Abstract
Gossypol has demonstrated significant antimalarial activity against chloroquine-resistant and susceptible Plasmodium falciparum parasites. However, data on its potency in clinical isolates of P. falciparum remains limited. This study aimed to assess the potency of gossypol against six laboratory strains and twenty-one clinical isolates of P. falciparum using optimized growth inhibition assays. Additionally, parasites with reduced susceptibility to gossypol were selected using the P. falciparum Dd2 background (Dd2_3.5 µM) and tested for cross-resistance to chloroquine, dihydroartemisinin (DHA), and three Malaria box compounds (MMV006087, MMV085203, and MMV008956). On average, gossypol was found to be twice as potent against the laboratory strains compared to the clinical isolates, with IC₅₀ values of 6.490 µM and 11.670 µM, respectively. Notably, Dd2_3.5 µM parasites displayed increased sensitivity after three months of exposure but developed decreased susceptibility after six months. Importantly, these gossypol-tolerant parasites showed no cross-resistance to chloroquine, DHA, or the three Malaria box compounds. These findings suggest that gossypol is effective against P. falciparum and holds potential as part of combination therapy with existing antimalarials. Furthermore, these results may support the identification of new antimalarial agents that are effective against drug-resistant malaria parasites.
Similar content being viewed by others
Introduction
The global malaria incidence declined from 216 million cases in 2009 to 198 million cases in 20131,2. However, since 2014, malaria cases have risen, reaching an estimated 249 million cases in 20223. This represents an increase of about 35 million cases compared to those reported in 20154,5. This trend corresponded to growing reports of resistance to artemisinin and its combination therapy, initially reported in Southeast Asia and Western Cambodia4,6,7. More recently, there are growing reports indicating delayed clearance or resistance to artemisinin-based treatments in sub-Saharan Africa4,8, where over 90% of global malaria cases occur. Studies in Eritrea9, Rwanda10, Tanzania and Uganda11 have reported partial artemisinin resistance linked to clonal expansion of Pfkelch13 mutations. The emergence of partial resistance to artemisinin and its partner drugs in sub-Saharan Africa presents a significant health risk to reducing the burden of malaria globally. Considering the limited efficacy of available malaria vaccines12, chemotherapeutics remain a formidable force in our quest to eliminate malaria globally13.
To accelerate the development of new chemotherapeutic agents for the treatment of drug-resistant malaria parasites, institutions such as Medicines for Malaria Venture (MMV) are collaborating with GlaxoSmithKline and St. Jude Children’s Research Hospital to promote research and the rapid development of new antimalarial agents (malaria or pathogen box)14. Also, several other studies have explored new classes of antimalarial compounds that target crucial parasite proteins expressed at different stages of the parasite life cycle15,16,17. With all these efforts to increase the repertoire of antimalarial agents in the drug development pipeline, there is also the need to explore antimalarial agents which have not made it to clinical studies. By using new ideas and current research tools, it is possible to discover novel therapeutic targets from these antimalarial agents that are crucial for developing new antimalarial drugs. Towards this goal, this study further explores gossypol, a natural product from cottonseed. This compound has been tested and validated for good antimalarial activities against chloroquine-resistant and susceptible P. falciparum parasites with IC50values ranging between 5 and 13 µM18. Despite the historic interest in gossypol’s antimalarial potential, its toxicity led to a disinterest in further researching this compound19. However, other studies have shown that less toxic derivatives of gossypol can retain potency similar to that of thbases with amino groups of proteinse parent compound19, suggesting renewed potential for gossypol as an antimalarial. The high toxicity associated with gossypol is attributed to its two functional aldehyde groups forming Schiff’s bases with amino groups of proteins20. However, studies in rats indicate that gossypol’s toxicity is related to the dose and duration of administration21, with recovery observed after withdrawal. In light of these studies, we believe that exploring the antimalarial potential of gossypol could offer new targets for drug development and combination therapies.
This study evaluated the antimalarial activity of gossypol by screening it against laboratory and clinical P. falciparum isolates. The clinical isolates were included to provide robust testing, an approach validated in our previous studies22,23. We first confirmed gossypol’s efficacy against laboratory strains and clinical isolates. We then selected P. falciparum parasites with reduced susceptibility to gossypol (Dd2_3.5 µM) and tested them for cross-resistance with chloroquine, dihydroartemisinin (DHA), and three Malaria box compounds. Finally, we investigated the impact of multiclonality and polymorphisms in the pfcrt and pfmdr1 genes on P. falciparum sensitivity to gossypol. This study represents one of the largest validations of gossypol’s potency across diverse P. falciparum parasites.
Results
Evaluating the potency of gossypol against laboratory strains and clinical isolates of P. falciparum
Since protocols for setting assays may vary from one laboratory to another, it was important to independently validate the potency of gossypol using our optimized protocol for setting growth inhibitory assays23. To achieve this objective, we first screened six (6) laboratory strains of P. falciparum (Table 1) against gossypol at final-well concentrations from 1.56 µM to 100 µM. The IC50 values observed ranged from 3.829 µM to 10.190 µM (Supplementary Fig. S2) with an average IC50 of 6.11 µM (Fig. 1). Gossypol was most efficacious against W2mef (IC50 of 3.829 µM) and least efficacious against NF54 (IC50of 10.190 µM). As we previously established the significance of including clinical isolates during antimalarial compound screen activities23, we further validated the antimalarial properties of gossypol using twenty-one (21) clinical isolates at final-well concentrations from 1.56 µM to 100 µM (Table 1). The observed IC50 values varied widely between 1.058 µM and 24.79 µM (Supplementary Fig. S3), with an average IC50 of 11.67 µM (Fig. 1). The overall average IC50 value for gossypol against both the laboratory and clinical isolates of P. falciparum was 10. 46 µM. Thus, the IC50 values observed in our study were within the range of IC50 values previously reported for gossypol. Furthermore, an independent t-test was conducted to compare the mean IC50 values between the laboratory strains (n = 6) and the clinical isolates (n = 21). The susceptibility of the laboratory strains to gossypol (Mean = 6.11, SD = 2.25) was significantly higher than the clinical isolates (Mean = 11.67, SD = 7.44), t (24.73) = 2.98, p < 0.006). The F test confirmed unequal variances (p = 0.015); hence, Welch’s correction was conducted. The difference in response between the laboratory strains and the clinical isolates was 5.557 ±1.865 (95% CI: 1.714–9.400), indicating a substantial difference in susceptibility between the two groups. Arguably, our data also suggested gossypol was about twice as potent against the laboratory strains compared to the clinical isolates.
