Abstract
Thyroid disorder patients are likely to have a prescription for various categories of drugs including those with a narrow therapeutic index and others, which affects thyroid function. However, information regarding drug therapy problems in thyroid patients has not been studied here yet. Thus this study aimed to assess drug therapy problems and associated factors among thyroid disorder patients, who had follow-ups at Northwest Hospitals of Ethiopia. A multicenter hospital-based cross-sectional study design was employed through patient interviews and chart review at public hospitals in Northwest Ethiopia. A simple random sampling technique was used to recruit patients for interviews. The identified drug-related problem was recorded and classified using Cipolle et al. 2012, adverse drug reactions were assessed by using the Naranjo algorithm of adverse drug reaction probability scale, and Up-to-date was used for the drug-drug interaction checker. The collected data was cleared, entered into epidata, checked for correctness, and exported to STATA version 17 for analysis. The results were summarized using descriptive statistics including frequency, mean, median, and standard deviation. Logistic regression analysis was conducted to identify the independent predictors of drug therapy problems. A P-value < 0.05 is considered statistically significant. Among 351 study participants most of them 300 (85.47%) were females. The study participants’ mean (± SD) age was 45.1± (0.74) years. At least one drug-related problem was recorded from 60.11%, (95% CI: 54.9-65.13) of study participants with a mean of 1.54 ± 0.046 drug-related problems per patient. The most common drug-related problems were non-adherence (34.47%) followed by adverse drug reactions (17.2%) and ineffective drug therapy (8.2%). Factors independently associated with drug-related problems were age [AOR = 2.85, 95%CI: (1.05–7.69), P-value = 0.039], poly-pharmacy [AOR = 2.57, 95%CI: (1.01–6.29), P-value = 0.046], comorbidity [AOR = 2.09, 95%CI: (1.07–4.05), P-value = 0.030], and purchasing medication from private pharmacy [AOR = 2.62, 95%CI: (1.06–6.49), P-value = 0.038]. The prevalence of drug-related problems among adult thyroid disease patients who had follow up at ambulatory clinics was very high. Age, poly-pharmacy, comorbidity, and purchasing medication in private pharmacies were independent predictors of drug-related problems. The most commonly involved medication class in experiencing drug-related problems was thionamides.
Similar content being viewed by others
Introduction
Thyroid disorders are conditions that result from either over or under-secretions of thyroid hormones as well as thyroid gland enlargement. Thyroid disorder can be primary, directly related to the gland itself, or secondary, which can be thyroid dysfunction due to other factors. About 1.6 billion people are at risk of thyroid disorders as described by 110 countries across the world1. Due to factors including environmental and nutritional, these disorders are commonly encountered in Africa2. The prevalence of hypothyroidism and hyperthyroidism in Ethiopia was 34.3% and 61.7% respectively3. The common causes of thyroid disorder are deficiency of iodine mostly followed by the toxicity of thiocyanate and also deficiency of selenium4. Thyroid dysfunction including overt hypothyroidism and goiter is caused by medication therapy of lithium which needs laboratory monitoring before initiation and then every 6 months after treatment. Thyroid disorders cause complications if untreated including heart failure, significant weight loss, and death therefore appropriate diagnosis and treatment are necessary to improve patient’s quality of life and reduce hospitalization, complication, and social interaction of thyroid disease patients2.
Drug-related problems (DRPs) is an event that occurs during the treatment of a disease that can actually or potentially interfere with the desired treatment outcomes of patients5,6, and DRPs are situations involving medication therapy that have a detrimental impact on health. Even though these medications play an important role in the cure, palliation, and prevention of disease, they also expose patients to drug-related problems7. Propylthiouracil, Beta-blockers, radiotherapy, and thyroxin are the commonly used management for thyroid disorders in Ethiopia8. These drugs have a risk for the occurrence of DRPs9. DRPs can occur at all steps of the treatment process, mainly during prescribing, transcribing, dispensing, and patient use of medication therapy10. DRPs are categorized into seven major classes composed of, unnecessary drug therapy, need additional drug therapy, ineffective drug therapy, dosing too low, dosage too high, adverse drug reaction, and noncompliance11.
Generally, DRPs may lead to reduced quality of life, increased hospital stay, increased overall healthcare cost, and increased risk of morbidity and mortality12. Despite more than 50% of DRPs being avoidable,5–10% of hospital admissions were due to DRPs13. According to the World Health Organization report more than half of medicines were inappropriately prescribed, dispensed, or sold and medicines were incorrectly used by half of patients14. A study conducted in Australia showed that about 1.3 million people were injured each year due to medication errors and adverse drug events (ADEs) in 16.6% of admissions, resulting in permanent disability in 13.7%and death in 4.9%of patients15. In the United States alone, it is estimated that 100,000 deaths occur annually due to drug therapy problems and approximately $201.4 billion in dollar in direct medical costs per year16. In the United States, it is estimated that the annual cost of drug-related morbidity and mortality is $177 and to solve adverse drug events and drug-related problems twice as much money as the drugs themselves is used17.
