Abstract
Bladder cancer often recurs, necessitating innovative treatments to reduce recurrence. We investigated non-thermal plasma’s potential as a novel anti-cancer therapy, focusing on plasma-activated solution (PAS), created by exposing saline to non-thermal plasma. Our study aims to elucidate the biological effects of PAS on bladder cancer cell lines in vitro, as well as the combination with mitomycin C (MMC), using clinically relevant settings. PAS treatment exerts a potent cytotoxic effect through the production of intracellular reactive oxygen species, resulting in DNA damage and subsequent induction of G1 cell cycle arrest/senescence. This is induced via upregulation of cell cycle checkpoint signalling and DNA damage repair pathways using LC-M/MS-based phospho-proteomics. Importantly, combining PAS with MMC reveals a synergistic effect (Combination Index of 0.59–0.67), suggesting the potential of utilizing PAS in combination therapies. Our findings demonstrate PAS’s mode of action and suggest its potential as a promising treatment for bladder cancer, warranting further clinical studies.
Similar content being viewed by others
Introduction
Bladder cancer is recognized as the tenth most prevalent cancer worldwide, with over 550,000 new cases diagnosed annually1. Non-muscle invasive bladder cancer (NMIBC) represents the most common subtype, accounting for approximately 70% of all bladder cancer cases2. Although initial treatments such as transurethral resection of the tumor (TURT) and mitomycin C (MMC) treatment can be effective, recurrence rates in NMIBC remain high, necessitating the exploration of novel and more effective therapeutic strategies3,4. Because MMC treatment is given via intravesical high local dose, this provides opportunities to improve therapy with effective novel local therapies.
Non-thermal plasma (ionized gas) treatment, in particularly the application of plasma-activated fluids such as plasma-activated solution (PAS), has emerged as a promising potential treatment option5,6,7,8,9,10. PAS is generated by exposing a solution, such as phosphate-buffered saline (PBS), to a non-thermal plasma beam created by plasma jets or dielectric barrier discharge devices. Non-thermal plasma, consists of charged particles, neutral species, radicals, and photons11. When PBS is irradiated with non-thermal plasma, these particles dissolve in the solution, conferring biological activity. The main reactive species found in PAS include reactive oxygen species (ROS) and reactive nitrogen species (RNS), hydrogen peroxide, superoxide anion, hypochlorite (ClO), singlet oxygen, nitrate, nitrite, and nitric oxide12,13.
Plasma as anti-cancer therapeutic option has demonstrated efficacy in inducing cell death in various cancer cell lines5,6,7,8,9,10,14,15,16,17,18,19,20,21,22,23,24,25. In addition, non-thermal plasma has been studied in head and neck cancer patients in a small clinical study, and demonstrated great efficacy26. For bladder cancer, it was demonstrated that plasma was effective in a cell line, in a xenografted tumor, and in 2 high grade bladder cancer cell lines6,8,9. However, its potential application in bladder cancer treatment using a clinical applicable method and its combination with MMC, have yet to be investigated. Considering that PAS can easily be combined with MMC-treatment, it holds promise for reducing the risk of tumor recurrence. The working mechanism of PAS is however scarcely studied. The reaction species formed suggest DNA damaging activity and protein changes. Therefore, the aim of this study was to evaluate the anti-cancer mechanisms of PAS on bladder cancer cells through LC–MS/MS-based phospho-proteomics analysis and cell cycle analysis, and to test whether a combination with MMC is more effective.
Results
Optimising PAS production and storage
To assess the cytotoxic potential of PAS, we evaluated its production and storage stability. H2O2 and NOx are commonly measured species in plasma-treated solutions as indicators of treatment efficacy13,27,28. We tested both long and short distance exposure of the plasma beam in PBS (Fig. 1A) and found no significant difference in the levels of reactive species (Fig. 1B). Next, we investigated the effect of PAS generated at both distances on cell growth using the SRB assay. Consistently, both long and short distance PAS showed similar growth inhibitory effects (Fig. 1C). Based on these findings, we selected long-distance PAS for all subsequent experiments due to its ease of application.
Effect of PAS on cell cytotoxicity. (A) Schematic overview of PAS exposure of long and short distance. (B) Effect of short/long distance PAS on formed reactive species in PBS. (C) Effect of short/long distance PAS on cellular cytotoxicity. (D) Effect of short-term storage time on PAS stability. (E) Effect of long-term storage of PAS on its stability. ***p < 0001, nd, not-detectable. (F) Comparison of PAS vs H2O2 on cellular cytotoxicity. ***p < 0001 (G) IC50 after PAS-exposure to different (precursor) HNSCC cell lines, datapoints show an average of triplicate measurements (H) Effect of 20% PAS on the mitochondrial membrane potential. (I) Effect of PAS on intracellular ROS formation. All datapoints show an average of 3 independent experiments, significance is shown across all timepoints of the graph compared to the 0 h timepoint.
To study the efficacy of PAS after storage, generated PAS was produced and stored at different temperatures. Even though the levels of the species showed some variation due to the visual readout of test strips, no significant decrease in the three species was observed during short-term storage at different temperatures or distances (Fig. 1D). H2O2 showed a 50% drop almost immediately after its production and remained at subsequent stable concentration. Considering that lower temperatures generally enhance stability, PAS was stored at − 80 °C immediately after production for all subsequent experiments.