A plot of the mean IC50 values of gossypol against the laboratory and clinical isolates of P. falciparum. The clinical isolates were generally less sensitive to gossypol compared to the laboratory strains of P. falciparum parasites (Unpaired t-test, *p < 0.05). Error bars denote SEM. The overall average (both clinical isolates and laboratory strains) average IC50 was 10.46 µM.
Selection of Dd2 P. falciparum parasites with reduced susceptibility to gossypol
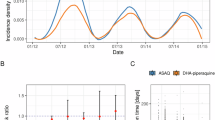
Following the validation of the antimalarial activity of gossypol against the laboratory and clinical isolates of P. falciparum, we further selected parasites with reduced susceptibility to gossypol using the P. falciparum Dd2 strain. The Dd2 strain was chosen due to its intrinsic resistance to multiple antimalarial drugs24, making it an ideal model for studying the genetic and biochemical mechanisms driving antimalarial resistance. Investigating resistance in Dd2 parasites not only deepens our understanding of how P. falciparum develops drug resistance but also helps identify new therapeutic targets and elucidate gossypol’s mechanism of action. To achieve this objective, Dd2 parasites were cultured in media supplemented with gossypol at sub-IC50 concentrations, starting at 0.5 µM for two weeks, followed by 2.5 µM for three weeks. These concentrations were below the baseline IC50 for Dd2 (5.049 µM). No significant changes in IC50 values were observed during this period (data not shown). Following this, the concentration of gossypol was increased to 3.5 µM, and the culture was monitored continuously. After three months, the IC50 values for two independent replicates (Dd2_3.5 µM_1 and Dd2_3.5 µM_2) had decreased to 2.599 µM and 2.970 µM, respectively, representing nearly half the initial IC50 (Fig. 2 and Supplementary Fig. S6). Interestingly, after four months of continuous culture, the IC50 values increased to 10.860 µM and 11.480 µM, respectively (Fig. 2B). After five months, we observed an increase in susceptibility, with IC50 values for Dd2_3.5 µM_1 and Dd2_3.5 µM_2 decreasing to 6.645 µM and 7.684 µM, respectively (Fig. 2B). However, after six months, the IC50 values increased again to 14.940 µM and 15.670 µM for the two replicates. Surprisingly, after seven months of culturing, the IC50 values for Dd2_3.5 µM_1 and Dd2_3.5 µM_2 decreased once more to 2.519 µM and 4.651 µM, respectively(Fig. 2B). The IC50 values after six months were nearly three times higher than the starting values (5.049 µM) and about six times higher than the values recorded at three-months (Fig. 2A and B). This pattern of fluctuating susceptibility, with an increase in IC50(14.940 µM and 15.670 µM) after six months compared to the parental strain, suggests the emergence of Dd2 parasites with reduced susceptibility to gossypol (Dd2_3.5 µM). These results represent the first report of a dynamic sensitivity response in malaria parasites exposed to gossypol over time, where susceptibility both increases and decreases throughout the selection process. The potency of standard antimalarials against the Dd2_3.5 µM parasites was also similar to those previously reported for Dd2 parasites against chloroquine and artemisinin-based compounds25, suggesting these parasites were not contaminated. Furthermore, molecular analyses of the Dd2_3.5 µM parasites for the presence or absence of the P. falciparum histidine-rich protein 2 and 3 (PfHRP2 and PfHRP3) (Supplementary Fig. S4 and Table S.2) confirmed that they were not contaminated with other P. falciparum strains26.
Selection of Dd2 P. falciparum parasites with reduced susceptibility (Dd2_3.5 µM) to gossypol. (A) Dose-response curves showing the susceptibility of Dd2_3.5 µM_1 parasites at baseline (IC50 values of 5.049 µM (95% CI: 4.291–5.883)), three months (IC50 values of 2.599 μM (95% CI: 1.826–3.737)) and finally at six months (14.94 µM (95% CI: 11.55–21.47) ; (B) Susceptibility pattern of the Dd2_3.5 µM parasites (two replicates) during the in vitro selection process.
Dd2_3.5 µM parasites screened against standard antimalarial drugs
To determine the existence of cross-resistance between gossypol and existing antimalarials, we screened Dd2_3.5 µM parasites against chloroquine and dihydroartemisinin (DHA) (Fig. 3). The difference in IC50 values observed between Dd2_3.5 µM (2.686 nM) and the parental Dd2 strain (9.126 nM) (Fig. 3A) was about 6.44 nM, which suggested that Dd2_3.5 µM parasites were more sensitive to DHA compared to the Dd2 parental strain. Again, the Dd2_3.5 µM parasites were almost two times more sensitive to chloroquine (249.90 nM) compared to the parental Dd2 strain (425.20 nM) (Fig. 3B), which also alluded to the fact that the Dd2_3.5 µM parasites had higher sensitivity to chloroquine compared to the parental Dd2 strain. Therefore, based on these observations, our data suggests that the Dd2_3.5 µM parasites were generally more sensitive to chloroquine and DHA than their parental Dd2 strains. This data further suggests the existence of no observable cross-resistance between gossypol, DHA and chloroquine. Additionally, the Dd2_3.5 µM parasites and the parental Dd2 strains were sensitive to DHA (IC50 value < 12 nM) and resistant to chloroquine (IC50 value > 100 nM) further suggests no contamination with other strains in the process of culturing them (Fig. 3A-C).