A study of the drug-related problem of thyroid disorder in Kenya showed that it was higher in hyperthyroidism patients. The most frequent DRP was noncompliance and it was positively associated with personal risk factors and drug therapy18. Medication must be taken as prescribed by the patient and healthcare professional to provide the best possible therapeutic results and patient safety.
The medication review process in daily practice is not common in Ethiopia due to the lack of clinical pharmacists in healthcare settings which might be a risk factor for DRPs. Despite the large prevalence of the disease, there are limited studies published on the type, extent, and associated factors of DRPs in developing countries19specifically in Ethiopia. Still, there is a study in Kenya that showed the prevalence of DRPs specifically in thyroid disease patients18. The Ethiopian government is aiming to strengthen the health care system. The vast majority of Ethiopia’s population lives in rural areas, where they have limited access to food, clean water, housing, sanitary facilities, and medical care which could contribute to patients’ development of DRPs20.
The results of this study will inform the possible patient-specific risk factors of thyroid disease that lead to DRPs and their impact on achieving the desired goal of treatment that will emphasize medication information provision and counseling for the patients and health care professionals. In addition, this study may be useful to other researchers as a reference material while conducting further studies on related topics. The results of this study may potentially impact the formulation of sensible plans, policies, and intervention strategies for the management and avoidance of medication therapy-related issues. Consequently, this study aims to assess the different classes of drug-related problems and associated factors that occur in thyroid patients.
Methods
A cross-sectional study involved 351 thyroid disease patients visited at ambulatory endocrinology clinic, and was conducted in five hospitals in Ethiopia from July 01- September 30, 2022. The identification of DRPs was based on pharmaceutical care practice, the patient-centered approach, and DRPs were identified and assessed using the American Thyroid Association Guideline 2016 and Ethiopian Standard Treatment Guideline 2014 and intervention were done using PCNE DRP classification. The identified DRPs were resolved by clinical pharmacists who provided patient counseling and communicated with prescriber physicians and Nurses treating thyroid disease patients. Data was analyzed using STATA version 14. Logistic regression analysis was conducted and outliers, multicollinearity, the normality test, and the correlation coefficient test were among the statistical methods’ presumptions that were investigated. In multivariable analysis, independent variables with a p-value of less than 0.25 in bivariate analysis were studied. To assess the association of variables with DRPs a p-value of less than 0.05 was considered to be statistically significant.
Study area and period
The study was conducted at UoGCSH, TGCSH, FHCSH, DMCSH, and DTCSH found in Northwest Ethiopia from July 01 to September 30, 2022. UoGCSH is one of the largest teaching hospitals in the Amhara region providing tertiary-level care for more than 7 million people in the Northwest part of the country and other regions. UoGCSH is located at 727 km and 180 km from Addis Ababa and Bahir Dar, the capital city of Ethiopia, and the Amhara region to the Northwest respectively. UoGCSH has Emergency, ICU, in-patient and outpatient departments. The Ambulatory clinic serves patients with endocrinology disorders such as diabetes and thyroid disease. The diabetic patients are the largest endocrinology disease and the second one is patients with thyroid disease. Debre Tabor Comprehensive and Specialized Hospital is located at Debre Tabor Town, which is the capital city of South Gondar Zone and is located in the Southwest of Gondar Zone in the Amhara Region. It is about 667 km from Addis Ababa (the capital city of Ethiopia) and 100 km from Bahirdar. The hospital was established in 1920 and serves more than three million people both outpatients and inpatients. Felegehiwot and Tibebe Ghion comprehensive and specialized Hospitals are found in the capital city of Amhara Regional State, Bahir Dar, which is 565 km away from the capital city of Ethiopia, Addis Ababa. Felegehiwot Hospital was established in 1963. The hospital provides different clinical services for 7 million populations in the catchment area. Debre Markos Hospital is found in East Gojam, which is located 300 and 265 km from Addis Ababa and Bahir Dar, the capitals of Ethiopia and the Amhara Regional State, respectively. Around 3.5 million individuals have been attended by the hospital as inpatients and outpatients.
Study design
A multicenter hospital-based, cross-sectional study was conducted in five hospitals in Northwest Ethiopia from July 01- September 30, 2022.