To test whether long term storage at − 80 °C had any influence, we also tested whether a 3-year storage had any effect on species levels and cytotoxicity. The inhibitory concentration where 50% of cell growth is inhibited (IC50) of PAS increased by 1.8-fold for both RT112 and T24 after 3 years of storage at − 80 °C, suggesting a decrease in PAS effectiveness (data not shown). In agreement to that, the levels of H2O2, NO3− decreased by approximately 50%, and NO2− was undetectable (Fig. 1E). Consequently, to ensure the quality of PAS, short-term storage was employed.
Hydogen peroxide (H2O2) was the most abundant reactive species that we measured. To examine whether the cytotoxicity of PAS is solely related to H2O2 formation, the cytotoxicity of PAS was compared to a similar concentration H2O2. Importantly, PAS has a greater cytotoxicity that H2O2 alone (Fig. 1F), indicating that other formed products contribute to the cytotoxicity of PAS. As previously shown by others, primary heatlhy cells (HUVECs) were not sensitive to PAS exposure, in which 100% PAS did not reach the IC50 (Fig. 1G). In addition, the IC50 was also determined for a panel of cancer and precursors cell lines of primary and immortalized head and neck squamous cancer (HNSCC). Interesgtingly, precursor HNSCC cell lines were highly senstive to PAS treatment, while 2 immortalized primary HNSCC cancer cell lines showed significant lower sensitivity to PAS. These data further demontstarate its potential use for treatment against (percursor) HNSCC (Fig. 1G).
Previous studies showed that plasma may activate the mitochondrial membrane potential, and ROS formation, however we observed a non-significant change in the membrane potential for both RT112, and T24, though there was a small decrease in the potential in RT112 cells after 100% PAS exposure (Fig. 1H). ROS was produced in both cell lines at similar levels with the higest concentration after 4 h, which decreased 24 h after PAS exposure (Fig. 1I).
PAS induces DNA damage-response and cell cycle arrest
To determine whether cells arrested in a specific cell cycle-phase, we performed FACS analysis on cell cycle. Exposure to PAS lead to a decrease of the number of cells in the S and G2-M-phase, and an increase in the G1 phase, indicative of cell cycle arrest induction (Fig. 2A). In addition, we see an upregulation of p21-protein levels using Western blotting, a protein involved in cell cycle arrest (Fig. 2B). ROS formation frequently leads to the induction of DNA damage, therefore we measured DNA damage by the formation УH2Ax-foci using (Fig. 2C). DNA damage is highly induced directly after 1 h PAS exposure. Upon removal of the PAS, the formed УH2Ax foci increased, which is may be related to a accumulation of DNA damage by ROS and the induction of double stranded DNA damage which needs longer to be repaired. In conclusion, the findings indicate that PAS treatment leads to the induction of DNA damage, and subsequent arrest of cells in the G1 phase of the cell cycle.
Effect of PAS on cell cycle and DNA damage. (A) Effect of 1 h of 20% PAS on cell cycle distribution, *p < 0.05; **p < 0.01. (B) Effect of 20% PAS on p21 induction and its quantification. *p < 0.05. All datapoints show an average of 3 independent experiments. (C) Effect of 20% PAS on the formation of yH2Ax foci using fluorescence microscopy. The foci intensity was quantified and corrected for the number of nuclei per image. *p < 0.05. All datapoints show an average of 3 independent experiments.
To analyze the level of cell death, the sub-G1-fraction of the FACS-analyses was determined. However, cell death was hardly induced up to 72 h after PAS exposure (Fig. 3A). To see if cell cycle inhibition was related to senescence, we performed clonogenic cell survival, and observed that less than 10% of the cells were vital (e.g. capable of proliferation) after PAS exposure (Fig. 3B). Cleavage of caspase 3 and cathepsin B shows very low levels (hence minor activation) using Western blotting, which agrees with the findings of FACS (Fig. 3C).
Effect of PAS on cell death and phosphoproteome. (A) Effect of 1 h of 20% PAS exposure on the induction of cell death. (B) The effect of 1 h 20% PAS exposure on clonogenic cell survival. *p < 0.05; **p < 0.01. (C) Western blot of cleaved caspase 3 and cleaved cathepsin B after 1 h 20% PAS exposure and its quantification. *p < 0.05. All datapoints show an average of 3 independent experiments. (D) Supervised heatmap (p < 0.05) of phosphopeptides measured using LC–MS/MS based proteomics, 1 h after 20% PAS exposure. (E) Inka-ratio, calculated by dividing the Inka score of PAS treated cells vs untreated cells, showing an increased in various cell cycle related kinases. (F) String-network of significantly (p < 0.05) up and downregulated phosphoproteins. All datapoints show an average of 3 independent experiments.