Dose-response curves for the Dd2_3.5 µM parasites, Dd2 parental strain and 3D7 parental strains of P. falciparum against standard antimalarial drugs. (A) Dose-response curves showing the response of chloroquine against Dd2_3.5 µM and Dd2 parental strain; (B) Dose-response curves showing the response of dihydroartemisinin (DHA) against Dd2_3.5 µM and Dd2 parental strain and (C) Dose-response curves showing the response of DHA and chloroquine against 3D7. Each data point represents the mean ± SEM (n = 2). The plot shows the percentage parasitemia against the log of the concentration of the compound.
Response of Dd2_3.5 µM parasites to MMV006087, MMV085203 and MMV008956
In our previous study on the Malaria box compounds, we identified MMV006087, MMV085203 and MMV008956 (Supplementary Fig. S1) as the most potent compounds against four clinical isolates of P. falciparum23. For this study, we also tested for the existence of cross-resistance between gossypol and the three Malaria box compounds. This was to examine if gossypol had cross-resistance to potentially new antimalarial compounds. To accomplish this aim, we screened Dd2_3.5 µM parasites against the three Malaria box compounds and compared the IC50 values to that of the parental Dd2 strain (Fig. 4). The Dd2_3.5 µM parasites were about five times more sensitive to MMV006087 compared to the parental Dd2 strain (IC50 values of 18.43 nM and 92.38 nM, respectively) (Fig. 4A). The Dd2_3.5 µM parasites were also about five times more sensitive to the MMV085203 (IC50 values of 140.60 nM) compared to the parental strain with an IC50 value of 649.50 nM (Fig. 4B). For MMV008956 against Dd2_3.5 µM parasites and parental Dd2 strain, IC50 values of 139.50 nM and 280.90 nM were observed, respectively (Fig. 4C). Therefore, based on the difference in IC50 values, the Dd2_3.5 µM parasites were more sensitive to the three Malaria box compounds compared to their parental strains. Additionally, it was observed that MMV006087 was more potent against the Dd2_3.5 µM parasites and Dd2 parental strains compared to MMV008956 and MMV085203.
Dose-response curves for Dd2_3.5 µM against three Malaria box compounds. Panels A–C, are the dose-response curves showing the response of Dd2_3.5 µM parasites against (A)MMV006087, (B) MMV085203 and (C)MMV008956, at concentrations from 0.064 nM to 25 µM. Each data point represents the mean ± SEM (n = 2). The plot shows the percentage parasitemia against the log of the concentration of the compound.
Determination of copy number variation in the clinical isolates and Dd2_3.5 µM parasites
Studies have suggested that mutations and copy number variations in genes such as pfcrt and pfmdr1mediating malarial drug resistance can modulate the sensitivity of the parasites to antimalarial drugs27. Therefore, we first evaluated copy number variations in the pfmdr1 and pfcrt genes in the clinical isolates (Fig. 5). From our results, there were no differences in copy number of the pfcrt gene in all the clinical isolates (data not shown), which was not surprising as copy number variations in this gene have not been previously reported in P. falciparum parasites. We also observed that almost all the clinical isolates had pfmdr1 gene copy numbers of one except isolate 14400, which had a copy number of two (Fig. 5). Although this was interesting, the increased pfmdr1 gene copy number in this clinical isolate did not seem to modulate its sensitivity to gossypol relative to the other clinical isolates that had pfmdr1 gene copy number of one. Additionally, we determined if copy number variation in the pfmdr1 and pfcrt genes were responsible for the reduced sensitivity in the Dd2_3.5 µM parasites (Fig. 5). This was achieved by evaluating and comparing the copy numbers in these genes in the Dd2_3.5 µM parasites and their parental strains. From our data, we observed no differences in copy numbers of pfmdr1 and pfcrt genes between the Dd2_3.5 µM parasites and the parental line (Fig. 5). These results may suggest that there could be other genetic signatures that might explain the variations in the sensitivity observed in the clinical isolates and the Dd2_3.5 µM parasites.
Graphs showing pfmdr1 and pfcrt copy number variation in Dd2 parental strain (Dd2), Dd2_3,5 μM parasites, 3D7 and clinical isolates. A All the clinical isolates had one pfmdr1 copy number, except for the clinical isolate 14400, which had a copy number of two. There was also no difference in pfmdr1 copy number between Dd2 parental strain and Dd2_3,5 μM parasites.
Evaluating the effect of multiple clones in clinical isolates on their susceptibility to antimalarial compounds
In this study, 17 of the clinical isolates were successfully genotyped using the MSP1 and MSP2 genotyping techniques. For the msp1 gene, there were more monoclonal infections (67%) compared to polyclonal infections (32%) (Table 2). The K1 allele was the most prevalent (65%), followed by the RO33 (41%) and then MAD20 (30%). In the msp2 gene, there were also more monoclonal infections (77%) than polyclonal infections (23%) (Table 2). The 3D7 allele was the most prevalent (88%), followed by the FC27 (53%). A comparison of the monoclonal and polyclonal infection frequencies between MSP1 and MSP2 showed no statistically significant difference (Fisher’s Exact Test, p = 0.41), indicating similar rates of single and multiple genotype infections between the two genes. The average multiplicity of infection (MOI) for MSP1 was 2.0 and 1.8 for MSP2, with individual samples showing between 1 and 4 alleles per sample (Table 2). Thus, a moderate level of genetic diversity was observed within the clinical isolates sampled. Following this, we further evaluated the effect of multiple P. falciparum genotypes on the susceptibility of the clinical isolates to gossypol. Since all the isolates contained at least two genotypes, we compared the mean IC50 of isolates with two genotypes to those with three or more genotypes. From the data (Fig. 6), the mean IC50 value for isolates with two genotypes was 11.04 µM and 13.14 µM for those with three or more genotypes. An unpaired t-test was subsequently conducted to compare the mean IC50 values between the clinical isolates with two clones (n = 10) and those with more than two clones (n = 7). The susceptibility of the clinical isolates with two clones against gossypol (Mean = 11.04, SD = 7.37) was not significantly different from those with more than two clones (Mean = 13.14, SD = 6.70), t (15) = 0.589, p < 0.565). The F test confirmed equal variances (p = 0.845), hence, a standard t-test was conducted. The difference in susceptibility of the parasites with two clones to those with more than two clones was 2.064 ±3.505 (95% CI: −5.409-9.543), indicating no substantial difference in susceptibility between the two groups.