Source of population
All adult thyroid disease patients on follow-up at the ambulatory clinic of Northwest Hospital of Ethiopia.
Study population
All thyroid disease patients who fulfilled the inclusion criteria and on follow-up at ambulatory clinic in Northwest hospitals of Ethiopia between July 01-September 30, 2022.
Inclusion and exclusion criteria
All thyroid disease patients aged > 18 years, those who are treated and have follow-ups for at least 3 months, and those who gave informed consent to participate in the study were included. In contrast, those who have incomplete documented data, and patients with hearing and speaking problems were excluded.
Sample size determination and sampling techniques
The sample size was calculated using a single population proportion formula21 as follows; n = Zα/22 p (1-p) / d2 where n = is desired sample size; Zα/2 = is standard normal distribution at a 95% confidence level usually 1.96, p = proportion of Thyroid patients who had DRPs (p = 0.5), and d = marginal error (5%=0.05) n = 1.962 0.5(1-0.5) / 0.052 = 384.16 = ~ 384. Since the study population is less than 10,000 correction formula was used to get the final sample size (nf). nf = n/1 + n/N = 384/1 + 384/2400 = 331.Where nf = final sample size, N = total study population (2400). After considering a 10% contingency, 364 study participants were included in the study. 13 patients were excluded from the study (6 had incomplete data, and 7 were not willing to participate) and a final analysis was done on 351 patients. Five hospitals found in Northwest Ethiopia were included in the study. A simple random sampling procedure was used to choose study participants. Then, the total sample size was proportionally allocated for each selected teaching hospital. Proportional allocation of samples to the total population of each department was applied using the formula as follows: n = n×Ni/N, Where n = required sample size Ni = the total number of patients in each hospital N = Total number of patients of selected hospitals (Fig. 1). The Number of participants who visited each hospital was as follows:
Study subjects recruited from UoGCSH having 500 patients = 364*500/2400 = 76.
Study subjects recruited from DMCSH having 600 patients = 364*600/2400 = 91.
Study subjects recruited from DTCSH having 350 patients = 364*350/2400 = 53.
Study subjects recruited from FHCSH having 700 patients = 364*700/2400 = 106.
Study subjects recruited from TGSH having 250 patients = 364*250/240 = 38.
Variables of the study
The dependent variable was Drug-related problems among thyroid disorder patients on treatments. Independent variables were socio-demographic characteristics, source of the drug, level of education, social drug use, clinical characteristics, duration of thyroid disease, presence of co-morbidity, number of comorbidities, class and number of prescribed drugs, laboratory value, and availability of the drug.
Operational definitions
Drug-related problem: based on Cipolle et al. 2012, DRP is an undesirable event experienced by the patient that involves or is suspected to involve drug therapy and that actually or potentially interferes with desired health outcomes.
Medication adherence: This is the extent to which patients take medications according to the physician prescribed22. In different medical literature, the term “adherence” has replaced the term “compliance”. It reflects a patient-centered center rather than patients unilaterally following physicians’ instructions.
Non-adherence: When individuals do not take their medications as prescribed, it is unfavorably merely widespread.
Substance use history: refers to using khat, cigarettes, and tobacco within 3 months23.
Co-morbidity: indicates the existence of two or more diseases24.
Poly-pharmacy: Is recognized as the use of five or more medications25.
Adverse drug reactions(ADRs): This is an unwanted or harmful reaction experienced following the administration of a drug or combination of drugs under normal conditions of use and is suspected to be related to the drug26.
Data collection procedures
Data was collected using a pretested structured questionnaire and data extraction format. The data collection tool was developed after reviewing published literature and from pharmaceutical care practice, the patient-centered approach27. The data abstraction format consists of the patient’s demographics and patient medication experience, diagnosis, disease duration, dosage regimen, ADRs, complications of thyroid disease, history of hospitalization, and laboratory results. Patients with evidence of circumstances or events related to drug therapy that actually or potentially interfere with desired health outcomes were considered to have DRP. DRPs and possible causes of DRPs were identified using the American Thyroid Association Guideline 2016 and Ethiopian Standard Treatment Guideline 2014. An up-to-date drug interaction checker was used to identify drug-drug interactions. Clinical pharmacists assessed the DRPs based on clinical judgment supported by updated evidence-based disease management guidelines and literature. The causes of DRPs and the type of intervention by pharmacists were also recorded.
The Naranjo ADR probability scale was used to assess the patient’s ADRs. The Naranjo criteria determine the likelihood that an adverse event is related to the treatment of drugs using a set of weighted questions that look at elements such as the relationship between drug use and the incidence of the event. The Naranjo asks for ADR using objective evidence. Drugs are evaluated individually for causality and points are deducted if another factor is involved in ADR28.