To further in-depth assess the immediate impact of PAS exposure on the changes in cellular protein-signaling, the phospho-proteome was measured using LC–MS/MS-based phospho-proteomics. Because 1 h PAS exposure led to the highest levels of MAPK-phosphorylation, this time-point was selected for the phospho-proteomics measurement (Supplementary Fig. S1). In total 14,162 phospho-sites were identified, belonging to 3602 proteins, of which 828 significantly deregulated (P < 0.05) (Fig. 3D and Supplementary Table S1). Of these proteins, 359 proteins had upregulated phospho-sites (total 517 sites detected), and 469 proteins that had downregulated phospho-sites (of in total 617 sites). Proteins involved in DNA-damage/repair, cell cycle checkpoints, and RNA processing were changed (Fig. 3E,F and Supplementary Fig. S1). Mostly the altered biological processes were related to cell cycle arrest, mediated by activation of the G1 checkpoints. Inka analyses of the most changed kinase-activity showed activation of several cell cycle (checkpoint) related proteins (Fig. 3E,F). These observations further underline the role of cell cycle arrest/senescence due to the induction of (double-stranded)-DNA damage as mechanism of action of the cytotoxicity induced by PAS.
Synergistic combination of PAS with mitomycin C
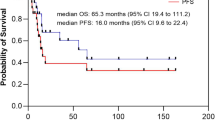
We investigated whether combination of PAS and MMC can potentiate their cytotoxic effect. Bladder cancer cells were exposed to PAS and MMC for 1 h. Since 10 and 20% of PAS was too toxic to eneable to measure a synergistic effect, we tested this on lower concentrations, 5% and 2.5% PAS. In both cell lines the combination of MMC with 5% PAS shows a highly synergistic effect, with a Combination index (CI) of of 0.67 and 0.59 for RT-112 and T24, respectively (Fig. 4). However, when cells were exposed to a lower concentratoin of PAS, the combination was additive (CI ~ 1.1) in both cell lines. A higher percentage of PAS is probably more effective for the induction of dsDNA damage, while too low PAS may not cause enough damage to induce its cytotoxicity. In conclusion, the combination of PAS with MMC can be synergistic at higher, clinical relevant, doses of PAS.
Discussion
This study demonstrates the significant cytotoxic effect of PAS on bladder cancer cells. PAS, generated by subjecting PBS to a non-thermal plasma beam, exerts its cytotoxicity through two main mechanisms. Firstly, it induces intracellular production of reactive oxygen species (ROS), leading to oxidative stress and DNA damage within the cancer cells. Secondly, PAS triggers the activation of cell cycle checkpoints and DNA repair, resulting in cell cycle arrest primarily in the G1 phase. The combination of PAS with MMC, a standard chemotherapy for bladder cancer, shows synergistic effects at clinically relevant doses. These findings underscore the potential clinical utility of combining PAS with existing treatments to enhance therapeutic outcomes in bladder cancer patients.
Previous studies have demonstrated the anticancer effects of direct plasma treatment, plasma-activated medium (PAM), and PAS in various cancer types25,29,30,31. Multiple investigations explored the stability of PAS and PAM across different temperatures based on the concentrations of H2O2, NO2−, or NO3−32,33,34,35. In our study, we observed the formation of these species within PAS and their intracellular ROS-inducing effects. However, due to limited data availability and variations in plasma devices and PAS production methods, consensus on optimal storage temperature and duration remains elusive. We found no significant decrease in H2O2, NO2−, or NO3− levels over a 14-day period across different storage temperatures, though longer storage times are not recommended as they may reduce ROS levels and efficacy. In clinical practice, chemotherapeutic agents or radioisotopes used in cancer treatment are typically produced either on-site at the hospital or at nearby facilities to ensure maximal potency and minimize degradation. Therefore, the observed decrease in PAS activity after three years of storage at − 80 °C is unlikely to pose a significant challenge in real-world applications.
The primary aim of our project was to investigate PAS as a potential treatment for bladder cancer and elucidate its cellular mechanisms of action. Our results indicate that PAS exhibits potent anticancer effects, with healthy primary cells (HUVECs) showing significantly lower sensitivity to PAS, suggesting a cancer-specific effect, consistent with previous reports9,10. While apoptosis induction via caspase 3 activation has been observed in other cancer cell lines10,24,36, our study in bladder cancer cells primarily implicates induction of cell cycle arrest or senescence rather than immediate cell death. Our phosphoproteomics data reveal dysregulation of cellular processes post-PAS exposure, notably activation of cell cycle checkpoints and downregulation of proteins involved in mitotic spindle formation, critical for early G1 phase inhibition observed in our cell lines37. Wang et al.23 performed gene expression analysis on HNSCC after exposing cells to the plasma beam directly, where an increase in MAPK and MTOR and in cell cycle (KEGG-pathways), without any enrichment for apoptotic pathways.
The observed G1 cell cycle arrest likely results from DNA damage that activated a range of kinases, including CHEK2, RAD9A, PRKDC, MAPKs, and MTOR. Phosphorylation of these key proteins signals the cell to pause its cycle and target downstream proteins involved in DNA damage response, chromatin remodeling, and metabolic pathways. The most significantly affected proteins in our data are closely related to cell cycle regulation (RPS6KB2, MTOR, CHEK2, MAPK3, MAPK14) and microtubule formation (GSK3A/B and BRSK2). In addition, RSF1 may induce G1 arrest by modulating chromatin architecture. Nuclear proteins like CHEK2, NBN, POU2F1, PRKDC, RAD9A, SMARCAD, TRRAP, ATAD2, FIGNL1 regulate DNA-damage repair mechanisms, including double stranded DNA damage repair, nonhomologous end joining, while POU2F1 may attenuate DNA-damage induced cell death38. All these processes may contribute to the halting of the cell cycle. Further research is needed to elucidate the specific molecular and cellular processes that are induced in different cell bladder cancer cell types, including clinical tissues. Furthermore, it is important to identify the reactive species involved in the activation of these pathways. A deeper understanding of the dynamics between these species, their interactions with cellular targets, and the downstream signalling cascades they trigger could provide valuable insights.