Comparing the susceptibility of clinical isolates with two clones to those with more than two clones. The IC50 values of the clinical isolates with two P. falciparum genotypes were not significantly different from those with more than two genotypes (Unpaired t-test, p = 0.56). Error bars denote SEM.
Discussion
The limited number of partially effective malaria vaccines coupled with growing reports of resistance to the frontline antimalarial drug, especially in sub-Saharan Africa, has created the need for new antimalarial drugs with novel targets and mechanisms of action4,6,7,9,13,28. In this regard, it was important to take a further look at gossypol, which has historically been shown to possess antimalarial activity18. Previous studies have demonstrated that gossypol is effective against Plasmodium falciparum at concentrations above 1 µM, with IC50values of 10 µM against chloroquine-resistant and chloroquine-susceptible strains18. However, despite its potential, the toxic effects of gossypol—primarily due to its aldehyde functional groups—have limited its development as a viable antimalarial treatment29,30. Fortunately, derivatives of gossypol have been demonstrated to be less toxic and have similar potency as the parent compound29,30. Based on these findings, we found it prudent to further explore the potency of gossypol using laboratory strains and clinical isolates of P. falciparum.
Our study confirmed that the potency of gossypol against laboratory strains of P. falciparum was consistent with previous research18, which not only reaffirmed the compound’s potential but also validated our growth inhibition assays. While earlier investigations predominantly focused on laboratory-adapted strains, the efficacy of gossypol against clinical isolates remained unclear. Therefore, it was imperative to adequately validate the potency of gossypol using the clinical isolates. Clinical isolates offer a more accurate representation of the parasite population encountered in endemic regions, and our previous studies have highlighted the significance of including them in antimalarial compound screening efforts23. The significance of thorough evaluation of the potency compounds before clinical use is highlighted in a study by Arrowsmith et al.31. After analysing 108 reports of Phase II failures from 2008 to 2010 for new drugs and major new indications of existing drugs, the authors found that 51% of the clinical failure of drugs resulted from insufficient efficacy32. The study further indicated that the failure arising from insufficient efficacy could be due to a lack of sufficient evidence to prove the efficacy advantage of the compounds over an existing or more advanced drug32. Our findings revealed that the efficacy of gossypol against half of the clinical isolates screened was similar to data from earlier studies19,29. However, several clinical isolates exhibited almost two-fold less susceptibility to gossypol compared to the laboratory strains, substantiating the need to include clinical isolates in antimalarial drug screening activities. To our knowledge, this is the largest screen of gossypol against this number of laboratory strains and clinical isolates of P. falciparum in a single study.
Several studies have shown that clinical isolates harbour multiple P. falciparum clones with different drug-resistance backgrounds, and this has the potential to affect the efficacy of antimalarial drug treatment outcomes33,34. Our study showed that clinical isolates with two genotypes were more susceptible to gossypol than those with more than two genotypes, though the difference was not statistically significant. This may suggest that factors beyond genotype number, such as specific genetic polymorphisms, including mutations, could influence gossypol sensitivity. Following this, we also examined the potential contribution of polymorphisms in the P. falciparum multidrug resistance gene 1 (pfmdr1) and the chloroquine resistance transporter (pfcrt) gene, which has been shown to modulate sensitivity to antimalarials27,35. Interestingly, all clinical isolates had the same number of pfcrt and pfmdr1 gene copies, except for one isolate with two pfmdr1 copies, but this did not affect its sensitivity to gossypol. These findings could suggest that other genetic or, potentially, epigenetic factors could be responsible for the observed differences in gossypol sensitivity.
During the resistance selection process, we observed varied susceptibility patterns of the Dd2_3.5 µM parasites in response to gossypol, with reduced susceptibility to the compounds after six months. The continuous exposure of the P. falciparum parasites to gossypol likely produced a heterogeneous parasite population with varying levels of susceptibility or resistance36,37,38. This could result from competitive suppression between parasites more sensitive to gossypol and those less sensitive39,40. Furthermore, studies indicate that artemisinin induces a subpopulation of P. falciparum parasites with decreased susceptibility to artemisinin within a clonal population into quiescence41,42. Other studies have also implicated the role of epigenetic mechanisms mediating drug resistance in P. falciparum within the isogenic parasite population, where only a subset of parasites can survive drug pressure43,44. For instance, inhibition of the histone acetyltransferase PfGCN5 in artemisinin-resistant parasites was shown to increase their sensitivity to artemisinin treatment45. In line with these studies, we hypothesize that short-term epigenetic or metabolic changes might have occurred during the selection period, leading to altered susceptibility of the Dd2_3.5 µM parasites to gossypol. Thus, our next step will involve isolating and characterizing the drug susceptibility phenotypes of the different clones within the heterogeneous parasite population. Additionally, whole-genome and epigenetic analyses will be conducted to identify genetic and epigenetic signatures that may explain the variation in gossypol sensitivity.