The Adherence in Chronic Diseases Scale (ACDS) was used to assess patient’s adherence status. The ACDS includes 7 questions with sets of 5 suggested answers to each question. The questions consider the behavior directly determining adherence (Questions 1–5), as well as the situations and views that may indirectly affect adherence (Questions 6 and 7). This tool must not only reflect the actual implementation of the treatment approach in terms of medication but also emphasize the variables that influence patient adherence. The results can help undertake activities aimed at improving the regularity of medication in clinical practice29.
Data quality control and data analysis
To ensure the quality of the data; training to data collectors was given and an English version of the data collection questionnaire was translated into Amharic and back-translated to English. A structured questionnaire was designed by reviewing different works of literature to include important variables. The data collection tool was pretested on 5%18 of participants who were not included in the analysis. The questionnaires were sent to two senior clinical pharmacists who are academician researchers and physicians for face validity and approval. The collected data was cleared, entered into epi data version 4.6, checked for correctness, and exported to STATA version 17 for analysis. Descriptive analysis was used to compute frequency, mean, and standard deviation (SD) for continuous variables and categorical data. Logistic regression analysis was conducted to identify the independent predictors of drug therapy problems. Independent variables having p-value < 0.2 in the bivariate logistic regression analysis were entered into multivariable logistic regression analysis to control the confounding effect. P-value < 0.05 was considered significant.
Results
Socio-demographic characteristics of the study participants
A total of 351 study participants were approached and more than half of them 300 (85.47%) were females. The study participants’ mean (± SD) age was 45.1 ± 0.74 years. Among the participants, 264 (75.21%) were married and 241 (68.66%) were living in a rural area. 259 (74.8%) of the study participants had no formal education. 249 (70.94%) of the participants were housewives and 30 (8.6%) were farmers. The majority of the study subjects 280 (89.17%) drink coffee and Almost all of the study participants 326 (93.41%) were living with their families (Table 1).
Clinical characteristics of the study participants
Most of the study participants were diagnosed with hyperthyroidism 318 (90.60%), of which were diagnosed with TMNG 186 (58.5%) followed by Graves’ Disease 28 (8.8%), and the rest 33 (9.40%) were diagnosed with hypothyroidism. Out of the study participants, 13 (3.7%) had a history of thyroidectomy. The median duration of treatment was 2 years and 57.3% of the study participants had treatment duration of 1 year or less. Of the total study participants, one–third of patients (33.33%) had comorbid conditions. The most common comorbid diseases were Hypertension 29(26.85%) followed by diabetes mellitus18 (16.67%) and 9(8.33%) (Table 2).
Prevalence of drug-related problems (DRPs)
In this study, the overall prevalence of DRP was 60.11%, (95%CI: 54.9–65.13). The most common DRPs were non-adherence (34.47%) followed by adverse drug reactions (17.2%) and Ineffective Drugs (8.2%).
Types of drug-related problems and possible causes
A total of 211 DRPs from 351 patients were screened with a mean (± SD) of 1.54± (0.046) DRPs per patient. More than one-third (34.5%) of patients were non-adherent to their medications. The most common cause for non-adherence to medication was simply forgetfulness (36.56%) and the most common cause for the ineffective drug was that the prescribed drug was not available (60.71%) (Table 3).
Numbers of DRPs among the study participants
Over one-third of the study participants (33.10%) had at least one DRP. Two, three, and, no DRPs were reported from 21.10%, 5.90%, and 39.90% of the participants respectively.
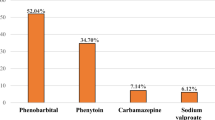
Prescribed medications at the ambulatory clinic of thyroid disorder patients
In the current study, the median number of medications prescribed per patient was two (2.0). Propylthiouracils 318 (47.5%) were frequently prescribed drugs followed by propranolol 75 (11.2%) and levothyroxine 33 (4.9%).
Medications class involved in experiencing Drug-related problems
The most commonly involved medications class in experiencing DRPs were Thionamides (74.3%) followed by Levothyroxine (34%) and other medications (9.9%) were attributed to experiencing DRPs. Non-adherence, ADR, and Ineffective drug categories of DRPs were mainly encountered in those patients who were on Thionamides, Levothyroxine, and others respectively.