The combination of PAS with MMC, which induces DNA damage through DNA crosslinks, highlights a synergistic interaction capable of causing irreparable DNA damage through ROS formation and additional DNA damage induction. This synergistic effect suggests the potential of PAS as a novel therapeutic option against bladder cancer, aiming to reduce recurrence rates associated with MMC treatment alone.
Furthermore, our study extends beyond bladder cancer, demonstrating the activity of non-thermal plasma against precursor head and neck squamous cell carcinoma (HNSCC). Previous clinical and in vitro studies have shown PAS efficacy against HNSCC, supporting its clinical potential in treating cancers amenable to non-thermal plasma therapy23,26.
In summary, our findings underscore the promising therapeutic potential of PAS as an innovative approach for bladder cancer treatment. The cytotoxic effects of PAS, mediated through ROS-induced DNA damage and cell cycle arrest, along with its synergistic interaction with MMC, provide a strong rationale for further investigation and clinical development of PAS-based therapies in oncology.
Methods
Cell culture and chemicals
RT112 and T24 bladder cancer cells (ATCC) were cultured as monolayers in RPMI 1640 (Gibco; Thermo Fisher Scientific, Waltham, USA) with 10% heat-inactivated fetal bovine serum (Biowest#S181H-500, VWR, Amsterdam, Netherlands) in 25 cm2 flasks (Greiner Bio-One, Frickenhausen, Germany). The FaDu cell line (ATCC) and UM-SCC-22A (gift from Thom Carey PhD, Ann Arbor, Michigan) were cultured in DMEM with 5% FBS. VU-preSCC-M3, VU-preSCC-LP67-F (Fibroblasts), and VU-preSCC-LP67-K (Keratinocytes) were primary cell cultures. Keratinocytes were grown in Keratinocyte Growth Medium, and fibroblasts in DMEM for head and neck squamous cell carcinoma lines. VU-SCC-1131 and VU-SCC-OE cell lines were generated from tumor biopsies39. The head and neck cancer cell lines were cultured in DMEM with 5% FBS (Lonza #12–708). VU-pre-SCC-M3 and VU-preSCC-LPk were cultured in Lonza™ KGM™ Gold Keratinocyte Growth Medium BulletKit™ (#192060). HUVECs, kindly provided by Dr. J. van Beijnum. HUVECs were cultured in RPMI 1640 with 10% FBS, 10% human serum, and 1% pen/strep. Cells were maintained at 37 °C in a humidified atmosphere with 5% CO2. Mitomycin C was dissolved in DMSO to a stock solution of 15 mg/ml, aliquoted, and stored at − 20 °C.
Plasma activated solution (PAS)
PAS was created by exposing 5 ml PBS to a plasma beam for 5 min, using a plasma jet (kINPen 09, Neoplas tool GmbH, Germany). The applied voltage frequency was 1 MHz, modulated at 5 kHz to reduce gas temperature. Argon was used as the carrier gas. The plasma beam was held at either a long distance (beam tip just contacting PBS) or a short distance (beam immersed in PBS until color changed from blue to white–blue) (Fig. 2A). Unless specified otherwise, long distance PAS was used for experiments. PAS was used fresh (within 1 h of production) or stored at − 80 °C. For storage, PAS was made in 30–45 ml batches, frozen in 1.5 and 2 ml aliquots. Some PAS batches were frozen long-term (~ 3 years) and tested for effectiveness.
Quantification of hydrogen peroxide, nitrate, and nitrite in PAS
Directly after producing 5 ml of long and short distance PAS, aliquots of 0.5 ml were made and stored at room temperature, at 4 °C, or at − 80 °C. The H2O2, NO3−, NO2− concentrations were measured immediately, and after 1, 3, 7, and 14 days using test strips (Quantofix Peroxide 25/Nitrate and Nitrite, Macherey–Nagel, Düren, Germany, #91,319/#91,313).
Sulphorhodamine B (SRB)-assay
Cytotoxicity of PAS and/or MMC was determined using the SRB-assay, which was performed as described previously40,41. In brief, RT112 and T24 cells (1500–2000, respectively) were seeded in 96-wells plates. After 24 h, the medium was removed, and increasing concentrations of PAS, MMC or the combination was added for 1 h at 37 °C. Subsequently, the PAS/drugs were removed, and new medium was added to each well and cells were allowed to grow for another 72 h. Cells were precipitated with 25 µl cold 50% trichloroacetic acid (TCA), washed, stained with SRB, washed, and solubilized with Tris-buffer. The optical density (OD) was measured at 540 nm by a Biotek Synergy HT platereader (BioTek Instruments Inc.,Winooski, VT, USA). For some cell lines the CellTiter-Blue assay (Promega) was used as previously described42. Growth-inhibition curves were plotted based on the OD values, with the untreated controls set to 100%.