Our study also explored the potential for cross-resistance, which occurs when resistance to one drug confers resistance to other drugs with similar mechanisms of action4. Interestingly, the Dd2_3.5 µM parasites in our study were more sensitive to chloroquine, DHA, and the three Malaria box compounds, suggesting that gossypol did not have cross-resistance to these compounds. Additionally, this data may indicate that gossypol could enhance the efficacy of other drugs. While the absence of cross-resistance to chloroquine, DHA, and the Malaria box compounds in the Dd2_3.5 µM parasites suggests that gossypol may not share resistance pathways with these compounds, we are unable to rule out the possibility of a gossypol-specific resistance mechanism. Thus, further studies in the form of target deconvolution and genetic analyses will be necessary to confirm whether gossypol acts on a novel target or whether resistance mechanisms are unique to gossypol itself.
In conclusion, our study confirmed the potency of gossypol against P. falciparum laboratory strains and clinical isolates, although the clinical isolates generally show reduced susceptibility to gossypol. The absence of cross-resistance with other antimalarials further suggests that gossypol may target a unique pathway, making it a promising candidate for future therapeutic development. Future studies will involve whole-genome and epigenetic investigations to explore the mechanisms of action and resistance to gossypol, as well as identify potentially new antimalarial drug targets.
Materials and methods
P. falciparum parasites and parasite culture
For this study, P. falciparum laboratory-adapted parasites, 3D7, W2mef, Dd2, GB4, 7G8 and K1 and twenty-one randomly selected clinical isolates (Table 1) were cultured using standard methods46,47 with slight modifications. The laboratory strains were cultured with RPMI-1640 (Sigma) that was supplemented with 0.5% AlbuMAX II (Gibco), 20 mg hypoxanthine, 2 g sodium bicarbonate (Sigma). For the clinical isolates, the media was further modified with 2% normal human serum (PAN-Biotech, Germany). The cultures were maintained at 37 °C using human group O+ erythrocytes at 4% hematocrit and mixed gas composed of 93% nitrogen (N2), 5% carbon dioxide (CO2), and 2% oxygen (O2) (Air Liquide, Birmingham, United Kingdom). The laboratory strains (Table 3) used for this study each have different drug-resistant phenotypes. The clinical isolates used for this study are archived samples collected for a study on erythrocyte invasion mechanisms (EIM)48,49. These samples were processed upon arrival from the field, cryopreserved using the glycerolyte method50and stored in liquid nitrogen tanks48for future use. Details regarding ethical clearance and study sites for the samples were previously described48. The samples were thawed using serial NaCl solutions50 whenever there was the need to set assays. The selection of 21 clinical isolates was based on parasites that adapted well to in vitro culture conditions at the time of the study. This number allowed us to perform an initial screening to evaluate the efficacy of gossypol against a range of diverse P. falciparum isolates representing various genetic backgrounds. For the drug assays, P. falciparum parasites were cultured to > 5% parasitemia of ring-stage parasites. Using 5% Sorbitol treatment, a synchronised culture of ring-stage parasites51was obtained and diluted to 1% parasitemia and 2% haematocrit for conducting the growth inhibition assays as previously described23. In order not to lose some of the clones in the clinical isolates during synchronization, the assays for the clinical isolates were set up with cultures containing > 90% ring-stage parasites.
Selection of parasites with reduced susceptibility to gossypol (Dd2_3.5 µM)
A step-wise selection process was used to select parasites with reduced susceptibility to gossypol using the Dd2 laboratory strains (Dd2_3.5 µM) based on established approaches39,40,41,42,43,44,45,46,47,48,49,50,51,52. Briefly, the parasites were cultured in vitro at a starting parasitemia of 5% with media containing 0.5 µM of gossypol for two weeks and subsequently cultured in media containing 2.5 µM gossypol for three weeks. The concentration of gossypol was increased to 3.5 µM gossypol and used to culture the parasites from the 2.5 µM gossypol for a further seven months. Microscopy and growth inhibitory assays were conducted at least once every month to monitor and assess the emergence of parasites with reduced susceptibility to gossypol23. The cultures were maintained daily with media containing gossypol at the appropriate concentration. Two biological replicates (Dd2_3.5 µM_1 and Dd2_3.5 µM_2) were used during the selection process. Before setting up the in vitro growth inhibitory assays, the parasites were washed thrice with RPMI to wash off the gossypol-containing media.
In vitro drug susceptibility assay
To evaluate the potency of gossypol against the laboratory, clinical isolates and Dd2_3.5 µM parasites, a stock of 10 mM gossypol (Sigma-Aldrich, USA) was serially diluted and screened against the parasites at final-well concentrations between 1.56 µM to 100 µM as previously described23. The growth inhibition assays were set up in triplicate wells with a total volume of 100 µL consisting of 10 µL of gossypol and 90 µL parasite culture at 1% parasitemia and 2% haematocrit in a 96-well plate. RPMI containing 1% DMSO was used as a negative control, and uninfected erythrocytes at 2% haematocrit were used to correct for background fluorescence. The parasitemia corresponding to each culture well after 72 h of incubation was determined by removing 80 µL of the supernatant and adding 80 µL of 0.2× SYBR Green I (Invitrogen, USA) stain in lysis buffer (20 mM Tris (pH 7.5), 5 mM EDTA, 0.008% (W/V) saponin and 0.08% (V/V) Triton X-100)) based on established methods54. The plates were then incubated in the dark at 37oC for a minimum of 30 min, and the total fluorescence from each of the wells was determined with the Varioskan Lux multimode microplate fluorescent plate reader (ThermoFisher Scientific, USA) at an excitation of 485 nm, emission of 520 nM and gain at 100.