Factors associated with the occurrence of DRPs
The findings from multivariate logistic regression showed a significant association between DRPs and Four independent variables (Age, Polypharmacy, Comorbidity, and purchasing medications in the private pharmacy). Accordingly, patients who are above 60 years of age were 2.85 times more likely to have DRPs than those who are less than 40 years of age [AOR = 2.85 CI: 1.05–7.69, P = 0.039]. Those who have poly-pharmacy were 2.57 times more likely to experience DRPs than those who have not poly-pharmacy [AOR = 2.57, 95%CI: (1.01–6.29), P = 0.046]. Meanwhile, those who have comorbid disease are 2.09 times more likely to have DRPs than those who did not have comorbidity [AOR = 2.09, 95% CI: (1.07–4.05), P = 0.030]. On the other hand, those who purchase medication in a private pharmacy are 2.62 times more experienced DRPs than those who purchase medication from a government pharmacy [AOR = 2.62,95%CI: (1.06–6.49), P = 0.038] (Table 4).
Discussion
This is a multi-centered cross-sectional observational study to identify the prevalence of DRPs and associated factors among adult thyroid disease patients in Northwest Ethiopia. Drug-related problems are becoming a major health concern30. Due to several comorbidities and the complexity of drug regimens, thyroid disorder patients are more at risk of developing DRPs. Therefore Identification and resolution Of DRPS in this population is decisive.
In our study, the mean age was 45.1 ± 0.74 years with females (85.47%) and rural dwellers (68.66%) dominance. This finding was also supported by different studies that revealed the higher magnitude of the disease among middle-aged, females, and rural dwellers living in iodine-deficient areas3,31. The female-to-male ratio of the study participants with thyroid disease was 5.8:1 and cardiovascular complications of thyrotoxicosis, namely heart failure and atrial fibrillation, were the most common comorbid disease. Which are similar to studies conducted in Nigeria and Kenya18,32. This study revealed that the most prevalent thyroid disorder was hyperthyroidism which is in line with studies conducted in Jimma33and Addis Ababa34. The present study revealed that propranolol was mostly used for the control of symptoms of hyperthyroidism which agreed with the findings of a study in Europe35.
The current study revealed that the overall prevalence of DRPs in the study subjects was 60.11%. This result is comparable with the study conducted by European Community Pharmacists on drug therapy problems in patients discharged from hospital, which was 63.7%36but lower than the study conducted in Kenya(87%)18, Minnesota (77%) and Australia (90%). The possible reason for this discrepancy might be the difference in pharmaceutical care practice, professionals working in the area, and their awareness of identifying and resolving DRPs and the availability of drugs37.
The present study revealed that the most prevalent DRP was nonadherence, the overall adherence was 65.53% adherent and 34.47% of non-adherence. This finding is in line with the study conducted in Kenya 38%18lower than the adherence rate conducted in Lebanon (54.9%)38. But this finding is higher than the studies conducted in Manchester United of which adherence was 22% this might be the difference in study design they used a Randomized controlled trial39and the difference in the tools they used as well as the difference of the sociodemographic characteristics of the study participants.
The current study showed that ADR was the second most prevalent DRP (17.2%). This finding is higher than the study done in Kenya which was (2.4%)18. The possible reason might be the difference of the drugs they used for hyperthyroidism of which they used Carbimazole.
In this study, the ineffective drug use category of DRPs identified was the third most prevalent DRPs (8.2%). This finding is higher than the study conducted in Kenya which was 1.2%18. This might be due to the non-availability of the Thionamides especially Carbimazole and Methimazole in the study area other than PTU. On the other hand, a Dose too high was the other prevalent DRP (7.9%) among the study participants in this study. This finding is in line with the study done in Kenya which was 3.5%18.
In this study, PTU was the only Thionamide used to treat hyperthyroidism but studies in Kenya showed carbimazole is used for the management of hyperthyroidism18. This discrepancy might be the difference in the availability of Antithyroid drugs. This finding is similar to the study done in Addis Ababa, Ethiopia where almost all of the patients received PTU for the management of thyrotoxicosis40. This finding contradicts a survey done by members of the Endocrine Society (ES), American Thyroid Association (ATA), and American Association of Clinical Endocrinologists (AACE) where the most commonly used drug was Methimazole (83.5% of cases) while the use of PTU was limited to 2.7%40,41. Methimazole has become more popular in the industrialized world due to its high rate of free T4 normalization and fewer adverse effects. However, in developing countries like Ethiopia, Methimazole is not available and almost all Hyperthyroidism patients are treated with PTU40. Methimazole is currently recommended as the first-line anti-thyroid medication, except for pregnancy, while PTU is the treatment of choice because of rare reports of birth defects related to Methimazole32,42. Whereas hypothyroidism is treated by thyroxin similar to other studies8. Most of the study participants (78.1%) were on propranolol.