Global phosho-proteomics
T24 and RT112 bladder cancer cells were cultured in 14 cm petri dishes. At 80% confluency, 10 ml of 20% PAS or PBS was added. After 1 h, PAS/PBS was removed, plates were washed twice with 4 °C PBS, and lysed with 4 ml of urea lysis buffer (8 M urea/20 mM HEPES, pH 8, with 1 mM sodium orthovanadate, 2.5 mM sodium pyrophosphate, and 1 mM β-glycerophosphate). Samples were sonicated and centrifuged at 5400 × g for 10 min. 500 µg of protein was reduced with 5 mM DTT at 56 °C and alkylated with 10 mM IAA. Samples were digested with trypsin (1:100 ratio) overnight at 23 °C, acidified with TFA (1% final concentration), and centrifuged for 5 min at 4000 × g. Digests were desalted using Oasis HLB columns (30 mg) and eluted in 80% ACN/0.1% TFA to achieve a peptide concentration of 2 µg/µl. Samples were used for global phosphoproteomics on the BRAVO platform (Agilent) using Fe(III)-NTA cartridges and the Phospho Enrichment v2.0 protocol. Cartridges were primed with 100% ACN/0.1% TFA, equilibrated with 80% ACN/0.1% TFA, then samples (200 µg, 100 µl) were loaded and washed with 80% ACN/0.1% TFA. Phosphopeptides were eluted in 25 µl 5% NH4OH/30% ACN, transferred to glass-lined autosampler vials, and dried in a vacuum centrifuge at 45 °C. Phosphopeptides were dissolved in 20 µl 4% ACN/0.5% TFA before LC–MS injection.
Data acquisition by LC–MS/MS
Peptides were separated on an Ultimate 3000 nanoLC-MS/MS system (Dionex LCPackings, Amsterdam, The Netherlands) equipped with a 50-cm 75 μm ID C18 Acclaim pepmap column (Thermo Scientific). After injection, peptides were trapped at 3 μl/min on a 10-mm, 75-μm ID Acclaim Pepmap trap column (Thermo Scientific) in buffer A (buffer A:0.1% formic acid, buffer B: 80% ACN/0.1% formic acid), and separated at 300 nl/min with a 10–40% buffer B gradient in 90 min (120 min inject-to-inject). Eluting peptides were ionized at a potential of + 2 kV and introduced into a Q Exactive HF mass spectrometer (Thermo Fisher, Bremen, Germany). Intact masses were measured in the Orbitrap with a resolution of 120,000 (at m/z 200) using an automatic gain control (AGC) target value of 3 × 106 charges. Peptides with the top 15 highest signals (charge states 2 + and higher) were submitted to MS/MS in the higher-energy collision cell (1.6-Da isolation width, 25% normalized collision energy). MS/MS spectra were acquired in the Orbitrap with a resolution of 15 k (at m/z 200) using an AGC target value of 1 × 106 charges and an under-fill ratio of 0.1%. Dynamic exclusion was applied with a repeat count of 1 and an exclusion time of 30 s. Swissprot human reference proteome FASTA file (MaxQuant version 2.1.3.0) was used to identify the proteins present in the samples. The different variations that were allowed are Methionine oxidation, N-terminal acetylation and Cysteine carboxamidomethylation. Trypsin was selected as cutting enzyme and an FDR of 0.01 was used to statistically analyze the identified peptides and proteins. 4.5 ppm deviations were allowed for intact peptide ions and 20 ppm was allowed for fractured peptide ions, and a beta-binominal test was performed for statistical differences. Data is available in Supplementary Table S1.
Data analyses
StringDB v11.5 and Cytoscape v3.9.1 were used to create the different protein–protein interaction clusters, DAVID (https://david.ncifcrf.gov/) was used to determine Gene Ontology. MsigDB Molecular Signatures Database v7.5.1 was used for Gene Set Enrichment Analysis (GSEA). Integrative iNferred Kinase Activity (INKA) scores are calculated based on the phosphoproteomic measures as described previously (https://inkascore.org)43,44.
Flow cytometry measurement
About 200,000 RT112 and T24 cells/well were seeded in 6-well plates. After 24 h, the medium was replaced with 2 ml of 20% PAS (treated) or PBS (control). After 1 h, PAS/PBS was removed, fresh medium added, and cells were harvested at four time points: 24 h, 48 h, and 72 h for flow cytometry. Cells were trypsinized, resuspended in medium with dead cells, and centrifuged for 10 min at 500 × g. After removing the supernatant, 500 µl of propidium iodide (0.1 mg/ml) was added, and samples were measured using FACSscan (Becton Dickinson) with 20,000 events acquired. The subG1 peak indicated cell death.