Data analysis
The data acquired from the fluorescent plate reader were initially processed using Microsoft Excel software (Version 16.89.1) by subtracting background fluorescence from all values. After processing, the data were imported into GraphPad Prism (Version 9.01) for further analysis. Sigmoidal dose-response curves were generated, and IC50 values were estimated for each assay. Briefly, the compound’s concentrations were transformed to a logarithmic scale. The fluorescence readings corresponding to parasitemia were then normalized by setting the lowest mean in each data set to 0% and the highest mean to 100%. Given the typical sigmoidal (S-shaped) nature of dose-response curves, a non-linear regression analysis was performed using the four-parameter logistic model (4PL). This model was selected because it provides key information about the minimum and maximum response levels, the IC50 value, and the slope of the curve. To assess the quality of the curve fitted to the data, the R-squared value, a statistical test for goodness-of-fit, was calculated for each data set. In this study, R-squared values greater than 0.9 were considered to represent a good fit for the dose-response curves. The IC50 values were derived from the fitted dose-response curves, and each data point is presented as the mean ± standard error of the mean (SEM) from two independent experiments, each conducted in triplicate. The IC50 values and their corresponding 95% confidence intervals (CI) were used to compare the efficacy of gossypol in laboratory strains, clinical isolates, and the Dd2_3.5 µM parasites. Additionally, the GraphPad Prism software was also used to test for statistically significant differences in mean IC50 values. An unpaired (independent) t-test was used to determine whether there was a statistically significant difference between the mean IC50 values of the laboratory strains and the clinical isolates or clinical isolates with different clones. Before performing the t-test, the assumptions of normality and homogeneity of variances were evaluated. The Shapiro-Wilk test was used to assess the normality of the data in each group. The F test for equality of variances was employed to check for homogeneity of variances. If the F test indicated that the variances were not equal, Welch’s t-test, which does not assume equal variances, was used to correct for this violation.
Evaluating copy number variation in pfcrt and pfmdr1 genes
To understand the differences in the response of the P. falciparum parasites to gossypol, the copy numbers in the pfcrt and pfmdr1genes were determined using a SyBr green-based real-time quantitative polymerase chain reaction assay (RT-qPCR)55. Each sample was set up with a total reaction volume of 10 µL comprising 1X Luna Universal qPCR Master Mix (New England Biolabs, Hitchin, UK), 0.2 µM of each of the primers, and 2 µL of DNA template in triplicates on the QuantStudio5 system (Applied Biosystems, Waltham, MA). The cycling conditions for the assay were an initial amplification at 50oC for 2 min, 95oC for 1 min, 40 cycles at 95oC for 30 s, 54oC for 40 s and 60oC for 1 min. The specificity of the resulting amplicons was analyzed using the melt curve. The endogenous control was the P. falciparum Beta-tubulin gene. DNA from the 3D7 and Dd2 laboratory strains was also used as reference samples, and a non-template control was also included in each run. The Ct values for each gene of interest (pfcrt and pfmdr1) were normalized to the Ct values of the reference gene, yielding ΔCt. The ΔCt values were then compared to a control strain known to have a single copy of pfcrt and pfmdr1 to obtain ΔΔCt. The delta-delta Ct (2—ΔΔCt) method was used to estimate the relative copy numbers of the pfcrt and pfmdr1genes38. For each sample, the copy number was determined as the mean value from the triplicate qPCR reactions. Copy number results were expressed as approximations (e.g., 1.0, 2.0, 3.0 copies), with minor variations (e.g., 0.8 or 2.2) rounded up to the nearest whole number for clarity.
Genotyping parasites for multiclonality
The different parasite genotypes in the clinical isolates and Dd2_3.5 µM parasites were identified by analysis of polymorphic genetic loci of the merozoite surface protein genes msp1 and msp256. Briefly, genomic DNA was extracted from seventeen (17) of the clinical isolates of P. falciparum parasites (four of the clinical isolates were lost at the time of this experiment) and amplified in a polymerase chain reaction (PCR) with primers targeting conserved regions of msp1 block 2 and msp2 block 3 (Table S1). In a nested PCR reaction, the DNA from the first reaction was amplified with primer sets targeting specific allelic families of msp1 (MAD20, K1 and RO33) and msp2 (3D7/IC and FC27). Genomic DNA from laboratory strains was used as a positive control and a template-free control was also included as a negative control for all the reactions. The size of the PCR product was determined using a 100 bp DNA ladder (Supplementary Fig. S5) and the polymorphisms in each allelic family of the msp1 and msp2 genes were determined as previously described57. The allele frequencies and multiplicity of infection (MOI) were determined by computing the number of unique alleles in the msp1 and msp2 genes. A MOI of one (1) indicates monoclonal infection and greater than one (> 1) indicates polyclonal infection. The proportion of mono- and polyclonal infections was computed and compared between MSP1 and MSP2 using the Fisher’s Exact test.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
WHO. in WHO global malaria programme: world malaria report 2010 204–204. (2010).
WHO. World Malaria Report 2014Vol. 23 (World Health Organization, 2014).
Organization, W. H. World Malaria Report 2023 (World Health Organization, 2023).
WHO. World malaria report 2019. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO. WHO (2019). (2019).
WHO. World Malaria report 2015. Geneva: World Health Organization. WHO (2015). (2015).
Dondorp, A. M. et al. Artemisinin resistance in Plasmodium Falciparum malaria. N Engl. J. Med. 361, 455–467. https://doi.org/10.1056/NEJMoa0808859 (2009).
Imwong, M. et al. The spread of artemisinin-resistant Plasmodium falciparum in the Greater Mekong subregion: a molecular epidemiology observational study. Lancet Infect. Dis. 17, 491–497. https://doi.org/10.1016/S1473-3099(17)30048-8 (2017).
WHO. World Malaria Report 2022 (World Health Organization, 2022).
Mihreteab, S. et al. Increasing prevalence of artemisinin-resistant HRP2-negative malaria in Eritrea. N. Engl. J. Med. 389, 1191–1202 (2023).
Uwimana, A. et al. Emergence and clonal expansion of in vitro artemisinin-resistant Plasmodium Falciparum kelch13 R561H mutant parasites in Rwanda. Nat. Med. 26, 1602–1608 (2020).
Asua, V. et al. Changing prevalence of potential mediators of aminoquinoline, antifolate, and artemisinin resistance across Uganda. J. Infect. Dis. 223, 985–994 (2021).