This study revealed that the most commonly involved medication class in experiencing DRPs was Thionamides (Propylthiouracil) (74.3%). Non-adherence, ADR, and Ineffective drug categories of DRPs were mainly encountered in those patients who were on Thionamides. This finding was not similar to studies conducted in Kenya in which levothyroxine was the most common medication class in experiencing non-adherence, needing additional drug therapy, and dose to low category of DRPs18. It might be due to the difference in the type of Thionamide drugs being used that leads to ADR and decreases patient adherence as PTU is more frequently administered than carbimazole and physician’s consideration of weight-based dosing especially patients on levothyroxine. The current study revealed that the overall prevalence of DDI was 19.9%. This finding is higher than the study done in Kenya (12.9%)18. It might be due to the difference in the type of Thionamide drugs being used that is Propylthiouracil leads to Drug-drug interaction (DDI).
The results obtained from multivariate logistic regression indicated that Age, comorbidity, polypharmacy, and purchasing medication in private pharmacies were significantly associated with the occurrence of Drug-related problems (DRP). Patients who were above 60 years of age were about 2.85 times more likely to develop drug-related problems compared to patients who were 18–40 years of age. The highest risk of DRPs in above 60 years of age might be due to the inadequacy of medical follow-up due to shortage of income and high health care related costs as with increasing age the patient develops comorbid diseases, generally in the elderly, the tendency to acquire multiple and chronic diseases led to have DRPs25. The other possible reasons might be medication instruction is not appropriately acquired in older patients, which leads to poor understanding of the instruction of the medication usage and the fear of disbelief in the medication’s effectiveness which leads to non-adherence to the medication.
Patients who had Polypharmacy were found to be 2.57 times more likely to have DRPs than those who had no polypharmacy. This might be due to regimen complexity and Polypharmacy is often associated with multiple comorbidities, and increasing age was found to be the independent predictor of adverse drug reactions (ADRs)25. The finding of this study showed a clear association between the number of comorbidities and DRPs among thyroid disease patients like a study done in Nigeria32. Patients who had comorbid disease were 2.09 times more likely to have DRPs than those who had no comorbid disease. The possible reason might be due to the increase in the number and complexity of medications for treating the comorbid condition, which may lead to exposure to the medication’s adverse effects. The adverse drug reactions of Antithyroid drugs can lead to drug-related consequences. Individuals with thyroid disorders are particularly vulnerable to drug-related problems (DRPs) because of their adverse drug reactions, which are taken over long periods.
Patients who get their medication in a private pharmacy were 2.62 times more likely to have DRPs than those who get medications from a government pharmacy. The possible reason might be due to the non-availability of the Antihyroid drugs from the government pharmacy which leads the patient to get their medication from the private pharmacy which increases the cost of medication, which finally results in the patient losing to take their medication. In addition, the low-income status of patients who live in rural areas cannot afford to buy medications in the private pharmacy which leads the patient to develop DRPs.
Strengths and limitations of the study
The fact that this study is multicenter, which improves the data’s generalizability, is one of its advantages.
The current study is limited by its shorter study time and cross-sectional design, which may introduce biases. Additionally, the outcome of the intervention remains unknown.
Conclusion
The prevalence of drug-related problems among adult thyroid disease patients who had follow up at ambulatory clinics was 60.11%. The most commonly involved medication class in experiencing DRPs was Thionamides. Non-adherence, ADR, and Ineffective drug categories of DRPs were mainly encountered in those patients who were on Thionamides. Age, poly-pharmacy, comorbidity, and purchasing medication in private pharmacies were independent predictors of DRPs.
Data availability
Data will be available based on reasonable request of corresponding author.
Abbreviations
- ADE:
-
Adverse Drug Event
- ADR:
-
Adverse Drug Reaction
- ACDS:
-
Adherence for Chronic Disease Scale
- ATA:
-
American Thyroid Association
- ATD:
-
Anti Thyroid Drugs
- CBHI:
-
Community-based health insurance
- CMHS:
-
College of Medicine and Health Science
- DDI:
-
Drug-Drug Interaction
- DRP:
-
Drug Therapy Problem
- DRP:
-
Drug Related Problem
- DMCSH:
-
Debre Markos Comprehensive and Specialized Hospital
- DTCSH:
-
Debre Tabor Comprehensive and Specialized Hospital
- FHCSH :
-
Felegehiwot Comprehensive and Specialized Hospital
- PCNE:
-
Pharmaceutical Care Network Europe
- PPI :
-
Protein pump Inhibitor
- TGCSH:
-
Tibebe Ghion Comprehensive and Specialized Hospital
- UoGCSH :
-
University of Gondar Comprehensive and Specialized Hospital
References
Khan, A. Thyroid disorders, ethiology and prevalence Journal of medical sciences. (2002).