Clonogenic assay
Cell survival was measured using a clonogenic assay as described previously41. Briefly, 100–5000 single cells/well were seeded in 6-well plates (Greiner). After 24 h, the medium was replaced with 1.5 ml PAS at increasing concentrations, while controls received 1.5 ml PBS. After 1 h, PAS was replaced with 2.5 ml fresh medium. Colonies were grown for 7–10 days, fixed with 2 ml 70% ethanol for 15 min, washed with PBS, and stained with 2 ml crystal violet for 5–10 min. Colonies with 50 or more cells were counted as 1 surviving cell. Surviving fractions were calculated as follows:
Mitochondrial membrane potential
The mitochondrial membrane potential (MMP) was measured using a JC-10 assay (Sigma-Aldrich, #MAK159). RT-112 (1500 cells/well) and T24 (2500 cells/well) were seeded. After 24 h, the medium was replaced with 100 µl PAS (0%, 10%, 20%, 50%, 100%) for 1 h. After PAS removal, 100 µl fresh medium was added. 24 h later, 50 µl JC-10 Dye Loading solution was added, and cells were incubated for 45 min at 37 °C. Then, 50 µl Assay Buffer B was added, and fluorescence intensity was measured at λex = 490/λem = 525 (green) and λex = 540/λem = 590 (red) nm using a Biotek Synergy HT plate reader (BioTek Instruments). The red/green fluorescence ratio determined the MMP as a ratio of the control.
Intracellular ROS concentration
The effect of 10% and 20% PAS on intracellular IC ROS production was analyzed using a fluorometric ROS kit (Sigma-Aldrich, #MAK143). Cells (1500 and 2500 cells/well) were incubated overnight. A Master Reaction Mix was prepared by mixing 4 µl stock solution with 2 ml assay buffer. After removing the medium, 58 µl medium and 100 µl Master Reaction Mix were added per well and incubated for 1 h. Then, 48 µl PAS was added per well, with PBS as the negative control. Fluorescence intensity was measured at λex = 490/λem = 525 nm after 10 min, 30 min, 1 h, 2 h, 4 h, and 24 h, and expressed as a ratio of the untreated control.
Western blotting
Western blot was performed as described previously41. The protein concentration of each sample was determined by the BCA Protein Assay Kit (Thermo Scientific, Rochford, USA, #23225). In brief, 20–45 ug/sample was loaded onto a 12% SDS-PAGE gel. Protein was blotted onto a PVDF-membrane membrane (Immobilon-P, Merck, Kenilworth, USA, #IPVH00010). Membranes were blocked in 5% BSA/PBS and subsequently exposed to anti-cleaved caspase 3, anti-cathepsin B and anti-P21, or anti-phospho-MAPK antibodies O/N at 4 °C (1:1000 in 5% BSA). Secondary antibodies (anti-mouse-HRP, and anti-rabbit-HRP) were incubated for 1 h at RT (1:4000). The proteins were visualized using SuperSignal WestPico Chemiluminescent substrate kit (#34077, Thermo Scientific) and read-out using the UVitec (Cambridge, UK). Membranes that were incubated with anti-p-MAPK, or P21 were exposed for 20 s to 1 min. Membranes that were incubated with anti-caspase 3 or anti-cathepsin B were exposed for 50 min. Full membranes are shown in Supplementary Fig. S2.
Immunofluorescent staining of DNA damage
Immunofluorescent staining of γH2Ax foci was performed as described previously45. Briefly, cells were treated with 20% PAS for 1 h. Cells were fixed in 4% formaldehyde immediately after treatment and 1 h after PAS removal. Membranes were permeabilized with Triton X-100, then blocked with 5% BSA/PBS for 20 min. Phosphorylated γH2Ax foci were stained with an anti-phosphorylated γH2Ax antibody (Ser139 #05-636, 1:1000; Upstate, Billerica, MA, USA) overnight at 4 °C. Cells were washed with PBS-Tween and exposed to anti-rabbit-Alexa Fluor-592. Foci were imaged using Leica confocal microscopy (SP8-X SMD, Leica, Mannheim, Germany). Images were processed and γH2Ax intensity quantified using ImageJ.
Combination analysis
Combination analysis was performed as described previously45. In brief, fraction affected was calculated from the SRB-growth inhibition curves. Calcusyn software (Biosoft, Cambridge, UK) was used to calculate the combination index (CI) between Mitomycin C and PAS. The CI was calculated from mutually non-exclusive calculations and averaged between the fraction affected values.
Statistical analysis
Statistical analyses of the in vitro cytotoxicity experiments are performed using the Student’s T-test. Spectral counts of global proteomics were normalized using the average of the sum of raw counts across all samples as previously described46,47. The group fold change of intensity phospho-proteomics data was calculated as exponentiation of the difference of the means of the two groups in log space. p-values < 0.05 were considered significant.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Wong, M. C. S. et al. The global epidemiology of bladder cancer: A joinpoint regression analysis of its incidence and mortality trends and projection. Sci. Rep. https://doi.org/10.1038/s41598-018-19199-z (2018).
Sylvester, R. J. et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: A combined analysis of 2596 patients from seven EORTC trials. Eur. Urol. 49, 466–477 (2006).
Bosschieter, J. et al. Value of an immediate intravesical instillation of mitomycin C in patients with non–muscle-invasive bladder cancer: A prospective multicentre randomised study in 2243 patients. Eur. Urol. 73, 226–232 (2018).