Olotu, A. et al. Seven-year efficacy of RTS,S/AS01 malaria vaccine among young African children. N Engl. J. Med. 374, 2519–2529. https://doi.org/10.1056/NEJMoa1515257 (2016).
Coelho, C. H., Doritchamou, J. Y. A., Zaidi, I. & Duffy, P. E. Advances in malaria vaccine development: report from the 2017 malaria vaccine symposium. NPJ Vaccines 2, 34 (2017). https://doi.org/10.1038/s41541-017-0035-3
Van Voorhis, W. C. et al. Open Source Drug Discovery with the Malaria Box compound Collection for Neglected diseases and Beyond. PLoS Pathog. 12, e1005763. https://doi.org/10.1371/journal.ppat.1005763 (2016).
Douglas, R. G., Reinig, M., Neale, M. & Frischknecht, F. Screening for potential prophylactics targeting sporozoite motility through the skin. Malar. J. 17, 1–10 (2018).
Feng, L. S. et al. Hybrid molecules with potential in vitro antiplasmodial and in vivo antimalarial activity against drug-resistant Plasmodium falciparum. Med. Res. Rev. 40, 931–971. https://doi.org/10.1002/med.21643 (2020).
Schiafino-Ortega, S. et al. 1, 2-Diphenoxiethane salts as potent antiplasmodial agents. Bioorg. Med. Chem. Lett. 28, 2485–2489 (2018).
Heidrich, J., Hunsaker, L. & Vander Jagt, D. Gossypol, an antifertility agent, exhibits antimalarial activity in vitro. IRCS J. Med. Sci. (1983).
Razakantoanina, V., Kim, N., Jaureguiberry, G. & P. P. & Antimalarial activity of new gossypol derivatives. Parasitol. Res. 86, 665–668. https://doi.org/10.1007/pl00008549 (2000).
Moh, P., Li, P., Darby, M., Brueggemeier, R. & Lin, Y. Characteristics of covalent gossypol binding to microsomal proteins. Res. Commun. Chem. Pathol. Pharmacol. 76, 305–322 (1992).
National, C. G. o. M. A. A. Gossypol-a new antifertility agent for males. Chin. Med. J. 4, 417–428 (1978).
Chirawurah, J. D. et al. MMV006087 is a potent Malaria Box compound against Plasmodium Falciparum clinical parasites. Front. Drug Discovery. 3, 1190471 (2023).
Chirawurah, J. D. et al. Antimalarial activity of Malaria Box compounds against Plasmodium falciparum clinical isolates. Int. J. Parasitol. Drugs Drug Resist. 7, 399–406. https://doi.org/10.1016/j.ijpddr.2017.10.005 (2017).
Chugh, M. et al. Identification and deconvolution of cross-resistance signals from antimalarial compounds using multidrug-resistant Plasmodium falciparum strains. Antimicrob. Agents Chemother. 59, 1110–1118 (2015).
Pradines, B., Bertaux, L., Pomares, C., Delaunay, P. & Marty, P. Reduced in vitro susceptibility to artemisinin derivatives associated with multi-resistance in a traveller returning from South-East Asia. Malar. J. 10, 268. https://doi.org/10.1186/1475-2875-10-268 (2011).
Walker-Jonah, A., Dolan, S. A., Gwadz, R. W., Panton, L. J. & Wellems, T. E. An RFLP map of the Plasmodium falciparum genome, recombination rates and favored linkage groups in a genetic cross. Mol. Biochem. Parasitol. 51, 313–320. https://doi.org/10.1016/0166-6851(92)90081-t (1992).
Sa, J. M. et al. Geographic patterns of Plasmodium Falciparum drug resistance distinguished by differential responses to amodiaquine and chloroquine. Proc. Natl. Acad. Sci. U S A. 106, 18883–18889. https://doi.org/10.1073/pnas.0911317106 (2009).
Tse, M. T. Antimalarial drugs: speeding to a new lead. Nat. Rev. Drug Discov. 9, 842. https://doi.org/10.1038/nrd3301 (2010).
Royer, R. E., Deck, L. M., Campos, N. M. & Hunsaker, L. A. Vander Jagt, D. L. Biologically active derivatives of gossypol: synthesis and antimalarial activities of peri-acylated gossylic nitriles. J. Med. Chem. 29, 1799–1801. https://doi.org/10.1021/jm00159a043 (1986).
VanderJagt, D., Baack, B., Campos, N., Hunsaker, L. & Royer, R. A derivative of gossypol retains antimalarial activity. IRCS Med. SCIENCE-BIOCHEMISTRY. 12, 845–846 (1984).
Arrowsmith, J., Miller, P. & Phase II and phase III attrition rates 2011–2012. Nat. Rev. Drug Discovery. 12, 569–570 (2013).
Arrowsmith, J. & Phase, I. I. 2008–2010. Nat. Rev. Drug Discovery 10 (2011).
Bushman, M. et al. Within-host competition and drug resistance in the human malaria parasite Plasmodium Falciparum. Proc. Biol. Sci. 283, 20153038. https://doi.org/10.1098/rspb.2015.3038 (2016).
de Roode, J. C., Culleton, R., Bell, A. S. & Read, A. F. Competitive release of drug resistance following drug treatment of mixed Plasmodium chabaudi infections. Malar. J. 3, 33. https://doi.org/10.1186/1475-2875-3-33 (2004).
Gresty, K. J. et al. Genetic mutations in pfcrt and pfmdr1 at the time of artemisinin combination therapy introduction in South Pacific islands of Vanuatu and Solomon Islands. Malar. J. 13, 406 (2014).
Langreth, S. G., Nguyen-Dinh, P. & Trager, W. Plasmodium Falciparum: merozoite invasion in vitro in the presence of chloroquine. Exp. Parasitol. 46, 235–238 (1978).