Ogbera, A. O. & Kuku, S. F. Epidemiology of thyroid diseases in Africa. Indian J. Endocrinol. Metab. 15 (Suppl 2), S82–S88 (2011).
Toyib, S., Kabeta, T., Dendir, G., Bariso, M. & Reta, W. Prevalence, clinical presentation and patterns of thyroid disorders among anterior neck mass patients visiting Jimma Medical Center, Southwest Ethiopia. Biomed. J. Sci. Tech. Res. 18 (2), 13431–13435 (2019).
Krotkiewski, M. J. Thyroid hormones in the pathogenesis and treatment of obesity. Eur. J. Op. 440(2–3), 85–98 (2002).
Europe, P. C. N. PCNE Classification for drug-related problems V5. 01. (2017).
Mil, F. V., Harvat, N. & Westerlund, T. Classification for Drug Related Problems V8. 02 (Pharmaceutical Care Network Europe Foundation, 2017).
Nascimento, Y. A. Carvalho WdS, Acurcio FdA. Drug-related problems observed in a pharmaceutical care service, Belo Horizonte, Brazil. Brazilian J. Pharm. Sci. 45, 321–330 (2009).
Gaitonde, D. Y., Rowley, K. D. & Sweeney, L. B. Hypothyroidism: an update. South. Afr. Family Pract. 54 (5), 384–390 (2012).
Taylor, P. N. & Vaidya, B. Side effects of anti-thyroid drugs and their impact on the choice of treatment for thyrotoxicosis in pregnancy. Eur. Thyroid J. 1 (3), 176–185 (2012).
Bp Sk, Dahal, P., Venkataraman, R. & Fuloria, P. Assessment of clinical pharmacist intervention in Tertiary Care Teaching Hospital of Southern India. Asian J. Pharm. Clin. Res. 6 (2), 258–261 (2013).
Cipolle, R. J., Strand, L. M. & Morley, P. C. Pharmaceutical care practice: the patient-centered approach to medication management services. (No Title). (2012).
Guignard, B. et al. (eds) Drug-related problems in a general internal medicine service. International Journal of Clinical Pharmacy; 2013: Springer Van Godewijckstraat 30, 3311 Gz Dordrecht, Netherlands.
Nivya, K., Sri Sai Kiran, V., Ragoo, N., Jayaprakash, B. & Sonal Sekhar, M. Systemic review on drug related hospital admissions - a pubmed based search. Saudi Pharm. J. 23 (1), 1–8 (2015).
Scholten BMaW. The world medicines situation 2011 access to controlled medicines. (2011).
Bekele, F., Tsegaye, T., Negash, E. & Fekadu, G. Magnitude and determinants of drug-related problems among patients admitted to medical wards of southwestern Ethiopian hospitals: a multicenter prospective observational study. PLoS One. 16 (3), e0248575 (2021).
Dn, O. & Fa, N. The Disease Burden and the extent of drug therapy problems in an Underserved Minority Population receiving medication Therapy Management at an Ambulatory Care Free Clinic. J. Pharm. Care Health Syst. 3(2), (2016).
Lagnaoui, R., Moore, N., Fach, J., Longy-Boursier, M. & Begaud, B. Adverse drug reactions in a department of systemic diseases-oriented internal medicine: prevalence, incidence, direct costs and avoidability. Eur. J. Clin. Pharmacol. 56 (2), 181–186 (2000).
Kamau, S. K. Drug Therapy Problems among Patients with Thyroid Disorders in Kenyatta National (university of Nairobi, 2020).
Yusuff, K. B. & Tayo, F. Frequency, types and severity of medication use-related problems among medical outpatients in Nigeria. Int. J. Clin. Pharm. 33(3), 558–564 (2011).
EFDA. Pharmaceutical products Traceability Master Data Guideline. March, 1–5 (2021).
Pourhoseingholi, M. A., Vahedi, M. & Rahimzadeh, M. Sample size calculation in medical studies. Gastroenterol. Hepatol. bed Bench. 6 (1), 14 (2013).
Kumar, R. & Shaukat, F. Adherence to levothyroxine tablet in patients with hypothyroidism. Cureus;11(5). (2019).
Group, W. A. W. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. 1183–1194. (2002).
Jaafar, A. F., Heycock, R. & George, J. Frailty–a clinical overview. Reviews Clin. Gerontol. 17 (3), 171–175 (2007).
Rahmawati, F., Pramantara, D. P., Rohmah, W. & Sulaiman, S. A. S. Polypharmacy and unnecessary drug therapy on geriatric hospitalized patients in yogyakarta hospitals, Indonesia. Int. J. Pharm. Pharm. Sci. 1 (1), 6–11 (2009).