Yan, D., Sherman, J. H. & Keidar, M. Cold atmospheric plasma, a novel promising anti-cancer treatment modality. Oncotarget 8, 15977–15995 (2017).
Tavares-Da-silva, E. et al. Cold atmospheric plasma, a novel approach against bladder cancer, with higher sensitivity for the high-grade cell line. Biology (Basel) 10, 1–19 (2021).
Limanowski, R., Yan, D., Li, L. & Keidar, M. Preclinical cold atmospheric plasma cancer treatment. Cancers 14, 3461 (2022).
Mohades, S., Barekzi, N. & Laroussi, M. Efficacy of low temperature plasma against SCaBER cancer cells. Plasma Process. Polym. 11, 1150–1155 (2014).
Keidar, M. et al. Cold plasma selectivity and the possibility of a paradigm shift in cancer therapy. Br. J. Cancer 105, 1295–1301 (2011).
Nguyen, N. H., Park, H. J., Yang, S. S., Choi, K. S. & Lee, J. S. Anti-cancer efficacy of nonthermal plasma dissolved in a liquid, liquid plasma in heterogeneous cancer cells. Sci. Rep. https://doi.org/10.1038/srep29020 (2016).
Bekeschus, S. Medical gas plasma technology: Roadmap on cancer treatment and immunotherapy. Redox Biol. 65, 102798. https://doi.org/10.1016/j.redox.2023.102798 (2023).
Chauvin, J., Judée, F., Yousfi, M., Vicendo, P. & Merbahi, N. Analysis of reactive oxygen and nitrogen species generated in three liquid media by low temperature helium plasma jet. Sci. Rep. https://doi.org/10.1038/s41598-017-04650-4 (2017).
Tampieri, F., Gorbanev, Y. & Sardella, E. Plasma-treated liquids in medicine: Let’s get chemical. Plasma Process. Polym. 20, e2300077 (2023).
Kaushik, N., Kumar, N., Kim, C. H., Kaushik, N. K. & Choi, E. H. Dielectric barrier discharge plasma efficiently delivers an apoptotic response in human monocytic lymphoma. Plasma Process. Polym. 11, 1175–1187 (2014).
Panngom, K. et al. Preferential killing of human lung cancer cell lines with mitochondrial dysfunction by nonthermal dielectric barrier discharge plasma. Cell Death Dis 4, e642 (2013).
Guerrero-Preston, R. et al. Cold atmospheric plasma treatment selectively targets head and neck squamous cell carcinoma cells. Int. J. Mol. Med. 34, 941–946 (2014).
Zucker, S. N. et al. Preferential induction of apoptotic cell death in melanoma cells as compared with normal keratinocytes using a non-thermal plasma torch. Cancer Biol. Ther. 13, 1299–1306 (2012).
Iseki, S. et al. Selective killing of ovarian cancer cells through induction of apoptosis by nonequilibrium atmospheric pressure plasma. Appl. Phys. Lett. https://doi.org/10.1063/1.3694928 (2012).
Cheng, X. et al. The effect of tuning cold plasma composition on glioblastoma cell viability. PLoS One 9, e98652 (2014).
Mirpour, S. et al. The selective characterization of nonthermal atmospheric pressure plasma jet on treatment of human breast cancer and normal cells. IEEE Trans. Plasma Sci. 42, 315–322 (2014).
Torii, K. et al. Effectiveness of plasma treatment on gastric cancer cells. Gastric Cancer 18, 635–643 (2015).
Hirst, A. M. et al. Low-temperature plasma treatment induces DNA damage leading to necrotic cell death in primary prostate epithelial cells. Br. J. Cancer 112, 1536–1545 (2015).
Wang, Y. et al. Cold atmospheric plasma sensitizes head and neck cancer to chemotherapy and immune checkpoint blockade therapy. Redox Biol. 69, 102991 (2024).
Terefinko, D. et al. Comprehensive studies on the biological activities of human metastatic (MDA-MB-231) and non-metastatic (MCF-7) breast cancer cell lines, directly or combinedly treated using non-thermal plasma-based approaches. Toxicol. In Vitro 98, 105846 (2024).
Peng, S. et al. Synergism of non-thermal plasma and low concentration RSL3 triggers ferroptosis via promoting xCT lysosomal degradation through ROS/AMPK/mTOR axis in lung cancer cells. Cell Commun. Signal https://doi.org/10.1186/s12964-023-01382-z (2024).
Metelmann, H. R. et al. Clinical experience with cold plasma in the treatment of locally advanced head and neck cancer. Clin. Plasma Med. 9, 6–13 (2018).
Wende, K. et al. Identification of the biologically active liquid chemistry induced by a nonthermal atmospheric pressure plasma jet. Biointerphases 10, 029518 (2015).
Jablonowski, H., Santos Sousa, J., Weltmann, K. D., Wende, K. & Reuter, S. Quantification of the ozone and singlet delta oxygen produced in gas and liquid phases by a non-thermal atmospheric plasma with relevance for medical treatment. Sci. Rep. https://doi.org/10.1038/s41598-018-30483-w (2018).
Mohades, S., Laroussi, M., Sears, J., Barekzi, N. & Razavi, H. Evaluation of the effects of a plasma activated medium on cancer cells. Phys. Plasmas 22, 122001 (2015).