Lambros, C. & Notsch, J. Plasmodium Falciparum: mefloquine resistance produced in vitro. Bull. World Health Organ. 62, 433 (1984).
Brockelman, C., Monkolkeha, S. & Tanariya, P. Decrease in susceptibility of Plasmodium falciparum to mefloquine in continuous culture. Bull. World Health Organ. 59, 249 (1981).
Oduola, A. M., Milhous, W., Weatherly, N., Bowdre, J. & Desjardins, R. Plasmodium Falciparum: induction of resistance to mefloquine in cloned strains by continuous drug exposure in vitro. Exp. Parasitol. 67, 354–360 (1988).
Bushman, M. et al. Within-host competition and drug resistance in the human malaria parasite Plasmodium Falciparum. Proc. Royal Soc. B: Biol. Sci. 283, 20153038 (2016).
Witkowski, B. et al. Increased tolerance to artemisinin in Plasmodium Falciparum is mediated by a quiescence mechanism. Antimicrob. Agents Chemother. 54, 1872–1877 (2010).
Yu, X. et al. Ring-stage growth arrest: metabolic basis of artemisinin tolerance in Plasmodium Falciparum. Iscience 26 (2023).
Mira-Martínez, S. et al. Epigenetic switches in clag3 genes mediate blasticidin S resistance in malaria parasites. Cell. Microbiol. 15, 1913–1923 (2013).
Mira-Martínez, S. et al. Identification of antimalarial compounds that require CLAG3 for their uptake by Plasmodium falciparum-infected erythrocytes. Antimicrob. Agents Chemother. 63 https://doi.org/10.1128/aac.00052-19 (2019).
Rawat, M. et al. Histone acetyltransferase PfGCN5 regulates stress responsive and artemisinin resistance related genes in Plasmodium Falciparum. Sci. Rep. 11, 852 (2021).
Trager, W. & Jensen, J. B. Human malaria parasites in continuous culture. Science 193, 673–675. https://doi.org/10.1126/science.781840 (1976).
Maier, A. G. & Rug, M. In vitro culturing Plasmodium Falciparum erythrocytic stages. Malaria: Methods Protocols, 3–15 (2013).
Mensah-Brown, H. E. et al. Analysis of Erythrocyte Invasion mechanisms of Plasmodium Falciparum Clinical isolates across 3 Malaria-endemic areas in Ghana. J. Infect. Dis. 212, 1288–1297. https://doi.org/10.1093/infdis/jiv207 (2015).
Mensah-Brown, H. E. et al. Assessing the impact of differences in malaria transmission intensity on clinical and haematological indices in children with malaria. Malar. J. 16, 96. https://doi.org/10.1186/s12936-017-1745-8 (2017).
Ljungström, I., Moll, K., Perlmann, H., Scherf, A. & Wahlgren, M. Methods in malaria researchCiteseer,. (2008).
Lambros, C. & Vanderberg, J. P. Synchronization of Plasmodium Falciparum erythrocytic stages in culture. J. Parasitol. 65, 418–420 (1979).
Corey, V. C. et al. A broad analysis of resistance development in the malaria parasite. Nat. Commun. 7, 11901. https://doi.org/10.1038/ncomms11901 (2016).
Nzila, A. & Mwai, L. In vitro selection of Plasmodium Falciparum drug-resistant parasite lines. J. Antimicrob. Chemother. 65, 390–398. https://doi.org/10.1093/jac/dkp449 (2010).
Smilkstein, M., Sriwilaijaroen, N., Kelly, J. X., Wilairat, P. & Riscoe, M. Simple and inexpensive fluorescence-based technique for high-throughput antimalarial drug screening. Antimicrob. Agents Chemother. 48, 1803–1806. https://doi.org/10.1128/AAC.48.5.1803-1806.2004 (2004).
Ferreira, I. D., Rosario, V. E. & Cravo, P. V. Real-time quantitative PCR with SYBR Green I detection for estimating copy numbers of nine drug resistance candidate genes in Plasmodium Falciparum. Malar. J. 5, 1. https://doi.org/10.1186/1475-2875-5-1 (2006).
Snounou, G. et al. Biased distribution of msp1 and msp2 allelic variants in Plasmodium falciparum populations in Thailand. Trans. R Soc. Trop. Med. Hyg. 93, 369–374. https://doi.org/10.1016/s0035-9203(99)90120-7 (1999).
Mayengue, P. I., Ndounga, M., Malonga, F. V., Bitemo, M. & Ntoumi, F. Genetic polymorphism of merozoite surface protein-1 and merozoite surface protein-2 in Plasmodium Falciparum isolates from Brazzaville, Republic of Congo. Malar. J. 10, 276. https://doi.org/10.1186/1475-2875-10-276 (2011).
Acknowledgements
We thank the Medicines for Malaria Venture for giving us the Malaria box compounds for this work and the study participants who provided the samples through the Erythrocyte Invasion Mechanism (EIM) project for their support.
Funding
Jersley D. Chirawurah was supported by a DELTAS Africa grant (DEL-15-007: Awandare). The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS)’s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust (107755/Z/15/Z: Awandare) and the UK government. The views expressed in this publication are those of the author(s) and not necessarily those of AAS, NEPAD Agency, Wellcome Trust or the UK government.
Author information
Authors and Affiliations
Contributions
J.D.C., G.A.A. and Y.A. conceived the study; J.D.C., B.A., S.B, S.N.Y. and F.A. performed the experiments; J.D.C., S.B. S.N.Y. and F.A. analysed the data; J.D.C., Y.A., G.A.A., L.A-E. drafted the manuscript. All authors have critically reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chirawurah, J.D., Ansah, F., Blankson, S. et al. Gossypol is a natural product with good antimalarial activity against Plasmodium falciparum clinical isolates. Sci Rep 15, 1469 (2025). https://doi.org/10.1038/s41598-025-85643-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-85643-6