Basger, B. J., Moles, R. J. & Chen, T. F. Development of an aggregated system for classifying causes of drug-related problems. Ann. Pharmacother. 49 (4), 405–418 (2015).
Cipolle, R. J., Strand, L. M. & Morley, P. C. Pharmaceutical care Practice: The patient-centered Approach to Medication Management (McGraw Hill Professional, 2012).
Kose, S., Akin, E. & Cetin, M. Adverse drug reactions and causality: the Turkish version of Naranjo adverse drug reactions probability scale. Psychiatry Clin. Psychopharmacol. 27 (2), 205–206 (2017).
Kubica, A. et al. The adherence in chronic diseases Scale—a new tool to monitor implementation of a treatment plan. Folia Cardiol. 12 (1), 19–26 (2017).
Garin, N. et al. Drug related problems in clinical practice: a cross-sectional study on their prevalence, risk factors and associated pharmaceutical interventions. Sci. Rep. 11 (1), 883 (2021).
Tekle, H. A., Bobe, T. M., Tufa, E. G. & Solomon, F. B. Age-sex disparities and sub-clinical hypothyroidism among patients in Tikur Anbesa Specialized Hospital, Addis Ababa, Ethiopia. J. Health Popul. Nutr. 37 (1), 1–7 (2018).
Ogbera, A., Fasanmade, O. & Adediran, O. Pattern of thyroid disorders in the southwestern region of Nigeria. (2007).
Reta Demissie, W. Prevalence Clinical presentation and patterns of thyroid disorders among Anterior Neck Mass patients visiting Jimma Medical Center, Southwest Ethiopia. Biomedical J. Sci. Tech. Res. 18(2). (2019).
Dawit Kebede. Thyroid diseases in Endocrine Referral Clinic in Tikur Anbessa Specialized Tertiary Hospital in AddisAbaba Ethiopia,2012. Ethiop. Med. J. 50. (2012).
Henderson, J., Portmann, L., Van Melle, G., Haller, E. & Ghika, J. Propranolol as an adjunct therapy for hyperthyroid tremor. Eur. Neurol. 37 (3), 182–185 (1997).
Paulino, E. I., Bouvy, M. L., Gastelurrutia, M. A., Guerreiro, M. & Buurma, H. Drug related problems identified by European community pharmacists in patients discharged from hospital. Pharm. World Sci. 26 (6), 353–360 (2004).
Rao, D., Gilbert, A., Strand, L. M. & Cipolle, R. J. Drug Therapy Problems Found in Ambulatory Patient Populations in Minnesota and South Australia29647–654 (Pharmacy World & Science, 2007). 6.
El Helou, S. et al. Adherence to levothyroxine among patients with hypothyroidism in Lebanon. EMHJ 25, 3–2019 (2019).
Crilly, M. A. Thyroxine Adherence Study: Impact of an Educational Booklet on Thyroxine Adherence in Patients with Primary Hypothyroidism. A Randomised Controlled Clinical Trial in Primary care (The University of Manchester (United Kingdom), 2003).
Dawit Kebede, M., Zinahbezu Abay, M., Yeweyenhareg Feleke, M. & Pattern Clinical Presentations and Management of Thyroid Diseases in National Endocrine Referral Clinics, Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Ethiopian Medical Journal 294, 2012.
Association, A. T. et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid 21 (6), 593–646 (2011).
Woeber, K. A. Update on the management of hyperthyroidism and hypothyroidism. Arch. Intern. Med. 160 (8), 1067–1071 (2000).
Acknowledgements
The authors would like to thank all the pharmacists who participated in the data collection and we would like to extend our sincere thanks to all research participant.
Author information
Authors and Affiliations
Contributions
F.N.D, S.A.W, S.B.D, and T.A.M designed the study, analyzed the data, and drafted the manuscript Participated in formal analysis, wrote the main manuscript, and G.B.M and M.E.M participated in the designing of the study and critically reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was ethically approved by the institutional review board of the University of Gondar with reference number 122/2014. This study was done complying with the declaration of Helsinki. Participants gave informed consent to participate in the study before taking part. Then, permission was confirmed from the selected hospitals to proceed with the study. Participants were asked for written forms after the objectives of the study were briefed. They were conditioned to give consent, and after accessing it they were interviewed.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dagnew, F.N., Wondm, S.A., Mengistu, M.E. et al. Drug related problems and associated factors among thyroid disorder patients in Northwest Ethiopia. Sci Rep 15, 27132 (2025). https://doi.org/10.1038/s41598-025-86293-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-86293-4