Van Boxem, W. et al. Anti-cancer capacity of plasma-treated PBS: effect of chemical composition on cancer cell cytotoxicity. Sci. Rep. 7, 16478 (2017).
Yan, D. et al. The specific vulnerabilities of cancer cells to the cold atmospheric plasma-stimulated solutions. Sci. Rep. 7, 4479 (2017).
Boehm, D., Heslin, C., Cullen, P. J. & Bourke, P. Cytotoxic and mutagenic potential of solutions exposed to cold atmospheric plasma. Sci. Rep. 6, 21464 (2016).
Yan, D. et al. Stabilizing the cold plasma-stimulated medium by regulating medium’s composition. Sci. Rep. 6, 26016 (2016).
Yan, D., Sherman, J. H. & Keidar, M. The application of the cold atmospheric plasma-activated solutions in cancer treatment. Anticancer Agents Med. Chem. 18, 769–775 (2018).
Judée, F. et al. Short and long time effects of low temperature plasma activated media on 3D multicellular tumor spheroids. Sci. Rep. 6, 21421 (2016).
Zhunussova, A. et al. Mitochondria-mediated anticancer effects of non-thermal atmospheric plasma. PLoS One 11, e0156818 (2016).
Kimura, M. et al. Mitotic catastrophe and cell death induced by depletion of centrosomal proteins. Cell Death Dis. 4, e603–e603 (2013).
Lin, J. et al. The POU2F1-ALDOA axis promotes the proliferation and chemoresistance of colon cancer cells by enhancing glycolysis and the pentose phosphate pathway activity. Oncogene 41, 1024–1039 (2022).
van Harten, A. M. et al. Characterization of a head and neck cancer-derived cell line panel confirms the distinct TP53-proficient copy number-silent subclass. Oral Oncol. 98, 53–61 (2019).
Bijnsdorp, I. V., Giovannetti, E. & Peters, G. J. Analysis of Drug Interactions. Methods in Molecular Biology vol. 731 (2011).
Bijnsdorp, I. V., Peters, G. J., Temmink, O. H., Fukushima, M. & Kruyt, F. A. Differential activation of cell death and autophagy results in an increased cytotoxic potential for trifluorothymidine compared to 5-fluorouracil in colon cancer cells. Int. J. Cancer 126, 2457–2468 (2010).
de Boer, D. V. et al. Targeting PLK1 as a novel chemopreventive approach to eradicate preneoplastic mucosal changes in the head and neck. Oncotarget 8, 97928 (2017).
Vallés-Martí, A. et al. Phosphoproteomics guides effective low-dose drug combinations against pancreatic ductal adenocarcinoma. Cell Rep. 42, 112581 (2023).
Beekhof, R. et al. INKA, an integrative data analysis pipeline for phosphoproteomic inference of active kinases. Mol. Syst. Biol. https://doi.org/10.15252/msb.20198981 (2019).
Bijnsdorp, I. V., Kruyt, F. A., Gokoel, S., Fukushima, M. & Peters, G. J. Synergistic interaction between trifluorothymidine and docetaxel is sequence dependent. Cancer Sci. 99, 2302–2308 (2008).
Pham, T. V., Henneman, A. A. & Jimenez, C. R. Iq: An R package to estimate relative protein abundances from ion quantification in DIA-MS-based proteomics. Bioinformatics 36, 2611–2613 (2020).
Pham, T. V., Piersma, S. R., Oudgenoeg, G. & Jimenez, C. R. Label-free mass spectrometry-based proteomics for biomarker discovery and validation. Exp. Rev. Mol. Diagn. 12, 343–359. https://doi.org/10.1586/erm.12.31 (2012).
Acknowledgements
This project received financial support from Kapitein Labs. AS would like to acknowledge the TU/e-UU-UMCU Alliance program. The work presented in this article is associated to COST Actions PlAgri CA19110 and PlasTHER CA20114. Cancer Center Amsterdam and Netherlands Organization for Scientific Research (NWO Middelgroot, #91116017) are acknowledged for support of the mass spectrometry infrastructure.
Author information
Authors and Affiliations
Contributions
JS and ZK investigation and Writing—Original Draft Preparation. AS conceptualization, Resources, Writing—Review and Editing. RB Resources, Writing—Review and Editing. MS investigation, TP Formal Analysis, SP investigation, AH formal analysis, TL investigation, RGH investigation, Writing—Review and Editing, RJvM conceptualization and Writing—Review and Editing, CJ conceptualization and Writing—Review and Editing, supervision, IB conceptualization, supervision, Writing—Original Draft Preparation, formal analysis, visualisation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Stoof, J., Kalmoua, Z., Sobota, A. et al. Non-thermal plasma as promising anti-cancer therapy against bladder cancer by inducing DNA damage and cell cycle arrest. Sci Rep 15, 2334 (2025). https://doi.org/10.1038/s41598-025-85568-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-85568-0
Keywords
This article is cited by
-
Cellular senescence in cancer: from mechanism paradoxes to precision therapeutics
Molecular Cancer (2025)
-
Molecular dynamics insights into the redox effects on PD-1/PD-L1 and PD-1/PD-L2 interactions
Scientific Reports (2025)