheses with cantilever extension: A proof-of-principle study with a follow-up of at least 1 year. Clin. Oral Implants Res. 34, 1073–1082 (2023).
Jadaan, O., Esquivel-Upshaw, J., Nemeth, N. N. & Baker, E. Proof testing to improve the reliability and lifetime of ceramic dental prostheses. Dent. Mater. 39, 227–234 (2023).
Körber, K. H. Maximum masticatory force as a calculation factor of dental constructions. Dent. Lab. 31, 55–60 (1983).
Lundgren, D. & Laurell, L. Occlusal force pattern during chewing and biting in dentitions restored with fixed bridges of cross-arch extension. I. Bilateral end abutments. J. Oral Rehabil. 13, 57–71 (1986).
Funding
Open access funding provided by University of Zurich. The authors state that no financial support, grants, or funding of any kind were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
K.I.A.: Methodology, formal analysis, project administration, writing-original draft, writing-review and editing. B.S.: Methodology, validation, resources, supervision, writing-review and editing. A.W.: Investigation, data curation, writing-review and editing. D.M.S.: Data curation, resources, investigation. J.M.B.G.: Investigation, writing-review and editing. A.G.: Formal analysis, visualization, writing-review and editing. P.R.S.: Conceptualization, project administration, supervision, writing-review and editing. Each author contributed significantly to the completion of this work. The authors declare no competing financial interests that could have influenced the outcomes of this research.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Not applicable. No ethical approval was required according to the Ethics Committee of the University of Zurich after consultation.
Informed consent
No participants were involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Afrashtehfar, K.I., Stawarczyk, B., Wähli, A. et al. Effects of restorative material on the mechanical performance of three-unit implant-supported fixed dental prostheses with bilateral cantilevers: an in vitro study. Sci Rep 15, 35757 (2025). https://doi.org/10.1038/s41598-025-22671-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-22671-2